Abstract
Arthritis of the hip is a degenerative disease characterised by pain and inflammation. It is common and most often affects middle-aged to older adults, with the definitive management being total hip replacement. Advances in the surgical techniques has brought about the popularity of hip preservation surgery in patients with pre-arthritic hip abnormalities, with a goal to prevent progression to early arthritis and subsequently prolong the need for arthroplasty.
There is a large body of evidence correlating femoroacetabular impingement (FAI) and the progression of osteoarthritis. Hip arthroscopy is a successful technique in the management of FAI and labral damage. There is, however, less evidence behind its use in those patients with established arthritic changes.
After review of such evidence, we believe hip arthroscopy, and other hip preservation procedures, have a key role, and should be considered in the management of early hip arthritis. However, there is no role for such procedures in end-stage arthritis.
Keywords: Hip arthroscopy, Hip preservation surgery, Osteoarthritis, Femoroacetabular, Impingement
1. Introduction
Arthritis of the hip joint is a common disease characterised by pain and inflammation. It is degenerative in nature and most commonly affects middle-aged to older adults.
Arthroscopic hip surgery has gradually increased in popularity over the last 20 years. Newer indications include arthroscopic hip irrigation and debridement for septic/Rheumatoid arthritis, Perthes disease and other degenerative conditions which is now considered safe and effective treatment option for selected patients.1
Advances in technique, skills and instrumentation have led to expansion of indication and application of arthroscopy to include hip joint. There has been increasing interest and advances in arthroscopy of the hip with significant improvements in clinical outcome.2 Holgersson et al. described the use of hip arthroscopy in Juvenile Chronic Arthritis as early as 1981, over the years the target population has grown.3 Recent data has proven the role of arthroscopic synovium debridement in inflammatory arthropathies (rheumatoid/psoriatic/ankylosing spondylitic) patients, with significant improvement in outcome scores post-operatively.4
The goal of hip arthroscopy in young athletes has evolved with an aim to repair damaged tissue and improve biomechanics of the joint by removing areas of impingement, hence allowing them to get back to the same level of activity with good outcomes.5 Hip arthroscopy also appears to be a safe and efficacious treatment for labral tears and femoroacetabular impingement (FAI) in older patients who do not have significant underlying degenerative changes.6
At the other end of the spectrum, Total Hip Replacement (THR) remains to be one of the most successful and cost-effective interventions in medicine.7 There are, though associated risks of revision surgery in younger patients.
It is important to appreciate though, that most patients with end-stage arthritis of the hip, who require arthroplasty, will start with a condition where hip preservation surgery, such as hip arthroscopy may not only provide symptomatic relief but also delay the need for definitive arthroplasty surgery. The timing for such an intervention remains challenging.
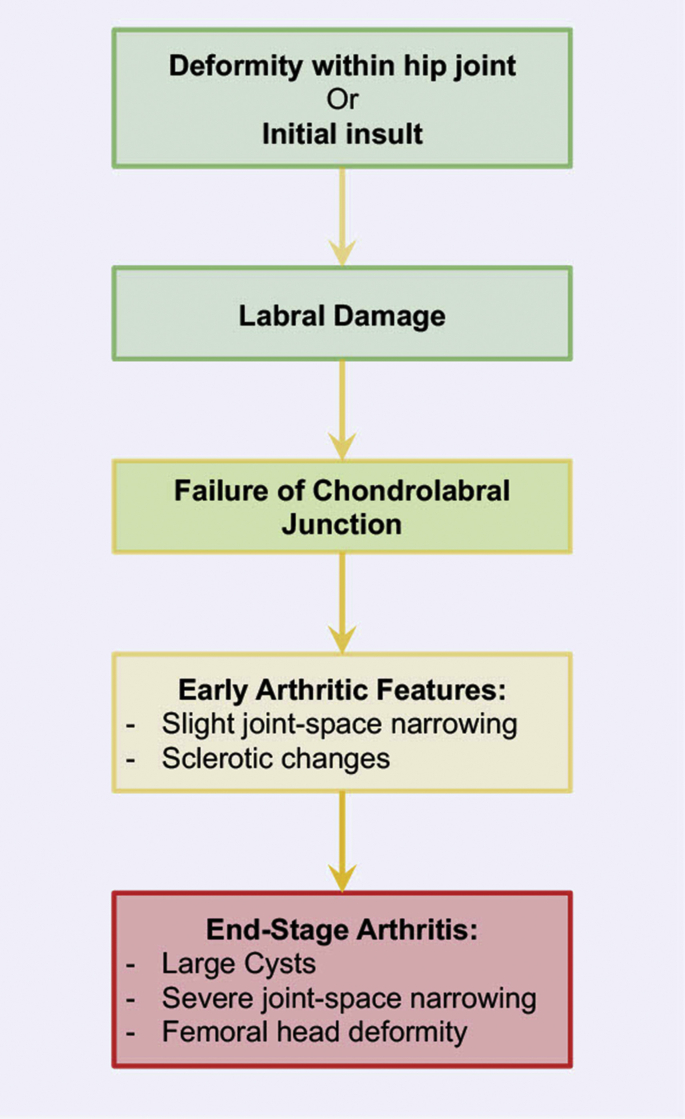
We believe that progression to end-stage arthritis maybe outlined in Fig. 1.
Fig. 1.
Flow-chart outlining the progression to End-Stage Arthritis.
2. Biomechanical pathology of hip arthritis
Most hip conditions start in childhood either in the form of Legg-Calve-Perthes disease and Slipped Upper Femoral Epiphysis (SUFE) with consequent femoral head deformity and impingement or hip dysplasia (established or borderline) and instability that leads chronic, persistent chondro-labral damage.
In both scenarios the common denominator remains repeated and persistent injury to articular and/or labral cartilage. Wenger et al. found that labral tear was associated with an underlying deformity of hip in 87% of cases.8 Healing potential of this cartilage injury is debatable and hence in due course osteo-arthritis sets in leading to end stage arthritis. The only option, then is an ‘amputation’ of the hip joint and prosthetic replacement.
Hip preservation surgery is still in its infancy, but we believe that there are several opportunities from the start of development of a hip deformity to the stage of established osteo-arthritis. Early intervention may well stop the progression to irreversible changes in articular cartilage and delay the need of arthroplasty.
This principle is well established in knee arthritis, where deformity correction with high tibial osteotomy has even shown regeneration of the articular cartilage.9 It is also well known that successful treatment of hip dysplasia in babies can delay the need for hip replacement by 45 years.10 It is therefore possible that if femoral head deformities, that lead to arthritic changes are corrected in good time, progression of arthritic changes may be interrupted and need for hip replacement delayed.
3. Current issue
Hip preservation procedures, such as arthroscopy, have increased exponentially in recent decades, with the possibility to postpone end-stage arthritis and subsequent need for arthroplasty.11,12
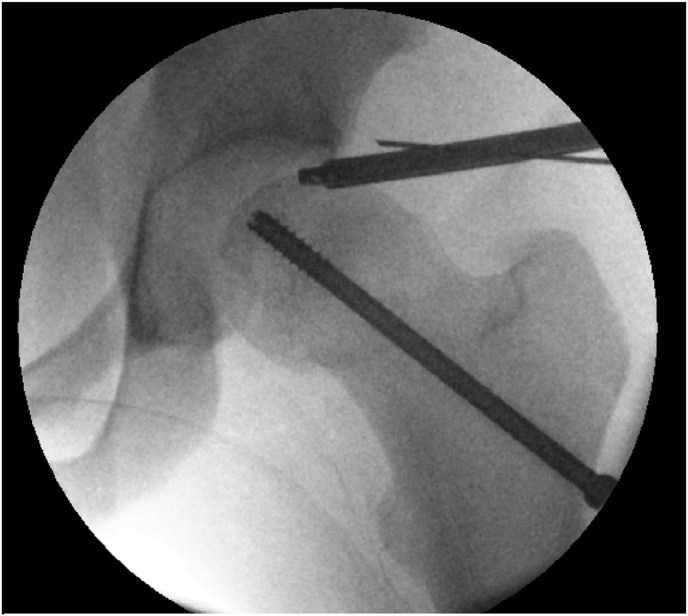
Arthroscopic findings – degenerate labral tear from the chondral junction, located superiorly and antero-superior. Impingement bump located anteriorly with the hip flexed 20°, 10° internally rotated and 10° externally rotated.
Arthroscopic management – Labral debridement and femoral osteochondroplasty.
Majority of young patients undergoing hip preservation surgery in recent years have underlying deformities of the hip, that include, but are not limited to, dysplasia, post-Perthes deformity and SUFE (Fig. 2). The deformity in these patients leads to a mismatch of the femoral head to the acetabulum, biomechanical alterations and can result in damage to labral/articular cartilage. Symptoms of groin pain, related to FAI, are a result of this damage. Cartilage damage may be prevented or halted, to delay hip arthritis by arthroscopic hip surgery, surgical dislocation of the hip and corrective pelvic or femoral osteotomies.
Fig. 2.
Left Hip arthroscopy being performed for patient with SUFE, previously managed with in-situ fixation. CAM deformity evident on this image.
4. FAI and hip osteoarthritis
With regards to FAI, there is a large body of evidence that supports the correlation between FAI and early OA,13 although there is some evidence to suggest that Pincer lesions can be protective for osteoarthritis (OA).14 In one radiological study, Bardakos et al. found 65% of patients progress to OA, with posterior wall sign and a reduction in medial proximal femoral angle to 81° being the most significant radiographic markers.15 Subsequently a systematic review by Viswanath et al. found that progressive abutment from CAM/Pincer deformities leads to a breakdown of the chondrolabral junction, and in reference to Fig. 1, we can see this can then progress to OA. They concluded that there is a correlation between an increased alpha angle >60° in FAI and OA.16
FAI leads to chondropathies that cause pain and limited functional activities affecting activities of daily living.17 In due course this ends in osteoarthritis. The treatment of these untreated chondral defects in the hip is still controversial and is evolving constantly.18 Several strategies have been attempted to restore large cartilage defects in the active patient, especially young adults including some with bilateral affection. Sobti et al. showed that biological reconstruction along with hip arthroscopy can bridge this osteoarthritis gap.19
We have used the same technique to apply osteochondral autologous transfers (OATs) for reconstruction of large osteochondral defects in the femoral head defects. The donor cartilage is harvested from impingement zones and with no added morbidity. Medium term outcome is very encouraging but long term studies are awaited.
The question, whether hip arthroscopy for FAI can prevent the progression of OA, is difficult to answer at this moment in time due to limited high level evidence.
We know that a cohort of professional athlete without radiographic signs of OA, when treated early with arthroscopic hip surgery, are able to return to play at their pre-injury professional level, with a mean return-time of 3.8 months. Subsequent significant improvements, were also observed, in their modified Harris Hip Score (mHHS) and Hip Outcome Scores. There has also been a 10-year follow-up in recreational athletes suggesting hip arthroscopy has good long term outcomes with continued sporting activity and no evidence suggesting a deterioration in performance. However, it must be noted that there isn't necessarily evidence to suggest a decrease in progression of OA.5 We are, however, aware of the importance of specifically addressing the impingement lesions in our patients. Robertson et al. performed a systematic review which concluded that patients who underwent management of labral pathology without debridement of the impingement were left with persisting pain and dissatisfaction.20 A further study looked at a comparison of a control (no osteoplasty) with study group (osteoplasty performed) and although hip arthroscopy was noted to have a significant improvement in mHHS across both groups, the study group had a higher percentage of patients with excellent post-operative outcomes (83% vs 60%) and had a narrower range of post-op satisfaction with 13% fewer patients scoring poor outcomes. As well as this they noted a negative correlation between mHHS and age in the control group, but no such correlation in the study group, potentially suggesting a protective effect of osteochondroplasty with regards to development of OA.21
There is varying levels of evidence, with a heterogeneity across the studies when it comes to performing hip arthroscopy in patients with hip OA. Thinking back to the knee, when this was also a topic of conversation years back, the literature dismissed the use of arthroscopy for lavage and debridement of knee OA, but found there were potentially a small subset of clinical indications, mechanical derangement, in mild-to-moderate OA that could benefit from arthroscopy.2 Domb et al.’s systematic review found that 23% of patients with OA had a conversion to THR with a meant time of 23.1 months. This compares to the non-arthritic group of 8.3% conversion with a mean time of 26.1 months.
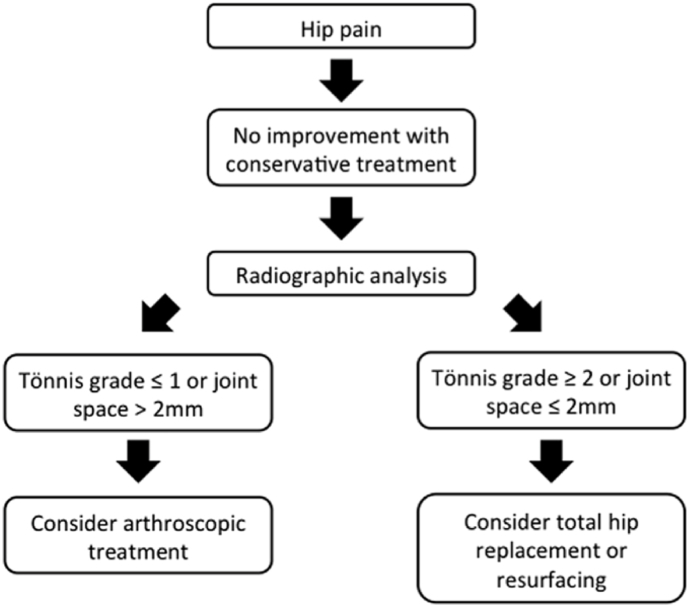
They therefore suggested a flow-diagram (Fig. 3) for management of hip pain and they recommend that if conservative measures failed there were two management options based on the level of OA. Patients with Tonnis Grade 1 or lower, or joint space with at least 2 mm, could be considered for hip arthroscopy; whilst those with Tonnis Grade 2 or more or less than 2 mm of joint space should be considered for arthroplasty or resurfacing.2 The most notable studies from their analysis included Larson et al. who found an 82% failure rate in advanced OA compared with 33% failure rate in moderate OA based on joint space narrowing.22 Meanwhile Kim et al. supported the previously described evidence on FAI, finding FAI present in 56% of patients with early stages of OA, compared with 29% of patients without OA. When looking at debridement of these patients, they had a satisfactory result in those patients with early OA. However, they did not have sufficient data with regards to FAI and ultimately concluded that patients with early OA and FAI would likely not benefit from hip arthroscopy.23
Fig. 3.
Flow diagram created by Domb et al. – ‘Proposed algorithm for patient selection for hip arthroscopy using radiographic parameters as a guide.’.2
Byrd et al. published an observational study at 2 and10 years follow up of patient's undergoing hip arthroscopy. They found that older age, male gender and longer duration of symptoms were poor prognostic indicators. Within their cohort there were 4 patients with degenerative arthritis who underwent THR at an average of 12 months post arthroscopy, although, notably 3 of these patients had normal radiographic findings pre-op and their intraoperative arthroscopic images were the indicator for their eventual THR. When looking at chondral lesions they had a mean improvement in mHHS of 19 points, but this improved to 38 points when arthritic patients were excluded from the cohort. Radiographic evidence of subchondral sclerosis, erosions, joint space narrowing and osteophyte formation, were the main indicators for arthritis. Subset analysis of these patients confirms that 50% of them were noted to have an improvement of at least 10 points mHHS at 2 years, which was maintained at 5 years and eventually 79% of patients underwent THR by 10 years.24,25
McCormick et al. had previously found that age was more of a stronger predictor of outcome than focal arthritic changes.26 Meanwhile Griffin et al. performed a systematic review subclassifying patients into ages with outcomes suggestive of and age-related prognostic indicator; with a 2-year conversion to THR of 16% for 40–49years, 3% < 40 and 35% for 60–69 years.6 Within their analysis they noted that Tonnis grade 2 patients were 4 times more likely to convert to THR than grade 1 and patients with <2 mm joint space narrowing were nearly 10 times more likely to need a THR.27,28
5. Our experience
Below is a case series from our practice, of 2 patients who had previously been informed that they needed to undergo THR to resolve their hip problems, but instead were offered and proceeded with hip preservation surgery.
5.1. Case 1
A 47-year-old extremely active lady was referred in early 2014 for management of her increasing left hip pain following a left hip arthroscopy 1 year prior. She had a CAM resection and had Grade1/2 arthritic changes. Subsequently she underwent 4–5 unsuccessful hip injections alongside an extended course of physiotherapy.
She had groin pain which was worsened by sitting for extended periods of time or crossing her legs. On examination she had a full pain free range of motion to the right hip, with a comparable range of motion in the left hip but with significant pain at the extremes of range in all movements. Positive impingement signs to the left hip.
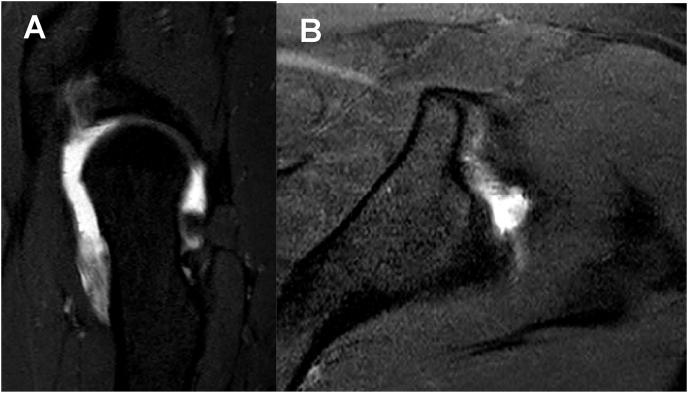
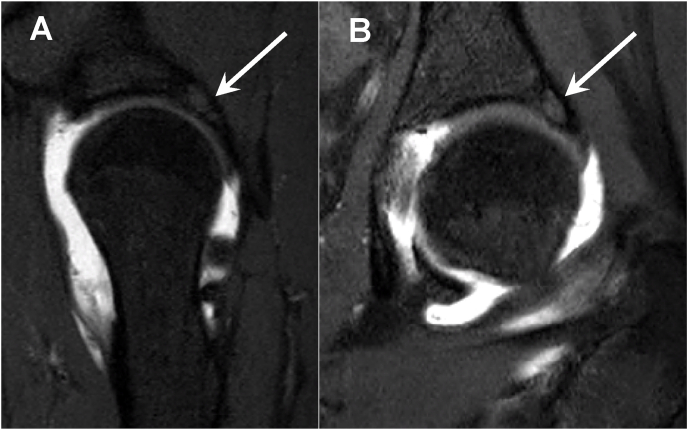
An up-to-date MR arthrogram of the left hip showed fraying and irregularity of the anterior acetabular labrum with seeping of contrast medium into this defect indicating a peripheral labral tear (Fig. 4). It also showed an area of bright signal intensity present in the posterior margin of the acetabular labrum representing subchondral geode (Fig. 5) indicating arthritic changes in the hip joint.
Fig. 4.
MR Arthrogram of Left Hip. (A) Sagittal STIR sequence and (B) Axial STIR sequence showing fraying and irregularity of acetabular labrum with infiltration of contrast.
Fig. 5.
MR Arthrogram of Left Hip. (A) Sagittal STIR sequence and (B) Coronal STIR sequence showing area of bright signal intensity to posterior margin of acetabular labrum representing subchondral geode, measuring 1.2 cm across.
The options discussed with the patient included to continue with non-operative management or to have a repeat arthroscopy. During the procedure she underwent a debridement of the labrum back to stable tissue, alongside acetabular microfracture and femoral osteochondroplasty. She had a complete resolution of symptoms and was able to return to her pre-morbid state with multiple half marathons being run.
Although she maintained her level of activity for a three-year period, developed some residual pain. A repeat MRI scan identified the presence of a loose body. The labrum was found to be intact. The case was discussed in multidisciplinary team meeting and decision for repeat arthroscopy to remove the loose body offered. This provided a further 3 year period of symptom relief and return to activities for the patient. Therefore this patient has had a 6 year period of delay in the need for THR.
5.2. Case 2
In 2014, a 24-year-old lady with a background of bilateral hip dysplasia, right side worse than left; who had previously undergone a right periacetabular osteotomy in 2011 and femoral derotation osteotomy in 2012, was seen in clinic with ongoing right hip pain. The pain was isolated deep to the groin and affected daily life. On examination she had reduced range of motion when compared to the contralateral side.
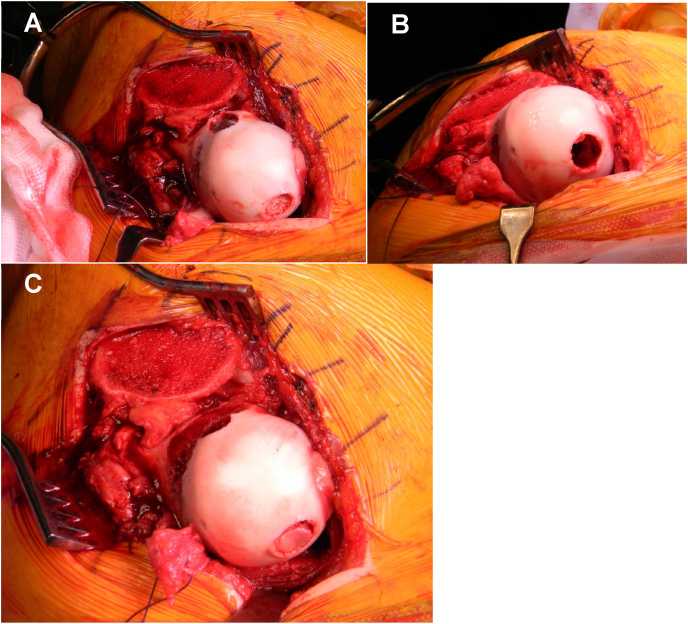
MR arthrogram of the right hip identified an area of 1 cm of cartilage loss to the femoral head. Given the MR findings the patient, who was keen to stave of THR, was offered surgery in the form of surgical dislocation of the hip with osteochondral autologous transfer (OATs). The defect was isolated to the superolateral aspect of the femoral head and the donor site was from the non-weight bearing area of the inferomedial aspect of the femoral head (Fig. 6).
Fig. 6.
Photographs of surgical hip dislocation procedure with OATs. (A) Dislocated femoral head showing 1 cm area of cartilage loss superolaterally, with donor site present inferomedially. (B) Recipient site post-curettage. (C) Successful transfer of bone from donor site to recipient site to fill the defect.
Postoperatively she managed well. Post-operative MRI confirmed that the recipient bone had integrated well and no further degenerative changes were noted. She had pains caused by irritation from the trochanteric screws, which were subsequently removed, and impingement from the anterior inferior iliac spine, which was subsequently debrided. Consequently, she progressed well following this for a few years before a return of progressive hip pain related to arthritic changes not amenable to hip preservation surgery. She is currently managing this with symptom control. Overall the OATs provided her with a reasonable period of 5–6 years benefit.
6. Conclusion
Pre-arthritic hip deformities and some early arthritic hips can be effectively managed with hip preservation options, either arthroscopic management of Cam/Pincer deformities or open reshaping of the femoral head.
We would agree with Domb et al. and Viswanath et al. in considering arthroscopic management of the hip in those patients with early OA stages such as Tonnis Grade 1 or less and if joint space is preserved by at least 2 mm. We believe in such patients with underlying deformities leading to FAI and labral injury, osteochondroplasty and labral repair/debridement has shown good benefit with symptomatic improvement and return to normal activities. Similar indications would be applicable to large femoral head deformities that could be corrected by safe surgical dislocation, femoral head reshaping (with or without cartilage transplantation), labral repair and trochanteric transfer.
However, hip arthroscopy does not have any role in the management of end-stage arthritis of the hip. This is well established and has been confirmed in a recent case of sports celebrity who required hip resurfacing with 18 months of hip arthroscopy.
Contributor Information
George W.V. Cross, Email: George.cross@nhs.net.
Anshul S. Sobti, Email: anshulsobti@nhs.net.
Tahir Khan, Email: tahir.khan5@nhs.net.
References
- 1.de Sa D., Cargnelli S., Catapano M. Efficacy of hip arthroscopy for the management of septic arthritis: a systematic review. Arthrosc J Arthrosc Relat Surg. 2015;31 doi: 10.1016/j.arthro.2014.12.028. [DOI] [PubMed] [Google Scholar]
- 2.Domb B., Gui C., Lodhia P. How much arthritis is too much for hip arthroscopy: a systematic review. Arthroscopy: the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2015;31(3):520–529. doi: 10.1016/j.arthro.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 3.Holgersson S., Brattström H., Mogensen B., Lidgren L. Arthroscopy of the hip in juvenile chronic arthritis. J Pediatr Orthop. 1981;1:273–278. doi: 10.1097/01241398-198111000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Zhou M., Li Z., Wang Y. Arthroscopic debridement and synovium resection for inflammatory hip arthritis. Chin Med Sci J. 2013;28(1):39–43. doi: 10.1016/s1001-9294(13)60017-6. [DOI] [PubMed] [Google Scholar]
- 5.Ellis H.B., Briggs K.K., Philippon M.J. Innovation in hip arthroscopy: is hip arthritis preventable in the athlete? Br J Sports Med. 2011;45(4):253–258. doi: 10.1136/bjsm.2010.082529. [DOI] [PubMed] [Google Scholar]
- 6.Griffin D.W., Kinnard M.J., Formby P.M., McCabe M.P., Anderson T.D. Outcomes of hip arthroscopy in the older adult: a systematic review of the literature. Am J Sports Med. 2017;45(8):1928–1936. doi: 10.1177/0363546516667915. [DOI] [PubMed] [Google Scholar]
- 7.Agency for Healthcare Research and Quality RMD HCUPnet, healthcare cost and utilization project. 2018. https://hcupnet.ahrq.gov/ Accessed.
- 8.Wenger D.E., Kendell K.R., Miner M.R., Trousdale R.T. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;426 doi: 10.1097/01.blo.0000136903.01368.20. https://journals.lww.com/clinorthop/Fulltext/2004/09000/Acetabular_Labral_Tears_Rarely_Occur_in_the.24.aspx [DOI] [PubMed] [Google Scholar]
- 9.Koshino T., Wada S., Ara Y., Saito T. Regeneration of degenerated articular cartilage after high tibial valgus osteotomy for medial compartmental osteoarthritis of the knee. Knee. 2003;10(3):229–236. doi: 10.1016/S0968-0160(03)00005-X. [DOI] [PubMed] [Google Scholar]
- 10.Thomas S.R., Wedge J.H., Salter R.B. Outcome at forty-five years after open reduction and innominate osteotomy for late-presenting developmental dislocation of the hip. JBJS. 2007;89(11) doi: 10.2106/JBJS.F.00857. https://journals.lww.com/jbjsjournal/Fulltext/2007/11000/Outcome_at_Forty_five_Years_After_Open_Reduction.3.aspx [DOI] [PubMed] [Google Scholar]
- 11.Bozic K.J., Chan V., Valone F.H., III, Feeley B.T., Vail T.P. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28(8):140–143. doi: 10.1016/j.arth.2013.02.039. [DOI] [PubMed] [Google Scholar]
- 12.Colvin A.C., Harrast J., Harner C. Trends in hip arthroscopy. JBJS. 2012;94(4) doi: 10.2106/JBJS.J.01886. https://journals.lww.com/jbjsjournal/Fulltext/2012/02150/Trends_in_Hip_Arthroscopy.16.aspx [DOI] [PubMed] [Google Scholar]
- 13.Kowalczuk M., Yeung M., Simunovic N., Ayeni O.R. Does femoroacetabular impingement contribute to the development of hip osteoarthritis? A systematic review. Sports Med Arthrosc Rev. 2015;23(4) doi: 10.1097/JSA.0000000000000091. https://journals.lww.com/sportsmedarthro/Fulltext/2015/12000/Does_Femoroacetabular_Impingement_Contribute_to.7.aspx [DOI] [PubMed] [Google Scholar]
- 14.Agricola R., Heijboer M., Roze R. Vol. 133. Osteoarthritis Research Society; 2013. Pincer deformity does not lead to osteoarthritis of the hip whereas acetabular dysplasia does: acetabular coverage and development of osteoarthritis in a nationwide prospective cohort study (CHECK). Osteoarthritis and cartilage/OARS. [DOI] [PubMed] [Google Scholar]
- 15.Bardakos N v, Villar R.N. Predictors of progression of osteoarthritis in femoroacetabular impingement. The Journal of Bone and Joint Surgery British. 2009;91-B(2):162–169. doi: 10.1302/0301-620X.91B2.21137. [DOI] [PubMed] [Google Scholar]
- 16.Viswanath A., Khanduja V. Can hip arthroscopy in the presence of arthritis delay the need for hip arthroplasty? Journal of hip preservation surgery. 2017;4(1):3–8. doi: 10.1093/jhps/hnw050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jannelli E., Fontana A. Arthroscopic treatment of chondral defects in the hip: AMIC, MACI, microfragmented adipose tissue transplantation (MATT) and other options. SICOT-J. 2017;3:43. doi: 10.1051/sicotj/2017029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Girolamo L., Jannelli E., Fioruzzi A., Fontana A. Acetabular chondral lesions associated with femoroacetabular impingement treated by autologous matrix-induced chondrogenesis or microfracture: a comparative study at 8-year follow-up. Arthroscopy. 2018;34(11):3012–3023. doi: 10.1016/j.arthro.2018.05.035. [DOI] [PubMed] [Google Scholar]
- 19.Sobti A.S., Baryeh K.W., Woolf R., Chana R. Autologous matrix-induced chondrogenesis and bone marrow aspirate concentrate compared with microfracture for arthroscopic treatment of femoroacetabular impingement and chondral lesions of the hip: bridging the osteoarthritis gap and facilitating enhanced recovery. Journal of hip preservation surgery. 2020;7(3):503–510. doi: 10.1093/jhps/hnaa047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robertson W.J., Kadrmas W.R., Kelly B.T. Arthroscopic management of labral tears in the hip: a systematic review. Clin Orthop Relat Res. 2007;455 doi: 10.1097/BLO.0b013e31802c7e0f. https://journals.lww.com/clinorthop/Fulltext/2007/02000/Arthroscopic_Management_of_Labral_Tears_in_the.15.aspx [DOI] [PubMed] [Google Scholar]
- 21.Bardakos N v, Vasconcelos J.C., Villar R.N. Early outcome of hip arthroscopy for femoroacetabular impingement. The Journal of Bone and Joint Surgery British. 2008;90-B(12):1570–1575. doi: 10.1302/0301-620X.90B12.21012. [DOI] [PubMed] [Google Scholar]
- 22.Larson C.M., Giveans M.R., Taylor M. Does arthroscopic FAI correction improve function with radiographic arthritis? Clin Orthop Relat Res. 2011;469(6):1667–1676. doi: 10.1007/s11999-010-1741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim K.-C., Hwang D.-S., Lee C.-H., Kwon S.-T. Influence of femoroacetabular impingement on results of hip arthroscopy in patients with early osteoarthritis. Clin Orthop Relat Res. 2007;456 doi: 10.1097/01.blo.0000246542.49574.2c. https://journals.lww.com/clinorthop/Fulltext/2007/03000/Influence_of_Femoroacetabular_Impingement_on.23.aspx [DOI] [PubMed] [Google Scholar]
- 24.Byrd J.W.T., Jones K. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy: the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2000;16:578–587. doi: 10.1053/jars.2000.7683. [DOI] [PubMed] [Google Scholar]
- 25.Byrd J.W., Jones K. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up (SS-57) Arthroscopy: the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2009;25:365–368. doi: 10.1016/j.arthro.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 26.Mccormick F., Nwachukwu B., Alpaugh K., Martin S. Predictors of hip arthroscopy outcomes for labral tears at minimum 2-year follow-up: the influence of age and arthritis. Arthroscopy: the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2012;28:1359–1364. doi: 10.1016/j.arthro.2012.04.059. [DOI] [PubMed] [Google Scholar]
- 27.Mardones R.M., Nemtala F., Tomic A. Arthroscopic treatment of femoroacetabular impingement in patients over 60 Years old: preliminary report of a pilot study. Cartilage. 2010;1(3):188–193. doi: 10.1177/1947603510364233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Philippon M., Souza B., Briggs K. Hip arthroscopy for femoroacetabular impingement in patients aged 50 Years or older. Arthroscopy: the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2012;28:59–65. doi: 10.1016/j.arthro.2011.07.004. [DOI] [PubMed] [Google Scholar]