Abstract
Objectives
Cerebral palsy is a unique physical disability that primarily affects children's gross motor functions and postural control. Cerebral palsy has a direct impact on children's daily activities and quality of life. This study aims to determine the relationship between spasticity, motor function, postural stability, and the quality life of children with cerebral palsy.
Methods
Forty-five children (age range 4–6 years) diagnosed with spasticity from cerebral palsy participated in this study. Spasticity was evaluated by the modified Ashwarth scale; the children's functions were evaluated by gross motor functional measures, postural stability was evaluated by biodex balance system, and quality of life was measured with the pediatric quality of life inventory.
Results
There was a strong positive correlation between the degree of spasticity and quality of life. Additionally, there was a significantly strong association between spasticity and gross motor function. In contrast, there was no correlation between spasticity and postural stability indices. Moreover, there was a strong positive correlation between quality of life and gross motor function. Lastly, there was no association between quality of life and the postural stability index.
Conclusion
The findings highlight the impact of spasticity on motor function and the quality of life of a cohort of children with cerebral palsy. These findings may determine therapeutic interventions and priorities to plan physical therapy programs. Such measures may overcome the main cause of disorders that delay and undermine the daily routines of the affected children.
Keywords: Cerebral palsy, Function, Postural stability, Quality of life, Spasticity
الملخص
أهداف البحث
الشلل الدماغي هو إعاقة جسدية فريدة تؤثر في الغالب على الوظائف الحركية الكبرى للأطفال مع تأثير مباشر على التحكم في الوضع. للشلل الدماغي تأثير مباشر على نشاط الطفل اليومي مع تأثيره على نوعية الحياة. تهدف هذه الدراسة إلى تحديد العلاقة بين التشنج، والوظيفة الحركية، والاستقرار الوضعي، ونوعية الحياة لدى الأطفال المصابين بالشلل الدماغي.
طرق البحث
شارك في هذه الدراسة ٤٥ طفلا (تتراوح أعمارهم من ٤ إلى ٦ سنوات)، تم تشخيص إصابتهم بالتشنج الناتج عن الشلل الدماغي. وتم تقييم التشنج بمقياس أشوارث المعدل. كما تم تقييم وظيفة الطفل من خلال المقاييس الوظيفية الحركية الإجمالية، وتم تقييم ثبات الوضع من خلال نظام توازن بيودكس، في حين تم قياس جودة الحياة من خلال موجودات جودة حياة الأطفال.
النتائج
توجد علاقة ارتباط موجبة قوية بين درجة التشنج ونسبة جودة الحياة. بالإضافة إلى ذلك، كان هناك ارتباط قوي بشكل ملحوظ بين التشنج والوظيفة الحركية الإجمالية. في المقابل، لم يكن هناك ارتباط بين مؤشرات استقرار التشنج والوضعية. علاوة على ذلك، كان هناك ارتباط إيجابي قوي بين نوعية الحياة والوظيفة الحركية الإجمالية. أخيرا، لم يكن هناك ارتباط بين النسبة المئوية لجودة الحياة ومؤشر ثبات الوضع.
الاستنتاجات
تسلط النتائج الضوء على تأثير التشنج على الوظيفة الحركية ونسبة صحة الجودة في مجموعة من الأطفال المصابين بالشلل الدماغي. قد تحدد هذه النتائج التدخلات العلاجية والأولويات لتخطيط برامج العلاج الطبيعي. وقد تتغلب هذه الإجراءات على السبب الرئيس للاضطراب الذي يؤخر ويقوض الروتين اليومي للأطفال المصابين.
الكلمات المفتاحية: الشلل الدماغي, الوظيفة, التشنج, الاستقرار الوضعي, نوعية الحياة
Introduction
Cerebral palsy (CP) is the primary origin of physical incapacity in children, with an expected frequency of 2.11 per 1,000 live births.1 Impaired development of movement and posture are essential for CP diagnoses.2 The problems associated with movement and posture in children with CP include abnormal muscle tone and spasticity, activity limitation, lack of equilibrium and alterations in the alignment that affect motor development, and gross motor function.2
Children with spastic CP are characterized by increased muscle tone, paresis, and involuntary motor control, and usually have difficulty in maintaining balance in an upright posture, which require a high center of mass and small base of support.3 Spasticity is a concern and involves neuromuscular syndromes that affect the health life quality of children with CP.4
Spasticity can lead to functional disorders associated with children's daily activities such as walking, dressing, eating, going to the toilet, and hygiene. Furthermore, spasticity can cause pain; muscular spasms; limitations of movement in bed; improper transfers; delayed development in sitting, standing, and walking; abnormal posture; and joint and bone deformity as a result of shorting and contractures that may lead to subluxation or dislocation with the children finally becoming full dependent.5
Postural and movement disorders that result in muscle tone abnormality, functional restriction, and improper body equilibrium and righting can affect sitting posture and lead to compensatory positions in the cardinal planes.6,7 This can result in a diminished ability to preserve one's posture against gravity due to inadequate trunk control and delayed limb movement. Abnormal posture and delayed development of motor control resulting in delayed sitting and standing are the main causes of postural instability.8
Postural stability is the ability to maintain the position of one's body in space to maintain alignment and control.9,10 Balance or postural control can be defined as the ability to preserve the center of body mass within its control area.9,11 Steady sitting positions for children with CP can maximize their development of hand-eye coordination, upper extremities functions, self-care and skill functions, cognitive development, and social communication.12,13
Health-related quality of life (HRQoL) is an individual multidimensional concept that measures the physical, social, and psychological aspects of children's health.14 HRQoL is an essential tool for assessing children and adolescents with CP.15
The functional deficits of children with CP due to the associated impairments of physical activities, social difficulties, cognitive delay, sensory disorders, and emotional problems lead to reductions in children's ability to accomplish their allocated-social communications and major breakdowns in HRQOL levels.16,17
QOL is an applicable health indicator that provides evidence about children's clinical state that influences their life and guides public policies for improving QOL.18 The National Policy on Health Promotion (PNPS) highlights the hunt for value and proposes the advancement of QOL and the decline of health threats related to conditioning variables, including lifestyle, education, culture, environment, and fundamental services.19
This study attempts to understand whether spasticity affects motor function, postural stability, and health life quality. Thus, the purpose of current study was to determine the relationship between spasticity, function, postural stability, and QOL in children with CP.
Materials and Methods
This study was conducted between April and October 2020. Parents were asked to an informed consent forms and agree to the participation and evaluation of their children in the study. Forty-five children with spastic CP were selected from the outpatient clinic of faculty of physical therapy at Cairo University. The inclusion criteria were a) spastic CP, b) age of 4–6 years of both genders, and c) spasticity grades 1 and 1+ on the modified Ashworth scale,20 while the exclusion criteria were a) permanent deformities or severe contractures of upper or lower limbs or vertebral column, b) breathing disorders, c) an epilepsy or seizure disorder that was resistant to treatment, or d) orthopedic surgery owing to pathology and Botox injections during the 12 months that preceded the study.
Procedures
-
1.
The modified Ashworth scale is quick and easy valid test used to grade the degree of spasticity that does not require any equipment. It is performed manually to determine the resistance of lower limb muscles to passive stretching as a measure of degree of spasticity.20 All selected children were affected by spasticity classified with grades 1 and 1+.21
-
2.
Gross Motor Functional Measurement-88 (GMFM-88): is a standard principle-test aiming to evaluate alterations of function in different milestones for children diagnosed with CP.22 There were 88 total items divided into five scopes: a) lying and rolling, b) sitting, c) crawling and kneeling, d) standing e) walking, running, and jumping. A 4-point Likert scale was used with the score. The GMFM scores are acceptably reliable for children with CP.23 The GMFCS has been successfully implemented worldwide in a range of settings including routine clinical management.20
-
3.
The pediatric quality of life inventory“TM”(PedsQLTM): Health-related QOL was used to assess QOL by (PedsQL™) 4.0 generic core scale which measures HRQOL in normal children and adolescents as well as those with acute or chronic disorders. PedsQL™ is a reliable and valid measurement of the pediatric health outcome, as it enables the evaluation of risk.24 The Arabic version of PedsQL™ 4.0 created by Arabiat et al.25 reflected adequate psychometric properties. The PedsQL™ 4.0 is suitable for children of all ages. In children older than 4 (5–7, 8–12, and 13–18 years), it includes parallel child self-reports and parent proxy reports and is composed of 23 items. Furthermore, in children between 2 and 4 years, a parent proxy report was used with 21 items. The scale was applied and analyzed according to PedsQL™ guidelines. The selected children were asked to identify problems related to physical, social, and emotional functions and school performance (total 23 items) that had occurred during the study. The items were scored on a 5-point Likert scale, with score 0 indicating no problem, score 1 indicating almost no problem, score 2 indicating occasional problems, score 3 indicating frequent problems, and score 4 indicating almost constant problems, with a final total score value of 100, 75, 50, 25, or 0. A higher score indicates a greater QOL, superior health, or a better function. The PedsQL revealed better reliability and validity for children with acute or chronic wellbeing problems, along with healthy children and teenagers.26
-
4.
Biodex balance system was used to evaluate the postural stability and dynamic balance of children through the tilting of a platform. The system was used to assess all stability indices. All instructions of test performance were explained to the children before applying the test. Children were then asked to stand in the middle of the platform with both legs and to look at a screen for feedback after adjusting the handrails to achieve the optimal safety. Then, children were instructed to stabilize the upright position on the middle of platform, as imitated in the mid screen feedback area, to stabilize the platform and determine foot angles. After introducing the angles to the device, the test starts, and the child is asked to look at the screen and maintain the cursor in the middle while the platform moves. Finally, a report is printed with stability indices.
Sample size
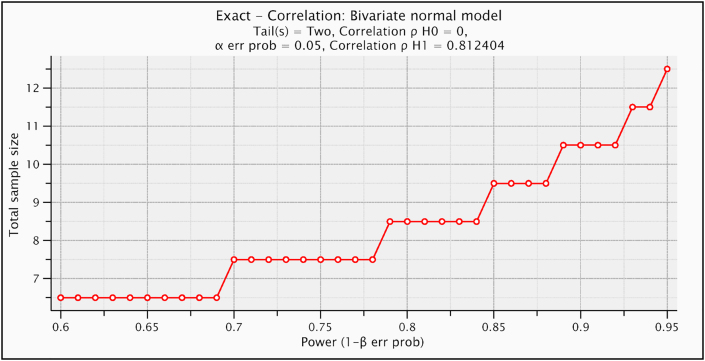
G∗POWER statistical programming was used to test size estimation [Exact- Correlation: Bivariate normal model, α = 0.05, β = 0.20, number of variables = 2, correlation ρH0 = 0, correlation ρH1 = 0.81, and coefficient of determination ρ2 = 0.66 and shown that the suitable sample size of current study was N = 13]. This coefficient of determination ρ2 was calculated from a pilot study of ten participants (between grades of spasticity and gross motor function) (Figure 1).
Figure 1.
Plot of sample size calculation.
Data analysis
Data analysis was conducted using SPSS for windows, version 23 (SPSS, Inc., Chicago, IL). The Spearman product–moment correlation was used to determine the strength and direction of the linear relationship between the ordinal variable (spasticity grades) and continuous variables (pedsQL, GMFM, 3 stability indices). While Pearson product–moment correlation was used to determine the strength and direction of the linear relationship between the continuous variable (Ped QL) and continuous variables (pedsQL, GMFM, 3 stability indices). The alpha level was set at 0.05.
Results
Forty-five participants (22 girls, 23 boys) were included in the current study. Their ages ranged between 4 and 6 years with mean 4.23 ± 0.98. The descriptive statistics of the study are expressed in Table 1. The Spearman's rank-order correlation between spasticity grades and pedsQl revealed a positive strong correlation (p < 0.05). This means that an increase in the spasticity grades is consistent with an increase in PedsQL. Further, there was a positive strong correlation (p < 0.05) between spasticity grades and gross motor function. This means that an increase in spasticity grades was consistent with an increase in GMFM, while there was no correlation (p > 0.05) between spasticity grades and postural stability indices. Thus, changes in the spasticity grades were not consistent with changes in postural stability indices (Tables 2 and 3).
Table 1.
Descriptive Statistics.
| N | Minimum | Maximum | Mean | Std. Deviation | |
|---|---|---|---|---|---|
| PedsQL | 45 | 60 | 85 | 70.6889 | 8.16818 |
| GMFM | 45 | 40.30 | 62.80 | 51.9333 | 6.94845 |
| overall | 45 | 2.50 | 4.80 | 3.4022 | 0.46048 |
| ap | 45 | 2.10 | 4.20 | 2.70202 | 0.40703 |
| ml | 45 | 1.20 | 3.70 | 2.5356 | 0.61132 |
| Valid N (listwise) | 45 |
PedsQL = pediatric quality of life, GMFM = gross motor function measure, ap = anteroposterior, ml = mdiolateral.
Table 2.
Correlations between spasticity grades, pedsQL, GMFM, and stability indices.
| Spasticity grades | PedsQL | GMFM | Overall stability index | Antero-posterior stability index | Medio-lateral stability index |
|---|---|---|---|---|---|
| Correlation Coefficient (Spearman's) (ρ) | 0.84 | 0.816 | −0.092 | 0.177 | −0.083 |
| p-value | 0.0001∗ | 0.0001∗ | 0.549 | 0.246 | 0.589 |
ρ: Spearman's correlation, p-value: probability value, GMFM: Gross Motor Function Measure, ∗significant <0.05.
Table 3.
Correlations between pedsQL and GMFM stability indices.
| PedsQL | GMFM | Overall stability index | Antero-posterior stability index | Medio-lateral stability index |
|---|---|---|---|---|
| Correlation Coefficient (Pearson's) (r) | 0.931 | 0.429 | 0.401 | 0.003 |
| p-value | 0.0001∗ | 0.217 | 0.25 | 0.994 |
r: Pearson's correlation, p-value: probability value, GMFM: Gross Motor Function Measure, ∗significant <0.05.
The Pearson correlation between pedsQL and GMFM revealed a positive strong correlation (p < 0.05). This means that an increase in the Peds QL was consistent with an increase in GMFM, while there was no correlation (p > 0.05) between Peds QL and postural stability indices. This means that changes in the Peds QL were not consistent with changes in postural stability indices (Table 2).
Discussion
The objective of this study was to determine whether there are associations between spasticity, motor function, postural stability, and life quality for children with cerebral palsy. The outcomes indicate a positive strong association between spasticity and health quality, as well as a strong significant association between spasticity and gross motor function, whereas no correlation was detected between spasticity and postural stability index. There was also a positive strong correlation between quality of life and gross motor function, but no association was identified between health quality and postural stability index.
The results of this study are reinforced by those of Gorter,27 who found that there is a strong positive association between spasticity and development of gross motor function in 18-month-olds.27 Muscular weakness, spasticity, selective motor control, and range of motion limitation directly compromise daily activities and gross motor tasks.28, 29, 30
A strong association between gross motor function and health quality percentage has also been identified.31,32 The results of the positive strong correction between gross motor and spasticity in our study are reinforced by previous studies that reported a positive relationship between motor function and spasticity.30,33,34
Gross motor function is considered to be a good index of the physical aspects of health life quality, but a poor index of the psychosocial element of HRQOL in these children.35
The results of the current study are confirmed by those of Gharaborghe et al.,36 who studied the association between gross motor function and health life quality in 60 children (4–12 year) diagnosed with CP who had been selected from different occupational therapy clinics. In this study, QoL was measured using CP-QoL and gross motor functions were tested with GMFM. The results revealed significant differences between gross motor function and QoL.36
In contrast, Dajpratham et al.37 reported that there is no relationship between spasticity and QOL in stroke patients.37 The differences between these findings and current finding could be attributed to culture differences, population type, and different measurement tools. In addition, Akodu et al.38 recognized that movement items and individual care of the HRQOL are strongly affected by spasticity in children with CP.38
Our findings are also aligned with those of other studies that have reported that children with CP that have gross motor function have advanced physical QOL39,40 Furthermore, Vanderslot et al.41 revealed that there is a positive association between gross motor function level and the physical quality aspects of HRQOL.41 By contrast, Dehno et al.42 indicated that motor function level may not modify quality of life.42
Gross motor functions were considered to be good predictors of the physical component of health life quality in children with CP.35 Finally the results of our study contradict those of Puspitasari et al.,43 who indicated that there was no significant relationship between gross motor function and QoL among children with CP after studying the relationship between gross motor function and quality of life among 31 children with CP aged 4–12 years.43
Conclusion
The results of this study indicate that spasticity is the main cause of delayed gross motor function for children with spastic CP that influence life quality of these children with no impact on the postural stability in mild degrees of spasticity so, these results might be a suggestion to determine therapeutic interventions and priorities to plan the physical therapy program according to the main cause of disorder which leading to delay in multi-aspects of daily living activities.
Recommendations
This study determined that spasticity has a positive effect on the motor function and health life quality of children with cerebral palsy; thus, we recommend that physiotherapists address spasticity as a first line of treatment to avoid delays in improving such children's ability to function normally and have a high quality of health.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The author has no conflict of interest to declare
Ethical approval
Approval was obtained from the ethics committee of the Faculty of Physical Therapy, Cairo University, Egypt (NO.P.T.REC|012|003020). Ethical approval date is 25/3/2020.
Acknowledgements
The authors would like to express their appreciation to all of the children and their parents who participated in this study.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Oskoui M., Coutinho F., Dykeman J., Jett_e N., Pringsheim T. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2013;55:509–519. doi: 10.1111/dmcn.12080. [DOI] [PubMed] [Google Scholar]
- 2.Rosenbaum P., Paneth N., Leviton A. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14. [PubMed] [Google Scholar]
- 3.Bobath B., Bobath K. William Heinemann Medical Books; London: 1975. Motor development in different types of cerebral palsy. [Google Scholar]
- 4.Bax M., Goldstein M., Rosenbaum P., Leviton A., Paneth N., Dan B. Proposed definition and classification of cerebral palsy. Dev Med Child Neurol. 2005;47:571–576. doi: 10.1017/s001216220500112x. [DOI] [PubMed] [Google Scholar]
- 5.Macias M.L. Abnormal sitting postures in children with neuromotor disabilities and use of the pelvic corset or molded seat for adaptative sitting. Pediatr Phys Ther. 1998;10:74–77. [Google Scholar]
- 6.Chung J., Evans J., Lee C., Lee J., Rabbani Y., Roxborough L. Effectiveness of adaptive seating on sitting posture and postural control in children with cerebral palsy. Pediatr Phys Ther. 2008;20:303–317. doi: 10.1097/PEP.0b013e31818b7bdd. [DOI] [PubMed] [Google Scholar]
- 7.Shumway-Cook A., Woollacott M.H. Motor control: translating research into clinical practice. 4th ed. Lippincott Williams & Wilkins; Baltimore, MD: 2012. Normal postural control; pp. 161–194. [Google Scholar]
- 8.Massion J. Postural control system. Curr Opin Neurobiol. 1994;4:877–887. doi: 10.1016/0959-4388(94)90137-6. [DOI] [PubMed] [Google Scholar]
- 9.Saether R., Helbostad J.L., Riphagen I.I., Vik T. Clinical tools to assess balance in children and adults with cerebral palsy: a systematic review. Dev Med Child Neurol. 2013;55:988–999. doi: 10.1111/dmcn.12162. [DOI] [PubMed] [Google Scholar]
- 10.Reid D.T. The effects of the saddle seat on seated postural control and upper-extremity movement in children with cerebral palsy. Dev Med Child Neurol. 1996;38:805–815. doi: 10.1111/j.1469-8749.1996.tb15115.x. [DOI] [PubMed] [Google Scholar]
- 11.Reid D., Rigby P., Ryan S. Functional impact of a rigid pelvic stabilizer on children with cerebral palsy who use wheelchairs: users' and caregivers' perceptions. Pediatr Rehabil. 1999;3:101–118. doi: 10.1080/136384999289513. [DOI] [PubMed] [Google Scholar]
- 12.Davis E., Shelly A., Waters E. Quality of life of adolescents with cerebral palsy: perspectives of adolescents and parents. Dev Med Child Neurol. 2009;51:193–199. doi: 10.1111/j.1469-8749.2008.03194.x. [DOI] [PubMed] [Google Scholar]
- 13.Livingston M.H., Rosenbaum P.L., Russell D.J., Palisano R.J. Quality of life among adolescents with cerebral palsy: what does the literature tell us? Dev Med Child Neurol. 2007;49:225–231. doi: 10.1111/j.1469-8749.2007.00225.x. [DOI] [PubMed] [Google Scholar]
- 14.Bjornson K., McLaughlin J. The measurement of health-related quality of life (HRQL) in children with cerebral palsy. Eur J Neurol. 2001;8(s5):183–193. doi: 10.1046/j.1468-1331.2001.00051.x. [DOI] [PubMed] [Google Scholar]
- 15.Schneider J.W., Gurucharri L.M., Gutierrez A.L., Gaebler-Spira D.J. Health-related quality of life and functional outcome measures for children with cerebral palsy. Dev Med Child Neurol. 2001;43(9):601–608. doi: 10.1017/s0012162201001098. [DOI] [PubMed] [Google Scholar]
- 16.Bhimani R., Anderson L. Clinical understanding of spasticity: implications for practice. Rehabil Res Pract. 2014;14(8) doi: 10.1155/2014/279175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lundy C., Lumsden D., Fairhurst C. Treating complex movement disorders in children with cerebral palsy. Ulster Med J. 2009;78:157–163. [PMC free article] [PubMed] [Google Scholar]
- 18.Poeta L.S., Duarte M.F.S., Giuliano I.C.B. Health-related quality of life in obese children. Rev Assoc Med Bras. 2010;56:168–172. doi: 10.1590/s0104-42302010000200014. [DOI] [PubMed] [Google Scholar]
- 19.The national policy on health promotion. Vol. 7. Ministry of Health; Brazil: 2006. pp. 29–33. [Google Scholar]
- 20.Sarathy K., Doshi C., Aroojis A. Clinical examination of children with cerebral palsy. Indian J Orthop. 2019;53:35–44. doi: 10.4103/ortho.IJOrtho_409_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bohannon R.W., Smith M.B. Inter rater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67:206–207. doi: 10.1093/ptj/67.2.206. [DOI] [PubMed] [Google Scholar]
- 22.Russel D., Rosenbaum P., Gowland C., Cadman D., Hardy S., Jarvis S. McMaster University; Hamilton. Canada: 1993. Gross motor function measure manual. [Google Scholar]
- 23.Nordmark E., Hägglund G., Jarnlo G. Reliability of the gross motor function measure in cerebral palsy. Scand J Rehabil Med. 1997;29:25–28. [PubMed] [Google Scholar]
- 24.Varni J.W., Burwinkle T.M., Seid M., Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3:329–341. doi: 10.1367/1539-4409(2003)003<0329:tpaapp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 25.Arabiat D., Elliott B., Draper P., Al Jabery M. Cross-cultural validation of the pediatric quality of life inventory 4.0 (PedsQL) generic core scale into Arabic language. Scand J Caring Sci. 2011;25:828–833. doi: 10.1111/j.1471-6712.2011.00889.x. [DOI] [PubMed] [Google Scholar]
- 26.Ismail A., Campbell M.J., Ibrahim H.M., Jones G.L. Health related quality of life in Malaysian children with thalassaemia. Health Qual Life Outcome. 2006;4:39. doi: 10.1186/1477-7525-4-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gorter w. The relationship between spasticity in young children (18 months of age) with cerebral palsy and their gross motor function development. BMC Muscoskel Disord. 2009;10(1):1–9. doi: 10.1186/1471-2474-10-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ross S.A., Engsberg J.R. Relationships between spasticity, strength, gait, and the GMFM-66 in persons with spastic diplegia cerebral palsy. Arch Phys Med Rehabil. 2007;88(9):1114–1120. doi: 10.1016/j.apmr.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 29.Ohata K., Tsuboyama T., Haruta T., Ichihashi N., Kato T., Nakamura T. Relation between muscle thickness, spasticity, and activity limitations in children and adolescents with cerebral palsy. Dev Med Child Neurol. 2008;50(2):152–156. doi: 10.1111/j.1469-8749.2007.02018.x. [DOI] [PubMed] [Google Scholar]
- 30.Østensjø S., Carlberg E.B., Vøllestad N.K. Motor impairments in young children with cerebral palsy: relationship to gross motor function and everyday activities. Dev Med Child Neurol. 2004;46(9):580–589. doi: 10.1017/s0012162204000994. [DOI] [PubMed] [Google Scholar]
- 31.Majnemer A., Shevell M., Rosenbaum P., Law M., Poulin C. Determinants of life quality in school-age children with cerebral palsy. J Pediatr. 2007;151(5):470–475. doi: 10.1016/j.jpeds.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 32.McCarthy M.L., Silberstein C.E., Atkins E.A., Harryman S.E., Sponseller P.D., Hadley-Miller N.A. Comparing reliability and validity of pediatric instruments for measuring health and well-being of children with spastic cerebral palsy. Dev Med Child Neurol. 2002;44(7):468–476. doi: 10.1017/s0012162201002377. [DOI] [PubMed] [Google Scholar]
- 33.Tuzson A.E., Granata K.P., Abel M.F. Spastic velocity threshold constrains functional performance in cerebral palsy. Arch Phys Med Rehabil. 2003;84(9):1363–1368. doi: 10.1016/s0003-9993(03)00199-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Damiano D.L. Activity, activity, activity: rethinking our physical therapy approach to cerebral palsy. Phys Ther. 2006;86(11):1534–1540. doi: 10.2522/ptj.20050397. [DOI] [PubMed] [Google Scholar]
- 35.Liu W.Y., Hou Y.J., Wong A.M. Relationships between gross motor functions and health-related quality of life of Taiwanese children with cerebral palsy. Am J Phys Med Rehabil. 2009;88(6):473–483. doi: 10.1097/PHM.0b013e3181a0de3a. [DOI] [PubMed] [Google Scholar]
- 36.Nurani S.G., Sarhady M., Mohammad S.S.H., Saeedeh S.M. Relationship between quality of life and gross motor function in children with cerebral palsy (age 4-12) Med J Tabriz Univ Med Sci Health Serv. 2015;37(2):48–53. [Google Scholar]
- 37.Dajpratham P., Kuptniratsaikul V., Kovindha A., Kuptniratsaikul P.S., Dejnuntarat K. Prevalence and management of poststroke spasticity in Thai stroke patients: a multicenter study. J Med Assoc Thai. 2009;92:1354–1360. [PubMed] [Google Scholar]
- 38.Akodu A.K., Oluwale O.A., Adegoke Z.O., Ahmed U.A., Akinola T.O. Relationship between spasticity and health related quality of life in individuals with cerebral palsy. Niger Q J Hosp Med. 2011;22:99–102. [PubMed] [Google Scholar]
- 39.Vargus-Adams J. Health-related quality of life in childhood cerebral palsy. Arch Phys Med Rehabil. 2003;84:E26–E27. doi: 10.1016/j.apmr.2004.10.036. [DOI] [PubMed] [Google Scholar]
- 40.Ko J., Lee B.H., Kim M. Relationship between function and health-related quality of life of school-aged children with cerebral palsy. J Phys Ther Sci. 2011;23:189–195. [Google Scholar]
- 41.Van der Slot W., Nieuwenhuijsen C., van den Berg-Emons R., Wensink-Boonstra A., Stam H., Roebroeck M. Participation and health-related quality of life in adults with spastic bilateral cerebral palsy and the role of self-efficacy. J Rehabil Med. 2010;42:528–535. doi: 10.2340/16501977-0555. [DOI] [PubMed] [Google Scholar]
- 42.Dehno N.S., Dehkordi S.N., Dadgoo M., Salehi M. Association between spasticity and the level of motor function with quality of life in community dwelling Iranian young adults with spastic cerebral palsy. Med J Islam Repub Iran. 2012;26:150. [PMC free article] [PubMed] [Google Scholar]
- 43.Puspitasari M., Rusmil K., Gurnida D. vol. 24. 2013. www.dcidj.org (The relationship between gross motor function and quality of life among children with cerebral palsy). [Google Scholar]