Abstract
Purpose
The latest version of the Gamma Knife, the Icon, allows for immobilization with a mask in lieu of the traditional frame during stereotactic radiosurgery. There have been some concerns regarding extent of immobilization during single fraction frameless treatment and potential effect on outcomes. As such, we reviewed outcomes in patients with brain metastases treated in a single fraction using either a frame or mask on the Gamma Knife Icon at our institution.
Methods and Materials
We reviewed the records of 95 patients with a total of 374 metastases treated between May 2019 and January 2021. Thirty-nine patients (41%) were treated using the Leksell frame with the remainder being immobilized with a mask. The median number of metastatic lesions was 2 (1–20). The median prescription dose was 20 Gy (11.5–24 Gy). Odds ratios were generated to identify predictors of mask use. Kaplan-Meier analysis was used to calculate survival, local failure, and distant failure rates. Cox regression was used to identify predictors of survival. Propensity matching was used to account for indication bias.
Results
Of the 95 patients treated, 88 (93%) had follow-up with a median duration of 5 months (1–18). Frame utilization was more likely with 6 to 10 brain metastases. Median overall survival was not reached and was 70% and 60% at 6 and 12 months for the entire cohort, respectively. There was no significant difference in survival by immobilization method (P = .12). Six patients had local failure in 10 total lesions (3 patients in each group). After propensity matching the 12 month tumor local control was 96% and 85% for framed and frameless cases, respectively (P = .07).
Conclusions
Frameless mask-based stereotactic radiosurgery using the Gamma Knife Icon is feasible and maintains the excellent local control seen with the use of the headframe.
Introduction
The use of radiation in the treatment of brain metastases has evolved over time, from the use of whole brain radiation (WBRT) alone, to combined WBRT and stereotactic radiosurgery (SRS), to SRS alone for appropriately selected patients.1, 2, 3 The Gamma Knife (GK; Elekta, Stockholm, Sweden), developed by Lars Leksell, was one of the first machines with the specific purpose of performing SRS for a variety of conditions.4 The original form of immobilization on the GK, which still exists today, was a frame which was placed under local anesthesia, remaining in place during planning and treatment.5 Rigid immobilization is critical in the realm of radiosurgery given the high doses, surrounding structures, and narrow (if any) margins. Multiple studies have shown that even movement in the range of 2 to 3 mm can result in underdosing of targets or overdosing normal tissue.6,7 The latest version of the GK, the Icon, now allows the use of a lightweight plastic mask for immobilization, similar to the type of immobilization used in radiation therapy for many years.8,9 The introduction of the mask to the GK opened the door for hypofractionation and perhaps even an increase in patient comfort.10,11 There have been some concerns over single fraction use with the mask on the GK due to less rigidity in comparison to the frame.12,13 As such, we sought to review outcomes in brain metastases patients treated on the Gamma Knife Icon in a single fraction using either the frame or mask for immobilization.
Methods and Materials
Patient selection
We reviewed the records of 95 patients with brain metastases treated in a single fraction on the GK Icon at our institution between May 2019 and January 2021. This study was reviewed and approved by our institutional review board. Patients were included if they had a diagnosis of brain metastases treated on the GK Icon in a single fraction during the course of the study period. Baseline characteristics of the cohort were tabulated including age, sex, primary malignancy, performance status, immobilization technique, and number of brain metastases. The process for treatment planning and delivery are outlined below.
Treatment planning
All patients were treated using the GK Icon with planning completed on the Leksell Gammaplan treatment planning software (version 11.1.1). For planning purposes, all patients had a 1 mm slice thickness contrast enhanced magnetic resonance imaging (MRI) scan obtained the day of frame placement or within 1 week of frameless treatment to allow for target delineation. The sequences used were a T1 with contrast and T2 without contrast.
The process for mask fabrication has been described before, but briefly, is as follows.9 A custom headrest is created on the GK unit at the time of mask immobilization. The mask is formed to the patient's face, with careful attention to apply the most pressure over the chin and forehead. The patient's nose extends from the mask, upon which a reflective marker is placed to aid with motion management (described below). The mask hardens as it cools over about 15 minutes. At that time, a cone beam CT (CBCT) is captured using a CT dose index of 6.3 mGy. This set of images becomes the reference for patient localization before treatment is started. The images are coregistered/fused with the planning MRI scan. For patients treated with the frame, the Leksell G frame was placed under local anesthesia with versed and fentanyl to aid with patient comfort. After frame placement, patients were transported to the MRI suite where the previously described sequences were obtained.
In terms of targeting, for those patients with intact tumors, the gross tumor volume was defined as the contrast enhancing lesion(s) seen on T1 MRI scan. The planning target volume (PTV) was equivalent to gross tumor volume in those patients, with no margin used. For patients being treated to a postoperative cavity, the clinical target volume encompassing possible microscopic disease was the resection cavity, surgical tract, and nearby meningeal surfaces as suggested by guidelines.14 A 0.1 cm margin was then applied to create a PTV. All doses were prescribed to the isodose line best covering the PTV. A modified dosing scheme based on the classic RTOG 9005 was used to determine prescription dose, mainly based on target volume, primary malignancy, number of lesions, and history of past radiation.15,16 Targeting and planning were carried out by a radiation oncologist, neurosurgeon, and medical physicist. Planning was typically a combined approach using both inverse and forward planning techniques. A plan was deemed appropriate and acceptable if coverage to the PTV was in the 99% to 100% range with a volume of normal brain receiving 12 Gy to <10 mL and no excessive dose to brain stem or optic structures.
Treatment delivery and motion management
Patients treated with the mask were set up the day of treatment within the mask with reflective marker placed upon the nose. A 2.5 mGy CBCT was obtained with the patient in the mask to check for any shifts or dramatic changes in dose distribution or target coverage. Ideally, target coverage was maintained in the 99% to 100% range. Once coverage was confirmed and verified treatment was started. High definition motion management was used during treatment with a motion tolerance of 1.0 mm based on physicist recommendations and institutional preference. If a patient exceeded tolerance for more than 30 seconds, the treatment was interrupted and the patient was given a break before resuming the workflow and treatment. For patients treated using the Leksell G frame, a CBCT was still acquired before treatment to verify frame position was stable and also to recheck and verify dose and target distribution/coverage. If target coverage was maintained and the frame had not moved, treatment was administered.
Statistics
Baseline characteristics of the patient cohort were tabulated, and odds ratios were generated to predict likelihood of frameless treatment compared with frame based treatment. Treatment plan characteristics such as prescription dose, target volume, and treatment time were also recorded. An independent samples t test was used to compare baseline characteristics. Univariate and multivariate Cox regression were used to identify predictors of survival.17 Kaplan-Meier curves were generated to calculate local control, distant brain control, and overall survival.18 Sample size calculation with an outcome of local control at 1 year determined that 300 lesions total would be required to show a 12% difference in outcome using a power of 80% and alpha of 0.05. A sample size of 210 would be required to show a difference of 15%.
Follow-up MRIs were typically acquired at 3 month intervals after SRS. Local failure was defined as per RANO criteria.19 If there was ever a question of local recurrence versus radionecrosis or reaction the case was reviewed in our multidisciplinary neurooncology conference to confirm outcome. Distant brain failure was defined as any number of new brain metastases seen on follow-up imaging outside of the treated areas. Survival was defined from time of SRS to death or last follow-up. Clinical follow-up was defined as time from SRS to last physician visit. Imaging follow-up was defined as time from SRS to most recent brain scan. A logistic regression analysis was used to generate a propensity score indicating the likelihood of frameless treatment. A case-control series was then generated based on a propensity score match within 0.10, resulting in 80 matched individual tumor pairs. Kaplan-Meier curve analysis was done on that matched set of pairs to compare local control. An independent samples t test was also conducted on those pairs to verify balance.
Results
As noted, 95 patients were included in this study with 374 metastatic lesions. Fifty-six patients (59%) were treated using the mask for immobilization. The majority of patients were female (57%) and the median age was 61 years (29-91). A variety of primary malignancies were represented, with lung and breast accounting for >80%. Two-thirds of patients had extracranial disease at the time of SRS and only 21% had prior WBRT (10 patients in each arm). A small portion of patients (<10%; 4 patients in each arm) had prior surgical resection followed by SRS within 3 to 4 weeks. The median number of tumors was 2 (1-20). Table 1 contains a comprehensive list of baseline characteristics. Using an independent samples t test, the only unbalanced characteristic was patients treated with the frame having a larger number of lesions. In addition, odds ratios revealed that patients treated earlier in the study period, with 6 to 10 brain metastases, and total target volume >1.65 cm3 were more likely to be treated using the frame. Table 1 contains a full list of odds ratios.
Table 1.
Baseline characteristics and odds ratios for likelihood of frameless SRS
| Characteristic | All patients (%) (n = 95) |
Framed cases (%) (n = 39) |
Frameless cases (%) (n = 56) |
Odds ratio (95% CI) |
P value |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 41 (43) | 19 (49) | 22 (39) | 1 | |
| Female | 54 (57) | 20 (51) | 34 (61) | 1.47 (0.64-3.35) | .36 |
| Age, y | |||||
| ≤61 | 48 (51) | 8 (21) | 40 (71) | 1 | |
| >61 | 47 (50) | 31 (79) | 16 (29) | 1.78 (0.78-4.08) | .17 |
| Primary malignancy | |||||
| Lung (NSCLC/SCLC/LCNEC) | 50 (53) | 18 (46) | 32 (57) | 1 | |
| Breast | 21 (22) | 9 (23) | 12 (21) | 0.75 (0.27-2.12) | .59 |
| Melanoma | 14 (15) | 7 (18) | 7 (13) | 0.56 (0.17-1.86) | .35 |
| GI (anal/colon/rectal) | 4 (4) | 1 (1) | 3 (5) | 1.69 (0.16-17.44) | .66 |
| Other* | 6 (6) | 4 (12) | 2 (4) | 0.28 (0.05-1.69) | .17 |
| KPS | |||||
| 50 | 2 (2) | 2 (5) | 0 (0) | 1 | |
| 60 | 3 (3) | 1 (3) | 2 (4) | 8.33 (0.22-320.40) | .25 |
| 70 | 8 (8) | 2 (5) | 6 (11) | 13.00 (0.45-377.49) | .14 |
| 80 | 48 (51) | 17 (44) | 31 (55) | 9.00 (0.41-198.22) | .16 |
| 90 | 31 (33) | 15 (38) | 16 (29) | 5.32 (0.24-119.88) | .29 |
| 100 | 3 (3) | 2 (5) | 1 (1) | 3.00 (0.08-115.35) | .56 |
| GPA score | |||||
| 0-1.0 | 34 (36) | 14 (36) | 23 (41) | 1 | |
| 1.5-2.5 | 49 (52) | 19 (49) | 29 (52) | 1.02 (0.42-2.47) | .97 |
| 3.0 | 5 (5) | 3 (8) | 2 (4) | 0.47 (0.07-3.17) | .44 |
| 3.5-4.0 | 7 (7) | 2 (7) | 5 (3) | 1.75 (0.30-10.34) | .54 |
| Extracranial disease | |||||
| No | 32 (34) | 16 (41) | 16 (29) | 1 | |
| Yes | 63 (66) | 23 (59) | 40 (71) | 1.74 (0.73-4.12) | .21 |
| Past WBRT | |||||
| No | 75 (79) | 29 (74) | 46 (82) | 1 | |
| Yes | 20 (21) | 10 (26) | 10 (18) | 0.63 (0.23-1.70) | .36 |
| Surgery to metastasis | |||||
| No | 87 (92) | 35 (90) | 52 (93) | 1 | |
| Yes | 8 (8) | 4 (10) | 4 (7) | 0.67 (0.16-2.87) | .59 |
| Total no. of metastases | |||||
| 1-5 | 74 (77) | 24 (62) | 50 (89) | 1 | |
| 6-10 | 12 (13) | 8 (21) | 4 (7) | 0.24 (0.07-0.88) | .03 |
| 11-15 | 5 (5) | 4 (12) | 1 (2) | 0.12 (0.01-1.13) | .06 |
| 16-20 | 4 (5) | 3 (5) | 1 (2) | 0.16 (0.02-1.62) | .12 |
| Total treatment volume (mL) | |||||
| 0.0048-0.17 | 24 (25) | 6 (15) | 18 (32) | 1 | |
| 0.17-0.68 | 24 (25) | 9 (23) | 15 (27) | 0.63 (0.18-2.16) | .46 |
| 0.69-1.65 | 23 (25) | 9 (23) | 14 (25) | 0.55 (0.16-1.92) | .35 |
| >1.65 | 24 (25) | 15 (38) | 9 (16) | 0.21 (0.06-0.74) | .01 |
| Date of treatment | |||||
| May 2019-Dececember 2019 | 32 (34) | 30 (77) | 2 (3) | 1 | |
| January 2020-June 2020 | 27 (28) | 6 (15) | 21 (38) | 52.50 (9.64-285.87) | <.0001 |
| July 2020-Jan 2021 | 36 (38) | 3 (7) | 33 (59) | 165.00 (25.78-1055.99) | <.0001 |
Abbreviations: CI = confidence interval; GI = gastrointestinal; GPA = Graded Prognostic Assessment; KPS = Karnofsky Performance Status; LCNEC = large cell neuroendocrine carcinoma; NSCLC = non small cell lung cancer; SCLC = small cell lung cancer; SRS = stereotactic radiosurgery; WBRT = whole brain radiation.
The median prescription dose delivered was 20 Gy (11.5–24 Gy) to a median isodose line of 57% (48%–94%). The median individual and total target volumes were 0.055 cm3 (0.002–8.61 cm3) and 0.68 cm3 (0.0048–33.507 cm3), respectively. The dose, isodose line, and volume per lesions were reasonably balanced between the 2 groups based on an independent samples t test. The treatment time was significantly longer in the frame based treatments. The median treatment times were 69 minutes (10–240) and 40 minutes (5–119) for the frame and mask, respectively. The median increase in treatment time on day of delivery versus plan was 1 minute (0–43 minutes) due to treatment break requiring image reacquisition. For patients who required a break, median increase in treatment time was 11 minutes (3–43 minutes). Median target coverage was 100% (95%–100%). Table 2 contains all treatment details.
Table 2.
Treatment characteristics for individual target lesions
| Characteristic median (range) | All targets (n = 374) | Framed cases (n = 220) | Frameless cases (n = 154) |
|---|---|---|---|
| Prescription dose | 20 Gy (11.5-24) | 23 Gy (11.5-24) | 20 Gy (15-24) |
| Isodose line | 57% (48-86) | 50% (48-86) | 50% (50-80) |
| Target volume | 0.055 mL (0.002-8.61) | 0.057 mL (0.002-8.61) | 0.049 mL (0.003-6.65) |
| Treatment Time | 39 mins (5-240) | 69 mins (10-240) | 31.5 mins (5-119) |
| Target coverage | 100% (99-100) | 100% (99-100) | 100% (99-100) |
| Interruptions | 0 (0-4) | 0 (0-3) | 0 (0-4) |
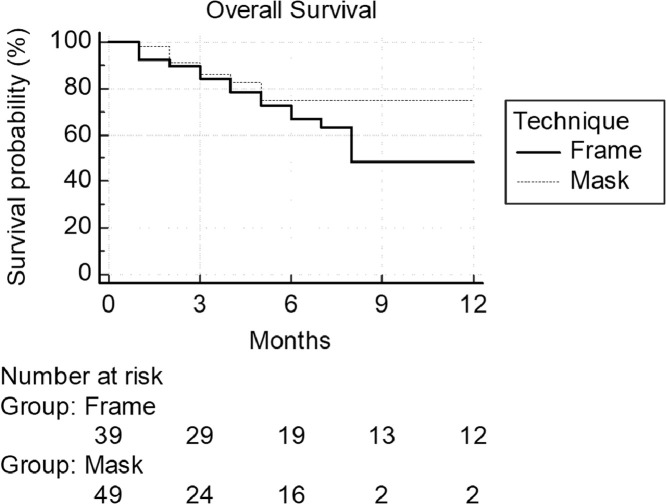
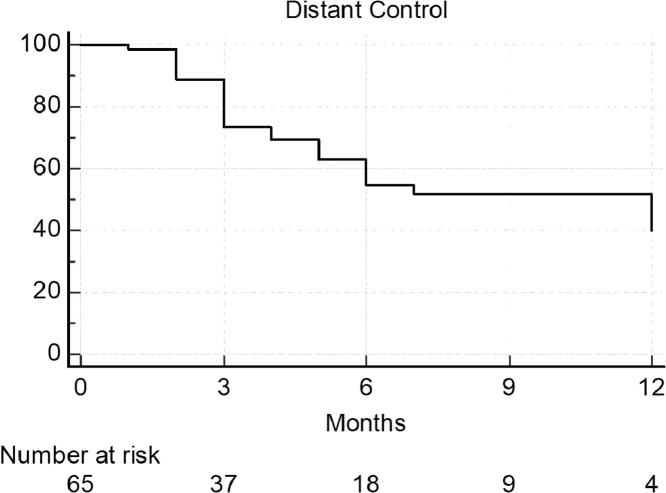
The median clinical follow-up was 5 months (1–19 months). Eighty-eight of 95 patients (93%) had imaging follow-up available for review with a median number of follow-up MRIs of 2 (1–19). Only patients with imaging follow-up were included in calculations for local control and distant failure. The median imaging follow-up was 6 months (1–18). The median survival was not reached in the mask group and was 8 months in the frame group with 1 year survivals of 75% and 48% for the mask and frame, respectively (P = .12; Fig. 1). The 1-year survival for all patients was 60%. The only predictor of survival on multivariate analysis was increasing number of brain metastases. The median time to development of new distant intracranial progression was 12 months across all patients (Fig. 2).
Fig. 1.
Median overall survival was not reached and was 70% and 60% at 6 and 12 months for the entire cohort, respectively. There was no significant difference in survival by immobilization method (P = .12). One year survival was 48% and 75% for framed and frameless cases, respectively.
Fig. 2.
The rate of distant intracranial control was 55% at 6 months and 40% at 1 year across the 65 patients with follow-up imaging.
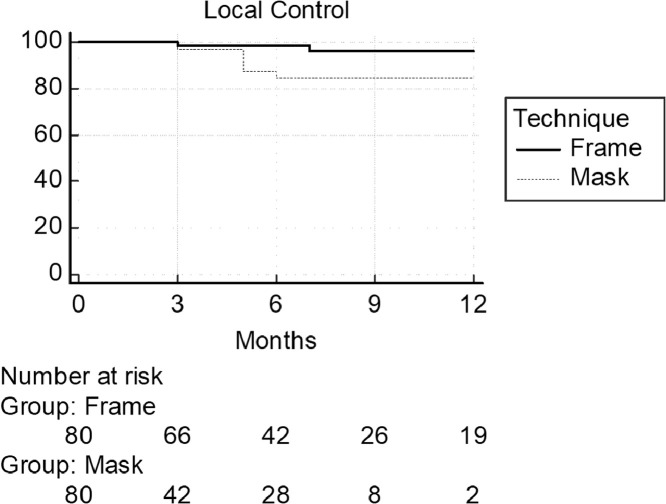
In terms of individual target lesions, 251 (67%) had follow-up imaging available (86 lesions in the mask group and 165 in the frame group) and were used in local control calculations. To account for lack of randomization a logistic regression analysis was used to generate a propensity score indicating likelihood of being treated using mask immobilization. Characteristics included in this analysis included age, sex, primary malignancy, dose, isodose line, and target volume. Lesions from each cohort (mask or frame) were then matched based on the propensity score allowing for a difference up to 0.10. This match resulted in 80 pairs of matched target lesions. Balance of the groups was verified by stratifying the groups into propensity-score based quintiles, confirming that a standardized difference between the treatment groups was less than 0.10. Characteristics of the 2 matched groups are displayed in Table 3. In total, 6 patients experienced a local failure (3 in each group). In total there was a local failure in 10 lesions (7 in the mask group and 3 in the frame group). Propensity-matched Kaplan-Meier analysis revealed 1 year local control of 96% and 85% for the frame and mask, respectively (P = .07; Fig. 3). Additional analysis looking at dose per lesion or volume of lesion did not predict for failure within these cohorts. On multivariable regression the only predictor of local failure was melanoma primary (odds ratio: 24.02; 95% confidence interval, 1.65%-348.61%; P = .02). Four patients developed acute treatment related toxicity (within 90 days of SRS), 2 patients in each group. All toxicity was grade 1 to 2 headaches or swelling which responded to steroid therapy.
Table 3.
Characteristics of propensity-matched target lesions
| Characteristic | All targets (n = 160) | Framed cases (n = 80) | Frameless cases (n = 80) |
|---|---|---|---|
| Prescription dose | 21 Gy (14-24) | 20.5 Gy (14-24) | 21 Gy (18-24) |
| Isodose line | 53% (50-94) | 54% (50-94) | 50% (50-90) |
| Target volume | 0.077 mL (0.002-6.15) | 0.089 mL (0.002-6.15) | 0.069 mL (0.003-4.39) |
| Age | 58 (30-91) | 58 (30-84) | 60 (44-91) |
| Sex | |||
| Male | 56 (35%) | 30 (38%) | 26 (33%) |
| Female | 104 (65%) | 50 (62%) | 54 (67%) |
| Primary | |||
| Lung | 76 (48%) | 36 (45%) | 40 (50%) |
| Breast | 61 (38%) | 33 (41%) | 28 (35%) |
| Melanoma | 17 (10%) | 8 (10%) | 9 (11%) |
| GI | 3 (2%) | 1 (2%) | 2 (2%) |
| Other* | 3 (2%) | 2 (2%) | 1 (2%) |
Renal cell carcinoma, urothelial carcinoma, and thyroid cancer.
Abbreviation: GI = gastrointestinal.
Fig. 3.
Propensity matched cuve showing 12 month local control was 96% and 85% for framed and frameless cases, respectively (P = .07).
Discussion
The results here are largest and most direct comparison of frame-based versus mask-based GK SRS delivered in a single fraction. The outcomes presented appear to show that regardless of immobilization choice, both offer similar excellent rates of local control in the 80% to 90% range. There has been some hesitation to offer a frameless technique with a single fraction given increased possibility of motion, especially with longer treatment times.9,12,20,21 With that thought in mind, we still use the frame for single fraction cases in which time will be prolonged (generally >60 minutes) to help avoid interruptions or the possibility of excessive motion which could affect outcome. With the global Coronavirus 2019 pandemic our program shifted to more single fraction frameless cases in the second quarter of 2020 to reduce possible exposure and staff involvement with placement of the frame.22 To help limit the possibility of excessive motion we used a tighter 1 mm motion with the high definition motion management system for all single fraction frameless cases, compared with the more traditional 1.5 mm used with fractionated GK cases. With the early follow up in this series we did not see any significant increase in local failures (3 patients in each group) with the use of the mask. Given small number of events we also looked at “per lesion” local control and performed a propensity match due to lack of randomization, showing a potential trend toward improved local control with the frame (P = .07). Those results must be interpreted with caution due to small number of events, short follow-up (6 months), lack of randomization, and likely lead time bias in the frame group which has longer follow-up.
A similar study has been presented in abstract form by the group at Columbia.23 In that study 41 patients with 95 brain metastases were treated with single-fraction frameless GK SRS and compared with 33 patients with 104 brain metastases treated using the frame. The median follow-up was 11 months and baseline characteristics were well balanced. Patients treated using the mask, however, had a larger, but not significantly so, tumor volume compared with the frame-based treatment group. At 1 year, local control was not significantly different at 92% and 86% for frameless and framed SRS, respectively (P = .62). Another similar study from the University of Maryland compared frame based single fraction SRS to single fraction LINAC-based SRS in 172 target lesions.24 The authors showed a similar rate of local control, 95% and 82% for frame-based and LINAC-based (frameless) treatments (P = .07); although mind these were not randomized or propensity matched series. There was in increase in the rate of symptomatic radionecrosis with the use of LINAC-based SRS in the study from the University of Maryland (1.4% vs 9.9%, P = .03). This study is currently only available in abstract form so the planning and dosing details are not known, as that may have contributed to that difference. In our series, with a short median follow-up, we did not observe differences in acute toxicity.
There is one prospective, nonrandomized study on this topic, from Germany.25 That group examined outcomes in 76 patients treated on the GK Icon, using either a frame or mask on a case-by-case basis. The vast majority were single fraction treatments (95%), and the median dose was 22 Gy in each group. There was actually a higher rate of local failure with frame use (hazard ratio: 3.69; 95% confidence interval, 1.13%-12.0%; P = .03), and no failures in the mask group. Of note and interest, with mask use the authors of that study did use a minimal margin (compared with traditional no margin for GK treatments). There was no significant difference in survival or toxicity within that study.
Of course, if there is no perceived or actual difference in clinical outcomes, the question becomes whether choice of immobilization matters. A recent publication thus looked at the patient experience to see if patients themselves had a preference in terms of immobilization.11 That study looked at 117 patients treated over 1 year on the GK Icon using either the frame or the mask for various conditions (nonmalignant and benign). An 8 question survey was administered to the patients to assess pain and comfort associated with the frame or the mask. Results showed pain was higher for the frame based group, and comfort was higher for the mask based group. These results certainly help support the notion that even for single fraction treatments mask-based immobilization may be optimal.
The present study is not without limitations. It is retrospective and nonrandomized in nature resulting in likely selection bias, as well as lead time bias because frame-based treatments were administered earlier within the timeframe. In addition, the follow-up is relatively short, and longer follow-up will be needed to verify local control rates, rates of radionecrosis, and other toxicity rates. Also, there is almost certainly some experience bias present, as our institution transitioned from a frameless LINAC-based SRS program to the GK Icon in 2019, and we were thus already quite comfortable with a frameless SRS approach. It should also be mentioned that in this series frame based treatments were longer, and the frame may be preferable in those situations to avoid interruptions and continued prolongation of treatment.9 To that end, the patient experience, also plays a large role in immobilization choice. We were unable to assess that outcome within this study, and additional studies will be necessary to help further validate outcomes and any differences between the 2 techniques.
Conclusions
With our short follow-up, frameless GK SRS appears to be a viable treatment option for patients eligible for single fraction treatment, with no acute discernable differences compared with frame based GK SRS. Longer follow-up and larger comparisons will be necessary to validate these results.
Footnotes
Sources of support: This work had no specific funding.
Disclosures: None.
It is our institution's policy to not share data without institutional review board approval or a data use agreement.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.adro.2021.100736.
Appendix. Supplementary materials
References
- 1.Brown PD, Jaeckle K, Ballman KV. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: A randomized clinical trial. JAMA. 2016;316:401–409. doi: 10.1001/jama.2016.9839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang EL, Wefel JS, Hess KR. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: A randomised controlled trial. Lancet Oncol. 2009;10:1037–1044. doi: 10.1016/S1470-2045(09)70263-3. [DOI] [PubMed] [Google Scholar]
- 3.Aoyama H, Shirato H, Tago M. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: A randomized controlled trial. JAMA. 2006;295:2483–2491. doi: 10.1001/jama.295.21.2483. [DOI] [PubMed] [Google Scholar]
- 4.Leksell L. The stereotaxic method and radiosurgery of the brain. Acta Chir Scand. 1951;102:316–319. [PubMed] [Google Scholar]
- 5.Seneviratne DS, Vallow LA, Hadley A. Intracranial motion during frameless Gamma-Knife stereotactic radiosurgery. J Radiosurg SBRT. 2020;6:277–285. [PMC free article] [PubMed] [Google Scholar]
- 6.Beltran C, Trussell J, Merchant TE. Dosimetric impact of intrafractional patient motion in pediatric brain tumor patients. Med Dosim. 2010;35:43–48. doi: 10.1016/j.meddos.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fu W, Yang Y, Yue NJ, Heron DE, Saiful Huq M. Dosimetric influences of rotational setup errors on head and neck carcinoma intensity-modulated radiation therapy treatments. Med Dosim. 2013;38:125–132. doi: 10.1016/j.meddos.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Vulpe H, Save AV, Xu Y. Frameless stereotactic radiosurgery on the gamma knife icon: early experience from 100 patients. Neurosurgery. 2020;86:509–516. doi: 10.1093/neuros/nyz227. [DOI] [PubMed] [Google Scholar]
- 9.Wegner RE, Xu L, Horne Z. Predictors of treatment interruption during frameless gamma knife icon stereotactic radiosurgery. Adv Radiat Oncol. 2020;5:1152–1157. doi: 10.1016/j.adro.2020.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Samanci Y, Sisman U, Altintas A. Hypofractionated frameless gamma knife radiosurgery for large metastatic brain tumors. Clin Exp Metastasis. 2021;38:31–46. doi: 10.1007/s10585-020-10068-6. [DOI] [PubMed] [Google Scholar]
- 11.Pavlica M, Dawley T, Goenka A, Schulder M. Frame-based and mask-based stereotactic radiosurgery: The patient experience, compared. Stereotact Funct Neurosurg. 2021:1–9. doi: 10.1159/000511587. [DOI] [PubMed] [Google Scholar]
- 12.Lunsford LD, Niranjan A, Fallon K, Kim JO. Frame versus frameless Leksell stereotactic radiosurgery. Prog Neurol Surg. 2019;34:19–27. doi: 10.1159/000493046. [DOI] [PubMed] [Google Scholar]
- 13.Peach MS, Trifiletti DM, Dutta SW, Larner JM, Schlesinger DJ, Sheehan JP. Spatial shifts in frame-based Gamma Knife radiosurgery: A case for cone beam CT imaging as quality assurance using the Gamma Knife Icon. J Radiosurg SBRT. 2018;5:315–322. [PMC free article] [PubMed] [Google Scholar]
- 14.Soliman H, Ruschin M, Angelov L. Consensus contouring guidelines for postoperative completely resected cavity stereotactic radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys. 2018;100:436–442. doi: 10.1016/j.ijrobp.2017.09.047. [DOI] [PubMed] [Google Scholar]
- 15.Shaw E, Scott C, Souhami L. Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: Final report of RTOG protocol 90-05. Int J Radiat Oncol Biol Phys. 2000;47:291–298. doi: 10.1016/s0360-3016(99)00507-6. [DOI] [PubMed] [Google Scholar]
- 16.Colaco RJ, Yu JB, Bond JS. A contemporary dose selection algorithm for stereotactic radiosurgery in the treatment of brain metastases: An initial report. J Radiosurg SBRT. 2016;4:43–52. [PMC free article] [PubMed] [Google Scholar]
- 17.Cox DR. Regression models and life- tables. J R Stat Soc. 1972;34:187–220. [Google Scholar]
- 18.Meier ELKaP. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 19.Lin NU, Lee EQ, Aoyama H. Response assessment criteria for brain metastases: proposal from the RANO group. Lancet Oncol. 2015;16:e270–e278. doi: 10.1016/S1470-2045(15)70057-4. [DOI] [PubMed] [Google Scholar]
- 20.MacDonald RL, Lee Y, Schasfoort J, Soliman H, Sahgal A, Ruschin M. Real-time infrared motion tracking analysis for patients treated with gated frameless image guided stereotactic radiosurgery. Int J Radiat Oncol Biol Phys. 2020;106:413–421. doi: 10.1016/j.ijrobp.2019.10.030. [DOI] [PubMed] [Google Scholar]
- 21.Carminucci A, Nie K, Weiner J, Hargreaves E, Danish SF. Assessment of motion error for frame-based and noninvasive mask-based fixation using the Leksell Gamma Knife Icon radiosurgery system. J Neurosurg. 2018;129:133–139. doi: 10.3171/2018.7.GKS181516. [DOI] [PubMed] [Google Scholar]
- 22.Wegner RE, Horne ZD, Xu L. Adaptation of a Gamma Knife Icon stereotactic radiosurgery program in the face of the COVID-19 pandemic. J Radiosurg SBRT. 2020;7:5–10. [PMC free article] [PubMed] [Google Scholar]
- 23.Buss EJ, Vulpe H, Jacobsen J. Single-fraction stereotactic radiosurgery outcomes for brain metastases with frameless Gamma Knife ICON radiosurgery: An update. Int J Radiat Oncol Biol Phys. 2020;108:E676. [Google Scholar]
- 24.Alexander GS, Remick J, Kowalski ES. Frame based versus linac-based stereotactic radiosurgery for the treatment of brain metastases: Clinical outcomes and toxicity analysis. Int J Radiat Oncol Biol Phys. 2020;108:E705–E706. [Google Scholar]
- 25.Grimm MA, Koppen U, Stieler F. Prospective assessment of mask versus frame fixation during Gamma Knife treatment for brain metastases. Radiother Oncol. 2020;147:195–199. doi: 10.1016/j.radonc.2020.05.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.