Highlights
-
•
Variation in H1N1 vaccination rate among Medicaid enrollees is huge across states and racial subgroups.
-
•
Black enrollees have lower vaccination rates than white enrollees in most states.
-
•
Asian/Pacific islander and Hispanic enrollees have higher vaccination rates than white enrollees in most states.
-
•
Degree of racial disparity in H1N1 vaccination rate varies considerably across states.
Keywords: H1N1 vaccination, Racial disparity, COVID vaccination, Geographic disparity, Medicaid
Abstract
Background
Racial and ethnic minorities in the US have been disproportionately affected by the COVID-19 pandemic and are at risk for disparities in COVID-19 vaccinations. The H1N1 flu vaccine experience provides lessons learned to address and prevent racial and ethnic disparities in COVID-19 vaccinations. We aim to identify racial/ethnic and geographic disparities in H1N1 vaccinations among Medicaid enrollees to inform equitable COVID-19 vaccination policies and strategies.
Methods
The study population included people under 65 who were continuously enrolled in Medicaid in 2009 and 2010 from 28 states and the District of Columbia. H1N1 vaccinations were identified from Medicaid outpatient claims. Vaccination rates were calculated for the overall sample and subpopulations by race/ethnicity and state.
Results
3,708,894 (12.3%) Medicaid enrollees in the sample were vaccinated for H1N1 in 2009–2010. Race-specific vaccination rates ranged from 8.1% in American Indian/Alaska Native (AI/AN) to 19.8% in Asian/Pacific Islander Medicaid enrollees. NHB enrollees had lower vaccination rates than non-Hispanic White (NHW) enrollees in all states, with the exceptions of Maryland, Missouri, Ohio, and Washington. The largest disparity between NHB and NHW was in Pennsylvania (1.0% vs. 7.0%), while the largest absolute difference between NHB and NHW enrollees was in Georgia (17.4% vs. 30.7%).
Conclusions
Our study found huge variation in H1N1 vaccinations across states and racial/ethnic disparities in H1N1 vaccinations within states. In most states, NHB and AI/AN Medicaid enrollees had lower vaccination rates than Whites. Hispanic and Asian/Pacific Islander Medicaid enrollees in most states had higher vaccination rates than Whites.
1. Introduction
The COVID-19 pandemic has disproportionately impacted racial and ethnic minority communities in the US (Mahajan & Larkins-Pettigrew, 2020). In December 2020, the Food and Drug Administration granted emergency approval of two SARS-COV-2 vaccines in the United States (US). Within days, limited quantities of the vaccines were shipped to every state in the nation. Supply was limited and the Centers for Disease Control and Prevention’s (CDC) Advisory Committee on Immunization Practices (ACIP) developed guidance for prioritizing populations, which most states used to develop their implementation plans (Dooling et al., 2021, Dooling et al., 2020). States implemented phased approaches to vaccination allocation, with many prioritizing populations at highest risk first, including health care workers, people with high-risk medical conditions, people aged 65 and over and other essential workers.
As a key source of insurance coverage for low-income adults, pregnant women, people with disabilities, and children in the US, Medicaid programs are central to mitigating the disproportionate impact of COVID-19. Medicaid covers almost 20% of the US population and insures disproportionate shares of racial and ethnic minorities (Andrews et al., 2015) Medicaid has historically played a significant role in vaccination efforts by increasing access and ensuring affordability of vaccines for low-income children and adults (Johnson et al., 2000). Racial and ethnic disparities in vaccination uptake are long-standing. In the 1970 s, White children were 18% more likely to receive a measles vaccination than children of other racial/ethnic groups (Hutchins et al., 2004). Medicaid was a key component to eliminating this gap through targeted efforts, including mandatory coverage through the Vaccines for Children program, linking social services programs with immunization efforts, partnering with minority health organizations, and executing culturally and linguistically tailored communication campaigns (Conis, 2019, Hutchins et al., 2004). Adult disparities in vaccination rates remain, with 41.8% of adults enrolled in Medicaid HMO plans receiving an influenza vaccination in 2018 compared with 52% of those enrolled in commercial insurance plans (Flu vaccinations, 2020).
Racial and ethnic minority populations are at risk for similar disparities in COVID-19 vaccinations, despite being at higher risk for COVID-19 exposure and infection (Mahajan & Larkins-Pettigrew, 2020). As of February 1, 2021, 39.6% of vaccine recipients with documented race/ethnicity were people of color, but importantly, 50% of vaccination records were missing race/ethnicity data (Painter et al., 2021). More recent data show some improvement in vaccination rates for people of color, with 30% of vaccines administered from July 4–18, 2021 going to Hispanic people and 14% to Black people (Ndugga et al., 2021). However, inequities in vaccine uptake remain.
Although the current COVID-19 pandemic is unprecedented, the H1N1 flu vaccine experience may provide insight for addressing and preventing potential racial and ethnic disparities in COVID-19 vaccination rates (Baumgartner et al., 2020). Despite dramatic differences in case incidence, hospitalizations, mortality, and vaccine development and distribution processes between H1N1 and COVID-19, H1N1 also was a global pandemic that required introduction of a novel vaccine, with an urgency to distribute the vaccine widely in order to prevent further virus spread. In the H1N1 vaccination response, White people were significantly more likely to receive the H1N1 vaccine than Black people (Flu vaccination coverage, 2020) but little is known about parallel racial and ethnic disparities in H1N1 vaccine uptake within the Medicaid population. In this study, our goal was to identify racial/ethnic and geographic disparities in the uptake of H1N1 vaccine among Medicaid enrollees in 28 states and the District of Columbia in order to highlight potential successes and challenges that support equitable distribution of the COVID-19 vaccine in the Medicaid population.
2. Materials and Methods
The study population was drawn from 2009 to 2010 Medicaid Analytic eXtract (MAX) files from 28 states (Alabama, Arizona, Arkansas, California, Colorado, Connecticut, Florida, Georgia, Illinois, Indiana, Louisiana, Maryland, Massachusetts, Michigan, Mississippi, Missouri, New Jersey, New Mexico, New York, North Carolina, Ohio, Oklahoma, Pennsylvania, South Carolina, Tennessee, Texas, Virginia, and Washington) and the District of Columbia. The 28 states comprise the complete data set available to the study team for the period of interest and includes 80% of all Medicaid enrollees and 90% of racial/ethnic minority enrollees at the time. Medicaid enrollees were included in this study based on the following criteria: (1) 12 months of continuous enrollment from August 1, 2009 to July 31, 2010, (2) younger than 65 years old, and (3) not Medicare and Medicaid dual eligible.
The main outcome was receipt of H1N1 vaccination during the study period. H1N1 vaccination was identified by the following codes in outpatient claims data: (1) CPT codes = 90470, 90662, 90663, 90655–90661, 90724, or (2) Healthcare Common Procedure Coding System (HCPCS) codes = G0008, Q2035, Q2036, Q2037, Q2038. We also obtained demographic information of the study population (including age, race/ethnicity, gender), Elixhauser Comorbidity Index (ECI), Medicaid eligibility, and managed care/fee for service (FFS) plan enrollment. The ECI, a validated approach that summarizes disease burden and predicts risk using administrative claims data (Elixhauser et al., 1998), was determined through outpatient and inpatient claims data. Medicaid eligibility was categorized into four groups: (1) age/blind/disabled, (2) child, (3) adult, and (4) other. Medicaid plan enrollment type was categorized into three groups: (1) enrolled in FFS for the entire study period, (2) enrolled in managed care for the entire study period, and (3) switched between managed care and FFS one or more times during the study period.
Characteristics of the study population are presented for the overall sample, enrollees who had any H1N1 vaccination, and enrollees who had no H1N1 vaccination during 2009–2010. We calculated overall vaccination rate (proportion of enrollees who had any H1N1 vaccination) and vaccination rates for racial/ethnic subpopulations for the overall sample and subpopulations by state. Using enrollee receipt of H1N1 vaccine as the outcome variable, we conducted unadjusted and adjusted logistic regression, with odds ratios, 95% confidence intervals, and p-values reported for each independent variable. All analyses were completed using SAS 9.4 (Carey, NC).
We created maps to illustrate state-level vaccination rates across the overall sample, vaccination rates among Non-Hispanic Black (NHB) subpopulation, vaccination rates among Non-Hispanic White (NHW) subpopulation, and vaccination rate ratio between NHW and NHB populations using ArcGIS Pro (ESRI, Redland, CA). The Morehouse School of Medicine Institutional Review Board approved this study, and all patient records and information were anonymized and deidentified.
3. Results
There were 30,232,340 Medicaid enrollees who met inclusion criteria for the study. Table 1 presents the descriptive statistics of the sample. A total of 3,708,894 (12.3%) received the H1N1 in 2009–2010. Enrollees 18 years of age and younger were most overrepresented in the vaccinated group compared to the overall sample (81.3% versus 63.7%), while those aged 50–64 were slightly more overrepresented in the vaccinated group (7.66% versus 5.9%). Enrollees aged 19–35 were the most underrepresented in the vaccinated group compared to the overall sample (7.4% versus 20.6%), while those aged 36–50 were somewhat less underrepresented in the vaccinated group (5.3% versus 9.9%). Hispanic enrollees were overrepresented in the vaccinated group compared to the overall population (36.6% versus 29.4%), while NHB and American Indian/Alaska Native (AI/AN) enrollees were underrepresented in the vaccinated group (20.2% versus 27.8% and 0.8% versus 1.3% respectively).
Table 1.
Overall description of Medicaid enrollees in 28 states and the District of Columbia with and without H1N1 vaccination in 2009–2010, n = 30,232,340.
| Vaccinated (n = 3,708,894) | Unvaccinated (n = 26,523,446) | Overall(n = 30,232,340) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Age | ||||||
| <=18 | 3,013,621 | 81.3 | 16,233,600 | 61.2 | 19,247,221 | 63.7 |
| 19–35 | 274,213 | 7.4 | 5,939,677 | 22.4 | 6,213,890 | 20.6 |
| 36–50 | 197,965 | 5.3 | 2,782,529 | 10.5 | 2,980,494 | 9.9 |
| 50–64 | 223,095 | 6.0 | 1,567,640 | 5.9 | 1,790,735 | 5.9 |
| Race/Ethnicity | ||||||
| NHW | 1,341,021 | 36.2 | 10,020,012 | 37.8 | 11,361,033 | 37.6 |
| NHB | 750,410 | 20.2 | 7,649,998 | 28.8 | 8,400,408 | 27.8 |
| AI/AN | 31,067 | 0.8 | 353,206 | 1.3 | 384,273 | 1.3 |
| A/PI | 213,569 | 5.8 | 867,846 | 3.3 | 1,081,415 | 3.6 |
| Hispanic | 1,355,457 | 36.6 | 7,530,124 | 28.4 | 8,885,581 | 29.4 |
| Other | 17,370 | 0.5 | 102,260 | 0.4 | 119,630 | 0.4 |
| Gender | ||||||
| Female | 1,981,031 | 53.4 | 15,373,784 | 58.0 | 17,354,815 | 57.4 |
| Male | 1,727,863 | 46.6 | 11,149,662 | 42.0 | 12,877,525 | 42.6 |
| ECI | ||||||
| 0 | 3,365,574 | 90.7 | 23,932,838 | 90.2 | 27,298,412 | 90.3 |
| 1 to 2 | 277,634 | 7.5 | 2,234,415 | 8.4 | 2,512,049 | 8.3 |
| 3 and above | 65,686 | 1.8 | 356,193 | 1.3 | 421,879 | 1.4 |
| Medicaid Eligibility | ||||||
| Aged/Blind/Disabled | 395,703 | 10.7 | 3,403,184 | 12.8 | 3,798,887 | 12.6 |
| Child | 2,874,966 | 77.5 | 15,887,483 | 59.9 | 18,762,449 | 62.1 |
| Adult | 368,677 | 9.9 | 6,757,080 | 25.5 | 7,125,757 | 23.6 |
| Other | 69,548 | 1.9 | 475,699 | 1.8 | 545,247 | 1.8 |
| MC/FFS | ||||||
| FFS only | 111,544 | 3.0 | 2,512,155 | 9.5 | 2,623,699 | 8.7 |
| MC only | 2,649,241 | 71.4 | 16,359,415 | 61.7 | 19,008,656 | 62.9 |
| Any Switching | 948,109 | 25.6 | 7,651,876 | 28.9 | 8,599,985 | 28.5 |
NHW, non-Hispanic white; NHB, non-Hispanic Black; AI/AN, American Indian/Alaska Natives; A/PI, Asian/Pacific Islanders; ECI, Elixhauser Comorbidity Index; MC, managed care; FFS, fee for service.
Table 2 presents vaccination rates by race/ethnicity and across the 28 states and Washington, DC. The overall H1N1 vaccination rate in the sample was 12.3%, with rates of NHB, NHW and AI/AN enrollees below the overall rate (8.9%, 11.8% and 8.1% respectively) and Hispanic and Asian/Pacific Islander (A/PI) enrollees exceeding the overall rate (15.3% and 19.8% respectively). H1N1 vaccination rates varied by state, ranging from 1.1% (Maryland) to 24.8% (Alabama). Approximately 80% of states had overall rates<20% with wide state-level variation across racial/ethnic subgroups. For NHB, rates ranged from 1.0% (Pennsylvania) to 21.0% (Alabama), with nearly all states vaccinating<20% of NHB enrollees. NHB rates slightly exceeded overall rates in three states (Maryland, Missouri, Ohio) and Washington, DC and fell below overall rates in all other states. Vaccination rates for AI/AN enrollees slightly exceeded overall rates in 10 states (Connecticut, Georgia, Indiana, Louisiana, New Jersey, New York, Ohio, South Carolina, Texas, Virginia) and fell below overall rates in all other states. Vaccination rates in Hispanic enrollees exceeded overall rates in all but five states (Massachusetts, Maryland, North Carolina, Oklahoma, Pennsylvania) and Washington, DC. Rates for A/PI enrollees exceeded overall rates in all but four states (Massachusetts, Maryland, Ohio, Pennsylvania). Vaccination rates for NHW enrollees exceeded overall rates in 16 states and Washington, DC and fell below overall rates in the remaining states.
Table 2.
Overall and state-level H1N1 vaccination rates by race/ethnicity among Medicaid enrollees, 2009–2010.
| Overall | Overall VR | NHB VR | NHW VR | Hispanic VR | A/PI VR | AI/AN VR | Other VR |
|---|---|---|---|---|---|---|---|
| 12.3 | 8.9 | 11.8 | 15.3 | 19.8 | 8.1 | 14.5 | |
| State | Overall VR | NHB VR | NHW VR | Hispanic VR | A/PI VR | AI/AN VR | Other VR |
| AL | 24.8 | 21.0 | 25.3 | 53.0 | 35.6 | 20.4 | NA |
| AR | 19.6 | 14.4 | 20.5 | 30.5 | 21.5 | 16.3 | 19.8 |
| AZ | 21.9 | 16.1 | 18.2 | 29.1 | 32.4 | 7.9 | NA |
| CA | 9.0 | 6.2 | 6.2 | 9.7 | 13.7 | 4.4 | NA |
| CO | 8.7 | 6.1 | 9.2 | 8.8 | 10.5 | 7.3 | NA |
| CT | 10.1 | 7.1 | 10.8 | 11.0 | 11.5 | 10.6 | NA |
| DC | 1.6 | 1.7 | 3.2 | 1.1 | 7.4 | NA | 1.9 |
| FL | 13.5 | 10.5 | 12.7 | 17.8 | 18.7 | 13.4 | NA |
| GA | 23.7 | 17.4 | 30.7 | 40.0 | 42.6 | 24.7 | NA |
| IL | 11.1 | 6.5 | 10.1 | 17.9 | 17.3 | 8.7 | 11.6 |
| IN | 13.7 | 10.7 | 14.1 | 17.8 | 19.7 | 19.2 | NA |
| LA | 8.1 | 7.3 | 8.3 | 20.0 | 17.2 | 9.0 | 9.8 |
| MA | 5.3 | 3.7 | 6.4 | 3.7 | 5.0 | 4.7 | 7.2 |
| MD | 1.1 | 1.2 | 1.0 | 0.9 | 1.0 | 1.0 | NA |
| MI | 16.8 | 13.1 | 17.7 | 27.7 | 27.9 | 13.9 | NA |
| MO | 11.1 | 11.2 | 10.1 | 22.1 | 18.7 | 8.1 | 23.9 |
| MS | 4.7 | 3.4 | 6.8 | 10.4 | 9.4 | 1.5 | NA |
| NC | 2.6 | 2.3 | 3.6 | 0.6 | 2.7 | 1.6 | 3.4 |
| NJ | 17.4 | 12.5 | 18.1 | 23.0 | 19.9 | 20.9 | NA |
| NM | 20.7 | 18.1 | 19.4 | 24.3 | 23.4 | 9.8 | NA |
| NY | 18.0 | 13.1 | 16.4 | 19.5 | 29.4 | 19.3 | 21.0 |
| OH | 1.6 | 1.8 | 1.6 | 1.7 | 1.5 | 2.1 | NA |
| OK | 2.7 | 2.3 | 3.2 | 2.6 | 3.7 | 1.9 | 2.4 |
| PA | 4.5 | 1.0 | 7.0 | 2.0 | 1.8 | 4.0 | 4.9 |
| SC | 2.6 | 1.6 | 3.4 | 5.7 | 4.0 | 6.3 | 1.5 |
| TN | 14.1 | 10.1 | 15.0 | 27.3 | 19.5 | 14.0 | NA |
| TX | 16.2 | 11.0 | 11.4 | 19.1 | 25.4 | 19.0 | NA |
| VA | 24.4 | 20.0 | 23.8 | 38.8 | 33.9 | 26.8 | 31.5 |
| WA | 20.6 | 19.5 | 17.5 | 28.3 | 28.4 | 12.3 | 21.9 |
VR, vaccination rate; NHB, non-Hispanic black; AI/AN, American Indian/Alaska Natives; A/PI, Asian/Pacific Islanders.
Table 3 presents bivariate and multivariate linear regression analysis of H1N1 vaccination among Medicaid enrollees in 2009–2010. Each predictor was significantly (p-value < 0.001) associated with H1N1 vaccination in the unadjusted regression model. In the adjusted model, older age groups had lower odds of vaccination compared to those 18 years or younger (Age 19–35: OR = 0.326, 95% CI = 0.324–0.328; Age 36–50: OR = 0.442, 95%CI = 0.438–0.445; Age 50–64: OR = 0.711, 95%CI = 0.706–0.716). NHB (OR = 0.688, 95%CI = 0.686–0.690) and AI/AN (OR = 0.697, 95%CI = 0.689–0.705) enrollees were significantly less likely than NHW to have received H1N1 vaccination, while API (OR = 2.035, 95%CI = 2.204–2.045), and Hispanic (OR = 1.303, 95%CI = 1.300–1.307) enrollees had higher odds of vaccination compared to NHW enrollees. Odds of H1N1 vaccination increased by 46% for enrollees with 1–2 comorbidities (OR = 1.459, 95%CI = 1.453–1.466) and more than doubled for those with three or more comorbidities (OR = 2.171, 95%CI = 2.151–2.191). Enrollees who were eligible for Medicaid as adults (OR = 0.776, 95%CI = 0.772–0.781) were 23% less likely to be vaccinated compared to those eligible as aged/blind/disabled. Enrollment in FFS plans only (OR = 0.384, 95%CI = 0.381–0.386) was associated with a 62% decrease in the odds of H1N1 vaccination, any switching between the FFS and MC plans (OR = 0.803, 95%CI = 0.801–0.805) was associated with a 20% decrease in the odds of vaccination.
Table 3.
Bivariate and multivariate linear regression analysis of H1N1 vaccination among Medicaid enrollees, 2009–2010.
| Unadjusted OR | 95% CI | P-value | Adjusted OR | 95% CI | P-value | |
|---|---|---|---|---|---|---|
| Age | ||||||
| 18 and younger | ref | ref | ||||
| 19–35 | 0.249 | 0.248–0.250 | <0.001 | 0.326 | 0.324–0.328 | <0.001 |
| 36–50 | 0.383 | 0.381–0.385 | <0.001 | 0.442 | 0.438–0.445 | <0.001 |
| 50–64 | 0.767 | 0.763–0.770 | <0.001 | 0.711 | 0.706–0.716 | <0.001 |
| Race/Ethnicity | ||||||
| NHW | ref | ref | ||||
| NHB | 0.733 | 0.731–0.735 | <0.001 | 0.688 | 0.686–0.69 | <0.001 |
| AI/AN | 0.657 | 0.650–0.665 | <0.001 | 0.697 | 0.689–0.705 | <0.001 |
| API | 1.839 | 1.829–1.848 | <0.001 | 2.035 | 2.024–2.045 | <0.001 |
| Hispanic | 1.345 | 1.342–1.348 | <0.001 | 1.303 | 1.3–1.307 | <0.001 |
| Other | 1.269 | 1.249–1.290 | <0.001 | 1.255 | 1.235–1.276 | <0.001 |
| Gender | ||||||
| Female | 0.831 | 0.830–0.833 | <0.001 | 1.046 | 1.044–1.049 | <0.001 |
| Male | ref | ref | ||||
| Elixhauser Comorbidity | ||||||
| 0 | ref | ref | ||||
| 1 to 2 | 0.884 | 0.880–0.887 | <0.001 | 1.459 | 1.453–1.466 | <0.001 |
| 3 and above | 1.312 | 1.301–1.323 | <0.001 | 2.171 | 2.151–2.191 | <0.001 |
| Medicaid Eligibility | ||||||
| Aged/Blind/Disabled | ref | ref | ||||
| Child | 1.556 | 1.551–1.562 | <0.001 | 1.034 | 1.028–1.04 | <0.001 |
| Adult | 0.469 | 0.467–0.472 | <0.001 | 0.776 | 0.772–0.781 | <0.001 |
| Other | 1.257 | 1.247–1.268 | <0.001 | 1.048 | 1.038–1.058 | <0.001 |
| Managed Care/FFS | ||||||
| FFS only | 0.274 | 0.273–0.376 | <0.001 | 0.384 | 0.381–0.386 | <0.001 |
| MC only | ref | ref | ||||
| Any Switching | 0.765 | 0.763–0.767 | <0.001 | 0.803 | 0.801–0.805 | <0.001 |
OR, odds ratio; CI, confidence interval; NHB, non-Hispanic black; AI/AN, American Indian/Alaska Natives; A/PI, Asian/Pacific Islanders; MC, managed care; FFS, fee for service.
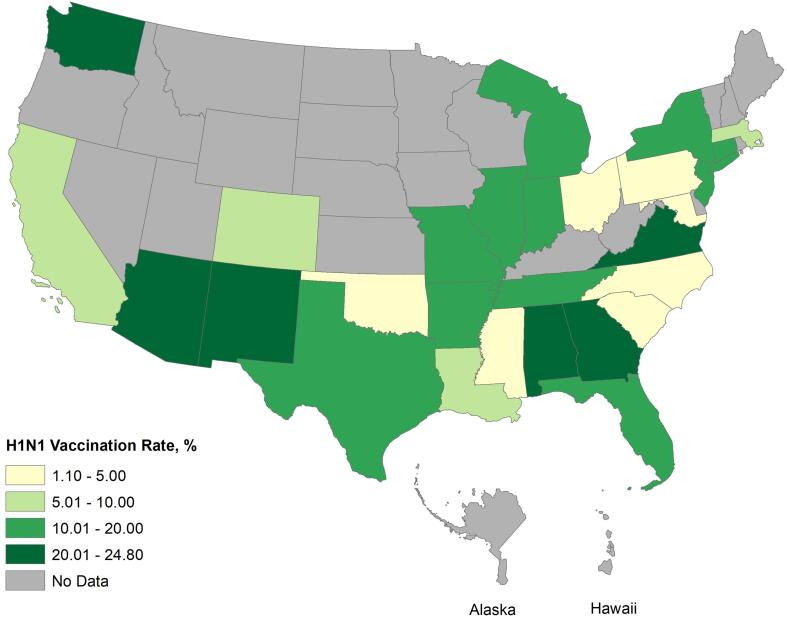
Fig. 1 maps state-level variation in overall vaccination rates, showing that geographic patterning by region is not strong, as many states with the highest rates neighbor states with the lowest rates. In all but five states (California, Maryland, Missouri, Ohio, Washington), NHB enrollees had lower vaccination rates than NHW. The largest absolute difference between NHW and NHB enrollee vaccination rates was 13.3%, in Georgia. A/PI rates exceeded NHB and NHW in all states except Massachusetts, Maryland, North Carolina, Ohio and Pennsylvania. Among Hispanic enrollees, Alabama’s vaccination rate was the highest for any state and racial/ethnic group. Among A/PI enrollees, vaccination rates ranged from 1.0% (Maryland) to 42.6% (Georgia). Finally, among AI/AN enrollees, rates ranged from 1.0% (Maryland) to 26.8% (Virginia).
Fig. 1.
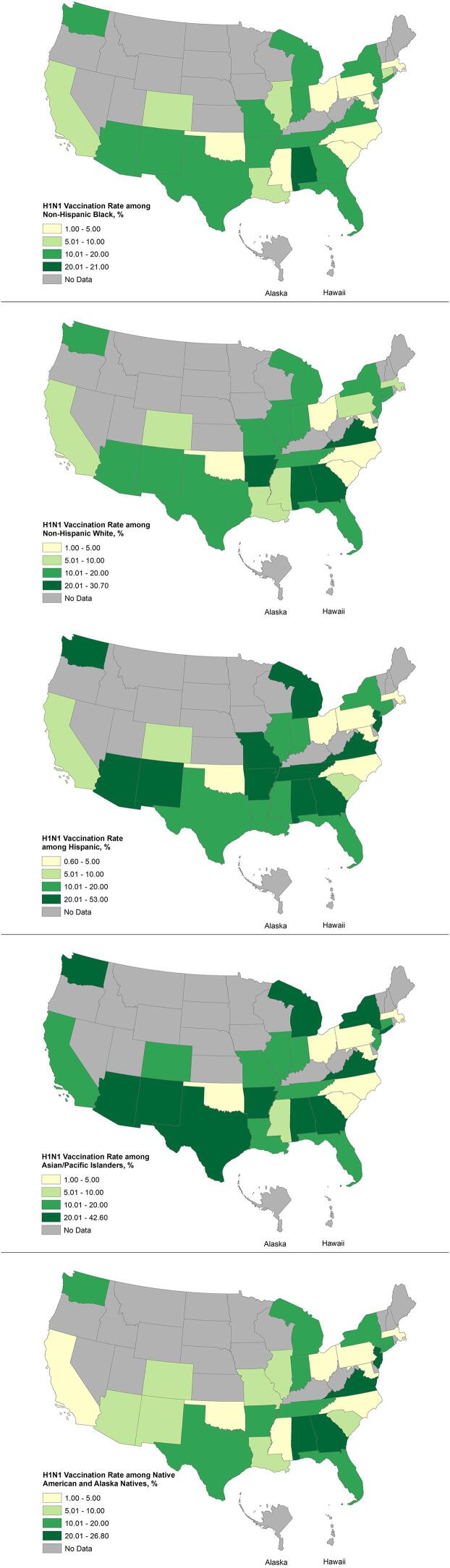
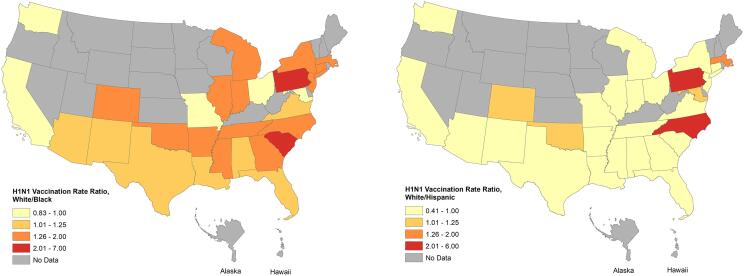
Fig. 2 shows state-level H1N1 vaccination rates among (a) NHB, (b) NHW, (c) Hispanic, (d) A/PI, (e) AI/AN Medicaid enrollees, 2009–2010. Fig. 3 compares the H1N1 rate ratios between NHB/NHW and Hispanic/NHW. The vaccine rate ratio of NHW to NHB was highest in PA where NHW were 7.0 times more likely to have H1N1 vaccination compared to NHB. Hispanic rates exceeded NHW rates in all but seven states, with considerably higher Hispanic rates in some states, like Alabama, where rates were more than double the NHW rates (53.0% Hispanic, 25.3% NHW).
Fig. 2.
Fig. 3.
4. Discussion
Although the H1N1 pandemic occurred more than a decade ago, it is our most recent experience of a global pandemic and subsequent vaccination rollout. Despite widespread availability in the US, uptake of the H1N1 vaccine was low, even among populations at highest risk for complications (Galarce et al., 2011, Final estimates FOR –102009, 2010). Racial and ethnic disparities in uptake of H1N1 vaccinations are particularly important to examine as vaccination disparities underscore lasting geographic patterns of inequitable distribution of vital health resources. Medicaid enrollees are an important group to illustrate these disparities in H1N1 vaccination, because they represent a disproportionately socioeconomically disadvantaged group often with high comorbidity burdens who have the same insurance coverage. We found large state-level variation in overall H1N1 vaccination rates and across racial/ethnic groups. In most states NHB and AI/AN enrollees had lower H1N1 vaccination rates than NHW, Hispanic and A/PI enrollees. Our finding that patients with higher medical comorbidity were more likely to be vaccinated is consistent with other studies (Harrison et al., 2018) and we hypothesize this is due to higher perceived risk of severe illness by patients and health care providers as well as more interactions with the health care system. Although COVID-19 vaccinations are not reported with information on underlying medical conditions, people with high-risk underlying conditions have been prioritized by federal and state COVID-19 vaccination plans.
Despite dramatic differences in case incidence, hospitalizations, mortality, and vaccine development and distribution processes between H1N1 and COVID-19, we observe some comparable trends in the two vaccination efforts. Most notably, high levels of geographic variation in vaccination rates generally and by race/ethnicity across both pandemics. Trends in COVID-19 vaccination rates across racial/ethnic groups show some improvements from the H1N1 vaccination disparities, especially for AI/AN people, who have the highest percent of people receiving the COVID-19 vaccine (fully vaccinated) by race/ethnicity in the US at 46.6%, followed by Asian (41.4%), Native Hawaiian or Pacific Islander (38.8%), NHW (37.3%), Hispanic/Latino (35%), and NHB (29.1%) (Percent of People Receiving COVID-19, 2021). COVID-19 vaccination trends indicate barriers to vaccination in Hispanic/Latino people that may not have existed for H1N1 and maintenance of barriers to vaccination for NHB people.
Geographic variation in vaccination rates may be driven by state-level Medicaid policies, including reimbursement rates and coverage parameters. A recent survey of Medicaid programs found that only 22 of 51 programs covered all adult vaccines recommended by ACIP and variations in reimbursement to health care professionals for administering vaccines (Granade et al., 2020). Because of the wide range in Medicaid vaccination rates across states and in different racial/ethnic groups, health departments are tailoring their COVID-19 vaccination rollout efforts to account for state-level demographics and designing outreach strategies for reaching communities of color. States with success in achieving high H1N1 vaccination rates for specific racial/ethnic groups may serve as models for their equitable responses. Historical barriers to vaccination affecting Medicaid enrollees include cost, transportation, and availability of health professionals who accept Medicaid. Unlike H1N1, COVID-19 vaccines are provided without cost to patients, eliminating this barrier. To overcome transportation challenges, many state and local health agencies are implementing mobile vaccination clinics and bringing vaccines directly to underserved communities (2021). Furthermore, the federal government has increased the Federal Medicaid Assistance Percentage (FMAP) to states so that COVID-19 vaccinations for Medicaid enrollees are fully covered, alleviating cost burdens to state governments (2021). Such policies could prevent the repetition of disparities seen in H1N1 vaccination rates.
Vaccine hesitancy has been identified as a compelling predictor of low H1N1 vaccine uptake across all racial/ethnic groups and may be a latent driver of disparities in H1N1 and COVID-19 vaccinations (Jarrett et al., 2015, Schmid et al., 2017). There have been substantial studies addressing vaccine hesitancy. However, inconsistent study of the components that comprise hesitancy has hindered determining its verifiable impact on racial and ethnic disparities in vaccine uptake. It is crucial to address vaccine hesitancy across all racial/ethnic groups to mitigate disparities observed in COVID-19 vaccinations. Although the number of people who express hesitancy to receive the COVID-19 vaccine has declined from 21% in December 2020 to 16% in March 2021, persistent differences in self-reported vaccination readiness across race/ethnicity, geography, and political identity remain (Societal Experts Action Network, 2020).
This study has several limitations. While the sample represents 80% of all Medicaid enrollees in 2009–2010, we are only able to analyze the claims data from 28 states and the District of Columbia. As the H1N1 vaccination required health care providers and practices to implement new coding practices for billing, there may be incomplete data due to slow implementation and diffusion of appropriate coding practices. Thus, the H1N1 vaccination rates reported here may be underreported if they were not captured on the Medicaid claim. It is also possible that Medicaid enrollees obtained the vaccination elsewhere or paid out of pocket for the vaccine, which would have led to the vaccination not being captured in a claim. Given the wide variation in vaccination rates across states, we hypothesize that inaccurate coding practices or unique state-level factors may have contributed to states with very low H1N1 vaccination rates across all groups, like Maryland and Ohio.
5. Conclusion
In conclusion, our analysis showed racial/ethnic disparities in receipt of the H1N1 vaccine in the Medicaid population. These disparities varied greatly between states. It is hoped that awareness of these disparities, and further examination of the reasons for these disparities, will inform a more equitable rollout and uptake of the COVID-19 vaccine.
CRediT authorship contribution statement
Chaohua Li: Methodology, Software, Validation, Formal analysis, Writing - original draft, Writing - review & editing, Visualization. Megan Douglas: Conceptualization, Methodology, Writing - original draft, Writing - review & editing, Supervision, Funding acquisition. Rabab Zahidi: Writing - original draft, Writing - review & editing. Robina Josiah Willock: Writing - original draft, Writing - review & editing. Lee Caplan: Writing - original draft, Writing - review & editing. Peter Baltrus: Writing - original draft, Writing - review & editing. Eric Gillis: Writing - original draft. Dominic Mack: Writing - original draft, Supervision, Funding acquisition. Anne Gaglioti: Writing - original draft, Writing - review & editing, Supervision, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This work was supported in part by a $40 million award from the US Department of Health and Human Services Office of Minority Health’s National Infrastructure for Mitigating the Impact of COVID-19 Within Racial and Ethnic Minority Communities through a cooperative agreement to create the National COVID-19 Resiliency Network (award 1CPIMP201187-01-00).
References
- Andrews C.M., Guerrero E.G., Wooten N.R., Lengnick-Hall R. The Medicaid expansion gap and racial and ethnic minorities with substance use disorders. Am. J. Public Health. 2015;105(S3):S452–S454. doi: 10.2105/AJPH.2015.302560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgartner J.C., Radley D.C., Shah A., Schneider E.C. How Prepared Are States to Vaccinate the Public Against COVID-19? Learning from Influenza and H1N1 Vaccination Programs. Commonwealth Fund. 2020 Retrieved March 03 2021 from 10.26099/y667-yr94. [Google Scholar]
- Mobile Vaccination Resources. CDC (2021). Retrieved April 23, 2021 from https://www.cdc.gov/vaccines/covid-19/planning/mobile.html.
- CMCS informational Bulletin - Medicaid. (n.d.). Retrieved September 7, 2021, from https://www.medicaid.gov/federal-policy-guidance/downloads/cib060321.pdf.
- Conis E. Measles and the Modern History of Vaccination. Public Health Rep. 2019;134(2):118–125. doi: 10.1177/0033354919826558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dooling K., McClung N., Chamberland M., Marin M., Wallace M., Bell B.P., Lee G.M., Talbot H.K., Romero J.R., Oliver S.E. The Advisory Committee on Immunization Practices' Interim Recommendation for Allocating Initial Supplies of COVID-19 Vaccine - United States, 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69(49):1857–1859. doi: 10.15585/mmwr.mm6949e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dooling K., Marin M., Wallace M., McClung N., Chamberland M., Lee G.M., Talbot H.K., Romero J.R., Bell B.P., Oliver S.E. The Advisory Committee on Immunization Practices' Updated Interim Recommendation for Allocation of COVID-19 Vaccine - United States, December 2020. MMWR Morb. Mortal. Wkly Rep. 2021;69(5152):1657–1660. doi: 10.15585/mmwr.mm695152e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elixhauser A., Steiner C., Harris D.R., Coffey R.M. Comorbidity measures for use with administrative data. Med. Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. PMID: 9431328. [DOI] [PubMed] [Google Scholar]
- Final estimates FOR 2009–10 seasonal influenza and Influenza A (H1N1) 2009 monovalent vaccination COVERAGE – United states, August 2009 through May, 2010. (2011, May 13). Retrieved September 07, 2021, from https://www.cdc.gov/flu/fluvaxview/coverage_0910estimates.htm.
- Flu vaccination coverage, United States, 2019–20 influenza season. (2020, October 01). Retrieved September 07, 2021, from https://www.cdc.gov/flu/fluvaxview/coverage-1920estimates.htm.
- Flu vaccinations. (2020, December 22). Retrieved September 07, 2021, from https://www.ncqa.org/hedis/measures/flu-vaccinations/.
- Galarce E.M., Minsky S., Viswanath K. Socioeconomicstatus, demographics, beliefs and A (H1N1) vaccine uptake in the United States. Vaccine. 2011;29(32):5284–5289. doi: 10.1016/j.vaccine.2011.05.014. [DOI] [PubMed] [Google Scholar]
- Granade C.J., McCord R.F., Bhatti A.A., Lindley M.C. State policies on access to vaccination services for low-income adults. JAMA network open. 2020;3(4):e203316. doi: 10.1001/jamanetworkopen.2020.3316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison S.M., Wei M.Y., Lamerato L.E., Petrie J.G., Toth Martin E. Multimorbidity is associated with uptake of influenza vaccination. Vaccine. 2018;36(25):3635–3640. doi: 10.1016/j.vaccine.2018.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchins S.S., Jiles R., Bernier R. Elimination of measles and of disparities in measles childhood vaccine coverage among racial and ethnic minority populations in the United States. J. Infect. Dis. 2004;189(Suppl 1):S146–152. doi: 10.1086/379651. [DOI] [PubMed] [Google Scholar]
- Jarrett C., Wilson R., O'Leary M., Eckersberger E., Larson H.J., Hesitancy S.W.G.o.V. Strategies for addressing vaccine hesitancy - A systematic review. Vaccine. 2015;33(34):4180–4190. doi: 10.1016/j.vaccine.2015.04.040. [DOI] [PubMed] [Google Scholar]
- Johnson K.A., Sardell A., Richards B. Federal immunization policy and funding: a history of responding to crises. Am. J. Prev. Med. 2000;19(3):99–112. doi: 10.1016/S0749-3797(00)00210-5. [DOI] [PubMed] [Google Scholar]
- Mahajan U.V., Larkins-Pettigrew M. Racial demographics and COVID-19 confirmed cases and deaths: a correlational analysis of 2886 US counties. J. Public Health. 2020;42(3):445–447. doi: 10.1093/pubmed/fdaa070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ndugga, N., Hill, L., Artiga, S., Parker, N. Latest Data on COVID-19 Vaccinations Race/Ethnicity. KFF. (2021, August 18). Retrieved September 05, 2021 from https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-race-ethnicity/.
- Societal Experts Action Network [SEAN] COVID-19 Survey Archive. (Dec 18, 2020). Retrieved Apr 9, 2021 from https://covid-19.parc.us.com/client/index.html#/.
- Painter E.M., Ussery E.N., Patel A., Hughes M.M., Zell E.R., Moulia D.L., Scharf L.G., Lynch M., Ritchey M.D., Toblin R.L., Murthy B.P., Harris L.Q., Wasley A., Rose D.A., Cohn A., Messonnier N.E. Demographic Characteristics of Persons Vaccinated During the First Month of the COVID-19 Vaccination Program - United States, December 14, 2020-January 14, 2021. MMWR Morb. Mortal. Wkly Rep. 2021;70(5):174–177. doi: 10.15585/mmwr.mm7005e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Percent of People Receiving COVID-19 Vaccine by Race/Ethnicity and Date Reported to CDC, United States (December 14, 2020 – September 4, 2021). Centers for Disease Control and Prevention. (n.d.). Retrieved September 07, 2021, from https://covid.cdc.gov/covid-data-tracker/#vaccination-demographics-trends.
- Schmid P., Rauber D., Betsch C., Lidolt G., Denker M.-L., Cowling B.J. Barriers of Influenza Vaccination Intention and Behavior - A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE. 2017;12(1):e0170550. doi: 10.1371/journal.pone.0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]