Abstract
Objective/Background:
Adolescence is a crucial time period in which individuals are at high risk for depression and anxiety. Associations between screen time and adolescent depression and anxiety have been inconclusive. We examined 1) the associations of screen time with adolescent depression and anxiety and 2) whether sleep duration mediates these relationships.
Methods:
This study utilized data from the 2018 U.S. National Survey of Children’s Health, a large cross-sectional population representative dataset with parent/caregiver responses. Multivariable logistic regression was used to estimate the associations between screen time and depression and anxiety in separate models. Path models were used to test the mediating role of sleep duration. Confounders, as sex, age, and sociodemographic variables were included in our adjusted models.
Results:
Data of 10,907 adolescents aged 13 to 17 were included in this study. The average screen time was 3.76 hours daily. Compared to no screen time, adolescents who used over 4 hours of screen time per day had higher odds of depression (OR=2.23, 95% CI:1.27 – 3.91) and anxiety (OR=1.85, 95% CI: 1.26 – 2.72). Sleep duration did not mediate the associations between screen time and depression and anxiety.
Conclusions
Further research is necessary to examine the associations of screen time content with depression and anxiety, as well as the effects of sleep quality in conjunction with sleep duration on the relationships of screen time and depression and anxiety.
Keywords: sleep duration, adolescents, anxiety, depression, screen time
1. Introduction
Adolescence is a vulnerable period in which developing and maintaining healthy social and emotional habits are important for mental health and well-being. This crucial period when there are tremendous changes places adolescents at high-risk for mental health conditions. It is estimated that half of all mental health conditions begin by 14 years of age but are often not detected or treated [1]. Depression is one of the leading causes of illness and disability as well as the most common mental health disorder among adolescents [2]. In the United States, a staggering 2.3 million or 9.4% of adolescents aged 12 to 17 years of age had at least one major depressive episode [3]. Depression can manifest during early adolescence [4], with the prevalence increasing during this period [5], and may recur during adulthood [6]. Furthermore, depression can lead to poorer outcomes including academic achievement, cognitive development, and social skills [7] as well as lead to high-risk behaviors, such as suicide [8], drug and alcohol abuse [9].
Depression and anxiety disorders in adolescence are highly comorbid, whether concurrently or sequentially, and may increase the risk of one another over time [10]. Some studies have identified that anxiety disorders are the most common mental health conditions among adolescents, with a lifetime prevalence rate estimated at 31.9% [10]. Additionally, anxiety disorders affect about 2–7% of the child and adolescent populations [10]. Anxiety disorders often begin during childhood [1] and may predict future recurrence, as well as other mental health issues including, depression, and substance use disorders [11–14]. Since both adolescent anxiety and depression are associated with poorer health outcomes and increased health care utilization [15, 16], it is critical to not only diagnose and manage these mental health conditions early but also identify predictors associated with these conditions.
Screen-based technology is rapidly evolving. While traditional screen time once consisted of television viewing and videogame playing, it now includes a plethora of content and through several types of devices, including cell phones, computers, and tablets. Based on a 2016 population-based study, it was estimated that U.S. adolescents aged 14–17 years spent approximately 4.59 hours on recreational screen time each day [17]. Another study in 2010 highlighted that adolescents spend over 7 hours on screen time [18]. While the American Academy of Pediatrics (AAP) does not have specific recommendations on time spent on electronic devices, they recommend that consistent limits are placed on screen time and media use [19]. Additionally, the AAP warns that screen time should not take the place of experiences and behaviors essential to physical and mental health, including adequate sleep [19].
Research on screen time as a risk factor for adolescent depression and anxiety has been inconclusive. While most studies have documented significant associations between screen time and anxiety and depression [15, 20–23], some have identified no associations [24, 25], negative associations, or even positive associations [26–28] with more screen time on overall mental health and well-being. Thus, it is imperative to clarify screen time as a predictor for adolescent mental health conditions since screen-based technologies are ever changing and excessive screen time can replace adolescent experiences and peer relationships, which have been reported beneficial for adolescent health [29].
The association between screen time with depression may be mediated through sleep duration [30]. However, the role of sleep as a mediator of the associations of screen time and anxiety are less clear. The AAP recommends that adolescents aged 13 to 18 years of age sleep for 8 to 10 hours each night [31], but sleep may be disrupted and substituted by increased use of screen time [32]. Forty-four percent of parents were concerned that their children had inadequate sleep on weekdays and 56% of parents reported that their adolescents (15 to 17 years of age) slept for less than 7 hours each night [33]. Research has shown that screen time can have negative impacts on sleep [34], while sleep has been reported to be associated with depression [35, 36] and anxiety [37]; therefore, sleep may play a mediating role between the associations of screen time and depression and anxiety. This study aims to 1) examine the associations of recreational screen time (time spent using a device that does not promote activity or have an educational component) with depression and anxiety in separate models and 2) test whether sleep mediates the associations between screen time with depression and anxiety. To our knowledge, our study is the first to explore the mediating role of sleep on screen time and two mental health outcomes, depression and the less studied anxiety, in separate models, utilizing a large population-representative sample.
2. Methods
2.1. Participants
The U.S. National Survey of Children’s Health (NSCH) is a large cross-sectional population representative dataset that is designed to evaluate the well-being and physical and emotional health of U.S. children from 0 to 17 years of age in all 50 states. The 2018 NSCH was conducted by the Centers for Disease Control’s National Center for Health Statistics. Households were contacted by random mailing to identify households with one or more children between 0 and 17. One child was randomly selected for the survey if households had more than one child. A parent or caregiver provided responses either online or on a paper. A total of 30,540 surveys were completed, with an overall weighted response rate of 43.1%. The public use dataset is available at the Data Resource Center for Child and Adolescent Health (DRC) website at http://www.childhealthdata.org.
2.2. Measures
2.2.1. Independent Variable
Screen time was measured by using the questions pertaining to time spent watching TV or videos and time spent using electronic devices. Screen time was obtained from the question “ON MOST WEEKDAYS, about how much time did this child spend in front of a TV, computer, cellphone or other electronic device watching programs, playing games, accessing the internet or using social media?” Responses were categorized as: less than “1 hour,” “1 hour,” “2 hours,” “3 hours,” and “4 or more hours.”
2.2.2. Dependent Variables
2.2.2.1. Depression
Depression was ascertained through the question “Has a doctor or health professional ever told you that your child has depression?” Estimates included “yes” and “no” responses while responses of “don’t know” or “refused” were excluded.
2.2.2.2. Anxiety
Anxiety was obtained similarly, through the question “Has a doctor or health professional ever told you that your child has anxiety problems? Estimates included “yes” and “no” responses while responses of “don’t know” or “refused” were excluded.
2.2.3. Mediating variable
Sleep duration was obtained from the question “During the past week, how many hours of sleep did this child get on most weeknights?” Responses were categorized as “less than 6 hours”, “6 hours,” “7 hours,” “8” hours,” “9 hours,” “10 hours,” and “11 hours.”
2.2.4. Confounders
The following confounders were included in our study: sex (male or female); age; federal poverty level (FPL; 0–99% FPL, 100–199% FPL, 200–399% FPL, 400% FPL or greater); insurance type (public insurance, private insurance, both private and public, and uninsured); parent education (less than high school, high school graduate, or more than high school); primary language spoken at home (English or other); race/ethnicity (Hispanic; White, Non-Hispanic; Black, Non-Hispanic; Asian, Non-Hispanic; and Other, Non-Hispanic); household generational status (1st, 2nd, 3rd generation, and other); and family structure (two biological or adoptive parents, two parents with one step-parent, single parent, grandparent and other family type).
Comorbid (medical and behavioral) conditions were included in our analyses. Conditions as brain injury, intellectual disability, cerebral palsy, autism, behavior problems, and ADD/ADHD were measured by the questions: 1) “Has a doctor or other health care provider EVER told you that this child has…” and 2) “If yes, does this child CURRENTLY have the condition? The responses were categorized as “yes” and “no.” Additionally, medications for emotions/behavior were included in our study. These medications were asked by the question: DURING THE PAST 12 MONTHS, has this child taken any medication because of difficulties with his or her emotions, concentration, or behavior?” The responses were categorized as “yes” and “no.”
2.3. Statistical Analyses
Data were analyzed using STATA v15.0 [38]. Differences in characteristics of the adolescents by screen time were assessed using the Chi-square test. The prevalence of depression was generated by comorbid conditions as well as emotional/behavioral medications.
Multivariable logistic regression to estimate the relationships between screen time (independent variable) and the mental health outcomes, depression and anxiety (dependent variables), from which estimated odds ratios (ORs) with 95% confidence intervals (CIs) are presented. We presented 3 models adjusting for confounders. The first model adjusted for age, and sex. The second model additionally adjusted for sociodemographic status, including poverty level, insurance type, parent education. Lastly, the third model additionally adjusted for primary language spoken at home, household generation, family structure, race/ethnicity, comorbid conditions, and emotional/behavioral medications.
The examination of the mediating role of sleep duration between screen time and the mental health outcomes, adjusting for all confounders, was conducted with path models. We followed a two-step procedure to test for mediation, which requires significant associations between 1) the independent variable (predictor) and mediating variable and 2) the mediating variable and dependent variable (outcome) adjusting for the independent variable (predictor) [39]. Estimations were calculated using the Paramed command in STATA v15.0 to measure mediating effects [40]. 2.7% of cases were removed through listwise deletion, and missing data was not replaced. The indirect effects of screen time and depression were determined using the bias-corrected bootstrap 95% CI in 1,000 samples. Figure 1 shows the complete model with sleep duration as the mediating variable, screen time as the predictor, and depression as the dependent variable. Figure 2 shows the complete model with sleep duration as the mediating variable, screen time as the predictor, and anxiety as the dependent variable.
Figure 1. Mediation analysis.
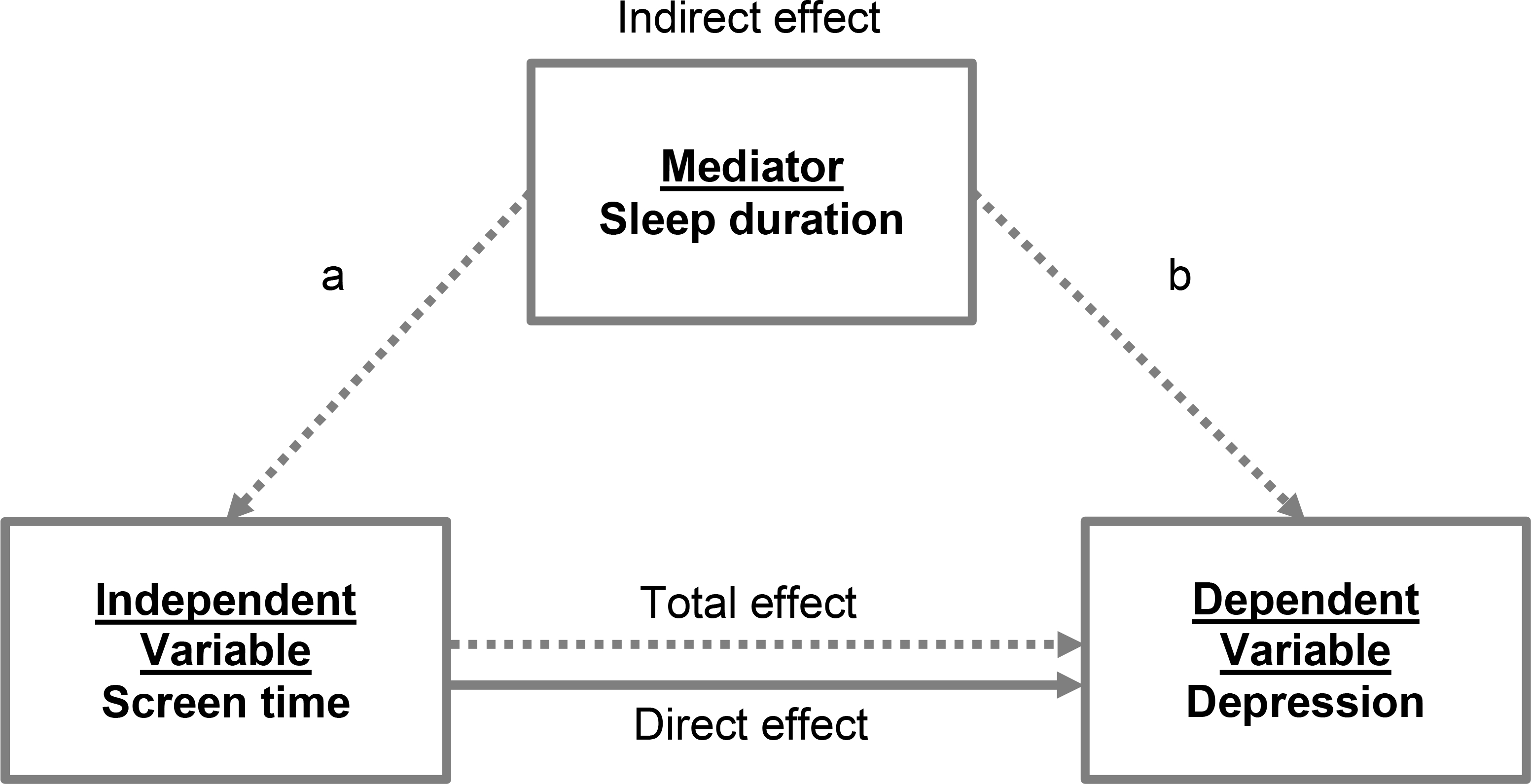
The figure depicts the hypothesized relationship between screen time, sleep, and depression. a represents the “a” path and b represents the “b” path. Analysis adjusted for confounders (not shown) including sex, age, poverty level, insurance type, parent education, language spoken at home, race/ethnicity, household generation, family structure, comorbid conditions, and emotional/behavioral medications.
Figure 2. Mediation analysis.
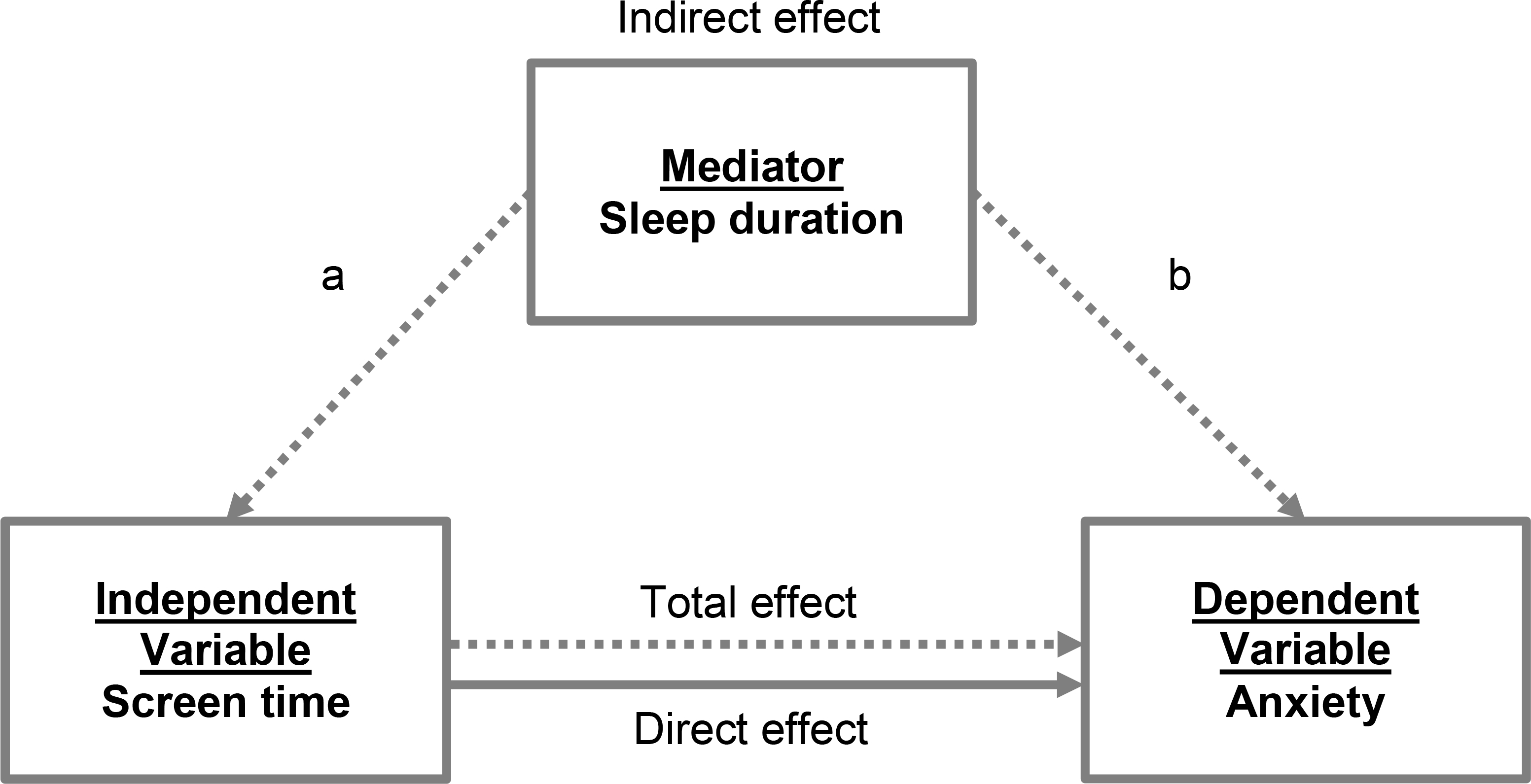
The figure depicts the hypothesized relationship between screen time, sleep, and anxiety. a represents the “a” path and b represents the “b” path. Analysis adjusted for confounders (not shown) including sex, age, poverty level, insurance type, parent education, language spoken at home, race/ethnicity, household generation, family structure, comorbid conditions, and emotional/behavioral medications.
3. Results
Data from 10,907 adolescents between the ages of 13 to 17 were included in this study. In this cohort of adolescents aged 13–17 years of age, the participants were primarily White, Non-Hispanic, English speaking, 3rd generation, from a two-parent household, had 400% FPl or greater, received public insurance, and had parents who had a high school education or higher. Descriptive characteristics of the adolescents in this study are described in Table 1. The Chi-square p-values indicate that all characteristics, except sex, were associated with screen time. Furthermore, the average screen time was 3.76 hours (standard deviation=1.12). Figure 3 shows the distribution of screen time based on age.
Table 1.
Adolescent characteristics by screen time (hours per weekday) from the 2018 National Survey of Children’s Health (NSCH) dataset
| Screen time (hours per weekday) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Less than 1 | 1 | 2 | 3 | 4 or more | X2 P-Value | ||||||
|
|
|||||||||||
| Characteristics | n | % | n | % | n | % | n | % | n | % | |
| Individual characteristics | |||||||||||
| Sex | |||||||||||
| Male | 176 | 3.08 | 506 | 8.86 | 1615 | 28.28 | 1435 | 25.13 | 1978 | 34.64 | 0.006 |
| Female | 186 | 3.66 | 544 | 10.7 | 1420 | 27.93 | 1254 | 24.67 | 1680 | 33.04 | |
| Race/Ethnicity | |||||||||||
| Hispanic | 50 | 4.13 | 123 | 10.15 | 320 | 26.40 | 291 | 24.01 | 428 | 35.31 | <0.001 |
| White, Non-Hispanic | 225 | 2.95 | 756 | 9.92 | 2218 | 29.11 | 1931 | 25.34 | 2490 | 32.68 | |
| Black, Non-Hispanic | 32 | 4.48 | 52 | 7.28 | 163 | 22.83 | 174 | 24.37 | 293 | 41.04 | |
| Asian, Non-Hispanic | 26 | 4.90 | 66 | 12.43 | 146 | 27.50 | 109 | 20.53 | 184 | 34.65 | |
| Other, Non-Hispanic | 29 | 4.04 | 53 | 7.39 | 188 | 26.22 | 184 | 25.66 | 263 | 36.68 | |
| Family characteristics | |||||||||||
| Primary language spoken at home | |||||||||||
| English | 314 | 3.11 | 969 | 9.61 | 2855 | 28.31 | 2526 | 25.04 | 3422 | 33.93 | <0.001 |
| Other | 44 | 6.70 | 77 | 11.72 | 166 | 25.27 | 148 | 22.53 | 222 | 33.79 | |
| Household generation | |||||||||||
| 1 st generation | 9 | 3.81 | 25 | 10.59 | 57 | 24.15 | 63 | 26.69 | 82 | 34.75 | <0.001 |
| 2nd generation | 68 | 4.64 | 162 | 11.06 | 405 | 27.65 | 332 | 22.66 | 498 | 33.99 | |
| 3rd generation | 252 | 2.98 | 810 | 9.59 | 2423 | 28.67 | 2132 | 25.23 | 2833 | 33.53 | |
| Other | 28 | 5.48 | 41 | 8.02 | 119 | 23.29 | 128 | 25.05 | 195 | 38.16 | |
| Family structure | |||||||||||
| Two Parents | 236 | 3.39 | 765 | 10.98 | 2067 | 29.68 | 1737 | 24.94 | 2160 | 31.01 | <0.001 |
| Two Parents (step-parent) | 23 | 2.43 | 67 | 7.08 | 242 | 25.58 | 205 | 21.67 | 409 | 43.23 | |
| Single Parent | 72 | 3.10 | 172 | 7.41 | 598 | 25.75 | 599 | 25.80 | 881 | 37.94 | |
| Grandparent | 14 | 4.46 | 21 | 6.69 | 74 | 23.57 | 83 | 26.43 | 122 | 38.85 | |
| Other | 5 | 4.10 | 12 | 9.84 | 24 | 19.67 | 34 | 27.87 | 47 | 38.52 | |
| Socioeconomic status | |||||||||||
| Poverty status (FPLa) | |||||||||||
| 0–99% FPL | 69 | 5.82 | 113 | 9.53 | 274 | 23.10 | 293 | 24.70 | 437 | 36.85 | <0.001 |
| 100–199% FPL | 63 | 3.70 | 151 | 8.87 | 466 | 27.36 | 406 | 23.84 | 617 | 36.23 | |
| 200–399% FPL | 109 | 3.38 | 282 | 8.73 | 895 | 27.72 | 816 | 25.27 | 1127 | 34.90 | |
| 400% FPL or greater | 121 | 2.59 | 504 | 10.78 | 1400 | 29.94 | 1174 | 25.11 | 1477 | 31.59 | |
| Insurance type | |||||||||||
| Private | 76 | 4.15 | 152 | 8.29 | 448 | 24.44 | 464 | 25.31 | 693 | 37.81 | <0.001 |
| Public | 218 | 2.78 | 787 | 10.03 | 2294 | 29.25 | 1978 | 25.22 | 2566 | 32.72 | |
| Both Private and Public | 17 | 3.96 | 29 | 6.76 | 123 | 28.67 | 99 | 23.08 | 161 | 37.53 | |
| Uninsured | 41 | 7.66 | 64 | 11.96 | 128 | 23.93 | 120 | 22.43 | 182 | 34.02 | |
| Parent education | |||||||||||
| Less than high school | 27 | 7.99 | 32 | 9.47 | 77 | 22.78 | 77 | 22.78 | 125 | 36.98 | <0.001 |
| High school | 53 | 3.31 | 130 | 8.12 | 402 | 25.11 | 413 | 25.80 | 603 | 37.66 | |
| High school or higher | 282 | 3.18 | 888 | 10.03 | 2556 | 28.87 | 2199 | 24.83 | 2930 | 33.09 | |
| Individual characteristics | |||||||||||
| Sex | |||||||||||
| Male | 176 | 48.62 | 506 | 48.19 | 1615 | 53.21 | 1435 | 53.37 | 1978 | 54.07 | 0.006 |
| Female | 186 | 51.38 | 544 | 51.81 | 1420 | 46.79 | 1254 | 46.63 | 1680 | 45.93 | |
| Race/Ethnicity | |||||||||||
| White, non-Hispanic | 225 | 62.15 | 756 | 72 | 2218 | 73.08 | 1931 | 71.81 | 2490 | 68.07 | <0.001 |
| Other | 137 | 37.85 | 294 | 28 | 817 | 26.92 | 758 | 28.19 | 1168 | 31.93 | |
| Family characteristics | |||||||||||
| Primary language spoken at home | |||||||||||
| English | 314 | 87.71 | 969 | 92.64 | 2855 | 94.51 | 2526 | 94.47 | 3422 | 93.91 | <0.001 |
| Other | 44 | 12.29 | 77 | 7.36 | 166 | 5.49 | 148 | 5.53 | 222 | 6.09 | |
| Household generation | |||||||||||
| 1 st generation | 9 | 2.52 | 25 | 2.41 | 57 | 1.9 | 63 | 2.37 | 82 | 2.27 | <0.001 |
| 2nd generation | 68 | 19.05 | 162 | 15.61 | 405 | 13.48 | 332 | 12.5 | 498 | 13.8 | |
| 3rd generation | 252 | 70.59 | 810 | 78.03 | 2423 | 80.66 | 2132 | 80.3 | 2833 | 78.52 | |
| Other | 28 | 7.84 | 41 | 3.95 | 119 | 3.96 | 128 | 4.82 | 195 | 5.4 | |
| Family structure | |||||||||||
| Two Parents | 236 | 67.43 | 765 | 73.77 | 2067 | 68.79 | 1737 | 65.35 | 2160 | 59.68 | <0.001 |
| Two Parents (step-parent) | 23 | 6.57 | 67 | 6.46 | 242 | 8.05 | 205 | 7.71 | 409 | 11.3 | |
| Single Parent | 72 | 20.57 | 172 | 16.59 | 598 | 19.9 | 599 | 22.54 | 881 | 24.34 | |
| Grandparent | 14 | 4 | 21 | 2.03 | 74 | 2.46 | 83 | 3.12 | 122 | 3.37 | |
| Other | 5 | 1.43 | 12 | 1.16 | 24 | 0.8 | 34 | 1.28 | 47 | 1.3 | |
| Socioeconomic status | |||||||||||
| Poverty status (FPLa) | |||||||||||
| 0–99% FPL | 69 | 19.06 | 113 | 10.76 | 274 | 9.03 | 293 | 10.9 | 437 | 11.95 | <0.001 |
| 100–199% FPL | 63 | 17.4 | 151 | 14.38 | 466 | 15.35 | 406 | 15.1 | 617 | 16.87 | |
| 200–399% FPL | 109 | 30.11 | 282 | 26.86 | 895 | 29.49 | 816 | 30.35 | 1127 | 30.81 | |
| 400% FPL or greater | 121 | 33.43 | 504 | 48 | 1400 | 46.13 | 1174 | 43.66 | 1477 | 40.38 | <0.001 |
| Insurance type | |||||||||||
| Private | 76 | 21.59 | 152 | 14.73 | 448 | 14.97 | 464 | 17.44 | 693 | 19.24 | |
| Public | 218 | 61.93 | 787 | 76.26 | 2294 | 76.65 | 1978 | 74.33 | 2566 | 71.24 | |
| Both Private and Public | 17 | 4.83 | 29 | 2.81 | 123 | 4.11 | 99 | 3.72 | 161 | 4.47 | |
| Uninsured | 41 | 11.65 | 64 | 6.2 | 128 | 4.28 | 120 | 4.51 | 182 | 5.05 | |
| Parent education | |||||||||||
| Less than high school | 27 | 7.46 | 32 | 3.05 | 77 | 2.54 | 77 | 2.86 | 125 | 3.42 | <0.001 |
| High school | 53 | 14.64 | 130 | 12.38 | 402 | 13.25 | 413 | 15.36 | 603 | 16.48 | |
| High school or higher | 282 | 77.9 | 888 | 84.57 | 2556 | 84.22 | 2199 | 81.78 | 2930 | 80.1 | |
Abbreviation: FPL, federal poverty level
Figure 3. Average screentime by age.
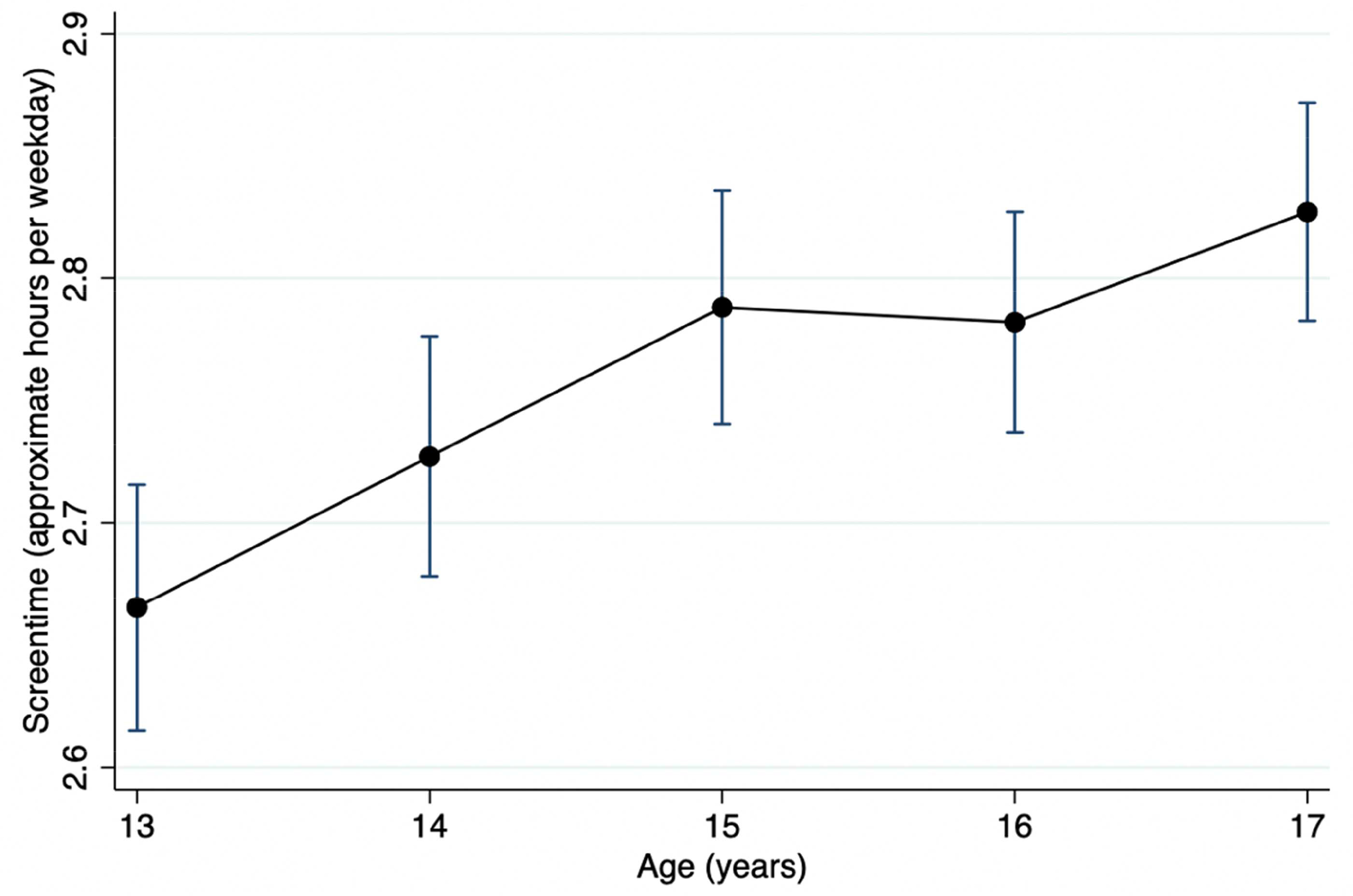
Hours per weekday spent on screens by age (13–17 years). Error bars are ±1 SE.
Tables 2 and 3 show the prevalence of depression and anxiety, respectively by comorbidities (medical and behavioral conditions) and emotional and behavioral medications. The prevalence of depression among this cohort of 13 to 17 year old adolescents was 8.64%. The prevalence of anxiety among this cohort was 14.3%. Additionally, while 8,902 participants (83.6%) did not have any comorbid conditions, 1,740 (16.4%) had one or more comorbid conditions. One thousand five hundred and sixty three participants (14.5%) were taking emotional/behavior medications, with over two thirds of the depressed participants (68.4%) taking these medications and over half of the anxious participants (56.2%) taking these medications.
Table 2.
Prevalence of parent-reported depression among U.S. adolescents aged 13–17 years by medical conditions/behavioral conditions, and medications from the 2018 National Survey of Children’s Health (NSCH) dataset
| No depression (n=9918, 91.36%) |
Depression (n=938, 8.64%) |
||||
|---|---|---|---|---|---|
| Characteristic | n | % | n | % | X2 p-value |
| Intellectual disability | |||||
| No | 9791 | 91.50 | 909 | 8.50 | <0.001 |
| Yes | 109 | 78.99 | 29 | 21.01 | |
| Brain injury | |||||
| No | 9807 | 91.43 | 919 | 8.57 | 0.002 |
| Yes | 75 | 82.42 | 16 | 17.58 | |
| Cerebral palsy | |||||
| No | 9855 | 91.40 | 927 | 8.60 | 0.050 |
| Yes | 27 | 81.82 | 6 | 18.18 | |
| Autism | |||||
| No | 9622 | 91.94 | 843 | 8.06 | <0.001 |
| Yes | 265 | 74.23 | 92 | 25.77 | |
| Behavioral problems | |||||
| No | 9430 | 93.26 | 681 | 6.74 | <0.001 |
| Yes | 456 | 64.14 | 255 | 35.86 | |
| ADD/ADHD | |||||
| No | 8774 | 93.76 | 584 | 6.24 | <0.001 |
| Yes | 1016 | 74.65 | 345 | 25.35 | |
| Medications a | |||||
| No | 8863 | 96.78 | 295 | 3.22 | <0.001 |
| Yes | 919 | 58.95 | 640 | 41.05 | |
Medications taken for emotions, concentration, and/or behavior
Table 3.
Prevalence of parent-reported anxiety among U.S. adolescents aged 13–17 years by medical conditions/behavioral conditions, and medications from the 2018 National Survey of Children’s Health (NSCH) dataset
| No anxiety (n=9268, 85.30%) |
Anxiety (n=1597, 14.70%) |
||||
|---|---|---|---|---|---|
| Characteristic | n | % | n | % | X 2 p-value |
| Intellectual disability | |||||
| No | 9176 | 85.70 | 1531 | 14.30 | <0.001 |
| Yes | 75 | 54.35 | 63 | 45.65 | |
| Brain injury | |||||
| No | 9181 | 85.52 | 1555 | 14.48 | <0.001 |
| Yes | 55 | 60.44 | 36 | 39.56 | |
| Cerebral palsy | |||||
| No | 9216 | 85.39 | 1577 | 14.61 | <0.001 |
| Yes | 20 | 60.61 | 13 | 39.39 | |
| Autism | |||||
| No | 9081 | 86.69 | 1394 | 13.31 | <0.001 |
| Yes | 164 | 45.94 | 193 | 54.06 | |
| Behavioral problems | |||||
| No | 8892 | 87.87 | 1227 | 12.13 | <0.001 |
| Yes | 346 | 48.66 | 365 | 51.34 | |
| ADD/ADHD | |||||
| No | 8342 | 89.03 | 1028 | 10.97 | <0.001 |
| Yes | 812 | 59.75 | 547 | 40.25 | |
| Medications a | |||||
| No | 8471 | 92.41 | 696 | 7.59 | <0.001 |
| Yes | 666 | 42.75 | 892 | 57.25 | |
Medications taken for emotions, concentration, and/or behavior
Table 4 shows the associations between screen time and depression and anxiety. In separate models, adolescents who used screen time for 4 or more hours were associated with an increased odds of depression and anxiety. In the fully adjusted model, adolescents using 4 or more hours of screen time, compared to less than 1 hour of screen time, had a 2.23 times odds (95% CI: 1.27 to 3.91) of having depression and 1.85 times odds (95% CI: 1.26 to 2.72) of having anxiety. The associations were attenuated by the addition of more covariates as seen in Models 2 and 3.
Table 4.
Adjusted associations of screen time (hours per weekday) with depression and anxiety using multivariable logistic regression from the 2018 National Survey of Children’s Health (NSCH) dataset
| Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|
| Mental health outcome | Screen time | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Depression | |||||||
| Less than 1 hour | 1 | 1 | 1 | ||||
| 1 hour | 0.59 | (0.33 – 1.04) | 0.62 | (0.34 – 1.12) | 0.66 | (0.34 – 1.28) | |
| 2 hours | 1.24 | (0.76 – 2.02) | 1.22 | (0.34 – 1.12) | 1.26 | (0.71 – 2.25) | |
| 3 hours | 1.56 | (0.96 – 2.53) | 1.55 | (0.94 – 2.57) | 1.48 | (0.83 – 2.63) | |
| 4 or more hours | 2.77** | (1.72 – 4.44) | 2.62** | (1.60 – 4.29) | 2.23* | (1.27 – 3.91) | |
| Anxiety | |||||||
| Less than 1 hour | 1 | 1 | 1 | ||||
| 1 hour | 0.67* | (0.45 – 1.00) | 0.66* | (0.44 – 0.99) | 0.69 | (0.44 – 1.07) | |
| 2 hours | 1.11 | (0.78 – 1.57) | 1.08 | (0.76 – 1.53) | 1.14 | (0.77 – 1.69) | |
| 3 hours | 1.36 | (0.96 – 1.92) | 1.32 | (0.93 – 1.87) | 1.34 | (0.90 – 1.98) | |
| 4 or more hours | 2.04** | (1.45 – 2.86) | 1.97** | (1.40 – 2.78) | 1.85* | (1.26 – 2.72) | |
p<0.05
p<0.001
Abbreviation: OR, odds ratio; CI, confidence interval
Adjusted for sex and age
Additionally adjusted for poverty level, insurance type, and parent education
Additionally adjusted for language spoken at home, race/ethnicity, household generation, family structure, comorbid conditions and emotional/behavior medications
For our depression outcome, screen time was significantly associated with sleep duration (path a; β=−0.022, 95% CI: −0.040 to −0.003) using the ordinary least squares regression model. Sleep duration was significantly associated with depression (path b; OR=0.828, 95% CI: 0.780 to 0.879) using a logistic regression model. Table 5 shows the total, direct, and indirect effects of screen time and depression using mediation analysis. The total effect from screen time to depression was statistically significant (OR=1.347, p<0.001) while the direct path from screen time to depression was slightly diminished yet remained significant (OR=1.345, p=0.374) and the indirect path from screen time to depression was not significant (OR=1.001, p=0.374). Therefore, sleep duration did not play a mediating role in the relationships of screen time and depression.
Table 5.
Mediation analysis of the relationship between screen time and depression by sleep durationa
| OR | SE | 95% CI | |
|---|---|---|---|
| Screen time --> Depression total | 1.347** | <0.001 | (1.243 – 1.460) |
| Screen time --> Depression direct | 1.345** | <0.001 | (0.998 – 1.004) |
| Screen time --> Depression indirect | 1.001 | 0.374 | (1.241 – 1.458) |
| Proportion of mediation | 0.744 |
p<0.001
Abbreviation: OR, odds ratio; SE, standard error; CI, confidence interval
Adjusted for sex, age, poverty level, insurance type, parent education, language spoken at home, race/ethnicity, household generation, family structure, and comorbid conditions, and emotional/behavioral medications.
Similarly, for our anxiety outcome, screen time was significantly associated with sleep duration (path a; β=−0.022, 95% CI: −0.040 to −0.003) using the ordinary least squares regression model. Sleep duration was significantly associated with depression (path b; OR=0.914, 95% CI: 0.871 to 0.958) using a logistic regression model. Table 6 shows the total, direct, and indirect effects of screen time and anxiety using mediation analysis. The total effect from screen time to anxiety was statistically significant (OR=1.230, p<0.001) as well, and the direct path from screen time to anxiety was slightly diminished and significant (OR=1.229, p<0.001) and the indirect path from screen time depression was not significant (OR=1.001, p=0.386). Thus, sleep duration did not play a mediating role in the relationships of screen time and anxiety.
Table 6.
Mediation analysis of the relationship between screen time and anxiety by sleep durationa
| OR | SE | 95% CI | |
|---|---|---|---|
| Screen time --> Anxiety total | 1.230** | 0.314 | (1.156 – 1.307) |
| Screen time --> Anxiety direct | 1.229** | 0.009 | (1.555 – 1.308) |
| Screen time --> Anxiety indirect | 1.001 | 0.314 | (0.998 – 1.001) |
| Proportion of mediation | 0.813 |
p<0.001
Abbreviation: OR, odds ratio; SE, standard error; CI, confidence interval
Adjusted for sex, age, poverty level, insurance type, parent education, language spoken at home, race/ethnicity, household generation, family structure, cormorbid conditions, and emotional/behavior medications.
4. Discussion
In this large population-representative U.S. cohort, adolescents averaged over 3 hours of screen time per weekday, 8.6% of adolescents had depression, and 14.3% of adolescents had anxiety. Only the associations of screen time of 4 or more hours per day with depression and anxiety were statistically significant. There was a negative association between screen time and sleep, such that more screen time was associated with less sleep. Furthermore, more sleep was associated with a lower odds having depression and anxiety. However, sleep duration did not play a mediating role in the associations between screen time and our mental health outcomes, depression and anxiety.
There are several psychosocial reasons for our findings. With limited exposure or exposure in moderation, adolescents can possibly benefit from devices and screen time. With controlled or limited exposure, adolescents are perhaps spending their time wisely on viewing more positive, protective content. However, as screen time increases, adolescents may begin to displace healthy habits, such as sleep, reading, physical activity, and physical social interactions, with screen time. Adolescents who use more screen time may also have a tendency to self-isolate [41], which may result in a higher risk for depression and anxiety. There is also the possibility that this increased risk for depression and anxiety may lead to more screen time, as evidenced by Houghton et al.’s (2018) study on the reciprocal relationships between depressive symptoms and screen use [42]. Our findings that screen time in moderation is protective in some models is consistent with findings from a few studies [26, 27], whereas findings that increased screen time predict depression and anxiety are more strongly supported [43]. Furthermore, increased screen time may expose adolescents to more negative content, such as cyberbullying [44], that can affect their mental health. Nonetheless, one recent study by Orben and Przybylski (2019) found that although a relationship exists between screen use and psychological well-being, the association is small, explaining no more than 0.4% of the variation of well-being [45]. As such, our findings suggest that the AAP consider providing more guidance on screen time as parents and guardians may not always be able to monitor their adolescents’ exposure to negative, harmful content. Our findings also suggest that parents and guardians should be educated about the risk for depression when their adolescents spend more than 4 hours a day on their screens.
Additionally, our findings support the AAP recommendations that adolescents sleep more than 8 or more hours nightly [31]. Consistent with previous studies, relationships exist among screen time and sleep duration [46], and sleep duration with depression and anxiety [47, 48]. While our study did not examine at what times during the day the adolescents were engaging in screen time, this factor may play an important role in sleep duration. Previous studies have reported negative effects of adolescents using screen time 30 minutes to 2 hours before bedtime, which can contribute to delayed bedtimes [25] and both reduced and worse sleep [32]. Additionally, screen time on social media and internet surfing had the strongest associations with poor sleep [49]. Therefore, further investigation into screen time content, screen time duration in relation to bedtime, and poor sleep is warranted. Furthermore, since sleep deprivation can have a reciprocal relationship with adolescent depression and its related symptoms [48], which our study was unable to assess for due to its cross-sectional design, considerations for future longitudinal studies to clarify these relationships are necessary. However, unlike previous studies on adolescent depression [41] and psychological symptoms [32], sleep duration as a mediating role between screen time with depression and anxiety was not supported by our study findings. As such, there may be other mediating variables associated with screen time and depression and anxiety as sleep partially mediated the associations of screen time and depression in these previous studies [25, 30, 50] Further, the relationships between screen time and depression and anxiety are complex, as these previous studies included sleep quality and its interactions with sleep duration and sleep onset difficulties in their models.”
While this study is population-representative with a large sample size and caregiver-reported diagnoses of both adolescent anxiety and depression, as opposed to the use of screening tools, there are some limitations. First, all variables in this study are caregiver-reported, which can introduce bias. As opposed to adolescent self-report, caregivers may underestimate the number of hours spent on screen time as well as misreport of sleep duration. Second, the questions pertaining to depression and anxiety were asked in such a way that medical diagnoses were implied. However it is unclear how the children were diagnosed since parents were asked whether they were ever told by a healthcare provider their child has depression. Furthermore, caregivers may under-report symptoms and behaviors to health care providers due to the stigma on mental illness,44 resulting in misdiagnosis or lack of diagnosis, leading to under-reporting on the NSCH. Third, screen time was limited to one question and did not differentiate among the devices, while media content was not elicited in the 2018 NSCH survey as in other studies [32]. Nonetheless, the relationship between screen time and mental health outcomes is crucial to examine as a prerequisite for further investigation of content. Fourth, screen time and sleep were limited to weekdays, so weekend activity is unknown. However, investigating weekday screen time in previous studies have shown similar results [17, 28], and increased weekday screen time can replace weekday sleep, disrupt sleep patterns, educational activities, and physically activity, all of which are associated with mental health and well-being. Fifth, sleep quality was not assessed as previous studies have shown that the sleep quality may both affect depression and anxiety [30, 37, 51]. Previous research has also shown that screen time has a negative impact on sleep duration, which could also impact depression and anxiety in adolescents. Lastly, this was a cross-sectional study, thus does not provide a temporal relationship between the variables. However, longitudinal studies have consistently shown that screen time and sleep leads to poorer mental health outcomes [30, 52] with few studies showing bidirectional relationships between screen time, sleep, and depression and anxiety [53]. Nevertheless, our findings have clinical implications. Health care providers should consider educating adolescents that increased screen time and less than the recommended 8 hours of sleep on weekdays are associated with depression and anxiety risk.
5. Conclusions
In summary, this study highlights that increased screen time and less sleep may contribute to poorer adolescent mental health outcomes. Since this is a period in which adolescents are at risk for depression and anxiety due to their development and social surroundings, it is critical that researchers continue to examine the relationships between screen-based technologies and content with sleep duration and quality as they relate to depression and anxiety. Sequentially, healthcare providers should consider educating adolescents and their families that excessive screen time can be detrimental to sleep and mental health.
Supplementary Material
Highlights.
There is conflicting evidence on the associations of screen time and depression and limited studies examining the relationships between screen time and anxiety in adolescents.
Our study found that screen time greater than 4 hours per weekday is associated with adolescent depression and anxiety.
Our study found that while sleep duration is associated with both our independent (screen time) and dependent (depression and anxiety) variables, sleep duration does not play a mediating role in these relationships.
Funding:
This work was funded by the National Institute of Nursing Research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: None declared.
References
- [1].Kessler RC, Angermeyer M, Anthony JC, Graaf DE, Demyttenaere K, Gasquet I, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6:168–76. [PMC free article] [PubMed] [Google Scholar]
- [2].Adolescent mental health. World Health Organization; 2019. [Google Scholar]
- [3].National Institute of Mental Health. Major Depression. 2019.
- [4].Witvliet M, Brendgen M, van Lier PA, Koot HM, Vitaro F. Early adolescent depressive symptoms: prediction from clique isolation, loneliness, and perceived social acceptance. J Abnorm Child Psychol. 2010;38:1045–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Whittle S, Lichter R, Dennison M, Vijayakumar N, Schwartz O, Byrne ML, et al. Structural brain development and depression onset during adolescence: a prospective longitudinal study. Am J Psychiatry. 2014;171:564–71. [DOI] [PubMed] [Google Scholar]
- [6].Rohde P, Lewinsohn PM, Klein DN, Seeley JR, Gau JM. Key Characteristics of Major Depressive Disorder Occurring in Childhood, Adolescence, Emerging Adulthood, Adulthood. Clin Psychol Sci. 2013;1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Bickham DS, Hswen Y, Rich M. Media use and depression: exposure, household rules, and symptoms among young adolescents in the USA. Int J Public Health. 2015;60:147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR. Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry. 2015;54:37–44 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Asarnow JR, Zeledon LR, D'Amico E, LaBorde A, Anderson M, Avina C, et al. Depression and Health Risk Behaviors: Towards Optimizing Primary Care Service Strategies for Addressing Risk. Prim Health Care. 2014;4:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bushnell GA, Gaynes BN, Compton SN, Dusetzina SB, Brookhart MA, Sturmer T. Incidence of mental health hospitalizations, treated self-harm, and emergency room visits following new anxiety disorder diagnoses in privately insured U.S. children. Depress Anxiety. 2019;36:179–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Birmaher B, Brent D, AWGoQ Issues, Bernet W, Bukstein O, Walter H, et al. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry. 2007;46:1503–26. [DOI] [PubMed] [Google Scholar]
- [12].Connolly SD, Bernstein GA, Work Group on Quality I. Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2007;46:267–83. [DOI] [PubMed] [Google Scholar]
- [13].Dahne J, Banducci AN, Kurdziel G, MacPherson L. Early adolescent symptoms of social phobia prospectively predict alcohol use. J Stud Alcohol Drugs. 2014;75:929–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Zimmermann M, Chong AK, Vechiu C, Papa A. Modifiable risk and protective factors for anxiety disorders among adults: A systematic review. Psychiatry Res. 2020;285:112705. [DOI] [PubMed] [Google Scholar]
- [15].Keenan-Miller D, Hammen CL, Brennan PA. Health outcomes related to early adolescent depression. J Adolesc Health. 2007;41:256–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Dark T, Flynn HA, Rust G, Kinsell H, Harman JS. Epidemiology of Emergency Department Visits for Anxiety in the United States: 2009–2011. Psychiatr Serv. 2017;68:238–44. [DOI] [PubMed] [Google Scholar]
- [17].Twenge JM, Campbell WK. Associations between screen time and lower psychological well-being among children and adolescents: Evidence from a population-based study. Prev Med Rep. 2018;12:271–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Rideout V, Foher U, Roberts D. Generation M2: Media in the Lives of 8–18-Year-Olds: A Kaiser Family Foundation Study. Menlo Park, CA2010. [Google Scholar]
- [19].AAP Council on Communications and Media. Virtual Violence. Pediatrics. 2016;138(1):e20161298. [DOI] [PubMed] [Google Scholar]; Pediatrics. 2016;138.27544347 [Google Scholar]
- [20].Maras D, Flament MF, Murray M, Buchholz A, Henderson KA, Obeid N, et al. Screen time is associated with depression and anxiety in Canadian youth. Prev Med. 2015;73:133–8. [DOI] [PubMed] [Google Scholar]
- [21].Goldfield GS, Murray M, Maras D, Wilson AL, Phillips P, Kenny GP, et al. Screen time is associated with depressive symptomatology among obese adolescents: a HEARTY study. Eur J Pediatr. 2016;175:909–19. [DOI] [PubMed] [Google Scholar]
- [22].Kremer P, Elshaug C, Leslie E, Toumbourou JW, Patton GC, Williams J. Physical activity, leisure-time screen use and depression among children and young adolescents. J Sci Med Sport. 2014;17:183–7. [DOI] [PubMed] [Google Scholar]
- [23].Khouja JN, Munafo MR, Tilling K, Wiles NJ, Joinson C, Etchells PJ, et al. Is screen time associated with anxiety or depression in young people? Results from a UK birth cohort. BMC Public Health. 2019;19:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Ohannessian C. Media use and adolescent psychological adjustment: An examination of gender differences. J Child Fam Stud. 2009;18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Orben A, Przybylski AK. Screens, Teens, and Psychological Well-Being: Evidence From Three Time-Use-Diary Studies. Psychol Sci. 2019;30:682–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Granic I, Lobel A, Engels RC. The benefits of playing video games. Am Psychol. 2014;69:66–78. [DOI] [PubMed] [Google Scholar]
- [27].Odgers C. Smartphones are bad for some teens, not all. Nature. 2018;554:432–4. [DOI] [PubMed] [Google Scholar]
- [28].Przybylski AK, Weinstein N. A Large-Scale Test of the Goldilocks Hypothesis. Psychol Sci. 2017;28:204–15. [DOI] [PubMed] [Google Scholar]
- [29].Roach A. Supportive Peer Relationships and Mental Health in Adolescence: An Integrative Review. Issues Ment Health Nurs. 2018;39:723–37. [DOI] [PubMed] [Google Scholar]
- [30].Li X, Buxton OM, Lee S, Chang AM, Berger LM, Hale L. Sleep mediates the association between adolescent screen time and depressive symptoms. Sleep Med. 2019;57:51–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Jenco M. AAP endorses new recommendations on sleep times. 2016.
- [32].Hisler G, Twenge JM, Krizan Z. Associations between screen time and short sleep duration among adolescents varies by media type: evidence from a cohort study. Sleep Med 2020;66:92–102. [DOI] [PubMed] [Google Scholar]
- [33].Buxton OM, Chang AM, Spilsbury JC, Bos T, Emsellem H, Knutson KL. Sleep in the modern family: protective family routines for child and adolescent sleep. Sleep Health. 2015;1:15–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. 2015;21:50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Lovato N, Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med Rev. 2014;18:521–9. [DOI] [PubMed] [Google Scholar]
- [36].Berger AT, Wahlstrom KL, Widome R. Relationships between sleep duration and adolescent depression: a conceptual replication. Sleep Health. 2019;5:175–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].McMakin DL, Alfano CA. Sleep and anxiety in late childhood and early adolescence. Curr Opin Psychiatry. 2015;28:483–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- [39].Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. [DOI] [PubMed] [Google Scholar]
- [40].Hayes A. Introduction to Mediation, Moderation, and Conditional Process Analysis. A Regression-Based Approach. 2nd ed ed. New York: Guilford; 2017. [Google Scholar]
- [41].Bohnert AM, Garber J. Prospective relations between organized activity participation and psychopathology during adolescence. J Abnorm Child Psychol. 2007;35:1021–33. [DOI] [PubMed] [Google Scholar]
- [42].Houghton S, Lawrence D, Hunter SC, Rosenberg M, Zadow C, Wood L, et al. Reciprocal Relationships between Trajectories of Depressive Symptoms and Screen Media Use during Adolescence. J Youth Adolesc. 2018;47:2453–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Hoare E, Milton K, Foster C, Allender S. The associations between sedentary behaviour and mental health among adolescents: a systematic review. Int J Behav Nutr Phys Act. 2016;13:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Bottino SM, Bottino CM, Regina CG, Correia AV, Ribeiro WS. Cyberbullying and adolescent mental health: systematic review. Cad Saude Publica. 2015;31:463–75. [DOI] [PubMed] [Google Scholar]
- [45].Orben A, Przybylski AK. The association between adolescent well-being and digital technology use. Nat Hum Behav. 2019;3:173–82. [DOI] [PubMed] [Google Scholar]
- [46].Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Med. 2010;11:735–42. [DOI] [PubMed] [Google Scholar]
- [47].Ojio Y, Nishida A, Shimodera S, Togo F, Sasaki T. Sleep Duration Associated with the Lowest Risk of Depression/Anxiety in Adolescents. Sleep. 2016;39:1555–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Roberts RE, Duong HT. The prospective association between sleep deprivation and depression among adolescents. Sleep. 2014;37:239–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Twenge JM, Hisler GC, Krizan Z. Associations between screen time and sleep duration are primarily driven by portable electronic devices: evidence from a population-based study of U.S. children ages 0–17. Sleep Med. 2019;56:211–8. [DOI] [PubMed] [Google Scholar]
- [50].Vandendriessche A, Ghekiere A, Van Cauwenberg J, De Clercq B, Dhondt K, DeSmet A, et al. Does Sleep Mediate the Association between School Pressure, Physical Activity, Screen Time, and Psychological Symptoms in Early Adolescents? A 12-Country Study. Int J Environ Res Public Health. 2019;16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Lofthouse N, Gilchrist R, Splaingard M. Mood-related sleep problems in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2009;18:893–916. [DOI] [PubMed] [Google Scholar]
- [52].Babic M, Smith J, Philip J, Morgan P, Eather N, Plotnikoff R, et al. Longitudinal associations between changes in screen-time and mental health outcomes in adolescents. Mental Health and Physical Activity. 2017;12. [Google Scholar]
- [53].Clarke G, Harvey AG. The complex role of sleep in adolescent depression. Child Adolesc Psychiatr Clin N Am. 2012;21:385–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


