Summary
This study aims to review articles reporting the perspectives and experiences of pandemic-related discrimination among racially minoritized peoples in high-income contexts. We searched online databases (Medline, EMBASE, PsycINFO, Web of Science, and ProQuest) for peer-reviewed articles published between January 2002 and October 2020. Eligible studies reported either quantitative or qualitative accounts of pandemic-related discrimination from the perspectives of racially minoritized peoples in high-income contexts. Two authors screened 30% of titles/abstracts, and all full-text articles. Each article included for extraction underwent a quality assessment by two reviewers. Data were extracted and categorized thematically using NVivo 12, followed by a secondary analysis informed by critical race theory. Of the 1289 articles screened, 16 articles from five countries met the inclusion criteria. Racial discrimination is heightened during pandemic periods, due to the social association of specific racial groups with pandemic diseases including COVID-19, SARS (Asian), H1N1 (Hispanic) and Ebola (African). Fear based responses to racially minoritized peoples during pandemic periods included verbal/physical abuse, hypersurveillance, and avoidance, often occurring in public spaces. Pandemic-related racism had subsequent impacts on mental health and health care accessibility. Various coping strategies, including community support, avoidance, and problem solving, were documented in response to racial discrimination. Racialized discrimination and violence is a serious threat to the health and wellbeing of racially minoritized peoples, particularly due to its increase during pandemic periods. Racism must be recognized as a public health issue, and efforts to address its increased impact in pandemic contexts should be made, including ensuring that adequate representation of racially minoritized groups is present in policy, planning, and implementation.
Keywords: public health, stigma, racial discrimination, pandemic, ethnic minorities
INTRODUCTION
Racial discrimination is linked to health outcomes in ways that are both structural and individual. The former places race as the linking factor between persistent systemic social inequities experienced by racially minoritized communities, and the prevalence of health problems they face as a result, including most recently the impact of the novel coronavirus disease (COVID-19) (McKnight-Eily et al., 2021). The latter looks at experiences of or exposure to racial discrimination as a determinant of health, and its association with poor mental health outcomes such as depression, post-traumatic stress disorder and suicidal ideation; and physical health outcomes including obesity and high blood pressure (Paradies et al., 2015). Previous research has explored the connection between stress neurobiology and the mental health of racially minoritized peoples, highlighting the long-term negative health impact of elevated cortisol levels (stress) among those who have experienced discrimination (Berger and Sarnyai, 2015).
In high-income contexts, racial discrimination is experienced by ethnic and cultural groups that are marginal from the dominant culture, largely comprising those of Asian, African, Hispanic and Indigenous descent (Paradies et al., 2015). Despite the impact of racial discrimination on the health of racially minoritized peoples, this remains an emerging area of research. Furthermore, how racism operates in moments of generalized moral panic experienced through a pandemic is not well explored (Leung, 2008). Generally, pandemics evidence rising levels of fear, as quarantine and isolation are introduced as public health measures (Person et al., 2004; Weiss et al., 2006). There is currently a limited understanding of how pandemic-related racial discrimination is experienced, nor how experiences of racism intersect with poorer determinants of health. This is a problem when those experiencing racism and poverty are less likely to seek help or adhere to population-based health advice in a global pandemic (Keil and Ali, 2006; Truman et al., 2009).
Racially minoritized (Milner and Jumbe, 2020) people have historically faced discrimination during pandemics and epidemics. Previous evidence has shown that pandemics and discriminatory behavior coincide, including the Severe Acute Respiratory Syndrome (SARS) pandemic (Eichelberger, 2007). More recently, as a consequence of the novel SARS coronavirus 2 and the associated COVID-19, racially minoritized people are facing a new wave of racism as a result of misleading and biased media (Larsson, 2020; Shimizu, 2020; Wen et al., 2020). Following Milner and Jumbe’s (Milner and Jumbe, 2020) call for using appropriate language to discuss the racial health disparities foregrounded by COVID-19, we use the term ‘racially minoritized’. This term pays attention to how people from non-dominant cultural backgrounds are actively racialized, or minoritized, in ways socially constructed and shaped by power (Milner and Jumbe, 2020).
Our review aimed to identify and describe pandemic-related experiences or perceptions of discrimination among non-Indigenous, racially minoritized groups in high-income contexts, including whether this impacts health outcomes or access to health services. We chose to focus on high-income countries as it is primarily within these contexts where groups of people are classified as ‘racial minorities’, due to ethnic and cultural differences in relation to dominant Western value systems and norms. We respectfully excluded Indigenous peoples from this review for two reasons. First, we acknowledge that the types of racism toward and experienced by Indigenous peoples in high-income contexts are different to that of migrant settlers that comprise racially minoritized groups. The complexities around active resistance of ongoing settler colonization, and its centrality in the cultural and physical survival, places Indigenous peoples in a different and sometimes conflicting position with other racially minoritized groups, who are also settlers. We did not wish to homogenize these differing realities. Second, evidence discussing the rise in racism at the onset of the COVID-19 pandemic, particularly toward people of Asian descent (Larsson, 2020), prompted us to focus on non-Indigenous racially minoritized groups. Furthermore, HIV/AIDS pandemic research was also excluded from this review. The focus was pandemic diseases that are communicable via non-sexual transmission such as, but not limited to, influenza and coronaviruses. Additionally, the authors agreed that as a sexually transmitted infection, the complexities associated with the spread of HIV/AIDS may not apply to pandemics associated with airborne or direct contact transmission.
METHODS
The search strategy followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Moher et al., 2009) and Realist And Meta-narrative Evidence Syntheses: Evolving Standards guidelines (Wong et al., 2013). The following databases were searched for studies published between January 2002 and October 2020: Medline/EMBASE, PsycINFO, Web of Science and ProQuest Central/Coronavirus Database. A set of search terms (Table 1) used for each area of interest were compiled. Where available MeSH terms were used in addition to key words, and where relevant proximity operators were used to minimize capturing irrelevant papers. The database search results were imported into a single library in EndNote (Clarivate Analytics, USA) where duplicates were removed. The combined library was imported into Covidence systematic review software (Veritas Health Information, Australia) for title/abstract and full text screening. As this was a desk-based review of literature, ethical approval was not required.
Table 1:
Search term groups were combined with the Boolean operator ‘AND’
| SEARCH #1 Pandemics |
| Pandemics/or Epidemics/OR Disease Outbreaks/OR Coronavirus/OR Coronavirus Infections/OR COVID-19 or COVID 19 or coronavirus or corona virus or SARS-CoV-2 or novel coronavirus or sars cov or SARS or MERS or Middle East Respiratory Syndrome or H1N1 or pandemic or epidemic |
| SEARCH #2 Racism |
| Racism/OR Prejudice/OR racism or racial discrimination or racial bias or perceived discrimination or prejud* or hostil* or harass* or bully* or unfair* treat* or oppress* or abuse* or abusive or stigma* |
| SEARCH #3 Population |
| Ethnic Groups/ |
| Minority Groups/ |
| [(ethnic$or racial$or cultur$) adj3 (group$or minorit$or population$or diverse$or origin$)].tw. |
| [(ethnic$or racial$or cultur$) adj3 (inequalit$or inequit$or disparit$or equit$or disadvantage$or depriv$)].tw. |
| [(population$or communit$) adj3 (divers$or disadvantage$or depriv$)].tw. |
| non-Indigenous.tw. |
| (visible adj1 minorit$).tw. |
| Refugees/ |
| ‘emigrants and immigrants’/ |
| (migrant$or immigrant$or emigrant$or refugee$or expatriate$).tw. |
| asylum seeker$.tw. |
| Urban population/ |
| Cultural characteristics/ |
| Cross-cultural comparison/ |
| Cultural diversity/ |
| Cultural competency/ |
| Cultural deprivation/ |
| exp African continental ancestry group/ |
| exp Asian continental ancestry group/ |
| Continental population groups/ |
| (Afr$adj2 American$).tw. |
| (Afr$adj2 Caribbean$).tw. |
| [west adj2 (india$or indies)].tw. |
| (American$adj1 black).tw. |
| (Asian$or Indian$or Pakistan$or Bangladesh$or Bengal$or Chinese$).tw. |
| [(Asia$or Pacific) adj4 American$].tw. |
| [(Asia$or Pacific) adj4 Islander$].tw. |
| (Hispanic or Latino or Latin American$or Puerto Ric$or Mexican$).tw. |
Inclusion and exclusion criteria
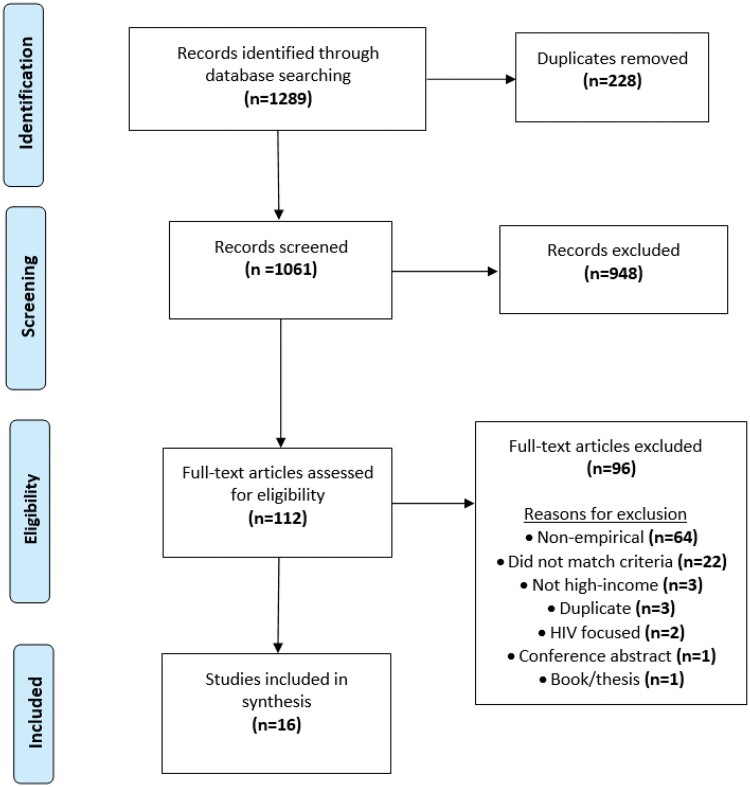
Articles were included in the review if they: (i) included the perspectives of racially minoritized, non-dominant, non-Indigenous people on pandemic-related discrimination, (ii) contained empirical research, (iii) are in a high-income context and (iv) were published in a peer-reviewed journal. Articles were excluded if they: (i) were reviews, study protocols, commentaries, editorials, gray literature or books/theses, (ii) did not contain data related to pandemic-related discrimination, (iii) were HIV related or (iv) were not in English. Reasons for exclusion are shown in the PRISMA flow diagram (Figure 1).
Fig. 1:
PRISMA flow chart of systematic review process and sampling.
Study selection
Using the inclusion and exclusion criteria, titles and abstracts of all articles retrieved were assessed by an independent reviewer and a 30% sample were reviewed by a second reviewer to address risk of selection bias. Where it was unclear whether the selection criteria were met, studies were included for full text review. All full text articles were reviewed by two independent reviewers. Disagreements were resolved by a third reviewer.
Quality assessment
To limit the risk of bias, the quality of included articles was independently assessed by two reviewers using the QualSyst tool (Kmet, 2004) and disagreements were resolved by discussion. The QualSyst tool, developed for assessing qualitative and quantitative studies, applies a scoring system to specific aspects of study design and reporting (final calculated score: range, 0–1.00). For mixed methods studies, both qualitative and quantitative aspects were assessed using the QualSyst tool and a combined average score was calculated.
Data analysis and synthesis
For the purpose of this review, several key concepts were defined to guide the review and analysis process. Central to this paper is the concept of race, which has been defined as constructed through the perception of physical (e.g. skin color) and non-physical (e.g. language) signifiers that are used to socially construct classifications of difference (Hall, 1996), which subsequently reinforce existing stereotypes (Fanon, 1967). The plural term ‘racisms’ is used to acknowledge the diverse ways that the phenomenon manifests across time and place, including the importance of historical power relationships, ideology and forms of discrimination (Garner, 2017). We refer to the racial concepts of white and whiteness, not as pigmentation, but as a social construct that reinforces the materialization and naturalization of power through identification with dominant cultural values (Leonardo, 2002). Importantly, we use the classical definition of a pandemic as ‘an epidemic occurring worldwide, or over a very wide area, crossing international boundaries and usually affecting a large number of people’ (Porta, 2014), while clarifying that this does not include seasonal epidemics such as influenza (Kelly, 2011).
An inductive thematic narrative analysis (Glaser and Strauss, 2009) was performed on each paper identified for inclusion in the final synthesis, whereby any references (qualitative or quantitative) to discrimination, and/or its impact on health access or outcomes from the perspectives of racially minoritized people were coded using NVivo qualitative data analysis software (QSR International Pty Ltd. Version 12, 2018). Only direct quotes or statistical data from included studies were analyzed. Interpretive or synthesized data within papers was excluded. Where studies included non-racially minoritized perspectives, these were excluded from the analysis. Relevant data from included studies were inductively coded line by line, enabling the organic emergence of a thematic framework categorized broadly as perceptions and experiences of pandemic-related racial discrimination which is presented in the results. Critical race theories were drawn upon to further synthesize the identified themes including understanding the way physical and non-physical signifiers (Hall, 1996) acted as a mechanism for racial discrimination. After initial inductive coding was complete, a clear pattern of fear-based reactions and responses to racially minoritized peoples had emerged across the set of included studies. Fanon’s psychoanalytic concept of the ‘phobogenic’ was drawn upon to further synthesize experiences of racial discrimination in the identified papers (Fanon, 1967). Phobogenic responses position racially minoritized peoples as fear-causing by the dominant culture, and are characterized by an internal exaggeration of imminent danger, leading to behaviors associated with fear, hatred, revulsion and paranoid anxiety (Hook, 2004). Application of the theoretical concept of the phobogenic allowed a deeper analysis and understanding of emergent themes. Final codes were discussed and agreed upon by two of the authors, and discrepancies were discussed with the additional two authors. The themes reported in the results are an analytic application of critical race theories to understand structural issues including those related to public health, and the concept of the phobogenic to understand the experiences and perspectives of discrimination among racially minoritized peoples including how this impacts health outcomes. As this was a desk-based systematic review of existing literature, no patients or the public were involved in the design, or conduct, or reporting, or dissemination of the study. For the same reason, ethics approval to conduct the study was not needed or obtained.
RESULTS
The database search identified 1289 potential studies. After removal of duplicates, 1061 titles and abstracts were screened. Of these, 112 full-text publications were retrieved for consideration. A total of 96 articles were excluded after performing the full text review, leaving 16 articles for inclusion. The characteristics and quality assessment scores of the 16 included articles are outlined in Table 2. Quality assessment scores (Kmet, 2004) ranged from low (0.35) to very high (1.00); the mean score was 0.84 (SD, 0.15) reflecting an overall high quality of the studies included. Studies were largely conducted in the United States (USA) (n = 10), while two were conducted in the United Kingdom (UK), and the remainder in Japan, Hong Kong and Poland (n = 3). One study (Abidin and Zeng, 2020) used data from a Facebook group comprising Asian participants from various countries.
Table 2:
Characteristics of included studies
| Reference | Year | Location | Pandemic | Racially minoritized group (sub-group where available) | Study participants | Methods | Quality assessmenta |
|---|---|---|---|---|---|---|---|
| Abidin and Zeng, 2020 | 2020 | Global (Online) | COVID-19 | Asian | Facebook users, sample/demographic data unavailable | Qualitative analysis of social media posts | 0.35 |
| Baptist et al., 2020 | 2020 | USA | COVID-19 | African/Hispanic | Adults with asthma (n = 118) (not racially disaggregated) | Survey | 0.95 |
| Cheah et al., 2020 | 2020 | USA | COVID-19 | Asian (Chinese) | Parents (n = 543), their children (n = 230) | Survey | 0.95 |
| Choi et al., 2020 | 2020 | USA | COVID-19 | Asian (Korean) | Adults (n = 790) | Survey | 0.95 |
| Eichelberger, 2007 | 2007 | USA | SARS | Asian (Chinese) | Community members (residents, business owners, employees of China Town) (n = 37) | Semi-structured interviews | 0.85 |
| Iob et al., 2020 | 2020 | UK | COVID-19 | African/Asian | Adults (n = 5259) | Survey | 1.00 |
| Liu et al., 2020 | 2020 | USA | COVID-19 | African/Hispanic/Asian | Black (n = 229), Hispanic (n = 317), Asian (n = 96) | Survey | 1.00 |
| McCauley et al., 2013 | 2013 | USA | H1N1 | African/Hispanic | African (n = 13), Hispanic (n = 13) | Focus groups | 0.90 |
| Pang, 2021 | 2021 | UK | COVID-19 | Asian (Chinese) | Adults, Children (11–15 years), N not stated | Interviews, field notes | 0.80 |
| Person et al., 2004 | 2004 | USA | SARS | Asian | 70 Key informants | Focus groups | 0.75 |
| Rzymski and Nowicki, 2020 | 2020 | Poland | COVID-19 | Asian (Chinese) | Medical students (n = 85) | Survey | 0.79 |
| Schoch-Spana et al., 2010 | 2010 | USA | H1N1 | Hispanic (Mexican) | Key community informants (n = 33) | Interviews | 0.80 |
| Siu, 2015 | 2015 | Hong Kong | Ebola | African | African residents with a chronic illness (n = 30) | Semi-structured interviews | 0.85 |
| Smith-Morris, 2017 | 2017 | USA | Ebola | African, Hispanic (Mexican) | African (n = 10), Mexican (n = 3) | Interviews, ethnography | 0.90 |
| Yang et al., 2020 | 2020 | USA | COVID-19 | Asian | Adults (n = 242) | Survey | 0.86 |
| Zheng et al., 2005 | 2005 | Japan | SARS | Asian (Chinese) | Students (n = 161) | Semi-structured questionnaire | 0.75 |
Two independent reviewers used the QualSyst tool (Kmet et al. 2004) for mixed method studies to assess quality
Racially minoritized participants from all studies were broadly identified as Asian (n = 11), African (n = 6) or Hispanic (n = 5). The majority of studies were focused on COVID-19 (n = 9), followed by SARS (n = 3), swine flu (H1N1) (n = 2) and Ebola (n = 2). A coding framework is presented in Table 3, which shows how identified themes were organized, and examples of references from the included studies. The results of the thematic synthesis are presented in four overarching domains: (i) phobogenic basis to pandemic-related racism; (ii) experiences of pandemic-related racism; (iii) coping strategies and (iv) impact on health equity.
Table 3:
Thematic synthesis coding framework
| Parent code | Sub-code 1 | Sub-code 2 | Relevant study quote (reference) |
|---|---|---|---|
| Perceptions of racially minoritized people during pandemics | Phobogenic responses | Xenophobia |
|
| Sinophobia | ‘The media needs to educate ALL people not to relate the virus only with the Chinese. Just like would you say all Blacks have Ebola, or AIDS? Of course not. This is the same racial mentality. This is how the society has constructed fear towards the Chinese’ (Pang, 2021). | ||
| Negrophobia | ‘Many Hong Kong people were unfriendly to me when I first came here. They called me ‘black ghost’, and they kept a distance from me. They labelled us as AIDS carriers, and they were afraid of me. No matter when I went to a shop or a restaurant, I was not welcomed by them’ (Siu, 2015). | ||
| Maskaphobia | ‘Apparently when you wear a mask, it sends a signal to the White people, it’s like you’ve got the virus’ (Pang, 2021). | ||
|
| |||
| Experiences of pandemic-related racism among racially minoritized people | External | Abuse (verbal & physical) | ‘I think now people, those who are not Chinese, they see the coronavirus as a further chance to racially abuse the Chinese. It’s like there’s an increase to racial abuse now. They have another weapon to like aim at you. The previous one is like the standard small eyes’ (Pang, 2021). |
| Discrimination in social/public spaces | ‘I was shocked when I saw a standing board in front of a store, which said Chinese and Taiwanese were prohibited to enter for prevention of SARS. That’s a discrimination’ (Zheng et al., 2005). ‘Shops in one community reportedly had signs in their windows telling Mexicans to keep out’ (Schoch-Spana et al., 2010). |
||
| Hypersurveillance/avoidance |
|
||
| Internal | Fear of discrimination | ‘The biggest issue is not the actual virus, but the exclusion, bullying, abuse, and racism. Once you’ve got it, you’ll become scared and lose confidence and hope which will have a longer-term impact’ (Pang, 2021). | |
| Vicarious racism | ‘The Chinese school has a WeChat group where parents talk about things. There was this person whom I know, and her White Dad said don’t be friends with this Chinese girl as he doesn’t want his daughter to get the coronavirus. I feel sad and I’m not friends with this person anymore’ (Pang, 2021). | ||
| Internalized racism | ‘I even did not touch Chinese newspapers in the international students’ center of the University for fear of SARS virus left on the paper by others’ (Zheng et al., 2005). | ||
|
| |||
| Responses to pandemic-related racism among racially minoritized people | Coping strategies | Camaraderie/community support | ‘[The online forum] Subtle Asian Traits is the ‘go to’ arena for airing our grievances and for seeking resonance and support within the East Asian (diaspora) community’ (Abidin and Zeng, 2020). |
| Avoidance/silencing | ‘Take non-confrontational approaches such as quietly enduring the pain or walking away’ (Abidin and Zeng, 2020). | ||
| Problem solving | ‘Local providers reached out to a national [Hispanic] farmworker health organization for assistance in correcting misinformation about migrant and seasonal farmworkers, including the perception that they had higher rates of influenza infection than the larger U.S. population’ (Schoch-Spana et al., 2010). | ||
| Religion/faith |
|
||
|
| |||
| Pandemic-related racism impact on health equity | Structural | Social determinants | ‘Lack of sick leave prevents many from seeking care, because they fear losing their jobs, and clinics may be open only during work hours’ (Schoch-Spana et al., 2010). |
| Health care accessibility |
|
||
| Individual | Mental health outcomes |
|
|
PHOBOGENIC BASIS TO PANDEMIC-RELATED RACISMS
Xenophobia
Several studies (Zheng et al., 2005; Eichelberger, 2007; Schoch-Spana et al., 2010; McCauley et al., 2013; Siu, 2015; Smith-Morris, 2017; Pang, 2021) described xenophobic beliefs around pandemic origins, attributing blame on ‘foreign’ places (China, Mexico, Liberia), which were framed as poor and unhygienic, in comparison to ‘clean’ high-income contexts. Hispanic participants in a US study (McCauley et al., 2013) discussed the subtle stigma they had experienced noting the lack of sensitivity to minorities during disease outbreaks, and questioning unfounded judgments of cleanliness in their home country (Mexico). Associatively, racially minoritized people were perceived as carriers of pandemic diseases (Eichelberger, 2007; Schoch-Spana et al., 2010; McCauley et al., 2013; Siu, 2015, Smith-Morris, 2017; Abidin and Zeng, 2020; Rzymski and Nowicki, 2020; Pang, 2021), regardless of naturalization or long-term residency in the study location. However, three studies highlighted the link between pandemic-related discrimination and immigration status (Liu et al., 2020, Schoch-Spana et al., 2010), with new or recent immigrants being perceived as more of a threat (Eichelberger, 2007).
Sinophobia
Sinophobia (anti-Chinese sentiment) was associated with COVID-19 (Abidin and Zeng, 2020; Cheah et al., 2020; Liu et al., 2020; Rzymski and Nowicki, 2020; Pang, 2021) and SARS (Zheng et al., 2005; Eichelberger, 2007), placing China as the origin, and Chinese people in the study locations as vectors of these diseases. A COVID-19-focused study identified that Chinese American parents (49%, n = 543) and their children (71%, n = 230) agreed on the presence of health-related Sinophobia, including the media’s role in its perpetuation (Cheah et al., 2020). Chinese participants in a UK study (Pang, 2021) expressed that COVID-19 provided an opportunity for people to enact or express underlying Sinophobia. Chinese ‘customs’ and ‘culture’ were framed as dirty and disregarding of public health, which justified discrimination of Chinese students in Japan (Zheng et al., 2005), and intraracial Sinophobia between long-term and recent Chinese immigrants (Eichelberger, 2007), and within broader Asian communities (Person et al., 2004) in the USA during the SARS pandemic.
Negrophobia
Negrophobia (racist sentiment toward people of African descent) was identified primarily in relation to Ebola (Siu, 2015; Smith-Morris, 2017; Pang, 2021); however, one study (Liu et al., 2020) reported non-Hispanic Black participants in the USA as more likely to have persistently experienced COVID-19-associated discrimination. Similar to Sinophobia elsewhere, African immigrants (regardless of their country of origin), who were long-term residents of Hong Kong, were framed as unhygienic vectors of Ebola, which fueled underlying Negrophobic sentiments (Siu, 2015). Non-physical signifiers, such as having an African accent, or communicating they were from an African country (Liberia), resulted in phobogenic assumptions of Ebola infection (Smith-Morris, 2017). African immigrants living in Hong Kong and the USA (Siu, 2015; Smith-Morris, 2017) described how Ebola had invoked interracial and intraracial discrimination from South Asian, Hispanic and African American people in the study locations.
Maskaphobia
Several studies discussed fearful reactions to racially minoritized people wearing masks in the context of COVID-19 (Abidin and Zeng, 2020; Rzymski and Nowicki, 2020; Pang, 2021) and SARS (Eichelberger, 2007). Studies conducted in the UK (Pang, 2021), Poland (Rzymski and Nowicki, 2020) and online (Abidin and Zeng, 2020) highlighted racially minoritized peoples’ perceptions of Western European misconceptions around mask-wearing. Chinese medical students were asked to remove masks to avoid tensions with patients in a hospital setting, and peers in a university setting during the onset of the COVID-19 pandemic (Rzymski and Nowicki, 2020). Asian members of an online forum shared accounts of being avoided, or attacked in response to wearing a mask (Abidin and Zeng, 2020). Participants in a US study were more likely to perceive COVID-19-related discrimination when wearing a mask (Liu et al., 2020).
EXPERIENCES OF PANDEMIC-RELATED RACISMS
Verbal discrimination and physical abuse
Verbal discrimination (Zheng et al., 2005; Schoch-Spana et al., 2010; Siu, 2015; Smith-Morris, 2017; Abidin and Zeng, 2020; Rzymski and Nowicki, 2020; Pang, 2021) and physical abuse (Abidin and Zeng, 2020; Iob et al., 2020; Rzymski and Nowicki, 2020) were identified as prominent experiences of pandemic-related racism. Reports of physical abuse included being physically attacked, ‘beaten up’ (Abidin and Zeng, 2020), spat on and having objects thrown at them (Rzymski and Nowicki, 2020). Supporting these findings are statistics from a US study which found racially minoritized participants (n = 5259) experienced higher proportions of both psychological (12.5%) and physical abuse (4.3%) than their white counterparts (psychological abuse 7.8%, physical abuse 2.8%, n = 39 516) during the COVID-19 pandemic (Iob et al., 2020).
Anti-Asian (discrimination toward people of Asian descent) verbal discrimination was reported in COVID-19 and SARS studies, reflecting the specific racializing of these diseases (Zheng et al., 2005; Abidin and Zeng, 2020; Rzymski and Nowicki, 2020; Pang, 2021); including Chinese participants being told ‘you’re the virus’ (Pang, 2021), being pointed at, or told to keep one’s distance (Rzymski and Nowicki, 2020), and wearing a mask in response to being identified as Chinese (Zheng et al., 2005). Similar types of verbal discrimination were reported by participants of African descent in relation to Ebola, including being asked whether they have the disease (Siu, 2015; Smith-Morris, 2017), or being the recipient of discriminatory comments or racial slurs such as ‘black ghost’ or ‘AIDS carriers’ (Siu, 2015).
Discrimination in public/social spaces
Discrimination in public or social spaces was reported in the majority of identified studies (Zheng et al., 2005; Eichelberger, 2007; Schoch-Spana et al., 2010; Siu, 2015; Smith-Morris, 2017; Abidin and Zeng, 2020; Cheah et al., 2020; Liu et al., 2020; Rzymski and Nowicki, 2020; Yang et al., 2020) and largely experienced in school or work settings (Zheng et al., 2005; Schoch-Spana et al., 2010; Siu, 2015; Smith-Morris, 2017; Rzymski and Nowicki, 2020). In an H1N1 study from the USA (Schoch-Spana et al., 2010), a school denied admission to Mexican students who were asked to quarantine despite having no symptoms. During the Ebola pandemic, African participants in the USA and Hong Kong experienced discrimination at work (Smith-Morris, 2017), or in finding work (Siu, 2015). Hospitals were also identified as public spaces where racism was experienced, including by Chinese medical students in Poland (Rzymski and Nowicki, 2020), African hospital staff in the USA (Smith-Morris, 2017) and African patients in Hong Kong (Siu, 2015). Other places where racist experiences occurred included restaurants, shops and hotels (Zheng et al., 2005; Schoch-Spana et al., 2010; Siu, 2015; Rzymski and Nowicki, 2020). Hispanic participants in a US study (Schoch-Spana et al., 2010) were accused of bringing H1N1 into a grocery store, with some stores reportedly displaying signs ‘telling Mexicans to keep out’. While participants in a SARS-related study were denied entry to hotels or stores for being Chinese (Zheng et al., 2005). COVID-19-related discrimination was most commonly experienced (47%, n = 85) on public transport (Rzymski and Nowicki, 2020), echoing experiences in an earlier SARS-related study in the USA (Eichelberger, 2007).
Anti-Asian racism was prevalent in online spaces (Abidin and Zeng, 2020; Cheah et al., 2020; Liu et al., 2020; Yang et al., 2020), with several US studies reporting the relationship between engagement in social media and experiences of discrimination (Cheah et al., 2020; Liu et al., 2020; Yang et al., 2020). For example, 46% of Chinese American parents (n = 543) and their children (n = 230) experienced direct COVID-19-related racial discrimination online (Cheah et al., 2020).
Hyper-surveillance and avoidance
Hyper-surveillance (heightened scrutiny as a result of being racially minoritized) was a common experience among racially minoritized participants in pandemic-related contexts (Zheng et al., 2005; Eichelberger, 2007; Schoch-Spana et al., 2010; Siu, 2015; Smith-Morris, 2017; Abidin and Zeng, 2020; Cheah et al., 2020; Liu et al., 2020; Rzymski and Nowicki, 2020; Pang, 2021). Media stigmatization was identified as a primary manifestation of hyper-surveillance (Eichelberger, 2007; Schoch-Spana et al., 2010; Smith-Morris, 2017; Cheah et al., 2020; Pang, 2021) with participants from several studies perceiving discriminatory reporting practices (Eichelberger, 2007; Schoch-Spana et al., 2010; Smith-Morris, 2017; Cheah et al., 2020; Pang, 2021). In the USA, media-based stigmatization was perceived in response to COVID-19 (50.4% of parents n = 274, and 56% of youth n = 129) (Cheah et al., 2020), and attributed to racialized places, including health clinics frequented by Hispanic migrant workers (Schoch-Spana et al., 2010), and Chinatown (New York) (Eichelberger, 2007), which were characterized as ‘hot spots’. Hyper-surveillance was experienced by participants in the identified studies as being stared at (Zheng et al., 2005; Eichelberger, 2007; Siu, 2015; Smith-Morris, 2017; Rzymski and Nowicki, 2020), being policed by neighbors about hygiene practices (Siu, 2015) and being physically avoided (Eichelberger, 2007; Siu, 2015; Smith-Morris, 2017; Abidin and Zeng, 2020; Rzymski and Nowicki, 2020; Pang, 2021). Racialized places were also perceived to be avoided, including Chinese schools (COVID-19) (Pang, 2021), shopping malls (Siu, 2015) and community spaces frequented by people of African descent (Ebola) (Smith-Morris, 2017).
Internal experiences
Internal and/or internalized experiences of pandemic-related discrimination were discussed in half of the identified studies (Zheng et al., 2005; Eichelberger, 2007; McCauley et al., 2013; Siu, 2015; Cheah et al., 2020; Liu et al., 2020; Yang et al., 2020; Pang, 2021). Fear of being stigmatized was a common internal experience for racially minoritized participants (Eichelberger, 2007; Siu, 2015; Yang et al., 2020; Pang, 2021). One study showed this fear to extend to worry over being deported among Hispanic participants (McCauley et al., 2013). Often, internal experiences were discussed in relation to previous discrimination as being a risk factor for experiencing pandemic-related discrimination (McCauley et al., 2013; Liu et al., 2020; Yang et al., 2020). Previous discrimination was reported as a strong predictor for COVID-19-related discrimination (Liu et al., 2020), but also led participants to be more concerned about experiencing racism generally (McCauley et al., 2013; Yang et al., 2020).
Vicarious racial discrimination, including hearing about or witnessing other peoples’ racist experiences, was explored in several studies (Zheng et al., 2005; Eichelberger, 2007; Cheah et al., 2020; Pang, 2021). In a US study, one in four parents (n = 543) and youth (n = 230) reported experiencing vicarious racial discrimination frequently (Cheah et al., 2020); and in Japan, 31.7% (n = 161) of Chinese students surveyed had heard of SARS-related discrimination against other Chinese people (Pang, 2021).
In two studies, participants linked being perceived as second-class or poor, to fear of not being able to access care (Pang, 2021), and to the spread of pandemic disease in their home country (Siu, 2015). As a response to phobogenic behavior from others, racially minoritized people reported feeling dirty (Siu, 2015), and hyper-vigilant about presenting as ‘clean’ (Eichelberger, 2007); while others adopted phobogenic behavior, avoiding contact with people, spaces and objects associated with their own cultural group (Zheng et al., 2005).
COPING STRATEGIES
Camaraderie, community support
Camaraderie and community support were explored as strategies for coping with pandemic-related racism (Eichelberger, 2007; Schoch-Spana et al., 2010; McCauley et al., 2013; Abidin and Zeng, 2020; Choi et al., 2020). In an online study, Asian participants shared messages of support, worry and catharsis (Abidin and Zeng, 2020). Resilience and social support was also a protective factor to psychological distress related to COVID-19 (Choi et al., 2020). Grassroots organization among community groups and service providers was also discussed (Eichelberger, 2007; McCauley et al., 2013; Schoch-Spana et al., 2010; Abidin and Zeng, 2020), including the instance of a US community health center organizing a press conference to warn against race-based discrimination during the SARS pandemic (Eichelberger, 2007).
Avoidance, silencing
Race-related impression management was another coping strategy employed by study participants (Eichelberger, 2007; McCauley et al., 2013; Smith-Morris, 2017; Abidin and Zeng, 2020). Specific strategies included choosing to be silent about racisms by ‘quietly enduring the pain’ or ‘walking away’ (Abidin and Zeng, 2020), or in the case of another participant, choosing not to speak to avoid their accent marking them as a danger (Smith-Morris, 2017). To abate the stress of not having reliable support and information, participants in one study avoided news coverage of the H1N1 pandemic (McCauley et al., 2013).
Problem solving
Problem solving among racially minoritized peoples emerged as a key coping strategy in several studies (Eichelberger, 2007; Schoch-Spana et al., 2010; Abidin and Zeng, 2020; Pang, 2021). In response to heightened prejudice, study participants employed various solutions including learning self-defense, supporting local Asian businesses (Abidin and Zeng, 2020), working with local providers to correct misinformation that supported discrimination (Schoch-Spana et al., 2010) and introducing routines to address concerns of their children’s health (Pang, 2021).
Religion/faith
Two studies discussed the use of religion among participants as a means to understand and cope with the effects of pandemics (McCauley et al., 2013; Siu, 2015). Belief in God made Hispanic participants feel safe during H1N1 (McCauley et al., 2013). Conversely for an African participant, their understanding of Ebola was that it was a punishment from God (Siu, 2015).
IMPACT ON HEALTH EQUITY
Socioeconomic factors
Racially minoritized participants in the identified studies were more likely to have faced unemployment (Baptist et al., 2020), or fear of unemployment (Schoch-Spana et al., 2010) due to the related pandemics, which impacted care-seeking behavior (Schoch-Spana et al., 2010). They were also more likely to be from low-income households (Baptist et al., 2020), experience language barriers (Choi et al., 2020) and reside in a community with a higher number of pandemic disease cases (Baptist et al., 2020).
Mental health impact
Half of all identified studies discussed the mental health impact of pandemic-related racisms among racially minoritized people, including emotional stress (Abidin and Zeng, 2020), anxiety (Zheng et al., 2005; McCauley et al., 2013; Cheah et al., 2020; Pang, 2021) and depressive symptoms (Zheng et al., 2005; Cheah et al., 2020). Experience of (Cheah et al., 2020) and worry about discrimination were found to be associated with psychological distress and poorer subjective wellbeing (Choi et al., 2020; Yang et al., 2020). Half of Korean immigrants (49%, n = 790) in a US study (Choi et al., 2020) reported high levels of psychological distress of which everyday discrimination and a perceived increase in anti-Asian racism were predicting factors. Where parents were the recipients of pandemic-related racism, there was an associated impact on their child’s mental health (Cheah et al., 2020). A UK study reported a higher frequency of abuse, self-harm and thoughts of suicide/self-harm among racially minoritized groups during COVID-19, when compared with white counterparts (Iob et al., 2020).
Health care accessibility
The impact of pandemic-related discrimination on health equity was largely discussed in relation to accessing health treatments (Baptist et al., 2020), services (Person et al., 2004; Zheng et al., 2005; Schoch-Spana et al., 2010; Siu, 2015; Baptist et al., 2020; Rzymski and Nowicki, 2020; Pang, 2021) and information (Person et al., 2004; McCauley et al., 2013; Siu, 2015). When compared with white counterparts, racially minoritized participants were more likely to experience difficulties accessing regular medication during COVID-19, and/or lose their health insurance due to COVID-19 (Baptist et al., 2020). Chinese participants detailed reports of not being able to access public health services despite testing positive for COVID-19 (Pang, 2021). Earlier studies focused on SARS (Person et al., 2004; Zheng et al., 2005) and H1N1 (Schoch-Spana et al., 2010) identified similar factors among Asian and Mexican participants, who when experiencing flu-like symptoms were less likely to be referred or to seek out care in fear of being stigmatized. Other studies confirmed these fears, whereby African (Siu, 2015) and Chinese (Rzymski and Nowicki, 2020) patients experienced discrimination within health spaces from clinical staff and fellow patients.
DISCUSSION
The purpose of this review was to identify and describe pandemic-related experiences or perceptions of discrimination among non-Indigenous racially minoritized groups in high-income contexts, and its impact on health outcomes or access to health services using critical race theory to guide our analytic approach. Critical race theory has had limited application in public health discourse, emphasizing the need to center race (a common epidemiological variable) in public health research (Yam et al., 2021), and better understand the racial determinants of health and their intersection with gender. Our findings present a clear link between pandemics in high-income contexts, and fear-based (phobogenic) stereotyping of racially minoritized people, which results in racialized discrimination, violence and health inequity. The ideology of race and its implications on social locations and bodies are historically constructed, and continue to shape relations between individuals, collectives and governments. Racisms persist in non-pandemic periods, and are a key mechanism to the reproduction of ill health (Paradies et al., 2015) and social marginalization among racially minoritized groups (Fanon, 1963). Understanding how and why phobogenic responses to pandemics occur is crucial to addressing the discrimination experienced by racially minoritized peoples. Fanon’s psychoanalysis of the internal and external processes of racialization, presents the idea that beneath the physical surface of racialized bodies, is a non-physical schema that comprises the stereotypes, mythologies and pathologies that underpin socially constructed classifications of difference (Fanon, 1967). During times of pandemic, widespread fear evokes the ‘other’ (Husserl, 2012) and becomes an assertion of domination (Fanon, 1963), whereby existing racial schemas lend justification to violence and discrimination.
Evidence from our review show that different pandemic diseases are socially associated with racially minoritized groups, resulting in blame and stigmatization of people who identify, or are identified, as part of that group. Broadly, this included Asian (COVID-19, SARS), African (Ebola) and Hispanic (H1N1) peoples in various high-income contexts. The racialization of the pandemic diseases discussed provides further evidence of the way social classifications of difference are biologized, despite having no material genesis (Davis, 2017). Through this redefinition, the unique combination of pandemic disease and existing racial schemas provide a mechanism by which racially minoritized groups are subject to increased health-related risk factors, resulting in higher instances of physical and verbal abuse, stress, anxiety and depression. Our results therefore suggest that through the racialization of pandemic disease, whiteness (or association with the dominant culture) becomes a defining feature of humanness (Montag, 1997), whereby its lack emerges as a physical marker of pandemic-related risk. The biologizing of social difference shows the category of ‘human’ is not neutral, but a normative category governing access to privileges, such as health care, and producing the other as a passive object (Braidotti, 2020). The re/production of racial othering during a pandemic is therefore also productive of whiteness, which is framed as pure and at risk of infection by an outside force (Sithole, 2016) (whether the disease, the racially minoritized or an indistinguishable mix of the two).
Fear of stigmatization and distrust of health systems and governments (Pang, 2021), among racially minoritized groups (Weiss et al., 2006), is also heightened during pandemic periods, solidifying existing barriers to health care, and subsequently reinforcing existing health inequities. Expressions and experiences of pandemic-related discrimination are reflective of existing tensions between racially minoritized peoples and dominant cultural values and structures, which can and do result in exclusion from health information, care and treatments (Yashadhana et al., 2020). It is clear that racially minoritized people have existing health and coping strategies that support wellness during periods of pandemic (Eichelberger, 2007; Schoch-Spana et al., 2010; McCauley et al., 2013; Abidin and Zeng, 2020; Choi et al., 2020; Pang, 2021). While some of these strategies provided catharsis, and strengthened support systems and networks, other strategies including avoidance and silencing may reinforce negative stereotypes, and contribute to increased isolation and mental health issues, further perpetuating or failing to address racial discrimination. Religious beliefs served as both a system of support, and a psychological justification for the contraction of pandemic diseases, highlighting the need to tackle biomedical misinformation among some racially minoritized groups. These strategies blanket the limitations of public health care services to provide culturally responsive and inclusive health care to all. The role of health professionals and service providers are key to addressing racism in pandemic and non-pandemic times, whereby the provision of cultural responsivity training may provide part of the solution. While cultural responsivity training can raise awareness of racisms, individual approaches also need to be at the forefront. Practices such as critical reflection, critical reflexivity and active listening (Jayatilleke and Mackie, 2013), and considering these as a lifelong process (Facione and Facione, 2013), will support health professionals in raising their own awareness to the presence or perpetuation of racism. In turn, this may provide awareness on their own worldviews and influences to care, highlighting how racisms manifest in times of pandemic. This provides an opportunity for health professionals to adapt their practices and direct their attention to the needs of their client, regardless of racial or cultural background (Wilson et al., 2018). Considering the context of the COVID-19 pandemic, and the persistent racial tensions that exist in high-income countries such as the USA, the timing is apt to set new standards in public health. Past US Public Health Frameworks for example, (1.0, 2.0) failed to adequately recognize the social, environmental and economic determinants of health. While Public Health Framework 3.0 does (DeSalvo et al., 2016), it falls short of addressing structural racism as a barrier to public health both within and outside pandemic contexts. Deconstructing the systemic factors that link race to health requires us to question the ontological and epistemological approach to global healthcare (Affun-Adegbulu and Adegbulu, 2020). Only when we start to question healthcare from beyond the lens of Western biomedical perspectives, will the absolute potential of approaches to decolonize public health be revealed. This requires a scrutinizing and rethinking of dominant public health epistemologies, and the opportunity for non-dominant voices to be truly heard.
Policy praxis, as representative of dominant cultural values and the distribution of power, must be examined as key to the causative pathway leading to inequitable health outcomes (Harris et al., 2020). Doing so, requires platforming racism as a public health problem (Devakumar et al., 2020), recognizing its increased impact in pandemic contexts, and ensuring adequate representation of racially minoritized groups is present in policy, planning and implementation. As Morrison (Morrison, 1994) states, the act of enforcing racelessness in public discourse is itself a racial act. Acknowledging race as a public health problem also reinforces the fact that health is created largely outside the health sector, and real change requires intersectoral engagement and action (de Leeuw, 2017). With the absence of an international anti-racism strategy, a unified response requires unified public health messaging. This may be inclusive of National Anti-Racism strategies in high-income countries, which solidify understanding and commitment to the United Nations Declaration of Human Rights (United Nations General Assembly, 1948).
Inclusion and consultation of racially minoritized groups in the policy process provides an opportunity to understand how existing coping strategies and wellness processes have been applied during times of pandemic, inclusive of how social resilience amongst racially minoritized people contributes to positive shifts in health outcomes. Finally, our review identified the need for further research in the area of pandemic-related racisms, as relatively, only a small number of studies were identified globally of which a large majority were situated in the USA. For example, pandemic-related discrimination in contexts where there are considerable migrant populations such as Australia, Canada or New Zealand is needed. Furthermore, very limited information on the gendered aspects of pandemic-related racisms were reported in the included articles, pointing to the need for further research that investigates these complexities.
LIMITATIONS
This systematic review was limited to peer-review articles, and therefore may have missed potentially relevant information in gray literature articles, books and theses. This review did not include papers investigating pandemic-related racisms experienced by Indigenous peoples, or papers related to AIDS/HIV, as the authors agreed these topics require separate reviews due to their unique complexities.
CONCLUSION
In conclusion, this review has made a novel contribution to the existing literature, outlining important implications on how pandemic-related racism is expressed and experienced, and how this intersects with social determinants and health equity. Our results reinforce the need to frame racism as a public health problem, and for health policy and practice to be responsive to the differing needs and experiences of all peoples. The latter requires individual health practitioner’s awareness of the pervasive presence of racisms during times of pandemic.
FUNDING
Funding to conduct this study was provided by an internal grant provided by Charles Sturt University.
REFERENCES
- Abidin C., Zeng J. (2020) Feeling Asian together: coping with #COVIDRacism on subtle Asian traits. Social Media + Society, 6, 2056305120948223.10.1177/2056305120948223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Affun-Adegbulu C., Adegbulu O. (2020) Decolonising global (public) health: from western universalism to global pluriversalities. BMJ Global Health, 5, e002947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baptist A. P., Lowe D., Sarsour N., Jaffee H., Eftekhari S., Carpenter L. M.. et al. (2020) Asthma disparities during the COVID-19 pandemic: a survey of patients and physicians. The Journal of Allergy and Clinical Immunology: In Practice, 8, 3371–3377.e1. 10.1016/j.jaip.2020.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger M., Sarnyai Z. (2015) “More than skin deep”: stress neurobiology and mental health consequences of racial discrimination. Stress (Amsterdam, Netherlands), 18, 1–10. [DOI] [PubMed] [Google Scholar]
- Braidotti R. (2020) “We” are in this together, but we are not one and the same. Journal of Bioethical Inquiry, 17, 465–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheah C. S. L., Wang C., Ren H., Zong X., Su Cho H., Xue X. (2020) COVID-19 racism and mental health in Chinese American families. Pediatrics, 146, e2020021816. [DOI] [PubMed] [Google Scholar]
- Choi S., Hong J. Y., Kim Y. J., Park H. (2020) Predicting psychological distress amid the COVID-19 pandemic by machine learning: discrimination and coping mechanisms of Korean immigrants in the U.S. International Journal of Environmental Research and Public Health, 17, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis N. (2017) Material culture: epigenetics and the molecularisation of the social. In Kirby V. (ed), What If Culture Was Nature All Along? Edinburgh University Press, Edinburgh, UK, pp. 110–133. [Google Scholar]
- de Leeuw E. (2017) Engagement of sectors other than health in integrated health governance, policy, and action. Annual Review of Public Health, 38, 329–349. [DOI] [PubMed] [Google Scholar]
- DeSalvo K. B., O’Carroll P. W., Koo D., Auerbach J. M., Monroe J. A. (2016) Public health 3.0: time for an upgrade. American Journal of Public Health, 106, 621–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devakumar D., Selvarajah S., Shannon G., Muraya K., Lasoye S., Corona S.. et al. (2020) Racism, the Public Health Crisis We Can No Longer Ignore. Lancet, London, UK. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eichelberger L. (2007) SARS and New York’s Chinatown: the politics of risk and blame during an epidemic of fear. Social Science & Medicine (1982), 65, 1284–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Facione P. A., Facione N. C. (2013) Critical thinking for life: valuing, measuring, and training critical thinking in all its forms. Inquiry: Critical Thinking across the Disciplines, 28, 5–25. [Google Scholar]
- Fanon F. (1967) Black Skin, White Masks. Grove Press, New York, NY. [Google Scholar]
- Fanon F. (1963) The Wretched of the Earth. Grove Press, New York, NY. [Google Scholar]
- Garner S. (2017) Chapter 1: the idea of ‘Race’ and the practice of racisms, In Racisms: An Introduction. Sage, UK. [Google Scholar]
- Glaser B. G., Strauss A. L. (2009) The Discovery of Grounded Theory: Strategies for Qualitative Research. Routledge, London, UK. [Google Scholar]
- Hall S. (1996) Race: The Floating Signifier. Media Education Foundation, Northampton MA, USA. [Google Scholar]
- Harris P., Baum F., Friel S., Mackean T., Schram A., Townsend B. (2020) A glossary of theories for understanding power and policy for health equity. Journal of Epidemiology and Community Health, 74, 548–552. [DOI] [PubMed] [Google Scholar]
- Hook D. (2004) Fanon and the psychoanalysis of racism, London: LSE Research Online. Available at: http://eprints.lse.ac.uk/2567.
- Husserl E. (2012) Ideas: General Introduction to Pure Phenomenology. Routledge, New York, USA. [Google Scholar]
- Iob E., Steptoe A., Fancourt D. (2020) Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. The British Journal of Psychiatry: The Journal of Mental Science, 217, 543–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayatilleke N., Mackie A. (2013) Reflection as part of continuous professional development for public health professionals: a literature review. Journal of Public Health (Oxford, England), 35, 308–312. [DOI] [PubMed] [Google Scholar]
- Keil R., Ali H. (2006) Multiculturalism, racism and infectious disease in the global city: the experience of the 2003 SARS outbreak in Toronto. Topia: Canadian Journal of Cultural Studies, 16, 23–49. [Google Scholar]
- Kelly H. (2011) The classical definition of a pandemic is not elusive. Bulletin of the World Health Organization, 89, 540–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kmet L., Lee R. C., Cook L. S. (2004) Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields. Institute of Health Economics, Alberta, Canada. [Google Scholar]
- Larsson P. (2020) Anti-Asian racism during coronavirus: how the language of disease produces hate and violence. The Conversation 31 (2020). [Google Scholar]
- Leonardo Z. (2002) The souls of white folk: critical pedagogy, whiteness studies, and globalization discourse. Race Ethnicity and Education, 5, 29–50. [Google Scholar]
- Leung C. (2008) The yellow peril revisited: the impact of SARS on Chinese and Southeast Asian communities. Resources for Feminist Research, 33, 135. [Google Scholar]
- Liu Y., Finch B. K., Brenneke S. G., Thomas K., Le P. D. (2020) Perceived discrimination and mental distress amid the COVID-19 pandemic: evidence from the understanding America study. American Journal of Preventive Medicine, 59, 481–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley M., Minsky S., Viswanath K. (2013) The H1N1 pandemic: media frames, stigmatization and coping. BMC Public Health, 13, 1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKnight-Eily L. R., Okoro C. A., Strine T. W., Verlenden J., Hollis N. D., Njai R.. et al. (2021) Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic—United States, April and May 2020. MMWR. Morbidity and Mortality Weekly Report, 70, 162–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milner A., Jumbe S. (2020) Using the right words to address racial disparities in COVID-19. The Lancet. Public Health, 5, e419–e420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G. and PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine, 6, e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montag W. (1997) The universalization of whiteness: racism and enlightenment, in Hill, M. (Ed.) Whiteness: A Critical Reader, 281–293. [Google Scholar]
- Morrison T. (1994) Playing in the Dark: Whiteness and the Literary Imagination. Vintage New York, New York, NY. [Google Scholar]
- Pang B. N. (2021) Beyond hypervisibility and fear: British Chinese Communities’ leisure and health-related experiences in the time of coronavirus. Leisure Sciences, 43, 111–117. 10.1080/01490400.2020.1773991. [Google Scholar]
- Paradies Y., Ben J., Denson N., Elias A., Priest N., Pieterse A.. et al. (2015) Racism as a determinant of health: a systematic review and meta-analysis. PLoS One, 10, e0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Person B., Sy F., Holton K., Govert B., Liang A., Garza B.. et al.; National Center for Inectious Diseases/SARS Community Outreach Team. (2004) Fear and stigma: the epidemic within the SARS outbreak. Emerging Infectious Diseases, 10, 358–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porta M. (2014) A Dictionary of Epidemiology. Oxford University Press, Oxford, UK. [Google Scholar]
- Rzymski P., Nowicki M. (2020) COVID-19-related prejudice toward Asian medical students: a consequence of SARS-CoV-2 fears in Poland. Journal of Infection and Public Health, 13, 873–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoch-Spana M., Bouri N., Rambhia K. J., Norwood A. (2010) Stigma, health disparities, and the 2009 H1N1 influenza pandemic: how to protect Latino farmworkers in future health emergencies. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science, 8, 243–254. [DOI] [PubMed] [Google Scholar]
- Shimizu K. (2020) 2019-nCoV, fake news, and racism. The Lancet, 395, 685–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sithole T. (2016) The concept of the black subject in Fanon. Journal of Black Studies, 47, 24–40. [Google Scholar]
- Siu J. Y. M. (2015) Influence of social experiences in shaping perceptions of the Ebola virus among African residents of Hong Kong during the 2014 outbreak: a qualitative study. International Journal for Equity in Health, 14, 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith-Morris C. (2017) Epidemiological placism in public health emergencies: Ebola in two Dallas neighborhoods. Social Science & Medicine (1982), 179, 106–114. [DOI] [PubMed] [Google Scholar]
- Truman B. I., Tinker T., Vaughan E., Kapella B. K., Brenden M., Woznica C. V.. et al. (2009) Pandemic influenza preparedness and response among immigrants and refugees. American Journal of Public Health, 99 Suppl 2, S278–S286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations General Assembly. (1948) Universal declaration of human rights. UN General Assembly, 302, 14–25. [Google Scholar]
- Weiss M. G., Ramakrishna J., Somma D. (2006) Health-related stigma: rethinking concepts and interventions. Psychology, Health & Medicine, 11, 277–287. [DOI] [PubMed] [Google Scholar]
- Wen J., Aston J., Liu X., Ying T. (2020) Effects of misleading media coverage on public health crisis: a case of the 2019 novel coronavirus outbreak in China. Anatolia, 31, 331–336. [Google Scholar]
- Wilson D., Heaslip V., Jackson D. (2018) Improving equity and cultural responsiveness with marginalised communities: understanding competing worldviews. Journal of Clinical Nursing, 27, 3810–3819. [DOI] [PubMed] [Google Scholar]
- Wong G., Greenhalgh T., Westhorp G., Buckingham J., Pawson R. (2013) RAMESES publication standards: meta-narrative reviews. Journal of Advanced Nursing, 69, 987–1004. 10.1111/jan.12092. [DOI] [PubMed] [Google Scholar]
- Yam E. A., Silva M., Ranganathan M., White J., Hope T. M., Ford C. L. (2021) Time to take critical race theory seriously: moving beyond a colour-blind gender lens in global health. The Lancet. Global Health, 9, e389–e390. [DOI] [PubMed] [Google Scholar]
- Yang C. C., Tsai J. Y., Pan S. Y. (2020) Discrimination and well-being among Asians/Asian Americans during COVID-19: the role of social media. Cyberpsychology, Behavior and Social Networking, 23, 865–870. 10.1089/cyber.2020.0394. [DOI] [PubMed] [Google Scholar]
- Yashadhana A., Fields T., Blitner G., Stanley R., Zwi A. B. (2020) Trust, culture and communication: determinants of eye health and care among Indigenous people with diabetes in Australia. BMJ Global Health, 5, e001999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng G., Jimba M., Wakai S. (2005) Exploratory study on psychosocial impact of the severe acute respiratory syndrome (SARS) outbreak on Chinese students living in Japan. Asia-Pacific Journal of Public Health, 17, 124–129. [DOI] [PubMed] [Google Scholar]