Abstract
Objectives
This study evaluates the effectiveness of a mindfulness-based intervention (MBI), called Koru mindfulness, among college students.
Methods
Undergraduate students (N = 34) participated in a 4-week mindfulness curriculum embedded within a college course, while a control group (N = 35) taking a different course did not. Notably, the intervention coincided with the start of a state-wide lockdown due to the COVID-19 pandemic.
Results
Despite the additional external stress, there was a significant main effect and a significant interaction between the intervention and time for state mindfulness, (the treatment group experienced increased state mindfulness). There was a significant main effect (higher for the control group) on coronavirus worry and a significant interaction between the intervention and time for perceived stress, with the treatment/control group experiencing decreased/increased stress over time. There was also a significant interaction between the intervention and time for sleep problems with the intervention group experiencing declines in sleep problems over time and also being more likely to experience optimal amounts of sleep over time.
Conclusions
The Koru intervention effectively increased state mindfulness, decreased stress, and improved sleep, suggesting that it is robust even under extremely stressful conditions. This study adds to the growing evidence that MBIs can play an important role in addressing rising concerns regarding the mental health of college students.
Keywords: Koru mindfulness intervention, College students, Sleep, Stress, Pandemic, Coronavirus, Personality
Stress and its mental health implications are growing concerns in college campuses worldwide (Halladay et al., 2019). A recent national research survey found that students in the USA reported several factors impacting their academic performance in the last 12 months, with the top factors being stress (34.2%), anxiety (28%), sleep difficulties (22%), and depression (20%) (American College of Health Association, 2019, p. 5). Moreover, 24% of students reported having been diagnosed or treated within the last 12 months by a health professional for anxiety, 20% for depression, 12% for panic attacks, and 6% for insomnia (American College of Health Association, 2019, p. 15). Using data from the same research survey from 2009 to 2015, Oswalt et al. (2020) determined that college students’ mental health diagnoses have been growing over the years, with anxiety and panic attacks having the highest growth rate.
Several factors contribute to increased stress in college, including academic pressure, work/life balance, interpersonal relationship distress, financial challenges, and the transition from home to a more independent lifestyle (Freligh & Debb, 2019). Students’ inability to cope effectively with these stressors can increase the risk of substance abuse and lead to the onset of various mental health disorders, including anxiety, depression, and suicidal ideation (Bodenlos et al., 2013; Greeson et al., 2014). Poor coping with stress can also lead to lower levels of academic performance and engagement, lower graduation rates, higher likelihood of students dropping out of college or experiencing physical illness, and declines in mental, social, and emotional functioning (Amanvermez et al. 2020; Halladay et al., 2019).
One increasingly popular approach to combat the rise of mental health problems on college campuses is mindfulness-based interventions (MBIs). Mindfulness is a state of consciousness associated with paying attention to and being aware of what is happening in the present moment (Brown & Ryan, 2003). Mindfulness involves both self-regulation in order to stabilize attention to the immediate (bare) experience and the adoption of an orientation of one’s present-moment experience rooted in curiosity, openness, and acceptance (Bishop et al., 2004). Mindfulness practice supports decentering (defined as seeing thoughts and feelings as temporary and separate from oneself), emotion regulation, focused attention, decreased attachment/aversion to feelings, and decreased mental proliferation, all of which can lead to an increase in well-being and reductions in mental agitation (Grabovac et al., 2011; Hölzel et al., 2011).
Many studies have found that MBIs are associated with health and well-being benefits in the general population (Querstret et al., 2020). Although less common, several studies have investigated a variety of MBIs for college students, such as the well-known Mindfulness-Based Stress Reduction (MBSR), Acceptance and Commitment Therapy, and Mindfulness-Based Cognitive Therapy, as well as more specialized programs specifically targeting college students, such as Learning to BREATH (Dvořáková et al., 2017) and Koru mindfulness (Greeson et al., 2014); for an extensive list of such interventions, see Chiodelli et al. (2020) and Ma et al. (2019). Several meta-analyses and systematic reviews of MBIs for college students have found that they can reduce self-reported anxiety (Dawson et al., 2019), depressive symptoms (Huang et al., 2018; Ma et al., 2019), and perceived stress (Amanvermez et al., 2020; Halladay et al., 2019), as well as increase mindfulness (Bamber & Schneider, 2016). Bamber and Schneider (2016) theorized that MBIs immediately increase college students’ state mindfulness, which can decrease both stress and anxiety, and that with repetitive practice, state mindfulness can also increase trait mindfulness, which likewise reduces stress and anxiety. The evidence for the effect of MBIs on various sleep outcomes is somewhat more mixed with some studies reporting benefits while others reporting no change (Rusch et al., 2019; Winbush et al., 2007).
Even though the majority of studies have found MBIs to be beneficial for college students, the reported effect sizes on outcomes such as stress, anxiety, depression, and sleep have been inconsistent, ranging from small to large and depending on the specific outcome considered (Dawson et al., 2019). Moreover, some of the evidence is of lower quality due to the risk of study bias, publication bias, and small sample sizes (Halladay et al., 2019). Further research is needed to identify which MBIs are most effective for various college student populations (e.g., students of different majors or students diagnosed with a specific mental disorder). Further research is also needed to identify the ideal intervention dosage (number of sessions per week, number of weeks, duration of each practice session, expected amount of practice outside formal sessions), and ideal mode of delivery (on-line vs. in-person; Bamber & Schneider, 2016; Spijkerman et al., 2016). Currently, there is also ambiguity as to whether interventions tailored-made for college students may hold certain advantages over interventions developed for the general population. Prior work by Bamber and Schneider (2020) suggests that some college students may be ambivalent about MBIs, have anxiety/fear about meditation practice, or perceive lack of time as a barrier to continuing practice. Targeted MBIs may be more effective in reducing students’ ambivalence and addressing perceived college-related stressors and time barriers. In that vein, Bamber and Morpeth (2019) recently proposed that interventions that fit the needs of college students and minimize out-of-classroom practice should be further tested (see also Bamber & Schneider, 2020).
Koru is an MBI designed specifically to support the development of emerging adults. Only a handful of studies have evaluated the Koru program so far (Gonzalez-Voller et al., 2019; Gray et al., 2018; Greeson et al., 2014), yet the results have been encouraging and indicate that it warrants further investigation. Greeson et al. (2014) employed a randomized controlled trial (N = 90) to compare the effects of Koru training relative to the control group on college students. They found significant, medium-sized, group, and time (pre, post) interactions in perceived stress, sleep problems, and mindfulness. Gray et al. (2018) evaluated the Koru curriculum among undergraduate students that had aged out of foster care (N = 16) against a control group (N = 20) and found significant reductions in stress levels and improvements in sleep quality post intervention. Gonzalez-Voller et al. (2019) compared the effectiveness of a 5-h “all-in-one-day” mindfulness program with a modified 4-week Koru curriculum adapted for the needs of family caregivers (N = 12), and found that both programs experienced medium-sized effects of increased mindfulness and stress reduction, although the all-day participants experienced higher scores.
While Koru mindfulness is promising in improving various mental health outcomes for different student populations, it remains unclear how robust this intervention is under various scenarios, such as method of delivery (i.e., on-line, or course-embedded), or exceptionally stressful circumstances, such as a pandemic. The effects of personality traits, such as extraversion and neuroticism, have also not been examined in prior work in the context of the Koru program, even though they have all been linked to mindfulness (Giluk, 2009).
Our study examines the effectiveness and robustness of the Koru mindfulness curriculum, compared to a control group that did not receive the intervention. Unlike prior Koru studies, in which the intervention was evaluated as a stand-alone, in-person program, this study examines the effectiveness of the Koru program when delivered on-line, embedded within a full-semester course, and delivered under the stressful conditions of a pandemic lockdown. Recent studies attest that the COVID-19 pandemic and implied mandatory confinements have been challenging for college students, increasing their stress, anxiety, and depression (Cao et al., 2020; Debowska et al., 2020; Husky et al., 2020). The primary outcomes considered are perceived stress, sleep problems, sleep duration, and coronavirus worry, while the secondary outcome considered is state mindfulness. In addition, neuroticism and extraversion are introduced as control variables.
Method
Participants
A total of 70 college students enrolled in two different courses from a medium-sized, private, non-profit university in the northeast of the USA were invited to participate in a series of on-line surveys; the university serves about 4000 undergraduate and 1000 graduate students and is geared towards business education. To increase response rates, the majority of the surveys were conducted during class time, and, for the intervention group, mindfulness-based exercises were also assigned outside of class; for those reasons, students were eligible for a small grade adjustment (up to 2 points) for their participation. The students were equally divided across two business electives attracting students from various disciplines, including management, marketing, finance, and economics. The treatment group consisted of 35 students enrolled in a positive psychology–based management elective, while the control group also consisted of 35 students enrolled in another management elective. One observation was deleted from the treatment group sample due to several failed attention checks (5 out of the 6), bringing the final sample size to 69 students.
The sample included 27 females (39%) and 42 males (61%), which is fairly representative of the university’s student population; the treatment group had more males (25) relative to the control group (17). Twelve sophomores (17%), 39 juniors (57%), and 18 seniors (26%) participated in the study; this composition was similar for the two groups. The most common majors were management (53%), finance (10%), and marketing (9%); the control group had more management majors (24) compared to the treatment group (13). The majority of students (57 of them) identified as white (75%), while 8 students identified as Asian (12%), 2 students identified as African Americans (3%), and 7 students (10%) checked the “other” race category.
We conducted a power analysis with G*Power (Faul et al., 2007) using repeated measures analysis of variance (ANOVA), with the within-between interaction option, specifying a significance level of 0.05. We found that to detect a small effect (partial η2 = 0.02) at 0.80 power and 5 time points (since we measured both the control and treatment group five times), a sample size of 60 is required. Thus, our sample size of 69 was sufficient to detect a small effect.
Procedures
The study was approved by the Institutional Review Board (IRB) of the university (#01,242,030). All students were able to opt out of participation at the start of each survey, or exit the survey at any time without any penalty. The introductory statement of each on-line survey informed students that the survey will ask them to answer some questions about themselves, and no specific mention to mindfulness was made. Students in the management elective course (control group) received no intervention. The Koru curriculum was introduced to the treatment group in the middle of the semester. Notably, right before the Koru curriculum was introduced, concerns over rising infection rates in Massachusetts resulted in the governor declaring a state of emergency on March 10, 2020 (Office of Governor Charlie Baker & Lt. Governor Karyn Polito, 2020). As a result, all classes were delivered on-line for the remainder of the semester for both the control and treatment groups.
Intervention (reduce font size - this is sub-header under Procedure)
Koru differs from other mindfulness interventions in both its content and structure. In terms of structure, Koru is based on four weekly meetings of approximately 75 min each other college-based MBIs are either adaptations of MBSR programs, which typically run for 8 weeks, or programs of various lengths ranging from 2 to 24 weeks in length (Chiodelli et al., 2020; Ma et al., 2019). Students are expected to attend all four class sessions and are also encouraged to practice meditation for approximately 10 min a day for the duration of the program. In terms of content, each Koru session includes formal meditation practice as well as other mindfulness-based exercises such as breathing, visualization, mindful walking, and mindful eating; while other MBIs introduce some of these elements as well, no other program includes all of them in their prescribed sequence. Other unique features of the program include the use of a custom textbook, an accompanied mobile app, and the requirement for Koru certified instructors (in this study, the same Koru certified instructor taught both the intervention and control group courses). The accompanied textbook (Rogers, 2016) was specifically written for the Koru program and includes metaphors and stories aimed to resonate with college students and to help them learn how to more mindfully handle common concerns, such as academic pressures, roommate conflicts, skepticism about unfamiliar practices, overthinking, or worrying about exams and future career prospects. The Koru mobile app includes all the guided meditations and other practices introduced in class so that registered students can use the app to log their meditations and reflections, and get feedback, mentoring, and support from their instructor.
Surveys were distributed on-line across 6 different time periods: at the start of the semester in late January (Baseline 1 at T1), before the start of the spring break in late February (Baseline 2 at T2), at the end of weeks 2 to 4 of the Koru intervention, which span from mid-March to mid-April (T3 to T5), and 1 week after the end of the intervention in late April (T6). To avoid survey fatigue, we excluded the control group from one of the surveys (at time T4), while the control variables were measured only at time T1. During the spring break and before students in the treatment group were to start the Koru mindfulness intervention, the state governor ordered a lockdown to prevent the spread of the novel coronavirus. We thus decided to include in time periods T3 to T6 a measure of the degree of worry students may be experiencing about the pandemic and sought and received approval from the university’s IRB for this amendment to our survey questions. The state was still in lockdown in late April 2020, when we distributed the last survey (T6). A follow-up at a later time was deemed difficult given that students had already participated in 6 prior surveys, were already dispersed across the world due to the pandemic, and were busy finishing a difficult and unusual semester. All scales were rated by the focal participant.
Measures
State Mindfulness
We measured state mindfulness with the State Mindfulness Scale (SMS) because it was designed to reflect a conceptual model of mindfulness consistent with traditional Buddhist scholarship and has good discriminant and convergent validity (Tanay & Bernstein, 2013), and its conceptual model is consistent with the Koru curriculum. The SMS aims to quantify perceived levels of awareness of physical sensations (body) and mental events (mind). The scale typically invites participants to rate their perceived awareness level during a specific period of time (Ruimi et al., 2019). We instructed students to consider the last 15 min when answering the questions. The full SMS scale has 20 items, but to reduce survey time, we employed only the 10-item mind awareness subscale. Example questions for the mind subscale are the following: “I noticed pleasant and unpleasant thoughts” and “I was aware of different emotions that arose in me.” Participants rated items on a 5-point scale ranging from 1 (not at all) to 5 (very much). Our sample’s reliability (Cronbach’s alpha) ranged from a = 0.86 to 0.94 across the times it was measured (T1–T6).
Coronavirus Worry
We adapted four items from the 16-item Penn State Worry Questionnaire (Meyer et al., 1990). The scale has good reliability, and correlates with stress, anxiety, and depressive symptoms (Joos et al., 2012), but is generally considered an independent construct able to capture severe anxiety in individuals. We employed the following four adapted questions: “I noticed that I have been worrying about the coronavirus lately,” “Once I start worrying about the coronavirus, I cannot stop,” “I find it easy to dismiss worrisome thoughts about the coronavirus” (reversed), and “My thoughts about the coronavirus have increased my stress level.” Participants rated items on a 7-point scale ranging from 1 (strongly disagree) to 7 (strongly agree). Our sample’s reliability ranged from a = 0.82 to 0.88 (across times T3–T6). This variable was used as both an outcome and control variable.
Perceived Stress
We measured stress with 10 items from the perceived stress scale (PSS; Cohen et al., 1983). The scale has a 4-, 10-, and 14-item versions, with good convergent and discriminant validity (Roberti et al., 2006). Unlike the specific coronavirus worry scale we discussed earlier, the PSS focuses on a global appraisal of stress based on participants’ perceptions of the frequency with which they experience their lives as unpredictable, uncontrollable, or overloaded or dependent on events occurring in the lives of friends and relatives, or on expectations concerning future events. Example questions include “how often have you felt nervous and “stressed”?” and “how often have you been able to control irritations in your life?” Participants rated items on a 5-point scale ranging from 1 (never) to 5 (very often). Our sample’s reliability ranged from a = 0.77 to 0.89 across the times it was measured (T1–T6).
Sleep Problems and Duration
We utilized two sleep constructs: (a) sleep problems via the 9-item sleep problems index II scale (SLPII) and (b) the 1-item sleep quality/duration. Both scales are based on the Medical Outcome Sleep (MOS) questionnaire (Hays & Stewart, 1992), which includes 12 patient-reported, non-disease-specific questions that can be used to generate a number of different sleep scales. The MOS has been used extensively in various clinical applications and has also been shown to have good psychometric properties in the general US population (Hays et al., 2005). Example questions include “over the past week, did you feel that your sleep was not quiet (moving restlessly, feeling tense, speaking, etc., while sleeping)?” and “over the past week, did you get enough sleep to feel rested upon waking in the morning?” Participants rated items on a 6-point scale ranging from 1 (none of the time) to 6 (all of the time). Our sample’s reliability ranged from a = 0.77 to 0.89 across the times it was measured (T1–T6). Regarding sleep duration, we followed the scoring instructions of the MOS and transformed this variable into a binary outcome that reflects whether sleep was optimal (i.e., 7 or 8 h = 1) or not (i.e., 6 h or less and 9 h or more = 0).
Control Variables
We collected demographic information to control for participants’ class year, as well as gender given previous research suggesting women may possess greater mindfulness (Katz & Toner, 2013). We also collected race demographics and considered race as a control variable, but we ultimately chose not to include it since we did not have enough non-white participants to draw meaningful comparisons.
In addition, we measured the Big Five personality characteristics (i.e., Openness to Experience, Conscientiousness, Extraversion, Agreeableness, and Neuroticism). All the Big Five traits have been linked to mindfulness (Giluk, 2009). Previous research has also found neuroticism to be significantly associated with both mindfulness and stress (e.g., Drake et al., 2017), and neuroticism and extraversion to be negatively and positively associated with sleep quality, respectively (Stephan et al., 2018). We employed the 10-item short version of the Big Five Inventory (Rammstedt & John, 2007). We included three additional items for neuroticism from the Big Five 44-item inventory (John et al., 1991). Participants rated items on a 5-point scale ranging from 1 (strongly disagree) to 5 (strongly agree). Our sample’s reliability was acceptable for neuroticism at a = 0.78, and for extraversion at a = 0.72, but not for the other personality traits. We thus included only neuroticism and extraversion in our analysis.
We also controlled for trait mindfulness using the Mindful Attention Awareness Scale (MAAS). This scale measures individual differences in the frequency of mindful states over time. It aims to capture intraindividual variations of mindfulness, based on individuals’ inherent capabilities, discipline, self-regulation, or personality (Brown & Ryan, 2003). The MAAS allows us to control for between-person, trait effects of mindfulness. It is a 15-item scale and has good convergent and discriminant validity and good internal consistency (Brown & Ryan, 2003; Carlson & Brown, 2005). Items were rated on a 6-point scale ranging from 1 (almost always) to 6 (almost never). Example scale questions are “I rush through activities without being really attentive to them” and “I snack without being aware that I’m eating.” Our sample’s reliability for the MAAS was a = 0.86 (measures at time T1). We reverse-coded all items so that high scores reflect higher levels of mindfulness because the items on this scale are originally coded such that high scores reflect low mindfulness. Given that the MAAS is unidimensional, it is important to note previous scholars have critiqued this measure (Grossman, 2011; Van Dam et al., 2010) for failing to capture other features of mindfulness (Baer et al., 2006), such as acceptance (Sauer et al., 2013), by exclusively assessing inattention. Furthermore, a study with a large undergraduate student sample (N = 711) did not find any significant differences in mindfulness, as measured via MAAS, between novice meditators and those with no experience (MacKillop & Anderson, 2007). In any case, as stated in the “Results” section, a robustness check indicated that our findings were equivalent when controlling for or excluding the MAAS from the analyses (Tables 1 and 2).
Table 1.
Baseline group differences between control and treatment (Koru) group
| Control group | Koru group | |||||
|---|---|---|---|---|---|---|
| Time | M | SD | M | SD | t valuea | |
| Trait extraversion | T1 | 3.35 | 0.99 | 3.38 | 0.97 | − 0.10 |
| Trait neuroticism | T1 | 2.22 | 0.91 | 2.37 | 0.85 | − 0.69 |
| Trait mindfulness (MAAS) | T1 | 3.02 | 0.70 | 3.14 | 0.79 | − 0.63 |
| State mindfulness (SMS) | T2 | 3.30 | 0.73 | 3.48 | 0.76 | − 0.97 |
| Perceived stress | T2 | 2.62 | 0.53 | 2.54 | 0.49 | 0.64 |
| Sleep problems | T2 | 34.98 | 16.06 | 36.89 | 15.74 | − 0.49 |
| Sleep duration (h) | T2 | 6.90 | 1.34 | 6.97 | 0.78 | − 0.26 |
| Optimal Sleep | T2 | 0.57 | 0.50 | 0.62 | 0.49 | 0.15b |
N = 69. For optimal sleep N = 64
aIndependent samples t test
bChi-square test statistic (ns)
Table 2.
Descriptive statistics and bivariate (Pearson) correlations between study variables at time T1
| Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 Neuroticism | 2.30 | 0.87 | ||||||||
| 2 Extraversion | 3.37 | 0.97 | − .06 | |||||||
| 3 Coronavirus worry | 3.99 | 1.35 | .16 | .25 | ||||||
| 4 Trait mindfulness (MAAS) | 3.91 | 0.75 | − .40** | − .12 | .05 | |||||
| 5 State mindfulness (SMS) | 3.48 | 0.53 | − .16 | .13 | − .14 | .14 | ||||
| 6 Perceived stress | 2.63 | 0.46 | .55** | .04 | .58** | − .39** | − .50** | |||
| 7 Sleep Problems | 33.40+ | 15.74 | .40** | .14 | .44** | − .23 | − .22 | .55** | ||
| 8 Sleep Duration | 7.33++ | 1.03 | − .03 | − .13 | − .20 | .09 | .03 | − .35** | − .61** |
N = 64–69
**p < .01 two-tailed significance
+Scale recoded to be from 0 to 100 as per scoring instructions
++Units in hours of sleep
Data Analyses
We conducted the statistical analyses using SPSS version 27. Specifically, we used multilevel modeling where observations were nested within individuals (i.e., MIXED command). This analytic strategy has been found to produce more robust estimates than repeated measures ANOVA (Snijders & Bosker, 2011). We utilized restricted maximum likelihood estimation given our sample size (McNeish, 2017). We constructed two models for each dependent variable. First, in models denoted by “A” in Tables 3, 4, 5, and 6, we tested the main effect of the intervention on the outcome while simultaneously controlling for several variables, which we introduced above. Second, in models denoted by “B,” we added an interaction term between the intervention and time to examine the effect of the intervention over the course of the study. In both A and B models, we allow for random time slopes in addition to random intercepts. For significant interactions, we conducted follow-up simple slopes analyses using the on-line calculator published by Kristopher Preacher, Ph.D. (Preacher et al., 2006; see also http://www.quantpsy.org/interact/hlm2.htm). We used generalized estimating equations (GEE; Ballinger, 2004) to model within-person dependency and test our hypotheses related to the binary optimal sleep outcome. This analysis specified a binomial distribution with a logit link function.
Table 3.
Multilevel modeling results testing intervention effect on state mindfulness
| Model 1A | Model 1B | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient γ | SE | t value | 95% LL | 95% UL | Coefficient γ | SE | t value | 95% LL | 95% UL | ||
| Intercept | 3.26 | 0.16 | 19.75** | 2.93 | 3.59 | 3.34 | 0.17 | 19.74** | 3.00 | 3.67 | |
| Sophomorea | 0.22 | 0.20 | 1.09 | − 0.18 | 0.61 | 0.22 | 0.20 | 1.09 | − 0.18 | 0.61 | |
| Juniora | − 0.10 | 0.15 | − 0.66 | − 0.40 | 0.20 | − 0.10 | 0.15 | − 0.66 | − 0.40 | 0.20 | |
| Sex(male) | − 0.02 | 0.15 | − 0.10 | − 0.32 | 0.29 | − 0.01 | 0.15 | − 0.10 | − 0.32 | 0.29 | |
| Neuroticism | − 0.03 | 0.08 | − 0.34 | − 0.20 | 0.14 | − 0.03 | 0.08 | − 0.34 | − 0.20 | 0.14 | |
| Extraversion | 0.11 | 0.07 | 1.63 | − 0.03 | 0.25 | 0.11 | 0.07 | 1.63 | − 0.03 | 0.25 | |
| Trait mindfulness | 0.13 | 0.09 | 1.43 | − 0.05 | 0.32 | 0.13 | 0.09 | 1.43 | − 0.05 | 0.32 | |
| Coronavirus worry | − 0.08 | 0.06 | − 1.33 | − 0.21 | 0.04 | − 0.08 | 0.06 | − 1.34 | − 0.21 | 0.04 | |
| Time | 0.03 | 0.02 | 1.43 | − 0.01 | 0.06 | − 0.01 | 0.03 | − 0.44 | − 0.06 | 0.04 | |
| Intervention | 0.27 | 0.14 | 1.99ϯ | 0.00 | 0.55 | 0.12 | 0.16 | 0.76 | − 0.19 | 0.43 | |
| Intervention × time | 0.07 | 0.04 | 2.03* | 0.00 | 0.14 | ||||||
| − 2LL deviance | 648.3 | 649.1 | |||||||||
| Residual | 0.262 | 0.025 | 10.34** | 0.217 | 0.317 | 0.262 | 0.025 | 10.34** | 0.217 | 0.317 | |
| Intercept variance | 0.197 | 0.065 | 3.02** | 0.103 | 0.376 | 0.192 | 0.064 | 3.01** | 0.100 | 0.368 | |
| Slope variance | 0.005 | 0.004 | 1.25 | 0.001 | 0.023 | 0.004 | 0.004 | 1.05 | 0.001 | 0.025 | |
| Intercept-slope covariance | − 0.006 | 0.013 | − 0.50 | − 0.031 | 0.019 | − 0.004 | 0.012 | − 0.36 | − 0.028 | 0.020 | |
N = 69 (between subjects) and N = 355 (within subjects). LL/UL, lower/upper confidence interval limit
γ, multilevel regression coefficient; SE, standard error
Model 1A does not include the time × intervention coefficient, whereas Model 1B does
aReference group = senior
*p < .05; **p < .01; ϯp < .10
Table 4.
Multilevel modeling results testing intervention effect on coronavirus worry
| Model 2A | Model 2B | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient γ | SE | t value | 95% LL | 95% UL | Coefficient γ | SE | t value | 95% LL | 95% UL | |
| Intercept | 5.16 | 0.30 | 17.08** | 4.55 | 5.76 | 5.19 | 0.30 | 17.09** | 4.58 | 5.79 |
| Sophomorea | 0.21 | 0.40 | 0.51 | − 0.60 | 1.01 | 0.20 | 0.40 | 0.50 | − 0.60 | 1.01 |
| Juniora | − 0.43 | 0.30 | − 1.43 | − 1.03 | 0.17 | − 0.43 | 0.30 | − 1.43 | − 1.03 | 0.17 |
| Sex (male) | − 1.04 | 0.28 | − 3.73** | − 1.59 | − 0.48 | − 1.04 | 0.28 | − 3.75** | − 1.60 | − 0.48 |
| Neuroticism | 0.41 | 0.17 | 2.49* | 0.08 | 0.75 | 0.41 | 0.17 | 2.50* | 0.08 | 0.75 |
| Extraversion | 0.36 | 0.14 | 2.67* | 0.09 | 0.64 | 0.36 | 0.14 | 2.66* | 0.09 | 0.64 |
| Trait mindfulness | 0.01 | 0.19 | 0.07 | − 0.37 | 0.40 | 0.01 | 0.19 | 0.07 | − 0.37 | 0.40 |
| Time | − 0.05 | 0.07 | − 0.70 | − 0.18 | 0.09 | − 0.10 | 0.10 | − 1.08 | − 0.30 | 0.09 |
| Intervention | − 0.64 | 0.27 | − 2.38* | − 1.18 | − 0.10 | − 0.69 | 0.28 | − 2.51* | − 1.24 | − 0.14 |
| Intervention × time | 0.11 | 0.13 | 0.83 | − 0.16 | 0.38 | |||||
| − 2LL deviance | 491.8 | 493.3 | ||||||||
| Residual | 0.337 | 0.063 | 5.37** | 0.234 | 0.485 | 0.335 | 0.062 | 5.37** | 0.233 | 0.483 |
| Intercept variance | 0.775 | 0.210 | 3.70** | 0.456 | 1.316 | 0.774 | 0.209 | 3.70** | 0.455 | 1.314 |
| Slope variance | 0.099 | 0.062 | 1.59 | 0.029 | 0.341 | 0.103 | 0.063 | 1.64 | 0.031 | 0.342 |
| Intercept-slope covariance | 0.051 | 0.082 | 0.62 | − 0.109 | 0.211 | 0.049 | 0.082 | 0.60 | − 0.112 | 0.211 |
N = 69 (between subjects) and N = 355 (within subjects). LL/UL, lower/upper confidence interval limit
γ, multilevel regression coefficient, SE, standard error
Model 2A does not include the time × intervention coefficient, whereas Model 2B does
aReference group = senior
*p < .05; **p < .01; ϯp < .10
Table 5.
Multilevel modeling results testing intervention effect on perceived stress
| Model 3A | Model 3B | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient γ | SE | t value | 95% LL | 95% UL | Coefficient γ | SE | t value | 95% LL | 95% UL | |
| Intercept | 2.78 | 0.08 | 34.67** | 2.62 | 2.95 | 2.74 | 0.08 | 33.43** | 2.57 | 2.90 |
| Sophomorea | 0.05 | 0.10 | 0.51 | − 0.14 | 0.24 | 0.05 | 0.10 | 0.51 | − 0.14 | 0.24 |
| Juniora | 0.07 | 0.07 | 0.90 | − 0.08 | 0.21 | 0.07 | 0.07 | 0.91 | − 0.08 | 0.21 |
| Sex (male) | − 0.08 | 0.07 | − 1.04 | − 0.22 | 0.07 | -0.08 | 0.07 | − 1.04 | − 0.22 | 0.07 |
| Neuroticism | 0.17 | 0.04 | 4.09** | 0.09 | 0.25 | 0.17 | 0.04 | 4.10** | 0.09 | 0.25 |
| Extraversion | 0.00 | 0.03 | − 0.01 | − 0.07 | 0.07 | 0.00 | 0.03 | − 0.01 | − 0.07 | 0.07 |
| Trait mindfulness | − 0.11 | 0.05 | − 2.40* | − 0.20 | − 0.02 | − 0.11 | 0.05 | − 2.41* | − 0.20 | − 0.02 |
| Coronavirus worry | 0.10 | 0.03 | 3.34** | 0.04 | 0.16 | 0.10 | 0.03 | 3.33** | 0.04 | 0.16 |
| Time | 0.001 | 0.01 | 0.08 | − 0.02 | 0.03 | 0.03 | 0.02 | 2.07* | 0.00 | 0.07 |
| Intervention | 0.002 | 0.07 | 0.04 | − 0.13 | 0.14 | 0.10 | 0.07 | 1.29 | − 0.05 | 0.25 |
| Intervention × time | − 0.07 | 0.02 | − 2.80** | − 0.11 | − 0.02 | |||||
| − 2LL deviance | 281.4 | 279.6 | ||||||||
| Residual | 0.084 | 0.008 | 10.31** | 0.069 | 0.102 | 0.084 | 0.008 | 10.31** | 0.069 | 0.102 |
| Intercept variance | 0.032 | 0.017 | 1.90ϯ | 0.012 | 0.091 | 0.030 | 0.016 | 1.87 ϯ | 0.011 | 0.086 |
| Slope variance | 0.005 | 0.002 | 2.60** | 0.002 | 0.010 | 0.004 | 0.002 | 2.25* | 0.002 | 0.009 |
| Intercept-slope covariance | − 0.002 | 0.005 | − 0.34 | − 0.011 | 0.008 | 0.000 | 0.004 | − 0.05 | − 0.009 | 0.008 |
N = 69 (between subjects) and N = 355 (within subjects). LL/UL, lower/upper confidence interval limit
γ, multilevel regression coefficient, SE, standard error
Model 3A does not include the time × intervention coefficient, whereas Model 3B does
aReference group = senior
*p < .05; **p < .01; ϯp < .10
Table 6.
Multilevel modeling results testing intervention effect on sleep problems
| Model 4A | Model 4B | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient γ | SE | t value | 95% LL | 95% UL | Coefficient γ | SE | t value | 95% LL | 95% UL | |
| Intercept | 34.35 | 4.17 | 8.23** | 26.00 | 42.70 | 32.92 | 4.23 | 7.77** | 24.45 | 41.39 |
| Sophomorea | − 0.05 | 5.08 | − 0.01 | − 10.23 | 10.13 | − 0.04 | 5.08 | − 0.01 | − 10.23 | 10.15 |
| Juniora | − 3.99 | 3.82 | − 1.04 | − 11.64 | 3.66 | − 3.99 | 3.82 | − 1.04 | − 11.64 | 3.67 |
| Sex (male) | 4.72 | 3.86 | 1.22 | − 3.02 | 12.46 | 4.72 | 3.87 | 1.22 | − 3.03 | 12.46 |
| Neuroticism | 6.92 | 2.17 | 3.19** | 2.58 | 11.27 | 6.92 | 2.17 | 3.19** | 2.58 | 11.27 |
| Extraversion | 1.93 | 1.79 | 1.08 | − 1.66 | 5.53 | 1.94 | 1.79 | 1.08 | − 1.66 | 5.53 |
| Trait mindfulness | − 0.16 | 2.42 | − 0.06 | − 5.00 | 4.68 | − 0.17 | 2.42 | − 0.07 | − 5.01 | 4.68 |
| Coronavirus worry | 3.57 | 1.60 | 2.22* | 0.35 | 6.78 | 3.57 | 1.61 | 2.22* | 0.35 | 6.79 |
| Time | − 0.77 | 0.44 | − 1.76ϯ | − 1.64 | 0.10 | 0.09 | 0.61 | 0.14 | − 1.14 | 1.31 |
| Intervention | 1.30 | 3.50 | 0.37 | − 5.70 | 8.31 | 4.09 | 3.78 | 1.08 | − 3.48 | 11.66 |
| Intervention × time | − 1.65 | 0.85 | − 1.94ϯ | − 3.35 | 0.05 | |||||
| − 2LL deviance | 2607.2 | 2602.0 | ||||||||
| Residual | 77.42 | 7.53 | 10.28** | 63.98 | 93.68 | 77.54 | 7.55 | 10.27** | 64.06 | 93.84 |
| Intercept variance | 152.01 | 38.30 | 3.97** | 92.77 | 249.07 | 150.40 | 37.73 | 3.99** | 91.98 | 245.92 |
| Slope variance | 7.47 | 2.21 | 3.38** | 4.18 | 13.35 | 6.89 | 2.14 | 3.22** | 3.75 | 12.66 |
| Intercept-slope covariance | − 9.25 | 7.60 | − 1.22 | − 24.14 | 5.63 | − 8.25 | 7.29 | − 1.13 | − 22.55 | 6.04 |
N = 69 (between subjects) and N = 355 (within subjects). LL/UL, lower/upper confidence interval limit
γ, multilevel regression coefficient, SE, standard error
Model 4A does not include the time × intervention coefficient, whereas Model 4B does
aReference group = senior
*p < .05; **p < .01; ϯp < .10
All invited students (in both the control and treatment groups) opted to participate in the survey. One student dropped out of the treatment course soon after the first survey was distributed and we did not include that data in our analysis. Attention checks were incorporated in each survey. Observations from a participant who failed an attention check on a given survey were not included in our analysis; specifically, a total of 6 observations were excluded, bringing the total number of within-subject observations to 355. Based on the students’ logs in the Koru app, students in the treatment group meditated outside of class for an average of 6 min a day (standard deviation of 3 min, with the minimum duration at 1 min and the maximum at 12 min); however, several students reported that sometimes they would meditate but forget to log their effort, so the average meditation length outside of class is an underestimate. Twenty-six out of 35 students in the treatment group attended all four Koru sessions.
Group Equivalence
Table 1 reports baseline group differences. Given that participants were assigned to the experimental conditions based on course membership, rather than random assignment, we examined the equivalence between the Koru treatment and control group using t tests. In sum, there were no significant baseline differences on extraversion, neuroticism, and trait mindfulness at time T1 (− 0.69 ≤ t ≤ − 0.10). Additionally, state mindfulness, stress, and sleep duration were measured at time T2, just before the start of the intervention. Again, we found no baseline group differences for these variables (− 0.97 ≤ t ≤ 0.64). Chi-square analyses found no differences in terms of class standing across the two groups (χ2 = 3.85, ns), or likelihood of optimal sleep (χ2 = 0.15, ns), but, we found a significant sex difference where the proportion of men in the treatment group was significantly higher than in the control (χ2 = 4.51, p < 0.05).
Results
Table 2 reports means, standard deviations, and Pearson correlations for all the variables. Consistent with prior research, state (SMS) and trait (MAAS) mindfulness were significantly and negatively correlated with perceived stress (e.g., Brown & Ryan, 2003; Trigueros et al., 2019), and trait mindfulness was significantly and negatively correlated with neuroticism (e.g., Zhao et al., 2019), while neuroticism was significantly and positively correlated with perceived stress and sleep problems (e.g., Drake et al., 2017; Stephan et al., 2018). Furthermore, coronavirus worry significantly and positively correlated with perceived stress and sleep problems (Joos et al., 2012; Meyer et al., 1990) while perceived stress significantly and positively/negatively correlated with sleep problems/sleep duration, respectively (e.g., Friedrich & Schlarb, 2018; Greeson et al., 2014).
Intraclass correlations (ICCs) were first calculated with null empty means models for each dependent variable in our study to determine whether multilevel modeling was appropriate. Approximately 56% of the variance in perceived stress, 44% of the variance in state mindfulness, and 66% of the variance in sleep problems were between subjects. Additionally, 81% of the variance in coronavirus worry was between subjects. To account for this dependency in these data, we created hierarchical models where repeated measurements were nested within individuals. We grand-mean-centered between-subject variables. When we report simple slope results, we use the letter b to denote the simple slope and SE to denote its standard error.
State Mindfulness
We observed a significant main effect of the intervention on state mindfulness (γ = 0.27, SE = 0.14, p = 0.051), where participants in the Koru intervention reported greater level of mindfulness overall (see Table 3). Additionally, we examined the effect of the intervention during the course of the study and observed a significant interaction between the intervention and time (γ = 0.07, SE = 0.04, p < 0.05; Model B in Table 3). There were no significant differences in state mindfulness between the groups at the baseline (at time T1; b = 0.08, SE = 0.15, ns), and the simple slopes indicated that while the Koru group experienced increased state mindfulness over time (b = 0.06, SE = 0.02, p = 0.01), the control group did not (b = − 0.01, SE = 0.03, ns). As we anticipated, the Koru group reported significantly more mindfulness than the control group during the final time point (b = 0.44, SE = 0.17, p < 0.01). The effect size for the difference between the means of the treatment and control groups in state mindfulness at the last measurement time point (T6), based on Cohen’s d, was large at d = 0.91.
Coronavirus Worry
We observed a significant main effect of the intervention on coronavirus worry (γ = -0.64, SE = 0.27, p < 0.05), where participants in the Koru intervention reported fewer worrying thoughts about the coronavirus overall (see Table 4). Additionally, we examined the effect of the intervention during the course of the study but failed to observed a significant interaction between the intervention and time (γ = 0.11, SE = 0.13, ns). The effect size for the difference between the means of the treatment and control group in coronavirus worry at time T6 was medium, at d = − 0.50, but this effect was actually stronger at T3 (d = − 0.81). Thus, although differences in worry between the groups somewhat declined over time, the interaction between intervention and time was not significant.
Perceived Stress
We failed to observe a significant main effect of the intervention on stress (γ = 0.002, SE = 0.07, ns; see Table 5). Additionally, we examined the effect of the intervention during the course of the study and observed a significant interaction between the intervention and time (γ = − 0.07, SE = 0.02, p < 0.01). There were no significant differences between the groups at the baseline (b = 0.10, SE = 0.08, ns), and the simple slopes indicate that while the Koru group experienced decreased stress over time (b = − 0.03, SE = 0.016, p = 0.06), the control group actually experienced increased stress (b = 0.04, SE = 0.017, p < 0.05). Furthermore, the control group had significantly more stress than the intervention group during the final time point (b = − 0.23, SE = 0.11, p < 0.05). The effect size for the difference between the means of the treatment and control group in perceived stress at time T6 was small, at d = − 0.42.
Sleep Problems and Duration
We again failed to observe a significant main effect of the intervention on sleep problems (γ = 1.30, SE = 3.50, ns; see Table 6). Additionally, we examined the effect of the intervention during the course of the study and observed a significant interaction between the intervention and time (γ = − 1.65, SE = 0.85, p = 0.057). There were no significant differences between the groups at the baseline (b = 4.14, SE = 3.85, ns), and the simple slopes indicate that while the Koru group experienced significant declines in sleep problems over time (b = − 1.56, SE = 0.59, p < 0.01), the control group did not (b = 0.09, SE = 0.06, ns). The effect size for the difference between the means of the treatment and control group in sleep problems at time T6 was small, at d = − 0.08.
We used GEE to model the effects of the intervention on the probability of obtaining an optimal amount of sleep. We again failed to observe a significant main effect of the intervention on sleep duration (B = 0.28, SE = 0.36, ns; see Table 7). Additionally, we examined the effect of the intervention during the course of the study and observed a significant interaction between the intervention and time (B = 0.32, SE = 0.13, p < 0.05). As illustrated in Fig. 1, Koru participants (59%) did not show any appreciable differences in the likelihood of obtaining optimal sleep compared to the control group (62%) at the baseline. By the end of the study, however, Koru participants experienced an 18% increase in the likelihood of getting optimal sleep (i.e., 76%, which is a 30% improvement), while the control group experienced a 19% decrease in the likelihood of getting optimal sleep (i.e., 43%, which is a 31% decrement).
Table 7.
Generalized estimating equations results testing intervention effect on optimal sleep
| Model 5A | Model 5B | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient B | SE | Wald | 95% LL | 95% UL | Coefficient B | SE | Wald | 95% LL | 95% UL | |
| Intercept | 0.08 | 0.39 | 0.04 | − 0.69 | 0.85 | 0.57 | 0.43 | 1.77 | − 0.27 | 1.40 |
| Sophomorea | 0.94 | 0.59 | 2.55 | − 0.21 | 2.08 | 1.10 | 0.61 | 3.33ϯ | − 0.08 | 2.29 |
| Juniora | 0.11 | 0.40 | 0.07 | − 0.67 | 0.88 | − 0.01 | 0.41 | 0.00 | − 0.82 | 0.80 |
| Sex (male) | 0.08 | 0.50 | 0.02 | − 0.90 | 1.06 | 0.04 | 0.49 | 0.01 | − 0.92 | 1.00 |
| Neuroticism | 0.09 | 0.24 | 0.15 | − 0.38 | 0.57 | 0.05 | 0.22 | 0.05 | − 0.39 | 0.49 |
| Trait mindfulness | 0.32 | 0.26 | 1.47 | − 0.20 | 0.84 | 0.41 | 0.27 | 2.31 | − 0.12 | 0.94 |
| Coronavirus worry | − 0.04 | 0.19 | 0.04 | − 0.41 | 0.33 | − 0.08 | 0.19 | 0.18 | − 0.45 | 0.29 |
| Time | 0.13 | 0.08 | 2.66 | − 0.03 | 0.28 | − 0.16 | 0.09 | 3.38ϯ | − 0.32 | 0.01 |
| Intervention | 0.28 | 0.36 | 0.59 | − 0.43 | 0.99 | − 0.16 | 0.42 | 0.15 | − 0.99 | 0.67 |
| Intervention × time | 0.32 | 0.13 | 5.75* | 0.06 | 0.58 | |||||
| QIC goodness of fit | 364.2 | |||||||||
N = 64 (between subjects) and N = 268 (within subjects). LL/UL, lower/upper confidence interval limit
B, generalized estimation coefficient; SE, standard error
Model 5A does not include the time × intervention coefficient, whereas Model 5B does
aReference group = senior
*p < .05; **p < .01; ϯp < .10
Fig. 1.
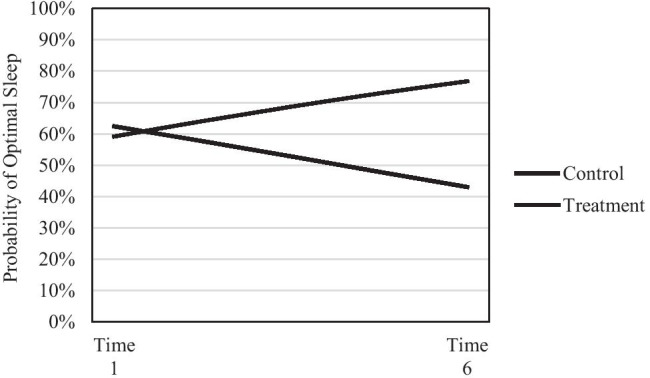
Simple slopes for probability of obtaining optimal sleep interaction
Robustness Checks
To test the robustness of our findings, we reanalyzed our hypotheses using the same procedures, but excluding control variables. None of the results was substantively changed by excluding controls, with the exception of sleep problems. In this case, the p value for the interaction term increased to p = 0.11 from p = 0.057. Exploratory analyses indicate that neuroticism was largely responsible for this change, which is unsurprising given its strong links to sleep (Duggan et al., 2014).
Discussion
This study evaluated a 4-week MBI called Koru mindfulness targeting college students. We found that the intervention buffered participants from worrying about the novel coronavirus during a global pandemic, while simultaneously increasing state mindfulness and reducing perceived stress and sleep problems. Conversely, while control participants did not experience changes in state mindfulness or sleep problems during the study time period, they did experience greater coronavirus worry and stress. These effects held when controlling for trait mindfulness, neuroticism, and extraversion. We can thus infer that the Koru program is robust in improving state mindfulness, reducing perceived stress and context-specific worry (e.g., about a pandemic), and improving sleep outcomes. These findings are noteworthy given that we were able to obtain pre-pandemic baselines for the participants on our dependent variables, and consequently, able to observe how the Koru intervention affected them as the pandemic unfolded during the spring semester. The current study contributes to extant literature by providing evidence for the effectiveness of this particular intervention amidst very stressful conditions and by providing further validation that MBIs tailored for college students can be beneficial to the well-being of young adults.
Our findings are generally consistent with prior studies on the effect of MBIs in college populations, which overall conclude that MBIs can be helpful in reducing stress, anxiety, and depression and in enhancing students’ well-being (Amanvermez et al., 2020; Ma et al., 2019). Prior studies have also reported that MBIs increase mindfulness (Bamber & Schneider, 2016), and decrease worry by improving emotional and physiological regulatory processes (Delgado et al., 2010). More specific comparisons of effect sizes between this study and other MBIs may be difficult to interpret given the somewhat unique context of our study (pandemic) and the various differences in measures, sample sizes, and other study design characteristics in existing literature (Dawson et al., 2019). One study we can more readily compare our results to, however, is by Greeson et al. (2014), who also evaluated the Koru intervention and employed two identical scales, for perceived stress and sleep problems. Greeson et al.’s (2014) perceived stress score effect size was similar to ours, while the effect size on perceived sleep problems scores was medium in Greeson et al. (2014), but fairly small in this study. The unique context of this intervention (during a pandemic) may explain the difference of the effect size in sleep problems; more generally, prior meta-analyses on the effects of MBIs on sleep outcomes have reported highly variable effect sizes and some mixed results (Rusch et al., 2019; Winbush et al., 2007).
Our findings with respect to control variables in our regression models also relate to prior work. Specifically, the finding that neurotic individuals experienced higher levels of coronavirus worry, perceived stress, and sleep problems is not surprising since neurotic individuals are more susceptible and cope more poorly with stress (Giluk, 2009). Our results are also in agreement with past findings suggesting that mindfulness can reduce the perceived distress of neurotic individuals (Drake et al., 2017). Therefore, MBIs are especially important for college students with this particular personality trait, and targeted interventions to this sub-population of college students should be considered by university wellness programs. We also found that extraverted individuals reported a higher level of coronavirus worry. Since extraverted people tend to be social and require higher levels of excitement and stimulation (Digman, 1990), the pandemic lockdown and its forced social distancing may have been especially hard for them, thus leading to higher levels of coronavirus worry. We also found that male students reported less coronavirus worry than female students, which is consistent with prior findings of gender differences in worry (Bottesi et al., 2018; Robichaud et al., 2003) and with recent evidence that female university students experienced greater anxiety and stress during the pandemic (Debowska et al., 2020). Finally, our findings that students with higher levels of coronavirus worry reported more sleep problems are intuitive and have been reported in past research (e.g., Friedrich & Schlarb, 2018).
Overall, our results suggest that the Koru program is a promising intervention for college students that merits further exploration and should be considered by student wellness programs on university campuses. The Koru intervention can be considered not only under typical semester conditions but also on a COVID-impacted environment.
Limitations and Future Research
This study’s strength is evaluating an MBI during very stressful conditions against a control group and over time with high level of program adherence and minimal attrition. We should, however, acknowledge several limitations. All scales were self-reported and thus not as reliable as more objective measures such as salivary cortisol levels or breath monitoring. Our sample is also not representative of the general college population, since it consisted of predominantly male and white students in a college that focuses primarily in business education. Although these demographics mirrored the broader campus, our racially homogeneous sample precluded us from assessing students’ multicultural characteristics. Future research should make intentional efforts to recruit more diverse samples to promote inclusivity and enhance the generalizability of results, as suggested by Chin et al. (2019). Stratified sampling is a natural choice, which could involve intentional recruitment efforts among underrepresented samples.
Furthermore, it is possible that there was some selection bias in our sample, since students interested in enrolling in a positive psychology course may choose to do so because they are experiencing some psychological distress. However, since students were not aware that the Koru curriculum would be included in the course, selection bias specifically about the Koru curriculum is minimal and circumvents the need for a waitlist control group. Furthermore, our analyses did not reveal any substantive differences between the treatment and control groups at baseline (see Table 1).
To measure worry about the novel coronavirus, we chose to adapt an existing scale, given that no validated scales existed in the literature at the time. As such, it is necessary to accumulate additional evidence for the validity and reliability of this adapted scale. Additionally, the final measurement of this study, post intervention, happened a little more than a week after the intervention ended (due to the final exam period starting); hence, we do not know how long the effects would last after that. We hypothesize that the intervention would only continue to be beneficial for those students continuing with the practice on their own, but further research is needed to determine this. Finally, practical constraints (i.e., recruiting students via course enrollment) combined with the unique circumstances of the study due to the pandemic limited our ability to collect additional comparable data. Although a larger sample size would be ideal, we did detect significant effects with a reasonable level of power.
Several factors may have contributed to the robustness of the Koru program during the pandemic lockdown in our study, including a curriculum specifically targeting college students’ concerns, support from a trained course leader, low attrition rates, and the expectation for consistent practice. Future research could further tease out the effect of each of these factors. Specifically, while Koru is an intervention targeting college students, its effectiveness relative to other targeted interventions such as the Learning to BREATH program remains unclear. The importance of the facilitator’s role has recently been noted by Bamber et al. (2020) and Dawson et al. (2019) who suggested that MBIs may generate uncomfortable states in some students that may require special attention from the course leader or more specialized support services. Given that the Koru curriculum is offered by trained and certified instructors, the risk of not properly attending to possible difficulties students may be experiencing during an intervention is reduced, but certainly not eliminated. Future studies could elaborate on the role of a Koru facilitator in addressing student concerns. The challenge with low attrition in free-standing MBIs for college students and other populations has also been identified in past work (e.g., Nam & Toneatto, 2016; Nich & Carroll, 2002). Because in this study Koru was embedded within a regular semester course, there was minimal attrition; all students (except one who dropped the course early on) completed and passed the course and the Koru curriculum. Consistency of practice in this study was also facilitated by encouraging (but not requiring) students to practice outside of class and by enabling them to easily access meditation scripts and log their practice via the Koru app. Interestingly, Bamber et al.’s (2019) meta-analysis revealed that interventions that did not require home meditation practice showed larger decreases in anxiety, possibly because already overwhelmed students would resist meditation practice as yet another requirement. Future research designs could more directly compare the effect of requiring a home meditation practice versus leaving it optional.
Another topic for further exploration would be to examine the ideal length of an MBI for college students. Given its relatively short duration (4 weeks) and its relatively short out-of-class suggested practice times (10 min a day), Koru can fit fairly easily with the competing priorities many college students juggle (Greeson et al., 2014). This is particularly important given the rising levels of students’ stress and given that rising budget restrictions, perceived stigma, and perceived time pressure can make mental health services unreachable to a large number of college students (Greeson et al., 2014; Halladay et al., 2019). However, it remains unclear if more weeks of practice would bring significantly higher benefits. Prior studies have found that MBIs with a greater number of sessions show greater reductions in anxiety (Bamber & Morpeth, 2019). Future research designs could compare more directly—ideally with common scales and diverse student populations—the effect of the length and overall program structure of MBIs on young adults.
Author Contribution
BS: collaborated with the design and execution of the study, took the lead in deriving and writing the results, and collaborated in the writing and editing of the final manuscript. ES: collaborated with the design and execution of the study, assisted with preliminary data analysis, wrote the first draft of the paper and revision (other than the results), and collaborated in the revising and editing of the final manuscript.
Data Availability
The data that support the findings of this study are available on request from the corresponding author (ES). The data are not publicly available due to them containing information that could compromise research participant privacy/consent.
Declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of Bentley University’s institutional review board and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Amanvermez, Y., Rahmadiana, M., Karyotaki, E., de Wit, L., Ebert, D. D., Kessler, R. C., & Cuijpers, P. (2020). Stress management interventions for college students: A systematic review and meta‐analysis. Clinical Psychology: Science and Practice, e12342. 10.1111/cpsp.12342
- American College of Health Association. (2019). National College Health Assessment Spring 2019 reference group executive summary. https://www.acha.org/documents/ncha/NCHA-II_SPRING_2019_US_REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdf
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Ballinger GA. Using generalized estimating equations for longitudinal data analysis. Organizational Research Methods. 2004;7(2):127–150. doi: 10.1177/1094428104263672. [DOI] [Google Scholar]
- Bamber MD, Schneider JK. Mindfulness-based meditation to decrease stress and anxiety in college students: A narrative synthesis of the research. Educational Research Review. 2016;18:1–32. doi: 10.1016/j.edurev.2015.12.004. [DOI] [Google Scholar]
- Bamber MD, Morpeth E. Effects of mindfulness meditation on college student anxiety: A meta-analysis. Mindfulness. 2019;10(2):203–214. doi: 10.1007/s12671-018-0965-5. [DOI] [Google Scholar]
- Bamber, M. D., & Schneider, J. K. (2020). College students’ perceptions of mindfulness-based interventions: A narrative review of the qualitative research. Current Psychology. 10.1007/s12144-019-00592-4.
- Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., Segal, Z. V., Abbey, S., Speca, M., Velting, D., & Devins, G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11(3), 230-241. 10.1093/clipsy.bph077
- Bodenlos JS, Noonan M, Wells SY. Mindfulness and alcohol problems in college students: The mediating effects of stress. Journal of American College Health. 2013;61(6):371–378. doi: 10.1080/07448481.2013.805714. [DOI] [PubMed] [Google Scholar]
- Bottesi G, Martignon A, Cerea S, Ghisi M. Worry and associated cognitive features in Italian university students: Does gender make a difference? Personality and Individual Differences. 2018;126:38–43. doi: 10.1016/j.paid.2018.01.016. [DOI] [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson LE, Brown KW. Validation of the Mindful Attention Awareness Scale in a cancer population. Journal of Psychosomatic Research. 2005;58(1):29–33. doi: 10.1016/j.jpsychores.2004.04.366. [DOI] [PubMed] [Google Scholar]
- Chin G, Anyanso V, Greeson J. Addressing diversity in mindfulness research on health: A narrative review using the ADDRESSING framework. Cooper Rowan Medical Journal. 2019;1(1):1–13. doi: 10.31986/issn.2578-3343_vol1iss1.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiodelli, R., Mello, L. T. N. D., Jesus, S. N. D., Beneton, E. R., Russel, T., & Andretta, I. (2020). Mindfulness-based interventions in undergraduate students: A systematic review. Journal of American College Health, 1-10. 10.1080/07448481.2020.1767109 [DOI] [PubMed]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Dawson, A. F., Brown, W. W., Anderson, J., Datta, B., Donald, J. N., Hong, K., ... & Galante, J. (2019). Mindfulness‐based interventions for university students: A systematic review and meta‐analysis of randomised controlled trials. Applied Psychology: Health and Well‐Being, 12(2), 384–410. 10.1111/aphw.12188 [DOI] [PubMed]
- Debowska, A., Horeczy, B., Boduszek, D., & Dolinski, D. (2020). A repeated cross-sectional survey assessing university students’ stress, depression, anxiety, and suicidality in the early stages of the COVID-19 pandemic in Poland. Psychological Medicine, 1-4. 10.1017/S003329172000392X [DOI] [PMC free article] [PubMed]
- Delgado LC, Guerra P, Perakakis P, Vera MN, del Paso GR, Vila J. Treating chronic worry: Psychological and physiological effects of a training programme based on mindfulness. Behaviour Research and Therapy. 2010;48(9):873–882. doi: 10.1016/j.brat.2010.05.012. [DOI] [PubMed] [Google Scholar]
- Digman JM. Personality structure: Emergence of the five-factor model. Annual Review of Psychology. 1990;41(1):417–440. doi: 10.1146/annurev.ps.41.020190.002221. [DOI] [Google Scholar]
- Dvořáková K, Kishida M, Li J, Elavsky S, Broderick PC, Agrusti MR, Greenberg MT. Promoting healthy transition to college through mindfulness training with first-year college students: Pilot randomized controlled trial. Journal of American College Health. 2017;65(4):259–267. doi: 10.1080/07448481.2017.1278605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake MM, Morris M, Davis TJ. Neuroticism’s susceptibility to distress: Moderated with mindfulness. Personality and Individual Differences. 2017;106:248–252. doi: 10.1016/j.paid.2016.10.060. [DOI] [Google Scholar]
- Duggan KA, Friedman HS, McDevitt EA, Mednick SC. Personality and healthy sleep: The importance of conscientiousness and neuroticism. PLoS ONE. 2014;9(3):e90628. doi: 10.1371/journal.pone.0090628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang AG, Buchner A. G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- Freligh CB, Debb SM. Nonreactivity and resilience to stress: Gauging the mindfulness of African American college students. Mindfulness. 2019;10(11):2302–2311. doi: 10.1007/s12671-019-01203-w. [DOI] [Google Scholar]
- Friedrich A, Schlarb AA. Let’s talk about sleep: A systematic review of psychological interventions to improve sleep in college students. Journal of Sleep Research. 2018;27(1):4–22. doi: 10.1111/jsr.12568. [DOI] [PubMed] [Google Scholar]
- Giluk TL. Mindfulness, big five personality, and affect: A meta-analysis. Personality and Individual Differences. 2009;47(8):805–811. doi: 10.1016/j.paid.2009.06.026. [DOI] [Google Scholar]
- Gonzalez-Voller J, Wood AW, Marrs F, Ephraimson-Abt V, Sharp J, Garcia A. A randomized-controlled pilot study comparing a one-day and four-week mindfulness-based group intervention for family caregivers. The Journal for Specialists in Group Work. 2019;44(4):228–234. doi: 10.1080/01933922.2019.1669753. [DOI] [Google Scholar]
- Grabovac AD, Lau MA, Willett BR. Mechanisms of mindfulness: A Buddhist psychological model. Mindfulness. 2011;2(3):154–166. doi: 10.1007/s12671-011-0062-5. [DOI] [Google Scholar]
- Gray L, Font S, Unrau Y, Dawson A. The effectiveness of a brief mindfulness-based intervention for college freshmen who have aged out of foster care. Innovative Higher Education. 2018;43(5):339–352. doi: 10.1007/s10755-018-9433-3. [DOI] [Google Scholar]
- Greeson JM, Juberg MK, Maytan M, James K, Rogers H. A randomized controlled trial of Koru: A mindfulness program for college students and other emerging adults. Journal of American College Health. 2014;62(4):222–233. doi: 10.1080/07448481.2014.887571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman P. Defining mindfulness by how poorly I think I pay attention during everyday awareness and other intractable problems for psychology’s (re)invention of mindfulness: Comment on Brown et al. (2011) Psychological Assessment. 2011;23(4):1034–1040. doi: 10.1037/a0022713. [DOI] [PubMed] [Google Scholar]
- Halladay JE, Dawdy JL, McNamara IF, Chen AJ, Vitoroulis I, McInnes N, Munn C. Mindfulness for the mental health and well-being of post-secondary students: A systematic review and meta-analysis. Mindfulness. 2019;10(3):397–414. doi: 10.1007/s12671-018-0979-z. [DOI] [Google Scholar]
- Hays RD, Stewart AL. Sleep measures. In: Stewart AL, Ware JE, editors. Measuring functioning and well-being: The medical outcomes study approach. Duke University Press; 1992. pp. 235–259. [Google Scholar]
- Hays RD, Martin SA, Sesti AM, Spritzer KL. Psychometric properties of the medical outcomes study sleep measure. Sleep Medicine. 2005;6(1):41–44. doi: 10.1016/j.sleep.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science. 2011;6(6):537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Huang J, Nigatu YT, Smail-Crevier R, Zhang X, Wang J. Interventions for common mental health problems among university and college students: A systematic review and meta-analysis of randomized controlled trials. Journal of Psychiatric Research. 2018;107:1–10. doi: 10.1016/j.jpsychires.2018.09.018. [DOI] [PubMed] [Google Scholar]
- Husky MM, Kovess-Masfety V, Swendsen JD. Stress and anxiety among university students in France during COVID-19 mandatory confinement. Comprehensive Psychiatry. 2020;102:152191. doi: 10.1016/j.comppsych.2020.152191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John, O., Donahue, E., & Kentle, R. (1991). The Big Five Inventory-versions 4a and 54. Berkeley, CA: University of California. Berkeley, Institute of Personality and Social Research. 10.1037/t07550-000
- Joos E, Vansteenwegen D, Hermans D. Worry as a predictor of fear acquisition in a nonclinical sample. Behavior Modification. 2012;36(5):723–750. doi: 10.1177/0145445512446477. [DOI] [PubMed] [Google Scholar]
- Katz D, Toner B. A systematic review of gender differences in the effectiveness of mindfulness-based treatments for substance use disorders. Mindfulness. 2013;4(4):318–331. doi: 10.1007/s12671-012-0132-3. [DOI] [Google Scholar]
- Ma L, Zhang Y, Cui Z. Mindfulness-based interventions for prevention of depressive symptoms in university students: A meta-analytic review. Mindfulness. 2019;10:2209–2224. doi: 10.1007/s12671-019-01192-w. [DOI] [Google Scholar]
- MacKillop J, Anderson EJ. Further psychometric validation of the Mindful Attention Awareness Scale (MAAS) Journal of Psychopathology and Behavioral Assessment. 2007;29(4):289–293. doi: 10.1007/s10862-007-9045-1. [DOI] [Google Scholar]
- McNeish D. Small sample methods for multilevel modeling: A colloquial elucidation of REML and the Kenward-Roger correction. Multivariate Behavioral Research. 2017;52(5):661–670. doi: 10.1080/00273171.2017.1344538. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28(6):487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Nam S, Toneatto T. The influence of attrition in evaluating the efficacy and effectiveness of mindfulness-based interventions. International Journal of Mental Health and Addiction. 2016;14(6):969–981. doi: 10.1007/s11469-016-9667-1. [DOI] [Google Scholar]
- Nich C, Carroll KM. Intention-to-treat meets missing data: Implications of alternate strategies for analyzing clinical trials data. Drug and Alcohol Dependence. 2002;68(2):121–130. doi: 10.1016/S0376-8716(02)00111-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Governor Charlie Baker and Lt. Governor Karyn Polito, (2020, March 10). Governor Baker declares state of emergency to support commonwealth’s response to coronavirus. https://www.mass.gov/news/governor-baker-declares-state-of-emergency-to-support-commonwealths-response-to-coronavirus
- Oswalt SB, Lederer AM, Chestnut-Steich K, Day C, Halbritter A, Ortiz D. Trends in college students’ mental health diagnoses and utilization of services, 2009–2015. Journal of American College Health. 2020;68(1):41–51. doi: 10.1080/07448481.2018.1515748. [DOI] [PubMed] [Google Scholar]
- Querstret, D., Morison, L., Dickinson, S., Cropley, M., & John, M. (2020). Mindfulness-Based Stress Reduction and Mindfulness-Based Cognitive Therapy for psychological health and wellbeing in non-clinical samples: A systematic review and meta-analysis. International Journal of Stress Management, 27(4), 394-411. https://doi.org/10.1037/str0000165
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31(4):437–448. doi: 10.3102/10769986031004437. [DOI] [Google Scholar]
- Rammstedt B, John OP. Measuring personality in one minute or less: A 10-item short version of the Big Five Inventory in English and German. Journal of Research in Personality. 2007;41(1):203–212. doi: 10.1016/j.jrp.2006.02.001. [DOI] [Google Scholar]
- Roberti JW, Harrington LN, Storch EA. Further psychometric support for the 10-item version of the perceived stress scale. Journal of College Counseling. 2006;9(2):135–147. doi: 10.1002/j.2161-1882.2006.tb00100.x. [DOI] [Google Scholar]
- Rogers HB. The Mindful twenty-something: Life skills to handle stress... and everything else. New Harbinger Publications; 2016. [Google Scholar]
- Rogers H, Maytan M. Mindfulness for the next generation: Helping emerging adults manage stress and lead healthier lives. Oxford University Press; 2019. [Google Scholar]
- Robichaud M, Dugas MJ, Conway M. Gender differences in worry and associated cognitive-behavioral variables. Journal of Anxiety Disorders. 2003;17(5):501–516. doi: 10.1016/S0887-6185(02)00237-2. [DOI] [PubMed] [Google Scholar]
- Ruimi L, Hadash Y, Tanay G, Bernstein A. State Mindfulness Scale (SMS) In: Medvedev ON, Krägeloh CU, Siegert RJ, Singh NN, editors. Handbook of assessment in mindfulness. Springer; 2019. [Google Scholar]
- Rusch HL, Rosario M, Levison LM, Olivera A, Livingston WS, Wu T, Gill JM. The effect of mindfulness meditation on sleep quality: A systematic review and meta-analysis of randomized controlled trials. Annals of the New York Academy of Sciences. 2019;1445(1):5–16. doi: 10.1111/nyas.13996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauer S, Walach H, Schmidt S, Hinterberger T, Lynch S, Büssing A, Kohls N. Assessment of mindfulness: Review on state of the art. Mindfulness. 2013;4(1):3–17. doi: 10.1007/s12671-012-0122-5. [DOI] [Google Scholar]
- Snijders TA, Bosker RJ. Multilevel analysis: An introduction to basic and advanced multilevel modeling. Sage; 2011. [Google Scholar]
- Spijkerman MPJ, Pots WTM, Bohlmeijer ET. Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clinical Psychology Review. 2016;45:102–114. doi: 10.1016/j.cpr.2016.03.009. [DOI] [PubMed] [Google Scholar]
- Stephan Y, Sutin AR, Bayard S, Križan Z, Terracciano A. Personality and sleep quality: Evidence from four prospective studies. Health Psychology. 2018;37(3):271–281. doi: 10.1037/hea0000577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanay, G., & Bernstein, A. (2013). State Mindfulness Scale (SMS): Development and initial validation. Psychological Assessment, 25(4), 1286. 10.1037/a0034044 [DOI] [PubMed]
- Trigueros R, Aguilar-Parra JM, Cangas AJ, Mullor D, Álvarez JF, García-Mas A. Adaptation and validation the State Mindfulness Scale (SMS) to physical education in a Spanish context. Sustainability. 2019;11(20):5681. doi: 10.3390/su11205681. [DOI] [Google Scholar]
- Van Dam NT, Earleywine M, Borders A. Measuring mindfulness? An item response theory analysis of the Mindful Attention Awareness Scale. Personality and Individual Differences. 2010;49(7):805–810. doi: 10.1016/j.paid.2010.07.020. [DOI] [Google Scholar]
- Winbush NY, Gross CR, Kreitzer MJ. The effects of Mindfulness-Based Stress Reduction on sleep disturbance: A systematic review. Explore. 2007;3(6):585–591. doi: 10.1016/j.explore.2007.08.003. [DOI] [PubMed] [Google Scholar]
- Zhao D, Wang H, Feng X, Lv G, Li P. Relationship between neuroticism and sleep quality among asthma patients: The mediation effect of mindfulness. Sleep and Breathing. 2019;23(3):925–931. doi: 10.1007/s11325-019-01814-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author (ES). The data are not publicly available due to them containing information that could compromise research participant privacy/consent.


