Abstract
It is unclear to what extent the COVID-19 pandemic has influenced the use of remote monitoring (RM) of cardiac implantable electronic devices (CIEDs). The present physician-based European Heart Rhythm Association (EHRA) survey aimed to assess the influence of the COVID-19 pandemic on RM of CIEDs among EHRA members and how it changed the current practice. The survey comprised 27 questions focusing on RM use before and during the pandemic. Questions focused on the impact of COVID-19 on the frequency of in-office visits, data filtering, reasons for initiating in-person visits, underutilization of RM during COVID-19, and RM reimbursement. A total of 160 participants from 28 countries completed the survey. Compared to the pre-pandemic period, there was a significant increase in the use of RM in patients with pacemakers (PMs) and implantable loop recorders (ILRs) during the COVID-19 pandemic (PM 24.2 vs. 39.9%, P = 0.002; ILRs 61.5 vs. 73.5%, P = 0.028), while there was a trend towards higher utilization of RM for cardiac resynchronization therapy-pacemaker (CRT-P) devices during the pandemic (44.5 vs. 55%, P = 0.063). The use of RM with implantable cardioverter-defibrillators (ICDs) and CRT-defibrillator (CRT-D) did not significantly change during the pandemic (ICD 65.2 vs. 69.6%, P = 0.408; CRT-D 65.2 vs. 68.8%, P = 0.513). The frequency of in-office visits was significantly lower during the pandemic (P < 0.001). Nearly two-thirds of participants (57 out of 87 respondents), established new RM connections for CIEDs implanted before the pandemic with 33.3% (n = 29) delivering RM transmitters to the patient’s home address, and the remaining 32.1% (n = 28) activating RM connections during an in-office visit. The results of this survey suggest that the crisis caused by COVID-19 has led to a significant increase in the use of RM of CIEDs.
Keywords: Remote monitoring, Cardiac implantable electronic devices, COVID-19, EHRA survey
Introduction
Remote monitoring (RM) of cardiac implantable electronic devices (CIEDs) was initially introduced for complementary evaluation of device function but now represents the standard of care and is recommended by major cardiology societies worldwide.1,2 Remote monitoring of CIEDs reduces the number of scheduled in-office visits and leads to early detection of events, such as atrial fibrillation and ventricular arrhythmias, inappropriate shocks, lead failure, premature battery depletion, loss of biventricular capture, and mortality.3,4 However, despite the international guidelines’ recommendations based on these numerous benefits, its use in the routine clinical setting remains modest.1,2,5
Although the COVID-19 pandemic caught us unprepared, it facilitated and accelerated the use of telemedicine and digital solutions.6 Remote monitoring and teleconsultations, new digital tools, mobile health apps were available to replace traditional clinician-patient, face-to-face interaction, and enabled the follow-up and treatment of patients during the lockdown.7 Although it is clear that the COVID-19 pandemic has expedited the utilization of digital tools, it remains unclear to what extent the pandemic has influenced the use of RM of CIEDs.
The aim of this physician-based survey, disseminated by the Scientific Initiatives Committee of the European Heart Rhythm Association (EHRA), was to evaluate and describe the impact of the COVID-19 pandemic on the use of RM of CIEDs among EHRA members.
Methods
An online survey was prepared and disseminated by the EHRA Scientific Initiatives Committee to the EHRA Scientific Research Network members, national electrophysiology working groups, and social media platforms (Twitter, LinkedIn and Facebook), with the help of the EHRA e-Communication Committee. The survey was conducted between 17 March 2021 and 30 April 2021. It was designed after reviewing the literature and using expert opinion to examine the changes in RM practice induced by COVID-19 pandemic, and comprised a total of 28 questions distributed in four blocks focusing on the impact of COVID-19 on the frequency of in-office visits, data filtering, reasons for initiating in-person visits, underutilization of the RM during the pandemic and RM reimbursement (Supplementary material online, Table S1).
Participants who disagreed with GDPR compliance were excluded from the analysis.
Statistical analysis
Mean and standard deviation were used to present continuous variables, while categorical variables are expressed as numbers and percentages. Student’s t-tests, Mann–Whitney U tests and one-way analysis of variance, as appropriate, and Chi-square test (χ2) for categorical variables were used to compare groups. Statistical analysis was performed using SPSS 25.0 for Macintosh (SPSS Inc., Chicago, IL, USA). P-values of <0.05 were considered statistically significant.
Results
The survey was completed by 160 participants from 28 countries [mean age 45.5 ± 11 years, female 28.3% (n = 37)] (Table 1). The majority of survey participants (76%) stated that their hospitals were partially turned into COVID-19 centres, while 16% declared that the entire hospital was converted into a COVID-19 centre at some point during the pandemic.
Table 1.
Basic characteristics of the respondents (full list of responding countries available from Supplementary material online, Table S2)
| Mean age (years) | 45.55 ± 10.62 | |
| Female respondents | 28.31% (n = 37) | |
| Current working position (n = 152) | EP specialist | 77.34% |
| Cardiologist | 8.67% | |
| EP fellow | 4% | |
| Cardiology fellow | 3.33% | |
| Nurse | 5.33% | |
| Allied professional | 1.33% | |
| Main working environment (n = 152) | University hospital | 58.67% |
| Specialized public cardiology centre | 7.33% | |
| Public hospital | 16% | |
| Private hospital | 16% | |
| Private practice | 2% | |
| Country (top 5, total 28) (n = 152) | France | 32.67% |
| Spain | 18% | |
| Poland | 11.33% | |
| Serbia | 6.67% | |
| Italy | 4.67% | |
| The hospital turned in the COVID-19 centre (n = 152) | Yes, the entire hospital | 16% |
| Yes, part of the hospital | 76% | |
| No | 8% | |
Remote monitoring before, during, and after the COVID-19 pandemic
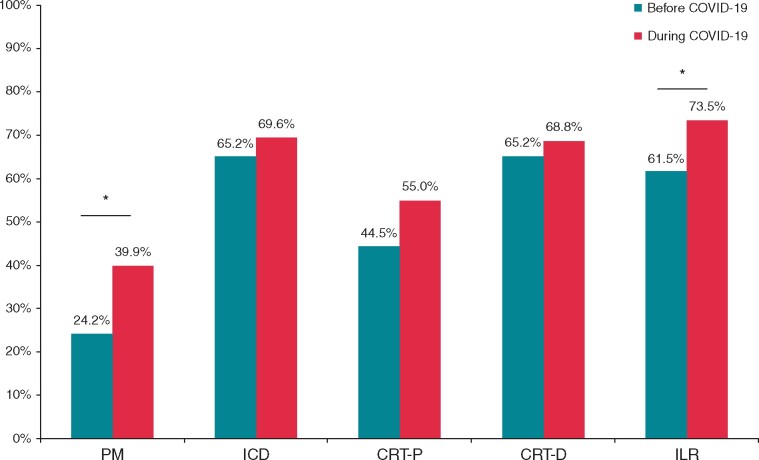
Remote monitoring was used in 24.2% of pacemaker (PM) patients before the COVID-19 pandemic. The percentage of PM patients with RM increased significantly during the pandemic to 39.9% (P = 0.002). Similarly, usage of RM for implantable loop recorders (ILRs) increased from 61.5% to 73.5% (P = 0.028) (Figure 1). Utilization of RM for implantable cardioverter-defibrillators (ICDs) did not change significantly during the pandemic [ICD: 65.2% before vs. 69.6% during the pandemic, P = 0.408; cardiac resynchronization therapy-defibrillators (CRT-D): 65.2% before vs. 68.8% during the pandemic, P = 0.513]. There was a trend for a higher utilization of RM for CRT-pacemakers (CRT-P), with 44.5% of devices with RM before and 55% of devices with RM during the pandemic (P = 0.063).
Figure 1.
Question: ‘What percentage of implanted CIEDs before/during COVID-19 had remote monitoring?’ Total number of respondents 114. *P < 0.05. CIED, cardiac implantable electronic device; CRT-D, cardiac resynchronization therapy-defibrillator; CRT-P, cardiac resynchronization therapy-pacemaker; ICD, implantable cardioverter-defibrillator; ILR, implantable loop recorder; PM, pacemaker.
The majority of the respondents declared willingness to increase the use of RM of all CIEDs after the pandemic: 53.7% for PM, 80% for ICD, 71.5% for CRT-P, 80.5% for CRT-D, and 81.8% for ILR.
New RM connections for pre-COVID implanted CIEDs and adherence to the official guidance
Nearly two-thirds of participants (57 out of 87 respondents), established new RM connections for CIEDs implanted before the pandemic with 33.3% (n = 29) delivering RM transmitters to the patient’s home address, and the remaining 32.1% (n = 28) activating RM connections during an in-office visit.
More than half of the respondents (54.1%) stated that recent guidance by the European Society of Cardiology (ESC)8 and Heart Rhythm Society (HRS)9 on management of cardiovascular disease during the COVID19 pandemic did not lead to any significant changes on their management of CIED patients. Up to 42.2% acknowledged some degree of modification in practice, and only 3.7% stated that it ‘absolutely changed’ their practice during the pandemic.
Frequency of in-person visits of RM patients
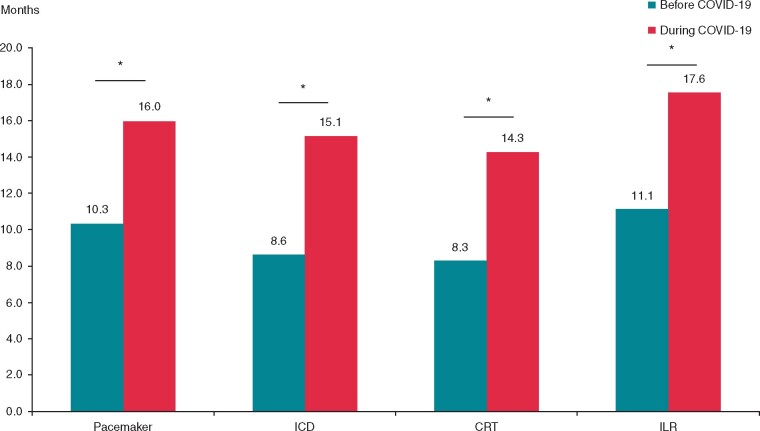
Of 109 responses, respondents stated that 57.4% of all CIEDs in-clinic follow-ups were delayed due to the pandemic. The mean period between face-to-face appointments for RM patients with an implanted PM changed from 10.3 ± 5.4 months to 16 ± 12.5 months during the pandemic (P < 0.001). For patients with an ICD, this changed from 8.6 ± 5.8 months to 15.1 ± 13.9 months during the COVID-19 pandemic (P < 0.001), and for CRT patients, it increased from 8.3 ± 6 months to 14.3 ± 14 months (P < 0.001). Implantable loop recorder were checked in person every 11.1 ± 11.9 months before vs. 17.6 ± 17.2 months during the pandemic (P = 0.002) (Figure 2).
Figure 2.
Question: ‘How frequent were in-person checkups with your remotely monitored patients, before/during COVID-19?’. Total number of respondents 114. *P < 0.05. CIED, cardiac implantable electronic device; CRT, cardiac resynchronization therapy; ICD, implantable cardioverter-defibrillator; ILR, implantable loop recorder.
Remote monitoring data filtering
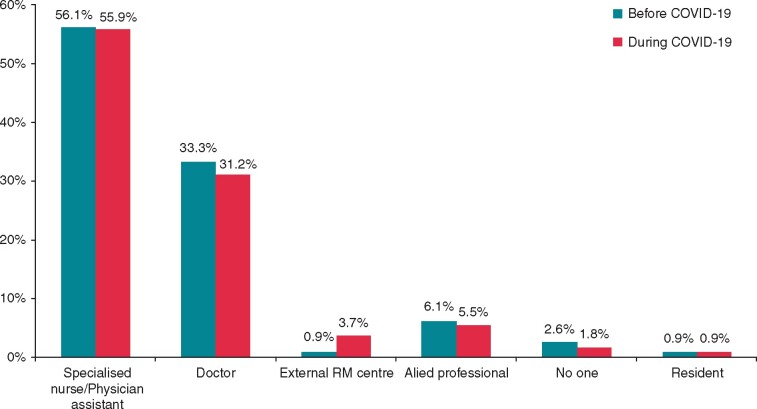
The COVID-19 pandemic did not significantly impact on the recruitment and organization of the RM data filtering personnel (P = 0.818) (Figure 3). In most cases, a specialized nurse or physician assistant was in charge of data filtering (56.1% before vs. 55.9% during the pandemic), followed by doctors (33.3% vs. 31.2%) and allied professionals (6.1% vs. 5.5%, respectively).
Figure 3.
Question: ‘Who was in charge of filtering remote monitoring data of CIEDs before/during COVID-19?’ Total number of respondents 114. CIED, cardiac implantable electronic device; RM, remote monitoring.
Clinical impact of RM during the pandemic
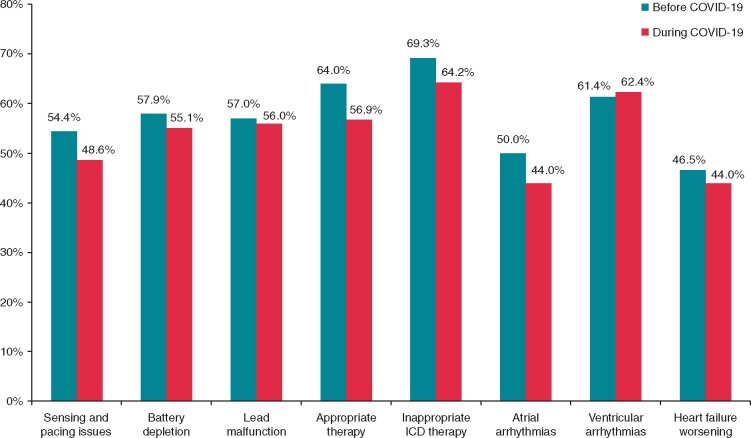
The clinical impact of RM findings did not significantly differ before and during the COVID-19 (P = 0.687). Of 114 responses, participants replied that the need for phone calls (64% vs. 64.2%) or in-office visits (12.3% vs. 15.6%) following significant RM findings was similar between the pre-and post-pandemic period.
According to the responses, the most frequent reasons for face-to-face visits before and during the pandemic were inappropriate ICD therapies (69.3% vs. 64.2% responses, respectively, P = 0.321), followed by appropriate ICD therapies (64% before vs. 56.9% during the COVID-19; P = 0.242). Even though no significant differences in reasons for initiating in-office visits for RM patients when comparing before and during pandemic were reported (Figure 4), there was a trend towards fewer face-to-face appointments for all indications during COVID-19, except for ventricular arrhythmias (61.4% vs. 62.4%, P = 0.424).
Figure 4.
Question: ‘Please specify the main reasons for initiating in-clinic visits of remotely monitored patients before/during COVID-19 pandemic’. Total number of respondents 114. ICD, implantable cardioverter-defibrillator.
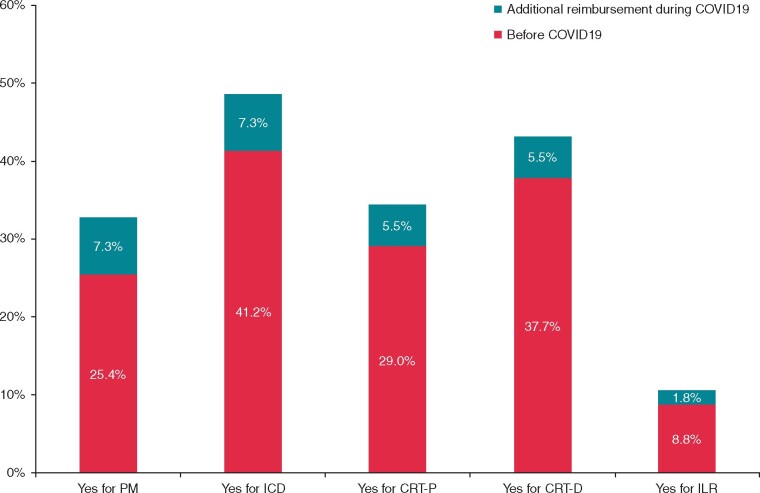
Reimbursement for RM of CIEDs
Of 114 respondents, 57% (n = 65) did not receive any reimbursement for RM of CIEDs, before the pandemic. Reimbursement of RM before the pandemic was declared by 25.4% of the respondents for PM, 41.2% for ICD, 29% for CRT-P, 37.7% for CRT-D, and only 8.8% of the centres received reimbursement for RM of ILR. Additional reimbursement for RM of CIEDs was declared by 7.3% respondents for PM and ICD during the COVID-19 pandemic of 109 respondents. A 5.5% increase in respondents receiving reimbursement for RM of CRT-P and CRT-D was observed during the pandemic. Only 1.8% of participants received additional reimbursement for RM of ILR during the COVID-19 (Figure 5).
Figure 5.
Question: ‘Did you receive any reimbursement for remote monitoring before/during COVID-19? If yes, please specify for which devices’. Total number of respondents 114. CRT-D, cardiac resynchronization therapy-defibrillator; CRT-P, cardiac resynchronization therapy-pacemaker; ICD, implantable cardioverter-defibrillator; ILR, implantable loop recorder; PM, pacemaker.
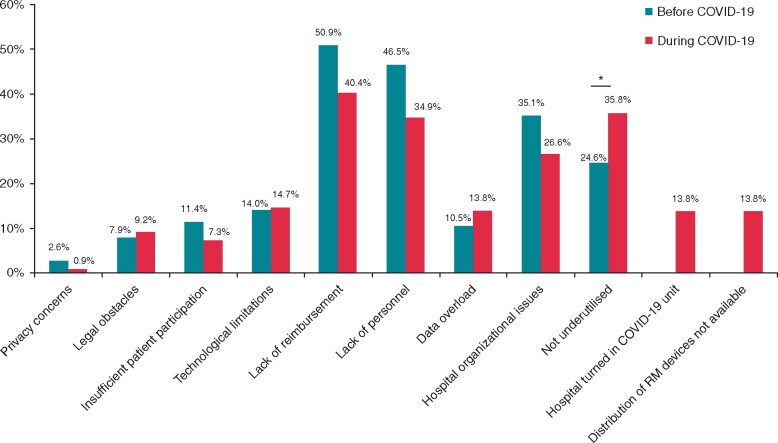
Reasons for underutilization of RM
Out of 114 respondents, only one-quarter of the participants (24.6%) considered RM sufficiently utilized prior to the pandemic. During the pandemic, this proportion has significantly increased to 35.8% (P = 0.048). The main reasons for underutilization of RM before the pandemic were lack of personnel (46.5%) and lack of reimbursement (50.9%). Interestingly, during the pandemic, these percentages dropped to 34.7% (P = 0.053) and 40.4% (P = 0.085) (Figure 6).
Figure 6.
Question: ‘If you consider that remote monitoring was underutilized before/during COVID-19, please specify the main reasons’. Total number of respondents 114. *P < 0.05. RM, remote monitoring.
Discussion
The main findings of this survey are: (i) use of RM increased during COVID-19, and a further increase may be expected after the pandemic; (ii) the pandemic significantly reduced the frequency of face-to-face appointments of RM patients with CIEDs; (iii) the reasons for in-office visits of RM patients during the pandemic were similar to those prior to it; and (iv) COVID-19 did not change the RM data filtering personnel profile.
Use of RM of CIEDs pre-, during, and planning for the post-COVID period
Even though RM had been available for two decades before the pandemic and international guidelines recommend its use since 2015, the full capacities of RM had not been fully exploited, with a low adoption rate across European centres.2,4,10 The measures of physical distancing implemented in many countries during the COVID-19 created a broader and urgent need for a wider adoption of digital solutions, among them, RM. Indeed, the wEHRAbles survey-II showed an increased use of teleconsultations during the pandemic, while the HRS survey showed almost a 10-fold higher adoption of routine use of video-telehealth.6,11 The results of our survey confirm the greater use of RM in patients with CIEDs, particularly with PM and ILR, and, to a less extent, CRT-P. Remote monitoring of high-energy devices was adopted in a larger number of centres during the pandemic but differences were not significant. These findings are in concordance with the results of the 2015 EHRA survey on the RM implementation across Europe, which showed a very high rate of RM use in ICD and CRT devices, comparable to the rate in our survey.4 Additionally, in Italy, there was no significant increase in the use of RM for ICD and CRT devices from 2012 to 2017, although there was a significantly higher use of RM for ILR, as we have seen in our study.12 Unlike the wEHRAbles survey-II results, which showed that the same level of telemedicine use is expected after the COVID-19 pandemic, our survey shows that a further increase of RM use after the pandemic is likely and is planned by the majority of physicians.11
Frequency of in-office visits of RM patients, changes introduced by ESC and HRS guidance and establishment of new RM connections for pre-COVID implanted CIEDs
To reduce transmission of the SARS-CoV-2 virus, ‘lock-down’ measures were put into practice worldwide. In addition, the ESC and HRS guidance for cardiac electrophysiologists during the COVID-19 pandemic recommended the postponement of elective or in-person visits for CIED routine follow-up.8,9 Our findings revealed a significantly lower frequency of in-office visits of RM patients with CIEDs during the pandemic, showing an adjustment of the clinical practice to the emerging epidemiological situation. Despite the application of measures presented in the ESC and HRS guidance, more than half of the respondents stated that such guidance did not lead to any significant changes in their clinical practice. Reasons for this lack of change in behaviour remain to be clarified, and we consider these results as a call for action for further official guidance promotion.
Controversially, the approach for establishing new RM connections for pre-COVID implanted CIEDs was equally split between delivering an RM transmitter to the patient’s home address and in-office RM connection activation. Noteworthy, one-third of centres did not offer RM connections to patients with CIEDs implanted prior to the pandemic. This discrepancy in the respondents’ answers to this survey, and non-compliance with the advice of the practice document proposed by the ESC and HRS should be indicative, and eventually helpful for further recommendations or consensus documents. Recent studies on patients that received RM devices at home addresses show that the majority of patients were able to successfully activate the transmitter, and experienced higher degree of satisfaction, as well as a reduced anxiety levels when compared to the face-to-face activation of RM connection.13,14 This increase in RM utilization, even for CIEDs implanted before the pandemic, was in accordance with the ESC and HRS guidance for COVID-19.8,9
RM data filtering and initiation of in-office visits of RM patients
RM is an efficient and safe method of monitoring patients with CIEDs, while simultaneously reducing the number of in-office visits and mortality of these patients, mainly by earlier recognition and management of arrhythmias, device malfunction and heart failure.3,4,15 Our survey shows that despite COVID-19, there were no changes in the clinical value of the data received via RM before and during the pandemic. However, the volume of transmissions is increasing alongside the alerts. In a recent study, 40% of all RM transmissions were alerts, with 50% of all alerts being produced by ILR, even though these only accounted for 18.8% of all followed devices.16 This represents a considerable burden, and therefore, efficient data filtering is a crucial part of RM by reducing data overload. In our survey, no changes were observed in the RM data filtering personnel. Surprisingly, in 2.6% of the responding centres in pre- and 1.8% during COVID-19, no one filtered the data. Despite the tiny percentage of respondents for whom no one filters the data, concerns and encouragement for organizing teams for RM data filtering, according to the guidelines, must be expressed.2 In addition to data filtering, RM teams’ crucial tasks are timely recognition and initiation of in-person visits. In this survey, reasons for initiating an face-to-face visits did not differ before and during the COVID-19. Despite the lock-down measures, recent research investigating data from RM transmissions during COVID-19 showed a significant increase in thoracic impedance, decreased physical activity and a 33% increase in atrial fibrillation episodes in patients with CIEDs.17,18 In contrast, during the pandemic, a 32% reduction in ventricular arrhythmias requiring device therapies was observed with a more pronounced reduction in areas with a greater prevalence of COVID-19 infection.19
Reimbursement of RM during the pandemic
The results of the 2015 EHRA survey showed that 80% of the respondents did not receive reimbursement for RM of CIEDs and that the lack of reimbursement was the most significant barrier for implementation of RM of CIEDs.4 However, results from our survey show that the number of centres not receiving reimbursement for RM of CIEDs before the COVID-19 was now more than 50%, demonstrating a significant increase in the rate of reimbursement. Additionally, our results show an increase in the rate of participant centres being reimbursed during the COVID-19 pandemic across all devices. These results are promising, but it must be borne in mind that a large number of participants still do not receive reimbursement for RM preventing its wider use.
Reasons for underutilization of RM during COVID-19
Besides increased use of RM of CIEDs during COVID-19, a significant number of respondents expresses additional reasons for the relative underutilization of RM. Despite not achieving statistical significance, it is essential to note a declining trend of reasons, such as lack of reimbursement, personnel and hospital organizational issues during the COVID-19. Moreover, as a reason for the underutilization of RM in our survey, privacy concerns and legal obstacles represented an insignificant proportion. It can be interpreted either as: (i) the pandemic having reduced the legal and privacy concerns or (ii) as an improvement and a greater adherence to the GDPR during the crisis.
Limitations
Considering that 50% of the answers to the survey came from France and Spain, the results of this survey may not necessarily be generalizable to the whole of Europe. Additionally, the voluntary nature of surveys like this one adds uncertainty to the estimates and raises questions whether these results represent a realistic reflection of the actual situation. The lack of space for additional questions in the survey prevented a more detailed investigation of the observed changes, and further research is needed.
Conclusions
The results of this survey highlight the impact of COVID-19 on the increased use of RM of CIEDs, leading to a reduction of unnecessary in-office visits. The pandemic did not change RM data filtering personnel and the reasons for in-office visits of RM patients were similar to those prior to it. Further implementation of RM use after the pandemic is warranted and planned by the majority of physicians.
Supplementary material
Supplementary material is available at Europace online.
Supplementary Material
Acknowledgements
The production of this document is under the responsibility of the Scientific Initiatives Committee of the European Heart Rhythm Association: Serge Boveda (Chair), Giulio Conte (Co-Chair), Ante Anic, Sergio Barra, Julian K.R. Chun, Carlo de Asmundis, Nikolaos Dagres, Michal M. Farkowski, Jose M. Guerra, Konstantinos E. Iliodromitis, Kristine Jubele, Jedrzej Kosiuk, Eloi Marijon, Rui Providencia, Frits Prinzen.
The authors acknowledge the EHRA Scientific Research Network centres participating in this survey. A list of these centres can be found on the EHRA website.
The authors are deeply thankful to Vanessa Meyen for her support in coordinating the project.
Conflicts of interest: S.S. has received speaker honoraria from Bayer. R.P., S.B., and B.K. have nothing to declare. J.M.G. has served as a consultant for Medtronic, Boston Scientific, Microport and Abbott, received speaker fees from Medtronic, Boston Scientific and Abbott and received a research grant from Abbott. G.C. has nothing to declare. D.D. has received speaker honoraria and/or travel grants from Abbott, Astra Zeneca, Bayer, Biotronik, Boehringer Ingelheim, Boston Scientific, Medtronic, Pfizer and Zoll. E.M. has nothing to declare. A.A. has received consulting fees and speaker honoraria from Boston Scientific Inc., Farapulse Inc., Galaxy Medical Inc. and Biosense & Webster and a research honoraria from Boston Scientific Inc., Farapulse Inc., Galaxy Medical Inc., and Biosense & Webster. S.B. is a consultant for Medtronic, Boston Scientific, Microport and Zoll.
References
- 1. Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt O-A. et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapyThe Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace 2013;15:1070–118. [DOI] [PubMed] [Google Scholar]
- 2. Slotwiner D, Varma N, Akar JG, Annas G, Beardsall M, Fogel RI. et al. HRS Expert Consensus Statement on remote interrogation and monitoring for cardiovascular implantable electronic devices. Heart Rhythm 2015;12:e69–100. [DOI] [PubMed] [Google Scholar]
- 3. Saxon LA, Hayes DL, Gilliam FR, Heidenreich PA, Day J, Seth M. et al. Long-term outcome after ICD and CRT implantation and influence of remote device follow-up. Circulation 2010;122:2359–67. [DOI] [PubMed] [Google Scholar]
- 4. Mairesse GH, Braunschweig F, Klersy K, Cowie MR, Leyva F.. Implementation and reimbursement of remote monitoring for cardiac implantable electronic devices in Europe: a survey from the health economics committee of the European Heart Rhythm Association. Europace 2015;17:814–8. [DOI] [PubMed] [Google Scholar]
- 5. Braunschweig F, Anker SD, Proff J, Varma N.. Remote monitoring of implantable cardioverter-defibrillators and resynchronization devices to improve patient outcomes: dead end or way ahead? Europace 2019;21:846–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Han JK, Al-Khatib SM, Albert CM.. Changes in the digital health landscape in cardiac electrophysiology: a pre-and peri-pandemic COVID-19 era survey. Cardiovasc Digital Health J 2021;2:55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Varma N, Marrouche NF, Aguinaga L, Albert CM, Arbelo E, Choi JI. et al. HRS/EHRA/APHTS/LAHRS/ACC/AHA worldwide practice update for telehealth and arrhythmia monitoring during and after a pandemic. Europace 2021;23:313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic. https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance (10 June 2020, date last accessed).
- 9. Lakkireddy DR, Chung MK, Gopinathannair R, Patton KK, Gluckman TJ, Turagam M. et al. Guidance for cardiac electrophysiology during the coronavirus (COVID-19) pandemic from the Heart Rhythm Society COVID-19 Task Force; Electrophysiology Section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association. Heart Rhythm 2020;17:e233–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marinskis G, van Erven L, Bongiorni MG, Lip GYH, Pison L, Blomström-Lundqvist C.. Practices of cardiac implantable electronic device follow-up: results of the European Heart Rhythm Association survey. Europace 2012;14:423–5. [DOI] [PubMed] [Google Scholar]
- 11. Manninger M, Zweiker D, Svennberg E, Chatzikyriakou S, Pavlovic N, Zaman JAB. et al. Current perspectives on wearable rhythm recordings for clinical decision-making: the wEHRAbles 2 survey. Europace 2021;23:1106–13. [DOI] [PubMed] [Google Scholar]
- 12. Palmisano P, Melissano D, Zanotto G, Perego GB, Toselli T, Landolina M. et al. Change in the use of remote monitoring of cardiac implantable electronic devices in Italian clinical practice over a 5-year period: results of two surveys promoted by the AIAC (Italian Association of Arrhythmology and Cardiac Pacing). J Cardiovasc Med 2020;21:305–14. [DOI] [PubMed] [Google Scholar]
- 13. Magnocavallo M, Bernardini A, Mariani MV, Piro A, Marini M, Nicosia A. et al. Home delivery of the communicator for remote monitoring of cardiac implantable devices: a multicenter experience during the covid‐19 lockdown. Pacing Clin Electrophysiol 2021;31:2814–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Piro A, Magnocavallo M, Rocca DGD, Neccia M, Manzi G, Mariani MV. et al. Management of cardiac implantable electronic device follow‐up in COVID‐19 pandemic: lessons learned during Italian lockdown. J Cardiovasc Electrophysiol 2020;31:2814–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Garcia-Fernandez FJ, Asensi JO, Romero R, Lozano IF, Larrazabal JM, Ferrer JM. et al. Safety and efficiency of a common and simplified protocol for pacemaker and defibrillator surveillance based on remote monitoring only: a long-term randomized trial (RM-ALONE). Eur Heart J 2019;40:1837–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. O'Shea CJ, Middeldorp ME, Hendriks JM, Brooks AG, Lau DH, Emami M. et al. Remote monitoring alert burden: an analysis of transmitions in >26,000 patients. JACC Clin Electrophysiol 2021;7:226–34. [DOI] [PubMed] [Google Scholar]
- 17. Mascioli G, Lucca E, Napoli P, Giacopelli D.. Impact of COVID-19 lockdown in patients with implantable cardioverter and cardiac resynchronization therapy defibrillators: insights from daily remote monitoring transmissions. Heart Vessels 2021;29:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. O’Shea CJ, Middeldorp ME, Thomas G, Harper C, Elliott AD, Ray N. et al. Atrial fibrillation burden during the coronavirus disease 2019 pandemic. Europace 2021;doi:10.1093/europace/euab099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. O’Shea CJ, Thomas G, Middeldorp ME, Harper CC, Elliot AD, Ray N. et al. Ventricular arrhythmias burden during the coronavirus disease 2019 (COVID-19) pandemic. Eur Heart J 2021;42:520–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.