Abstract
Background and objectives
Assessing the co-infections with COVID-19 is crucial to delineate its true clinical impact. Pediatric information in this aspect is limited. Our study aims to analyze the spectrum of co-infections in pediatric COVID-19 patients and determine the clinical as well as laboratory parameters predicting co-infection.
Methodology
In this prospective observational study conducted from June to December 2020 in a single tertiary care institution, data pertaining to demographic, illness and treatment-related variables were analyzed among two subsets of pediatric patients of age 1 month–12 years with RT–PCR-confirmed COVID-19 infection-Group A: those with confirmed co-infection and Group B: moderate to severe disease without co-infection. Among Group A, etiology of co-infection was characterized through relevant microbiological examination within 48 h admission.
Result
Among our study population, 15.03% and 20.6% had co-infections and moderate to severe disease respectively. Among those with confirmed co-infection, 32.5%, 11.6% and 6.97% recorded blood culture, respiratory secretion and CSF growth, respectively, the picture being dominated by Methicillin resistant and sensitive Staphylococcus aureus. Serum serology demonstrated Scrub typhus infection to be most prevalent. Concurrent respiratory viral infections were seen in 11.6%. Children with co-infection had significantly higher morbidity and need for supportive therapy. Predictors of co-infection were localization of infection, Neutrophil count ≥10×109, age-specific lymphopenia, CRP > 100 mg/dl and hyperferritinemia.
Conclusion
Co-infections are an important factor prognosticating pediatric COVID infection. Their early detection, prompt and appropriate treatment is of paramount importance.
INTRODUCTION
Since last year, the world is witnessing the COVID-19 pandemic, caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), a novel Coronavirus, possessing a relatively high mortality rate, apart from being highly contagious.
Though initial studies showed pediatric involvement to be less in frequency and severity than adults, current scenario reveals increasing hospitalization rates among children with about one in three COVID-19 positive children in USA requiring intensive care unit, similar to the rate among adults [1–3]. Mirroring the adults, microbial co-infection rates in pediatric population are as high as 51% [4]. Co-infection of SARS-CoV-2 with other micro-organisms, such as virus, bacteria and fungi, have emerged as significant challenge influencing diagnosis, treatment and prognosis of COVID-19 infected adults [5].
The recommendation regarding empiric use of antibiotics, antiviral specially anti-influenza and antifungal differs widely between guidelines furnished by different international bodies. National Institutes of Health does not recommend empiric broad-spectrum antibiotic in absence of specific indication [6]. Surviving Sepsis Campaign suggested the use of empiric antimicrobials/antibacterial agents, in mechanically ventilated patients with COVID-19 and respiratory failure [7]. By contrast Canadian guideline, empiric antimicrobials used in treating all likely pathogens causing severe acute respiratory infection and sepsis [8]. So early prediction and identification of co-infection with COVID-19 are critically important for choosing right antimicrobials as well as escalation of supportive therapy.
Hence, understanding the dynamics of co-infection with COVID-19 is crucial to delineate its true clinical impact and early intervention. In spite of multiple adult studies being conducted, data on co-infections in pediatric COVID-19 cases from tropical countries like India are constrained. Moreover, among the COVID-19 afflicted children presenting with Multisystem inflammatory Syndrome in children [9], exclusion of other etiologies including infectious ones becomes paramount in diagnosis and further management. Unfortunately most of the centers of resource restricted settings facility of rapid diagnostic test like multiplex polymerase chain reaction (PCR) are lacking due to high cost. So it is crucial to identify the clinical and available laboratory predictors of co-infection along with COVID-19 in children.
Our study aims to analyze the spectrum of co-infections in pediatric COVID-19 patients with moderate to severe disease and determine clinical characteristics and laboratory parameters that can predict presence of co-infection.
MATERIALS AND METHODS
This single center prospective observational study was conducted from June to December of 2020 in a tertiary care institution, dedicated to COVID-19 care. The study was approved by the Institutional Ethics committee and was conducted in accordance with the amended Declaration of Helsinki. Informed consent was obtained from parents or legal guardian in their understandable language.
Pediatric patients within 1 month–12 years age with moderate to severe COVID-19 infection, admitted in the above-mentioned time period were considered. Disease severity was decided by the contemporary MoHFW guidelines. Inclusion Criteria: pediatric patients with confirmed moderate to severe COVID-19 infection, defined as a positive real-time reverse transcriptase polymerase chain reaction for SARS-CoV-2 from a nasopharyngeal swab associated with suggestive signs, symptoms and/or radiological findings [10] and hospitalized. Exclusion Criteria: Patients with mild COVID-19 infection. Subsequently, patients with confirmed co-infection were designated as Group A and patients who had moderate or severe disease were assigned Group B.
For determining presence of bacterial, viral and fungal co-infection, relevant microbiological investigations—blood culture, cerebro spinal fluid (CSF) culture, urine culture, culture of the respiratory tract secretions (Tracheal aspirate/Bronchoalveolar lavage) and multiplex respiratory PCRs detecting 4 bacteria and 15 viruses (Panel RP2 plus Film array Biomerieux ®)—from nasopharyngeal swab or on respiratory tract secretions were performed within the first 48 h of hospital admission. Microbiological investigations obtained after 48 h were not considered in order not to exclude patients with nosocomial infection. Serological investigations like malaria rapid diagnostic test, leptospira serology, dengue NS1 and IgM by ELISA, scrub typhus IgM ELISA serologic and/or nucleic acid-based diagnostic testing for EBV, serological testing for mycoplasma pneumonia and WIDAL tests were performed based on the clinical presentation and suspected etiology.
Demographic profiles like age, sex and nutritional status recorded in both the groups. Clinical features like fever, cough, breathing difficulty, rash, convulsion, altered sensorium, gastro intestinal symptoms, shock, myocardial dysfunction (ejection fraction <50%), bleeding manifestation and number of organs involved were noted. Severity of affliction was assessed by PIM II [11] and Psofa [12] score. Pre-existing comorbidity was recognized.
Laboratory investigations like hemoglobin, white blood cell (WBC) count, neutrophil and lymphocyte count, platelet count, trans-aminase level, international normalization ratio (INR), C-reactive protein (CRP), procalcitonine and albumin were measured. Investigations done soon after PICU admission were recorded. Where indicated other relevant investigations like pro BNP, serum ferritin, lactate dehydrogenase (LDH), D dimer, fibrinogen level and IL 6 were also done. For multivariate analysis the cut off for hematological parameters were defined as anemia (Hb <9 g/dl), thrombocytopenia (platelet ≤1.50 × 105/mm3), neutrophilia (≥10 × 109/l) and leucopenias (age appropriate cut off). The cut off values for other laboratory markers were taken as—high procalcitonin (≥2 ng/ml), hyperferritinemia (≥500 ng/ml) (23), hypoalbuminemia (≤2.5 mg/dl), CRP (≥100 mg/dl), raised ALT/SGPT (≥40 IU/l), INR (≥1.5).
Treatment-related variables like respiratory assistance required: invasive/non-invasive, inotrope requirement, vasoactive inotrope score (VIS) [13], blood component therapy required, antibiotic requirement, corticosteroids, low molecular weight heparin and immunomodulator requirement were noted. Outcome-associated variables; length of stay in intensive care, length of stay in hospital and mortality were recorded.
Broad spectrum empiric antibiotic therapy, based on local microbiology pattern, was initiated in critically ill patients as recommended by the Surviving Sepsis Campaign guidelines [14]. De-escalation was performed as soon as the results of microbiological investigations performed upon ICU admission were available.
STATISTICAL ANALYSIS
Statistical Packages for the Social Sciences [6] version 25 was used for statistical analysis of data of this study. Results of continuous variables were described by median (quartiles) while categorical variables were described by frequency (%). Quantitative continuous variables were compared between groups using Mann–Whitney’s non-parametric tests if the variable has a non-normal distribution or unpaired Student’s t-test if the variable had a normal distribution. Qualitative variables were compared by Chi-square test and Fisher Exact test. The factors identified as significantly different between two groups were further tested by reverse multivariate regression analysis for assessing the association between demographic and other clinical or laboratory factors that can predict associated co-infection. p-value <0.05 was taken as statistically significant.
RESULT
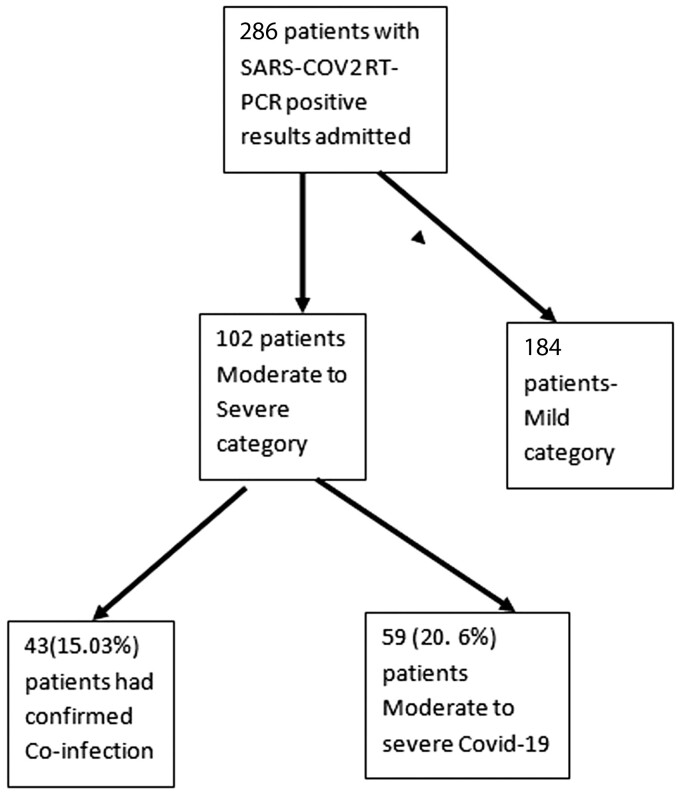
During the study period, 286 children with confirmed COVID-19 infection required hospital admission, out of which 43 cases (15.03%) were diagnosed with co-infection by isolation of organism, multiplex PCR or serological assay. During the same time period 59 (20.6%) admitted patients had moderate to severe disease (Fig. 1).
Fig. 1.
Flow diagram showing the study participants.
Out of 43 patients with confirmed co-infection (Table 1), blood culture was positive for 14 (32.5%) patients. The blood culture isolates were Methicillin resistant Staphylococcus aureus (MRSA) [n = 3 (21.4%)], Methicillin sensitive S.aureus (MSSA) [n = 2 (14.2%)], Coagulase negative Staphylococcus spp. (CONS) [n = 2(14.2%)], Pseudomonus aeruginosa [n = 2 (14.2%)], Salmonella typhi—1 [n = 1 (7.14%)] and Klebsiella pneumonia [n = 1 (7.14%)]. Respiratory secretion culture grew organisms in five (11.6%) patients and the isolates were MSSA (n = 3), MRSA (n = 1), CONS (n = 1) and P.aeruginosa (n = 1). CSF culture was positive in three patients. Serum serological investigations revealed scrub typhus as most prevalent (n = 7), followed by dengue, S.typhi, hepatitis A and Epstein–Barr virus-1. Multiplex PCR from respiratory secretion was positive in five patients for respiratory viruses like Respiratory syncital virus (RSV) (n = 2), Influenza-A (n = 1), Adenovirus (n = 1) and Rhinovirus (n = 1).
Table 1.
Type of specimen, test performed and organism identified
| Test performed | Type of specimen and positive rate | Organisms identified |
|---|---|---|
|
Blood—14 (32.5%) |
|
| Respiratory secretion—5 (11.6%) |
|
|
| Cerebrospinal fluid—3 (6.9%) |
|
|
|
Blood—16 (37.2%) |
|
|
Respiratory secretion—5 (11.6%) |
|
No difference was noticed in distribution of age, sex and nutritional status (Table 2). Duration of fever was significantly longer in children with co-infection [6 (3–10) vs. 3.5 (1–7), p = 0.012]. Incidence of shock, convulsion and altered sensorium was found significantly higher in co-infection group than without co-infection and p-value 0.001, 0.027 and 0.04, respectively. Respiratory distress as presenting symptom was more prevalent in children with moderate to severe covid infection than co-infection group 27 (45.7) vs. 14 (32.5) but was not statistically significant. Overall comorbidity and malignancy was noted to significantly higher in co-infection group. Severity of disease as measured by PRISM III and Psofa score was significantly high in co-infection group.
Table 2.
Comparison of demographic profile, clinical features and severity of disease between two groups
| Variable | COVID-19 with co-infection | Moderate to severe COVID-19 | p-value |
|---|---|---|---|
| (N = 43) | (N = 59) | ||
| Age, years, median (IQR) | 4.5 (0.4–7.5) | 5.5 (0.9–8) | 0.52 |
| Gender, Male | 23 (53.4%) | 30 (51%) | 0.84 |
| Nutritional status | |||
| Underweight | 17 (39.5) | 24 (40.6) | |
| Normal | 21 (48.8) | 29 (49.1) | 0.54 |
| Obese | 5 (11.5) | 6 (10.3) | |
| Fever duration, days, median (IQR) | 6 (3–10) | 3.5 (1–7) | 0.012 |
| Cough | 18 (41) | 35 (59.2) | 0.12 |
| Respiratory distress | 14 (32.5) | 27 (45.7) | 0.22 |
| Shock | 24 (55.8) | 13 (22) | 0.001 |
| Convulsion | 11 (25.5) | 5 (8.5) | 0.027 |
| Altered sensorium | 8 (18.6) | 3 (%) | 0.04 |
| Bleeding manifestation | 6 (14) | 2 (3.3) | 0.67 |
| Skin rash | 7 (16.2) | 15 (25.4) | 0.33 |
| Diarrhea | 4 (9.3) | 18 (30.5) | 0.014 |
| Decreased urine output | 10 (23.2) | 6 (10.1) | 0.09 |
| Number of organs involved, median (IQR) | 4 (2–6) | 2 (1–3) | 0.017 |
| Comorbidity | 25 (58) | 19 (32.2) | 0.015 |
| Malignancy | 13 (30) | 04 (6.7) | 0.003 |
| Neurological disability | 07 (16.2) | 08 (13.5) | 0.78 |
| Congenital heart disease | 02 (4.6) | 06 (10.1) | 0.46 |
| Chronic lung disease | 02 (4.6) | 01 (1.7) | 0.57 |
| Chronic kidney disease | 01 | – | |
| Localization of infection | |||
| Pneumonia | 14 (32.5) | 28 (49.1) | 0.10 |
| Meningitis | 7 (16.3) | 0 | 0.001 |
| Encephalitis | 6 (13.9) | 3 (4.5) | 0.16 |
| Soft tissue infection | 6 (13.9) | 0 | 0.001 |
| Myocarditis | 2 (4.6) | 9 (15.2) | 0.113 |
| Arthritis/osteomyelitis | 3 (7) | 0 | |
| GI infection | 5 (11.6) | 18 (30.5) | 0.03 |
| PRISM III score, median (IQR) | 16 (13–20) | 10 (8–14) | 0.01 |
| PSOFA score, median (IQR) | 10 (7–13) | 7 (5–10) | 0.01 |
Values are denoted as n (%), unless otherwise stated.
Among the laboratory parameters, children with co-infection had significantly lower hemoglobin percentage in comparison to moderate to severe COVID-19 infected children [8.6 (6.0–12.8) vs. 10.1 (6.5–15), p = 0.02] (Table 3). Total WBC and neutrophil count was significantly higher in con-infection group. Lymphopenia was more prevalent in children with co-infection (72% vs. 30%, p = 0.001). CRP and serum ferritin was significantly elevated in the former group and p-value was 0.001 for both. Serum Alanine aminotransferase, LDH and INR was significantly higher in children with co-infection.
Table 3.
Comparison of laboratory parameters between two groups
| Variable | COVID-19 with co-infection | Moderate to severe COVID-19 | p-value |
|---|---|---|---|
| (N = 43) | (N = 59) | ||
| Hemoglobin, g/dl | 8.6 (6.0–12.8) | 10.1 (6.5–15) | 0.02 |
| WBC, ×109/l | 11.7 (8.05–17.05) | 7.8 (5.0–10.7) | 0.03 |
| Neutrophil, ×109/l | 10.5 (6.8–14.68) | 6.5 (4.5–9.6) | 0.005 |
| Lymphocytes, ×109/l | 0.7 (0.5–1.1) | 1 (0.7–1.3) | 0.009 |
| Lymphopenia, n (%) | 31 (72) | 18 (30) | 0.001 |
| Thrombocytes, ×109/l | 133.5 (103.5–224.5) | 176 (138–262) | 0.388 |
| Creatinine, mg/dl | 0.8 (0.5–1.1) | 0.6 (0.4–0.9) | 0.09 |
| C-reactive protein, mg/dl | 114.7 (48.9–196.7) | 64.9 (24.5–113.8) | 0.001 |
| Alanine aminotransferase, U/l | 68 (46–112) | 43 (31–54) | 0.01 |
| Aspartate aminotransferase, U/l | 56 (38–84) | 48 (32–62) | 0.3 |
| Lactate dehydrogenase, U/l | 434 (350–586) | 368 (284–454) | 0.01 |
| International normalized ratio | 1.9 (1.3–2.4) | 1.4 (1.1–1.7) | 0.043 |
| D-dimer, μg/ml | 5.8 (2.4–12.6) | 7.1 (2.8–14.3) | 0.07 |
| Ferritin, ng/ml | 1135 (556–1685) | 583 (240–789) | 0.001 |
| Procalcitonin, ng/ml | 3.3 (0.6–5.2) | 2.57 (0.3–4.3) | 0.07 |
| IL-6, pg/ml | 89.4 (39.6–87) | 66.2 (35–122) | 0.022 |
| (n = 21) | (n = 34) | ||
| Albumin g/l | 34.4 (28.7–40.6) | 30.2 (24–34.7) | 0.12 |
Values are denoted as median (interquartile range), unless otherwise stated.
Significantly higher number of children with co-infection required mechanical ventilator support (34.8% vs. 15.2%, p = 0.03) in comparison to children without co-infection (Table 4). A total of 27 (62.8%) patients in co-infection group was cared in ICU in comparison to 21 (35.6%) in no co-infection group, p = 0.009. Other supportive therapy like need of inotropic support, vasoactive inotrope score, anticonvulsant and blood product transfusion was significantly higher in co-infection group. Co-infection group required longer stay in PICU [8 (5–11) vs. 6.5 (4.5–9.5), p = 0.02]. Although death rate was high in children in co-infection group (9.3%), but it was not statistically significant.
Table 4.
Comparison of treatment and outcome between groups
| Variable | COVID-19 with co-infection | Moderate to severe COVID-19 | p-value |
|---|---|---|---|
| (N = 43) | (N = 59) | ||
| NRM oxygen | 12 (27.9) | 38 (64.1) | 0.001 |
| HFNC | 16 (37.2) | 12 (20.34) | 0.07 |
| Mechanical ventilation | 15 (34.8) | 9 (15.2) | 0.03 |
| Inotrope | 24 (55.8) | 13 (22) | 0.001 |
| Vasoactive-inotropic score, median (IQR) | 32 (24–40) | 24 (20–32) | |
| Anticonvulsant | 11 (25.5) | 5 (8.4) | 0.027 |
| Raised ICP management | 9 (20) | 3 (5.08) | 0.26 |
| Antibiotic before hospitalization | 33 (76) | 37 (62.7) | 0.19 |
| Antibiotic >48 h | 38 (88.3) | 14 (23.7) | 0.001 |
| Renal replacement therapy | 1 | 0 | |
| Blood product | 14 (32.5) | 3 (5) | 0.001 |
| Corticosteroid | 18 (41.8) | 23 (39) | 0.83 |
| Low molecular weight heparin | 4 (9) | 18 (39) | 0.001 |
| Remdesivir | 5 (11.6) | 21 (35.6) | 0.006 |
| ICU care | 27 (62.8) | 21 (35.6) | 0.009 |
| Length of PICU stay, days, median (IQR) | 8 (5–11) | 6.5 (4.5–9.5) | 0.02 |
| Length of hospital stay, days, median (IQR) | 10 (8–13) | 7.5 (6–9) | 0.6 |
| Death | 4 (9.3) | 1 (1.7) | 0.15 |
Values are denoted as n (%), unless otherwise stated.
On stepwise sequential forward multivariable analysis of factors found significant in univariate analysis it was revealed that clinical features like prolonged duration of fever (>5 days) (r2 = 0.76, p = 0.001), presence of shock (r2 = 0.71, p = 0.001), convulsion (r2 = 0.67, p = 0.01) and altered sensorium (r2 = 0.59, p = 0.02) was significantly associated with co-infection (Table 5). Among the comorbidity, malignancy was significantly correlated with co-infection (r2 = 0.81, p = <0.001). Definite localization of infection like meningitis and soft tissue infection were predictors of co-infection. Among the laboratory parameters Neutrophil count ≥10 × 109/l, age-specific lymphopenia, elevated CRP > 100 mg/dl and hyperferritinemia were predictors of co-infection.
Table 5.
Multivariable analyses on the predictors of co-infections in patients hospitalized with COVID-19
| Baseline characteristic | Correlation coefficient | p-value |
|---|---|---|
| Duration of fever ≥5 days | 0.76 | 0.001 |
| Shock | 0.71 | 0.001 |
| Convulsion | 0.67 | 0.01 |
| Altered sensorium | 0.59 | 0.02 |
| Malignancy | 0.82 | <0.001 |
| Meningitis | 0.63 | 0.02 |
| Soft tissue infection | 0.69 | 0.01 |
| Neutrophil count ≥10 × 109/l | 0.54 | 0.03 |
| Lymphopenia | 0.65 | 0.01 |
| CRP≥100 mg/dl | 0.76 | 0.004 |
| Ferritin ≥500 ng/ml | 0.58 | 0.02 |
DISCUSSION
Our study documents 15.03% of the study population to harbor microbiologically confirmed infections, which is much lower than the recent investigations portraying a co-infection rate of 51% in the pediatric population [4, 5, 15]. Compared to the adult studies, where co-infection rates have ranged from 2.7% to 32.7%, the values lie somewhat midway [16–18]. The bacterial co-infection rate was 7.7%, higher than bacterial co-infection rates of 2.7–5.5% in adult [16, 18]. Bacteremia was found in 4.9%, higher than 1.2–1.6% seen in adults [18, 19]. Among the bacteria incriminated, Gram-positive bacteria: MRSA followed by MSSA and Staph cons were responsible for more than half of the infections. P.aeruginosa, succeeded by S.typhi and Klebsiella pneumoniae were the chief Gram-negative bacteria found. This mirrors the adult findings, where S.aureus dominated the picture in the first 48 h of hospital admission but with increased ICU stay duration, Gram-negative septicemia with Klebsiella pneumoniae and Escherichiacoli increased [16]. Taking due consideration of the association of S.aureus co-infections in Influenza pandemics too, further investigations are imperative to confirm an association between COVID-19 infection and susceptibility to S.aureus infections. In a similar study done in Dhaka by Ghosh, et al. [20] Typhoid fever (40%), Bacterial meningitis (20%), UTI (10%), Paratyphoid fever (6.7%), Rickettsial fever (6.7%), HAV infection (6.7%), HEV infection (3.3%), Septic arthritis (3.3%) and Bacterial pneumonia (3.3%) were documented in pediatric population. In tandem with other studies done in pediatric population reporting respiratory co-infection rate of 13.2–51.35%, respiratory co-infection was found by us in 23.2%, both bacterial and viral causes accounting for 50% of them [4, 15, 21]. But, whereas MSSA and RSV dominated our picture, Li, et al. [15] has found Mycoplasma pneumoniae (25%) to be the most common co-infection, followed by virus (7%) and bacteria (5%). Tiwari, et al. [22] and Skenderi, et al. [23] have reported single case of COVID-19 encephalitis with Dengue co-infection and COVID-19 with EBV co-infection, respectively. Co-infection with Varicella zoster has also been reported [24].
Such discrepancies can be explained by the numerous study design differences to a large extent, the notable ones pertaining to consideration of respiratory and extra-respiratory infections, pathogen considered, microbiological investigations employed, use of culture and non-culture methods, time of specimen collection, exclusion/inclusion of contaminants and study population itself.
Duration of fever, incidence of shock, convulsion and altered sensorium, increased disease severity (determined by PRISM III and Psofa score) and co-morbidities including malignancy were found to be significantly high in the co-infection group. Meningitis and soft tissue infections were more common in children with co-infection. Moreover, significantly higher number of children with co-infection required mechanical ventilation and other supportive therapy including inotrope, blood product transfusion, anticonvulsant therapy and had a longer PICU stay duration than those without co-infection. Though the findings resembled numerous adult studies conducted, the study conducted by Wang, etal. [18] found no significant difference in pre-existing illnesses, ICU admission or 30 day all-cause mortality in those with and without bacterial infection [25]. Also, Li, et al. [15] observed no significant difference in clinical characteristics or hospital stay in patients with co-infections.
Also, children with co-infection had significantly lower Hb, lymphopenia and higher total leukocyte count, absolute neutrophil count, CRP, serum ferritin, serum alanine aminotransferase, LDH and international normalized ratio similar to adults [18]. But, Li, et al. [15] showed children with co-infection to have lower WBC counts, neutrophil counts and lymphocyte counts.
Thus, co-infections play an important role in determining the prognosis of COVID infection and hence maintaining a low threshold of suspicion is necessary. The question arises whether to do universal screening for co-infections. Keeping in mind the huge spectrum of etiological agents and the low yield of the culture methods, we do not recommend universal screening. But, at the same time early diagnosis is crucial for early intervention and better management of COVID infection. From our study, we can pin-point the factors predicting the presence of co-infection and thus guide on the proper time to intervene. We can conclude that fever duration more than 5 days, presence of shock, convulsion and altered sensorium, definite localization of infection e.g. meningitis, soft tissue infection, pre-existing morbidity especially malignancy, neutrophil count ≥10× 109, age-specific lymphocytopenia, elevated CRP > 100 mg/dl and hyperferritinemia should prompt a physician to look out for co-infection. This will also aid in reducing irrational use of antibiotics and establishing antibiotic stewardship.
ETHICAL APPROVAL
Ethical clearance of the study & permission number—MC/KOL/IEC/NON-SPON/764/08/20 dated–7 July 2020.
REFERENCES
- 1. Centres for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19)-Associated Hospital Surveillance Network (COVID-NET). https://www.cdc.gov/coronavirus/2019ncov/covid-data/covid-net/purpose-methods.html. Accessed on 19th August 2021.
- 2. Kim L, Whitaker M, O’Halloran A, et al. ; COVID-NET Surveillance Team. Hospitalization rates and characteristics of children aged <18 years hospitalized with laboratory confirmed COVID-19-COVID-NET,14 states, March 1-July 25,2020. MMWR Morb Mortal Wkly Rep 2020;69:1081–8. doi:10.15585/mmwr.mm6932e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kim L, Garg S, O'Halloran A, et al. Risk factors for intensive care unit admission and in hospital mortality among hospitalized adults identified through the U.S. coronavirus disease 2019 (COVID-19)-associated hospitalization surveillance network (COVID-NET). Clin Infect Dis 2021;72:e206–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wu Q, Xing Y, Shi L, et al. Coinfection and other clinical characteristics of COVID-19 in children. Pediatrics 2020;146:e20200961. [DOI] [PubMed] [Google Scholar]
- 5. Mannheim J, Gretsch S, Layden JE, et al. Characteristics of hospitalized pediatric COVID-19 cases—Chicago, Illinois, March–April 2020. J Pediatric Infect Dis Soc 2020;9:519–22. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. National Institutes of Health. https://www.covid19treatmentguidelines.nih.gov/critical-care (8 May 2020, date last accessed).
- 7. Alhazzani W, Møller MH, Arabi YM, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Crit Care Med 2020;48:e440–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tamblyn S. Clinical Management of Patients with Moderate to Severe COVID-19 - Interim Guidance April 2, 2020. Available from https://www.ammi.ca/Content/Clinical%20Care%20COVID-19%20Guidance%20FINAL%20April2%20ENGLISH%281%29.pdf. Accessed on 19th August 2021.
- 9. World Health Organization. Multisystem Inflammatory Syndrome in Children and Adolescents with COVID-19. Scientific Brief. https://www.who.int/publications-detail/multisystem-inflammatory-syndrome-in-children-andadolescents-with-covid-19 (31 May 2020, date last accessed).
- 10. WHO. Clinical Management of COVID-19—Interim Guidance. https://www.who.int/publications/i/item/clinical-management-of-covid-19 (29 June 2020, date last accessed).
- 11. Lee OJ, Jung M, Kim M, et al. Validation of the pediatric index of mortality 3 in a single pediatric intensive care unit in Korea. J Korean Med Sci 2017;32:365–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Huerta LE, Wanderer JP, Ehrenfeld JM, et al. ; for the SMART Investigators and the Pragmatic Critical Care Research Group. Validation of a sequential organ failure assessment score using electronic health record data. J Med Syst 2018;42:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McIntosh AM, Tong S, Deakyne SJ, et al. Validation of the vasoactive-inotropic score in pediatric sepsis. Pediatr Crit Care Med 2017;18:750–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Alhazzani W, Møller MH, Arabi YM, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med 2020;46:854–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Li Y, Wang HM, Wang F, et al. Co-infections of SARS-CoV2 with multiple common respiratory pathogens in infected children: A retrospective study. Medicine (Baltimore). 2021; 19;100(11):e24315. doi: 10.1097/MD.0000000000024315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Baskaran V, Lawrence H, Lansbury L, et al. Coinfections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020;81:266-275. doi: 10.1016/j.jinf.2020.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Garcia-Vidal C, Sanjuan G, Moreno-García E, et al. ; COVID-19 Researchers Group. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. Clin Microbiol Infect 2021;27:83–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang L, Amin AK, Khanna P, et al. An observational cohort study of bacterial co-infection and implications for empirical antibiotic therapy in patients presenting with COVID-19 to hospitals in North West London. J Antimicrob Chemother 2021;76:796–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sepulveda J, Westblade LF, Whittier S, et al. Bacteremia and blood culture utilization during COVID-19 surge in New York City. J Clin Microbiol 2020;58:e00875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ghosh U, Baidya M, Sultana A, et al. Co-infections and COVID-19 in children: an observational study. IJISRT 2020;5:343–7. [Google Scholar]
- 21. Zhang D, Acree ME, Ridgway JP, et al. Characterizing coinfection in children with COVID-19: a dual center retrospective analysis. Infect Control Hosp Epidemiol 2020;1–3. doi:10.1017/1ce.2020.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tiwari L, Shekhar S, Bansal A, et al. COVID-19 with dengue shock syndrome in a child: coinfection or cross-reactivity? BMJ Case Rep 2020;13:e239315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Skenderi E, Sulovari A, Kuli-Lito G, et al. COVID-19 and EBV co-infection in a child. JBM 2021;09:20–7. [Google Scholar]
- 24. Karimi A, Rafiei Tabatabaei S, Khalili M, et al. COVID-19 and chickenpox as a viral co-infection in a 12-year-old patient, a case report. Arch Pediatr Infect Dis 2020;8:e105591. [Google Scholar]
- 25. Musuuza J, Watson L, Parmasad V, et al. Prevalence and outcomes of co-infection and super-infection with SARS-CoV-2 and other pathogens: a systematic review and meta-analysis. PLoS One. 20216;16:e0251170. doi: 10.1371/journal.pone.0251170. [DOI] [PMC free article] [PubMed] [Google Scholar]