Abstract
The cardiovascular system is significantly affected in coronavirus disease-19 (COVID-19). Microvascular injury, endothelial dysfunction, and thrombosis resulting from viral infection or indirectly related to the intense systemic inflammatory and immune responses are characteristic features of severe COVID-19. Pre-existing cardiovascular disease and viral load are linked to myocardial injury and worse outcomes. The vascular response to cytokine production and the interaction between severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) and angiotensin-converting enzyme 2 receptor may lead to a significant reduction in cardiac contractility and subsequent myocardial dysfunction. In addition, a considerable proportion of patients who have been infected with SARS-CoV-2 do not fully recover and continue to experience a large number of symptoms and post-acute complications in the absence of a detectable viral infection. This conditions often referred to as ‘post-acute COVID-19’ may have multiple causes. Viral reservoirs or lingering fragments of viral RNA or proteins contribute to the condition. Systemic inflammatory response to COVID-19 has the potential to increase myocardial fibrosis which in turn may impair cardiac remodelling. Here, we summarize the current knowledge of cardiovascular injury and post-acute sequelae of COVID-19. As the pandemic continues and new variants emerge, we can advance our knowledge of the underlying mechanisms only by integrating our understanding of the pathophysiology with the corresponding clinical findings. Identification of new biomarkers of cardiovascular complications, and development of effective treatments for COVID-19 infection are of crucial importance.
Keywords: Cardiovascular disease, COVID-19, SARS-CoV-2, cytokines, inflammation, Infection, endothelial dysfunction, microcirculation, thrombosis, Myocardial injury, post-acute COVID-19
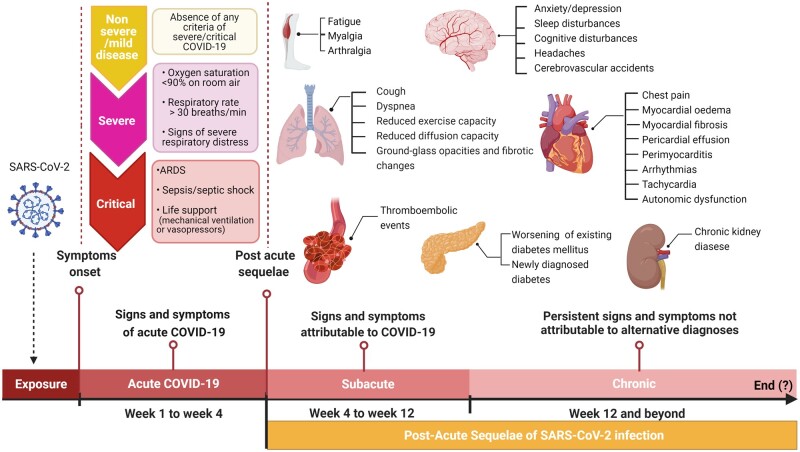
Graphical Abstract
Graphical Abstract.
Introduction
To date, the coronavirus disease 2019 (COVID-19) pandemic, has affected over 214 million of people and caused over 4.4 million deaths since December of 2019.1 Initially thought to be an acute respiratory distress syndrome (ARDS), it has since became clear that COVID-19 is in fact a multiple organ disease. The disease is characterized by cytokine storm, resulting in endothelial inflammation/dysfunction, micro- and macro-vascular thrombosis, which may damage organs other than the lung. Human studies have offered an alarming view of the risks of severe complications in elderly patients and in those with underlying cardiovascular disease or who are at high cardiovascular risk due to one or more risk factors such as hypertension, diabetes mellitus, hypercholesterolaemia, or obesity. Moreover, recent studies revealed that some biological changes induced by COVID-19 throughout the organs are long-lasting.2 Consistent with this finding, a large number of patients who have been infected with severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) continue to experience symptoms after the acute phase of the acute infection, which can evolve over time and persist for months. While still being defined, these effects are referred to as Post-Acute Sequelae of SARS-CoV-2 infection or ‘Long COVID’.3 Therefore, the magnitude of the problem is still unknown. Post-acute COVID-19 is a matter of major concern for patients affected by cardiovascular disease, given that the presence of underlying cardiovascular comorbidities in patients with COVID-19 is associated with high mortality and COVID-19 can cause cardiovascular disorders, including myocardial injury, arrhythmias, acute coronary syndrome (ACS), and venous thromboembolism (VTE). Cardiovascular disease remains the leading cause of morbidity and mortality globally and is associated with 17.8 million deaths annually.4 We cannot predict the impact of post-acute COVID-19 on future cardiovascular outcomes. Nevertheless, to meet the urgent need for effective treatment and preventative strategies, rigorous efforts should be made to investigate and integrate biological and clinical findings related to COVID-19 in cardiovascular disease.
In this position paper, we assessed the evidence supporting the mechanisms of acute and post-acute cardiovascular injury among patients with COVID-19 and their clinical features to identify gaps that need to be addressed in future research.
Inflammation and COVID-19
Severe COVID-19 patients have frequently lymphopenia, hypoalbuminaemia, and exhibit higher levels of transaminases, lactate dehydrogenase, C-reactive protein (CRP), ferritin, and D-dimer, as well as markedly higher levels of interleukin (IL)-2R, IL-6, Il-8, IL-10, and tumour necrosis factor-α (TNF-α). Cytokine production is induced by macrophage activation mediated by a disintegrin and metalloproteinase 17 (ADAM17) which is also responsible for the proteolytic cleavage of angiotensin-converting enzyme 2 (ACE2). In addition, CD14+ CD16+ monocytes producing high levels of IL-6 are observed in COVID-19 patients, suggesting that monocytes contribute to the cytokine storm.5
Increased activity of the angiotensin (Ang) II/Ang II receptor type 1 (AT1) receptor axis, due to the loss of function of ACE2 in combination with cytokines-induced hyperinflammation (Figure 1) can trigger systemic endothelial injury, overexpression of inflammatory mediators in the interstitial space of various organs causing parenchymal injury, hypercoagulability, microvascular thrombosis in the pulmonary and coronary microcirculation,6,7 myocardial injury, and multiple organ dysfunction in a positive feedback loop through circulating inflammatory mediators and organ dysfunction-mediated endothelial activation. Inflammation drives SARS-CoV-2-related mortality through pulmonary endothelial barrier dysfunction and left ventricular dysfunction.6 Cardiac microvascular endothelial cells, exert a positive effect on cardiomyocyte contractility mainly mediated by endothelium-derived nitric oxide (NO). Cytokines reduce endothelium-derived NO delivery likely through increased cytoplasmatic and mitochondrial oxidative stress that results in the scavenging of NO thus reducing cardiomyocyte contractility and relaxation.8 Pulmonary barrier dysfunction and left ventricular dysfunction may aggravate each other,9 causing a vicious cycle that results in pulmonary oedema. Lymphopenia occurs early and it is a prognostic factor, potentially associated with reduction of CD4+T and CD8+T cells. Main mechanisms contributing to lymphopenia are thought to be as follows: (i) direct viral infection of lymphocytes, leading to apoptosis and pyroptosis; (ii) viral mediated bone marrow damage and thymus suppression; (iii) lymphocyte apoptosis induced by TNF-α, IL-2R, IL-6, and other pro-inflammatory cytokines; (iv) tissue re-distribution of lymphocytes; and (v) suppression of lymphocyte proliferation caused by metabolic and biochemical changes such as hyperlactic acidemia and hyperbilirubinaemia.10 This leads to an imbalance of the innate/acquired immune response. Persistent immune activation in predisposed patients can lead to secondary haemophagocytic lymphohistiocytosis, an hyperinflammatory syndrome characterized by a cytokine storm that induces multi-organ failure and death similar to the events observed in septic patients.6,11
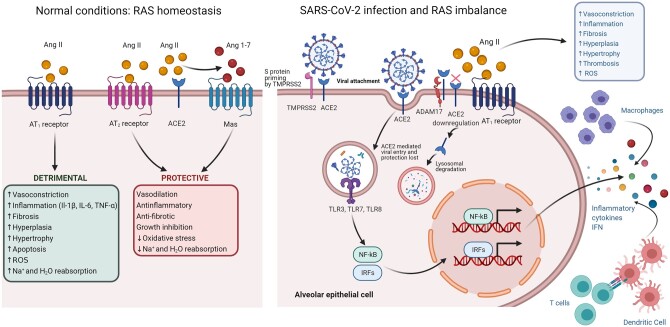
Figure 1.
Interplay between angiotensin II, ACE2 (angiotensin-converting enzyme 2), and SARS-CoV-2 binding in the pathogenesis of COVID-19, the inflammatory response and cardiovascular protection lost. Left panel: In physiological conditions, ACE2 balances renin–angiotensin system expression. Increased ACE2 increase the protective axis of ACE2/Angiotensin (Ang)1-7/Mas receptor axis counter-regulates the actions of the ACE/Ang II/angiotensin receptors 1 (AT1) axis. Right panel: SARS-CoV-2 spike (S) protein has a strong binding affinity to ACE2 which facilitate viral entry into target cells by transmembrane protease serine 2 (TMPRSS2) priming. Following binding of ACE2 with S protein, down-regulation of ACE2 is observed. Accumulation of Ang II increases the activity of AT1 receptors leading to internalization, down-regulation, and degradation of ACE2. In addition, endocytosed SARS-CoV-2 up-regulates the proteolytic cleavage of ACE2 mediated a disintegrin and metalloproteinase 17 (ADAM17), which activity is further increased by activation of AT1 receptors due to the accumulation of Ang II. Viral RNA activates toll-like receptor (TLR) 3, TLR 7, TLR 8. These receptors activate interferon regulatory factors (IRFs) and nuclear factor kappa-light-chain-enhancer of activated B cells (NFkB) to induce inflammatory cytokines including interferons (INF). Dendritic cells are able to produce IFN and augment the IFN signal, which also represents a risk for immunopathology. Systemic cytokines release in combination with cardiovascular risk factor and comorbidities can lead to a cytokine storm, whereas increased activity of Ang II/AT1 receptor axis, due to ACE2 loss of function, exerts vasoconstrictor, profibrotic, prothrombotic and proinflammatory effects. Figure created with BioRender.com. H2O, water; IL, interleukin; Na+, sodium; ROS, reactive oxygen species; SARS-CoV-2, Severe Acute Respiratory Syndrome-Coronavirus 2; TNF-α, tumour necrosis factor alpha.
ACE2 and cardiovascular manifestations
SARS-CoV-2 is a single-stranded ribonucleic acid (RNA) virus which shares 79.5% sequence identity with SARS-CoV.12 The outer membrane structural spike (S) protein, which binds with high affinity to the ACE2 receptor, is inserted into the viral envelope. Following binding, the S protein is cleaved and thus activated for membrane fusion by the transmembrane protease serine 2 (TMPRSS2) in a process known as S protein priming (Figure 1).13–15 Therefore, SARS-CoV-2 infection requires the co-expression of ACE2 and TMPRSS2. Spike protein/ACE2 internalization promote the up-regulation of ADAM17 and shedding of the extracellular domain of ACE2, increasing membrane ACE2 down-regulation and reducing surface ACE2 expression.15 The increased ADAM17-mediated ACE2 shedding exacerbates inflammatory responses by TNF-α and IL6R initiating the cytokine storm.15
ACE2 is a master regulator of the renin–angiotensin system (RAS). The activity of the RAS depends on the balance between the ACE/Ang II/AT1 and ACE2/Ang 1-7/Mas axes. ACE converts Ang I to the active vasoconstrictor Ang II, whose actions are mediated by AT1 and Ang II receptor type 2 (AT2). Activation of the ACE/Ang II/AT1 receptor axis, leads to deleterious effects, including vasoconstriction, inflammation, fibrosis, cellular growth and migration, as well as fluid retention. ACE2 is the main Ang 1-7 forming enzyme and the G-protein coupled Mas is a functional receptor for Ang 1-7.16 Angiotensin 1-7 binding to Mas induces several beneficial effects such as vasodilation, inhibition of cell growth, anti-thrombotic, and anti-arrhythmogenic effects17 (Figure 1). Given that ACE2 is widely expressed in endothelial cells, cardiofibroblasts, cardiomyocytes pulmonary epithelial cells, pulmonary vasculature, kidney, adipose tissue, liver, gut, and central nervous system (Figure 2), the loss of ACE2 function following binding of the S protein and ADAM17-mediated shedding along with cytokine storm, are likely involved in the multiple organ dysfunction including the cardiovascular manifestations of COVID-19 (Figures 1 and 2). Even though infection of human cardiomyocytes by SARS-CoV-2 with deleterious effects has been shown in vitro,18 clinical evidence of direct viral infection of cardiomyocytes has not been found, and myocarditis related to COVID-19 infection seems rare. As such the interaction between COVID-19 and ACE2 might affect the cardiovascular system in an indirect manner.19 SARS-CoV-2 entry into cells has been shown to down-regulate ACE2 expression, which can lead to a significant reduction in cardiac contractility and progression of atherosclerosis.20
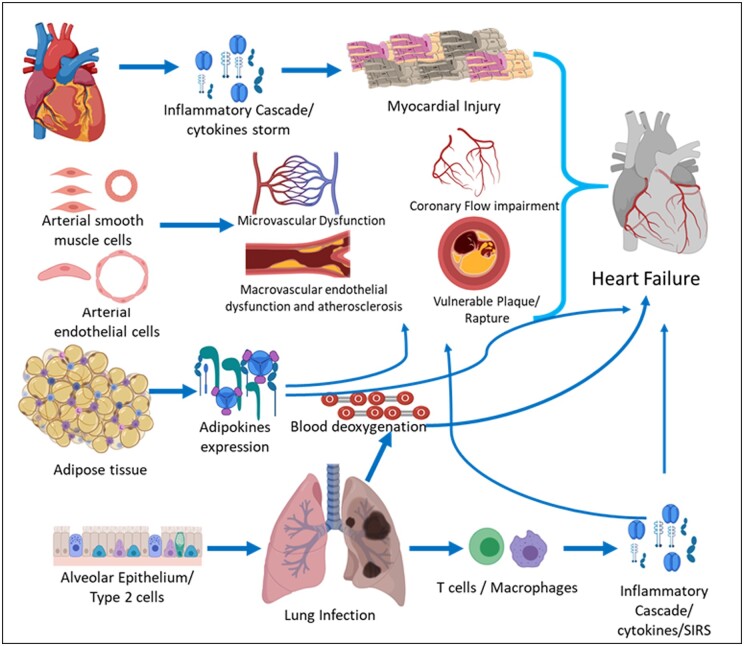
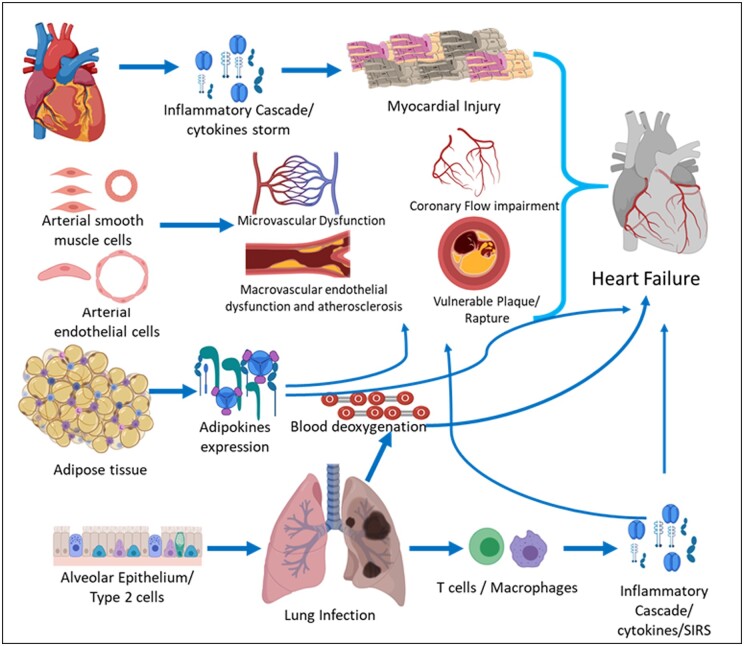
Figure 2.
Tissue expression of ACE2 and potential mechanisms involved in systemic inflammatory response and cardiovascular complications of COVID-19. ACE2 is widely expressed in endothelial cells, arterial smooth muscle cells, renal alveolar epithelial cells adipocytes, and cardiovascular system. Severe Acute Respiratory Syndrome-Coronavirus 2 (SARS-CoV-2) infection cause immune activation, tissue accumulation of T cells, and macrophages leading to myocardial injury. Cytokines release cause systemic inflammatory response which may cause further impairment in micro and macro-circulation and plaque rapture. Blood desaturation may further impair microcirculation and myocardial performance. SIRS, systemic inflammatory response system.
Underlying cardiometabolic risk factors associated with worse outcome in COVID-19
Several reports have consistently demonstrated that pre-existing cardiovascular disease and cardiometabolic risk factors such as hypertension, diabetes, obesity, and/or smoking are major risk factors for increased COVID-19 severity and mortality.21–24 In a recent comparative risk assessment analysis of over 900 000 patients with COVID-19 from the USA, nearly 30% of COVID‐19 hospitalizations were attributable to obesity, 26% to hypertension, 21% to diabetes mellitus, and 12% to heart failure. The study estimated that a 10% reduction in cardiometabolic risk factors could potentially prevent 11% of COVID‐19 hospitalizations.24 Therefore, patient’s awareness of preventive lifestyle measures improves cardiovascular health at large and may reduce COVID-19 severity risk.
Hypertension or age?
Globally, an estimated 1.13 billion individuals worldwide have hypertension, and the greatest burden is in individuals aged 60 years and older.25 Early small case series offered an alarming view suggesting that people living with hypertension were at higher risk of severe COVID-19 and mortality. Preliminary data showed that the incidence of hypertension ranged from 32.6% to 34% among confirmed patients with COVID-19.26,27 Among patients with myocardial injury and elevated cardiac troponin T levels, 63.5% had hypertension.27 Similar findings were observed concerning mortality from COVID-19.27 A meta-analysis incorporating early data of patients with COVID-19, demonstrated that the presence of hypertension was associated with nearly 2.5-fold higher risk of severe disease, intensive care unit (ICU) hospitalization, and mortality.28 Altogether, these findings indicate that hypertensive patients have a higher risk of developing severe COVID-19. However, the mechanisms that link pre-existing hypertension and COVID-19 are yet to be fully elucidated as hypertension coexists with many other risk factors. One approach to disentangle the independent relationship between COVID-19 outcomes and exposure to hypertension is to study patients with hypertension while excluding those with other known risk factors of adverse outcomes. Recent evidence from the UK population-based study OpenSAFELY involving over 17 million patients was based on this approach.29 OpenSAFELY quantified a wide range of clinical risk factors for death from COVID-19, some of which were not previously well characterized. There was no association between hypertension (defined as a recorded diagnosis, or blood pressure ≥140/90 mmHg at the last measurement) and COVID-19 mortality (hazard ratio: 0.95, 95% confidence interval: 0.89–1.01). In contrast, age, cardiovascular disease, diabetes, obesity, respiratory diseases, history of malignancy kidney, liver, neurological, and autoimmune diseases were all associated with increased risk of death. The strongest predictor of mortality was age.
Other recent studies reinforced these observations reporting that age >60 years, overweight/obesity and, diabetes but neither hypertension nor anti-hypertensive treatments were associated with adverse prognosis.30,31 Poor blood pressure control is associated with target end-organ damage, and mean blood pressure increases with age.32 Additionally, age-related low-grade chronic inflammation with enhanced pro-inflammatory cytokines and chemokines, underlie several cardiovascular diseases including hypertension, which in turn is associated with senescence of CD8+T cells, a mainstay of antiviral immunity.33–35 A small study showed that macrophages and neutrophils of hypertensive patients with COVID-19, exhibit higher expression of pro-inflammatory chemokines such as ligands for chemokines with two adjacent cysteines (CCL3, CCL4) and the chemokine receptor CCR1.36 A recent study showed an age-related increase of ACE2 expression in human kidney and lung tissues and lack of association between hypertension, RAS blockers, and renal expression of ACE2.30 These findings are in agreement with previous reports suggesting that RAS blockers use were not associated with higher ACE2 and TMPRSS2 expression in lung tissues, nor with increased circulating plasma concentrations of ACE2.37,38 Taken together, these observations may explain the reported associations between age, hypertension, and severity of COVID-19 infection. In sum, hypertension is very strongly associated with age and although many studies adjusted for this, disentangling the effects of each other is difficult. Age appears to be the strongest predictor for severe disease and mortality in COVID-19, which may be due to immunosenescence, inflammaging,39 exaggerated AT1 pro-inflammatory, pro-thrombotic, and pro-fibrotic signalling.17
Diabetes mellitus
The estimated global prevalence of type 2 diabetes is 9.3% (463 million people)40; therefore, it is not surprising that diabetes is a common cardiometabolic risk factors in patients with COVID-19.24,29,41–44 Early data reported a higher prevalence of diabetes in patients with severe disease as compared to those with mild to moderate disease (16.2% vs. 5.7%).41,45 Moreover, the unadjusted case fatality rate of COVID-19 was higher among diabetic patients than non-diabetic patients (7.3% vs. 2.3%).46 As the global COVID-19 pandemic progressed, a similar pattern of worse prognosis in patients with diabetes was reported across European and USA studies.24,29,42,47 The OpenSafely29 study showed a linear relationship between measured glycated haemoglobin (HbA1c) level of ≥58 mmol/mol (≥7.5%), recorded in primary care, and risk of COVID-19-related mortality, suggesting an association with hyperglycaemia. Other studies have provided similar results showing that the risk of COVID-19 related morbidity and mortality is independently associated to hyperglycaemia.47–49 Another UK population-based study using the QResearch database (QCOVID, n = 6 083 102) reported 4.74‐fold to 6.29‐fold higher risk of age-specific mortality for type 2 diabetes in men and women, respectively.44 Interestingly both OpenSafely and QCOVID reported a higher excess of death risk in younger patients with diabetes compared with older patients with diabetes, hypothesizing that the effective/biological age of a young patient with diabetes matches the chronological age of an older patient without diabetes.50 Although the absolute risk of COVID-19-related death in younger patients with diabetes is not as high as that in elderly, these observations along with the potential modulatory effect of hyperglycaemia on immune and inflammatory responses suggests that the relationship between COVID-19 and diabetes entails a more complex pathophysiology.
Potential mechanisms thought to increase susceptibility and disease severity of SARS-CoV-2 in patients with diabetes include: (i) cellular binding with higher affinity and efficient virus entry, due to glycosylation of S protein and ACE2.51,52 Circulating levels of furin, a cellular protease involved in facilitating viral entry by cleaving the S1 and S2 domain of the S protein and cell-to-cell spread, are elevated in patients with diabetes51,53,54; (ii) expression of ACE2 on pancreatic islets cells may lead to a direct effect of SARS-CoV-2 causing decreased β-cell insulin reserve.55 Interestingly, insulin administration attenuates ACE2 expression.56 (iii) Delayed SARS-CoV-2 clearance21; (iv) immunomodulation, cytokine-mediated dysregulation of glucose metabolism, and hypercoagulability.57 Patients with diabetes are at increased risk of infection due to impaired innate immunity with reduced neutrophil chemotaxis, phagocytosis, and intracellular killing of pathogens resulting in an impairment in adaptive immunity that is characterized by an initial delay in the activation of Th1 cell-mediated immunity and a late hyper-inflammatory response. This further increases insulin resistance and may results in endothelial dysfunction and injury, thereby ultimately promoting thrombotic microangiopathy.58 Additional mechanisms of adverse outcomes in COVID 19 include the effects of hyperglycaemia and glycolysis in monocytes, which may promote viral replication, cytokine production, and subsequent T-cell dysfunction through mitochondrial reactive oxygen species (ROS) production, and activation of hypoxia-inducible factor-1α52; and (v) higher prevalence of cardiovascular comorbidities that may help to explain the association with disease severity and adverse prognosis.
Obesity
Obesity and particularly metabolically unhealthy obesity are major contributors to cardiovascular disease, and mortality. Achieving a metabolically healthy weight is a risk modifier associated with improved cardiac and vascular function.59,60
Epidemiological data show a J-shaped relationship between body mass index (BMI), COVID-19 severity and mortality, with lower risks at BMI thresholds near normal weights.61–66 Interestingly, this relationship was more pronounced among younger patients (<65 years old).62,67,68 In COVID-19 patients from New York City, those aged under 60 years with a BMI ranging from 30 to 34 kg/m2 had a 2-fold increase in the probability of ICU admission compared to patients with a BMI <30 kg/m2. This likelihood increased to 3.6-fold in patients with a BMI ≥35 kg/m2.68 Likewise, a BMI >35 kg/m2 increased the risk of invasive mechanical ventilation 7-fold and was associated with lower survival rates.69 In the OpenSafely study, adjusted mortality rates increased with increasing BMI ranging from 1.05 for BMI <34.9 kg/m2 to 1.92 for BMI ≥40 kg/m2 when compared with non-obese patients.70 Thus, the relationship between obesity and severe COVID-19 and whether obesity could shift this increased risk into younger age groups is still a matter of concern given the high burden of obesity. Some studies addressed the question of why COVID-19 is deadlier in people with obesity, even if they are young. These studies noted that fat distribution and an impaired adipose tissue function, rather than total fat mass and BMI are related with COVID-19 complications at the individual level especially in younger patients.
In one small study of patients with COVID-19, 10 cm2 of increase in visceral adipose tissue area, measured by computed tomography (CT), was associated with a 1.36-fold increase in risk for ICU hospitalization.71 In contrast, BMI and total adipose tissue area showed weak association with COVID-19 severity.71
A combination of physiological and social factors likely drives the grim numbers of obesity-related COVID-19 risk. The biology of obesity includes impaired immunity, chronic inflammation, and increased risk of thrombosis, all of which can worsen COVID-19 outcomes. The devastating impact of obesity, particularly in younger people may have further explanations. A recent study found an increased epicardial adipose tissue attenuation index in the epicardial coronary arteries, which may reflect inflammation within the fat depot, with increasing COVID‐19 severity.72 Of note, epicardial adipose tissue attenuation was similar to that observed in many patients with coronary artery disease despite most of COVID 19 patients having no prior history of coronary artery disease and no coronary artery calcification.72 In a recent multicentre study of 119 patients with COVID-19 increasing epicardial adipose tissue volume and attenuation were associated with increasing burden of COVID-19 pneumonia, clinical deterioration, or death.73
The physical pathologies that render people with obesity vulnerable to severe COVID-19 are multiple. Adipose tissue is among the tissues with the highest expression of ACE2 receptors.74 It is also an important source of cytokines, known as adipokines, which in turn are involved in the regulation of glucose level, lipid metabolism, blood pressure (e.g. through angiotensinogen, angiotensin-II, ACE2 receptors), inflammation (e.g. through modulation of TNF-α, IL-6, macrophage chemo attractant protein-1), thrombosis, and oxidative stress.59 Moreover, prior studies have shown that adipose tissue may act as a virus reservoir.75 In particular, coronaviruses can infect bone marrow-derived macrophages and replicate in them.76 Therefore, abnormal adipose tissue distribution, composition and function, rather than total body fat, may play an important role in COVID-19 infection and related complications, amplifying the inflammatory response in a positive feedback loop.59 Accumulation and inflammation of perivascular, pericardial and epicardial fat surrounding the heart and connecting vessels, may increase local ACE2 expression and associate with an increased leptin/adiponectin ratio, which, in turn, enhances the effects of some pro-inflammatory cytokines with lipotoxicity, such as TNF-α and IL-6.
Pro-inflammatory cytokines increase oxidative stress and decrease glucose utilization exerting detrimental effects on endothelial function. They also increase myocardial inflammation and impair myocardial energetics59 which may result in negative inotropy and myocardial dysfunction.77 Ultimately, pro-inflammatory cytokines triggered by abnormalities in perivascular, pericardial and epicardial fat may aggravate hypoxia and increase arrhythmias.6,78 Other issues aggravate these physio-pathological problems. Obesity may alter the balance between pro and anti-thrombotic mechanisms and may be complicated by higher rates of thromboembolic events including pulmonary embolism.59,79 Yet larger studies are needed to support the hypothesis that visceral, perivascular, pericardial, and epicardial obesity plays an essential role in COVID-19 myocardial injury.
Smoking
Smoking remains a leading risk for early death and disability with 6.4 million deaths per year attributable to smoking worldwide.80 Smoking is an independent risk factor for atherosclerotic cardiovascular disease and a factor positively associated with respiratory diseases, impaired immune system and consequently increased incidence of infectious diseases.60 Smoking has been shown to up-regulate ACE2 expression especially in the lower respiratory tract which might make current smokers vulnerable to infection by COVID 19 compared with former/never smokers.81,82
However, data on this issue are controversial. Several early observational studies41,83,84 and subsequent meta-analyses85–87 based on these reports found an inverse relationship between smoking and severe COVID-19 leading to the misconception that current smoking is of benefit during COVID 19 infection. In contrast, other reports linked current smoking with severe clinical course of COVID-19 and need of ICU care.88,89 Among of 8910 hospitalized patients with COVID-19 current smokers accounted for 5.5% of the study population. A 1.79-fold increase in inhospital mortality was observed in current smokers as compared with former/never smokers.90 The same may also be the case for waterpipe, electronic cigarettes or ‘heat-not-burn’ IQOS users.82 Of note, the prevalence of smokers was higher amongst those patients with myocardial injury as assessed by increased cardiac troponin T levels compared with non-smokers (13.5% vs. 8.1%).27 In sum, further studies are needed to clarify the reasons behind the reported low prevalence of current smokers among hospitalized patients with COVID-19. The effect of current smoking on SARS-CoV-2 infection is a delicate and complex topic that should be addressed rigorously before delivering messages that could be misinterpreted.
Mechanism of disease in relation with the cardiovascular system
Endothelial injury and thrombosis
The prothrombotic and procoagulant state of COVID-19 entails a crucial role in the clinical manifestations of this disease. Viral infection with COVID 19 injures endothelial cells, which respond to the insult by activating the coagulation system.
Endothelial cell dysfunction induces the expression of tissue factor (TF) (through IL-1, TNF-α, and IL-6-mediated mechanisms), releases von Willebrand factor (vWF) from the Weibel-Palade bodies, and enhances surface expression of selectin class of leucocyte adhesion molecules such as P-selectin and E-selectin, overall promoting thrombus formation and leucocyte recruitment (i.e. thrombo-inflammation; Figure 3).91,92 Virus engagement with ACE2 endothelial receptor may also reduce angiotensin II conversion to angiotensin 1-7. Angiotensin II not only promotes thrombus formation but induces plasminogen-activator inhibitor-type 1 (PAI-1) production hampering fibrinolysis and thrombus dissolution.93 On the other hand, platelets are able to sense the viral infection and become activated through pattern recognition- [toll-like-receptors (TLR)], immunoglobulin Fc- and complement receptors. Activated platelets facilitate pathogen clearance by forming platelet aggregates and microthrombi, and by promoting the formation of neutrophil extracellular traps (NETs), web-like structures of decondensed chromatin containing DNA, histones, and granular components, inducing the so-called NETosis.94,95 NETs provide a scaffold and stimulus for thrombus formation by different mechanisms including: (i) the delivery of active TF, (ii) activation of the intrinsic (contact) coagulation pathway through electrostatic interactions between the histones and platelet phospholipids, (iii) induction of platelet activation through histone interaction with platelet TLR, and (iv) blockade of the endogenous anticoagulant antithrombin III and TF pathway inhibitor (TFPI) through activated serine proteases.94 Severe inflammation is also associated with deregulation of the coagulation and fibrinolytic systems by affecting key components involved in the atherothrombotic process such as TF, antithrombin-III, and protein C.
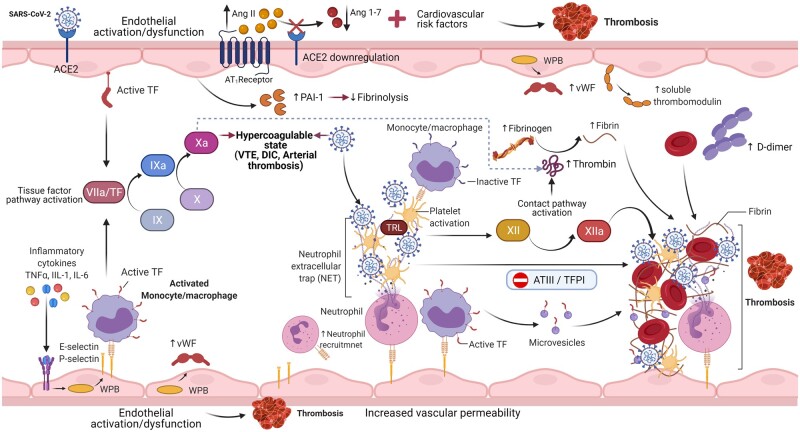
Figure 3.
Mechanisms of endothelial activation/dysfunction and immunothrombosis in COVID-19. SARS-CoV-2 activates the endothelium, either directly by interacting with angiotensin-converting enzyme (ACE) 2 receptor or indirectly by triggering hyperinflammation. Inflammatory cytokines induce the activation of tissue factor (TF) and exocytosis of Weibel Palade bodies (WPB) from endothelial cells, enhancing expression of P-selectin and E-selectin which in turn recruits’ neutrophils and monocytes/macrophages. Monocytes/macrophages activate and deliver through their microvesicles, TF to the sites of SARS-CoV-2 exposure, initiating the TF pathway activation (or extrinsic pathway). Neutrophils release neutrophil extracellular traps (NETs), which capture SARS-CoV-2, promote thrombus formation activation of factor XII (contact or intrinsic pathway of coagulation cascade), and promote platelet recruitment by binding von Willebrand factor (vWF). The NETs propagate coagulation by inactivating endogens anticoagulants such as tissue factor pathway inhibitor (TFPI) and antithrombin III (ATII). Concomitantly, thrombomodulin is shed from endothelial cells, which further promotes a procoagulant and pro-inflammatory milieu. Spike (S) protein binding to ACE2 endothelial receptor reduce angiotensin (Ang) II conversion to Ang 1-7. Accumulation of Ang II leads to plasminogen-activator inhibitor-type 1 (PAI-1) production inhibiting fibrinolysis and thrombus dissolution. Figure created with BioRender.com. IL, interleukin; TNF-α, tumour necrosis factor alpha; TLR, toll-like receptors.
Recent insights on prothrombotic state in COVID-19
Many studies have provided essential insights into the prothrombotic state in COVID-19. Clinical studies demonstrated significantly elevated markers of endothelial and platelet activation such as VWF, PAI-1, soluble thrombomodulin, soluble P-selectin and soluble CD40 ligand, as well as proinflammatory cytokines, components of NETs including cell-free DNA, nucleosomes, myeloperoxidase-DNA, TFPI, complement 5a, and membrane attack component (C5b-9) in severe COVID-19 patients suggesting ‘endotheliopathy’ and thrombo-inflammation as the main contributors of COVID-19 related severity and mortality.95–98 Furthermore, the cytokine storm induces coagulation disorders favouring the appearance of VTE or disseminated intravascular coagulation (DIC) leading to an increase in Factor VIII clotting activity, widespread thrombin formation and consequent elevated D-dimer levels, associated also with a reduced platelet count (Figure 3). In this regard, IL-6 levels have been shown to correlate with a procoagulant profile.99 Thrombocytopenia, which is secondary to excessive platelet consumption in the injured tissue or a result of immune-mediated haematopoietic stem cell damage, was associated with a 3-fold increased risk of severe COVID-19.100 Of note, in patients with SARS a negative correlation was reported between platelet count and circulating levels of the T-cell immunosuppressor soluble vascular cell adhesion molecule-1.101 Additionally, evidence suggests that ACE2 is highly expressed in cardiac pericytes which, when exposed to COVID 19, may lead to endothelial destabilization due to their firm interactions with endothelial cells.74 The interaction between angiopoietin ligands (ANGPT1/2) and Tie receptor (TIE2) appears to be responsible for the endothelial dysfunction that ensues, resulting in reduced endothelial cell survival and increased vascular permeability. Presence of viral elements within the endothelial cells as well as accumulation of inflammatory cells, with evidence of endothelial and inflammatory cell death (lymphocytic endotheliitis) were observed in histopathology specimens of patients with COVID-19.102–104 A recent study suggested that the S protein can exert endothelial cell damage manifested by decreased mitochondrial function and eNOS activity, leading to increased redox stress and ultimately impaired NO bioavailability and ACE2 down-regulation. Of note, the endothelium-dependent vasodilation induced by acetylcholine was impaired in isolated pulmonary arteries of hamsters, but not the endothelium-independent vasodilation induced by sodium nitroprusside.105 It is important to note that endothelial inflammation–endotheliitis affects many vascular beds, resulting in global microcirculatory dysfunction. Recently, soluble thrombomodulin has been suggested as a surrogate marker of endotheliopathy in COVID-19 and seems to provide prognostic information.97 However, this marker still needs further validation.
In summary, multiple pathogenic mechanisms seem to predispose COVID-19 patients to endotheliopathy and thrombosis. Future studies are clearly warranted to fill the current knowledge gaps and identify mechanism of short- and long-term effects of SARS-CoV-2 on endothelial function and novel prognostic endothelial biomarkers.
Myocardial injury
The Fourth Universal Definition of Myocardial Infarction defines myocardial injury (acute or chronic) as at least one cardiac troponin (cTn) value above the 99th percentile upper reference limit (URL).106 Recent reports indicate that myocardial injury, manifested by elevated levels of circulating cTn, electrocardiographic or imaging criteria is frequent among patients with COVID-19. Still there is much confusion about the pathophysiological entities underlying this injury. Here, we summarize few key points about myocardial injury and COVID-19.
Myocardial injury is common and impairs prognosis
The exact frequency of myocardial injury in patients with COVID-19 is difficult to ascertain due to variations in cTn assays, thresholds, studied populations, and clinical conditions. Myocardial injury has been demonstrated in 7–40% of patients with COVID-19 depending on the geographic areas, with a higher prevalence among those patients requiring intensive care.88,107–112 Mortality is approximately 22% among patients with cTn above the URL and 61.5% for those with cTn levels >10 times the URL.107,110,111,113
Mechanisms of elevated troponin in COVID-19 are likely to be multifactorial including sepsis-related cardiomyopathy triggered by the systemic hyperinflammatory state, coronary thrombotic and plaque rupture events, microvascular injury due to DIC and thrombosis, supply–demand mismatch, ARDS related hypoxia, and direct viral cardiotoxicity.114,115 Whether the hypercoagulable state and systemic inflammation observed in COVID-19 are unique features causing myocardial injury should be further investigated.
Clinical classification of acute myocardial injury
Following careful clinical evaluation and understanding of the clinical context in which cTn measurements were obtained, patients with cTn increases should be classified as having (i) Type 1 acute myocardial infarction (MI), (ii) Type 2 acute MI, or (iii) acute non-ischaemic myocardial injury.
Myocardial infarction
Type 1 MI: Immune response, acute infections, as well as local and systemic inflammation resulting in especially those of the respiratory tract are associated with an increased risk of ACS.116 Observational studies on prior virus epidemics support the concept of an association between viral infections affecting the respiratory tract and MI, as is the case of influenza A infections.117 In agreement with such prior observations, a recent systematic review with meta-analysis of self-controlled case series based on five independent studies found an increased risk of MI during the first week following influenza infection.118
As discussed above, a massive systemic inflammatory reaction associated with severe pneumonia as in COVID-19 may lead to an increased propensity for plaque disruption,116 and thrombus formation119 leading to type 1 MI.106 Histopathologic examination of autopsy specimens has evidenced that patients dying of acute systemic infections have consistently higher content of macrophages and T cells in the coronary adventitia and periadventitial fat than non-infected deceased patients, establishing a link between acute systemic infections and local increase of inflammatory cells in coronary arteries.116 In addition, patients with ACS have higher inflammatory activity across the coronary tree than those patients with chronic coronary syndrome. Arterial segments presenting culprit lesions are enriched in infiltrating inflammatory cells, such as macrophages, T cells, and neutrophils, when compared with other areas of the coronary bed.
Inflammatory cells may contribute to plaque instability by expressing active molecules including, cytokines, proteases, coagulation factors, oxygen radicals, and vasoactive molecules. In this respect, experimental studies in mice have demonstrated that infection with the influenza A virus associates with higher immune cell influx, increased production of inflammatory cytokines, and active metalloproteinases in the atherosclerotic plaque, which may account for a higher atherosclerotic plaque vulnerability.120 Evidence of concomitant COVID-19 in ACS patients has been reported.121–126 Higher troponin levels, D-dimer, and CRP, higher rates of multivessel thrombosis, stent thrombosis and higher thrombus burden have been reported in MI patients with COVID-19 as compared with non-infected.125 Additionally, MI patients with COVID-19 showed significantly higher rates of coronary no-reflow (myocardial blush grade 0 or 1) and lower left ventricular function after revascularization, despite similar ischaemic times, suggesting impaired myocardial perfusion at tissue level likely due to microvascular thrombi.125 Thus, MI patients with COVID-19 represent a high-risk group of patients with unique characteristics resulting in increased mortality risk.122–126 Yet, these reports are limited to a few small retrospective observational studies of ST-segment elevation myocardial infarction patients with a scarcity of data on non-ST elevation-acute coronary syndrome.121–126 As such these reports are unable to capture the real magnitude of the problem. Reasons behind this lack of data could be: (i) a decrease in health care–seeking behaviour in asymptomatic/suspected COVID-19 patients, as suggested by concerning reports of an increase in out-of-hospital cardiac arrests (OHCA) and sudden death that could have been secondary to MI127; (ii) difficult differential diagnosis as non-localized chest pain maybe present also in acute COVID-19 due to the underlying hypoxaemia and tachycardia, which in turn may also induce electrocardiographic changes suggestive of myocardial ischaemia.33 On the other hand, dyspnoea may be the only symptom of ACS which in turn in asymptomatic COVID-19 patients could be attributed to the underlying pneumonia; (iii) due to appropriate concerns regarding the safety of health care workers, COVID-19 positive patients with symptoms and electrocardiographic evidence of acute myocardial injury, were less likely to undergo invasive coronary angiography.126
Type 2 acute MI: Studies report that patients with COVID-19 often have chronic cardiovascular conditions such as hypertension, cardiomyopathy, coronary artery disease, or heart failure. All these conditions can be explanations for chronic stable increases >99th percentile URL in Type 2 MI for a number of reasons. First, systemic inflammation is associated with marked haemodynamic changes including sympathetic activation-mediated tachycardia, which results in increased myocardial oxygen requirements.128,129 Second, the direct effects of pathogens and/or their indirect effects through inflammatory cytokines and chemokines promote ROS which are associated with mitochondrial dysfunction including mitochondrial uncoupling, leading to increased mitochondrial oxygen utilization and hence myocardial oxygen demand.130,131 Furthermore, acute respiratory infections can cause ARDS that can result in hypoxia and consequent lowering of arterial oxygen content, thereby potentially further limiting myocardial oxygen delivery.128
As with other coronaviruses, COVID‐19 can elicit an intense release of multiple cytokines and chemokines that can lead not only to vascular inflammation but also to abnormal regulation of vascular tone leading to coronary vasospasm. These abnormalities, in turn, can cause cardiac perfusion abnormalities and even MI.
Cardiogenic shock in those patients may also be precipitated by a myocardial demand-supply mismatch. Increased cardiometabolic demand associated with the systemic infection or sepsis coupled with hypoxia caused by acute respiratory illness can impair myocardial oxygen demand-supply relationship and lead to additional myocardial injury.
Acute non-ischaemic myocardial injury
Emerging reports suggest that acute non-ischaemic myocardial injury is likely the predominant reason for cTn increases. Common cardiac aetiologies include myocarditis, Tako-Tsubo syndrome, and acute heart failure due to either systolic or diastolic dysfunction.106 Primary non-cardiac conditions, such as pulmonary embolism, critical illness, and sepsis, probably cause myocardial injury as well.106,111 Myocarditis and myopericarditis are causes of acute non-ischaemic myocardial injury that warrant particular concern in COVID-19. Depression of myocardial function can result in increased left ventricular diastolic filling pressures, and in combination with systemic vasodilation can cause lowering of diastolic arterial blood pressure, thereby further reducing effective coronary driving pressure. These haemodynamic changes affect particularly the left ventricular subendocardial layers, that are most dependent on perfusion during diastole and hence most vulnerable to ischaemia.132 Accordingly, COVID-19 studies have shown marked increases in N-terminal pro-B-type natriuretic peptides (NT-pro-BNP) in patients with myocardial injury, with studies reporting mean NT-pro-BNP concentrations of 72 pg/mL in patients who recovered compared with 800 pg/mL in those who died.26 Another cause for acute non-ischaemic myocardial injury is pulmonary embolism. In a study of 184 ICU patients with COVID-19 pneumonia, pulmonary embolism was the most frequent thrombotic complication (81%). These data have led to the recommendation to use prophylactic anticoagulation in the absence of randomized evidence.7 Another potential mechanism leading to acute non-ischaemic myocardial injury is direct injury by COVID 19 through ACE2 receptors, which are present in the myocardium and are functional receptors for COVID 19. Patients with heart failure have a higher expression of ACE2, which may explain their increased risk for myocardial injury following COVID-19.
Acute myocarditis
To date, a few cases-series of ‘COVID-19-related myocarditis’ with diverse clinical presentations, have been published.133–136 Patients with an exuberant immune response can manifest acute myocarditis with profound myocardial injury or cardiogenic shock.128,134 However, it is worth remembering that the available findings are more consistent with ‘clinically suspected myocarditis’ or possible Tako-Tsubo syndrome.133,137 A molecular analysis showed the absence of the SARS-CoV-2 genome in the myocardium of a patient diagnosed with COVID-19 and endomyocardial biopsy-proven lymphocytic myocarditis, indicating that the identification of SARS-CoV-2 in the respiratory tract is insufficient to prove that clinically suspected myocarditis is caused by SARS-CoV-2.133 Furthermore, the epidemiological features of COVID-19 do not fit well with the ‘classical’ biopsy-proven myocarditis. According to the current ESC guidelines, the diagnosis of viral myocarditis is a diagnosis of exclusion made with certainty only in the case when a viral genome is proven in endomyocardial specimens along with the histological findings of active myocarditis.137 SARS-CoV-2 infection of induced pluripotent stem cell-derived cardiomyocytes has been shown in vitro18 and SARS‐CoV‐2 genome has been identified in endomyocardial biopsies of patients with suspected myocarditis.135 However, there is no direct evidence of SARS-CoV-2 within cardiomyocytes as virus presence has been documented in interstitial cells within cardiac tissue but not in cardiomyocytes, suggesting that viral genome presence was due to infected macrophage migration.138
Recently, rare and self-limiting cases of myocarditis with temporal association to immunization with an mRNA-based COVID-19 vaccine have been reported, especially in young men (mean age 25 years old).139,140 Data from the Israeli Ministry of Health suggest a crude incidence rate of approximately 24 cases per million following a second dose.139,140 Still, the true incidence of this adverse event is unknown at this time. Although the specific mechanisms are unclear an immune-mediated mechanism is likely.141
In summary, to date, there is scarce evidence supporting direct myocardial injury through COVID 19 infection. Given the risks of COVID-19, including the risk of myocardial injury from COVID-19 infection, concerns about rare or even extremely rare adverse events following immunization should not undermine confidence in the value of vaccination.
Thromboembolism in patients with COVID-19
Coagulation abnormalities including arterial and especially VTE are recognised features of severe COVID-19 infection, manifesting in deep venous thrombosis, pulmonary embolism, and DIC. As discussed above, inflammation, endothelial activation, increased platelet reactivity, NETosis, alterations in coagulation factors, and stasis predispose to both arterial and venous thrombosis. In the setting of COVID-19 several studies have shown that the hyperinflammatory state may lead to pulmonary microthrombosis and pulmonary intravascular coagulopathy. Acquired antiphospholipid antibodies have been identified in 45–90% of COVID-19 patients, but the exact mechanism of antibody formation and its associated thrombogenicity remain unclear.142
Whilst all hospitalized patients are at risk of VTE, those with ARDS, severe sepsis and/or on ICU are at much higher risk, due to both patient-specific factors (including age, obesity, sepsis, hypoxia, due to concomitant respiratory or heart failure) and ICU-related factors (sedation, immobilization, vasopressors or central venous catheters). Coagulopathy is reflective of more severe disease and adverse prognosis, with DIC reported in 71% of COVID-19 patients who died compared to only 0.6% of survivors.119 Furthermore, fibrin-platelet microthrombi deposition in the pulmonary vasculature is apparent at autopsy in COVID-19 patients.143 Those presenting with myocardial injury appear to have elevated D-dimer, fibrinogen, low antithrombin levels, prothrombin time (PT), and activated partial thromboplastin time (APTT) compared to those without cardiac involvement.107
In recent meta-analyses, hospitalized patients have an overall estimated incidence of COVID-19 related VTE ranging from 15% to 21%. This is four-fold higher in critically ill patients admitted to the ICU compared with non-ICU settings (23–31% vs. 7–9%).144–146 Studies have also shown that age and coagulopathy, defined as spontaneous prolongation of PT > 3 s or APTT > 5 s, are associated with thrombotic complications and higher mortality.7,147 Furthermore, the true incidence of VTE may be underappreciated as it is often challenging to detect it in ICU patients. Moreover, pulmonary embolism may be under-diagnosed since respiratory deterioration is a prominent feature of the concomitant ARDS. The increased risk of thromboembolism that is known to be associated with COVID-19 can be appreciated also in other clinical conditions.148,149 The overall incidence of ischaemic stroke and MI is reported to be nearly 4% across studies.7,146 In a single-centre case series, 20 patients with COVID-19 developed acute limb ischaemia over a 3-month period.149 In a multicentre case-series of 209 critical COVID-19 patients, 9.6% developed atypical severe arterial thrombotic events.148 Of note, thrombosis occurred mainly in non-atherosclerotic vessels148 and successful revascularization was lower than expected probably due to the immunothrombosis model.149
In order to mitigate the prothrombotic state associated with COVID-19, guideline and consensus statements recommends standard thromboprophylaxis with low-molecular weight heparin (LMWH), unfractionated heparin, or fondaparinux over oral anticoagulants, in the absence of contraindications, in all acutely hospitalized patients with COVID-19.33,150,151 Unfractionated heparin and LMWH have anti-inflammatory effects being able to down-regulate TNF-α induced inflammatory responses and partially inhibit IL-6, and IL-8 release.152,153 Some studies have reported that heparin bind to the S protein of SARS-CoV-2, thus potentially blocking cellular invasion.154,155 Fibrinolytic therapy with tissue plasminogen activator (tPA) in refractory COVID-19 acute lung injury and ARDS has been reported to be associated with improved oxygenation, ventilation, and haemodynamic status,156 which supports that fibrin deposition in the airspaces and lung parenchyma, along with fibrin-platelet microthrombi in the pulmonary microvasculature contributes to ARDS and right heart failure.102,104,143 However, optimal thromboprophylaxis including regimen, intensity, and duration have yet to be established. Several other consensus statements, guidelines and reviews have also made similar recommendations for thromboprophylaxis in COVID-19 especially in hospitalized patients.150 Of note, the role of direct oral anticoagulants is still unproven. Nevertheless, they are increasingly adopted. Similarly, the role of fibrinolytic therapy for critically ill patients remains to be established. Results of ongoing randomized clinical trials will help to clarify these uncertainties.157
Acute heart failure: the right ventricle in COVID-19
A growing number of studies show evidence of heart failure in COVID-19 patients even without pre-existent cardiovascular diseases.26 Cardiac involvement in patients infected with SARS-CoV-2 may manifest as acute COVID-19 cardiovascular syndrome (ACovCS) that among other presentations also encompasses the whole spectrum of acute heart failure symptoms.158 Among hospitalized patients with COVID-19 the reported rates of acute heart failure varied from 23% to 33%.84,108 As previously mentioned acute heart failure may be due to negative inotropic effects of cytokines and pro-inflammatory ACE/angiotensin II, or myocardial injury.
However, in the setting of COVID-19 the right ventricle is at higher risk of failure due to its physiological relationship with the pulmonary circulation. Right ventricular (RV) dysfunction and failure may contribute to the rapid haemodynamic deterioration, arrhythmias, and sudden death seen in patients with COVID-19. Early post-mortem studies from severe COVID-19 patients showed evidence of RV dilatation.104,159 As the pandemic progressed, larger echocardiographic studies demonstrated that COVID-19 patients had RV dilation (12 to 15%), RV dysfunction (16–35%), and elevated pulmonary artery systolic pressure, even in the absence of known cardiomyopathy.160–165 In these patient’s adverse RV remodelling was associated with over two-fold increase in mortality risk.161,165 Additionally, many severe COVID-19 patients require positive pressure ventilation, which in turn affects preload, afterload and ventricular compliance and may further contribute to RV failure.
In summary, these observations highlight the clinical implications of RV dysfunction assessments and the possibility to risk-stratify COVID-19 patients based on this assessment.166–168
Arrhythmic manifestations
Arrhythmias are a common complication in patients with COVID-19. Early case-series of hospitalized patients reported rates ranged from 8–17% and 44–60% in ICU setting and fatal cases, respectively.169–173 In a recent international large survey of over 4500 patients, arrhythmias occurred in 18% of cases, with atrial fibrillation/flutter being the most common disorder in COVID-19.174 Atrial fibrillation/flutter, left bundle branch block, electrocardiogram (ECG) signs suggesting acute right ventricular pressure overload (e.g. right bundle branch block or S1Q3T3 pattern), premature ventricular contractions, and ST-segment deviation have been all associated with elevated troponin levels and mortality, in COVID-19 pateints.175 Life-threatening arrhythmias (ventricular tachycardia/ventricular fibrillation) can occur in 4–6% of hospitalized COVID-19 patients and are more common in those with elevated cardiac troponins27,174 thus the diagnostic workup for cardiac injury should be always accompanied by concurrent rhythm monitoring.176
Although the exact nature of these arrhythmias is currently unknown, there are several mechanisms by which arrhythmias may occur in COVID-19. Five pathophysiological conditions align with the clinical course of COVID-19 and may predispose to arrhythmias: (i) pre-existing pro-arrhythmic conditions (structural heart disease, ion channel disorders)177; (ii) direct cardiotropic effects of the SARS-CoV-2 virus or hyperinflammation response it evokes. Cytokines such as, IL 2, IL-6, and IL-8 as well as TNF-α may cause heart rhythm disorders.178,179 Cytokines may favour the development of long QT syndrome (LQTS) by affecting the function of the cardiomyocyte K+ and Ca2+ ion channels (inflammatory cardiac channelopathies).180 IL-6 enhances the L-type Ca2+ current and inhibits the rapidly activating repolarizing K+ current by targeting the human Ether-à-go-go-Related Gene (hERG) thus prolonging ventricular action potential duration.180 In addition, inflammation-associated tachycardia resulting either from increased sympathetic activation of β-adrenergic receptors,181 or direct activation of cardiac pacemaker cells by cytokines,182 may precipitate life-threatening arrhythmias, especially in patients with underlying heart disease. Beta-blockers were associated with a reduced risk of death in critically ill patients with COVID-19183; however, a protective effect needs to be confirmed in prospective studies. Ongoing studies will also determine if selected immune proteins may qualify as biomarkers for an increased arrhythmogenic risk or immunomodulating therapy; (iii) cardiorespiratory instability requiring critical care and positive pressure ventilation.176,184 Arrhythmias may indicate worsening of the patient’s underlying condition. Electrolyte abnormalities due to rapidly worsening renal function may act as potential triggers and should be closely controlled. Nevertheless, whether the incidence of arrhythmias is higher in COVID-19 than in other conditions of cardiorespiratory distress is currently unknown; (iv) medical therapy with QT-prolonging drugs. Several explorative treatments for COVID-19 such as hydroxychloroquine and azithromycin, may induce QT-prolonging culminating in torsades de pointes.185 A baseline ECG is warranted, if patients are receiving antiarrhythmic or psychotropics therapy. More importantly, QT-prolonging drugs, should be reconsidered if QTc >500 ms or QTc increase by ≥60 ms.33,176 (v) finally, residual myocardial dysfunction and arrhythmic risk following COVID-19 with cardiac involvement. In analogy to myocarditis, patients with reduced left ventricular ejection fraction, persistent ECG changes or cardiovascular magnetic resonance (CMR) evidence of fibrosis may qualify for long-term follow-up for potential arrhythmic complications post COVID-19.186 In this regard, digital health and remote monitoring has been accelerated by the pandemic, providing an opportunity to enhance the use of remote services in everyday medical practice worldwide.176
Cardiac arrest
Cardiac arrest, either in or out of hospital, is common in critically ill patients with COVID-19 and is associated with poor survival, particularly among women and men aged 80 or older.127,187 Initial experience from a tertiary teaching hospital in Wuhan, China, has demonstrated a very poor survival after in hospital cardiac arrest (IHCA).188 Only 4 out of 136 patients with IHCA survived for 30 days and only 1 with a favourable neurological outcome even though 93% of the patients were monitored and resuscitation was initiated in less than 1 min in 89%. A recent study from Sweden included 3027 people who suffered a cardiac arrest (OHCA 64.3% and IHCA 35.7%). COVID-19 patients, had a 3.4-fold and 2.3-fold increased risk of 30-day mortality after an OHCA and IHCA, respectively, compared with non-infected cases.127 Of note this study showed that witnessed IHCA were less common in COVID-19 cases, as were in-hospital ECG monitoring, shockable rhythm and defibrillations,127 highlighting the need for rhythm monitoring which is potentially life-saving.176 Respiratory failure and prothrombotic events that have been extensively described in patients with COVID-19 are probably major contributors to in-hospital cardiac arrest in this setting. Although there is no direct evidence that SARS-CoV-2 directly causes cardiac arrest, cytokine storm could contribute to multi-organ dysfunction and cardiac arrest. Some previous observations may strengthen such hypothesis. Thus, cardiac arrest and subsequent resuscitation is often followed by the so called ‘post cardiac arrest syndrome’ (PCAS).189 A dominating feature of the PCAS is a systemic inflammatory response syndrome with high levels of cytokines circulating in the blood associated with endothelial activation and endothelial injury.190,191 Adding COVID-19 to PCAS the systemic inflammatory response may be more pronounced. Further in a recent phase II trial, blocking of IL-6 signalling pathway with tocilizumab, reduced systemic inflammation after cardiac arrest and showed an apparent cardioprotective effect.192 The same reasoning applies to LQTS and Torsades de Pointes.174,180
Finally, in high prevalence areas it reasonable to encourage compression only resuscitation and public access defibrillation of adults with OHCA for lay people, as it has already been implemented in many first responder programmes in Europe.193,194
Sex differences of cardiovascular injury in COVID-19 and potential mechanism of sexual dimorphism
Robust sex-specific risk estimates for confirmed infection and preliminary case fatality for COVID19 are still lacking, with available data likely biased by incomplete outcome data and differences in testing policies within and between countries. Growing evidence in USA and western European countries documented a greater susceptibility to SARS-COV-2 infection among women compared with men at least in those aged up to 50 years. In contrast, men across all ages are 20% more likely than women to be hospitalized with COVID-19, to require intensive care and are reported to have a 1.74-fold increased risk of mortality compared with women.195,196 Similarly, hyperinflammation and myocardial injury are more pronounced in men.197 On the opposite, COVID-19-related endotheliopathy and thrombosis were not found in clinical studies so far.197 The reasons behind this increased risk are not completely understood. A possible explanation of the observed effect on mortality after infection with SARS-COV-2 is that comorbidities, such as hypertension, cardiovascular disease, chronic lung diseases, and tobacco smoking are more common among men than women.197 Alternatively, the finding of increased COVID-19 infection among young women and the higher risk of severe disease and death among men in all age groups suggests a potential role for sex differences in biology and pathophysiology in COVID-19 infection. Yet, several studies have hypothesized that sex differences in COVID-19 may result from an interplay between preexisting comorbidities and sex-based biological factors, including sex chromosomes, sex hormones, and genomic and epigenetic differences, underlying viral entry and the immune response, which in turn also modulate cardiovascular disease. Some of these observations require further discussion.
Androgen signalling up-regulate ACE2 and TMPRSS2 expression in pulmonary and prostate tissues.198 Androgen-deprivation therapy/androgen receptor antagonists have shown to reduce the SARS-CoV-2 S-mediated cellular entry.198 Similarly, oestrogen can up-regulate the expression of ACE2 in human atrial tissue and has shown immune modulating activity.195,199 In a pilot trial, progesterone therapy reduced the need for supplemental oxygen and hospitalization. Therefore, the effects of oestrogen on ACE2 expression may have paradoxical effects, aiding COVID-19 viral infection, yet conversely limiting viral pathogenicity.200 These insights could, at least partially, account for the better outcome and the lower myocardial injury and death rate in women compared with their male counterparts.
Furthermore, the gene encoding ACE2 is located on the X chromosome and is regulated by oestrogens.201 Inactivation silences transcription from one of the two X chromosomes in women (XX) and avoids redundant gene expression compared with men (XY). However, the silencing is not complete but about 10% of the genes escape the inactivation.201 Thus, XX cells over-express genes encoding ACE2 in women.201 Studies are mandatory to evaluate the role of inactivation of transcription of X genes, and of their regulators, which might represent a major challenge to understand the sex-specific pathogenic determinants of COVID-19 disease progression.
In addition, it is known that innate and acquired immune responses are more intense and stronger in women than in men. This can provide women with a more effective tool to fight infective pathogens, favouring viral clearance. There are a variety of X-linked genes, such as IL-13, IL-4, IL-10, XIST, TLR7, FOXP3, which may underlie sexually dimorphic responses that contribute to stronger cellular, and humoral immune responses which also enhances the susceptibility of women to autoimmune diseases in women compared with men.201 For example, recognition of viral RNA by TLR 7 is enhanced in women compared with men leading to a more robust, type I IFN secretion and response. Women show higher neutrophil and macrophage phagocytic capacity and IL-10 production, higher B-cell numbers, and antibody production and higher number of CD4+ T cells and activated T cells and T-cell proliferation than men.202
Sex is known to be associated with longevity. Immune-inflammatory responses play a key role in successful ageing. While men are usually physically stronger, women live longer. The variation in sex hormones levels over the course of life may partially contributes to sex differences in immune profiles and disease susceptibility to infection at different ages.195 Aging induces a decline in the proportion of naïve T cells and enhanced monocyte and cytotoxic cell functions that is more prominent in men, and a male-specific B cells decline after age 65 years old.202,203 In addition, a trend of age-related decrease was observed in the production of some cytokines. In particular, the rate of decline in IL-10 is greater in men than in women. Because IL-10 acts as an immune-inflammatory suppressor,204 this relatively lesser production can be consistent with the fact that the age-related decline of various immunological parameters is less pronounced in women than in men.202,203
In sum, unless the effects of biological sex are studied, we will continue to have gaps in the knowledge, which may result in missed opportunities for a better health care system response to the pandemic of COVID-19. Having greater awareness of the roles that sex may play, may guide personalized preventive measures and therapeutic options in women and men.
Therapy and clinical trials: where are we with treatments?
The urgent need for effective treatments has resulted in the implementation of potential therapies lacking strong scientific evidence. There are thousands of clinical trials investigating treatments and preventative measures for COVID-19. We summarize the most important features.
Remdesivir
Following the results of the Adaptive COVID-19 Treatment Trial (ACTT)-1 and 2 supportive trials GS-US-540-5774 and GS-US-540-5773, The European Medicines Agency (EMA), approved a conditional marketing authorization remdesivir for the treatment of COVID-19 in adults with pneumonia who require supplemental oxygen.205–207 The ACTT-1 which had the most robust study design, provided the most convincing evidence reporting a shorter time to recovery in the remdesivir group when compared with the placebo group (10 vs. 5 days), no differences in mortality risk were observed. Yet, on November 2020, the WHO issued a conditional recommendation against the use of remdesivir in hospitalized patients, regardless of disease severity, as there is currently no evidence that remdesivir improves survival and other outcomes in these patients.208 Interim results from the WHO Solidarity trial suggest that remdesivir has little or no effect on mortality in patients who are hospitalised with COVID-19.209 Larger randomized controlled trials (RCTs) are needed to approve or refute treatments that unintentionally may be damaging for the patients.
Corticosteroids
The Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial, a multicentre, randomized, open-label trial in hospitalized patients with COVID-19, showed that the mortality from COVID-19 was lower in patients who were randomized to receive dexamethasone than among those who received the standard of care.210,211 However, in the subgroup of participants who did not require supplemental oxygen at enrolment, no survival benefit was observed for dexamethasone. Thus, WHO has recommended dexamethasone plus remdesivir or dexamethasone alone only for hospitalized patients with severe or critical COVID-19.208,211 If dexamethasone is not available, alternative glucocorticoids such as prednisone, methylprednisolone, or hydrocortisone, may be used instead.208,211
Recently, the Steroids in COVID-19 (STOIC), a phase 2, open-label, randomised controlled trial, showed that early administration of inhaled budesonide when compared with usual care, reduced the likelihood of needing urgent medical care and reduced time to recovery in adult’s outpatients with mild COVID-19.212 However, STOIC data are insufficient and cannot exclude the possibility of harm from the use of inhaled corticosteroids, such as budesonide or ciclesonide, in outpatients with mild COVID-19 who have normal oxygen levels. As such EMA advise against the use of inhaled corticosteroids in this population.213 Therefore, more robust evidence from clinical trials is still needed, to establish the benefits of inhaled corticosteroids in outpatients with COVID-19.
Chloroquine/hydroxychloroquine, azithromycin, lopinavir/ritonavir
In the early phase of the pandemic hydroxychloroquine and chloroquine were widely used for COVID-19 patients. These two drugs have been used for decades in therapy and control of malaria and autoimmune diseases. Small early trials that evaluated hydroxychloroquine demonstrated no clinical benefits.208,214,215 The subsequent large multicentre RECOVERY trial showed that the 28-day mortality rates of hospitalized patients with COVID-19 in the hydroxychloroquine treatment group were even higher than those in the usual-care group (62.9% vs. 59.6%).214 Furthermore, combined use of hydroxychloroquine and the antibiotic azithromycin may prolong the QT-interval resulting in an increased risk of sudden death, and other adverse events.13 Following a review of emerging data from the RECOVERY trial, there was also no beneficial effect of lopinavir/ritonavir on 28-day mortality in patients hospitalised with COVID-19 compared to usual care alone.216 These data were confirmed by the Interim WHO Solidarity Trial.209 This trial concluded that remdesivir, hydroxychloroquine, lopinavir, and interferon regimens had little or no effect on COVID-19 mortality, initiation of ventilation, and duration of hospital stay.209 These disappointing results highlight the question whether it is appropriate to use any drug on COVID-19 patients before large-scale RCTs are completed.
Inhospital immunomodulatory therapies
The intense hyperinflammatory response to viral infections, led in the early stages of the pandemic to the drug repurposing of several agents able to modulate the immune response, including IL-1 (anakinra) or IL-6 (sarilumab, siltuximab, tocilizumab) inhibitors.5 Recent trials of these immunomodulatory therapies showed conflicting results.217–221 Tocilizumab intervention was frequently associated with improved outcomes and reduced mortality, whereas evidence for the efficacy of anakinra, siltuximab, or sarilumab in COVID-19 is currently insufficient217–221 An important concern on IL blockade in patients with COVID-19 is the risk of mid and long-term adverse events from secondary infections which is still under investigation. Further research is needed to identify participant and disease characteristics where immunomodulatory therapy is likely to be of maximal benefit, perhaps exploring the relationship of the effects of such drugs with baseline inflammatory biomarkers such as IL-1, IL-6 and CRP and myocardial healing.
Neutralizing monoclonal antibodies for high risk COVID-19 outpatients
Data suggesting that persistent SARS-CoV-2 replication portends severity of COVID-19 led to the development of treatments with the aim to prevent the progression of COVID-19 from the beginning of infection. In three trials early treatment with neutralizing monoclonal antibodies (mAb) REGN-COV2 (combination of casirivimab and imdevimab) or a combination of bamlanivimab and etesevimab significantly reduced SARS-CoV-2 viral load, COVID-19-related hospitalization and death compared to placebo in outpatients with recently diagnosed COVID-19 without need of supplemental oxygen.222–224 No benefit and possible worse clinical outcomes were shown in hospitalized patients requiring high flow oxygen or mechanical ventilation, most likely because inflammation and thrombosis, rather than viral replication, play a greater role in later stages of the disease.222–224
The EMA granted a conditional marketing authorization and FDA approved these neutralizing mAbs with an emergency use authorization in mild to moderate COVID-19 patients aged 12 years and older that do not require supplemental oxygen for COVID-19 and who are at high risk of progressing to severe COVID-19.225–228
SARS-CoV-2 mAbs have the potential to be used for both prevention and treatment of infection, as they are designed to block viral attachment and entry into human cells, thus neutralizing the virus. Bamlanivimab/etesevimab and casirivimab/imdevimab are recombinant, neutralizing human IgG1 mAb which are unmodified in the Fc regions. The mAbs bind to different sites on the receptor binding domain of the spike protein of SARS-CoV-2, blocking the binding of the virus to the ACE2 host cell surface receptor.229 Several factors still limit the successful contribution of approved mAbs to the control of the COVID-19 outbreak including the need for very-large-scale manufacturing and the need to rapidly shift to modalities of administration not requiring hospital settings.
Serine protease inhibitor therapy
Camostat mesylate and nafamostat mesylate are clinically proven inhibitors of TMPRSS2, used for the treatment of pancreatitis and DIC. Recently, both compounds have been identified as a promising antiviral therapy for COVID-19.230 Animal and in vitro human cell studies have shown that nafamostat mesylate, camostat mesylate, and its active metabolite 4-(4-guanidinobenzoyloxy)phenylacetic acid (GBPA), blocks TMPRSS2 thus inhibiting viral protein S priming and hence virus-cell membrane fusion.14,198,230 Moreover, animal studies have shown that camostat mesylate may reduce transforming growth factor-β production and associated fibrosis.231 Nevertheless in a recent small multicentre RCT, 200 mg camostat mesylate failed to show clinical improvement, progression to ICU admission or mortality when compared with placebo in hospitalized patients with COVID-19.232 Ongoing clinical trials will help to assess whether camostat mesylate or nafamostat mesylate administered in higher doses or during the very early phase of COVID-19 might be effective in reducing disease progression.
Cell-based therapy in COVID-19
Mesenchymal stem cells (MSCs) and cardiosphere-derived cells (CDCs), have been widely studied for clinical application in regenerative medicine and for their anti-inflammatory, immunomodulatory, anti-fibrotic and regenerative properties.233 MSCs can be isolated and grown from multiple human tissues, including the human umbilical cord (hUC).233 CDCs are intrinsic cardiac stem cells, with a distinctive antigenic profile (CD105+, CD45−, CD90low) and contain a small minority of c-kit+ cells putative cardiac progenitors.233,234 It has been hypothesized that MSCs and CDCs could reduce inflammation, ARDS and attenuate scar formation and fibrosis after myocardial injury in COVID-19.234–237 Furthermore, because they express low levels of ACE2 and TMPRSS2, MSCs and CDCs are thought to be resistant to SARS-CoV-2 infection.236,238
Data supporting the use of intravenous hUC-MSCs in patients with COVID-19 are limited to small pilot open-label uncontrolled trials.235–237 These studies reported improvement of inflammatory biomarkers such as CRP and cytokines,235–237 improved survival237 as well as a potential to reduce fibrosis associated with post-acute COVID-19.236,237 It should be noted, however, that results did not reach statistical significance. Data supporting intravenous allogeneic CDCs (known as CAP-1002) are limited to a single compassionate-use cohort of 6 severe COVID-19 patients pre-treated with tocilizumab.234 The study reported a good safety and tolerability profile of CAP-1002, followed by improvement in clinical status, pro-inflammatory biomarkers, cardiac troponin and D-dimer levels in most patients during hospitalization.234
Interpretation of these studies is further limited lack of randomization,234–236 small sample size,234–237 and shift in eligibility criteria from enrolling solely patients on invasive mechanical ventilation to including those on non-invasive ventilation.237 Moreover, a concern on cell-based therapy is the safety profile at long-term follow-up.
To date, no MSCs or CDCs products are approved for the treatment of COVID-19. Multiple ongoing trials, including the Intravenous Infusion of CAP-1002 in Patients With COVID-19 (INSPIRE) trial will help to assess the role of cell-based therapy for the treatment of COVID-19.
Post-acute sequelae of COVID-19
A large proportion of patients who have been infected from SARS-CoV-2 do not fully recover in the months after hospital discharge and continue experiencing debilitating symptoms such as fatigue, dyspnoea, chest pain, palpitations, thromboembolic events, myalgia, anxiety, depression and impaired quality of life.2 These symptoms, often referred to as ‘Long COVID’ or ‘Post-acute COVID-19 syndrome’, can persist for months in the absence of detectable viral infection and vary in form and severity. Recent data have shown that over 13% of infected individuals are likely to report symptoms of post-acute COVID-19 that persist over 4 weeks, 4.5% over 8 weeks, and 2.3% of individuals report symptoms over 12 weeks.239 These post-acute effects of COVID-19 are a matter of significant concern, as they potentially affect millions of people worldwide, increasing healthcare costs and disability.
The first major challenge in treatment of post-acute COVID-19 is establishing a universally accepted definition still need to be established. Recently, the NIH has proposed the term ‘Post-Acute Sequelae of SARS-CoV-2 infection (PASC)’ to collectively refer to these effects.3 Recent studies have suggested to include two categories to define the syndrome: (i) subacute or persistent symptomatic COVID-19, which includes signs and symptoms lasting from 4 to 12 weeks beyond acute infection and attributable to COVID-19; and (ii) chronic or post-COVID-19 syndrome, which includes signs and symptoms persisting or present beyond 12 weeks of the onset of acute COVID-19 and not attributable to alternative diagnoses.2,240–243
Reports on 2- to 6-month outcomes from hospital discharge showed that fatigue/muscle weakness (50–63%), cough (15%), dyspnoea/exertional dyspnoea (23–43%), arthralgias (27%), chest pain (22%), ongoing palpitations/arrhythmias (5%), loss of memory (34%), anxiety/depression (23%), concentration difficulties (28%), and sleep disorders (26–31%) were the most common patient-reported symptoms.244–248 Two recent large cohort studies showed that 14–30% of COVID-19 patients developed clinical sequelae that required medical care or hospital admission during the 4 months after the acute phase of the diseases.244,249
As the definition of long COVID or PASC is developing, the underlying causes of post-acute COVID-19 symptoms are poorly understood. Various mechanisms might be involved such as cellular injury due to direct viral invasion, systemic hyperinflammation, a procoagulant state leading to post-inflammatory cardiac and pulmonary fibrosis, impairment of pulmonary diffusion capacity, cardiac dysfunction, partially dissolved in situ thrombotic microangiopathy or emboli with flow limitation, and post-acute thromboembolism.243,250,251 Time course progression and most frequent symptoms and complications of post-acute COVID-19 syndrome are summarized in Figure 4.
Figure 4.
Post-acute sequelae of SARS-CoV-2 infection. As for the current literature, post-acute sequelae of SARS-CoV-2 infection may be defined as persistent signs and symptoms or long-term complications beyond 4 weeks from symptoms onset. The most frequent symptoms and complications are summarized in the figure. Figure created with BioRender.com.
Potential mechanisms of post-acute COVID-19
Post-acute COVID-19 may very well have multiple causes. For example, autoantibodies may have a role. Perhaps viral reservoirs or lingering fragments of viral RNA or proteins contribute to the condition. Systemic inflammatory response to COVID-19, involving IL-1, IL-6, and TNF-α have the potential to increase myocardial fibrosis in cardiac remodelling.252,253 Emerging evidence suggest that post-acute COVID-19 symptoms could be caused also by inappropriate sinus tachycardia (IST) and postural orthostatic tachycardia syndrome (PoTS).254,255 Autonomic dysfunction after viral infection, resulting in IST and PoTS, has previously been reported in SARS-CoV-1 infection.256 These are likely the result of increased catecholaminergic state and inflammatory cytokines such as IL-1, Il-6, TNF-α and autoantibodies that target cardiac Ca2+, K+ or Na+ channels leading to arrhythmogenic effects in the absence of evident changes in the myocardium.180 In summary, the exact cause of post-acute COVID-19 is currently unknown and it will take substantial efforts to uncover mechanisms invoked. This may require a multidisciplinary approach considering the multiple targets being affected by COVID-19. Below we will report early approaches to this issue.
Cardiac sequelae and complications
There is a bidirectional relationship between COVID-19 and the heart. Patients living with cardiovascular diseases are at higher risk of severe COVID-19 and death. On the other hand, myocardial oedema, fibrosis and related complications are observed in patients recovering from COVID-19.257 CMR data suggest that cardiac involvement is present in approximately 80% of patients and ongoing myocardial inflammation in 60% of patients, at a median time interval of 71 days since COVID-19 diagnosis, even in asymptomatic patients.258 Of note, when compared with healthy controls, patients who have recovered from COVID-19 have lower left ventricular ejection fraction, higher left ventricular volumes, late gadolinium enhancement (LGE) reflecting irreversible previous myocardial injury (necroptosis, fibrosis), and pericardial enhancement indicating pericardial inflammation. Additionally, these patients show raised native T1 signal suggesting expansion of the interstitial space due to fibrosis and native T2 signal suggesting myocardial oedema or necrosis. These findings correlate with higher levels of high-sensitivity troponin.114 In addition, active lymphocytic inflammation was observed in a subgroup of patients who underwent endomyocardial biopsy.258 Similar results were reported in other small studies of patients who recovered from COVID-19259–261 It should be noted that up to 12% of these patients had a history of coronary revascularization or MI.261 In contrast, another study did not show evidence of myocarditis, although CMR signs of subtle changes in myocardial structure and function and resolving pericardial inflammation were present in 30% of cases.262
Taken together, these observations support the hypothesis that abnormalities of myocardial tissue identified by CMR are common during COVID-19 recovery. These observations of myocardial fibrosis are worrisome, as resulting heart failure can lead to cardiac arrhythmias.
Yet, a raised T1 signal on CMR is not specific for oedema or acute myocardial inflammation, as it is observed in diffuse fibrosis or infiltration. Likewise, LGE reflects previous myocardial injury of any age.263 Furthermore, the differentiation of ischaemic or non-ischaemic LGE in high-risk patients may reflect events prior to SARS-CoV-2 infection. For example, it is well known that 15% to 33% of patients with at least one cardiovascular risk factor have silent ischaemia, and potentially may have ischaemic LGE.264,265
Imaging abnormalities and risk of future cardiac events
The relationship between imaging abnormalities and risk of future cardiac events are a matter of future research. A systematic evaluation of myocardial fibrosis (imaging/histology) may guide post-acute follow-up in COVID-19 patients with cardiac involvement and is clearly warranted. In addition, innovative biomarkers for cardiovascular disease are also warranted. In this regard circulating RNAs biomarkers represent a valuable tool due to their biological relevance, dynamic regulation in response to disease, tissue-specificity, and accessibility. For instance, a recent study showed that has-miR-Chr8:96, a human microRNA, was able to distinguish patients with myocarditis from those with MI with a sensitivity and specificity of over 90%.266
Post-acute pulmonary manifestations and risk future of cardiac events
Cohort studies have shown that at 6-month follow-up chest CT, residual ground-glass opacification and progression of fibrotic-like changes were present in one third of patients.243,250 Additionally, impaired pulmonary diffusion capacity was the most common physiological finding occurring more frequently in those patients with fibrosis-like changes, suggesting unresolved microvascular injury.243,250,251
Some investigators have proposed a combined physiological approach to follow-up imaging to determine tissue perfusion, such as novel CT perfusion methods and combinations of standard methods of ventilation/perfusion (VQ) single-photon emission computed tomography with CT pulmonary angiogram, with the potential to inform the underlying pathophysiology of prolonged symptoms and therapeutic strategies.
Given the patterns of in situ thrombotic microangiopathy and vascular endotheliitis the impact of residual thrombus burden and potential haemodynamic sequelae such as chronic thromboembolic embolism, chronic pulmonary hypertension and adverse RV remodelling in COVID-19 remain a topic of future research.267
Post-acute thromboembolic events
Most investigations have focused on the risk of thromboembolic events during the acute COVID-19 phase, while a few have focused on the post-acute phase of the disease. Current evidence shows conflicting results. In one study, 45-day post-discharge cumulative risk of VTE was 0.2%.268 In another cohort, rates of VTE post-discharge were reported to be 4.8 per 1000 discharges and were not significantly different from post-discharge VTE associated with other acute diseases in 2019.269 In a single-centre study, the cumulative incidence of thrombosis (including, pulmonary embolism, intracardiac thrombus, and ischaemic stroke) at day 30 post-discharge was 2.5%.270 Similar results were reported in another cohort.271
As described above the COVID-19 related thrombosis suggests an immunothrombotic pathophysiology either directly by interacting with ACE2 receptor or indirectly by triggering hyperinflammation (Figure 3). Similarly, the risk of post-acute COVID-19 thrombotic events may be linked to the duration and the severity of hyperinflammation. Unfortunately, lack of data on the duration of the hyperinflammatory state after the acute phase, and lack of large prospective cohorts and randomized controlled trials, limits our ability to risk stratify post-acute thromboembolic events, highlighting the need to answer the unsettled question of extended post-discharge thromboprophylaxis.
Metabolic sequelae of COVID-19 and diabetes
The relationship between COVID-19 and diabetes is complex and bidirectional. Patients with diabetes are at increased risk of severe COVID-19 and mortality. In turn, COVID-19 disrupts glucose metabolism which is a known feature of systemic infections. New-onset diabetes and severe complications of pre-existing diabetes such as insulin resistance, diabetic ketoacidosis, hyperosmolarity, microvascular and macrovascular complications have been described in patients with COVID-19.272–275 Similarly, during the SARS-CoV-1 outbreak, acute diabetes was frequently reported in patients with no history of diabetes or steroid use.276 ACE-2 and TMPRSS2 are expressed in pancreatic β cells,277 but whether this is sufficient to trigger new-onset diabetes in COVID-19 is uncertain.278 One study showed that SARS-CoV-2 infects and replicates in human pancreatic islet cultures inducing morphological, transcriptional and functional changes, including reduced numbers of insulin-secretory granules in β cells and impaired glucose-stimulated insulin secretion.277 This investigation also described detection of the N protein of the virus in pancreatic exocrine and homeobox protein NKX6.1-positive β cells, a transcription factor that plays a critical role in pancreatic β cell function and proliferation, in postmortem examinations. Another proposed mechanism include increased insulin resistance due to cytokinemia such as IL-6 and TNF-α, an oxidative stress storm, glycation of ACE2 receptors, activation of the Ang II–ACE2–MasR axis due to binding of ACE2 receptor of β-cells and vascular endothelial cell/pericyte cells promoting fibrosis through islet amyloid polypeptide and collagen types I and III deposition.274 These observations support the hypothesis of the potential diabetogenic effect of SARS-CoV-2 infection and are of particular concern given that diabetes promotes atherosclerosis and ischaemic heart disease.
Yet, there are several questions that remain unanswered: (i) What is the exact risk of new-onset diabetes in COVID-19? (ii) Does COVID-19 worsen the natural history of the disease in patients with pre-existing diabetes? (iii) Does COVID-19 increase long-term predisposition to diabetic ketoacidosis? and (iv) Can COVID-19-associated diabetes be reversed after the acute phase?
Conclusions and future directions
Given that we have only known about the SARS-CoV-2 for only one and a half year, it is actually quite remarkable how much we have learned about its epidemiology and pathophysiology. As we increase our understanding of the disease there is growing consensus that COVID-19 is a macro- and micro-vascular disease and as such the cardiovascular system is largely affected. While, both clinical and basic research has been very responsive to tackle the challenge, most questions, however, remain unsolved, as our understanding of the pathophysiology of the disease is still under evolving and needs to be addressed and expanded in future research efforts. The most pressing questions are:
What causes elderly patients, men and those with cardiometabolic risk factors to be at higher risk of severe—COVID-19? Observations suggest the importance of a ‘metabolic disease exposome’,279 including dietary lifestyle, glycaemic disorders, obesity, and sedentariness, among other potential disease severity modifiers such as systemic hypertension and aging, leading to chronic low grade inflammation, which may aggravate COVID-19-induced acute organ failure. Therefore, it is essential to precisely identify the factors underlying the severity and the clinical presentation of the disease, especially when considering the risk of COVID-19 epidemics.280 Aging has also a significant effect on the response to pharmacological interventions. It may be necessary to design trials that focus exclusively on elderly. Finally, ageing is associated to oxidative stress and immune-senescence impairing therefore the answer of the immune system against the viral insult. The study population of an RCT should ideally reflect the population that is at the highest risk of the disease and that is most difficult to treat in clinical practice.
How can we better address failure of the microcirculation in COVID-19 and personalize potential therapeutic approaches? Persistence of SARS-CoV-2 and viral RNA may act as potential viral reservoirs. They tend to induce an inflammatory response, stimulating endothelial dysfunction, accelerated atherosclerosis, hypercoagulability, and microvascular thrombosis. Thus, novel and prognostic biomarkers, combined with genetic differences and functional testing are required. To tackle the challenge, a large international interdisciplinary network of clinical and non-clinical scientists is needed. Initial examples of such cooperation is the EU-CardioRNA COST Action CA17129 which would try to identify RNA biomarkers combined with artificial intelligence.5,281
What will be the impact of myocardial injury on long-term functional status, quality of life and risk for arrhythmias? What makes some people more vulnerable than others? What are the biological mechanisms underlying this? Exercise intolerance, for example, is a condition that a cardiologist in this group of post-acute COVID patients faces. The diagnostic and prognostic role of pulmonary and myocardial fibrosis in COVID-19 remains to be established. The systematic follow-up of COVID-19 patients with a deep and complete clinical and biological phenotype will enable the identification of individuals at risk in order to provide personalized care and with the aim of preventing further vulnerability for-and exposure to long-term sequela.
Are SARS-CoV-2 infected persons without symptoms at a similar and proportional increased long-term risk of PASC compared with those with symptoms? Approximately 25% of individuals who had COVID-19 still have physical symptoms one month after they became ill, and about 10% have symptoms that persist after 12 weeks. COVID-19 is a ‘new disease’ that pushes the research community and the world more generally into ‘uncharted territories’. We should commit to set up a network of scientists and laboratories around Europe taking a multidisciplinary approach.
Authors’ contributions
E.C. and D.T. conceived and designed the manuscript, drafted the manuscript, and revised it for important intellectual content. L.B., R.B., M.J.C., G.D.L., C.d.W., D.D., M.D., D.J.D., E.C.E., D.A.G., C.H., F.R.H., K.H., O.M., D.M., E.O., T.P. D.T.Z., Z.V.P, M.V., and G.V. made substantial contributions to the conception and design of the manuscript, drafted the manuscript, and revised it for important intellectual content. All authors approved the final version of the manuscript.
Conflict of interest: None declared.
References
- 1. WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int/ (29 August 2021, date last accessed).
- 2. Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, Cook JR, Nordvig AS, Shalev D, Sehrawat TS, Ahluwalia N, Bikdeli B, Dietz D, Der-Nigoghossian C, Liyanage-Don N, Rosner GF, Bernstein EJ, Mohan S, Beckley AA, Seres DS, Choueiri TK, Uriel N, Ausiello JC, Accili D, Freedberg DE, Baldwin M, Schwartz A, Brodie D, Garcia CK, Elkind MSV, Connors JM, Bilezikian JP, Landry DW, Wan EY. Post-acute COVID-19 syndrome. Nat Med 2021;27:601–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. NIH launches new initiative to study “Long COVID”. https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nih-launches-new-initiative-study-long-covid (15 April 2021, date last accessed).
- 4. Group W. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health 2019;7:e1332–e1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Badimon L, Robinson EL, Jusic A, Carpusca I, de Windt LJ, Emanueli C, Ferdinandy P, Gu W, Gyongyosi M, Hackl M, Karaduzovic-Hadziabdic K, Lustrek M, Martelli F, Nham E, Potocnjak I, Satagopam V, Schneider R, Thum T, Devaux Y. Cardiovascular RNA markers and artificial intelligence may improve COVID-19 outcome: position paper from the EU-CardioRNA cost action CA17129. Cardiovasc Res 2021;117:1823–1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ; HLH Across Speciality Collaboration UK. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 2020;395:1033–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020;191:145–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Juni RP, Kuster DWD, Goebel M, Helmes M, Musters RJP, van der Velden J, Koolwijk P, Paulus WJ, van Hinsbergh VWM. Cardiac microvascular endothelial enhancement of cardiomyocyte function is impaired by inflammation and restored by empagliflozin. JACC Basic Transl Sci 2019;4:575–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Santos TM, Franci D, Gontijo-Coutinho CM, Ozahata TM, de Araújo Guerra Grangeia T, Matos-Souza JR, Carvalho-Filho MA. Inflammatory lung edema correlates with echocardiographic estimation of capillary wedge pressure in newly diagnosed septic patients. J Crit Care 2018;44:392–397. [DOI] [PubMed] [Google Scholar]
- 10. Jafarzadeh A, Jafarzadeh S, Nozari P, Mokhtari P, Nemati M. Lymphopenia an important immunological abnormality in patients with COVID-19: possible mechanisms. Scand J Immunol 2021;93:e12967. [DOI] [PubMed] [Google Scholar]
- 11. George MR. Hemophagocytic lymphohistiocytosis: review of etiologies and management. J Blood Med 2014;5:69–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020;579:270–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, Madhur MS, Tomaszewski M, Maffia P, D'Acquisto F, Nicklin SA, Marian AJ, Nosalski R, Murray EC, Guzik B, Berry C, Touyz RM, Kreutz R, Wang DW, Bhella D, Sagliocco O, Crea F, Thomson EC, McInnes IB. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res 2020;116:1666–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hoffmann M, Schroeder S, Kleine-Weber H, Muller MA, Drosten C, Pohlmann S. Nafamostat mesylate blocks activation of SARS-CoV-2: new treatment option for COVID-19. Antimicrob Agents Chemother 2020;64:e00754-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kreutz R, Algharably EAE, Azizi M, Dobrowolski P, Guzik T, Januszewicz A, Persu A, Prejbisz A, Riemer TG, Wang JG, Burnier M. Hypertension, the renin-angiotensin system, and the risk of lower respiratory tract infections and lung injury: implications for COVID-19. Cardiovasc Res 2020;116:1688–1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tipnis SR, Hooper NM, Hyde R, Karran E, Christie G, Turner AJ. A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase. J Biol Chem 2000;275:33238–33243. [DOI] [PubMed] [Google Scholar]
- 17. Ferrario CM, Ahmad S, Joyner J, Varagic J. Advances in the renin angiotensin system focus on angiotensin-converting enzyme 2 and angiotensin-(1-7). Adv Pharmacol 2010;59:197–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bojkova D, Wagner JUG, Shumliakivska M, Aslan GS, Saleem U, Hansen A, Luxan G, Gunther S, Pham MD, Krishnan J, Harter PN, Ermel UH, Frangakis AS, Milting H, Zeiher AM, Klingel K, Cinatl J, Dendorfer A, Eschenhagen T, Tschope C, Ciesek S, Dimmeler S. SARS-CoV-2 infects and induces cytotoxic effects in human cardiomyocytes. Cardiovasc Res 2020;116:2207–2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Murray E, Tomaszewski M, Guzik TJ. Binding of SARS-CoV-2 and angiotensin-converting enzyme 2: clinical implications. Cardiovasc Res 2020;116:e87–e89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Crackower MA, Sarao R, Oudit GY, Yagil C, Kozieradzki I, Scanga SE, Oliveira-dos-Santos AJ, da Costa J, Zhang L, Pei Y, Scholey J, Ferrario CM, Manoukian AS, Chappell MC, Backx PH, Yagil Y, Penninger JM. Angiotensin-converting enzyme 2 is an essential regulator of heart function. Nature 2002;417:822–828. [DOI] [PubMed] [Google Scholar]
- 21. Mechanick JI, Rosenson RS, Pinney SP, Mancini DM, Narula J, Fuster V. Coronavirus and cardiometabolic syndrome: JACC Focus Seminar. J Am Coll Cardiol 2020;76:2024–2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, Holden KA, Read JM, Dondelinger F, Carson G, Merson L, Lee J, Plotkin D, Sigfrid L, Halpin S, Jackson C, Gamble C, Horby PW, Nguyen-Van-Tam JS, Ho A, Russell CD, Dunning J, Openshaw PJ, Baillie JK, Semple MG; ISARIC4C investigators. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ 2020;369:m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell L, Chernyak Y, Tobin KA, Cerfolio RJ, Francois F, Horwitz LI. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ 2020;369:m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. O'Hearn M, Liu J, Cudhea F, Micha R, Mozaffarian D. Coronavirus disease 2019 hospitalizations attributable to cardiometabolic conditions in the United States: a comparative risk assessment analysis. J Am Heart Assoc 2021;10:e019259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet 2005;365:217–223. [DOI] [PubMed] [Google Scholar]
- 26. Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, Ma K, Xu D, Yu H, Wang H, Wang T, Guo W, Chen J, Ding C, Zhang X, Huang J, Han M, Li S, Luo X, Zhao J, Ning Q. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 2020;368:m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:811–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lippi G, Wong J, Henry BM. Hypertension in patients with coronavirus disease 2019 (COVID-19): a pooled analysis. Pol Arch Intern Med 2020;130:304–309. [DOI] [PubMed] [Google Scholar]
- 29. Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, Curtis HJ, Mehrkar A, Evans D, Inglesby P, Cockburn J, McDonald HI, MacKenna B, Tomlinson L, Douglas IJ, Rentsch CT, Mathur R, Wong AYS, Grieve R, Harrison D, Forbes H, Schultze A, Croker R, Parry J, Hester F, Harper S, Perera R, Evans SJW, Smeeth L, Goldacre B. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020;584:430–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jiang X, Eales JM, Scannali D, Nazgiewicz A, Prestes P, Maier M, Denniff M, Xu X, Saluja S, Cano-Gamez E, Wystrychowski W, Szulinska M, Antczak A, Byars S, Skrypnik D, Glyda M, Krol R, Zywiec J, Zukowska-Szczechowska E, Burrell LM, Woolf AS, Greenstein A, Bogdanski P, Keavney B, Morris AP, Heagerty A, Williams B, Harrap SB, Trynka G, Samani NJ, Guzik TJ, Charchar FJ, Tomaszewski M. Hypertension and renin-angiotensin system blockers are not associated with expression of angiotensin-converting enzyme 2 (ACE2) in the kidney. Eur Heart J 2020;41:4580–4588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hosseinzadeh R, Goharrizi M, Bahardoust M, Alvanegh AG, Ataee MR, Bagheri M, Navidiyan ES, Zijoud SRH, Heiat M. Should all patients with hypertension be worried about developing severe coronavirus disease 2019 (COVID-19)? Clin Hypertens 2021;27:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018;39:3021–3104. [DOI] [PubMed] [Google Scholar]
- 33. ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic. https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance#p03. Last updated on 10 June 2020 (03 June 2021, date last accessed).
- 34. Youn JC, Yu HT, Lim BJ, Koh MJ, Lee J, Chang DY, Choi YS, Lee SH, Kang SM, Jang Y, Yoo OJ, Shin EC, Park S. Immunosenescent CD8+ T cells and C-X-C chemokine receptor type 3 chemokines are increased in human hypertension. Hypertension 2013;62:126–133. [DOI] [PubMed] [Google Scholar]
- 35. Guzik TJ, Hoch NE, Brown KA, McCann LA, Rahman A, Dikalov S, Goronzy J, Weyand C, Harrison DG. Role of the T cell in the genesis of angiotensin II induced hypertension and vascular dysfunction. J Exp Med 2007;204:2449–2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Trump S, Lukassen S, Anker MS, Chua RL, Liebig J, Thurmann L, Corman VM, Binder M, Loske J, Klasa C, Krieger T, Hennig BP, Messingschlager M, Pott F, Kazmierski J, Twardziok S, Albrecht JP, Eils J, Hadzibegovic S, Lena A, Heidecker B, Burgel T, Steinfeldt J, Goffinet C, Kurth F, Witzenrath M, Volker MT, Muller SD, Liebert UG, Ishaque N, Kaderali L, Sander LE, Drosten C, Laudi S, Eils R, Conrad C, Landmesser U, Lehmann I. Hypertension delays viral clearance and exacerbates airway hyperinflammation in patients with COVID-19. Nat Biotechnol 2020;39:705–716. [DOI] [PubMed] [Google Scholar]
- 37. Milne S, Yang CX, Timens W, Bosse Y, Sin DD. SARS-CoV-2 receptor ACE2 gene expression and RAAS inhibitors. Lancet Respir Med 2020;8:e50–e51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sama IE, Ravera A, Santema BT, van Goor H, Ter Maaten JM, Cleland JGF, Rienstra M, Friedrich AW, Samani NJ, Ng LL, Dickstein K, Lang CC, Filippatos G, Anker SD, Ponikowski P, Metra M, van Veldhuisen DJ, Voors AA. Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors. Eur Heart J 2020;41:1810–1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Franceschi C, Santoro A, Capri M. The complex relationship between Immunosenescence and Inflammaging: special issue on the New Biomedical Perspectives. Semin Immunopathol 2020;42:517–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R; IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract 2019;157:107843. [DOI] [PubMed] [Google Scholar]
- 41. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Barron E, Bakhai C, Kar P, Weaver A, Bradley D, Ismail H, Knighton P, Holman N, Khunti K, Sattar N, Wareham NJ, Young B, Valabhji J. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. Lancet Diabetes Endocrinol 2020;8:813–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Dennis JM, Mateen BA, Sonabend R, Thomas NJ, Patel KA, Hattersley AT, Denaxas S, McGovern AP, Vollmer SJ. Type 2 diabetes and COVID-19-related mortality in the critical care setting: a National Cohort Study in England, March-July 2020. Diabetes Care 2021;44:50–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Clift AK, Coupland CAC, Keogh RH, Diaz-Ordaz K, Williamson E, Harrison EM, Hayward A, Hemingway H, Horby P, Mehta N, Benger J, Khunti K, Spiegelhalter D, Sheikh A, Valabhji J, Lyons RA, Robson J, Semple MG, Kee F, Johnson P, Jebb S, Williams T, Hippisley-Cox J. Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: national derivation and validation cohort study. BMJ 2020;371:m3731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020;8:475–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239–1242. [DOI] [PubMed] [Google Scholar]
- 47. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, Cereda D, Coluccello A, Foti G, Fumagalli R, Iotti G, Latronico N, Lorini L, Merler S, Natalini G, Piatti A, Ranieri MV, Scandroglio AM, Storti E, Cecconi M, Pesenti A; COVID-19 Lombardy ICU Network. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA 2020;323:1574–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Holman N, Knighton P, Kar P, O'Keefe J, Curley M, Weaver A, Barron E, Bakhai C, Khunti K, Wareham NJ, Sattar N, Young B, Valabhji J. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol 2020;8:823–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Zhu L, She ZG, Cheng X, Qin JJ, Zhang XJ, Cai J, Lei F, Wang H, Xie J, Wang W, Li H, Zhang P, Song X, Chen X, Xiang M, Zhang C, Bai L, Xiang D, Chen MM, Liu Y, Yan Y, Liu M, Mao W, Zou J, Liu L, Chen G, Luo P, Xiao B, Zhang C, Zhang Z, Lu Z, Wang J, Lu H, Xia X, Wang D, Liao X, Peng G, Ye P, Yang J, Yuan Y, Huang X, Guo J, Zhang BH, Li H. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab 2020;31:1068–1077.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. McGovern AP, Thomas NJ, Vollmer SJ, Hattersley AT, Mateen BA, Dennis JM. The disproportionate excess mortality risk of COVID-19 in younger people with diabetes warrants vaccination prioritisation. Diabetologia 2021;64:1184–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Fernandez C, Rysa J, Almgren P, Nilsson J, Engstrom G, Orho-Melander M, Ruskoaho H, Melander O. Plasma levels of the proprotein convertase furin and incidence of diabetes and mortality. J Intern Med 2018;284:377–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Codo AC, Davanzo GG, Monteiro LB, de Souza GF, Muraro SP, Virgilio-da-Silva JV, Prodonoff JS, Carregari VC, de Biagi Junior CAO, Crunfli F, Jimenez Restrepo JL, Vendramini PH, Reis-de-Oliveira G, Bispo Dos Santos K, Toledo-Teixeira DA, Parise PL, Martini MC, Marques RE, Carmo HR, Borin A, Coimbra LD, Boldrini VO, Brunetti NS, Vieira AS, Mansour E, Ulaf RG, Bernardes AF, Nunes TA, Ribeiro LC, Palma AC, Agrela MV, Moretti ML, Sposito AC, Pereira FB, Velloso LA, Vinolo MAR, Damasio A, Proenca-Modena JL, Carvalho RF, Mori MA, Martins-de-Souza D, Nakaya HI, Farias AS, Moraes-Vieira PM. Elevated glucose levels favor SARS-CoV-2 infection and monocyte response through a HIF-1alpha/glycolysis-dependent axis. Cell Metab 2020;32:437–446.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Liu H, Gai S, Wang X, Zeng J, Sun C, Zhao Y, Zheng Z. Single-cell analysis of SARS-CoV-2 receptor ACE2 and spike protein priming expression of proteases in the human heart. Cardiovasc Res 2020;116:1733–1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Papa G, Mallery DL, Albecka A, Welch LG, Cattin-Ortola J, Luptak J, Paul D, McMahon HT, Goodfellow IG, Carter A, Munro S, James LC. Furin cleavage of SARS-CoV-2 Spike promotes but is not essential for infection and cell-cell fusion. PLoS Pathog 2021;17:e1009246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Liu F, Long X, Zhang B, Zhang W, Chen X, Zhang Z. ACE2 expression in pancreas may cause pancreatic damage after SARS-CoV-2 infection. Clin Gastroenterol Hepatol 2020;18:2128–2130.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Roca-Ho H, Riera M, Palau V, Pascual J, Soler MJ. Characterization of ACE and ACE2 expression within different organs of the NOD mouse. Int J Mol Sci 2017;18:563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Guo W, Li M, Dong Y, Zhou H, Zhang Z, Tian C, Qin R, Wang H, Shen Y, Du K, Zhao L, Fan H, Luo S, Hu D. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev 2020;36:e3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol 2021;17:11–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Badimon L, Bugiardini R, Cenko E, Cubedo J, Dorobantu M, Duncker DJ, Estruch R, Milicic D, Tousoulis D, Vasiljevic Z, Vilahur G, De Wit C, Koller A. Position paper of the European Society of Cardiology-working group of coronary pathophysiology andmicrocirculation: obesity and heart disease. Eur Heart J 2017;38:1951–1958. [DOI] [PubMed] [Google Scholar]
- 60. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corra U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FDR, Lochen ML, Lollgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WMM, Binno S. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kim TS, Roslin M, Wang JJ, Kane J, Hirsch JS, Kim EJ; Northwell Health C-RC. BMI as a risk factor for clinical outcomes in patients hospitalized with COVID-19 in New York. Obesity (Silver Spring); 2021; 29:279–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kass DA, Duggal P, Cingolani O. Obesity could shift severe COVID-19 disease to younger ages. Lancet 2020;395:1544–1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sattar N, Ho FK, Gill JM, Ghouri N, Gray SR, Celis-Morales CA, Katikireddi SV, Berry C, Pell JP, McMurray JJ, Welsh P. BMI and future risk for COVID-19 infection and death across sex, age and ethnicity: preliminary findings from UK biobank. Diabetes Metab Syndr 2020;14:1149–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Tartof SY, Qian L, Hong V, Wei R, Nadjafi RF, Fischer H, Li Z, Shaw SF, Caparosa SL, Nau CL, Saxena T, Rieg GK, Ackerson BK, Sharp AL, Skarbinski J, Naik TK, Murali SB. Obesity and mortality among patients diagnosed with COVID-19: results from an Integrated Health Care Organization. Ann Intern Med 2020;173:773–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Kompaniyets L, Goodman AB, Belay B, Freedman DS, Sucosky MS, Lange SJ, Gundlapalli AV, Boehmer TK, Blanck HM. Body mass index and risk for COVID-19-related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death—United States, March-December 2020. MMWR Morb Mortal Wkly Rep 2021;70:355–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Soares RCM, Mattos LR, Raposo LM. Risk factors for hospitalization and mortality due to COVID-19 in Espirito Santo State, Brazil. Am J Trop Med Hyg 2020;103:1184–1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Garg S, Kim L, Whitaker M, O'Halloran A, Cummings C, Holstein R, Prill M, Chai SJ, Kirley PD, Alden NB, Kawasaki B, Yousey-Hindes K, Niccolai L, Anderson EJ, Openo KP, Weigel A, Monroe ML, Ryan P, Henderson J, Kim S, Como-Sabetti K, Lynfield R, Sosin D, Torres S, Muse A, Bennett NM, Billing L, Sutton M, West N, Schaffner W, Talbot HK, Aquino C, George A, Budd A, Brammer L, Langley G, Hall AJ, Fry A. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 States, March 1-30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Lighter J, Phillips M, Hochman S, Sterling S, Johnson D, Francois F, Stachel A. Obesity in patients younger than 60 years is a risk factor for Covid-19 hospital admission. Clin Infect Dis 2020;71:896–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, Labreuche J, Mathieu D, Pattou F, Jourdain M, Caizzo R, Caplan M, Cousin N, Duburcq T, Durand A, El Kalioubie A, Favory R, Garcia B, Girardie P, Goutay J, Houard M, Jaillette E, Kostuj N, Ledoux G, Mathieu D, Moreau AS, Niles C, Nseir S, Onimus T, Parmentier E, Préau S, Robriquet L, Rouze A, Six S, Verkindt H; the LICORN and the Lille COVID‐19 and Obesity study group. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring, Md) 2020;28:1195–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Shashaty MG, Stapleton RD. Physiological and management implications of obesity in critical illness. Ann Am Thorac Soc 2014;11:1286–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Petersen A, Bressem K, Albrecht J, Thieß H-M, Vahldiek J, Hamm B, Makowski MR, Niehues A, Niehues SM, Adams LC. The role of visceral adiposity in the severity of COVID-19: highlights from a unicenter cross-sectional pilot study in Germany. Metabolism 2020;110:154317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Iacobellis G, Secchi F, Capitanio G, Basilico S, Schiaffino S, Boveri S, Sardanelli F, Corsi Romanelli MM, Malavazos AE. Epicardial fat inflammation in severe COVID-19. Obesity (Silver Spring) 2020;28:2260–2262. [DOI] [PubMed] [Google Scholar]
- 73. Grodecki K, Lin A, Razipour A, Cadet S, McElhinney PA, Chan C, Pressman BD, Julien P, Maurovich-Horvat P, Gaibazzi N, Thakur U, Mancini E, Agalbato C, Mene R, Parati G, Cernigliaro F, Nerlekar N, Torlasco C, Pontone G, Slomka PJ, Dey D. Epicardial adipose tissue is associated with extent of pneumonia and adverse outcomes in patients with COVID-19. Metabolism 2021;115:154436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Chen L, Li X, Chen M, Feng Y, Xiong C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc Res 2020;116:1097–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Damouche A, Lazure T, Avettand-Fenoel V, Huot N, Dejucq-Rainsford N, Satie AP, Melard A, David L, Gommet C, Ghosn J, Noel N, Pourcher G, Martinez V, Benoist S, Bereziat V, Cosma A, Favier B, Vaslin B, Rouzioux C, Capeau J, Muller-Trutwin M, Dereuddre-Bosquet N, Le Grand R, Lambotte O, Bourgeois C. Adipose tissue is a neglected viral reservoir and an inflammatory site during chronic HIV and SIV infection. PLoS Pathog 2015;11:e1005153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Grunewald ME, Chen Y, Kuny C, Maejima T, Lease R, Ferraris D, Aikawa M, Sullivan CS, Perlman S, Fehr AR. The coronavirus macrodomain is required to prevent PARP-mediated inhibition of virus replication and enhancement of IFN expression. PLoS Pathog 2019;15:e1007756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Patel VB, Mori J, McLean BA, Basu R, Das SK, Ramprasath T, Parajuli N, Penninger JM, Grant MB, Lopaschuk GD, Oudit GY. ACE2 deficiency worsens epicardial adipose tissue inflammation and cardiac dysfunction in response to diet-induced obesity. Diabetes 2016;65:85–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Bourgeois C, Gorwood J, Barrail-Tran A, Lagathu C, Capeau J, Desjardins D, Le Grand R, Damouche A, Béréziat V, Lambotte O. Specific biological features of adipose tissue, and their impact on HIV persistence. Front Microbiol 2019;10:2837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Movahed MR, Khoubyari R, Hashemzadeh M, Hashemzadeh M. Obesity is strongly and independently associated with a higher prevalence of pulmonary embolism. Respir Investig 2019;57:376–379. [DOI] [PubMed] [Google Scholar]
- 80. GBD 2015 Tobacco Collaborators. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet 2017;389:1885–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Leung JM, Yang CX, Tam A, Shaipanich T, Hackett TL, Singhera GK, Dorscheid DR, Sin DD. ACE-2 expression in the small airway epithelia of smokers and COPD patients: implications for COVID-19. Eur Respir J 2020;55:2000688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Brake SJ, Barnsley K, Lu W, McAlinden KD, Eapen MS, Sohal SS. Smoking upregulates angiotensin-converting enzyme-2 receptor: a potential adhesion site for novel coronavirus SARS-CoV-2 (Covid-19). J Clin Med 2020;9:841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Miyara M, Tubach F, Pourcher V, Morelot-Panzini C, Pernet J, Haroche J, Lebbah S, Morawiec E, Gorochov G, Caumes E, Hausfater P, Combes A, Similowski T, Amoura A. Low incidence of daily active tobacco smoking in patients with symptomatic COVID-19. Qeios. 2020. doi: 10.32388/WPP19W.3 [DOI] [Google Scholar]
- 84. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Lippi G, Henry BM. Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). Eur J Intern Med 2020;75:107–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Emami A, Javanmardi F, Pirbonyeh N, Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emerg Med 2020;8:e35. [PMC free article] [PubMed] [Google Scholar]
- 87. Simons D, Shahab L, Brown J, Perski O. The association of smoking status with SARS-CoV-2 infection, hospitalization and mortality from COVID-19: a living rapid evidence review with Bayesian meta-analyses (version 7). Addiction 2021;116:1319–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Liu W, Tao ZW, Lei W, Ming-Li Y, Kui L, Ling Z, Shuang W, Yan D, Jing L, Liu HG, Ming Y, Yi H. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J (Engl) 2020;133:1032–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN. Cardiovascular disease, drug therapy, and mortality in Covid-19. N Engl J Med 2020;382:2582. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 91. Subramaniam S, Scharrer I. Procoagulant activity during viral infections. Front Biosci 2018;23:1060–1081. [DOI] [PubMed] [Google Scholar]
- 92. Giannis D, Ziogas IA, Gianni P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol 2020;127:104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Vaughan DE, Lazos SA, Tong K. Angiotensin II regulates the expression of plasminogen activator inhibitor-1 in cultured endothelial cells. A potential link between the renin-angiotensin system and thrombosis. J Clin Invest 1995;95:995–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Badimon L, Vilahur G. Neutrophil extracellular traps: a new source of tissue factor in atherothrombosis. Eur Heart J 2015;36:1364–1366. [DOI] [PubMed] [Google Scholar]
- 95. Ng H, Havervall S, Rosell A, Aguilera K, Parv K, von Meijenfeldt FA, Lisman T, Mackman N, Thalin C, Phillipson M. Circulating markers of neutrophil extracellular traps are of prognostic value in patients with COVID-19. Arterioscler Thromb Vasc Biol 2021;41:988–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Dupont A, Rauch A, Staessens S, Moussa M, Rosa M, Corseaux D, Jeanpierre E, Goutay J, Caplan M, Varlet P, Lefevre G, Lassalle F, Bauters A, Faure K, Lambert M, Duhamel A, Labreuche J, Garrigue D, De Meyer SF, Staels B, Vincent F, Rousse N, Kipnis E, Lenting P, Poissy J, Susen S, Lille Covid Research N; Lille Covid Research Network (LICORNE). Vascular endothelial damage in the pathogenesis of organ injury in severe COVID-19. Arterioscler Thromb Vasc Biol 2021;41:1760–1773. [DOI] [PubMed] [Google Scholar]
- 97. Goshua G, Pine AB, Meizlish ML, Chang CH, Zhang H, Bahel P, Baluha A, Bar N, Bona RD, Burns AJ, Dela Cruz CS, Dumont A, Halene S, Hwa J, Koff J, Menninger H, Neparidze N, Price C, Siner JM, Tormey C, Rinder HM, Chun HJ, Lee AI. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol 2020;7:e575–e582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Rauch A, Dupont A, Goutay J, Caplan M, Staessens S, Moussa M, Jeanpierre E, Corseaux D, Lefevre G, Lassalle F, Faure K, Lambert M, Duhamel A, Labreuche J, Garrigue D, De Meyer SF, Staels B, Van Belle E, Vincent F, Kipnis E, Lenting PJ, Poissy J, Susen S, Lille CRN; Members of the LSC. Endotheliopathy is induced by plasma from critically ill patients and associated with organ failure in severe COVID-19. Circulation 2020;142:1881–1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Libby P, Simon DI. Inflammation and thrombosis: the clot thickens. Circulation 2001;103:1718–1720. [DOI] [PubMed] [Google Scholar]
- 100. Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta 2020;506:145–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Chen RF, Chang JC, Yeh WT, Lee CH, Liu JW, Eng HL, Yang KD. Role of vascular cell adhesion molecules and leukocyte apoptosis in the lymphopenia and thrombocytopenia of patients with severe acute respiratory syndrome (SARS). Microbes Infect 2006;8:122–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, Li WW, Li VW, Mentzer SJ, Jonigk D. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N Engl J Med 2020;383:120–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Menter T, Haslbauer JD, Nienhold R, Savic S, Hopfer H, Deigendesch N, Frank S, Turek D, Willi N, Pargger H, Bassetti S, Leuppi JD, Cathomas G, Tolnay M, Mertz KD, Tzankov A. Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction. Histopathology 2020;77:198–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020;395:1417–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Lei Y, Zhang J, Schiavon CR, He M, Chen L, Shen H, Zhang Y, Yin Q, Cho Y, Andrade L, Shadel GS, Hepokoski M, Lei T, Wang H, Zhang J, Yuan JX, Malhotra A, Manor U, Wang S, Yuan ZY, Shyy JY. SARS-CoV-2 Spike protein impairs endothelial function via downregulation of ACE 2. Circ Res 2021;128:1323–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD, Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD; ESC Scientific Document Group. Fourth universal definition of myocardial infarction (2018). Eur Heart J 2019;40:237–269. [DOI] [PubMed] [Google Scholar]
- 107. Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020;5:802–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, Lee M. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA 2020;323:1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 2020;46:846–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Lala A, Johnson KW, Januzzi JL, Russak AJ, Paranjpe I, Richter F, Zhao S, Somani S, Van Vleck T, Vaid A, Chaudhry F, De Freitas JK, Fayad ZA, Pinney SP, Levin M, Charney A, Bagiella E, Narula J, Glicksberg BS, Nadkarni G, Mancini DM, Fuster V, Mount Sinai CIC. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol 2020;76:533–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Giustino G, Pinney SP, Lala A, Reddy VY, Johnston-Cox HA, Mechanick JI, Halperin JL, Fuster V. Coronavirus and cardiovascular disease, myocardial injury, and arrhythmia: JACC Focus Seminar. J Am Coll Cardiol 2020;76:2011–2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Wei JF, Huang FY, Xiong TY, Liu Q, Chen H, Wang H, Huang H, Luo YC, Zhou X, Liu ZY, Peng Y, Xu YN, Wang B, Yang YY, Liang ZA, Lei XZ, Ge Y, Yang M, Zhang L, Zeng MQ, Yu H, Liu K, Jia YH, Prendergast BD, Li WM, Chen M. Acute myocardial injury is common in patients with COVID-19 and impairs their prognosis. Heart 2020;106:1154–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Metkus TS, Sokoll LJ, Barth AS, Czarny MJ, Hays AG, Lowenstein CJ, Michos ED, Nolley EP, Post WS, Resar JR, Thiemann DR, Trost JC, Hasan RK. Myocardial injury in severe COVID-19 compared with non-COVID-19 acute respiratory distress syndrome. Circulation 2021;143:553–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Sandoval Y, Januzzi JL Jr, Jaffe AS. Cardiac troponin for assessment of myocardial injury in COVID-19: JACC Review Topic of the Week. J Am Coll Cardiol 2020;76:1244–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Atri D, Siddiqi HK, Lang JP, Nauffal V, Morrow DA, Bohula EA. COVID-19 for the cardiologist: basic virology, epidemiology, cardiac manifestations, and potential therapeutic strategies. JACC Basic Transl Sci 2020;5:518–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Madjid M, Vela D, Khalili-Tabrizi H, Casscells SW, Litovsky S. Systemic infections cause exaggerated local inflammation in atherosclerotic coronary arteries: clues to the triggering effect of acute infections on acute coronary syndromes. Tex Heart Inst J 2007;34:11–18. [PMC free article] [PubMed] [Google Scholar]
- 117. Kwong JC, Schwartz KL, Campitelli MA, Chung H, Crowcroft NS, Karnauchow T, Katz K, Ko DT, McGeer AJ, McNally D, Richardson DC, Rosella LC, Simor A, Smieja M, Zahariadis G, Gubbay JB. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med 2018;378:345–353. [DOI] [PubMed] [Google Scholar]
- 118. Caldeira D, Rodrigues B, David C, Costa J, Pinto FJ, Ferreira JJ. The association of influenza infection and vaccine with myocardial infarction: systematic review and meta-analysis of self-controlled case series. Expert Rev Vaccines 2019;18:1211–1217. [DOI] [PubMed] [Google Scholar]
- 119. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020;18:844–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Lee HS, Noh JY, Shin OS, Song JY, Cheong HJ, Kim WJ. Matrix metalloproteinase-13 in atherosclerotic plaque is increased by influenza A virus infection. J Infect Dis 2020;221:256–266. [DOI] [PubMed] [Google Scholar]
- 121. Bangalore S, Sharma A, Slotwiner A, Yatskar L, Harari R, Shah B, Ibrahim H, Friedman GH, Thompson C, Alviar CL, Chadow HL, Fishman GI, Reynolds HR, Keller N, Hochman JS. ST-segment elevation in patients with Covid-19—a case series. N Engl J Med 2020;382:2478–2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Kite TA, Ludman PF, Gale CP, Wu J, Caixeta A, Mansourati J, Sabate M, Jimenez-Quevedo P, Candilio L, Sadeghipour P, Iniesta AM, Hoole SP, Palmer N, Ariza-Sole A, Namitokov A, Escutia-Cuevas HH, Vincent F, Tica O, Ngunga M, Meray I, Morrow A, Arefin MM, Lindsay S, Kazamel G, Sharma V, Saad A, Sinagra G, Sanchez FA, Roik M, Savonitto S, Vavlukis M, Sangaraju S, Malik IS, Kean S, Curzen N, Berry C, Stone GW, Gersh BJ, Gershlick AH; International C-ACSRI. International Prospective Registry of Acute Coronary syndromes in patients with COVID-19. J Am Coll Cardiol 2021;77:2466–2476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Hamadeh A, Aldujeli A, Briedis K, Tecson KM, Sanz-Sánchez J, Al Dujeili M, Al-Obeidi A, Diez JL, Žaliūnas R, Stoler RC, McCullough PA. Characteristics and outcomes in patients presenting with COVID-19 and ST-segment elevation myocardial infarction. Am J Cardiol 2020;131:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Stefanini GG, Montorfano M, Trabattoni D, Andreini D, Ferrante G, Ancona M, Metra M, Curello S, Maffeo D, Pero G, Cacucci M, Assanelli E, Bellini B, Russo F, Ielasi A, Tespili M, Danzi GB, Vandoni P, Bollati M, Barbieri L, Oreglia J, Lettieri C, Cremonesi A, Carugo S, Reimers B, Condorelli G, Chieffo A. ST-elevation myocardial infarction in patients with COVID-19: clinical and angiographic outcomes. Circulation 2020;141:2113–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Choudry FA, Hamshere SM, Rathod KS, Akhtar MM, Archbold RA, Guttmann OP, Woldman S, Jain AK, Knight CJ, Baumbach A, Mathur A, Jones DA. High thrombus burden in patients with COVID-19 presenting with ST-segment elevation myocardial infarction. J Am Coll Cardiol 2020;76:1168–1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Garcia S, Dehghani P, Grines C, Davidson L, Nayak KR, Saw J, Waksman R, Blair J, Akshay B, Garberich R, Schmidt C, Ly HQ, Sharkey S, Mercado N, Alfonso CE, Misumida N, Acharya D, Madan M, Hafiz AM, Javed N, Shavadia J, Stone J, Alraies MC, Htun W, Downey W, Bergmark BA, Ebinger J, Alyousef T, Khalili H, Hwang CW, Purow J, Llanos A, McGrath B, Tannenbaum M, Resar J, Bagur R, Cox-Alomar P, Stefanescu Schmidt AC, Cilia LA, Jaffer FA, Gharacholou M, Salinger M, Case B, Kabour A, Dai X, Elkhateeb O, Kobayashi T, Kim HH, Roumia M, Aguirre FV, Rade J, Chong AY, Hall HM, Amlani S, Bagherli A, Patel RAG, Wood DA, Welt FG, Giri J, Mahmud E, Henry TD; Society for Cardiac Angiography and Interventions, the Canadian Association of Interventional Cardiology, and the American College of Cardiology Interventional Council. Initial findings from the North American COVID-19 Myocardial Infarction Registry. J Am Coll Cardiol 2021;77:1994–2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Sultanian P, Lundgren P, Stromsoe A, Aune S, Bergstrom G, Hagberg E, Hollenberg J, Lindqvist J, Djarv T, Castelheim A, Thoren A, Hessulf F, Svensson L, Claesson A, Friberg H, Nordberg P, Omerovic E, Rosengren A, Herlitz J, Rawshani A. Cardiac arrest in COVID-19: characteristics and outcomes of in- and out-of-hospital cardiac arrest. A report from the Swedish Registry for Cardiopulmonary Resuscitation. Eur Heart J 2021;42:1094–1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Liu PP, Blet A, Smyth D, Li H. The Science underlying COVID-19: implications for the cardiovascular system. Circulation 2020;142:68–78. [DOI] [PubMed] [Google Scholar]
- 129. Bugiardini R, Cenko E. A short history of vasospastic angina. J Am Coll Cardiol 2017;70:2359–2362. [DOI] [PubMed] [Google Scholar]
- 130. Van Wyngene L, Vandewalle J, Libert C. Reprogramming of basic metabolic pathways in microbial sepsis: therapeutic targets at last? EMBO Mol Med 2018;10:e8712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Pan P, Wang X, Liu D. The potential mechanism of mitochondrial dysfunction in septic cardiomyopathy. J Int Med Res 2018;46:2157–2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Duncker DJ, Bache RJ. Regulation of coronary blood flow during exercise. Physiol Rev 2008;88:1009–1086. [DOI] [PubMed] [Google Scholar]
- 133. Sala S, Peretto G, Gramegna M, Palmisano A, Villatore A, Vignale D, De Cobelli F, Tresoldi M, Cappelletti AM, Basso C, Godino C, Esposito A. Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection. Eur Heart J 2020;41:1861–1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Tavazzi G, Pellegrini C, Maurelli M, Belliato M, Sciutti F, Bottazzi A, Sepe PA, Resasco T, Camporotondo R, Bruno R, Baldanti F, Paolucci S, Pelenghi S, Iotti GA, Mojoli F, Arbustini E. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail 2020;22:911–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Escher F, Pietsch H, Aleshcheva G, Bock T, Baumeier C, Elsaesser A, Wenzel P, Hamm C, Westenfeld R, Schultheiss M, Gross U, Morawietz L, Schultheiss HP. Detection of viral SARS-CoV-2 genomes and histopathological changes in endomyocardial biopsies. ESC Heart Fail 2020;7:2440–2447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Wenzel P, Kopp S, Gobel S, Jansen T, Geyer M, Hahn F, Kreitner KF, Escher F, Schultheiss HP, Munzel T. Evidence of SARS-CoV-2 mRNA in endomyocardial biopsies of patients with clinically suspected myocarditis tested negative for COVID-19 in nasopharyngeal swab. Cardiovasc Res 2020;116:1661–1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, Fu M, Heliö T, Heymans S, Jahns R, Klingel K, Linhart A, Maisch B, McKenna W, Mogensen J, Pinto YM, Ristic A, Schultheiss HP, Seggewiss H, Tavazzi L, Thiene G, Yilmaz A, Charron P, Elliott PM; European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 2013;34:2636–2648, 2648a–2648d. [DOI] [PubMed] [Google Scholar]
- 138. Lindner D, Fitzek A, Brauninger H, Aleshcheva G, Edler C, Meissner K, Scherschel K, Kirchhof P, Escher F, Schultheiss HP, Blankenberg S, Puschel K, Westermann D. Association of cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiol 2020;5:1281–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Shay DK, Shimabukuro TT, DeStefano F. Myocarditis occurring after immunization with mRNA-based COVID-19 vaccines. JAMA Cardiol 2021. doi: 10.1001/jamacardio.2021.2821. [DOI] [PubMed] [Google Scholar]
- 140. Surveillance of Myocarditis (Inflammation of the Heart Muscle) Cases Between December 2020 and May 2021 (Including). https://www.gov.il/en/departments/news/01062021-03 (02 July 2021 date last accessed).
- 141. Petersen BW, Damon IK, Pertowski CA, Meaney-Delman D, Guarnizo JT, Beigi RH, Edwards KM, Fisher MC, Frey SE, Lynfield R, Willoughby RE. Clinical guidance for smallpox vaccine use in a postevent vaccination program. MMWR Recomm Rep 2015;64:1–26. [PubMed] [Google Scholar]
- 142. Tung ML, Tan B, Cherian R, Chandra B. Anti-phospholipid syndrome and COVID-19 thrombosis: connecting the dots. Rheumatol Adv Pract 2021;5:rkaa081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Dolhnikoff M, Duarte‐Neto AN, Almeida Monteiro RA, Silva LFF, Oliveira EP, Saldiva PHN, Mauad T, Negri EM. Pathological evidence of pulmonary thrombotic phenomena in severe COVID-19. J Thromb Haemost 2020;18:1517–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Jiménez D, García-Sanchez A, Rali P, Muriel A, Bikdeli B, Ruiz-Artacho P, Le Mao R, Rodríguez C, Hunt BJ, Monreal M. Incidence of VTE and bleeding among hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Chest 2021;159:1182–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Malas MB, Naazie IN, Elsayed N, Mathlouthi A, Marmor R, Clary B. Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: a systematic review and meta-analysis. EClinicalMedicine 2020;29:100639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Tan BK, Mainbourg S, Friggeri A, Bertoletti L, Douplat M, Dargaud Y, Grange C, Lobbes H, Provencher S, Lega JC. Arterial and venous thromboembolism in COVID-19: a study-level meta-analysis. Thorax 2021;76:970–979. [DOI] [PubMed] [Google Scholar]
- 147. Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost 2020;18:1421–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. de Roquetaillade C, Chousterman BG, Tomasoni D, Zeitouni M, Houdart E, Guedon A, Reiner P, Bordier R, Gayat E, Montalescot G, Metra M, Mebazaa A. Unusual arterial thrombotic events in Covid-19 patients. Int J Cardiol 2021;323:281–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Bellosta R, Luzzani L, Natalini G, Pegorer MA, Attisani L, Cossu LG, Ferrandina C, Fossati A, Conti E, Bush RL, Piffaretti G. Acute limb ischemia in patients with COVID-19 pneumonia. J Vasc Surg 2020;72:1864–1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Moores LK, Tritschler T, Brosnahan S, Carrier M, Collen JF, Doerschug K, Holley AB, Jimenez D, Le Gal G, Rali P, Wells P. Prevention, diagnosis, and treatment of VTE in patients with coronavirus disease 2019: HEST Guideline and Expert Panel Report. Chest 2020;158:1143–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Spyropoulos AC, Levy JH, Ageno W, Connors JM, Hunt BJ, Iba T, Levi M, Samama CM, Thachil J, Giannis D, Douketis JD; Subcommittee on Perioperative, Critical Care Thrombosis, Haemostasis of the Scientific, Standardization Committee of the International Society on Thrombosis and Haemostasis. Scientific and Standardization Committee communication: Clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost 2020;18:1859–1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Salas A, Sans M, Soriano A, Reverter JC, Anderson DC, Pique JM, Panes J. Heparin attenuates TNF-alpha induced inflammatory response through a CD11b dependent mechanism. Gut 2000;47:88–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Young E. The anti-inflammatory effects of heparin and related compounds. Thromb Res 2008;122:743–752. [DOI] [PubMed] [Google Scholar]
- 154. Mycroft-West CJ, Su D, Pagani I, Rudd TR, Elli S, Gandhi NS, Guimond SE, Miller GJ, Meneghetti MCZ, Nader HB, Li Y, Nunes QM, Procter P, Mancini N, Clementi M, Bisio A, Forsyth NR, Ferro V, Turnbull JE, Guerrini M, Fernig DG, Vicenzi E, Yates EA, Lima MA, Skidmore MA. Heparin inhibits cellular invasion by SARS-CoV-2: structural dependence of the interaction of the spike S1 receptor-binding domain with heparin. Thromb Haemost 2020;120:1700–1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Tree JA, Turnbull JE, Buttigieg KR, Elmore MJ, Coombes N, Hogwood J, Mycroft-West CJ, Lima MA, Skidmore MA, Karlsson R, Chen YH, Yang Z, Spalluto CM, Staples KJ, Yates EA, Gray E, Singh D, Wilkinson T, Page CP, Carroll MW. Unfractionated heparin inhibits live wild type SARS-CoV-2 cell infectivity at therapeutically relevant concentrations. Br J Pharmacol 2021;178:626–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Arachchillage DJ, Stacey A, Akor F, Scotz M, Laffan M. Thrombolysis restores perfusion in COVID-19 hypoxia. Br J Haematol 2020;190:e270–e274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Talasaz AH, Sadeghipour P, Kakavand H, Aghakouchakzadeh M, Kordzadeh-Kermani E, Van Tassell BW, Gheymati A, Ariannejad H, Hosseini SH, Jamalkhani S, Sholzberg M, Monreal M, Jimenez D, Piazza G, Parikh SA, Kirtane AJ, Eikelboom JW, Connors JM, Hunt BJ, Konstantinides SV, Cushman M, Weitz JI, Stone GW, Krumholz HM, Lip GYH, Goldhaber SZ, Bikdeli B. Recent randomized trials of antithrombotic therapy for patients with COVID-19: JACC State-of-the-Art Review. J Am Coll Cardiol 2021;77:1903–1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Hendren NS, Drazner MH, Bozkurt B, Cooper LT. Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation 2020;141:1903–1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med 2020;8:681–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Li Y, Li H, Zhu S, Xie Y, Wang B, He L, Zhang D, Zhang Y, Yuan H, Wu C, Sun W, Zhang Y, Li M, Cui L, Cai Y, Wang J, Yang Y, Lv Q, Zhang L, Xie M. Prognostic value of right ventricular longitudinal strain in patients with COVID-19. JACC Cardiovasc Imaging 2020;13:2287–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Kim J, Volodarskiy A, Sultana R, Pollie MP, Yum B, Nambiar L, Tafreshi R, Mitlak HW, RoyChoudhury A, Horn EM, Hriljac I, Narula N, Kim S, Ndhlovu L, Goyal P, Safford MM, Shaw L, Devereux RB, Weinsaft JW. Prognostic utility of right ventricular remodeling over conventional risk stratification in patients with COVID-19. J Am Coll Cardiol 2020;76:1965–1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Soulat-Dufour L, Fauvel C, Weizman O, Barbe T, Pezel T, Mika D, Cellier J, Geneste L, Panagides V, Marsou W, Deney A, Attou S, Delmotte T, Ribeyrolles S, Chemaly P, Karsenty C, Giordano G, Gautier A, Duceau B, Sutter W, Chaumont C, Guilleminot P, Sagnard A, Pastier J, Trimaille A, Bonnet G, Canu M, Coisne A, Cohen A. Prognostic value of right ventricular dilatation in patients with COVID-19: a multicentre study. Eur Heart J Cardiovasc Imaging 2021;jeab067. doi: 10.1093/ehjci/jeab067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Dweck MR, Bularga A, Hahn RT, Bing R, Lee KK, Chapman AR, White A, Salvo GD, Sade LE, Pearce K, Newby DE, Popescu BA, Donal E, Cosyns B, Edvardsen T, Mills NL, Haugaa K. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J Cardiovasc Imaging 2020;21:949–958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Szekely Y, Lichter Y, Taieb P, Banai A, Hochstadt A, Merdler I, Gal Oz A, Rothschild E, Baruch G, Peri Y, Arbel Y, Topilsky Y. Spectrum of cardiac manifestations in COVID-19: a systematic echocardiographic study. Circulation 2020;142:342–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Lassen MCH, Skaarup KG, Lind JN, Alhakak AS, Sengelov M, Nielsen AB, Espersen C, Ravnkilde K, Hauser R, Schops LB, Holt E, Johansen ND, Modin D, Djernaes K, Graff C, Bundgaard H, Hassager C, Jabbari R, Carlsen J, Lebech AM, Kirk O, Bodtger U, Lindholm MG, Joseph G, Wiese L, Schiodt FV, Kristiansen OP, Walsted ES, Nielsen OW, Madsen BL, Tonder N, Benfield T, Jeschke KN, Ulrik CS, Knop FK, Lamberts M, Sivapalan P, Gislason G, Marott JL, Mogelvang R, Jensen G, Schnohr P, Sogaard P, Solomon SD, Iversen K, Jensen JUS, Schou M, Biering-Sorensen T. Echocardiographic abnormalities and predictors of mortality in hospitalized COVID-19 patients: the ECHOVID-19 study. ESC Heart Fail 2020;7:4189–4197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129–2200. [DOI] [PubMed] [Google Scholar]
- 167. Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, Huisman MV, Humbert M, Jennings CS, Jimenez D, Kucher N, Lang IM, Lankeit M, Lorusso R, Mazzolai L, Meneveau N, Ni Ainle F, Prandoni P, Pruszczyk P, Righini M, Torbicki A, Van Belle E, Zamorano JL; ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J 2020;41:543–603. [DOI] [PubMed] [Google Scholar]
- 168. Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Munoz D, Rosenhek R, Sjogren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL; ESC Scientific Document Group. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 2017;38:2739–2791. [DOI] [PubMed] [Google Scholar]
- 169. Du Y, Tu L, Zhu P, Mu M, Wang R, Yang P, Wang X, Hu C, Ping R, Hu P, Li T, Cao F, Chang C, Hu Q, Jin Y, Xu G. Clinical features of 85 fatal cases of COVID-19 from Wuhan: a retrospective observational study. Am J Respir Crit Care Med 2020;201:1372–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 2020;323:1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, Satlin MJ, Campion TR Jr, Nahid M, Ringel JB, Hoffman KL, Alshak MN, Li HA, Wehmeyer GT, Rajan M, Reshetnyak E, Hupert N, Horn EM, Martinez FJ, Gulick RM, Safford MM. Clinical characteristics of Covid-19 in New York City. N Engl J Med 2020;382:2372–2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Wetterslev M, Jacobsen PK, Hassager C, Jøns C, Risum N, Pehrson S, Bastiansen A, Andreasen AS, Tjelle Kristiansen K, Bestle MH, Mohr T, Møller-Sørensen H, Perner A. Cardiac arrhythmias in critically ill patients with coronavirus disease 2019: a retrospective population-based cohort study. Acta Anaesthesiol Scand 2021;65:770–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Parwani AS, Haug M, Keller T, Guthof T, Blaschke F, Tscholl V, Biewener S, Kamieniarz P, Zieckler D, Kruse J, Angermair S, Treskatsch S, Muller-Redetzky H, Pieske B, Stangl K, Landmesser U, Boldt LH, Huemer M, Attanasio P. Cardiac arrhythmias in patients with COVID-19: lessons from 2300 telemetric monitoring days on the intensive care unit. J Electrocardiol 2021;66:102–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Coromilas EJ, Kochav S, Goldenthal I, Biviano A, Garan H, Goldbarg S, Kim J-H, Yeo I, Tracy C, Ayanian S, Akar J, Singh A, Jain S, Zimerman L, Pimentel M, Osswald S, Twerenbold R, Schaerli N, Crotti L, Fabbri D, Parati G, Li Y, Atienza F, Zatarain E, Tse G, Leung KSK, Guevara-Valdivia ME, Rivera-Santiago CA, Soejima K, De Filippo P, Ferrari P, Malanchini G, Kanagaratnam P, Khawaja S, Mikhail GW, Scanavacca M, Abrahão Hajjar L, Rizerio B, Sacilotto L, Mollazadeh R, Eslami M, Laleh Far V, Mattioli AV, Boriani G, Migliore F, Cipriani A, Donato F, Compagnucci P, Casella M, Dello Russo A, Coromilas J, Aboyme A, O'Brien CG, Rodriguez F, Wang PJ, Naniwadekar A, Moey M, Kow CS, Cheah WK, Auricchio A, Conte G, Hwang J, Han S, Lazzerini PE, Franchi F, Santoro A, Capecchi PL, Joglar JA, Rosenblatt AG, Zardini M, Bricoli S, Bonura R, Echarte-Morales J, Benito-González T, Minguito-Carazo C, Fernández-Vázquez F, Wan EY. Worldwide survey of COVID-19-associated arrhythmias. Circ Arrhythm Electrophysiol 2021;14:e009458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Lanza GA, De Vita A, Ravenna SE, D’Aiello A, Covino M, Franceschi F, Crea F. Electrocardiographic findings at presentation and clinical outcome in patients with SARS-CoV-2 infection. Europace 2021;23:123–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Varma N, Marrouche NF, Aguinaga L, Albert CM, Arbelo E, Choi JI, Chung MK, Conte G, Dagher L, Epstein LM, Ghanbari H, Han JK, Heidbuchel H, Huang H, Lakkireddy DR, Ngarmukos T, Russo AM, Saad EB, Saenz Morales LC, Sandau KE, Sridhar ARM, Stecker EC, Varosy PD. HRS/EHRA/APHRS/LAHRS/ACC/AHA worldwide practice update for telehealth and arrhythmia monitoring during and after a pandemic. Europace 2021;23:313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Kytomaa S, Hegde S, Claggett B, Udell JA, Rosamond W, Temte J, Nichol K, Wright JD, Solomon SD, Vardeny O. Association of influenza-like illness activity with hospitalizations for heart failure: the Atherosclerosis Risk in Communities Study. JAMA Cardiol 2019;4:363–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Guo Y, Lip GY, Apostolakis S. Inflammation in atrial fibrillation. J Am Coll Cardiol 2012;60:2263–2270. [DOI] [PubMed] [Google Scholar]
- 179. Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chem Lab Med 2020;58:1021–1028. [DOI] [PubMed] [Google Scholar]
- 180. Lazzerini PE, Boutjdir M, Capecchi PL. COVID-19, arrhythmic risk and inflammation: mind the gap! Circulation 2020;142:7–9. [DOI] [PubMed] [Google Scholar]
- 181. Tracey KJ. The inflammatory reflex. Nature 2002;420:853–859. [DOI] [PubMed] [Google Scholar]
- 182. Takayama K, Yuhki K, Ono K, Fujino T, Hara A, Yamada T, Kuriyama S, Karibe H, Okada Y, Takahata O, Taniguchi T, Iijima T, Iwasaki H, Narumiya S, Ushikubi F. Thromboxane A2 and prostaglandin F2alpha mediate inflammatory tachycardia. Nat Med 2005;11:562–566. [DOI] [PubMed] [Google Scholar]
- 183. Gao P, Wu W, Tian R, Yan X, Qian H, Guo F, Li T, Liu Z, Wang J, Zhou X, Qin Y, Zhao D, Bian X, Lin X, Zhang S. Association between tachyarrhythmia and mortality in a cohort of critically ill patients with coronavirus disease 2019 (COVID-19). Ann Transl Med 2021;9:883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Boriani G, Fauchier L, Aguinaga L, Beattie JM, Blomstrom Lundqvist C, Cohen A, Dan GA, Genovesi S, Israel C, Joung B, Kalarus Z, Lampert R, Malavasi VL, Mansourati J, Mont L, Potpara T, Thornton A, Lip GYH; ESC Scientific Document Group. European Heart Rhythm Association (EHRA) consensus document on management of arrhythmias and cardiac electronic devices in the critically ill and post-surgery patient, endorsed by Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), Cardiac Arrhythmia Society of Southern Africa (CASSA), and Latin American Heart Rhythm Society (LAHRS). Europace 2019;21:7–8. [DOI] [PubMed] [Google Scholar]
- 185. Rosenberg ES, Dufort EM, Udo T, Wilberschied LA, Kumar J, Tesoriero J, Weinberg P, Kirkwood J, Muse A, DeHovitz J, Blog DS, Hutton B, Holtgrave DR, Zucker HA. Association of treatment with hydroxychloroquine or azithromycin with in-hospital mortality in patients with COVID-19 in New York State. JAMA 2020;323:2493–2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Ali-Ahmed F, Dalgaard F, Al-Khatib SM. Sudden cardiac death in patients with myocarditis: evaluation, risk stratification, and management. Am Heart J 2020;220:29–40. [DOI] [PubMed] [Google Scholar]
- 187. Hayek SS, Brenner SK, Azam TU, Shadid HR, Anderson E, Berlin H, Pan M, Meloche C, Feroz R, O'Hayer P, Kaakati R, Bitar A, Padalia K, Perry D, Blakely P, Gupta S, Shaefi S, Srivastava A, Charytan DM, Bansal A, Mallappallil M, Melamed ML, Shehata AM, Sunderram J, Mathews KS, Sutherland AK, Nallamothu BK, Leaf DE; STOP-COVID Investigators. In-hospital cardiac arrest in critically ill patients with covid-19: multicenter cohort study. BMJ 2020;371:m3513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Shao F, Xu S, Ma X, Xu Z, Lyu J, Ng M, Cui H, Yu C, Zhang Q, Sun P, Tang Z. In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan. China. Resuscitation 2020;151:18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189. Nolan JP, Neumar RW, Adrie C, Aibiki M, Berg RA, Böttiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC, Kern KB, Laurent I, Longstreth WT, Merchant RM, Morley P, Morrison LJ, Nadkarni V, Peberdy MA, Rivers EP, Rodriguez-Nunez A, Sellke FW, Spaulding C, Sunde K, Hoek TV. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A Scientific Statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke. Resuscitation 2008;79:350–379. [DOI] [PubMed] [Google Scholar]
- 190. Bro-Jeppesen J, Kjaergaard J, Wanscher M, Nielsen N, Friberg H, Bjerre M, Hassager C. The inflammatory response after out-of-hospital cardiac arrest is not modified by targeted temperature management at 33°C or 36°C. Resuscitation 2014;85:1480–1487. [DOI] [PubMed] [Google Scholar]
- 191. Bro-Jeppesen J, Johansson PI, Hassager C, Wanscher M, Ostrowski SR, Bjerre M, Kjaergaard J. Endothelial activation/injury and associations with severity of post-cardiac arrest syndrome and mortality after out-of-hospital cardiac arrest. Resuscitation 2016;107:71–79. [DOI] [PubMed] [Google Scholar]
- 192. Meyer MAS, Wiberg S, Grand J, Meyer ASP, Obling LER, Frydland M, Thomsen JH, Josiassen J, Moller JE, Kjaergaard J, Hassager C. Treatment effects of interleukin-6 receptor antibodies for modulating the systemic inflammatory response after out-of-hospital cardiac arrest (The IMICA Trial): a double-blinded, placebo-controlled, single-center, randomized, clinical trial. Circulation 2021;143:1841–1851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Hassager C, Price S, Huber K. Cardiac arrest in the COVID-19 era. Eur Heart J Acute Cardiovasc Care 2020;9:239–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Andelius L, Oving I, Folke F, de Graaf C, Stieglis R, Kjoelbye JS, Hansen CM, Koster RW, Lt H, Blom MT; ESCAPE-NET investigators. Management of first responder programmes for out-of-hospital cardiac arrest during the COVID-19 pandemic in Europe. Resusc Plus 2021;5:100075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Scully EP, Haverfield J, Ursin RL, Tannenbaum C, Klein SL. Considering how biological sex impacts immune responses and COVID-19 outcomes. Nat Rev Immunol 2020;20:442–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Gadi N, Wu SC, Spihlman AP, Moulton VR. What's sex got to do with COVID-19? gender-based differences in the host immune response to coronaviruses. Front Immunol 2020;11:2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Medzikovic L, Cunningham CM, Li M, Amjedi M, Hong J, Ruffenach G, Eghbali M. Sex differences underlying preexisting cardiovascular disease and cardiovascular injury in COVID-19. J Mol Cell Cardiol 2020;148:25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Deng Q, Rasool RU, Russell RM, Natesan R, Asangani IA. Targeting androgen regulation of TMPRSS2 and ACE2 as a therapeutic strategy to combat COVID-19. iScience 2021;24:102254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Wang H, Sun X, L VonCannon J, Kon ND, Ferrario CM, Groban L. Estrogen receptors are linked to angiotensin-converting enzyme 2 (ACE2), ADAM metallopeptidase domain 17 (ADAM-17), and transmembrane protease serine 2 (TMPRSS2) expression in the human atrium: insights into COVID-19. Hypertens Res 2021;44:882–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Ghandehari S, Matusov Y, Pepkowitz S, Stein D, Kaderi T, Narayanan D, Hwang J, Chang S, Goodman R, Ghandehari H, Mirocha J, Bresee C, Tapson V, Lewis M. Progesterone in addition to standard of care vs standard of care alone in the treatment of men hospitalized with moderate to severe COVID-19: a randomized, controlled pilot trial. Chest 2021;160:74–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201. Tukiainen T, Villani AC, Yen A, Rivas MA, Marshall JL, Satija R, Aguirre M, Gauthier L, Fleharty M, Kirby A, Cummings BB, Castel SE, Karczewski KJ, Aguet F, Byrnes A; GTEx Consortium; Laboratory, Data Analysis &Coordinating Center (LDACC)—Analysis Working Group; Statistical Methods groups—Analysis Working Group; Enhancing GTEx (eGTEx) groups; NIH Common Fund; NIH/NCI; NIH/NHGRI; NIH/NIMH; NIH/NIDA; Biospecimen Collection Source Site—NDRI; Biospecimen Collection Source Site—RPCI; Biospecimen Core Resource—VARI; Brain Bank Repository—University of Miami Brain Endowment Bank; Leidos Biomedical—Project Management; ELSI Study; Genome Browser Data Integration &Visualization—EBI; Genome Browser Data Integration &Visualization—UCSC Genomics Institute, University of California Santa Cruz, Lappalainen T, Regev A, Ardlie KG, Hacohen N, MacArthur DG. Landscape of X chromosome inactivation across human tissues. Nature. 2017;550:244–248.29022598 [Google Scholar]
- 202. Takahashi T, Iwasaki A. Sex differences in immune responses. Science 2021;371:347–348. [DOI] [PubMed] [Google Scholar]
- 203. Marquez EJ, Chung CH, Marches R, Rossi RJ, Nehar-Belaid D, Eroglu A, Mellert DJ, Kuchel GA, Banchereau J, Ucar D. Sexual-dimorphism in human immune system aging. Nat Commun 2020;11:751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Balistreri CR, Caruso C, Listi F, Colonna-Romano G, Lio D, Candore G. LPS-mediated production of pro/anti-inflammatory cytokines and eicosanoids in whole blood samples: biological effects of +896A/G TLR4 polymorphism in a Sicilian population of healthy subjects. Mech Ageing Dev 2011;132:86–92. [DOI] [PubMed] [Google Scholar]
- 205. Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, Hohmann E, Chu HY, Luetkemeyer A, Kline S, Lopez de Castilla D, Finberg RW, Dierberg K, Tapson V, Hsieh L, Patterson TF, Paredes R, Sweeney DA, Short WR, Touloumi G, Lye DC, Ohmagari N, Oh MD, Ruiz-Palacios GM, Benfield T, Fatkenheuer G, Kortepeter MG, Atmar RL, Creech CB, Lundgren J, Babiker AG, Pett S, Neaton JD, Burgess TH, Bonnett T, Green M, Makowski M, Osinusi A, Nayak S, Lane HC, Members A-SG. Remdesivir for the treatment of Covid-19—final report. N Engl J Med 2020;383:1813–1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Spinner CD, Gottlieb RL, Criner GJ, Arribas Lopez JR, Cattelan AM, Soriano Viladomiu A, Ogbuagu O, Malhotra P, Mullane KM, Castagna A, Chai LYA, Roestenberg M, Tsang OTY, Bernasconi E, Le Turnier P, Chang SC, SenGupta D, Hyland RH, Osinusi AO, Cao H, Blair C, Wang H, Gaggar A, Brainard DM, McPhail MJ, Bhagani S, Ahn MY, Sanyal AJ, Huhn G, Marty FM; GS-US-540-5774 Investigators. Effect of remdesivir vs standard care on clinical status at 11 days in patients with moderate COVID-19: a randomized clinical trial. JAMA 2020;324:1048–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Goldman JD, Lye DCB, Hui DS, Marks KM, Bruno R, Montejano R, Spinner CD, Galli M, Ahn MY, Nahass RG, Chen YS, SenGupta D, Hyland RH, Osinusi AO, Cao H, Blair C, Wei X, Gaggar A, Brainard DM, Towner WJ, Munoz J, Mullane KM, Marty FM, Tashima KT, Diaz G, Subramanian A; GS-US-540-5773 Investigators. Remdesivir for 5 or 10 days in patients with severe Covid-19. N Engl J Med 2020;383:1827–1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Rochwerg B, Agarwal A, Siemieniuk RA, Agoritsas T, Lamontagne F, Askie L, Lytvyn L, Leo Y-S, Macdonald H, Zeng L, Amin W, Burhan E, Bausch FJ, Calfee CS, Cecconi M, Chanda D, Du B, Geduld H, Gee P, Harley N, Hashimi M, Hunt B, Kabra SK, Kanda S, Kawano-Dourado L, Kim Y-J, Kissoon N, Kwizera A, Mahaka I, Manai H, Mino G, Nsutebu E, Preller J, Pshenichnaya N, Qadir N, Sabzwari S, Sarin R, Shankar-Hari M, Sharland M, Shen Y, Ranganathan SS, Souza JP, Stegemann M, De Sutter A, Ugarte S, Venkatapuram S, Dat VQ, Vuyiseka D, Wijewickrama A, Maguire B, Zeraatkar D, Bartoszko JJ, Ge L, Brignardello-Petersen R, Owen A, Guyatt G, Diaz J, Jacobs M, Vandvik PO. A living WHO guideline on drugs for covid-19. BMJ 2020;370:m3379. [DOI] [PubMed] [Google Scholar]
- 209. WHO Solidarity Trial Consortium; Pan H, Peto R, Henao-Restrepo A-M, Preziosi M-P, Sathiyamoorthy V, Abdool Karim Q, Alejandria MM, Hernández García C, Kieny M-P, Malekzadeh R, Murthy S, Reddy KS, Roses Periago M, Abi Hanna P, Ader F, Al-Bader AM, Alhasawi A, Allum E, Alotaibi A, Alvarez-Moreno CA, Appadoo S, Asiri A, Aukrust P, Barratt-Due A, Bellani S, Branca M, Cappel-Porter HBC, Cerrato N, Chow TS, Como N, Eustace J, García PJ, Godbole S, Gotuzzo E, Griskevicius L, Hamra R, Hassan M, Hassany M, Hutton D, Irmansyah I, Jancoriene L, Kirwan J, Kumar S, Lennon P, Lopardo G, Lydon P, Magrini N, Maguire T, Manevska S, Manuel O, McGinty S, Medina MT, Mesa Rubio ML, Miranda-Montoya MC, Nel J, Nunes EP, Perola M, Portolés A, Rasmin MR, Raza A, Rees H, Reges PPS, Rogers CA, Salami K, Salvadori MI, Sinani N, Sterne JAC, Stevanovikj M, Tacconelli E, Tikkinen KAO, Trelle S, Zaid H, Røttingen J-A, Swaminathan S. Repurposed antiviral drugs for Covid-19—interim WHO solidarity trial results. N Engl J Med. 2021;384:497–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210. Group RC, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, Staplin N, Brightling C, Ustianowski A, Elmahi E, Prudon B, Green C, Felton T, Chadwick D, Rege K, Fegan C, Chappell LC, Faust SN, Jaki T, Jeffery K, Montgomery A, Rowan K, Juszczak E, Baillie JK, Haynes R, Landray MJ. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2021;384:693–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Sterne JAC, Murthy S, Diaz JV, Slutsky AS, Villar J, Angus DC, Annane D, Azevedo LCP, Berwanger O, Cavalcanti AB, Dequin PF, Du B, Emberson J, Fisher D, Giraudeau B, Gordon AC, Granholm A, Green C, Haynes R, Heming N, Higgins JPT, Horby P, Juni P, Landray MJ, Le Gouge A, Leclerc M, Lim WS, Machado FR, McArthur C, Meziani F, Moller MH, Perner A, Petersen MW, Savovic J, Tomazini B, Veiga VC, Webb S, Marshall JC. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020;324:1330–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212. Ramakrishnan S, Nicolau DV Jr, Langford B, Mahdi M, Jeffers H, Mwasuku C, Krassowska K, Fox R, Binnian I, Glover V, Bright S, Butler C, Cane JL, Halner A, Matthews PC, Donnelly LE, Simpson JL, Baker JR, Fadai NT, Peterson S, Bengtsson T, Barnes PJ, Russell REK, Bafadhel M. Inhaled budesonide in the treatment of early COVID-19 (STOIC): a phase 2, open-label, randomised controlled trial. Lancet Respir Med 2021;9:763–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Insufficient data on use of inhaled corticosteroids to treat COVID-19. https://www.ema.europa.eu/en/news/insufficient-data-use-inhaled-corticosteroids-treat-covid-19. (29 May 2021, date last accessed).
- 214. Group RC, Horby P, Mafham M, Linsell L, Bell JL, Staplin N, Emberson JR, Wiselka M, Ustianowski A, Elmahi E, Prudon B, Whitehouse T, Felton T, Williams J, Faccenda J, Underwood J, Baillie JK, Chappell LC, Faust SN, Jaki T, Jeffery K, Lim WS, Montgomery A, Rowan K, Tarning J, Watson JA, White NJ, Juszczak E, Haynes R, Landray MJ. Effect of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med 2020;383:2030–2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Cavalcanti AB, Zampieri FG, Rosa RG, Azevedo LCP, Veiga VC, Avezum A, Damiani LP, Marcadenti A, Kawano-Dourado L, Lisboa T, Junqueira DLM, de Barros E, Tramujas L, Abreu-Silva EO, Laranjeira LN, Soares AT, Echenique LS, Pereira AJ, Freitas FGR, Gebara OCE, Dantas VCS, Furtado RHM, Milan EP, Golin NA, Cardoso FF, Maia IS, Hoffmann Filho CR, Kormann APM, Amazonas RB, Bocchi de Oliveira MF, Serpa-Neto A, Falavigna M, Lopes RD, Machado FR, Berwanger O; Coalition Covid-19 Brazil II. Hydroxychloroquine with or without azithromycin in mild-to-moderate Covid-19. N Engl J Med 2020;383:2041–2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. RECOVERY Collaborative Group. Lopinavir-ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet 2020;396:1345–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217. Lescure FX, Honda H, Fowler RA, Lazar JS, Shi G, Wung P, Patel N, Hagino O, Sarilumab C-G; Sarilumab COVID-19 Global Study Group. Sarilumab in patients admitted to hospital with severe or critical COVID-19: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Respir Med 2021;9:522–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218. Group RC. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet 2021;397:1637–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Soin AS, Kumar K, Choudhary NS, Sharma P, Mehta Y, Kataria S, Govil D, Deswal V, Chaudhry D, Singh PK, Gupta A, Agarwal V, Kumar S, Sangle SA, Chawla R, Narreddy S, Pandit R, Mishra V, Goel M, Ramanan AV. Tocilizumab plus standard care versus standard care in patients in India with moderate to severe COVID-19-associated cytokine release syndrome (COVINTOC): an open-label, multicentre, randomised, controlled, phase 3 trial. Lancet Respir Med 2021;9:511–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220. The REMAP-CAP Investigators; Gordon AC, Mouncey PR, Al-Beidh F, Rowan KM, Nichol AD, Arabi YM, Annane D, Beane A, van Bentum-Puijk W, Berry LR, Bhimani Z, Bonten MJM, Bradbury CA, Brunkhorst FM, Buzgau A, Cheng AC, Detry MA, Duffy EJ, Estcourt LJ, Fitzgerald M, Goossens H, Haniffa R, Higgins AM, Hills TE, Horvat CM, Lamontagne F, Lawler PR, Leavis HL, Linstrum KM, Litton E, Lorenzi E, Marshall JC, Mayr FB, McAuley DF, McGlothlin A, McGuinness SP, McVerry BJ, Montgomery SK, Morpeth SC, Murthy S, Orr K, Parke RL, Parker JC, Patanwala AE, Pettila V, Rademaker E, Santos MS, Saunders CT, Seymour CW, Shankar-Hari M, Sligl WI, Turgeon AF, Turner AM, van de Veerdonk FL, Zarychanski R, Green C, Lewis RJ, Angus DC, McArthur CJ, Berry S, Webb SA, Derde LPG. Interleukin-6 receptor antagonists in critically ill patients with Covid-19. N Engl J Med 2021;384:1491–1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Rosas IO, Brau N, Waters M, Go RC, Hunter BD, Bhagani S, Skiest D, Aziz MS, Cooper N, Douglas IS, Savic S, Youngstein T, Del Sorbo L, Cubillo Gracian A, De La Zerda DJ, Ustianowski A, Bao M, Dimonaco S, Graham E, Matharu B, Spotswood H, Tsai L, Malhotra A. Tocilizumab in hospitalized patients with severe Covid-19 pneumonia. N Engl J Med 2021;384:1503–1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222. Weinreich DM, Sivapalasingam S, Norton T, Ali S, Gao H, Bhore R, Musser BJ, Soo Y, Rofail D, Im J, Perry C, Pan C, Hosain R, Mahmood A, Davis JD, Turner KC, Hooper AT, Hamilton JD, Baum A, Kyratsous CA, Kim Y, Cook A, Kampman W, Kohli A, Sachdeva Y, Graber X, Kowal B, DiCioccio T, Stahl N, Lipsich L, Braunstein N, Herman G, Yancopoulos GD; Trial Investigators. REGN-COV2, a neutralizing antibody cocktail, in outpatients with Covid-19. N Engl J Med. 2021;384:238–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223. Chen P, Nirula A, Heller B, Gottlieb RL, Boscia J, Morris J, Huhn G, Cardona J, Mocherla B, Stosor V, Shawa I, Adams AC, Van Naarden J, Custer KL, Shen L, Durante M, Oakley G, Schade AE, Sabo J, Patel DR, Klekotka P, Skovronsky DM; BLAZE-1 Investigators. SARS-CoV-2 neutralizing antibody LY-CoV555 in outpatients with Covid-19. N Engl J Med 2021;384:229–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Gottlieb RL, Nirula A, Chen P, Boscia J, Heller B, Morris J, Huhn G, Cardona J, Mocherla B, Stosor V, Shawa I, Kumar P, Adams AC, Van Naarden J, Custer KL, Durante M, Oakley G, Schade AE, Holzer TR, Ebert PJ, Higgs RE, Kallewaard NL, Sabo J, Patel DR, Klekotka P, Shen L, Skovronsky DM. Effect of bamlanivimab as monotherapy or in combination with etesevimab on viral load in patients with mild to moderate COVID-19: a randomized clinical trial. JAMA 2021;325:632–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. EMA issues advice on use of REGN-COV2 antibody combination (casirivimab/imdevimab). https://www.ema.europa.eu/en/news/ema-issues-advice-use-regn-cov2-antibody-combination-casirivimab-imdevimab (02 June 2021, date last accessed).
- 226. EMA issues advice on use of antibody combination (bamlanivimab/etesevimab). https://www.ema.europa.eu/en/news/ema-issues-advice-use-antibody-combination-bamlanivimab-etesevimab (02 June 2021, date last accessed).
- 227. Fact sheet for health care providers emergency use authorization (EUA) of bamlanivimab and etesevimab. https://www.fda.gov/media/145802/download (02 June 2021, date last accessed).
- 228. Fact sheet for health care providers emergency use authorization (EUA) of casirivimab and imdevimab. https://www.fda.gov/media/143892/download (02 June 2021, date last accessed).
- 229. Marovich M, Mascola JR, Cohen MS. Monoclonal antibodies for prevention and treatment of COVID-19. JAMA 2020;324:131–132. [DOI] [PubMed] [Google Scholar]
- 230. Hoffmann M, Hofmann-Winkler H, Smith JC, Krüger N, Arora P, Sørensen LK, Søgaard OS, Hasselstrøm JB, Winkler M, Hempel T, Raich L, Olsson S, Danov O, Jonigk D, Yamazoe T, Yamatsuta K, Mizuno H, Ludwig S, Noé F, Kjolby M, Braun A, Sheltzer JM, Pöhlmann S. Camostat mesylate inhibits SARS-CoV-2 activation by TMPRSS2-related proteases and its metabolite GBPA exerts antiviral activity. EBioMedicine 2021;65:103255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231. Okuno M, Akita K, Moriwaki H, Kawada N, Ikeda K, Kaneda K, Suzuki Y, Kojima S. Prevention of rat hepatic fibrosis by the protease inhibitor, camostat mesilate, via reduced generation of active TGF-beta. Gastroenterology 2001;120:1784–1800. [DOI] [PubMed] [Google Scholar]
- 232. Gunst JD, Staerke NB, Pahus MH, Kristensen LH, Bodilsen J, Lohse N, Dalgaard LS, Brønnum D, Fröbert O, Hønge B, Johansen IS, Monrad I, Erikstrup C, Rosendal R, Vilstrup E, Mariager T, Bove DG, Offersen R, Shakar S, Cajander S, Jørgensen NP, Sritharan SS, Breining P, Jespersen S, Mortensen KL, Jensen ML, Kolte L, Frattari GS, Larsen CS, Storgaard M, Nielsen LP, Tolstrup M, Sædder EA, Østergaard LJ, Ngo HTT, Jensen MH, Højen JF, Kjolby M, Søgaard OS. Efficacy of the TMPRSS2 inhibitor camostat mesilate in patients hospitalized with Covid-19-a double-blind randomized controlled trial. EClinicalMedicine 2021;35:100849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233. Fernández-Avilés F, Sanz-Ruiz R, Climent AM, Badimon L, Bolli R, Charron D, Fuster V, Janssens S, Kastrup J, Kim H-S, Lüscher TF, Martin JF, Menasché P, Simari RD, Stone GW, Terzic A, Willerson JT, Wu JC; TACTICS (Transnational Alliance for Regenerative Therapies in Cardiovascular Syndromes) Writing Group; Authors/Task Force Members. Chairpersons; Basic Research Subcommittee; Translational Research Subcommittee; Challenges of Cardiovascular Regenerative Medicine Subcommittee; Tissue Engineering Subcommittee; Delivery, Navigation, Tracking and Assessment Subcommittee; Clinical Trials Subcommittee; Regulatory and funding strategies subcommittee; Delivery, Navigation, Tracking and Assessment Subcommittee. Global position paper on cardiovascular regenerative medicine. Eur Heart J 2017;38:2532–2546.28575280 [Google Scholar]
- 234. Singh S, Chakravarty T, Chen P, Akhmerov A, Falk J, Friedman O, Zaman T, Ebinger JE, Gheorghiu M, Marban L, Marban E, Makkar RR. Allogeneic cardiosphere-derived cells (CAP-1002) in critically ill COVID-19 patients: compassionate-use case series. Basic Res Cardiol 2020;115:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235. Shu L, Niu C, Li R, Huang T, Wang Y, Huang M, Ji N, Zheng Y, Chen X, Shi L, Wu M, Deng K, Wei J, Wang X, Cao Y, Yan J, Feng G. G. Treatment of severe COVID-19 with human umbilical cord mesenchymal stem cells. Stem Cell Res Ther 2020;11:361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236. Leng Z, Zhu R, Hou W, Feng Y, Yang Y, Han Q, Shan G, Meng F, Du D, Wang S, Fan J, Wang W, Deng L, Shi H, Li H, Hu Z, Zhang F, Gao J, Liu H, Li X, Zhao Y, Yin K, He X, Gao Z, Wang Y, Yang B, Jin R, Stambler I, Lim LW, Su H, Moskalev A, Cano A, Chakrabarti S, Min KJ, Ellison-Hughes G, Caruso C, Jin K, Zhao RC. Transplantation of ACE2(-) mesenchymal stem cells improves the outcome of patients with COVID-19 pneumonia. Aging Dis 2020;11:216–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237. Lanzoni G, Linetsky E, Correa D, Messinger Cayetano S, Alvarez RA, Kouroupis D, Alvarez Gil A, Poggioli R, Ruiz P, Marttos AC, Hirani K, Bell CA, Kusack H, Rafkin L, Baidal D, Pastewski A, Gawri K, Lenero C, Mantero AMA, Metalonis SW, Wang X, Roque L, Masters B, Kenyon NS, Ginzburg E, Xu X, Tan J, Caplan AI, Glassberg MK, Alejandro R, Ricordi C. Umbilical cord mesenchymal stem cells for COVID-19 acute respiratory distress syndrome: A double-blind, phase 1/2a, randomized controlled trial. Stem Cells Transl Med 2021;10:660–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238. Schafer R, Spohn G, Bechtel M, Bojkova D, Baer PC, Kuci S, Seifried E, Ciesek S, Cinatl J. Human mesenchymal stromal cells are resistant to SARS-CoV-2 infection under steady-state, inflammatory conditions and in the presence of SARS-CoV-2-infected cells. Stem Cell Reports 2021;16:419–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239. Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, Pujol JC, Klaser K, Antonelli M, Canas LS, Molteni E, Modat M, Jorge Cardoso M, May A, Ganesh S, Davies R, Nguyen LH, Drew DA, Astley CM, Joshi AD, Merino J, Tsereteli N, Fall T, Gomez MF, Duncan EL, Menni C, Williams FMK, Franks PW, Chan AT, Wolf J, Ourselin S, Spector T, Steves CJ. Attributes and predictors of long COVID. Nat Med 2021;27:626–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240. Datta SD, Talwar A, Lee JT. A proposed framework and timeline of the spectrum of disease due to SARS-CoV-2 infection: illness beyond acute infection and public health implications. JAMA 2020;324:2251–2252. [DOI] [PubMed] [Google Scholar]
- 241. Greenhalgh T, Knight M, A'Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ 2020;370:m3026. [DOI] [PubMed] [Google Scholar]
- 242. Shah W, Hillman T, Playford ED, Hishmeh L. Managing the long term effects of covid-19: summary of NICE, SIGN, and RCGP rapid guideline. BMJ 2021;372:n136. [DOI] [PubMed] [Google Scholar]
- 243. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, Kang L, Guo L, Liu M, Zhou X, Luo J, Huang Z, Tu S, Zhao Y, Chen L, Xu D, Li Y, Li C, Peng L, Li Y, Xie W, Cui D, Shang L, Fan G, Xu J, Wang G, Wang Y, Zhong J, Wang C, Wang J, Zhang D, Cao B. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 2021;397:220–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244. Daugherty SE, Guo Y, Heath K, Dasmarinas MC, Jubilo KG, Samranvedhya J, Lipsitch M, Cohen K. Risk of clinical sequelae after the acute phase of SARS-CoV-2 infection: retrospective cohort study. BMJ 2021;373:n1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245. Chopra V, Flanders SA, O'Malley M, Malani AN, Prescott HC. Sixty-day outcomes among patients hospitalized with COVID-19. Ann Intern Med 2021;174:576–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Carfi A, Bernabei R, Landi F; Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19. JAMA 2020;324:603–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247. Carvalho-Schneider C, Laurent E, Lemaignen A, Beaufils E, Bourbao-Tournois C, Laribi S, Flament T, Ferreira-Maldent N, Bruyère F, Stefic K, Gaudy-Graffin C, Grammatico-Guillon L, Bernard L. L. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin Microbiol Infect 2021;27:258–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Garrigues E, Janvier P, Kherabi Y, Le Bot A, Hamon A, Gouze H, Doucet L, Berkani S, Oliosi E, Mallart E, Corre F, Zarrouk V, Moyer JD, Galy A, Honsel V, Fantin B, Nguyen Y. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Infect 2020;81:e4–e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249. Ayoubkhani D, Khunti K, Nafilyan V, Maddox T, Humberstone B, Diamond I, Banerjee A. Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study. BMJ 2021;372:n693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250. Han X, Fan Y, Alwalid O, Li N, Jia X, Yuan M, Li Y, Cao Y, Gu J, Wu H, Shi H. Six-month follow-up chest CT findings after severe COVID-19 pneumonia. Radiology 2021;299:E177–E186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251. Mendez R, Latorre A, Gonzalez-Jimenez P, Feced L, Bouzas L, Yepez K, Ferrando A, Zaldivar-Olmeda E, Reyes S, Menendez R. Reduced diffusion capacity in COVID-19 survivors. Ann Am Thorac Soc 2021;18:1253–1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252. Kumar S, Wang G, Zheng N, Cheng W, Ouyang K, Lin H, Liao Y, Liu J. HIMF (Hypoxia-Induced Mitogenic Factor)-IL (Interleukin)-6 signaling mediates cardiomyocyte-fibroblast crosstalk to promote cardiac hypertrophy and fibrosis. Hypertension 2019;73:1058–1070. [DOI] [PubMed] [Google Scholar]
- 253. Frangogiannis NG. Cardiac fibrosis: cell biological mechanisms, molecular pathways and therapeutic opportunities. Mol Aspects Med 2019;65:70–99. [DOI] [PubMed] [Google Scholar]
- 254. Johansson M, Stahlberg M, Runold M, Nygren-Bonnier M, Nilsson J, Olshansky B, Bruchfeld J, Fedorowski A. Long-Haul post-COVID-19 symptoms presenting as a variant of postural orthostatic tachycardia syndrome: the Swedish Experience. JACC Case Rep 2021;3:573–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255. Arano Llach J, Victor Bazan V, Gemma Llados G, Raquel Adelino R, Maria Jesus Dominguez M, Marta Massanella M, Felipe Bisbal F, Axel Sarrias A, Antoni Bayes-Genis A, Lourdes Mateu L, Roger Villuendas Sabate R. Inappropriate sinus tachycardia in post-covid-19 Syndrome. Europace 2021;23:euab116.114. doi. 10.1093/europace/euab116.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256. Lau ST, Yu WC, Mok NS, Tsui PT, Tong WL, Cheng SW. Tachycardia amongst subjects recovering from severe acute respiratory syndrome (SARS). Int J Cardiol 2005;100:167–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257. Raman B, Cassar MP, Tunnicliffe EM, Filippini N, Griffanti L, Alfaro-Almagro F, Okell T, Sheerin F, Xie C, Mahmod M, Mozes FE, Lewandowski AJ, Ohuma EO, Holdsworth D, Lamlum H, Woodman MJ, Krasopoulos C, Mills R, McConnell FAK, Wang C, Arthofer C, Lange FJ, Andersson J, Jenkinson M, Antoniades C, Channon KM, Shanmuganathan M, Ferreira VM, Piechnik SK, Klenerman P, Brightling C, Talbot NP, Petousi N, Rahman NM, Ho LP, Saunders K, Geddes JR, Harrison PJ, Pattinson K, Rowland MJ, Angus BJ, Gleeson F, Pavlides M, Koychev I, Miller KL, Mackay C, Jezzard P, Smith SM, Neubauer S. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. EClinicalMedicine 2021;31:100683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258. Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, Shchendrygina A, Escher F, Vasa-Nicotera M, Zeiher AM, Vehreschild M, Nagel E. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:1265–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259. Rajpal S, Tong MS, Borchers J, Zareba KM, Obarski TP, Simonetti OP, Daniels CJ. Cardiovascular magnetic resonance findings in competitive athletes recovering from COVID-19 infection. JAMA Cardiol 2021;6:116–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260. Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C, Liu W, Zeng H, Tao Q, Xia L. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc Imaging 2020;13:2330–2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261. Kotecha T, Knight DS, Razvi Y, Kumar K, Vimalesvaran K, Thornton G, Patel R, Chacko L, Brown JT, Coyle C, Leith D, Shetye A, Ariff B, Bell R, Captur G, Coleman M, Goldring J, Gopalan D, Heightman M, Hillman T, Howard L, Jacobs M, Jeetley PS, Kanagaratnam P, Kon OM, Lamb LE, Manisty CH, Mathurdas P, Mayet J, Negus R, Patel N, Pierce I, Russell G, Wolff A, Xue H, Kellman P, Moon JC, Treibel TA, Cole GD, Fontana M. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur Heart J 2021;42:1866–1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262. Brito D, Meester S, Yanamala N, Patel HB, Balcik BJ, Casaclang-Verzosa G, Seetharam K, Riveros D, Beto RJ 2nd, Balla S, Monseau AJ, Sengupta PP. High prevalence of pericardial involvement in college student athletes recovering from COVID-19. JACC Cardiovasc Imaging 2021;14:541–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263. Friedrich MG, Cooper LT. What we (don't) know about myocardial injury after COVID-19. Eur Heart J 2021;42:1879–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264. Conti CR, Bavry AA, Petersen JW. Silent ischemia: clinical relevance. J Am Coll Cardiol 2012;59:435–441. [DOI] [PubMed] [Google Scholar]
- 265. Bugiardini R, Borghi A, Sassone B, Pozzati A, Puddu P. Prognostic significance of silent myocardial ischemia in variant angina pectoris. Am J Cardiol 1991;68:1581–1586. [DOI] [PubMed] [Google Scholar]
- 266. Blanco-Domínguez R, Sánchez-Díaz R, de la Fuente H, Jiménez-Borreguero LJ, Matesanz-Marín A, Relaño M, Jiménez-Alejandre R, Linillos-Pradillo B, Tsilingiri K, Martín-Mariscal ML, Alonso-Herranz L, Moreno G, Martín-Asenjo R, García-Guimaraes MM, Bruno KA, Dauden E, González-Álvaro I, Villar-Guimerans LM, Martínez-León A, Salvador-Garicano AM, Michelhaugh SA, Ibrahim NE, Januzzi JL, Kottwitz J, Iliceto S, Plebani M, Basso C, Baritussio A, Seguso M, Marcolongo R, Ricote M, Fairweather D, Bueno H, Fernández-Friera L, Alfonso F, Caforio ALP, Pascual-Figal DA, Heidecker B, Lüscher TF, Das S, Fuster V, Ibáñez B, Sánchez-Madrid F, Martín P. A novel circulating microRNA for the detection of acute myocarditis. N Engl J Med 2021;384:2014–2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267. Dhawan RT, Gopalan D, Howard L, Vicente A, Park M, Manalan K, Wallner I, Marsden P, Dave S, Branley H, Russell G, Dharmarajah N, Kon OM. Beyond the clot: perfusion imaging of the pulmonary vasculature after COVID-19. Lancet Respir Med 2021;9:107–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268. Rashidi F, Barco S, Kamangar F, Heresi GA, Emadi A, Kaymaz C, Jansa P, Reis A, Rashidi A, Taghizadieh A, Rezaeifar P, Moghimi M, Ghodrati S, Mozafari A, Foumani AA, Tahamtan O, Rafiee E, Abbaspour Z, Khodadadi K, Alamdari G, Boodaghi Y, Rezaei M, Muhammadi MJ, Abbasi M, Movaseghi F, Koohi A, Shakourzad L, Ebrahimi F, Radvar S, Amoozadeh M, Fereidooni F, Naseari H, Movalled K, Ghorbani O, Ansarin K. Incidence of symptomatic venous thromboembolism following hospitalization for coronavirus disease 2019: prospective results from a multi-center study. Thromb Res 2021;198:135–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269. Roberts LN, Whyte MB, Georgiou L, Giron G, Czuprynska J, Rea C, Vadher B, Patel RK, Gee E, Arya R. Postdischarge venous thromboembolism following hospital admission with COVID-19. Blood 2020;136:1347–1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270. Patell R, Bogue T, Koshy A, Bindal P, Merrill M, Aird WC, Bauer KA, Zwicker JI. Postdischarge thrombosis and hemorrhage in patients with COVID-19. Blood 2020;136:1342–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271. Salisbury R, Iotchkova V, Jaafar S, Morton J, Sangha G, Shah A, Untiveros P, Curry N, Shapiro S. Incidence of symptomatic, image-confirmed venous thromboembolism following hospitalization for COVID-19 with 90-day follow-up. Blood Adv 2020;4:6230–6239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272. Rubino F, Amiel SA, Zimmet P, Alberti G, Bornstein S, Eckel RH, Mingrone G, Boehm B, Cooper ME, Chai Z, Del Prato S, Ji L, Hopkins D, Herman WH, Khunti K, Mbanya JC, Renard E. New-onset diabetes in Covid-19. N Engl J Med 2020;383:789–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273. Li J, Wang X, Chen J, Zuo X, Zhang H, Deng A. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes Metab 2020;22:1935–1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274. Hayden MR. An immediate and long-term complication of COVID-19 may be type 2 diabetes mellitus: the central role of beta-cell dysfunction, apoptosis and exploration of possible mechanisms. Cells 2020;9:2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275. Cariou B, Hadjadj S, Wargny M, Pichelin M, Al-Salameh A, Allix I, Amadou C, Arnault G, Baudoux F, Bauduceau B, Borot S, Bourgeon-Ghittori M, Bourron O, Boutoille D, Cazenave-Roblot F, Chaumeil C, Cosson E, Coudol S, Darmon P, Disse E, Ducet-Boiffard A, Gaborit B, Joubert M, Kerlan V, Laviolle B, Marchand L, Meyer L, Potier L, Prevost G, Riveline J-P, Robert R, Saulnier P-J, Sultan A, Thébaut J-F, Thivolet C, Tramunt B, Vatier C, Roussel R, Gautier J-F, Gourdy P; CORONADO investigators. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia 2020;63:1500–1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276. Yang JK, Lin SS, Ji XJ, Guo LM. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol 2010;47:193–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277. Müller JA, Groß R, Conzelmann C, Krüger J, Merle U, Steinhart J, Weil T, Koepke L, Bozzo CP, Read C, Fois G, Eiseler T, Gehrmann J, van Vuuren J, Wessbecher IM, Frick M, Costa IG, Breunig M, Grüner B, Peters L, Schuster M, Liebau S, Seufferlein T, Stenger S, Stenzinger A, MacDonald PE, Kirchhoff F, Sparrer KMJ, Walther P, Lickert H, Barth TFE, Wagner M, Münch J, Heller S, Kleger A. SARS-CoV-2 infects and replicates in cells of the human endocrine and exocrine pancreas. Nat Metab 2021;3:149–165. [DOI] [PubMed] [Google Scholar]
- 278. Atkinson MA, Powers AC. Distinguishing the real from the hyperglycaemia: does COVID-19 induce diabetes? Lancet Diabetes Endocrinol 2021;9:328–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279. Derumeaux GA. From metabolic exposome to onset of diabetic cardiomyopathy. JACC Cardiovasc Imaging 2017;10:115–117. [DOI] [PubMed] [Google Scholar]
- 280. Di Domenico L, Pullano G, Sabbatini CE, Boëlle PY, Colizza V. Impact of lockdown on COVID-19 epidemic in Île-de-France and possible exit strategies. BMC Med. 2020;18(1):240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281. Emanueli C, Badimon L, Martelli F, Potocnjak I, Carpusca I, Robinson EL, Devaux Y. Call to action for the cardiovascular side of COVID-19. Eur Heart J 2020;41:1796–1797. [DOI] [PMC free article] [PubMed] [Google Scholar]