Abstract
Priority setting represents an even bigger challenge during public health emergencies than routine times. This is because such emergencies compete with routine programmes for the available health resources, strain health systems and shift health-care attention and resources towards containing the spread of the epidemic and treating those that fall seriously ill. This paper is part of a larger global study, the aim of which is to evaluate the degree to which national COVID-19 preparedness and response plans incorporated priority setting concepts. It provides important insights into what and how priority decisions were made in the context of a pandemic. Specifically, with a focus on a sample of 18 African countries’ pandemic plans, the paper aims to: (1) explore the degree to which the documented priority setting processes adhere to established quality indicators of effective priority setting and (2) examine if there is a relationship between the number of quality indicators present in the pandemic plans and the country’s economic context, health system and prior experiences with disease outbreaks. All the reviewed plans contained some aspects of expected priority setting processes but none of the national plans addressed all quality parameters. Most of the parameters were mentioned by less than 10 of the 18 country plans reviewed, and several plans identified one or two aspects of fair priority setting processes. Very few plans identified equity as a criterion for priority setting. Since the parameters are relevant to the quality of priority setting that is implemented during public health emergencies and most of the countries have pre-existing pandemic plans; it would be advisable that, for the future (if not already happening), countries consider priority setting as a critical part of their routine health emergency and disease outbreak plans. Such an approach would ensure that priority setting is integral to pandemic planning, response and recovery.
Keywords: Priority setting, equity, Africa region, COVID-19, national plans, effective priority setting
Key messages.
The COVID-19 pandemic has exemplified the critical need for explicit priority setting mechanisms.
If equity is considered, priority setting can mitigate the inequities that arise and are exacerbated during disease outbreaks.
If pandemic panning does not include priority setting and equity considerations, it is less likely that they are implemented during the pandemic.
Although most of the reviewed pandemic plans included some aspects of priority setting, very few explicitly included equity considerations.
Including parameters of high-quality priority setting and equity considerations in the plans will ensure that priority setting during the pandemic response is fair and equitable.
Introduction
Setting priorities for the use of limited resources, to meet competing health needs, challenges health policy makers globally (Mitton and Donaldson, 2004; Chalkidou et al., 2016; Terwindt et al., 2016). Priority setting represents an even bigger challenge during public health emergencies given public health emergencies compete with routine programmes for the available health resources, strain health systems and shift healthcare attention and resources towards containing the spread of the epidemic and treating those that fall seriously ill (Barnett et al., 2009; American Medical Association, 2021). Resource allocation decision-makers are often under heightened pressure to respond immediately, depending on the perceived or actual public health impact of the health emergency, which may result in inefficient resource use (Kapiriri and Be LaRose, 2019). In such pressing situations, the ‘rule of rescue’—the imperative to rescue identifiable individuals facing avoidable death and respond to the immediate threat to life—crowd out other less immediate priorities (Jonsen, 1986; Cookson et al., 2008; Moodley et al., 2013). In some instances, especially for deadly disease outbreaks, the mobilized resources may not benefit the populations most vulnerable to the outbreak (Kapiriri et al., 2021). Since priority setting has been recommended as a strategy to promote the effectiveness and fairness of resource allocation decisions, particularly in crisis situations when resources may be insufficient (Khan et al., 2018; Kapiriri and Be LaRose, 2019), it is necessary to explore the degree to which this priority setting occurs during public health emergencies.
The COVID-19 pandemic, which has affected countries throughout the world, provides a unique opportunity to examine and compare priority setting in pandemic planning across different jurisdictions, including different economic, political and health systems. The pandemic has made it necessary for policy makers and clinicians to make difficult decisions about competing interventions, populations and patient groups to prioritize for care, including ventilators, personal protective equipment (PPE), therapeutics and vaccines (Mitton et al., 2021). Although priority setting is crucial for pandemic preparedness and response and there is a growing body of literature on health system priority setting during normal times, there is limited empirical evidence regarding the extent to which priority setting is integrated in pandemic planning and the impact this integration might have on the response to the pandemic.
Much of the current literature on priority setting and resource allocation during COVID-19 has been primarily theoretical or focused on ethical considerations (Emanuel et al., 2020; Peterson et al., 2020; Wasserman et al., 2020; WHO, 2020).
This paper is part of a larger global study whose aim is to evaluate the degree to which national COVID-19 preparedness and response plans incorporated priority setting concepts. The global study includes a sample of over 60 countries from all six World Health Organization (WHO) regions. This paper offers a synthesis of how priority setting concepts were incorporated into COVID-19 preparedness plans in a variety of countries across the WHO-Africa (WHO-AFRO) region. Focusing on one region permitted some assumptions about shared characteristics and challenges faced by countries in the region: countries in the AFRO region had predominantly young populations, lack of universal health insurance and healthcare systems with limited human resources for health, hospitals, hospital beds, intensive care facilities and other high medical technologies (ventilators, dialysis and cardiac support measures) prior to the onset of the pandemic (Chu et al., 2020; Siedner et al., 2020; Wallace et al., 2020).
This paper provides important insights into what and how priority decisions were made in the context of a pandemic. Specifically, the paper aims to: (1) explore the degree to which the documented priority setting processes adhere to established quality indicators of effective priority setting and (2) examine if there is a relationship between the number of quality indicators present in the pandemic plans and the country’s economic context, health system and prior experiences with disease outbreaks.
Methods
Study approach
This was a mixed-methods study based on a review of COVID-19 planning documents (Bowen, 2009) and the COVID-19 morbidity and statistics. The document review provided information on the aspects of effective priority setting that were included in the pandemic plans, while the COVID-19 statistics provided evidence on the COVID-19 burden in the different countries.
Sampling of countries
Eighteen countries from the WHO-AFRO region were sampled for maximum variation with respect to: regional representation (Central, East, Southern and West), economic status (World Bank 2020–2021 country classification) (Serajuddin and Hamadeh, 2020; The World Bank, 2021), type of political (presidential republic, parliamentary republic or monarchy) and health system (public/private and universal/blended) and experiences with prior disease outbreaks (Table 1).
Table 1.
Priority setting context
| Economic level | Country | Geographical region | Political system | Health system financing (public, private and mixed) | UHC Service Coverage Index | Influenza plan (composite scores of preparedness plans by country) | Pre-COVID Plan | Experience with disease outbreaks |
|---|---|---|---|---|---|---|---|---|
| Low | Burkina Faso | West Africa | Presidential republic | Mixed public–private (donors) | 40 | 34% | Ebola, Influenza, SARS | Yes |
| Chad | Central Africa | Presidential republic, less stable | Mixed public–private (out-of-pocket and health insurance) | 28 | 11% | Polio, Influenza | Yes | |
| DR Congo | Central Africa | Semi-presidential republic, unstable | Non-universal insurance system | 41 | 46% | Ebola, Influenza | Yes | |
| Ethiopia | East Africa | Federal parliamentary republic | Non-universal insurance system | 39 | No | No | Yes | |
| Mali | West Africa | Semi-presidential republic | Mixed public–private (out-of-pocket and health insurance) | 38 | 20% | Influenza | Yes | |
| Mozambique | East Africa | Presidential republic | Mixed public–private (out-of-pocket and donors) | 46 | 27% | Influenza | Yes | |
| Niger | West Africa | Semi-presidential republic | Mixed public–private (out-of-pocket and donors) | 37 | 33% | Ebola, Influenza, Cholera | Yes | |
| Rwanda | East Africa | Presidential republic, stable | Mixed public–private (out-of-pocket, health insurance, and donors) | 57 | 30% | Influenza | Yes | |
| Uganda | East Africa | Presidential republic | Non-universal insurance system | 45 | 21% | Ebola, Influenza | Yes | |
| Lower-Middle | Algeria | North Africa | Presidential republic | Universal public–private insurance system | 78 | 35% | Influenza, H1N1, Ebola, Avian flu | Yes |
| Angola | Central Africa | Presidential republic, stable | Public–private | 40 | No | No | Yes | |
| Cameroon | Central Africa | Presidential republic, recent instability | Mixed public–private (out-of-pocket and community health insurance) | 46 | 60% | Ebola, Influenza | Yes | |
| Cape Verde | West Africa | Parliamentary republic | Social insurance | 69 | 30% | Ebola, Influenza | Yes | |
| Ghana | West Africa | Presidential republic | Social security and out-of-pocket | 47 | 50% | Influenza | Yes | |
| Kenya | East Africa | Presidential republic | Non-universal insurance system | 55 | 60% | Influenza | Yes | |
| Nigeria | West Africa | Federal presidential republic | Non-universal insurance system | 42 | 71% | Influenza, H1N1, Ebola | Yes | |
| Zambia | East Africa | Presidential republic, stable | Mixed public–private (out-of-pocket and donors) | 39 | No | Ebola | Yes | |
| Upper-Middle | South Africa | Southern Africa | Parliamentary republic, stable | Public health insurance and out-of-pocket and donors) | 69 | 79% | Influenza | Yes |
Document review
Document retrieval and review
Search strategy
A search strategy was developed by the research team to identify COVID-19 pandemic preparedness plans. Searches were conducted by two members of the research team. All searches were carried out between August and December 2020. First, they accessed the webpages of the ministries of health and official government websites for the selected countries from August to December 2020. The full list of websites consulted is available in Appendix 1. Second, they conducted searches in Google and Google Scholar to identify additional plans. In some cases, national pandemic plans were referenced but could not be located online. In such cases, the principle investigator (PI) contacted the respective health ministries and/or used the research team’s contacts within the respective countries, who shared the plans or directed us to where we could find the plans. We followed these steps until we had exhausted all leads. Where we were unable to identify or locate a plan, we added the label ‘missing plan’. This indicates that we were unable to access a relevant plan and that, to the authors’ knowledge, such documentation is not accessible in the public domain. We used native language speakers to screen and review any documents that were not written in the English language.
Inclusion and exclusion criteria
We aimed to identify national COVID-19 preparedness plans. In most cases, this was a single, general national COVID-19 response plan; in other instances, it was a health-specific COVID-19 response plan. Two researchers conducted an initial scan of the documents to ascertain their relevance. Documents that contained information on the mobilization and allocation of resources for health services were retained. Documents that focused on general government response (e.g. sustaining the economy) or other specific services (e.g. school closures) were excluded.
Data extraction
Two researchers conducted an initial scan of the documents to ascertain their relevance. Data extraction was guided by Kapiriri and Martin’s framework for assessing the quality of healthcare priority setting in low-income countries (Kapiriri and Martin, 2010). The quality parameters within the framework developed by Kapiriri and Martin were identified through a review of the literature on best practices in priority setting and interviews with priority setting experts. The framework was validated at the global level and has been used to evaluate priority setting in different health programmes, including disease outbreaks, in Uganda (Kapiriri, 2017). The framework is comprised of five domains: the priority setting context; prerequisites; the priority setting process; implementation and impact. Each domain includes several quality parameters, with a total of 26 across all domains. This framework provided a consistent standard against which sampled country pandemic plans were assessed.
In a prior project, a data extraction tool, based on the 20 quality indicators of effective priority setting, was developed and used to evaluate priority setting during disease outbreaks in Uganda (Kapiriri and Be LaRose, 2019). This formed the basis for the research team’s initial discussion of the data extraction tool. Based on the COVID-19 pandemic context, the research team identified four additional parameters, which were thought to be of specific relevance to priority setting during the COVID-19 pandemic. These included: level of resource scarcity, the resources identified, priority setting for health research and plan for continuity of care across the health system (See Additional file). The final tool was pilot tested by LK and SDR to extract data from one report. BE, IW and LK used the tool to extract data from the Uganda and South Africa plans. Their extraction was compared to SDR’s extraction to ensure consistency. Once consistency was established, the tool was used for the subsequent data extraction.
Before the synthesis of all the findings, MV independently reviewed and validated the extracted information against the original documents to ensure further consistency.
COVID-19 morbidity and mortality data
We used the Oxford COVID-19 Government Response Tracker (OxCGRT, 2020) to obtain the national COVID-19 morbidity distribution in the 18 countries. The statistics were obtained for a 1-year period (between March 2020 and April 2021).
Data analysis
Data analysis proceeded in three stages. First, we summarized all the abstracted information for each national plan. We then used the evaluation framework to assess the degree to which each of the national plans had incorporated the priority setting quality parameters. This provided an understanding of the aspects of priority setting considered within the different settings. Second, we conducted content analysis to understand and describe in more detail how each of the parameters was addressed in each plan, based on the available information; e.g. for stakeholder involvement, we described which stakeholders were identified and how they were engaged in the prioritization process. We also noted the existing gaps in the descriptions of the various parameters.
Third, we conducted a cross-country comparison. The purpose was to assess which country plans included the greatest number of parameters (dependent variables) and if this was associated with any of the independent variables, including the political system, social-economic context and type of healthcare and financing system and prior experience with disease outbreaks. A principal component analysis of Rasch residuals (PCAR; a technique that uses the dependencies between the variables to represent it in a more tractable, lower-dimensional form, without losing too much information) was performed (Mair, 2018; Boone and Staver, 2020). PCAR is one of the most robust ways of doing such dimensionality reduction. The aim of the factor analysis of Rasch residuals is thus to attempt to extract the common factor that explains the most residual variance under the hypothesis that there is such a factor (Mair, 2018; Boone and Staver, 2020).
Results
A total of 18 national COVID-19 plans were retrieved (about 40% of all WHO-AFRO countries). Of these, 16 were publicly available, and 2 were acquired through the research team’s contacts. All documents were published between February 2020 and August 2020. The sample included nine low-income countries (i.e. Burkina Faso, Chad, Democratic Republic of the Congo, Ethiopia, Mali, Mozambique, Niger, Rwanda and Uganda), eight low-middle-income countries (i.e. Algeria, Angola, Cameroon, Cape Verde, Ghana, Kenya, Nigeria and Zambia) and one upper-middle-income country (i.e. South Africa). The countries were at different stages of the COVID-19 pandemic (Figure 1) at the time of retrieval.
Figure 1.
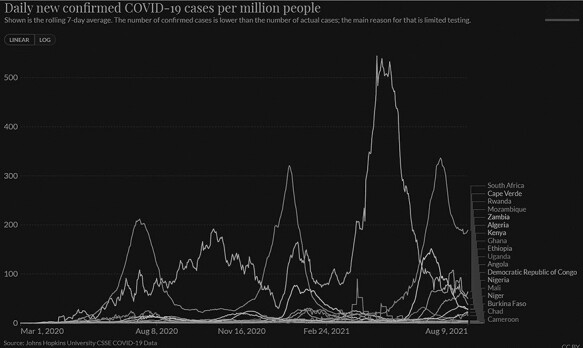
Total confirmed cases per million people
The rest of the results section is organized according to the five domains of priority setting, as identified in the framework, namely priority setting context, pre-requisites, priority setting process, implementation and outcomes/impact. For each domain, and related parameters, we describe how each country addressed the parameters in their plans and then describe the results of the cross-country comparison of the relationship between priority setting and the country contexts (including economic, political and health systems).
Priority setting contexts
Contextual factors, as defined by the framework, include the social-economic, cultural and political contexts of priority setting. Depending on the health issue, additional relevant contextual factors may include the physical environment, geographical and epidemiological factors (Table 1). While these are relevant to the kind of priority setting processes that may be feasible in different contexts, the reviewed documents did not contain information on the context. However, all documents were developed within the context of a global pandemic and this, among other contextual factors, influenced the planned activities, including priority setting.
Prerequisites
The framework identifies three parameters within this domain: presence of political will, availability of a legitimate priority setting institution and human and financial resources.
In relation to political will, the presence of a COVID-19 response plan, which, in many cases, was developed with the government’s support, was a strong indicator of political will. This is further supported by the fact that half of the sampled countries established inter-ministerial, multisectoral COVID-19 task forces (i.e. Angola, Cape Verde, Ghana, Kenya, Mozambique, Nigeria, Rwanda and Uganda), which would have not been possible without political will and support.
Considering the legitimacy and capacity of the priority setting institutions parameter, all sampled documents identified either a national task force or some form of co-ordinating committee responsible for COVID-19 planning. Many of these were based on the institutional legacy of previous coordination structures established to respond to prior outbreaks or public emergencies, e.g. the Ebola virus disease (EVD) outbreak structures and plans in Uganda and the pandemic influenza plans in Nigeria and Ethiopia. Based on their designations, the committee members seemed to have been appointed based on their technical expertise. The plans did not present any information on the stakeholders or the public opinions regarding their confidence in or the legitimacy of these institutions. We considered that since they comprise experts, those coordination structures might be appropriate to set priorities in the COVID-19 pandemic and plan for the maintenance of the routine services.
The resources parameter assesses the availability of financial, material and human resources to implement the identified priorities. Most plans (13/18), however, identified a general lack of these resources, for instance, health system infrastructure [e.g. low coverage of health services (i.e. Angola, Ghana and Mozambique) and limited response capacity of local teams (i.e. Angola and Mozambique)].
All 18 plans discussed resources relevant to COVID-19, identifying PPE and other infection prevention and control (IPC) materials, as well as the need for laboratory equipment and specimen transportation. Some of the plans also discussed the resource scarcity of healthcare facilities (six countries), insufficient ICU beds and life support equipment (five countries), lack of PPE and other IPC materials (four countries), low testing capacity (three countries) and insufficient medicines/supplies (three countries).
Notably, while all the reviewed national plans identified human resources and their training as essential for the response to the COVID-19 pandemic, 6 out of 18 countries specified a lack of trained human resources. Furthermore, while half the plans had a detailed budget and inventory for the required resources, only two countries identified life support equipment, ambulances, medical equipment and vaccines among the identified resources (Table 2: Identified resource scarcities).
Table 2.
Parameters found in the plans
| Country | Burkina Faso | Chad | DR Congo | Ethiopia | Mali | Mozambique | Niger | Rwanda | Uganda | Algeria | Angola | Cameroon | Cape Verde | Ghana | Kenya | Nigeria | Zambia | South Africa | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prerequisites | Political will | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 18 |
| Resources | Y | N | Y | N | N | N | N | Y | Y | N | Y | N | N | Y | Y | Y | N | Y | 9 | |
| Legitimate institutions | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | 15 | |
| Incentives for compliance | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | 0 | |
| The priority setting process | Stakeholder participation | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 18 |
| Clear priority setting process/tools | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | 0 | |
| Explicit priority setting criteria | N | N | N | Y | Y | Y | N | N | Y | Y | Y | N | N | Y | N | N | N | N | 7 | |
| Use of evidence | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 17 | |
| Reflection of public values | N | N | N | N | Y | N | N | N | N | N | N | N | N | N | N | N | N | N | 1 | |
| Publicity of priorities | N | N | N | N | N | N | N | N | N | N | Y | N | N | N | N | N | N | Y | 2 | |
| Mechanisms for appealing the decision | N | N | N | Y | Y | Y | N | N | Y | N | Y | N | Y | N | N | Y | N | Y | 8 | |
| Mechanisms for enforcement decisions | N | N | N | N | N | N | N | N | Y | N | Y | N | N | Y | N | Y | Y | Y | 6 | |
| Implementation of the set priorities | Allocation of resources according to priorities | N | Y | Y | N | Y | N | Y | Y | Y | N | Y | N | N | Y | Y | Y | N | N | 10 |
| Improved internal accountability | N | Y | Y | N | N | Y | N | N | N | N | Y | N | N | Y | N | N | N | Y | 6 | |
| Priority setting impact | Impact on swiftness | N | N | N | N | N | Y | N | N | Y | N | Y | N | Y | Y | N | Y | N | Y | 7 |
| Impact on population health | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | 0 | |
| Impact on reducing inequalities | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | 0 | |
| Fair financial contribution | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | 0 | |
| Increased public confidence in the health sector | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N | 0 | |
| Plan for continuity | N | N | N | Y | N | N | N | Y | Y | N | N | N | Y | Y | Y | Y | Y | N | 8 | |
| Number of criteria accomplished (of 20) | 5 | 6 | 7 | 7 | 6 | 8 | 5 | 6 | 11 | 5 | 12 | 4 | 7 | 11 | 6 | 10 | 6 | 10 |
Critical to pandemic planning is the need to maintain routine essential services. We assessed the degree to which the plans included strategies to sustain the country’s routine health programmes. Of the 18 plans, 8 included plans for sustaining essential services. Identified essential services included maternal and child health, HIV treatment and chronic diseases.
None of the reviewed plans specified incentives and/or mechanisms to ensure compliance with the stipulated priority setting plans.
The priority setting process
This domain assesses several aspects of the PS process, including whether it used an explicit guiding tool/method/framework or evidence and the articulated priority setting (PS) criteria (including equity considerations). Furthermore, the process domain emphasizes the need for stakeholder involvement. Although none of the plans presented clear priority setting process/tool/methods, several were based on the WHO recommended strategy of planning according to three pandemic phases and four scenarios—which do not incorporate priority setting (Kapiriri et al., 2021).
In relation to stakeholder participation, many plans identified inter-sectoral committees led by Ministries of Health. Commonly identified sectors included agriculture, environment, trade and industry, education, information and finance. Additional stakeholders included the national police, religious and traditional organizations (as public representatives), international development partners (e.g. the WHO, Africa Centres for Disease Control and Prevention, UNICEF, Save the Children, Red Cross and the World Bank) and the private sector. A couple of countries mentioned the participation of universities, for instance, Addis Ababa University (Ethiopia), Washington State University and Makerere University (Uganda).
The use of evidence is important to credible prioritization. All the country plans were in some way (and to varying extents) evidence informed. The sources of evidence included WHO pandemic planning guidelines and past pandemic plans (e.g. Ebola plans and influenza). An additional source of evidence was the legacy of past pandemic’s experience (in Algeria, Cameroon, DR Congo, Niger, Nigeria, Uganda and Zambia).
An additional parameter is the use of explicit criteria and principles. Five countries articulated explicit priority setting principles and/or criteria in their national COVID-19 plans. For example, Algeria’s plan identified three principles: ‘evolutivity’ (reflecting on the emerging nature of the pandemic); flexibility (which allows for readjustments based on the pandemic evolution) and adaptability. There were similarities and variations between these five countries when the explicit criteria were analysed. First, all these plans identified disease-related criteria, including risk, transmissibility and severity of the disease. Additional criteria that were mentioned in a single national plan included disease burden and population density (Ghana) and capacity to respond (Uganda) (Table 3).
Table 3.
Resource gaps identified
| Income | Country | Human resources and training | PPE and other IPC materials | Lab equipment | Healthcare facilities | Financial resources | Testing kits | Essential medicines | Ambulances | Medical equipment | ICU beds | Life support equipment | Vaccines |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low-income | Burkina Faso | x | x | ||||||||||
| Tchad | x | x | x | x | |||||||||
| RD Congo | x | x | x | x | x | x | |||||||
| Ethiopia | x | x | x | x | x | ||||||||
| Mali | x | x | x | x | |||||||||
| Mozambique | x | x | x | x | x | x | |||||||
| Niger | x | x | x | x | x | ||||||||
| Rwanda | x | x | x | x | x | x | x | ||||||
| Uganda | x | x | x | x | x | x | x | x | x | ||||
| Lower middle | Algeria | x | x | x | x | ||||||||
| Angola | x | x | x | x | |||||||||
| Cameroun | x | x | x | x | x | ||||||||
| Cape Verde | x | x | x | x | x | x | |||||||
| Ghana | x | x | x | x | x | ||||||||
| Kenya | x | x | x | x | x | x | |||||||
| Nigeria | x | x | x | x | x | x | x | x | x | ||||
| Zambia | x | x | x | x | x | x | x | ||||||
| Upper middle | South Africa | x | x | x | x | x |
Of the 18 plans that were reviewed, only three countries (Algeria, Ethiopia and Mali) explicitly stated that they considered people’s culture and background (further discussed below).
Equity considerations were assessed along two dimensions (1) whether the plans identified equity as a consideration and if they further identified the vulnerable populations that should be prioritized; (2) if the plans considered the need to ensure the sustenance of routine essential services (especially those most accessed by the vulnerable populations).
Although most of the plans did not explicitly name equity as a prioritization criterion, several plans identified various vulnerable populations that should be prioritized for the COVID-19 interventions. Eight plans (Ethiopia, Mozambique, Rwanda, Uganda, Angola, Cape Verde, Nigeria and Zambia) identified priority populations based on different considerations. For example, the elderly, people with pre-existing illnesses and people living with HIV were identified as priority populations for COVID-19 interventions due to their high risk to severe disease, while cross border travellers and health workers were prioritized by virtue of their occupations and risk of spreading COVID-19 (Table 4).
Table 4.
Prioritized population groups
| Income | Low income | Lower middle | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Ethiopia | Mozambique | Rwanda | Uganda | Angola | Cape Verde | Nigeria | Zambia | ||
| GINI coefficient | 35 | 54 | 43.7 | 42.8 | 42.7 | 47.2 | 43 | 57.1 | |
| Prioritization rationale | Prioritized populations | ||||||||
| Prioritized for continuity of services | Pregnant women | x | x | x | x | x | |||
| Young infants | x | x | x | ||||||
| People in need of sexual and reproductive services | x | ||||||||
| People with pre-existing illnesses | x | x | x | ||||||
| People with HIV | x | x | |||||||
| Prioritized given their vulnerability | Immigrants | x | x | ||||||
| Ethnic groups | x | ||||||||
| Population in rural areas | x | x | |||||||
| Refugees/internal displaced | x | x | |||||||
| Sexual and gender minorities | x | ||||||||
| People with disabilities | x | ||||||||
| Homeless population | x | ||||||||
| Inmates | x | ||||||||
| Prioritized given their risk of transmission | Travellers | x | x | x | x | x | x | ||
| Healthcare workers | x | x | x | x | x | ||||
| Prioritized given the greatest risk of seriously ill | Elderly | x | x | x | |||||
| People immune compromised | x | ||||||||
Only seven plans identified additional vulnerable populations and/or regions, and only two plans (Uganda and Zambia) explicitly prioritized such populations in relationship to COVID-19 planning. The vulnerable populations included immigrants, ethnic groups, populations in rural areas, refugees/internal displaced persons, sexual and gender minorities, people with disabilities, homeless population, inmates, the elderly and people who were immune compromised. Four plans (Angola, Cape Verde, Mozambique and Uganda) identified geographically vulnerable regions—often entry points for infected travellers. Only the Ghana plan prioritized geographical regions according to need, which was defined according to case burden, population density, rate of spread and potential for further spread.
We also sought to understand the extent to which plans were able to strike the delicate balance between responding to the COVID-19 pandemic and ensuring that essential services for vulnerable populations do not get disrupted. For example, pregnant women, children and people in need of sexual and reproductive services were identified as priority groups for service continuity in almost all national plans that identified health systems continuity as an important intervention. Additional populations that were identified in this regard included people living with chronic illnesses, including those living with HIV.
In addition to priority setting criteria, the framework requires that the decisions and their rationales also be publicized and that there should be appeals, revisions and enforcement mechanisms. While two plans included a section on communication, this was oriented to health education rather than publicizing the priorities or criteria. However, since we accessed all but two plans online, one can conclude that those plans are publicly available. While there were no clear appeals and revision mechanisms, nine plans (Angola, Cape Verde, Ethiopia, Mali, Mozambique, Nigeria, South Africa, Uganda and Zambia) mentioned that the established commissions/task forces would periodically review additional emerging national and/or international evidence and use it to revise their plans and activities.
Plans for enforcement (referring to the degree to which the prioritization process adheres to the conditions for a fair process) were not explicitly mentioned in any of the plans. However, the plans discussed mechanisms for supporting pandemic governance, coordination and accountability (Ghana and Uganda). Some of the plans (Angola, Nigerian and Zambia) mentioned enforcement in relationship to ensuring safety and quality control in health facilities as opposed to governance.
Implementation of the set priorities
It was beyond the scope of the plans to include implementation of the set priorities and their subsequent impact. While the plans included budget estimates, four national plans (Angola, Chad, Ghana and Mozambique) talked about aiming to improve internal accountability/reduced corruption by supporting transparency in the management of resources and accountability.
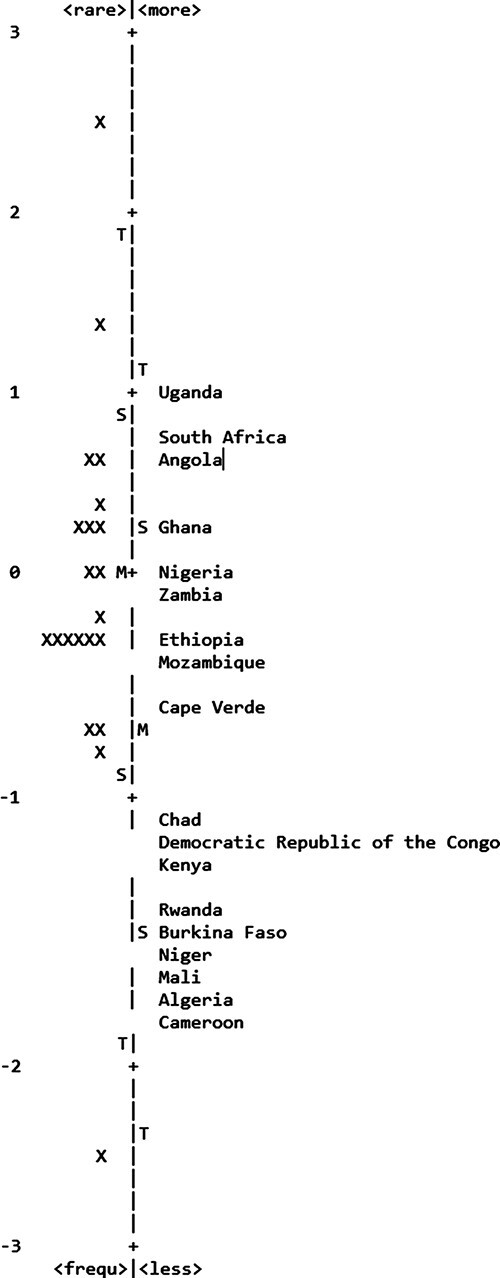
Cross country comparison
The PCAR enabled us to identify patterns between countries in relationship to the number of parameters their plans contained. Based on this analysis, three groups of countries were identified. The first group included countries whose plans had the highest number of parameters. These included: Uganda; South Africa; Angola and Ghana. The second group included most of the parameters but not as many as those in the first group. This group included Nigeria, Zambia, Ethiopia, Mozambique and Cape Verde. The third group, which included Chad, Democratic Republic of the Congo, Kenya, Rwanda, Burkina Faso, Niger, Mali, Algeria and Cameroon, lacked most of the parameters, including those associated with high-quality priority setting processes as per the evaluation framework.
All country groupings contained both high-middle-income and middle- and low-income countries with mixed health systems and variations in universal healthcare systems. However, all the countries in the first group have prior experience with national-level priority setting (and priority setting for health research) and only Uganda has prior serious disease outbreak experience. Countries in Group 2 are also mixed, with Ethiopia and Zambia having prior national priority setting and Universal Health Coverage (UHC) experiences. The third group of countries is also mixed but contains most of the lower-income countries, with limited documented national level health system priority setting. In this group, only the Democratic republic of Congo (DRC) has had prior disease outbreak experiences (Figure 2).
Figure 2.
Map of countries and items of priority setting
Discussion
We discuss five key issues that emerged from the results: the quality parameters found in the national plans and their associations with the country’s context; parameters that were common in all plans; the identified resource needs; the priority setting criteria and equity considerations and sustenance of essential services.
The parameters found in the national plans and their associations
While all the reviewed plans contained some aspects of priority setting, the number of quality indicators addressed in the different plans varied, with none of the national plans addressing all 20 quality parameters. The PCAR analysis exemplified the lack of a clear association between the independent variables: political system, economic status, health financing system and prior experience with disease outbreaks and the number of quality parameters. Most of the parameters were mentioned by less than 10 of the 18 country plans reviewed, and several plans identified one or two aspects of fair priority setting processes (Daniels and Sabin, 2008). These findings indicate that the stakeholders involved in the COVID-19 pandemic planning were aware of the need for including aspects of priority setting in their pandemic planning, although the plans did not cover all the quality indicators. This could be explained by the evolving nature of the pandemic, whereby many countries continued to develop guidance documents throughout the course of the pandemic. It is possible that other information relevant to some of the parameters is contained in other documents that were not reviewed. Conversely, the findings can also be explained by the number of quality parameters (20)—which may be too many to meaningfully include in plans that were developed during emergency contexts. Given that the parameters are relevant to the quality of priority setting that is implemented during public health emergencies and that most of the countries have pre-existing pandemic plans, it would be advisable that (if not already happening) countries consider priority setting as a critical part of their routine health emergency and disease outbreak plans. For example, based on the WHO four stages of pandemic planning, Kapiriri, Essue, et al. (Forthcoming) have proposed ways through which planners using the WHO framework could integrate priority setting in the four stages of their pandemic plans (Kapiriri et al., 2021). Such an approach would ensure that priority setting is integral to pandemic planning, response and recovery.
Parameters that were common to all national plans
The reviewed plans mentioned at least 4 of the 20 quality parameters in their plans. However, four parameters were common in all the reviewed plans. These included political will, legitimate institutions, broad stakeholder involvement and use of evidence. Possibly, due to the multi-sectoral nature of the COVID-19 pandemic, most of the national COVID-19 planning and coordinating mechanisms involved a broad spectrum of strategic stakeholders in addition to the technocrats, e.g. media communication, universities evidence, civil society organizations and human resources private sector-diverse resources from food, transport, hotel space and medicines/supplies. Broad stakeholder engagement was one of the most commonly discussed quality indicators. While the plans reflected multi-sectoral planning, it is important to note that there was limited mention of public engagement or any mechanisms to elicit public values. While meaningful broad stakeholder engagement can improve the quality of the priority setting decisions, limited reflection of meaningful public engagement or eliciting and considering of public values may negatively impact the acceptance of the priority setting decisions, which is relevant to the COVID-19 pandemic (Bruni et al., 2008; Mitton et al., 2009; Razavi et al., 2020).
While the priority setting literature discusses legitimate priority setting institutions, stakeholder engagement and the use of evidence as indicators of high-quality priority setting (Kapiriri and Norheim, 2004; Baltussen and Niessen, 2006; Hall et al., 2018), political will is often controversial, with some of the literature supporting it as a quality indicator and some negating its value. This is an anomaly since the priority setting literature recognizes that, as opposed to being an exclusively technical process, priority setting is a political process, requiring political will to succeed (Smith et al., 2014). Since public health emergencies (depending on their reach and severity) are often politicized, priority setting during public health emergencies tends to be political and politicized (Reichenbach, 2002; Kapiriri et al., 2007; Smith et al., 2014; Kapiriri and Be LaRose, 2019). It may, hence, not be surprising that all the reviewed plans had clear indications of high political support. Furthermore, since COVID-19 was labelled a global pandemic, it necessitated political action and may have also augmented the political will (Guest et al., 2020).
Resource needs
Most of the reviewed plans linked priority setting to resource availability or scarcity. The finding that all plans identified the need for trained personnel, PPE and other IPC to address the pandemic was not surprising. The region has been plagued with a lack of trained human resources (Africa, W. R. O., 2007; Moosa et al., 2014; Omer Elkhalifa, 2014; Willcox et al., 2015), as well as quality health infrastructure (including lab diagnostics) to deliver routine services (Petti et al., 2006; Hsia et al., 2012). Since health emergencies tend to highlight pre-existing health systems weaknesses and inequities (Birn et al., 2017), this is an expected finding. It was, however, surprising to find that only two countries identified life support equipment and vaccines. For the latter, it is possible that the plans were developed earlier in the pandemic when most countries, especially those within the WHO-AFRO region, could not imagine having access to a vaccine that was just in its initial stages of development, hence the tendency to focus on the more immediate scarcity issues identified above. It is difficult to explain why most of the plans did not contain information about life support equipment. We can, however, speculate that this could be linked to the limited personnel or lack of skilled personnel required to manage life support equipment. Conversely, the stakeholders may have thought about what would be realistic and achievable based on their local realities. Priority setting research in this region has sometimes been described as a process with many unfunded priorities (Essue and Kapiriri, 2018), whereby many items on even the routine ministry of health list, although prioritized, are never funded. Many policy makers and development assistance partners have argued that technocrats must make the difficult choices, recognizing the resource limitations and their inability to fund every item on the priority list (Kapiriri, 2012; Essue and Kapiriri, 2018; Razavi et al., 2019). The policy makers may have been realistic about which interventions may be feasible and de-prioritized those that may be perceived to be ‘out of reach’.
Priority setting criteria and equity considerations
Explicit prioritization tools and criteria are important to high-quality priority setting (Sibbald et al., 2010; Chalkidou et al., 2016; Kapiriri, 2017). While all the reviewed plans did not articulate a priority setting approach, they employed several identified explicit criteria for prioritizing different population groups (some for service continuity, and others for their vulnerability to COVID-19). The identified vulnerable groups, e.g. those with pre-existing conditions and the elderly, were consistent with those identified in the COVID-19 pandemic literature e.g. in terms of the population’s initial level of well-being, the degree of exposure to risk and their capacity to manage risk effectively in the context of the COVID-19 pandemic (Lancet, 2020; Scott and Beach, 2020). While we had expected there to be some alignment between the country’s general equity index (based on the GINI coefficient) and their inclusion of equity considerations within their plans, there was alignment with Zambia but not with the other countries, although all the countries that integrated some equity considerations all had a GINI coefficient above 40.
Sustenance of essential services
The ‘knee jerk’ resource reallocation response to disease epidemic has been found to be detrimental to essential health programmes as exemplified by a Uganda case study of priority setting during the EVD outbreak (Kapiriri and Be LaRose, 2019). The resource reallocation that tends to be prevalent during disease outbreaks involves e.g. budget reallocations, shifting of human resources, postponing of surgeries and other ‘nonurgent’ procedures. This occurs because of lack of planning for the sustenance of essential programmes during a pandemic and unfortunately results in loss of lives and increased morbidities as has been witnessed during the COVID-19 outbreak. Hence, although it was not included in the original framework as a parameter, plans for the sustenance of essential services emerged as a relevant parameter for evaluating priority setting during disease outbreaks, which most of the national plans lacked.
Limitations
This study was based on a review of the publicly available COVID-19 plans. We recognize that this approach, while it provides a synthesis of priority setting within the plans, is not devoid of limitations. First, the approach we used to access the documents—mainly from online sources—may have had implications for the completeness of the documents we reviewed, since some of the documents may not have been made available in the public domain. Second, even in the cases where we accessed a complete plan, the evolving nature of the pandemic meant that many countries continued to update and produce additional documents—our search was confined to the documents that supported the initial phase of the pandemic. Third, the intention is to understand the impact of priority setting on pandemic planning and response. While we could use proxy indicators to assess the impact, it is not possible, based on a document review, to credibly evaluate impact. We are cognizant that it is not uncommon to find very well-written plans that are never implemented. Assessment of the degree to which the plans are implemented would require systematic examination, involving consideration of the concurrent contextual factors that can explain the impact. Such an examination is amenable to interviews, and observations of actual implementation are being planned for a subsequent stage of the study.
Conclusions
Based on a review of a sample of national COVID-19 plans, we have assessed the degree to which the plans included aspects associated with effective priority setting. While all the reviewed plans had included some of these, none included all the quality parameters. The number of parameters included in the different plans was not associated with the kind of health or political system, socio-economic status or prior experience with a disease outbreak.
The importance of priority setting during pandemics and the political and politicized nature of priority setting during public health emergencies supports the need for routine inclusion of priority setting in all stages of pandemic planning to ensure that the agreed-on contextualized set of quality indicators are considered (Kapiriri, 2017). As the saying goes, ‘…if you fail to plan, you plan to fail…’. The inclusion of quality parameters and plans for sustaining essential health programmes in the pandemic planning is a first step in ensuring that, once a public health response is underway, the plans are readily available for implementation. This will support prioritization processes that are participatory, fair and equitable.
The framework enabled us to conduct this comparative analysis; however, in addition to the existing quality parameters, planning for sustenance of essential health programmes emerged as a critical parameter that should be added to the framework when used to evaluate priority setting during public health emergencies.
Since this study was based entirely on review of the plans, future research should focus on understanding the degree to which what was planned was implemented (identifying the contextual facilitators and barriers) and the resulting impact this had in terms of the number of COVID-19 cases, mortality and equity. Comparative analysis of such experiences across jurisdictions will facilitate the identification of key lessons that can be shared to support the ongoing preparedness planning as the pandemic continues into subsequent waves and to strengthen the role of priority setting during future health emergencies.
Appendix 1.
Reviewed documents by country
Contributor Information
Lydia Kapiriri, Department of Health, Aging & Society, McMaster University, 1280 Main Street West, Kenneth Taylor Hall Room 226, Hamilton, Ontario L8S 4M4, Canada.
Suzanne Kiwanuka, Department of Health Policy, Planning and Management, School of Public Health, College of Health Sciences, Makerere University, Upper Mulago Hill Road PO Box 7072, Kampala, Uganda.
Godfrey Biemba, National Health Research Authority, Pediatric Centre of Excellence, PO Box 30075, Lusaka, Zambia.
Claudia Velez, Department of Health, Aging & Society, McMaster University, 1280 Main Street West, Kenneth Taylor Hall Room 226, Hamilton, Ontario L8S 4M4, Canada.
S Donya Razavi, Department of Health, Aging & Society, McMaster University, 1280 Main Street West, Kenneth Taylor Hall Room 226, Hamilton, Ontario L8S 4M4, Canada.
Julia Abelson, Department Health Research Methods, Evidence, and Impact, McMaster University, 1280 Main Street West, Communications Research Building, 2nd Floor, Hamilton, Ontario L8S 4K1, Canada.
Beverley M Essue, Centre for Global Health Research, St. Michael’s Hospital, 30 Bond Street, Toronto, Ontario M5B 1W8, Canada.
Marion Danis, Department of Bioethics, National Institutes of Health, 9000 Rockville Pike, Bethesda, MD 20812, USA.
Susan Goold, Center for Bioethics and Social Sciences in Medicine, University of Michigan Medical School, 2800 Plymouth Road Building 14, G016, Ann Arbor, MI 48109, USA.
Mariam Noorulhuda, Department of Health, Aging & Society, McMaster University, 1280 Main Street West, Kenneth Taylor Hall Room 226, Hamilton, Ontario L8S 4M4, Canada.
Elysee Nouvet, School of Health Studies, Western University, 1151 Richmond Street, London, Ontario N6A 3K7, Canada.
Lars Sandman, National Centre for Priorities in Health, Department of Health, Medicine and Caring Sciences, Linköping University, Linköping, Sweden.
Iestyn Williams, Health Services Management Centre, University of Birmingham, 40 Edgbaston Park Road, Birmingham B15 2RT, UK.
Data availability statement
The data underlying this article are available in the article and in its online supplementary material.
Funding
This project was funded by the McMaster University COVID-19 research fund.
Ethical approval.
Ethical approval for this type of study is not required by our institute.
Conflict of interest statement.
The authors declare no conflict to declare.
References
- Africa, W. R. O . 2007. Crisis in Human Resources for health in the African Region. African Health Monitor 7: 15–21. [Google Scholar]
- American Medical Association . 2021. Prioritizing the Rest of Healthcare in a Public Health Crisis. https://www.ama-assn.org/delivering-care/ethics/prioritizing-rest-health-care-public-health-crisis, accessed 28 April 2021.
- Baltussen R, Niessen L. 2006. Priority setting of health interventions: the need for multi-criteria decision analysis. Cost Effectiveness and Resource Allocation 4: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett DJ, Taylor HA, Hodge JG. et al. 2009. Resource allocation on the frontlines of public health preparedness and response: report of a summit on legal and ethical issues. Public Health Reports 124: 295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birn A-E, Pillay Y, Holtz TH. 2017. Textbook of Global Health. 4th edn. New York: Oxford University Press. [Google Scholar]
- Boone WJ, Staver JR. 2020. Principal Component Analysis of Residuals (PCAR). In: Advances in Rasch Analyses in the Human Sciences. Cham: Springer, 1–24. [Google Scholar]
- Bowen GA. 2009. Document analysis as a qualitative research method. Qualitative Research Journal 9: 27–40. [Google Scholar]
- Bruni RA, Laupacis A, Martin DK. 2008. Public engagement in setting priorities in health care. Canadian Medical Association Journal 179: 15–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalkidou K, Glassman A, Marten R. et al. 2016. Priority-setting for achieving universal health coverage. Bulletin of the World Health Organization 94: 462–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu K, Reddy CL, Makasa E. 2020. The collateral damage of the COVID-19 pandemic on surgical health care in Sub-Saharan Africa. Journal of Global Health 10: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cookson R, McCabe C, Tsuchiya A. 2008. Public healthcare resource allocation and the Rule of Rescue. Journal of Medical Ethics 34: 540–4. [DOI] [PubMed] [Google Scholar]
- Daniels N, Sabin J. 2008. Setting Limits Fairly: Learning to Share Resources for Health. 2nd edn. New York, Oxford: Oxford University Press. [Google Scholar]
- Emanuel EJ, Persad G, Upshur R. et al. 2020. Fair allocation of scarce medical resources in the time of Covid-19. The New England Journal of Medicine 382: 2049–55.doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- Essue BM, Kapiriri L. 2018. The unfunded priorities: an evaluation of priority setting for noncommunicable disease control in Uganda. Globalization and Health 14: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guest JL, del Rio C, Sanchez T. 2020. The three steps needed to end the COVID-19 pandemic: bold public health leadership, rapid innovations, and courageous political will. JMIR Public Health and Surveillance 6: e19043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, Williams I, Smith N. et al. 2018. Past, present and future challenges in health care priority setting: findings from an international expert survey. Journal of Health Organization and Management 32: 444–62. [DOI] [PubMed] [Google Scholar]
- Hsia RY, Mbembati NA, Macfarlane S. et al. 2012. Access to emergency and surgical care in sub-Saharan Africa: the infrastructure gap. Health Policy and Planning 27: 234–44. [DOI] [PubMed] [Google Scholar]
- Jonsen AR. 1986. 3. Bentham in a box: technology assessment and health care allocation. The Journal of Law, Medicine & Ethics 14: 172–4. [DOI] [PubMed] [Google Scholar]
- Kapiriri L. 2012. Priority setting in low income countries: the roles and legitimacy of development assistance partners. Public Health Ethics 5: 67–80. [Google Scholar]
- Kapiriri L. 2017. International validation of quality indicators for evaluating priority setting in low income countries: process and key lessons. BMC Health Services Research 17: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapiriri L, Essue B, Bwire G. et al. 2021. A framework to support the integration of priority setting in the preparedness, alert, control and evaluation stages of a disease pandemic. Global Public Health. 10.1080/17441692.2021.1931402. [DOI] [PubMed] [Google Scholar]
- Kapiriri L, Be LaRose L. 2019. Priority setting for disease outbreaks in Uganda: a case study evaluating the process. Global Public Health 14: 241–53. [DOI] [PubMed] [Google Scholar]
- Kapiriri L, Martin DK. 2010. Successful priority setting in low and middle income countries: a framework for evaluation. Health Care Analysis 18: 129–47. [DOI] [PubMed] [Google Scholar]
- Kapiriri L, Norheim OF. 2004. Criteria for priority-setting in health care in Uganda: exploration of stakeholders’ values. Bulletin of the World Health Organization 82: 172–9. [PMC free article] [PubMed] [Google Scholar]
- Kapiriri L, Norheim OF, Martin DK. 2007. Priority setting at the micro-, meso- and macro-levels in Canada, Norway and Uganda. Health Policy 82: 78–94. [DOI] [PubMed] [Google Scholar]
- Khan Y, O’Sullivan T, Brown A. et al. 2018. Public health emergency preparedness: a framework to promote resilience 11 medical and health sciences 1117 public health and health services. BMC Public Health 18: 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancet T. 2020. Redefining vulnerability in the era of COVID-19. The Lancet 395: 1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair P. 2018. Item response theory. In: Modern Psychometrics with R. Springer International Publishing AG, 95–160.doi: 10.1080/00401706.2019.1708675. [DOI] [Google Scholar]
- Mitton C, Donaldson C, Dionne F, Peacock S. 2021. Addressing prioritization in healthcare amidst a global pandemic. Healthcare Management Forum 34: 252–5.doi: 10.1177/08404704211002539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitton C, Donaldson C. 2004. Health care priority setting: principles, practice and challenges. Cost Effectiveness and Resource Allocation 2: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitton C, Smith N, Peacock S. et al. 2009. Public participation in health care priority setting: a scoping review. Health Policy 91: 219–28. [DOI] [PubMed] [Google Scholar]
- Moodley K, Hardie K, Selgelid MJ. et al. 2013. Ethical considerations for vaccination programmes in acute humanitarian emergencies. Bulletin of the World Health Organization 91: 290–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moosa S, Downing R, Essuman A. et al. 2014. African leaders’ views on critical human resource issues for the implementation of family medicine in Africa. Human Resources for Health 12: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omer Elkhalifa G. 2014. The current crisis in human resources for health in Africa. South Sudan Medical Journal 7: 3–4. [Google Scholar]
- Oxford : The Oxford Covid-19 government response tracker (OxCGRT). 2020. https://covidtracker.bsg.ox.ac.uk/stringency-scatter, accessed20 June 2021.
- Peterson A, Largent EA, Karlawish J. 2020. Ethics of reallocating ventilators in the covid-19 pandemic. The BMJ 369: 10–3. [DOI] [PubMed] [Google Scholar]
- Petti CA, Polage CR, Quinn TC. et al. 2006. Laboratory medicine in Africa: a barrier to effective health care. Clinical Infectious Diseases 42: 377–82. [DOI] [PubMed] [Google Scholar]
- Razavi SD, Kapiriri L, Abelson J, Wilson M. 2020. Barriers to equitable public participation in health-system priority setting within the context of decentralization: the case of vulnerable women in a Ugandan District. International Journal of Health Policy and Management. 10.34172/ijhpm.2020.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razavi SD, Kapiriri L, Abelson J. et al. 2019. Who is in and who is out? A qualitative analysis of stakeholder participation in priority setting for health in three districts in Uganda. Health Policy and Planning 34: 358–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichenbach L. 2002. The politics of priority setting for reproductive of priority the politics health: setting cancer in Ghana breast and cervical. Reproductive Health Matters 10: 47–58. [DOI] [PubMed] [Google Scholar]
- Scott BD, Beach EDTM. 2020. The Covid-19 risks for different age groups, explained. 1–11. [Google Scholar]
- Serajuddin U, Hamadeh N. 2020. New World Bank Country Classifications by Income Level: 2020-2021, World Bank Blogs. https://blogs.worldbank.org/opendata/new-world-bank-country-classifications-income-level-2020-2021, accessed 28 April 2021.
- Sibbald SL, Gibson JL, Singer PA. et al. 2010. Evaluating priority setting success in healthcare: a pilot study. BMC Health Services Research 10: 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siedner MJ, Kraemer JD, Meyer MJ. et al. 2020. Access to primary healthcare during lockdown measures for COVID-19 in rural South Africa: an interrupted time series analysis. BMJ Open 10: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith N, Mitton C, Davidson A. et al. 2014. A politics of priority setting: ideas, interests and institutions in healthcare resource allocation. Public Policy and Administration 29: 331–47. [Google Scholar]
- Terwindt F, Rajan D, Soucat A. 2016. Prioritysetting for national health policies, strategies and plans In: Schmets G, Rajan D, Kadandale S (eds). Strategizing National Health in the 21st century: A Handbook. Geneva: World Health Organization. http://www.who.int/healthsystems/publications/nhpsp-handbook-ch4/en/, accessed 28 April 2021.
- The World Bank . 2021. World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups, accessed 20 June 2021.
- Wallace LJ, Nouvet E, Bortolussi R. et al. 2020. COVID-19 in sub-Saharan Africa: impacts on vulnerable populations and sustaining home-grown solutions. Canadian Journal of Public Health 111: 649–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman D, Persad G, Millum J. 2020. Setting priorities fairly in response to Covid-19: identifying overlapping consensus and reasonable disagreement. Journal of Law and the Biosciences 7: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. Ethics and COVID-19 : resource allocation and priority-setting. World Health Organization, pp. 1–5. https://www.who.int/ethics/publications/ethics-covid-19-resource-allocation.pdf?ua=1, accessed 20 June 2021.
- Willcox ML, Peersman W, Daou P. et al. 2015. Human resources for primary health care in sub-Saharan Africa: progress or stagnation? Human Resources for Health 13: 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.


