Abstract
Introduction
In patients with vaginismus, the treatment becomes more challenging and the treatment may take longer as the grade of vaginismus is higher or worsens. However, the differences regarding treatment duration, success, and treatment methods by grades are not evident in the literature.
Aim
The aim of this study is to answer the question, “Does the number of treatment sessions, dilator requirement, treatment success, pre-& post-treatment FSFI scores and obstetric results of vaginismus patients change depending on the vaginismus-grade?”
Methods
The patients were divided into 4 grades according to the Lamont classification. They underwent stepwise treatment sessions by a single gynecologist. Treatment success, duration of treatment, mechanical dilator requirement, duration from marriage, pre- and post-treatment FSFI scores, pregnancy rates, and delivery types were compared between patients at different grades.
Main Outcome Measures
Assessment of the differences between vaginismus-grades by comparing clinical observations and FSFI-scores.
Results
Pain-free sexual intercourse occurred in 85 (93.4%) of 91 primary-vaginismus patients included in our study. The success rate was 100% in grade 1, 95.2% in grade 2, 92.1% in grade 3, and 92% in grade 4. Treatment session durations of the patients differed significantly by grades (P < .05). Same way the duration from marriage at the time of application differed significantly by the grade (P < .05). While there was a significant relationship between vaginismus grade and dilator requirement, there was no significant relationship between vaginismus grade and delivery type (P < .05). 54.5% of 44 patients, who got pregnant, delivered by cesarean-section. There was a significant increase in FSFI scores in all groups in the pre- and post-treatment third month (P < ,05).
Conclusion
Patients should be notified that as the grades of vaginismus progress, the duration of the treatment may extend, and its success may decrease, the requirement for mechanical dilators will increase in the advanced grade, and the grade may progress as the application period for treatment is delayed.
Kiremitli S, Kiremitli T. Examination of Treatment Duration, Treatment Success and Obstetric Results According to the Vaginismus Grades. Sex Med 2021;9:100407.
Key words: Vaginismus, FSFI, Lamont Classification, Sexual Dysfunction, Vaginismus Treatment
INTRODUCTION
Vaginismus is a critical problem that causes severe mental pain in addition to the physical pain.1 Vaginismus is newly defined in the latest edition of Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5) as a "Genito-Pelvic Pain Disorder and/or Penetration Disorder," (GPPPD) which attempts to bring together the concepts and full spectrum of painful vaginal penetration. This new definition brings together the spectrum of dyspareunia to vaginismus and also accounts for other penetration difficulties such as tampon use, finger penetration, difficulty with gynecologic examinations, and intercourse.
GPPPD is diagnosed by experiencing one or more of the specified following criteria continuously and/or repeatedly for at least 6 months2: Significant difficulty during vaginal intercourse and/or penetration, prominent vulvovaginal or pelvic pain during vaginal intercourse and/or penetration, prominent fear or anxiety about vulvovaginal or pelvic pain during vaginal penetration, prominent contraction and/or stretching of the pelvic muscles during vaginal penetration attempt. In the general population, the prevalence of vaginismus is 1–6%, and this ratio between 5 and17% in sexual dysfunction clinics.3
Vaginismus was first defined by Sims as “involuntary spasmodic closure of the mouth of the vagina, attended with such excessive supersensitiveness as to form a complete barrier to coition. ”4 In fact, Sims ' definition has been reinforced by modern authorities, Masters and Johnson described a “spastic” and “involuntary reflex” of the pelvic musculature that severely, if not entirely, impede the freedom of sexual response and sexual function of the woman. This muscle spasm definition first appeared in the third edition of the DSM and has remained essentially unchanged through DSM-4-TR.5,6,7
In DSM-4, vaginismus was defined as recurrent or persistent involuntary spasm of the musculature of the outer third of the vagina that interferes with sexual intercourse.8 Methods such as cognitive therapy, cognitive restructuring, education, sexual therapy, psychotherapy, relaxation to relieve muscle spasm, pelvic floor physical therapy, dilator treatment, hypnotherapy, and local botulinum toxin injection are used to treat vaginismus.9 Cognitive and behavioral therapy are more frequently used and effective methods in treatment.10,11
Vaginismus was divided into 4 grades by Lamont based on the gynecological examination and the patient's history (Table 1).12 The most severe vaginismus, grade 5, was defined by Pacik as the form in which bodily reactions such as tremors, hyperventilation, palpitations, crying attacks, fainting spells, nausea, vomiting, running away from the table, attacking a doctor due to intense fear experienced during gynecological examination.13
Table 1.
Lamont classification (Lamont, 1978)11
| Grade 1 | It is the mildest form. These patients can control the contraction of their vaginal muscles with the suggestions given during the examination. |
| Grade 2 | Despite the suggestions given to the patient, they continue to contract the pelvic floor muscles throughout the examination. |
| Grade 3 | Throughout the examination, the patient raises or pulls her hip to the side, thus trying to prevent the gynecological examination. |
| Grade 4 | During the examination, the patient lifts her hips, pulls herself back, closes her legs, and thus prevents the examination. |
In patients with vaginismus, the patients' treatment becomes more difficult, and the treatment period prolongs as the grade progresses. Treatment failure, prolonged treatment, and discontinuation of treatment are more common in patients with advanced vaginismus.14,15 However, studies that report the duration of treatment, success, and the need for dilators according to the grades are not common in the literature.
The aim of the present study is to answer the question, “Does the number of treatment sessions, dilator requirement, treatment success, pre-&post-treatment FSFI scores and obstetric results of vaginismus patients change depending on the vaginismus grade?” We hypothesized the vaginismus’ grade would be associated with number of treatment sessions, dilator requirement, treatment success, pre-&post-treatment FSFI scores.
MATERIAL AND METHODS
Ethics committee approval was obtained from the Ethics Committee of our University on January 28, 2021. Clinical Research Ethics Committee no: 03/01. In this study, 91 primary vaginismus patients who applied to our clinic between March 2018 and July 2020 were included by retrospectively from their files. The vaginismus diagnosis was made according to DSM-5 diagnostic criteria. Patients with sexual dysfunction in their husbands, hymenal abnormalities, congenital vaginal abnormalities, vulvodynia, secondary vaginismus following physical or psychological trauma, psychiatric or physiological disease were not included in the study. A single gynecologist treated the patients.
The patients were divided into 4 groups, according to Lamont staging. The Female Sexual Function Index (FSFI) scale was asked face-to-face to the patient in the pre-treatment session and on post-treatment control (12 week after coitus), and the scores were recorded. FSFI scale is a questionnaire consisting of 19 questions that evaluate female sexual function in the last 4 weeks, which includes 6 sub-headings as desire, arousal, lubrication, orgasm, satisfaction and pain. The scores of the subgroups are between 0 and 5. In total scoring, participants can score between a minimum of 2 and a maximum of 36 points. Increased scores are indicative of better sexual function.
The sessions were arranged every 4 to 7 days, depending on the availability of the patient and the physician. The average time for each session was 50 minutes. After each session, the patient and her partner were given homework assignments. The last session was repeated for the patients who could not complete their home assignment or could not successfully perform the exercises.
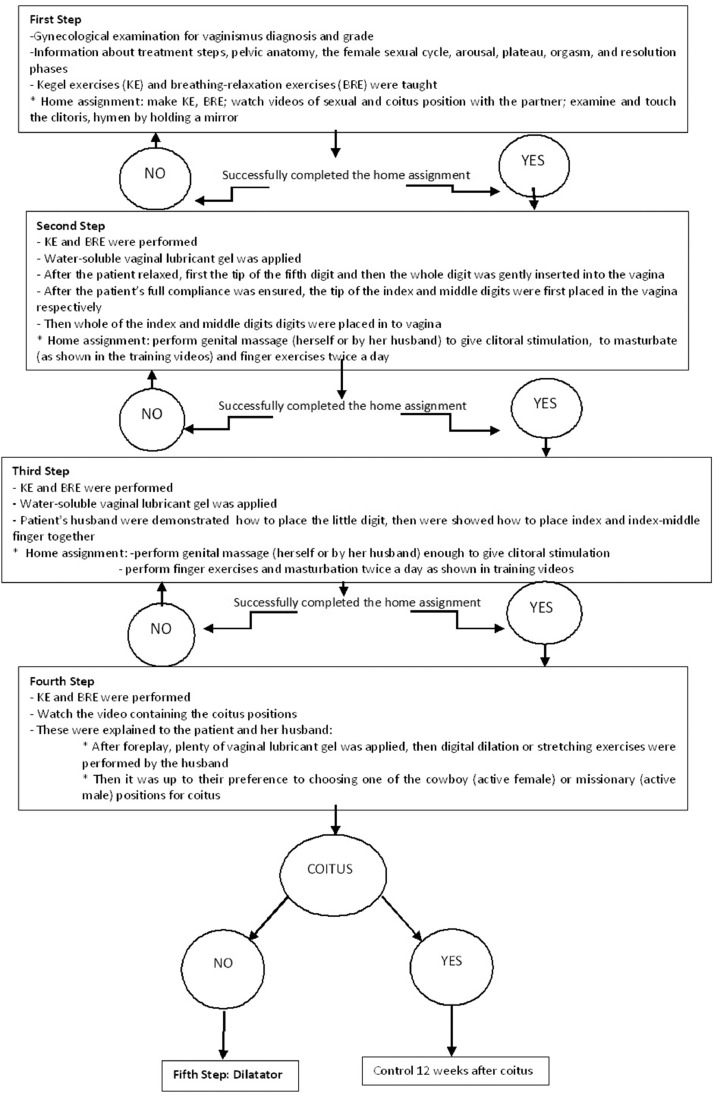
In the first step, the patients had a gynecological examination in the lithotomy position. After the diagnosis of vaginismus was made, its grade was determined. The patients and their husbands were informed about the treatment steps. Coitus was prohibited until the end of treatment. The patients had all sessions with their husbands, and the couples were given detailed information about the female sexual cycle, arousal, plateau, orgasm, and resolution phases.16 The anatomy and function of the hymen, pelvic floor, clitoris, and vagina were explained using models and anatomical drawings. Kegel exercises (KE) and breathing-relaxation exercises (BRE) were taught and written, and visual information was provided. At the end of the first session, the patients were given a home assignment to make KE, BRE, watch videos of sexual and coitus position with the partner, to examine and touch the clitoris, hymen by holding a mirror.
In the second step, the patient was placed in the lithotomy position. KE and BRE were performed under the guidance of the gynecologist. Water-soluble vaginal lubricant gel was applied to the vaginal area and the gynecologist's fingers. After the patient relaxed, first the tip of the fifth digit and then the whole digit was gently inserted into the vagina. While the digit was in, the patient was asked to do KE. After the patient's full compliance was ensured, the tip of the index and middle digits were first placed in the vagina respectively, and then whole of the digits were placed after complete relaxation was achieved. The patient was taught how to introduce her fingers to the vaginal area in the same way. At the end of this step as a homework, the patient was told to perform genital massage (herself or by her husband) to give clitoral stimulation, to masturbate (as shown in the training videos) and finger exercises twice a day.
In the third step, patients who fully complied with the second step exercises and completed their home assignments were taken to the third session treatment. After water-soluble vaginal lubricant gel was applied to the vaginal area, finger exercises applied in the second session were repeated by the gynecologist. Afterward, patient's husband was demonstrated how to place the little digit. Then we showed how to place index and index-middle finger together. At the end of this step as a homework; we told to patient perform genital massage (herself or by her husband) enough to give clitoral stimulation. Also was told to perform finger exercises and masturbation twice a day as shown in training videos.
In the fourth step, the couples who successfully implemented the third session home assignment were recommended to watch the video containing the coitus positions together. After foreplay, plenty of vaginal lubricant gel was applied, then digital dilation or stretching exercises were performed by the husband, and then it was up to their preference to choosing one of the cowboy (active female) or missionary (active male) positions for coitus.
The vaginismus treatment flow chart is shown in Figure 1.
Figure 1.
Vaginismus treatment flow chart.
Patients who failed to perform coitus after the fourth session treatment were included in the fifth step. At this stage, dilators of medical silicone structure were applied in 4 different sizes (1.5/2/2.5/3 cm in diameter and 6/8/10/13 cm in length). The patient was placed in the lithotomy position. After BRE, lubricant gel was applied to the vagina. First, the smallest dilator was applied. After 10 minutes, a larger-size dilator was switched to and waited for 10 other minutes. It was applied sequentially up to the largest size dilator that the patient could tolerate. The dilator application was given as a home assignment to be applied by the patient or her husband, starting from the smallest size twice per day about 15 minutes and continuing with a larger size each following day. The couples who successfully applied the largest dilator were asked to proceed to the coitus try as described previously.
IBM SPSS version 21 (IBM Corp. Armonk, N.Y. USA) was used in our analysis. In our analyzes, the relationship between categorical variables was examined with the Chi-square test. The Shapiro-Wilk test was used for detection the compliance of the data to normal distribution. Differences between pre- and post-treatment FSFI scores were analyzed with the Wilcoxon test. Multiple group comparisons with normally distributed data were compared using ANOVA test and presented as means ± standard deviations. The Kruskal-Wallis test was used for multiple group comparisons with non-normally distributed data and presented as median (minimum-maximum) value. For multiple comparisons; Tukey in the ANOVA test; Bonferroni-corrected Mann Whitney U test in Kruskal Wallis; Bonferroni test was used in Chi-square test. A level of P < .05 was considered statistically significant.
RESULTS
According to the Lamont grading, 91 primary vaginismus patients were divided to 4 groups. After the treatment, pain-free sexual intercourse occurred in 85 (93.4%) of the patients. The ages of the patients varied between 18 and 47 years, and the duration of marriage ranged between 7 and 60 months. Pregnancy occurred in 48.42% of the patients within one year after treatment. Relationship between variables and vaginismus grades are shown in Table 2.
Table 2.
Relationship between variables and vaginismus grades
| Grade | 1 | 2 | 3 | 4 | P |
|---|---|---|---|---|---|
| Age | 27.86 ± 4.1 | 26.86 ± 4.76 | 26.95 ± 4.61 | 29.44 ± 7.09 | .49 |
| The period from marriage to applying for treatment (month) | 11.14 ± 6.28 | 13.38 ± 7.11 | 18 ± 10.96 | 23.52 ± 13.89 | .01 (1<4,2<4) |
| Sessions of treatment | 4 ± 0 | 4.62 ± 1.4 | 6.08 ± 1.25 | 7.88 ± 1.94 | <.001 (1<3, 1<4, 2<3, 2<4, 3<4) |
| Duration of conception after treatment (month) | 4.33 ± 0.58 | 5.07 ± 2.50 | 6,3 ± 3,57 | 5.22 ± 2,59 | .684 |
| Mean sessions of dilatator using | 0 | 1.33 ± 0.58 | 1.73 ± 0.8 | 2.35 ± 0.88 | <.05 (1<2, 1<3, 1<4, 2<4) |
| Patients using dilator* | 0 | 3 | 15 | 20 | <.001 |
| Patients with failed treatment* | 0 | 1 | 3 | 2 | .851 |
| Pregnancy after treatment* | 3 | 14 | 19 | 8 | .131 |
| Total Patients | 7 | 21 | 38 | 25 |
Number of patient.
In the grade 1 group, 100% success was achieved. Pregnancy occurred in 3 patients, 2 of patients were delivered by cesarean, and one patient vaginally (Table 2).
In the grade 2 group, treatment was successful in 20 (95.2%) patients. Due to the inability to adapt to the exercises in the third session one patient was unsuccessful. Pregnancy occurred in 14 patients, 7 patients were delivered by cesarean, 4 patients vaginally. Three patients were still pregnant at the end of the study (Table 2).
In 38 patients of Grade 3, treatment was unsuccessful in 3 (7.9%) patients (due to loss of communication with one patient and inability to adapt to the finger and mechanical dilator in 2 patients). Pregnancy occurred in 19 patients. Twelve patients were delivered by cesarean and 2 patients vaginally. While pregnancy resulted in abortion in 2 patients, 3 patients were still pregnant when the study finished (Table 2).
In grade 4, treatment was unsuccessful in 2 patients (8%) (due to losing communication with one patient, one patient not adapting to exercises). Pregnancy occurred in 8 patients (48.4%). 3 patients were delivered by cesarean and 2 patients vaginally (Table 2). The pregnancy of 3 patients resulted in abortion.
In the grade 4 vaginismus group, the time from the first unsuccessful intercourse attempt to the admission for treatment was statistically significantly longer than in the grade 1 and grade 2 vaginismus group (23.5 ± 13.9 vs 11.1 ± 6.3, 23.5 ± 13.9 vs 13.4 ± 7.1 respectively) (P < .01). The marriage duration was 12 months or less in 71.4% of the first grade patients and 61.9% of the second grade patients. Therefore, the marriage period was longer than 12 months in 60.5% of the third grade and 80% of the fourth grade patients.
There was a significant relationship between grade and dilator requirement (P < .05). As the grade of vaginismus is higher or worsens, the need for a dilator increased. While no dilator was required in Grade 1, 76% of the patients in Grade 4 required a dilator (Table 2-3).
Table 3.
The relationship between coitus and dilator use with vaginismus grades
| Grade | 1 | 2 | 3 | 4 | |
|---|---|---|---|---|---|
| Total number of sessions with dilator used | *1 | 2 | 7 | 2 | |
| *2 | 1 | 5 | 12 | ||
| *3 | 3 | 3 | |||
| *4 | 3 | ||||
| After which session did coitus occur? | |||||
| †4th session | 7 | 15 | 1 | 0 | |
| †5th session | 3 | 15 | 2 | ||
| †6th session | 2 | 7 | 3 | ||
| †7th session | 7 | 7 | |||
| †8th session | 4 | 4 | |||
| †9th session | 1 | 3 | |||
| †10th session | 1 | ||||
| †11th session | 2 | ||||
| †13th session | 1 |
Sessions using dilator.
Treatment sessions.
No relationship was found between the grade and the delivery type (P > .05).
The pre- and post-treatment FSFI score increase showed a significant difference in total and desire, arousal, lubrication, orgasm, satisfaction, and pain subgroups in all groups except the arousal and orgasm subgroups in grade 1 (P < .05). The pre-treatment FSFI score of advanced-grade patients was lower. Post-treatment FSFI scores differed significantly according to the grades (P < .05). While the median score of grade 1 and grade 2 patients were higher, the median score of grade 4 patients was the lowest (Table 4).
Table 4.
Pre- and post-treatment FSFI scores in vaginismus grades
| Before treatment | After treatment | P | ||
|---|---|---|---|---|
| Grade 1 | Desire | 4.2 (3.6-4.8) | 5.4 (3.6-6) | .047 |
| Arousal | 3.3 (2.1-3.9) | 3.9 (3.3-4.2) | .054 | |
| Lubrication | 3.9 (3.6-4.2) | 5.7 (3.9-5.7) | .026 | |
| Orgasm | 2.4 (2-4.4) | 4.4 (2.4-4.8) | .062 | |
| Satisfaction | 2.8 (2.4-4) | 4.4 (2.8-4.8) | .027 | |
| Pain | 1.6 (1.2-2) | 5.2 (1.2-5.2) | .025 | |
| Total | 18.64 ± 1.82* | 28.9 (17.6-30.3)† | .028 | |
| Grade 2 | Desire | 4.2 (1.8-4.8) | 4.8 (3-5.4) | <.001 |
| Arousal | 3.3 (2.4-3.9) | 3.9 (3-4.5) | <.001 | |
| Lubrication | 3.9 (3-4.2) | 5.4 (3.6-5.7) | <.001 | |
| Orgasm | 2.4 (2-3.2) | 4.4 (2-4.8) | <.001 | |
| Satisfaction | 2.8 (1.6-3.6) | 4.4 (2-5.2) | <.001 | |
| Pain | 1.6 (1.2-2) | 5.2 (1.2-5.6) | <.001 | |
| Total | 17.86 ± 1.52* | 28.4 (15.1-30.4)† | <.001 | |
| Grade 3 | Desire | 3.6 (2.4-4.2) | 4.8 (3.6-5.4) | <.001 |
| Arousal | 3.0 (2-3.9) | 3.9 (3-4.5) | <.001 | |
| Lubrication | 3.6 (2.7-4.2) | 5.4 (4.8-5.7) | <.001 | |
| Orgasm | 2.0 (1.2-3.2) | 4.0 (3.2-5.2) | <.001 | |
| Satisfaction | 2.4 (2-3.6) | 4.4 (3.6-5.2) | <.001 | |
| Pain | 1.2 (0.4-2) | 4.8 (3.2-5.6) | <.001 | |
| Total | 15.94 ± 1.69* | 27.3 (23.9-30.8)† | <.001 | |
| Grade 4 | Desire | 3.0 (1.8-4.2) | 4.8 (3.6-5.4) | <.001 |
| Arousal | 2.7 (2.1-3.6) | 3.9 (3-4.5) | <.001 | |
| Lubrication | 3.6 (2.7-4.5) | 5.1 (4.5-5.4) | <.001 | |
| Orgasm | 2.0 (1.2-2.4) | 4.0 (3.2-4.8) | <.001 | |
| Satisfaction | 2.4 (1.6-3.6) | 4.4 (3.2-5.2) | <.001 | |
| Pain | 0.8 (0.4-1.6) | 4.8 (3.6-5.2) | <.001 | |
| Total | 14.62 ± 0.19* | 26.8 (22-30.1)† | <.001 | |
P < .001 (grade 1 > grade 3, grade 1 > grade 4, grade 2 > grade 3, grade 2 > grade 4, grade 3 > grade 4).
P = .01 (grade 1 > grade 4, grade 2 > grade 4).
The position in the first coitus was chosen by the patients. 75.3% of the couples chose the missionary position. There was no significant difference in position selection by grades.
DISCUSSION
Vaginismus is a sexual problem, and possibly end in divorce. Patients with vaginismus often make the first application to a gynecologist and get a diagnosis. Patients are diagnosed by gynecological examination, and Lamont staging is used to classify.17,18,19 Couples have many questions about uncertainty, embarrassment, anxiety for the future, and the method of treatment and success. The primary questions of the couples are the questions such as "What is the success rate?", "How long is the treatment period?", "What are the treatment steps?," and "What should my delivery method be?." There are no distinct studies in the literature enlightening the success rate and treatment method according to the patient's grade. It would be more accurate to present all patients with the expected results according to the disease's degree, rather than standard information about the treatment results.
With this study, we aimed to guide patients and gynecologists in this respect. More precise information can be given about the treatment success and duration of treatment according to the patients' grade. There are studies in the literature reporting treatment success between 43% and 100%.20,21 In our study, the treatment success rate was found to be 93.4%. This ratio differs by grades. In our study, the average treatment duration in grade 1 was 4 sessions, and complete success was achieved, while the average treatment duration in grade 4 was 7.8 sessions, and the success rate was 92%. We think that after the staging performed at the first examination, the applied couples can be informed more clearly about the duration of the treatment and the success rate in the light of this information. In this group of patients in which treatment anxiety is intense, the couples should be more patient as the grade progresses, and the information that the treatment may fail, although rarely, in the first session will ensure the safe progress of the patient-doctor relationship throughout the treatment period.
The desensitization method performed with vaginal penetration exercises is widely used today in the treatment of vaginismus.10 Finger exercises and/or dilators are frequently used. In the literature, there are studies that finger exercises are as effective as dilators, no dilator is required except for advanced vaginismus, and penetration with a foreign body is more difficult to be accepted by patients.22,23 A study conducted by Aslan et al. found that treatments with only gradual dilators had faster and more successful results than finger dilatations because they eliminated feelings of self-touch and disgust, and patients adhered to the situation better.24 In our study, all groups started with finger exercises and then switched to gradual dilator when pain-free sexual intercourse could not be achieved. When the grades were examined, while there was no need for dilators in grade 1, the need for dilators increased with advanced grades, and in grade 4, this rate increased up to 76.9%. In the light of these data, we think that it would be appropriate to explain to the patients that as the grade progresses, finger-only dilatation may not be sufficient and that a mechanical dilator may be needed.
It may be more appropriate to use a dilator instead of finger exercises to shorten the time and increase the patients' treatment motivation in advanced grades. However, more studies are needed to determine which dilatation method would be more successful in advanced grades.
In this study, there was a significant increase in FSFI total scores after treatment at all grades, in compliance with the literature.25 We think that the gynecologist can assure the patients that they will reach a better sexual function after treatment than the current status, regardless of their grade. Some vaginismus patients may enjoy sexual foreplay, have sexual desire, and lumbrication may occur, but tend to avoidance behavior due to penetration fear. The fear of penetration, which deepens with the unsuccessful attempts that increase over time, may cause the patient to move a way from every stage of sexuality and thus to decrease sexual desire.19,26,27 In our study, as the patients' grade advanced, the FSFI score at the time of application was observed to be lower. Patients in the 4th grade also had a lower score in all subgroups. In advanced grades, patients may develop more detachment, reluctance, avoidance behavior in their sexual life, and vaginal penetration failure. Like before the treatment, the total FSFI scores were significantly lower in the Grade 4 vaginismus group compared to the Grade 1 and Grade 2 groups. While the couples are given the first counseling, it can be promised that they will not only have pain-free sexual intercourse after treatment but also will reach a more satisfying sex life, regardless of the grade. For grade 4, although the score increased compared to pre-treatment, it remained lower than the other groups in the post-treatment period at the time of admission.
Increasing unsuccessful attempts, as the duration of the patients' struggle with vaginismus increases, may lead to an increase in the grade of patients' avoidance and distancing from sexuality.28 When the duration of marriage at the time of reference was examined according to the grades, we determined that the duration of marriage of the applying couples increased as the grade progressed. In the study conducted by Angin et al. they determined the long duration of marriage at the first application for treatment as a poor prognostic factor for success.29 Supporting this result, in our study, only 28.6% of grade 1 patients had a marriage duration longer than 12 months, while 80% of grade 4 patients had a marriage duration longer than 12 months. According to these results, patients should make their treatment applications to valid centers without delay. As the application is delayed, the patients' grades may progress, longer and more demanding treatment will be needed, and treatment success will decrease.
There are limited studies in the literature, conducted with a small number of patients, reported that the rate of cesarean section, perineal injury after vaginal delivery, and the frequency of dystocia increased in vaginismus patients.30 In our study, patients in all grades of vaginismus generally wanted cesarean delivery. Patients might prefer cesarean delivery due to anxiety of vaginismus recurrency. Since the obstetrician also supports this avoidance behavior, the cesarean rate may have increased in patients with vaginismus.
The relatively limited sample size and the inability to determine the delivery method and indications were the study's limitations. Another limitation of the study was that the FSFI score was only evaluated in the 3rd month. Score evaluations in the different time frames would enable us to provide more accurate information for the long term.
CONCLUSIONS
In conclusion, couples with vaginismus are a critical group of patients who need detailed and accurate information regarding the treatment results at the time of first application due to their anxiety, uncertainty, and embarrassment. Correct information about treatment results will lead to safer progress of subsequent treatments for both the couples and the doctor. With this study, the results waiting for them regarding treatment successes, durations, treatment methods, and delivery types by the patients' grades can be presented in an explanatory manner. It should be emphasized to couples that the treatment period in advanced-grade patients may be longer and more complicated, that dilators may be needed, and more efforts are needed to improve sexual function.
STATEMENT OF AUTHORSHIP
Sevil Kiremitli: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Software; Writing-original draft. Tunay Kiremitli: Formal analysis, Resources, Supervision, Validation, Visualization, Writing-review & editing.
We declare that this work was done by the authors named in this article and all liabilities pertaining to claims relating to the content of this article will be borne by the authors. All authors read and approved the manuscript for publication.
Footnotes
Conflict of Interest: We declare that there is no conflict of interest in this study.
Funding: None.
References
- 1.Pacik PT, Odyne Publishing. Manchester NH. Odyne Publishing; Manchester, NH: 2010. When sex seems impossible. Stories of vaginismus & how you can achieve intimacy. [Google Scholar]
- 2.American Psychiatric Association . 5th ed. American Psychiatric Press; USA: 2013. DSM-5: Diagnostic and Statistical Manual for Mental Disorders. [Google Scholar]
- 3.Konkan R, Bayrak M, Gonullu GO. Sexual function and satisfaction of women with vaginismus. J Psychiatry Neurol Sci. 2012;25:305–311. [Google Scholar]
- 4.Sims MJ. On vaginismus. Trans. Obstet. Soc. London. 1861;3:356–367. [Google Scholar]
- 5.American Psychiatric Association . 3rd ed. Author; Washington, DC: 1980. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 6.Masters WH, Johnson VE. Little, Brown; London: 1970. Human sexual inadequacy; p. 250. [Google Scholar]
- 7.Binik YM. The DSM diagnostic criteria for vaginismus. Arch Sex Behav. 2010;39:278–291. doi: 10.1007/s10508-009-9560-0. [DOI] [PubMed] [Google Scholar]
- 8.Association American Psychiatric. 4th ed., text rev. Author; Washington, DC: 2000. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 9.Pacik PT. Understanding and treating vaginismus: A multimodal approach. Int Urogynecol J. 2014;25:1613–1620. doi: 10.1007/s00192-014-2421-y. [DOI] [PubMed] [Google Scholar]
- 10.Melnik T, Hawton K, McGuire H. Interventions for vaginismus. Cochrane Database Syst Rev. 2012;12 doi: 10.1002/14651858.CD001760.pub2. CD001760–CD001760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eserdag S, Angin AD. Importance of gynecological assessment for the treatment of vaginismus as a predictive value. J Obstet Gynaecol Res. 2020 doi: 10.1111/jog.14600. [DOI] [PubMed] [Google Scholar]
- 12.Lamont JA. Vaginismus. Am J Obstet Gynecol. 1978;131:633–636. [PubMed] [Google Scholar]
- 13.Pacik PT. Vaginismus: The Lamont classification revisited. Poster presentation at the ISSWSH Annual Meeting; Scottsdale; 2011. [Google Scholar]
- 14.Pacik PT, Babb CR, Polio A. Case series: Redefining severe Grade 5 vaginismus. Sex Med. 2019;7:489–497. doi: 10.1016/j.esxm.2019.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pacik PT. Vaginismus: Review of current concepts and treatment using botox injections, bupivacaine injections, and progressive dilation with the patient under anesthesia. Aesthetic Plast Surg. 2011;35:1160–1164. doi: 10.1007/s00266-011-9737-5. [DOI] [PubMed] [Google Scholar]
- 16.Masters WH, Johnson VE. Masters and Johnson Inst; St. Louis, MO: 1986. Sex therapy on its twenty-fifth anniversary: Why it survives. [Google Scholar]
- 17.Daňková Kučerová J, Machač Š, Vrzáčková P. Vaginismus - who takes interest in it? Ceska Gynekol. 2019 Spring;84:233–239. English. [PubMed] [Google Scholar]
- 18.Reissing ED. Consultation and treatment history and causal attributions in an online sample of women with lifelong and acquired vaginismus. J Sex Med. 2012;9:251–258. doi: 10.1111/j.1743-6109.2011.02534.x. [DOI] [PubMed] [Google Scholar]
- 19.Muammar T, McWalter P, Alkhenizan A. Management of vaginal penetration phobia in Arab women: A retrospective study. Ann Saudi Med. 2015;35:120–126. doi: 10.5144/0256-4947.2015.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hawton K, Catalan J. Sex therapy for vaginismus. Characteristics of couples and treatment outcome. Sex Marital Ther. 1990;5:39–48. [Google Scholar]
- 21.Eserdag S, Zulfikaroglu E, Akarsu S. Treatment outcome of 460 women with vaginismus. Eur J Surg Sci. 2011;2:73–79. [Google Scholar]
- 22.Mousabi Nasab M, Farnoosh Z. Management of vaginismus with cognitive-behavioral therapy, self-finger approach: A study of 70 cases. Iran J Med Sci. 2003;28:69–71. [Google Scholar]
- 23.Saadat HS. Vaginismus: A review of literature and recent updated treatments. Int J Med Rev. 2014;1:97–100. [Google Scholar]
- 24.Aslan M, Yavuzkır S, Baykara S. Is “Dilator Use” more effective than “Finger Use” in exposure therapy in vaginismus treatment? J Sex Marital Ther. 2020;46:354–360. doi: 10.1080/0092623X.2020.1716907. [DOI] [PubMed] [Google Scholar]
- 25.Bokaie M, Bostani Khalesi Z. Couple therapy and vaginismus: A single case approach. J Sex Marital Ther. 2019;45:667–672. doi: 10.1080/0092623X.2019.1610126. [DOI] [PubMed] [Google Scholar]
- 26.van der Velde J, Laan E, Everaerd W. Vaginismus, a component of a general defensive reaction. an investigation of pelvic floor muscle activity during exposure to emotion-inducing film excerpts in women with and without vaginismus. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12:328–331. doi: 10.1007/s001920170035. [DOI] [PubMed] [Google Scholar]
- 27.Cherner RA, Reissing ED. A psychophysiological investigation of sexual arousal in women with lifelong vaginismus. J Sex Med. 2013;10:1291–1303. doi: 10.1111/jsm.12102. [DOI] [PubMed] [Google Scholar]
- 28.Jebelli F, Maaroufi M, Maracy M. Effectiveness of eye movement desensitization and reprocessing (EMDR) on the sexual function of Iranian women with lifelong vaginismus. Sexual and Relationship Therapy. 2018;33:325–338. [Google Scholar]
- 29.Angin AD, Gun I, Sakin O. Effects of predisposing factors on the success and treatment period in vaginismus. JBRA Assist Reprod. 2020;24:180–188. doi: 10.5935/1518-0557.20200018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tourrilhes E, Veluire M, Hervé D. Pronostic obstétrical des femmes atteintes de vaginisme primaire [Obstetric outcome of women with primary vaginismus] Pan Afr Med J. 2019;32:160. doi: 10.11604/pamj.2019.32.160.16083. French. [DOI] [PMC free article] [PubMed] [Google Scholar]