Abstract
Background
In response to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, clinicians in outpatient HIV practices began to routinely offer telemedicine (video and/or phone visits) to replace in-person appointments. Video visits are preferred over phone visits, but determinants of video visit uptake in HIV care settings have not been well described.
Methods
Trends in type of encounter (face-to-face, video, and phone) before and during the pandemic were reviewed for persons with HIV (PWH) at an urban, academic, outpatient HIV clinic in Seattle, Washington. Logistic regression was used to assess factors associated with video visit use including sociodemographic characteristics (age, race, ethnicity, language, insurance status, housing status) and electronic patient portal login.
Results
After an initial increase in video visits to 30% of all completed encounters, the proportion declined and plateaued at ~10%. A substantial proportion of face-to-face visits were replaced by phone visits (~50% of all visits were by phone early in the pandemic, now stable at 10%–20%). Logistic regression demonstrated that older age (>50 or >65 years old compared with 18–35 years old), Black, Asian, or Pacific Islander race (compared with White race), and Medicaid insurance (compared with private insurance) were significantly associated with never completing a video visit, whereas history of patient portal login was significantly associated with completing a video visit.
Conclusions
Since the pandemic began, an unexpectedly high proportion of telemedicine visits have been by phone instead of video. Several social determinants of health and patient portal usage are associated with video visit uptake.
Keywords: HIV, telemedicine, delivery of health care
Onset of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic disrupted health care in every field and threatened each stage of the HIV care continuum [1–8]. Clinical teams rapidly adapted workflows and care strategies to mitigate the impact. As a prime example, most clinics implemented telemedicine (real-time video visits and/or audio-only phone visits), which the Department of Health and Human Services endorsed as a means to help persons with HIV (PWH) maintain engagement in care while adhering to social distancing guidelines [9–12]. Evaluations of the telemedicine response in HIV practices are starting to accrue. Researchers at a community health clinic in Boston reported that visit frequency and viral suppression were not interrupted during the first 2 months of the pandemic due to a rapid pivot to video and phone visits [13]. Investigators in Omaha found that quick adoption of phone visits aided in maintenance of viral suppression in the early months of the pandemic despite an overall decrease in medical visit frequency. They reported that only phone visits were used during the study period, not video, in part because many patients had limited access to devices and broadband and many did not use the online patient portal [14]. Data from a safety net clinic in San Francisco showed increased odds of viral nonsuppression in the 1-month period after shelter-in-place orders compared with the 3 months prior, despite swift rollout of phone visits [15]. In this setting, phone visits helped maintain retention in care but were not sufficient to maintain viral suppression for PWH experiencing homelessness and needing social support services. Similar to the clinic in Omaha, only phone visits were employed and not video.
These reports suggest that successful utilization of telemedicine varies by patient population and that the “digital divide” (unequal access to means of connecting to virtual health care) affects uptake of virtual care services by PWH [16]. This correlates with studies from other fields, which have demonstrated that social determinants of health predict readiness to connect by telemedicine, especially video. Video visits are preferred over audio-only phone visits because they allow for greater interaction and visualization as well as a limited physical exam [16, 17]. Benefits of video visits for PWH have been documented, including reduced need to travel long distances to clinic, privacy for those not wanting to attend clinic in person, and scheduling flexibility [12]. However, many individuals are unable to connect by video due to lack of a device, high-speed broadband internet, comfort using the technology, English language proficiency, social support, a private space to join the visit, or other barriers [12, 16]. Analyses from primary care and subspecialty clinics in Philadelphia early in the pandemic demonstrated that older age, Asian race, limited English proficiency, and Medicaid insurance correlated with lower likelihood of using any telemedicine [18]. In addition, persons who were older, born female, Black, Latinx, or had lower income were less likely to utilize video visits. The Infectious Disease Society of America and HIV Medicine Association have called for assessments of disparities in telemedicine access in Infectious Diseases and HIV practices, along with efforts to bolster digital health equity [16].
To date, the reports on telemedicine usage in HIV clinics have primarily focused on phone visits, as opposed to video, and have examined utilization over relatively short periods of time (generally the first 1–3 months after start of local shelter-in-place ordinances). We aimed to evaluate temporal trends in both video and phone visits during multiple phases of social distancing measures and examined factors associated specifically with video visit uptake. Such data may inform interventions that aim to facilitate engagement in care for all PWH.
METHODS
Study Setting and Population
We conducted this study at a Ryan White–funded, academic HIV clinic in Seattle, Washington. We identified a cohort of PWH who were engaged in care before the pandemic, defined as those who had 2 or more clinic encounters (an HIV RNA result counted as an encounter) within the 24 months before March 15, 2020 (the date we began routinely offering video visits and billable audio-only telephone encounters). We encouraged video visits and offered phone visits as a backup option. Among the cohort of PWH, we identified those who were retained in care during the pandemic, defined as those who completed at least 1 clinic visit (a billable in-person, video, or phone visit) or completed an HIV RNA lab check between March 16, 2020, and December 31, 2020. We included an HIV RNA lab check as a marker of retention in care as per HIV/AIDS Bureau Performance Measure definitions [19]. We limited our analysis to retained patients (as opposed to all patients) in order to assess factors associated with completing a video visit for those patients who completed any visit during the study period and thereby had options for the type of visit.
Study End Points
Our primary end point was completion of at least 1 video visit between March 16 and December 31, 2020. We identified visit type by billing code input at the end of each encounter (as opposed to type of visit scheduled, to account for visits scheduled as video then converted to phone due to technical difficulties). Our explanatory variables included several sociodemographic factors known to be social determinants of health: age, race, ethnicity, gender identity, insurance status, and housing status (we attempted to include income, but data were too incomplete) [20, 21]. We extracted these elements from our clinical data warehouse, with the exception of housing status and gender identity, which came from an existing social work database (data collected at intake). We also assessed use of the electronic health record patient portal as a potential predictor of video visit use. This online portal can be used by patients to view laboratory results, send messages to the care team, request appointments, submit medication refill requests, and review other personal health data. Use of the portal requires initial activation; then it can be accessed from any desktop or mobile device. We defined usage of the portal as at least 1 login following initial activation because we find that some patients activate an account or receive assistance activating an account at intake but then never actively use the system.
Statistical Analysis
For the patient characteristics, we used the chi-square test to compare categorical variables and the Wilcoxon rank test for the continuous variable (age). We described general trends in video and phone visits during the time frame of interest. We consolidated categorical variables into meaningful and distinct groups for analysis and employed a logistic regression model for the univariate and multivariate analysis. We calculated adjusted and unadjusted odds ratios for the predictive variables. Analysis was performed using R, version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria).
Institutional Review Board Approval
This work was approved by the University of Washington Institutional Review Board.
RESULTS
We identified 2930 PWH who met criteria for being engaged in care during the 24 months before the pandemic. Of these, 2240 (76.5%) met the prespecified definition for being retained in care during the pandemic. Characteristics of the retained patient population are summarized in Table 1. Of the retained patients, 737 (32.9%) completed 1 or more video visits during the study period, 701 (31.3%) completed 1 or more phone visits and never completed a video visit, and 802 (35.8%) had only in-person visits. Of the individuals who completed a video visit, the number of video visits completed ranged from 1 to 9 (median, 1). Of the 737 patients who completed a video visit, 533 also completed at least 1 in-person visit and 203 also completed at least 1 in-person visit plus at least 1 phone visit; 1 person had only video visits during the study period.
Table 1.
Characteristics of Retained Patients Overall and Compared by Those who Completed at Least 1 Video Visit vs Those who Never Completed a Video Visit During the Study Period
| Category | Variable | No Video, No. (%) | Video, No. (%) | Overall, No. (%) | P Value |
|---|---|---|---|---|---|
| Number | 1503 | 737 | 2240 | ||
| Age | Median (IQR), y | 51 (40–58) | 48 (38–56) | 50 (40–57) | <.001 |
| 18–35 y | 210 (14) | 129 (17.5) | 339 (15.1) | <.001 | |
| 35–50 y | 488 (32.5) | 266 (36.1) | 754 (33.7) | ||
| 50–65 y | 674 (44.8) | 297 (40.3) | 971 (43.3) | ||
| >65 y | 131 (8.7) | 45 (6.1) | 176 (7.9) | ||
| Race | White | 795 (52.9) | 441 (59.8) | 1236 (55.2) | <.001 |
| Black | 503 (33.5) | 195 (26.5) | 698 (31.2) | ||
| Unknown | 56 (3.7) | 48 (6.5) | 104 (4.6) | ||
| Asian/Pacific Islander | 110 (7.3) | 43 (5.8) | 153 (6.8) | ||
| Other | 39 (2.6) | 10 (1.4) | 49 (2.2) | ||
| Insurance | Private | 545 (25.1) | 326 (43.1) | 871 (29.7) | <.001 |
| Medicaid | 538 (24.7) | 210 (27.8) | 748 (25.5) | ||
| Medicare | 328 (15.1) | 148 (19.6) | 476 (16.2) | ||
| Self-pay | 92 (4.2) | 53 (7) | 145 (4.9) | ||
| Birth sex | Cisgender female | 285 (19) | 153 (20.8) | 438 (19.6) | .3415 |
| Gender identity | Gender minoritya | 25 (1.7) | 10 (1.4) | 35 (1.6) | NAb |
| Ethnicity | Not Latinx | 1223 (81.4) | 581 (78.8) | 1804 (80.5) | .9095 |
| Latinx | 224 (14.9) | 104 (14.1) | 328 (14.6) | ||
| Unavailable or unknown | 56 (3.7) | 52 (7.1) | 108 (4.8) | ||
| Language | English | 1266 (84.2) | 672 (91.2) | 1938 (86.5) | .1315 |
| Spanish | 87 (5.8) | 33 (4.5) | 120 (5.4) | ||
| Other | 150 (10) | 32 (4.3) | 182 (8.1) | ||
| Patient portal login | Yes | 439 (29.2) | 337 (45.7) | 776 (34.6) | <.001 |
| Housing status | Permanent | 1308 (87) | 641 (87) | 1949 (87) | .4402 |
| Unstable | 97 (6.5) | 37 (5) | 134 (6) | ||
| Temporary | 59 (3.9) | 30 (4.1) | 89 (4) | ||
| Unknown | 39 (2.6) | 29 (3.9) | 68 (3) |
Abbreviation: IQR, interquartile range.
Transgender, gender nonbinary, or other listed gender that was not cisgender.
Number of gender minority patients too small for statistical comparison.
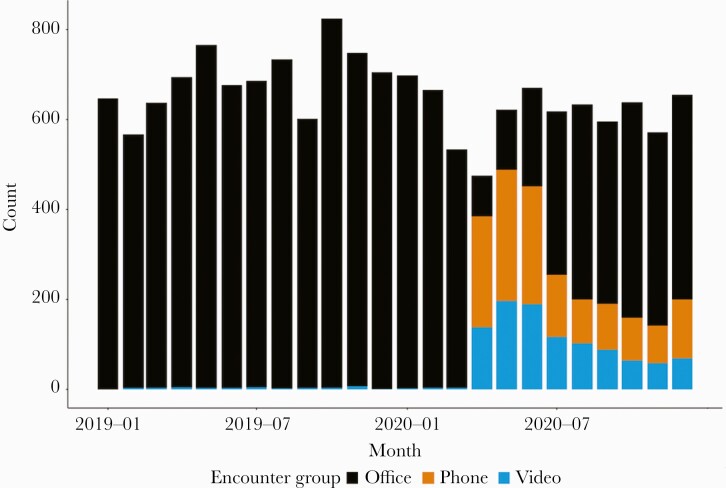
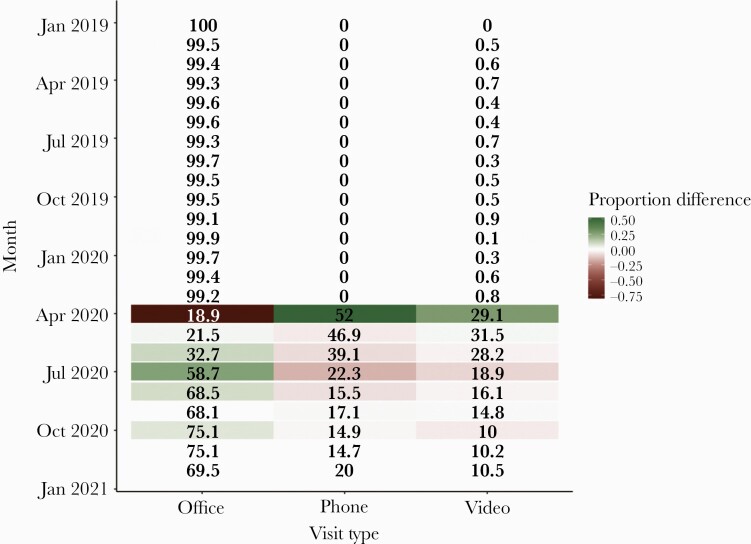
The overall volume of visits (all types) did not change markedly during the pandemic, aside from an initial transient drop, but the distribution of visit types had notable shifts at distinct time points (Figure 1). After a dramatic early increase in the proportion of visits by video (<1% before March 2020 to ~30% in April–June 2020), the proportion then decreased and plateaued at ~10% for the remainder of the study period (Figure 2). Early during the pandemic, a sizable proportion of visits were by phone (audio only), including 52% of visits in April 2020, which declined to ~15% in fall 2020 and rose again in winter 2020 to ~20%, corresponding to another period of heightened social distancing restrictions.
Figure 1.
Number of completed visits per month by visit type, comparing office (face-to-face), video, and phone (audio only).
Figure 2.
Visit type proportion (percentage of all completed visits) by month, comparing office (face-to-face), video, and phone (audio only).
Univariate analysis identified several factors associated with any video visit use, including age, race, insurance type, and patient portal login (Table 2). On multivariate analysis that included these factors as well as Latinx ethnicity, persons with HIV age 50–65 were less likely to complete a video visit compared with PWH age 18–35 (adjusted odds ratio [aOR], 0.75; 95% CI, 0.57–0.99; P = .04), as were PWH age >65 compared with age 18–35 (aOR, 0.56; 95% CI, 0.35–0.88; P = .01). Black PWH were less likely to complete a video visit as compared with White PWH (aOR, 0.81; 95% CI, 0.65–0.99; P = .04), as were Asian or Pacific Islander PWH as compared with White PWH (aOR, 0.67; 95% CI, 0.45–0.98; P = .045). Persons with HIV with Medicaid insurance were less likely to complete a video visit than PWH with private insurance (aOR, 0.73; 95% CI, 0.58–0.91; P = .01). Finally, PWH with history of at least 1 patient portal login were significantly more likely to complete a video visit compared with PWH with no history of login (aOR, 1.80; 95% CI, 1.48–2.19; P < .001). There were no significant differences by Latinx ethnicity in multivariate analysis.
Table 2.
Results of Univariate and Multivariate Analysis for Factors Associated With Completing at Least 1 Video Visit During the Study Period
| Variablea | Unadjusted OR | Adjusted OR | Adjusted OR Lower CI | Adjusted OR Upper CI | P Value |
|---|---|---|---|---|---|
| Age | |||||
| 35–50 y | 0.89 | 0.89 | 0.67 | 1.18 | .400 |
| 50–65 y | 0.72 | 0.72 | 0.54 | 0.96 | .025 |
| >65 y | 0.56 | 0.54 | 0.34 | 0.86 | .010 |
| Race | |||||
| Asian or Pacific Islander | 0.70 | 0.67 | 0.45 | 0.98 | .045 |
| Black | 0.70 | 0.77 | 0.62 | 0.95 | .018 |
| Other | 0.46 | 0.50 | 0.23 | 0.98 | .055 |
| Unknown | 1.80 | 1.82 | 0.07 | 48.01 | .679 |
| Ethnicity | |||||
| Latinx | 0.98 | 0.80 | 0.60 | 1.05 | .110 |
| Unknown | 1.95 | 1.50 | 0.66 | 3.39 | .325 |
| Patient portal login | 2.04 | 1.75 | 1.44 | 2.13 | <.001 |
| Insurance status | |||||
| Medicaid | 0.65 | 0.71 | 0.57 | 0.89 | <.001 |
| Medicare | 0.75 | 0.89 | 0.68 | 1.17 | .410 |
| Self-pay | 0.96 | 1.01 | 0.69 | 1.48 | .948 |
Abbreviation: OR, odds ratio.
Variables used as reference for comparisons in logistic regression: age 18–35 years, White race, not Latinx, no patient portal login, and private insurance.
DISCUSSION
A better understanding of predictors of telemedicine use could inform interventions to address disparities in access and decrease gaps in care. Our review of visit types and patient characteristics associated with video visit uptake at an urban, academic, safety net HIV clinic in the United States revealed several important results. Most notably, the overall volume of visits did not change substantially during the pandemic, and, after an initial dramatic increase in video visits, usage decreased and plateaued at around 10% of clinic encounters. Several factors were significantly associated with completing a video visit, including age, race, insurance status, and electronic patient portal login. Patterns of video and phone visit use mirrored local social distancing measures, and, even though our clinic encouraged video visits, a high proportion of face-to-face encounters were replaced by phone visits.
The trends in video visit use in this outpatient HIV practice are informative and show that video visit uptake has been modest during the pandemic and has leveled off at ~1 in 10 encounters. We anticipate that video visits will remain an important option for patients with barriers to in-person appointments (eg, distance or lack of transportation), but need to better understand why video visits have not been used more frequently. Factors associated with video visit use in our study include age, race, insurance status, and patient portal login. These findings are similar to those from analyses in other fields. For example, evaluations of telemedicine uptake from Cardiology and Gastroenterology clinics in Philadelphia demonstrated that individuals who were Black, born female, older, had lower income, or had limited English proficiency were more likely to use phone visits than video visits early in the pandemic [22, 23]. Similarly, a study from Cardiology in Boston showed that individuals who were older, had lower income, had Medicaid or Medicare insurance, or were Black or Latinx were less likely to use video visits during the pandemic [24]. However, while our results and other data demonstrate disparities in video visit usage based on social determinants of health, they do not explain why these differences exist. We suspect the explanation is a combination of disparities in access to devices and broadband internet, as well as differences in technical literacy, social support, trust in remote health care, and other factors described previously [12, 16]. That said, differences may be due to patient choice, provider preference, differences in medical status (presence of medical comorbidities and thereby appropriateness for remote visits), or a bias in which patients from certain demographic groups are less likely to be offered video visits. Assessments of reasons behind disparities in video visit uptake should be included in future work.
In our study, a remarkably high proportion of virtual visits conducted since the start of the pandemic were phone visits (audio only), and this pattern has persisted for nearly a year following initial implementation of social distancing measures. This is noteworthy because it remains unclear whether phone visits will be reimbursed by Medicare, Medicaid, or commercial insurers once the public health emergency ends. The frequency of phone visit use was higher than expected (we expected greater use of video visits) and strongly argues for ongoing payment parity for both video and phone encounters. Other data similarly support this need. An evaluation of visit trends from the Johns Hopkins HIV Clinical Cohort in Baltimore found that during the first 14 weeks after the transition to telemedicine, 30% of telemedicine visits were by video and 70% by telephone [25]. In the reports from Omaha and San Francisco, 100% of telemedicine visits were conducted by phone, not video [13, 14]. In an analysis of visit data from 41 Federally Qualified Health Centers in California, video visit use increased only modestly; phone visits replaced a majority of in-person appointments and accounted for overall stability in visit volume [26]. Phone visits offer a critical safety net option for individuals who have barriers to in-person appointments and are not ready for video visits. Our results confirm that eliminating reimbursement for phone visits could disproportionately harm PWH who are unable to access video visits.
Our finding that electronic patient portal login predicts video visit use is unique and notable. Even though we provide video visit login instructions and links by multiple modalities (short message service [SMS] or text in addition to patient portal), patient portal login appears to be a significant indicator of capacity to access electronic health care and should be considered a determinant of readiness for virtual health care, or, as other authors have stated, a “digital determinant of health” [27]. This finding suggests that at least a part of the reason for disparities in video visit use is lack of access to or comfort using the technology. Patient portals and electronic tools should be designed to improve access for all users, regardless of language or technical proficiency. Quality improvement interventions could focus on identifying patients who have not used the patient portal and addressing barriers to use. Some patients who access the online patient portal may prefer and choose in-person visits for other reasons, though usage of the online portal seems to be a marker of capacity for video visits.
The strengths of our analysis include an assessment of trends over an extended period of time and evaluation of a variety of potential predictors, including patient portal login. This analysis comes from a single center, which limits generalizability. Our data are also limited by a relatively small proportion of patients with a primary language identified as a language other than English and of gender minority patients. Additionally, housing data came from a social work database; data for individuals not engaged with social work may be missing, and thereby individuals with stable housing may be underrepresented. We did not find language or housing status to be significant predictors of video visit usage, but this may be due to limitations in the data.
In conclusion, video visit uptake has been modest at our academic HIV outpatient practice, and many patients rely on phone visits to remain engaged in care. Payment parity for phone visits as a safety net option will be critical even after the public health emergency ends. Several social determinants of health were associated with video visit usage, as was use of the electronic patient portal. Further work should explore patient awareness and attitudes toward telemedicine in order to elucidate sources of these disparities. In at least 1 early evaluation, PWH reported high satisfaction with telemedicine visits and that such visits may improve adherence to appointments, but this should be confirmed [28]. Further research should also assess the success of interventions aimed to mitigate access barriers, particularly during COVID-19 case surges, and evaluate differences in health outcomes (viral suppression, receipt of recommended vaccines and other preventative services, and other quality-of-care indicators) comparing PWH who opt for in-person vs virtual care. We hope that assessments of disparities in video visit uptake and barriers to usage will be replicated at other centers and on a larger scale to inform efforts toward digital inclusion.
Acknowledgments
The authors would like to thank Mei-Lan Huang, MSIS, MSW, Senior Computer Specialist for Harborview Medical Center Quality Improvement, for assistance with data extraction for the analysis of electronic patient portal login.
Patient consent. The design of the work was approved by the University of Washington Institutional Review Board.
Author contributions. All authors contributed to the design of the study, interpretation of the results, and preparation of the manuscript. Yuan Tao and Erin Aas collected the data, and Kristine Lan performed the statistical analysis.
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Karaosmanoglu HK. How does the Covıd-19 pandemic affect the target 90-90-90? Curr HIV Res 2021; 19:103–5. [DOI] [PubMed] [Google Scholar]
- 2. Gatechompol S, Avihingsanon A, Putcharoen O, et al. . COVID-19 and HIV infection co-pandemics and their impact: a review of the literature. AIDS Res Ther 2021; 18:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pinto RM, Park S.. COVID-19 pandemic disrupts HIV continuum of care and prevention: implications for research and practice concerning community-based organizations and frontline providers. AIDS Behav 2020; 24:2486–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Delaney KP, Jayanthi P, Emerson B, et al. . Impact of COVID-19 on commercial laboratory testing for HIV in the United States. Paper presented at: CROI, March 6–10, 2021; Virtual. Abstract 739. [Google Scholar]
- 5. Tedaldi EM, Hou Q, Armon C, et al. . HIV ambulatory care during COVID-19 pandemic in US: visits and viral load testing. Paper presented at: CROI, March 6–10, 2021; Virtual. Abstract 752. [Google Scholar]
- 6. Ridgway JP, Schmitt J, Friedman E, et al. . HIV care continuum and COVID-19 outcomes among people living with HIV during the COVID-19 pandemic, Chicago, IL. AIDS Behav 2020; 24:2770–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Menza TW, Zlot AI, Garai J, et al. . The impact of the SARS-CoV-2 pandemic on human immunodeficiency virus and bacterial sexually transmitted infection testing and diagnosis in Oregon. Sex Transm Dis 2021; 48:e59–63. [DOI] [PubMed] [Google Scholar]
- 8. Mitchell KM, Dimitrov D, Silhol R, et al. . The potential effect of COVID-19-related disruptions on HIV incidence and HIV-related mortality among men who have sex with men in the USA: a modelling study. Lancet HIV 2021; 8:e206–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Budak JZ, Scott JD, Dhanireddy S, Wood BR.. The impact of COVID-19 on HIV care provided via telemedicine—past, present, and future. Curr HIV/AIDS Rep 2021; 18:98–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dawson L, Kates J.. Delivering HIV care and prevention in the COVID era: a national survey of Ryan White providers. Kaiser Family Foundation. 2020. Available at: https://www.kff.org/report-section/delivering-hiv-care-prevention-in-the-covid-era-a-national-survey-of-ryan-white-providers-issue-brief/. Accessed 17 August 2021.
- 11.Department of Health and Human Services. Interim guidance for COVID-19 and persons with HIV. 2021. Available at: https://clinicalinfo.hiv.gov/en/guidelines/covid-19-and-persons-hiv-interim-guidance/interim-guidance-covid-19-and-persons-hiv. Accessed 17 August 2021.
- 12. Smith E, Badowski ME.. Telemedicine for HIV care: current status and future prospects. HIV AIDS (Auckl) 2021; 13:651–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mayer KH, Levine K, Grasso C, Multani A, Gonzalez A, Biello K.. Rapid migration to telemedicine in a Boston community health center is associated with maintenance of effective engagement in HIV care. Open Forum Infect Dis 2020; 7(Suppl 1):S337. [Google Scholar]
- 14. Fadul N. A quality management project of a Midwestern academic HIV clinic operation during COVID-19: implementation strategy and preliminary outcomes. Open Forum Infect Dis 2020; 7(Suppl 1):S184–5. [Google Scholar]
- 15. Spinelli MA, Hickey MD, Glidden DV, et al. . Viral suppression rates in a safety-net HIV clinic in San Francisco destabilized during COVID-19. AIDS 2020; 34:2328–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wood BR, Young JD, Abdel-Massih RC, et al. . Advancing digital health equity: a policy paper of the Infectious Diseases Society of America and the HIV medicine association. Clin Infect Dis 2021; 72:913–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rush KL, Howlett L, Munro A, Burton L.. Videoconference compared to telephone in healthcare delivery: a systematic review. Int J Med Inform 2018; 118:44–53. [DOI] [PubMed] [Google Scholar]
- 18. Eberly LA, Kallan MJ, Julien HM, et al. . Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open 2020; 3:e2031640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.HIV/AIDS Bureau. HIV/AIDS Bureau performance measures. Available at: http://hab.hrsa.gov/sites/default/files/hab/clinical-quality-management/coremeasures.pdf. Accessed 17 August 2021.
- 20.US Department of Health and Human Services. Social determinants of health. Available at:https://health.gov/healthypeople/objectives-and-data/social-determinants-health. Accessed 1 June 2021.
- 21.Centers for Disease Control and Prevention. Social determinants of health: know what affects health. Available at: https://www.cdc.gov/socialdeterminants/index.htm. Accessed 1 June 2021.
- 22. Eberly LA, Khatana SAM, Nathan AS, et al. . Telemedicine outpatient cardiovascular care during the COVID-19 pandemic: bridging or opening the digital divide? Circulation 2020; 142:510–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Serper M, Nunes F, Ahmad N, et al. . Positive early patient and clinician experience with telemedicine in an academic gastroenterology practice during the COVID-19 pandemic. Gastroenterology 2020; 159:1589–91.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brown KJ, Mathenge N, Crousillat D, et al. . Social determinants of telemedicine utilization in ambulatory cardiovascular patients during the COVID-19 pandemic. Eur Heart J Digital Health 2021; 2:244–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. El-Nahal W, Shen N, Lesko C, et al. . Visit completion during the telemedicine transition in early months of the pandemic. Paper presented at: CROI, March 6–10, 2021; Virtual. Abstract 734. [Google Scholar]
- 26. Uscher-Pines L, Sousa J, Jones M, et al. . Telehealth use among safety-net organizations in California during the COVID-19 pandemic. JAMA 2021; 325:1106–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Crawford A, Serhal E.. Digital health equity and COVID-19: the innovation curve cannot reinforce the social gradient of health. J Med Internet Res 2020; 22:e19361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Carvajal KL, Winbush A, Mangat R, Louie T.. Walking to the virtual era. Analysis of the telehealth experience in the infectious diseases clinic during the COVID pandemic. Paper presented at: ID Week, October 10–25, 2020; Virtual. Abstract 127. [Google Scholar]