Introduction
Verrucous candidiasis (VC) of the oral mucosa can present with pseudocarcinomatous hyperplasia, often confused with squamous cell carcinoma (SCC). Here, we describe a case of florid VC secondary to fluconazole-resistant Candida albicans and report an initial significant response to oral posaconazole and surgical excisions. However, after 12 months of close follow-up, the patient's VC progressed to frank SCC, demonstrating the malignant potential of refractory VC cases.
Case report
An 84-year-old woman with limited scleroderma presented with an 8-month history of multiple exophytic verrucous nodules on the lower vermilion and mucosal lip, mechanically limiting her oral intake (Fig 1, A). The remainder of the examination revealed moist pink patches on the bilateral oral commissures. Three years prior to the development of her nodules, the patient was diagnosed with angular cheilitis. Although initially responsive to iodochlorhydroxyquin 3%–hydrocortisone 0.5% cream and mupirocin 2% ointment, her angular cheilitis eventually became refractory to topical therapy. With the onset of verrucous nodules, she was subsequently treated with 2 courses of oral fluconazole again with minimal improvement. Other pertinent past medical history included esophageal strictures requiring esophageal dilatations multiple times per year, and on 1 occasion, several years prior, a brush biopsy had revealed candidal esophagitis. More recently, her dysphagia had worsened, resulting in significant weight loss and cachexia. To mitigate her symptoms, the patient often consumed sugar-containing lozenges.
Fig 1.
Clinical presentation. A, Initial presentation of verrucous nodules on the vermilion lip. B, Interval improvement at 4 months after several excisions and an 8-week course of posaconazole. C, Worsened disease of the lower mucosal and cutaneous lip refractory to antifungal therapy at 12 months.
Multiple diagnostic and therapeutic excisional biopsies revealed verrucous epithelial hyperplasia, variable degrees of focal dysplasia but with a well-circumscribed base, and florid superficial fungal hyphae (Fig 2, A), further highlighted by periodic acid–Schiff staining (Fig 2, B). Sterile fungal culture grew 4+ Candida albicans, and susceptibility testing revealed fluconazole resistance and posaconazole susceptibility. A diagnosis of VC was favored. The patient was started on an 8-week course of posaconazole oral suspension (400 mg twice daily for 3 days followed by 400 mg daily for 53 days). Two months following the completion of posaconazole, she had marked improvement (Fig 1, B), and her dysphagia symptoms had improved. However, a new nodule on the left side of the lower mucosal lip, not present on initial presentation, appeared (Fig 1, B) and rapidly enlarged over the ensuing months (Fig 1, C). Excision of this nodule was performed, and histopathologic examination exhibited infiltrative cords and strands of atypical squamous epithelium on pathology (Fig 2, C and D), which were not present in earlier biopsies. The new infiltrative architecture was diagnostic of SCC, and the patient was treated with palliative radiation (2000 cGy in 5 fractions).
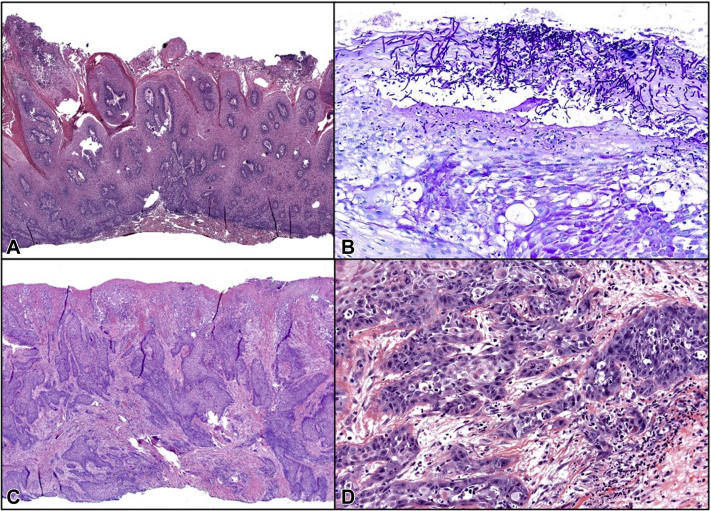
Fig 2.
Histopathology of verrucous nodules. A, Hematoxylin-eosin stain of an early verrucous nodule showing epithelial hyperplasia, focal dysplasia, and a well-circumscribed base. B, A representative PAS stain shows florid fungal organisms. C, Infiltrative stands and cords composed of (D) severely atypical squamous epithelium, with abundant mitoses confirming squamous cell carcinoma at the 12-month follow-up. (A, Hematoxylin-eosin stain; original magnification: ×20; B, PAS stain; original magnification: ×400; C, original magnification: ×25; D, original magnification: ×200.)
Discussion
VC or chronic hyperplastic candidiasis of the oral mucosa is a rare condition that often involves the buccal commissures, cheeks, palate, and tongue, although the inferior vermilion lip is also affected.1 Histologically, it presents as verrucous hyperplasia comprising keratinocytes with pink, glassy cytoplasm and typically mild nuclear atypia. In addition, pseudocarcinomatous hyperplasia may also be present. In our case, initial biopsies revealed orderly maturation, minimal pleomorphism, and absence of invasion, despite focal atypia supporting the diagnosis of VC over SCC or other neoplasia.
The management of VC may be challenging, and the prognosis is often uncertain due to the paucity of cases reported in the literature. In their series, Motaparthi et al1 reported that a majority of VC cases responded to antifungal therapy; of 9 cases, 1 resolved spontaneously, 5 with topical antifungals, and 2 required oral antifungals. In the ninth case, the disease persisted, despite systemic antifungal therapy. Unfortunately, the study was limited by the short follow-up (median 5 weeks), but other reports estimate that approximately 15% of VC cases progress to moderate or severe dysplasia.2 SCC has rarely been reported in cases resistant to medical therapy.3 Indeed, although our patient initially responded to serial excisional surgeries and posaconazole, her mucocutaneous nodules eventually progressed to unequivocal SCC. It is conceivable that the patient's SCC arose earlier in her clinical course and was hidden by VC; however, multiple excisions of individual nodules at presentation showed limited atypia without invasion into the lamina propria (Fig 1, A), so the risk of undersampling is low. Moreover, her initial response to posaconazole supports the hypothesis that her VC had truly transformed into SCC. This case demonstrates the need for vigilant follow-up in persistent or recurrent VC.
We have previously reported a series of challenging vermilion lip lesions that mimic SCC and devised a clinical algorithm.4 Our pathway highlights the importance of repeat sampling in this area to reconcile clinical and pathological findings and distinguish between reactive atypia and true dysplasia. The algorithm also recognizes that dysplasia may even evolve from inflammatory or infectious lesions, as in this case. In such instances of SCC arising in the setting of VC, the association between Candida infection and carcinogenesis remains unclear. Further studies are required to clarify this association.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Motaparthi K., Kapil J.P., Plaza J.A. Verrucous candidiasis of the orolabial mucosa: a clinicopathologic series. J Cutan Pathol. 2017;44(10):815–818. doi: 10.1111/cup.13003. [DOI] [PubMed] [Google Scholar]
- 2.Bartie K.L., Williams D.W., Wilson M.J., Potts A.J., Lewis M.A. Differential invasion of Candida albicans isolates in an in vitro model of oral candidosis. Oral Microbiol Immunol. 2004;19(5):293–296. doi: 10.1111/j.1399-302X.2004.00155.x. [DOI] [PubMed] [Google Scholar]
- 3.Eyre J., Nally F.F. Oral candidosis and carcinoma. Br J Dermatol. 1971;85(1):73–75. doi: 10.1111/j.1365-2133.1971.tb07183.x. [DOI] [PubMed] [Google Scholar]
- 4.Kibbi N., Christensen S.R., Ko C.J., Suozzi K.C. An algorithm for evaluating challenging lip cases: neoplastic versus inflammatory. Dermatol Surg. 2020;46(5):700–702. doi: 10.1097/DSS.0000000000001849. [DOI] [PubMed] [Google Scholar]