Abstract
Introduction
Vaccination is a key global strategy to mitigate the clinical impact of the COVID-19 virus. As part of local efforts to manage the outbreak, the government of Ghana announced its intention to vaccinate its population starting with essential and high-risk workers including radiographers. However, there were reports of hesitance to receiving the vaccine among the radiography workforce. This study was undertaken prior to the intended vaccination exercise to assess the willingness and concerns of radiographers to undergo the COVID-19 vaccination and to suggest recommendations to improve the vaccine uptake.
Methods
An ethically-approved online survey strategy was employed for this cross-sectional study conducted between 24th–28th February 2021. The survey employed quantitative questions and open text response options. Quantitative and open text responses were analysed using statistical and thematic analyses, respectively.
Results
There were 108 responses (response rate of 46.3%). The majority (n = 64, 59.3%) were willing to have the vaccine, however, some (n = 44, 40.7%) were not. The main reason behind their willingness to have the vaccine was its ability to reduce the spread of infections and lower mortality (n = 35, 54.7%). However, doubts about the vaccine's efficacy and side effects (n = 26, 56.8%), conspiracy theory concerns about its effects on the Ghanaian race (n = 4, 9.1%), and fertility concerns (n = 2, 4.5%) were some reasons for their hesitance to receive the vaccine. The open text commentary further revealed that the vaccine was thought of as a lifesaving medication, however, clinical safety concerns, lack of education/information and religious beliefs were affecting peoples' willingness to be vaccinated.
Conclusion
Our findings demonstrate the need for an urgent public health educational intervention to address the COVID-19 vaccine hesitancy concerns raised by radiographers to help increase the vaccine uptake.
Implication for practice
The study provides pertinent information to improve COVID-19 vaccine uptake among radiographers to limit the spread of infections.
Keywords: COVID-19, Vaccine hesitancy, Ghana, Radiographer, Survey
Introduction
The first case of Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome Coronavirus 2 (SARS CoV-2)1 was reported in December 2019.2 The disease has since spread to 220 countries and territories across the globe.3 The first cases of COVID-19 in Ghana were recorded on 13th March, 2020.4 As at June, 2021, Ghana had recorded a total of 95,259 cases, with a total of 974 deaths.3 About the same time, a total of 3, 899, 172 deaths had been recorded worldwide out of 179, 686, 071 infections.3 Healthcare workers are amongst those at a high risk for infection with COVID-19. They are a potential source of virus transmission to patients, colleagues, family and friends.5 , 6 Studies from Spain and Ireland, all conducted in 2020 showed very high infection rates amongst healthcare workers, despite provision of adequate personal protective equipment [PPEs] and implementation of suppression strategies for community spread of the virus.7 , 8 In Ghana (as of May 2021), a total of 2079 health workers had been infected with 11 deaths.9 , 10
COVID-19 predominantly affects the respiratory system, resulting in pneumonia.11 Medical imaging is crucial in the early diagnosis, monitoring disease progression and severity of COVID-19.12 , 13 Chest computed tomography (CT), lung ultrasound and chest radiographs, performed by radiographers, were critical adjunctive tools in the early diagnosis and management of COVID-19.14 For example, in a Singapore hospital, chest radiography formed part of the triage protocol in the emergency department, designated screening areas and on the wards for monitoring symptoms (e.g., among patients presenting with acute respiratory symptoms) as well as non-COVID-19 related emergency conditions.15 , 16 This puts radiographers at particularly increased risk of exposure to the virus, because by the nature of their clinical practice they have physical contacts with both confirmed positive and suspected infected patients.17 The complexities for risk of infection among this workforce is further increased in situations where radiological examinations are to be conducted in places not originally designed for this purpose, e.g., in newly created isolation centres with limited PPEs.18 , 19 For example, Foley and colleagues reported that a high proportion of Irish radiographers (45%) were inadvertently exposed to COVID-19-positive patients without adequate PPE.17 A similar trend was reported during the Middle East Respiratory Syndrome (MERS) outbreak in Saudi Arabia to indicate that radiographers had the highest infection rate of 29.4% relative to other healthcare workers.20
Vaccination has been shown to be effective in preventing infection and reducing mortality of most infectious pathologies.21 There has been a rapid development, approval and emergency use authorisation of several brands of COVID-19 vaccines and vaccination commenced by December 2020 in several European countries.22 , 23 Vaccination is confirmed as the key global strategy to protect and mitigate the clinical impact of the COVID-19 virus.24 Meanwhile, acceptability of vaccines is critical, because it underpins the success of any vaccination programme.25 According to the WHO, vaccine hesitancy (defined as the delay in acceptance, reluctance, or refusal of vaccination despite the availability of vaccination services) is one of the top ten threats to global health in 2019.26 Factors influencing vaccine hesitancy are complex, showing varying dynamics among different population groups and locations and to specific vaccines.25 Some of these factors have been identified to be trust in governmental policies and communications, socio-cultural/socioeconomic status, media, educational status, perception of individual and community risk, acquaintance with persons infected by COVID-19 and being a health worker.25, 26, 27, 28, 29
International population-wide studies provided predictions of up to 70% of vaccine acceptability of current potential vaccines.29 Health personnel are said to be a reliable source of vaccine-related information for the public. They are better placed to explain to their patients' concerns they may have about the importance and safety of vaccines.30 Although the frontline healthcare workforce is prioritised for vaccination against COVID-19,31 vaccine acceptance rates and perceptions are diverse. For example, studies among Congolese healthcare workers and Israeli doctors in March and April of 2020 reported acceptance rates of 27.7% and 78.1%, respectively.32 Other studies conducted in Canada and Belgium as well as parts of USA in the last quarter of 2020 reported vaccine acceptance rates in the range of 36%–72.4%.33, 34, 35 Of note, these studies were conducted either before vaccines were developed or before the actual commencement of the vaccination programmes.27 , 28 The lack of information about COVID-specific vaccines and their potential side effects at the time of the studies have the potential of influencing people's responses.29
Vaccine acceptance among the healthcare workforce is crucial to the success of all vaccination programmes globally. However, there were reports of hesitance to receiving the vaccine among the radiography workforce. This study was therefore undertaken as a part of a larger study of the healthcare workforce prior to the intended vaccination exercise to assess the willingness and concerns of radiographers to undergo the COVID-19 vaccination and to suggest recommendations to improve the vaccine uptake among radiographers.
Method
Study design, development and distribution
A cross-sectional research design employing an online survey strategy that uses quantitative questions and some open text response options were utilised to obtain data. The research instrument was a self-reported questionnaire (Appendix 1) developed by two of the researchers (BOB and WKA). This approach was also useful because rapid data/information was needed to develop strategies that would enhance the COVID-19 vaccination process and to promptly address any concern that radiographers may have about the vaccination exercise.
The online survey was active between the 24th-28th February 2021 prior to the commencement of the COVID-19 vaccination in Ghana on 1st March 2021. This gave all the registered radiographers (n = 234) with the professional council (Allied Health Professions Council, AHPC) the opportunity to participate in study. To prevent physical contact with the respondents while limiting the spread of COVID-19 infection during the study period, an online survey strategy was employed. Respondents were given the opportunity to provide their general perspectives about the COVID-19 vaccination as a sequel to the closed-ended questions to gain better understanding and in-depth insight of the research problem. Prior to the data collection process, expert review analysis was used to assess and approve the content and face validity of the questionnaire. This process involved two academic reviewers with experience in the research area. They also assessed the questionnaire functionality and presentation of the survey (across different types of devices, operating system platforms etc) using a 2-point content rating scale (0 = non important; 1 = important) of which none of the questions was rejected. This process helped in evaluating whether each of the measuring items match the given conceptual domain of the study objectives.36 The questionnaire was also piloted among three radiographers and the result was satisfactory. Moreover, a retest (second pilot) was conducted on the closed ended questions and a test-retest statistical analysis yielded a kappa score of 0.80 to imply a strong reliability.
Google Forms (Google, Mountain View, CA) was used to host the research instrument online along with the study information sheet and the associated link was shared and promoted on various platforms of the Ghana Society of Radiographers. The platform allowed respondents to give their consent before they could participate in the study. Each participants' response was coded to ensure anonymity and were digitally stored on google drive with an encrypted password. Prior to commencement, the study received ethical approval from the Ethics and Protocol Review Committee of the School of Biomedical & Allied Health Science (SBAHS/AA/RAD/10679769/2020–2021) and gatekeepers’ permission was obtained from the Ghana Society of Radiographers to engage its membership for this study.
Data analysis
At the end of the study, data was downloaded from Google Forms and prepared for analyses. For the quantitative responses Microsoft Excel 2013 was used to generate graphs for easy presentations of the results. Subsequently, the data were transferred into Statistical Package for the Social Sciences (SPSS) version 23 (IBM, Armonk, NY) for inferential analysis. Spearman correlation was used to assess the level of association between respondent's knowledge levels about COVID-19 vaccines and age. Mann–Whitney U test was used to compare the knowledge levels about COVID-19 vaccine among the gender groups. Furthermore, Wilcoxon signed-rank test was used to assess statistical differences in knowledge levels between those who indicated (un)/willingness to receive a COVID-19 vaccine. Since the intention to vaccinate or not (which is the dependent variable) is a dichotomous data, multivariate binary logistic regression analysis was used to determine the impact of the demographic variables on the intention to vaccinate or receive the COVID-19 vaccine. Statistical significance level was set at p < 0.005. For the open text commentary, thematic analysis was used to generate major themes as recommended.37
Results
-
1.
Quantitative results
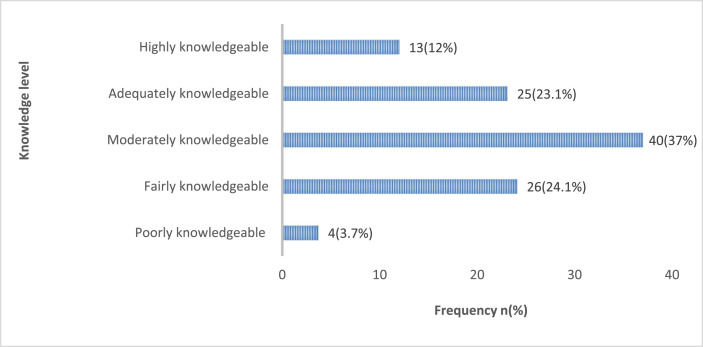
At the end of the study, 108 responses (representing a response rate of 46.1%) were received from radiographers in Ghana about their views on the acceptance of COVID-19 vaccine. The majority (n = 73, 67.6%) of the respondents were males and a good number (n = 66, 61.1%) had worked for 10 or less years. Details of the demographic characteristics of the study respondents are presented in Table 1 . Almost all, except two (1.9%), were aware of intention of the government of Ghana to embark on COVID-19 vaccination. When respondents were asked to self-describe their knowledge levels (on a scale of 1-5, where 1 is poorly knowledgeable and 5 is highly knowledgeable) about COVID-19 vaccines, the majority (n = 40, 37.0%) indicated that they were moderately (averagely) knowledgeable about them, only a few (n = 4, 3.7%) described their knowledge as poor (Fig. 1 ). However, the knowledge levels of the respondents did not significantly correlate with age (rs = 0.152, p = 0.117), neither did they differ among the gender groups (Mann Whitney U, p = 0.253). The results further showed that the respondents were aware of many types of COVID-19 vaccines (Table 2 ). Only one (0.9%) did not know about any of the COVID-19 vaccines.
Table 1.
Demographic characteristics of the respondents.
| Demographic parameters | Frequency n (%) |
|---|---|
| Gender | |
| Male | 73 (67.6%) |
| Female | 35 (32.4%) |
| Age (yrs) | |
| 20–29 | 55 (50.9%) |
| 30–39 | 35 (32.4%) |
| 40–49 | 16 (14.8% |
| 50–59 | 2 (1.9%) |
| ≥60 | 0 (0%) |
| Years of practice | |
| <10 | 66 (61.1%) |
| 10–20 | 35 (32.4%) |
| >20 | 7 (6.5%) |
| Sector of practice | |
| Government sector | 97 (73.1%) |
| Private sector | 20 (18.5%) |
| Quasi-government | 9 (8.3%) |
| Highest educational level | |
| Certificate/diploma qualification | 5 (4.6%) |
| Bachelor's degree (BSc) | 81 (75.0%) |
| Postgraduate certificate/diploma | 4 (3.7%) |
| Master's degree | 15 (13.9%) |
| Doctor of Philosophy | 3 (2.8%) |
Key:yrs = years
Figure 1.
Respondents self-described knowledge level about COVID-19 vaccines (Note: Moderate is average and Adequate is satisfactory).
Table 2.
Types of vaccines known by respondents.
| Types of vaccines | Frequency(n) | Percentage (%) |
|---|---|---|
| Oxford-Astra Zeneca | 64 | 59.3 |
| Pfizer-BioNTech | 71 | 65.7 |
| Moderna | 26 | 24.1 |
| Sputnik V | 29 | 26.9 |
| Novavax (NVX-CoV2373) | 16 | 14.8 |
| Sinopharm | 8 | 7.4 |
| Sinovac | 21 | 19.4 |
| Johnson and Johnson's Janssen | 2 | 1.9 |
| I do not know | 1 | 0.9 |
When questioned on whether they will receive a COVID-19 vaccine, the majority (n = 64, 59.3%) said yes, however, a significant number (n = 44, 40.7%), said no. Respondents who indicated their willingness to receive a COVID-19 vaccine revealed that the ability of the vaccine to help curb the spread and reduce the number of cases and deaths (n = 35, 54.7%) was their key reason among others (Table 3 ). However, the main reason provided for not receiving a COVID-19 vaccine was the fact that they were not convinced about its effectiveness, efficiency, and side effects (n = 26, 56.8%). Others mentioned the lack of adequate research evidence to back the potency of the vaccines (n = 5, 11.4%), limited evidence and concerns about its effects on the African race and Ghanaian population (n = 4, 9.1%), lack of adequate information and education (n = 3, 6.8%) about COVID-19 vaccines, lack of interest (n = 2, 4.5%) and a very small number of respondents appeared to be influenced by a range of conspiracy theories including the effects of the vaccine on fertility (n = 2, 4.5%). Further reasons are provided in Table 4 . Fig. 2 shows the key demographic characteristics of respondents who indicated their (un)/willingness to receive a COVID-19 vaccine. Given the opportunity for them to prescribe interventions that could be used to encourage them to have a COVID-19 vaccine, some said they would accept a COVID-19 vaccine if there were more than enough evidence to show that it provides immunity against the infection and it's variants (n = 14, 31.8%) and no adverse reactions happen to people of their race after they have taken it for a while (n = 10, 22.7%). Others also indicated that they would receive a vaccine if it were proven beyond reasonable doubt that it is generally safe and would not affect their spiritual wellbeing (n = 3, 6.8%). However, some (n = 17, 38%) indicated that nothing will encourage them except God. Inferential statistics further showed that the knowledge levels about COVID-19 vaccines between those who indicated their (un)/willingness to receive a vaccine were not statistically significant (Wilcoxon signed-rank, p = 0.132). Moreover, the intention to receive the vaccine did not statistically associate with educational level (AOR = 1.425; CI 95%: 0.596–3.404; p = 0.426), age (AOR = 0.927; CI 95%: 0.388–2.212; p = 0.864), gender (AOR = 0.494; CI 95%: 0.214–1.141; p = 0.099), years of practice (AOR = 0.942; CI 95%: 0.485–1.831; p = 0.861) and work setting (AOR = 0.842; CI 95%:0.337–2.016; p = 0.671).
-
2.
Open text results: perception about COVID-19 vaccination
Table 3.
Reasons why respondents will accept the COVID-19 vaccine (n = 64).
| Reason | Frequency |
|
|---|---|---|
| n | % | |
| Vaccination will help curb the spread and reduce the number of cases and deaths. | 35 | 54.7 |
| It will help us to achieve heard immunity. | 9 | 14.1 |
| I trust the effectiveness, efficiency of the vaccine which comes with minimal side effects. | 2 | 3.1 |
| Taking of the vaccine is inevitable, it is the only main solution to the pandemic. | 8 | 12.5 |
| I have enough knowledge of it. | 2 | 3.1 |
| It has been scientifically tested and approved by the food and drugs authority (FDA) and WHO. | 4 | 6.3 |
| It is quite safe, and the benefits outweigh the risk. | 3 | 4.7 |
| I think it will work like other vaccines worked in the past. | 1 | 1.6 |
Table 4.
Reasons for not accepting COVID-19 vaccines (n = 44).
| Reason | Frequency |
|
|---|---|---|
| n | % | |
| Not convinced about its effectiveness and side effects. | 25 | 56.8 |
| Not interested. | 2 | 4.5 |
| No evidence on effects on my type of race and population (Ghanaians). | 4 | 9.1 |
| Due to adverse reactions to previous vaccines eg. H1N1 vaccine in 2012. | 1 | 2.3 |
| Lack of adequate information and education. | 3 | 6.8 |
| Lack of enough research evidence to back the potency of the vaccines. | 5 | 11.4 |
| Not sure if it affects fertility. | 2 | 4.5 |
| I have heard of some severe side effects. | 1 | 2.3 |
| I do not know whether people with underlying conditions can take it. | 1 | 2.3 |
Figure 2.
Key demographic characteristics of respondents who indicated their unwillingness and willingness to have a COVID-19 vaccine.
The various themes developed from the open text responses on the perception of respondents about COVID-19 vaccination were (i) lifesaving medication, (ii) safety doubts and concerns, (iii) lack of education/information and (iv) religious beliefs. Further details are presented below and is schematically presented in Fig. 3 .
-
(i)
Lifesaving medication
Figure 3.
Respondents' perception of about COVID-19 vaccination.
Some respondents perceived COVID-19 vaccines as lifesaving medication that would fight against the COVID-19.
“I think it can prevent the spread of the virus” (Rad 3)
“it's been tested and proven to be effective against the pandemic” (Rad 56)
“It is a preventive way to control the spread and effect of the virus and reduce the death rates” (Rad 63).
-
(ii)
Safety doubts and concerns
Several of the respondents also had some doubts and concerns about the safety of the vaccines.
“Efficacy of the vaccines have not been adequately confirmed” (Rad 31).
“We should really consider the efficacy rate of the various vaccines taking into consideration our race and setting and not because it's considered safe for other races or settings” (Rad 22).
“I don't fully trust it” (Rad 98).
Again, some also held onto the opinion that since it is statistically evident that the Western world were more affected by COVID-19 than African countries there was no reason why African leaders should rush in getting its citizens vaccinated for a pandemic of which they suffer the least. Thus, some did not trust the government's intentions in the fight against COVID-19.
“I don't trust our leaders. Africans are less affected compared with the western world. Why should the government go for a vaccine and expose the citizens to be used for clinical trials for vaccination of a drug which has not been fully tried and tested. It has only pass emergency approval” (Rad 40).
-
(iii)
Lack of education
A few of the respondents also felt that education about the vaccines was not enough to help them make an informed decision on whether to receive the vaccines or not, this would help to allay the fears of people. Others also felt that lack of proper education created a vacuum or the platform for people to peddle falsehood information which has “polluted” people's mind about the vaccines.
“I think there should be enough education about the vaccine to allay people's fears about the vaccine” (Rad 50).
“I think it's a step in the right direction. It's unfortunate however that Nay Sayers and Charlatans have been given the platform to pollute people's minds” (Rad 17).
-
(iv)
Religious beliefs
Due to the religious belief, some respondents perceived that it was not necessary to accept the vaccine because God would protect them from getting infected by the COVID-19 virus. One respondent, in particular, indicated that:
“I have God” (Rad 10).
Discussion
Medical imaging is imperative in evidence-based choice of action in the diagnosis, management and treatment of COVID-19 patients.14 , 18 , 38, 39, 40, 41, 42, 43, 44, 45, 46, 47 Despite the dreadful nature of the COVID-19 pandemic and post lock down effects in Ghana, it took some time for the government to secure vaccines for its people. In an attempt to combat COVID-19, radiographers were identified as part of the front-line healthcare experts who are at a high risk to be infected.17 , 19 , 37, 38, 39 This is due to the nature of the profession and the role medical imaging plays in the diagnosis and care management of COVID-19 patients.
The current study sought to identify the concerns and readiness of radiographers in Ghana to take the COVID-19 vaccination. Out of 234 registered radiographers in Ghana, the study had a response rate of 46.1%, which is lower than the values obtained in quite recent studies among radiographers in Ghana48 , 49 but is within a reasonable range to yield comparable results for similar inferences.50 The awareness among the radiographers about the intent of the government to pursue COVID-19 vaccination was found to be encouraging which is attributed to the promotion of the vaccination process in the media. This was relatively higher than the COVID-19 vaccination awareness level (40.8%) observed in a similar Ethiopian cohort51 and other countries such as in Democratic Republic of Congo52 and Saudi Arabia.53 Similarly, Shaw et al.30 received good response to the uptake of the vaccination in the USA due to a high promotional approach of the vaccination programme which created more awareness among the people. In contrast to a related survey in Egypt, a greater number of respondents had inadequate information about the vaccination programme.54 Besides, the current study identified reasonable knowledge among respondents about various COVID-19 vaccines. It was also encouraging that the majority of respondents in the current study agreed to be vaccinated with several reasons including the capability of the COVID-19 vaccine to limit the spread of infections and reduce the number of deaths.
Notwithstanding, appreciable number of radiographers, who were youthful and self-reported their COVID-19 vaccine knowledge levels as mainly moderate/average (38.6%) and adequate/satisfactory (27.3%) (Fig. 1), were against the vaccination and gave noteworthy explanations. In particular, a few believed that they have God to protect them and so will not vaccinate, while others wanted to wait till when no adverse reaction happens to people of their race or population after they have taken it for a while. This was found to be interesting as one would have expected that as health professionals, they would rather take the vaccine to encourage family members to vaccinate. This attitude could be ascribed to misinformation (conspiracy theories) on social media regarding the vaccines and previous knowledge of vaccine risks which some respondents might have been exposed to. Again, some also held onto the opinion that since it is statistically evident that the western world is more affected by COVID-19 than African countries there was no reason why African leaders should rush in getting its citizens vaccinated for a pandemic of which they suffer the least. Thus, some did not trust the government's intentions in the fight against COVID-19 with the vaccination exercise. A study in Italy had respondents showing similar misconceptions about the vaccine which led to hesitancy to being vaccinated.55 Moreover, a reasonable number of the respondents questioned the intentions of the vaccination and indicated that unless it is established beyond reasonable uncertainty that the COVID-19 vaccine is generally safe and would not affect their spiritual well-being, they will not undergo the vaccination; a belief in illogical forces which appears to be endemic among some Ghanaian radiographers.56 Vaccine safety has been a concern among several healthcare workers which was demonstrated in the current study. A few of the respondents cited the known adverse reactions experienced with previous vaccines such as the H1N1 vaccine in 2012. These findings support previous conclusions about healthcare workers anxieties regarding the safety of vaccines.57 The unwillingness to be acquiescent to COVID-19 vaccine was as a result of suspicions about the efficacy and besides, the side effects of the vaccine, as was the case in the findings of Dini et al.55 Some respondents were also particularly concerned about the vaccine's tolerability among the Ghanaian race. This was not surprising as different racial/ethnic depictions in COVID-19 vaccine trials is imperative because drugs and vaccines can diversely affect groups reflecting disparity in underlying experiences and environmental exposure.58 Others felt there were not enough evidence to establish the potency of the vaccines. Although COVID-19 vaccines are highly effective, particularly against hospitalisation and severe disease, no vaccine is 100% protective.59 , 60 Based on some of these misgivings about the vaccines in general, some respondents reported that nothing will inspire them to take the vaccine apart from God. This is not surprising as Ghana's population is made up of about 71% Christians and 17% Muslims.61 Therefore, there would be a need for religious leaders to play a critical role in dispelling the myths for the success of the vaccination programmes. This is important because vaccination of healthcare personnel is a critical aspect of occupational medicine strategies and infection control programmes within the healthcare services.62
The survey further revealed that the awareness level about COVID-19 vaccines between those who showed their inclination to receive it and those otherwise, was not statistically significant. This implies that the unwillingness to partake in the vaccination was not because of lack of awareness. Moreover, the performed statistical tests demonstrated that the self-reported knowledge levels of the respondents did not significantly correlate with age, neither did they differ among the gender groups. This is contrary to the findings of Agyekum and colleagues63 which demonstrated that certain demographic parameters impact on the intention to vaccinate. The findings of the current study demonstrated that the demographic variables of the radiographers were not a determinant of an intention to vaccinate, and may further suggest that the positions taken by the radiographers could be due to their self-conviction about the vaccine.
Since 1st March 2021, when the vaccination programme (Oxford–AstraZeneca COVID-19 vaccines) started in Ghana, only 1.3% of the entire Ghanaian population (30+ million) had been fully vaccinated and 2.8% had received a single dose as of July 2021.64 , 65 Even though this study could not obtain data on the total number of radiographers who have been vaccinated so far, it is anticipated that an innovative strategy would be needed to address the concerns raised by participants of the current study to improve the vaccine acceptability among radiographers in Ghana. In tackling these concerns, public health education would be important. Particularly, there should be more proof to dispel the conspiracy theories being spread about the COVID-19 vaccination. As a proactive method to support the vaccination, this work has already led to the initiation of educational strategies aimed at encouraging vaccine uptake by radiographers.
Conclusion
The study showed that a large proportion of the Ghanaian radiography workforce were willing to receive the vaccine, however, a significant number were not. The observed results call for an urgent public health educational intervention from stakeholders to promptly address the COVID-19 vaccine hesitancy concerns raised by the radiographers to help increase vaccine uptake. In tackling these concerns, more education about the COVID-19 vaccines is needed to encourage radiographers to develop interest in accepting them. Particularly, when offering the education (through e.g. specialised CPD, seminars, conferences, talk shows etc), there should be more proof of the efficacy of the various vaccines in helping to limit the spread of infections of the various variants. Furthermore, there is a need for more information and evidence to be shared on the safety of the vaccines, particularly, among their race and tribes (e.g. among the Ghanaian population). This safety education must also try to allay the fears of those who have reacted adversely to other vaccines previously, those who think the vaccination is an attempt to make people infertile, and those with underlying medical conditions but were unsure they could take the vaccines. There should also be more than enough evidence to suggest that the vaccination exercise is generally safe. Moreover, education to dispel myths and conspiracy theories about the COVID-19 vaccine is highly needed.
Conflict of interest statement
None.
Acknowledgements
We would like to thank the leadership of the Ghana Society of Radiographers as well as the members for supporting and participating in this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.radi.2021.09.015.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.World Health Organization Naming the coronavirus disease (COVID-19) and the virus that causes it. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it Available from:
- 2.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio-Med Ateneo Parmense. 2020-19;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Worldometers Info [Internet] Reported cases and deaths by country or territory. https://www.worldometers.info/coronavirus/ Available from:
- 4.COVID-19 Updates Ghana. First confirmed COVID-19 cases in Ghana 12 Mar 2020 (ghanahealthservice.org). Accessed May 08, 2021.
- 5.Wang J., Zhou M., Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020 May;105(1):100–101. doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Asad H., Johnston C., Blyth I., Holborow A., Bone A., Porter L., et al. Health care workers and patients as Trojan horses: a COVID19 ward outbreak. Infect Prevent Pract. 2020;2:100073. doi: 10.1016/j.infpip.2020.100073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Suárez-García I., Martínez de Aramayona López M.J., Sáez Vicente A., Lobo Abascal P. SARS-CoV-2 infection among healthcare workers in a hospital in Madrid, Spain. J Hosp Infect. 2020;106(2):357–363. doi: 10.1016/j.jhin.2020.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Government of Ireland . Irish Statute Book; Dublin: 2020. Health (preservation and protection and other emergency measures in the public interest) act 2020.http://www.irishstatutebook.ie/eli/2020/act/1/enacted/en/html Available at: [Google Scholar]
- 9.MyJoyOnline 789 nurses and midwives test positive for covid-19 in 2021 – general secretary, GRNMA. https://www.myjoyonline.com/789-nurses-and-midwives-test-positive-for-covid-19-in-2021-general-secretary-grnma/?utm_source=rss&utm_medium=rss&utm_campaign=789-nurses-and-midwives-test-positive-for-covid-19-in-2021-general-secretary-grnma Available from:
- 10.Kwofi M. COVID-19 hits 450 Doctors,kills 7. https://www.graphic.com.gh/news/general-news/covid-19-hits-450-doctors-kills-7.html Available from.
- 11.Cellina M., Orsi M., Oliva G. How to reorganize the radiology departments to face the 2019 coronavirus disease outbreak. Disaster Med Public Health Prep. 2020;14(6):789–791. doi: 10.1017/dmp.2020.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kooraki S., Hosseiny M., Myers L., Gholamrezanezhad A. Coronavirus (COVID-19) outbreak: what the department of radiology should know. J Am Coll Radiol. 2020;17(4):447–451. doi: 10.1016/j.jacr.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu X., Yu C., Qu J., Zhang L., Jiang S., Huang D., et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imag. 2020;47:1275–1280. doi: 10.1007/s00259-020-04735-9N. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stogiannos N., Fotopoulos D., Woznitza N., Malamateniou C. COVID-19 in the radiology department: what radiographers need to know. Radiography. 2020 Aug;26(3):254–263. doi: 10.1016/j.radi.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chia A., Cheng L.T., Wijaya L., Png M.A., Sim W.Y., Hong W.L., et al. Chest radiographs and CTs in the era of COVID-19: indications, operational safety considerations and alternative imaging practices. Acad Radiol. 2020;27(9):1193–1203. doi: 10.1016/j.acra.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kooraki S., Hosseiny M., Myers L., Gholamrezanezhad A. Coronavirus (COVID-19) outbreak: what the department of radiology should know. J Am Coll Radiol. 2020;17(4):447–451. doi: 10.1016/j.jacr.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Foley S.J., O'Loughlin A., Creedon J. Early experiences of radiographers in Ireland during the COVID-19 crisis. Insights Imaging. 2020;11:104. doi: 10.1186/s13244-020-00910-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pereira J.M., Silva C., Freitas D., Salgado A. Burnout among Portuguese radiographers during the COVID-19 pandemic. Radiography. 2021;27(4):1118–1123. doi: 10.1016/j.radi.2021.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lewis S., Mulla F. Diagnostic radiographers' experience of COVID-19, Gauteng South Africa. Radiography. 2021 May;27(2):346–351. doi: 10.1016/j.radi.2020.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alraddadi B.M., Al-Salmi H.S., Jacobs-Slifka K., Slayton R.B., Estivariz C.F., Geller A.L., et al. Risk factors for Middle East respiratory syndrome coronavirus infection among healthcare personnel. Emerg Infect Dis. 2016;22:1915–1920. doi: 10.3201/eid2211.160920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Osterholm N.S., Kelley A., Sommer E.A., Belongia E.A. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:36–44. doi: 10.1016/S1473-3099(11)70295-X. [DOI] [PubMed] [Google Scholar]
- 22.European Centre for Disease Prevention and Control (ECDC) First COVID-19 vaccine authorized for use in the European union. https://www.ecdc.europa.eu/en/news-events/first-covid-19-vaccine-authorised-use-european-union Stockholm. Available online:
- 23.EMA recommends COVID-19 vaccine moderna for authorisation in the EU. https://www.ema.europa.eu/en/news/ema-recommends-covid-19-vaccine-moderna-authorisation-eu Available online:
- 24.Anderson R.M., Vegvari C., Truscott J., Collyer B.S. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet. 2020 Nov 21;396(10263):1614–1616. doi: 10.1016/S0140-6736(20)32318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.MacDonald N.E., Eskola J., Liang X., Chaudhuri M., Dube E., Gellin B. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization (WHO) 2019. Ten threats to global health in 2019.https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 Available online: [Google Scholar]
- 27.Harapan H., Wagner A.L., Yufika A., Winardi W., Anwar S., Gan A.K., et al. Acceptance of a COVID-19 vaccine in southeast Asia: a cross-sectional study in Indonesia. Front Public Health. 2020 Jul 14;8:381. doi: 10.3389/fpubh.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020 Sep 29;38(42):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021 Feb;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shaw J., Stewart T., Anderson K.B., Hanley S., Thomas S.J., Salmon D.A., et al. Assessment of U.S. health care personnel (HCP) attitudes towards COVID-19 vaccination in a large university health care system. Clin Infect Dis. 2021 Jan 25 doi: 10.1093/cid/ciab054. ciab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.WHO Coronavirus Disease (COVID-19): vaccine access and allocation. https://www.who.int/news-room/q-a-detail/coronavirus-disease-(covid-19)-vaccine-access-and-allocation Available online:
- 32.Sallam M. Vaccines; Basel: 2021. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Verger P., Scronias D., Dauby N., Adedzi K.A., Gobert C., Bergeat M., et al. Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020. Euro Surveill. 2021 Jan;26(3):2002047. doi: 10.2807/1560-7917.ES.2021.26.3.2002047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shekhar R., Sheikh A.B., Upadhyay S., Singh M., Kottewar S., Mir H., et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines. 2021 Feb 3;9(2):119. doi: 10.3390/vaccines9020119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gadoth A., Halbrook M., Martin-Blais R., Gray A., Tobin N.H., Ferbas K.G., et al. Cross-sectional assessment of COVID-19 vaccine acceptance among health care workers in Los Angeles. Ann Intern Med. 2021 Jun;174(6):882–885. doi: 10.7326/M20-7580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bolarinwa O.A. Principles and methods of validity and reliability testing of questionnaires used in social and health science researches. Niger Postgrad Med J. 2015 Oct-Dec;22(4):195–201. doi: 10.4103/1117-1936.173959. [DOI] [PubMed] [Google Scholar]
- 37.Hsieh H.F., Shannon S.E. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 38.Akudjedu T.N., Mishio N.A., Elshami W., Culp M.P., Lawal O., Botwe B.O., et al. The global impact of the COVID-19 pandemic on clinical radiography practice: a systematic literature review and recommendations for future services planning. Radiography. 2021;27(4):1219–1226. doi: 10.1016/j.radi.2021.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Akudjedu T.N., Botwe B.O., Wuni A.R., Mishio N.A. Impact of the COVID-19 pandemic on clinical radiography practice in low resource settings: the Ghanaian radiographers' perspective. Radiography. 2021 May;27(2):443–452. doi: 10.1016/j.radi.2020.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yasin B., Barlow N., Milner R. The impact of the Covid-19 pandemic on the mental health and work morale of radiographers within a conventional X-ray department. Radiography. 2021;27(4):1064–1072. doi: 10.1016/j.radi.2021.04.008. [DOI] [PubMed] [Google Scholar]
- 41.Elshami W., Akudjedu T.N., Abuzaid M., David L.R., Tekin H.O., Cavli B., et al. The radiology workforce’s response to the COVID-19 pandemic in the Middle East, North Africa and India. Radiography. 2021;27(2):360–368. doi: 10.1016/j.radi.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Akudjedu T.N., Lawal O., Sharma M., Elliott J., Stewart S., Gilleece T., et al. Impact of the COVID-19 pandemic on radiography practice: findings from a UK radiography workforce survey. BJR Open. 2020 Sep 2;2(1):20200023. doi: 10.1259/bjro.20200023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.England A., Littler E., Romani S., Cosson P. Modifications to mobile chest radiography technique during the COVID-19 pandemic - implications of X-raying through side room windows. Radiography. 2021 Feb;27(1):193–199. doi: 10.1016/j.radi.2020.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zanardo M., Martini C., Monti C.B., Cattaneo F., Ciaralli C., Cornacchione P., et al. Management of patients with suspected or confirmed COVID-19, in the radiology department. Radiography. 2020;26:264–268. doi: 10.1016/j.radi.2020.04.010. PMC-PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sim W.Y., Chen R.C., Aw L.P., Abu Bakar R., Tan C.C., Heng A.L., et al. How to safely and sustainably reorganise a large general radiography service facing the COVID-19 pandemic. Radiography. 2020 Nov;26(4):e303–e311. doi: 10.1016/j.radi.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ruiz C., Llopis D., Roman A., Alfayate E., Herrera-Peco I. Spanish radiographers' concerns about the COVID-19 pandemic. Radiography. 2021 May;27(2):414–418. doi: 10.1016/j.radi.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shanahan M.C., Akudjedu T.N. Australian radiographers' and radiation therapists' experiences during the COVID-19 pandemic. J Med Radiat Sci. 2021 Jun;68(2):111–120. doi: 10.1002/jmrs.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Botwe B.O., Antwi W.K., Arkoh S., Akudjedu T.N. Radiographers' perspectives on the emerging integration of artificial intelligence into diagnostic imaging: the Ghana study. J Med Radiat Sci. 2021 Feb 14 doi: 10.1002/jmrs.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ashong G.G.N.A., Rogers H., Botwe B.O. Anim-Sampong S. Effects of occupational stress and coping mechanisms adopted by radiographers in Ghana. Radiography. 2016;22(2):112–117. doi: 10.1016/j.radi.2015.09.002. [DOI] [Google Scholar]
- 50.Morton B.M.S., Bandara D.K., Carr A.E.P. In the 21st Century, what is an acceptable response rate? Aust N Z J Publ Health. 2012;36(2):106–108. doi: 10.1111/j.1753-6405.2012.00854.x. [DOI] [PubMed] [Google Scholar]
- 51.Zewude B., Habtegiorgis T. Willingness to take COVID-19 vaccine among people most at risk of exposure in southern Ethiopia. Pragmatic Observational Res. 2021 May 27;12:37–47. doi: 10.2147/POR.S313991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nzaji K.M., Ngombe K.L., Mwamba N.G., Ndala B.D.B., Miema M.J., Lungoyo L.C., et al. Acceptability of vaccination against covid-19 among healthcare workers in the democratic republic of the Congo. Pragmatic Observational Res. 2020;11:103–109. doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Qattan A.M.N., Alshareef N., Alsharqi O., Al Rahahleh N., Chirwa G.C., Al-Hanawi M.K. Acceptability of a COVID-19 vaccine among healthcare workers in the kingdom of Saudi Arabia. Front Med. 2021;8:644300. doi: 10.3389/fmed.2021.644300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fares S., Elmnyer M.M., Mohamed S.S., Elsayed R. COVID-19 vaccination perception and attitude among healthcare workers in Egypt. J Community Med Prim Health Care. 2021;(12):1–9. doi: 10.1177/21501327211013303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gerussi V., Peghin M., Palese A., Bressan V., Visintini E., Bontempo G., et al. Vaccine hesitancy among Italian patients recovered from COVID-19 infection towards influenza and sars-Cov-2 vaccination. Vaccines. 2021;9(2):172. doi: 10.3390/vaccines9020172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Antwi W.K., Reeves P., Ferris C., Aziato L. Behavioural beliefs of Ghanaian radiographers and reporting of child physical abuse. Radiography. 2019 Feb;25(1):51–57. doi: 10.1016/j.radi.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 57.Dini G., Toletone A., Sticchi L., Orsi A., Bragazzi N.L., Durando P. Human Vaccines & Immunotherapeutics; 2017. Influenza vaccination in healthcare workers: a comprehensive critical appraisal of the literature. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lopez L., Hart L.H., Katz M.H. Racial and ethnic health disparities related to COVID-19. J Am Med Assoc. 2021;325(8):719–720. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- 59.WHO Coronavirus disease (COVID-19): vaccines safety. https://www.who.int/news-room/q-a-detail/coronavirus-disease-(covid-19)-vaccines-safety
- 60.Yiwen K., Hegney D., Drury V. A comprehensive systematic review of healthcare workers' perceptions of risk from exposure to emerging acute respiratory infectious diseases and the perceived effectiveness of strategies used to facilitate healthy coping in acute hospital and community healthcare settings. JBI Libr Syst Rev. 2010;8(23):917–971. doi: 10.11124/01938924-201008230-00001. [DOI] [PubMed] [Google Scholar]
- 61.Ghana statistical Service Ghana population 2021. Worldpopulationreview.com/countries/ghana-population
- 62.Maltezou H.C., Theodoridou K., Ledda C., Rapisarda V., Theodoridou M. Vaccination of healthcare workers: is mandatory vaccination needed? Expet Rev Vaccine. 2018 doi: 10.1080/14760584.2019.1552141. [DOI] [PubMed] [Google Scholar]
- 63.Agyekum A.W., Afrifa-Anane G.F., Kyei-Arthur F., Addo B. Research article acceptability of COVID-19 vaccination among health care workers in Ghana. Adv Trop Med Public Health Int. 2021:1–18. doi: 10.1155/2021/9998176. [DOI] [Google Scholar]
- 64.Statista Cumulative number of COVID-19 vaccine doses administered in Ghana 2021. https://www.statista.com/statistics/1227780/total-number-of-covid-19-vaccination-doses-in-ghana/
- 65.Google COVID-19 Vaccination update COVID-19 vaccine Ghana. https://www.google.com/search?q=covid-19+vaccination+in+Ghana&rlz
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.