Abstract
Primary hyperparathyroidism caused by an ectopic parathyroid adenoma in the mediastinum is a rare clinical condition. We present a 75-year-old male with primary hyperparathyroidism caused by an ectopic parathyroid adenoma in the mediastinum. This patient was initially referred to the clinic for suspected incidental hypercalcemia. Initial imaging showed two suspicious lesions: one adjacent to the thyroid gland and another in the mediastinum. Further investigations identified a sole mediastinal adenoma. The diagnosis was confirmed by normalization of parathyroid hormone levels after its surgical resection. Thoroughly diagnosing such cases can prove challenging and using a single modality such as ultrasonography, computed tomography, or nuclear imaging alone may not yield conclusive findings or can give false positive results. Our case demonstrates that a combination of several imaging modalities can lead to accurate localization of the cause of primary hyperparathyroidism. This will obviate the performance of unnecessary surgical procedures. In addition, the possibility of missing additional sources of ectopic secretions of the parathyroid hormone will be reduced.
Keywords: Ectopic parathyroid adenoma, Hypercalcemia, Hyperparathyroidism, Mediastinum, Parathyroid adenoma
الملخص
يعتبر فرط نشاط جارة الدرقية الأولي الناجم عن ورم غدد جارات الدرقية خارج مكانها المعتاد في منطقة المنصف اكتشافا نادرا. نقدم هنا حالة من فرط نشاط جارة الدرقية الأولي الناجم عن ورم غدد جارات الدرقية خارج مكانها المعتاد يقع في منطقة المنصف لرجل يبلغ من العمر ٧٥ عاما. بداية تمت إحالة هذا المريض إلى العيادة للتحقيق في ارتفاع نسبة الكالسيوم في الدم الذي تم تشخيصه صدفة. وأظهر تصويره الأولي غدتين مشبوهتين، واحدة مجاورة للغدة الدرقية والأخرى في منطقة المنصف. عند التحقق بدراسات متكررة وإضافية، تم تحديد الغدة المنصفية لوحدها فقط باعتبارها الغدة المشبوهة المحتملة لورم غدة جارة الدرقية وتم التأكيد على ذلك بعد اعتدال مستويات هرمون الغدة جارة الدرقية بعد الاستئصال الجراحي. يمكن أن يكون التشخيص الدقيق لمثل هذه الحالات أمرا صعبا؛ واستخدام دراسة أشعة واحدة مثل التصوير بالموجات فوق الصوتية أو التصوير المقطعي المحوسب أو التصوير النووي وحده قد لا يؤدي إلى نتائج قاطعة أو يمكن أن يعطي نتائج إيجابية خاطئة. توضح حالتنا أن طرق التصوير المتعددة المستخدمة مجتمعة يمكن أن تؤدي إلى تشخيص دقيق لسبب فرط نشاط جارات الدرقية الأولي. وبالتالي يؤدي ذلك إلى تجنيب المرضى إجراءات استئصال جراحية إضافية غير ضرورية أو من ناحية أخرى، تقليل فرص نسيان مصادر أخرى للإفراز خارج مكانها المعتاد.
الكلمات المفتاحية: الورم الحميد الجار درقي خارج الدرقية, الورم الحميد لجارات الدرق, الورم الحميد لجار الدرقية في المنصف الأمامي, فرط نشاط جارات الدرق, ارتفاع نسبة كالسيوم الدم
Introduction
Primary hyperparathyroidism (PHPT) is characterized by excessive production of parathyroid hormone leading to high calcium level and low phosphate and vitamin D levels. The most common causes of PHPT are parathyroid hyperplasia and parathyroid adenomas. Ectopic parathyroid glands are somewhat common with an incidence of up to 25%.1 There is still disagreement on what constitutes the definition of a mediastinal parathyroid gland; therefore, their reported incidence varies between 1% and 2%.2 Ectopic locations of the parathyroid gland are related to the embryologic migratory pathway as it descends to the target location in adulthood.2 Multiple imaging modalities should be used as accurate localization is extremely important to guide surgery and reduce the rate of recurrence.3 In this report, we describe a rare case of mediastinal ectopic parathyroid adenoma that highlighted the importance of using multiple imaging modalities to reach a curative endpoint.
Case report
We present the case of a 75-year-old male diagnosed with diabetes mellitus, hypertension, and dyslipidaemia who presented to the endocrinology clinic after hypercalcemia was noted on routine serological investigations consistently over a period of 4 years. The patient complained of mild intermittent abdominal pain. He was otherwise asymptomatic. Physical examination was unremarkable with normal vital signs. He was on gliclazide, perindopril, amlodipine, and atorvastatin. There was no history of renal calculi.
His laboratory investigations showed a corrected calcium level of 3.0 mmol/L, an elevated parathyroid hormone (PTH) level of 10.9 ng/L, vitamin D level of 24 nmol/L, and a normal thyroid stimulating hormone level. His renal function was within normal limits with a serum creatinine level of 82 μmol/L. We requested a 24-h urine collection, which showed a calcium level of 16.77 mmol/L per 24 h. His complete blood count and liver function tests were also within normal limits (Table 1).
Table 1.
laboratory investigations pre and post operatively.
| Test | Pre-operative | Post-operative | Normal range |
|---|---|---|---|
| 24 h urine volume, ml | 2200 ml | – | 800–2000 |
| Creatinine 24 h (Urine), mmol/24 h | 16.77 | – | 9–21 |
| Calcium 24 h (Urine), mmol/24 h | 10.91 | – | 2.5–7.5 |
| Vitamin D, ng/ml | 24 | 69 | 30–100 |
| Phosphate, mmol/L | 0.8 | 1.0 | 0.81–1.45 |
| Creatinine, μmol/L | 82 | – | 62–106 |
| Calcium, mmol/L | 3.0 | 2.44 | 2.2–2.55 |
| PTH, pmol/L | 10.9 | 6.5 | 1.96–9.33 |
| TSH, mIU/L | 4.09 | 4.10 | 0.25–5.0 |
| Albumin, g/L | 43 | 42 | 35–52 |
| HbA1c, mmol/mol | 39 | – | 20–41 |
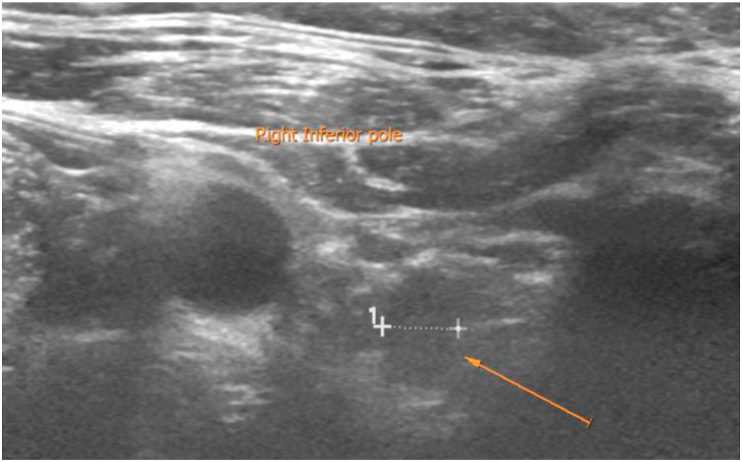
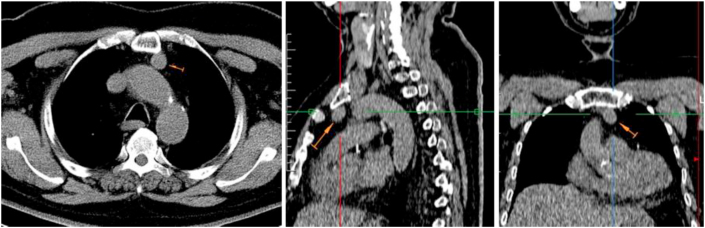
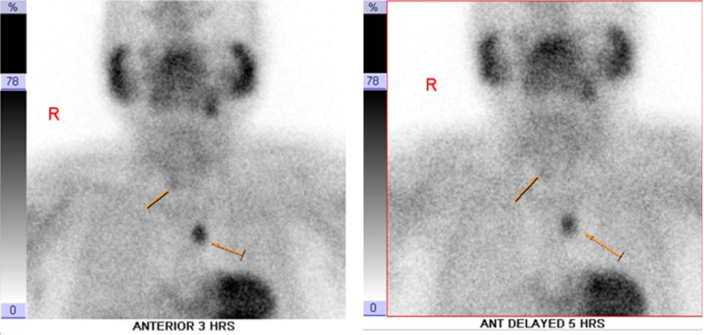
In terms of imaging, he initially underwent an ultrasound of the neck, which showed a small hypoechoic soft tissue nodule adjacent to the inferior pole of the right thyroid (Figure 1). A computed tomography (CT) scan was then performed, revealing a well-defined oval retrosternal soft tissue nodule involving the left side of the mediastinum situated anterior to the aortic arch and posterior to the manubrium, measuring 1.7 × 1.7 × 2.8 cm (Figure 2). The scan also confirmed the nodule adjacent to the right inferior pole of the thyroid. To confirm the diagnosis, a parathyroid sestamibi scan was performed, which showed a distinct MIBI-avid focus at the left side of the anterior mediastinal region, which persisted in the delayed 3- and 5-h phases. This was highly suggestive of an ectopic parathyroid adenoma. Another faint MIBI-avid focus was noted adjacent to the region of the right lower pole of the thyroid gland, which was also shown by 3- and 5-h images (Figure 3). When correlating these findings with the ultrasound images, it was evident that the faint focus most likely corresponded to the small hypoechoic soft tissue nodule originating outside the thyroid gland with a possibility of it being a lymph node or a parathyroid adenoma.
Figure 1.
Ultrasound showing a small hypoechoic soft tissue nodule adjacent to the lower pole of the right thyroid lobe measuring 0.9 × 0.7 × 0.5 cm which is suspicious for an adenoma.
Figure 2.
CT images of different views, axial (left), Sagittal (middle), and coronal (right) showing a well-defined oval retrosternal soft tissue nodule situated anterior to the aortic arch and posterior to the sternal manubrium measuring 1.7 × 1.7 × 2.8 cm.
Figure 3.
A distinct MIBI-avid focus left to the anterior aspect of the mediastinum persisted even at the delayed 3- and 5-h images suggesting an ectopic parathyroid adenoma. In addition to that, a faint MIBI avid focus is noted at the region of the right lower pole of the thyroid gland seen more clearly on the 3 h delayed images.
Subsequently, we requested a whole-body technetium-99m-labelled sestamibi parathyroid scan with additional single photon emission computed tomography (SPECT) at delayed images, which revealed a persistent MIBI-avid nodule at the left para-aortic anterior mediastinum, measuring 1.6 × 1.4 cm, suggestive of an ectopic mediastinal parathyroid adenoma. The scan, however, did not detect any other MIBI-avid lesions in the neck region or the rest of the body.
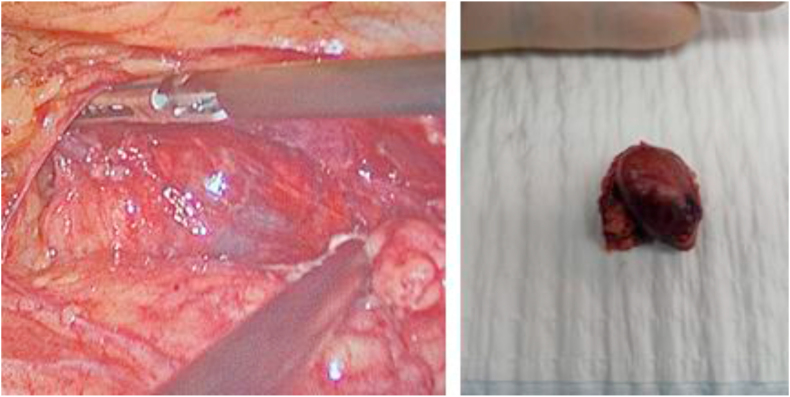
According to Endocrine Society management guidelines, our patient met the requirements for surgical excision as he was hypercalcaemic (3.0 mmol/L) and hypercalciuric (16.77 mmol/L per 24 h).4 After surgical review and approval for fitness, he underwent a left thoracoscopic mediastinal parathyroidectomy under general anaesthesia with no immediate complications.
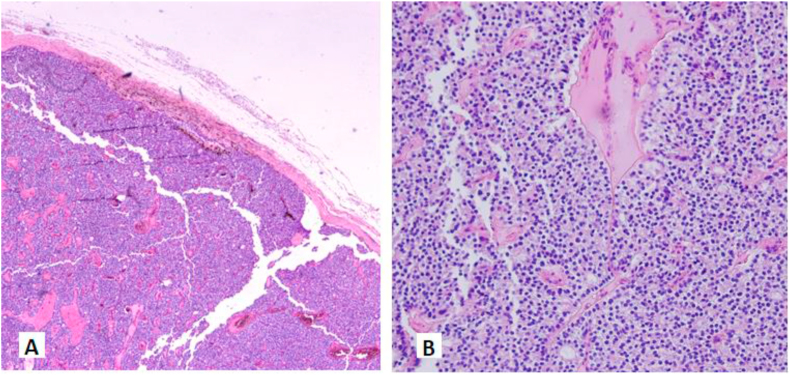
Grossly, the excised specimen consisted of a well-defined soft tissue mass measuring 30 × 25 × 15 mm. The cut-section showed a tan-coloured, well-circumscribed lesion (Figure 4). Microscopically, it showed a capsulated neoplasm composed of sheets of clear cells arranged in an acinar pattern with a capsule of uniform thickness. There was no capsular or vascular invasion and no central scar or necrosis. The periphery showed a thin strip of parathyroid tissue (Figure 5). This was consistent with parathyroid adenoma.
Figure 4.
Encapsulated 3 × 2.5 × 1.5 cm nodule consisting of fibrofatty tissue was excised from the anterior mediastinum. Grossly, the specimen consisted of a well-defined soft tissue tan colored mass with some fatty tissue on the surface.
Figure 5.
H&E stain × 40 magnification showing a parathyroid adenoma with a well-defined capsule (A); And × 200 magnification on intermediate power view showing the parathyroid adenoma composed of predominantly chief cells in acinar pattern (B).
Postoperatively, the PTH level increased gradually from 10.9 to 16.2 pmol/L, calcium level decreased from 3.0 to 2.36 mmol/L, and vitamin D level was at 69 nmol/L. Of note, our patient received one dose of oral vitamin D3 50,000 IU prior to surgery. He was discharged on day 3 of surgery with no complications. The unusual rise in PTH gave the suspicion of a possible missed parathyroid adenoma located elsewhere. Eventually, after 2 weeks, he was seen again, and clinical laboratory tests were performed. His PTH and calcium levels then normalized (6.5 pmol/L and 2.44 mmol/L respectively) (Table 1).
Discussion
PHPT is a cause of hypercalcemia with varying presentations, ranging from asymptomatic patients to those with severe symptoms of hypercalcemia. Symptoms of PHPT include renal calculi symptoms, bone aches, psychiatric symptoms, and abdominal symptoms.5 Many patients are symptomatic in the early stage, and the disease process is detected on routine investigations.6 PHPT can be caused by parathyroid hyperplasia, single or multiple adenomas, carcinoma, or an ectopic parathyroid gland. Some familial causes of PHPT include multiple endocrine neoplasia type 1 or 2A, familial benign hypocalciuric hypercalcemia, and hyperparathyroidism-jaw tumour syndrome.
In up to 90% of the cases, the cause of the PHPT is a single parathyroid adenoma, and the definitive treatment is surgical resection. This leads to curative treatment in as many as 98% of cases.7 If PTH levels remain elevated postoperatively, the search for an additional focus of PHPT is warranted.8 This was encountered in our study in the immediate postoperative phase. However, after a repeat investigation in our clinic, the PTH levels were found to be normalized. This phenomenon of persistently elevated PTH after curative parathyroidectomy is not uncommon and occurs in up to 27% of cases; It is usually transient and most likely related to a secondary response to bone remineralisation.9 The location of the ectopic parathyroid adenoma varies between cases. Most parathyroid adenomas are located within the parathyroid gland; however, in up to 22% of the cases, it is related to an ectopic parathyroid adenoma. These ectopic locations include the thymus (38%), the retro-paraesophageal region (31%), the intrathyroidal region (18%), the mediastinum (6%), undescended along the embryogenic tract (4%), and the carotid sheath (3%).10 Some cases have reported extremely rare and unusual locations, such as the pyriform sinus.11 Our case is rare as it represents a small proportion of all ectopic parathyroid adenomas.
Imaging studies are the main modalities to localize the lesions and allow for a definitive treatment. The imaging tests consist mainly of an initial 99mTc-sestamibi SPECT/CT of the neck region that extends to the whole body for locating the ectopic source. Thoracic CT or magnetic resonance imaging is sometimes additionally required to pinpoint the location and neighbouring structures. The type of surgical intervention is determined based on the location of the source of PTH secretion.12 When different imaging modalities are combined, the diagnostic sensitivity increases. The overall sensitivity and specificity of sestamibi scans are 73% and 80%, respectively.13 When combining sestamibi scans with ultrasound, the sensitivity can reach up to 96% diagnostic sensitivity.14 If additional CT or MRI scans are included, the sensitivity and specificity may even reach close to a 100%.3 When it comes to diagnosing and localizing ectopic parathyroid adenomas, a 99mTc-MIBI scan alone can sometimes be inconclusive; a combination of imaging modalities becomes indicated and has been shown to be cost-effective.15 This is evident by our case where the initial sestamibi scan showed a second faint suspicious focus in the thyroid gland, but a repeat study combining the sestamibi scan with additional SPECT/CT proved it to be insignificant. In addition, when correlated with ultrasonography, it indicated a small hypoechoic soft tissue nodule adjacent to the thyroid, which could indicate a lymph node. The rate of false positives in sestamibi scanning has yet to be described in the literature. However, it is a well-known fact that false positives can occur due to thyroid nodules, lymph nodes, and other thyroid abnormalities.16 Because the repeated imaging did not show an area of uptake in the neck, it was determined by the surgeon to be a false positive result. This was confirmed by the normalization of laboratory tests after surgical excision.
The need for multiple imaging studies to reach an accurate diagnosis in such cases has been described numerous times in the literature. This ensures the discovery of additional ectopic adenomas outside the thyroid and parathyroid glands. Kojidi et al. reported a large ectopic parathyroid adenoma in the mediastinum causing persistent primary hyperparathyroidism in a 70-year-old male. The adenoma weighed 75 g after resection.17 The patient previously had undergone a total parathyroidectomy with thymectomy; However, he remained hypercalcaemic with symptoms. He then underwent a 99m Tc-sestamibi scintigraphy with SPECT, which showed a focal zone of radiotracer accumulation in the midline aspect of the anterior chest wall at the xiphoid level. In another case reported by Gouveia et al., an ectopic parathyroid adenoma was the cause of persistent primary hyperparathyroidism found at the aorto-pulmonary window.12 The patient had presented with the complaint of renal calculi and further investigations confirmed PHPT. The patient then underwent subtotal parathyroidectomy; however, his PHPT persisted and on further investigation by 99mTc-sestamibi SPECT/CT, an ectopic parathyroid adenoma at the aortopulmonary window was discovered. In both cases, it was assumed that the origin of the patient's PHPT was the parathyroid gland only; however, it was then evident that an ectopic lesion was also responsible, stressing the need for multiple imaging modalities to reach an accurate and complete diagnosis.
Parathyroid crisis with a sudden marked increase in PTH and calcium can also be the presentation of parathyroid adenomas as reported by Zhou and Chen. The authors reported a patient presenting with parathyroid crisis that warranted investigation to look for the source. The patient was then diagnosed with a mediastinal ectopic parathyroid adenoma.18 Their patient later developed postoperative hungry bone syndrome in contrast to our patient who did not develop hypocalcaemia.
Conclusion
In PHPT without a definite parathyroid adenoma in the neck as the obvious cause, a combination of imaging modalities should be used to look for the ectopic focus to allow for maximum yield, as opposed to using any of the techniques alone. One of the less common areas of the ectopic parathyroid adenoma is the mediastinal region and should be searched for particularly. Once localized, and certain criteria are fulfilled, surgical resection remains the gold standard treatment for the lesion when aiming for a definitive cure.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
The patient understood that his clinical data would be used for publication purposes and provided his consent.
Consent
Informed consent was obtained from the patient for publication of this case report and any accompanying images.
Authors' contributions
SK and AAS delivered clinical care to the patient and acquired clinical information. AAS and SMG drafted the manuscript. MAS revised the manuscript critically and drew the final draft. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Navarro A., Vassallo J., Galea J. Excision of an Elusive Tiny Ectopic Parathyroid Adenoma. Case Rep Oncol. 2017 Dec 11;10(3):1105–1111. doi: 10.1159/000485075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Di Cosimo C., Metere A., Chiesa C., Di Rocco G., Trulli F., Paciaroni A. Mediastinal parathyroid adenoma: a case report. Eur Rev Med Pharmacol Sci. 2012;16(6):845–847. [PubMed] [Google Scholar]
- 3.Zerizer I., Parsaï A., Win Z., Al-Nahhas A. Anatomical and functional localization of ectopic parathyroid adenomas: 6-year institutional experience. Nucl Med Commun. 2011 Jun;32(6):496–502. doi: 10.1097/MNM.0b013e32834557a3. [DOI] [PubMed] [Google Scholar]
- 4.Bilezikian J.P., Brandi M.L., Eastell R., Silverberg S.J., Udelsman R., Marcocci C. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J Clin Endocrinol Metab. 2014 Oct;99(10):3561–3569. doi: 10.1210/jc.2014-1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Madkhali T., Alhefdhi A., Chen H., Elfenbein D. Primary hyperparathyroidism. Ulus Cerrahi Derg. 2016;32(1):58–66. doi: 10.5152/UCD.2015.3032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vilallonga R., Zafon C., Migone R., Baena J.A. Giant intrathyroidal parathyroid adenoma. J Emerg Trauma Shock. 2012;5(2):196–198. doi: 10.4103/0974-2700.96497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eslamy H.K., Ziessman H.A. Parathyroid scintigraphy in patients with primary hyperparathyroidism: 99mTc sestamibi SPECT and SPECT/CT. Radiographics. 2008 Sep-Oct;28(5):1461–1476. doi: 10.1148/rg.285075055. [DOI] [PubMed] [Google Scholar]
- 8.Howe J., editor. Endocrine and Neuroendocrine Surgery. 1st ed. Springer; 2017. [Google Scholar]
- 9.Mittendorf E.A., McHenry C.R. Persistent Parathyroid Hormone Elevation Following Curative Parathyroidectomy for Primary Hyperparathyroidism. Arch Otolaryngol Head Neck Surg. 2002;128(3):275–279. doi: 10.1001/archotol.128.3.275. [DOI] [PubMed] [Google Scholar]
- 10.Roy M., Mazeh H., Chen H., Sippel R. Incidence and Localization of Ectopic Parathyroid Adenomas in Previously Unexplored Patients. World Journal of Surgery. 2013;37:102. doi: 10.1007/s00268-012-1773-z. [DOI] [PubMed] [Google Scholar]
- 11.Mallon S., Patel S., Wright J., Griffith B. Ectopic Parathyroid Adenoma in the Pyriform Sinus: Case Report. Appl Radiol. 2020;49(3) 48J-48L. [Google Scholar]
- 12.GouveiaI S., RodriguesI D., BarrosI L., RibeiroI C., AlbuquerqueII A., CostaII G. Persistent primary hyperparathyroidism: An uncommon location for an ectopic gland - Case report and review. Arq Bras Endocrinol Metab. 2012;56(6):393–403. doi: 10.1590/s0004-27302012000600009. [DOI] [PubMed] [Google Scholar]
- 13.Allendorf J., Kim L., Chabot J., DiGiorgi M., Spanknebel K., LoGerfo P. The impact of sestamibi scanning on the outcome of parathyroid surgery. J Clin Endocrinol Metab. 2003 Jul;88(7):3015–3018. doi: 10.1210/jc.2002-021095. [DOI] [PubMed] [Google Scholar]
- 14.McHenry C.R. What's new in general surgery: endocrine surgery. J Am Coll Surg. 2002 Sep;195(3):364–371. doi: 10.1016/s1072-7515(02)01307-8. [DOI] [PubMed] [Google Scholar]
- 15.Elaraj D.M., Sippel R.S., Lindsay S., Sansano I., Duh Q.Y., Clark O.H. Are additional localization studies and referral indicated for patients with primary hyperparathyroidism who have negative sestamibi scan results? Arch Surg. 2010 Jun;145(6):578–581. doi: 10.1001/archsurg.2010.108. [DOI] [PubMed] [Google Scholar]
- 16.Alenezi S., Asa'ad S., Elgazzar A. Scintigraphic parathyroid imaging: concepts and new developments. Res Rep Nucl Med. 2015:5 9–18. [Google Scholar]
- 17.Taghavi Kojidi H, Vagharimehr N, Mohseni S, Pajouhi M, Mohajeri-Tehrani MR. Unusual Ectopic Parathyroid Adenoma: A Case Report. Acta Med Iran. 54(8):547-550. [PubMed]
- 18.Zhou W., Chen M. A case report of mediastinal ectopic parathyroid adenoma presented as parathyroid crisis localized by SPECT/CT. Medicine (Baltimore) 2016 Oct;95(41):e5157. doi: 10.1097/MD.0000000000005157. [DOI] [PMC free article] [PubMed] [Google Scholar]