Approximately 10% of cataract patients have a tilt of 7 degrees or greater and decentration of 0.4 mm or greater. Axial length, front curvature radius, lens thickness, and age correlate with tilt and decentration.
Purpose:
To investigate the characteristics and factors associated with crystalline lens tilt and decentration measured by CASIA2 anterior segment optical coherence tomography.
Setting:
Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou, China.
Design:
Cross-sectional study.
Methods:
1097 eyes of 1097 patients who planned to undergo cataract surgery were enrolled. All patients underwent a general ophthalmologic examination. Lens thickness (LT), front curvature radius (FCR), back curvature radius, lens equator diameter (LED), tilt, and decentration of preoperative crystalline lenses were measured by CASIA2. Univariate and multivariate regression analyses were performed to evaluate the relationships between the tilt and decentration of crystalline lens with related factors.
Results:
The natural crystalline lenses showed a mean tilt of 5.16 degrees toward the inferotemporal direction and a mean decentration of 0.22 mm toward the temporal direction. Of the total 1097 eyes, 119 eyes (10.85%) had a tilt greater than 7 degrees, and 89 eyes (8.11%) had a decentration more than 0.4 mm. Multivariate regression analysis showed that larger decentration, thicker LT, shorter axial length (AL), and FCR were associated with greater lens tilt (P < .001, P = .007, P = .006, and P = .003, respectively). In addition, greater tilt, older and thinner LT were correlated with larger decentration (all P < .001).
Conclusions:
Preoperative crystalline lens had a certain degree of tilt and decentration in age-related cataract. The greater tilt of the crystalline lens was, the larger decentration of it was. In addition, AL, FCR, LT, and age also correlated with tilt and decentration.
Tilt and decentration of the natural crystalline lens affect not only optical quality of the foveal image but also intraocular lens (IOL) position. It is well known that the misalignment of IOL is an important risk factor for the deterioration of visual quality after cataract surgery.1–3 Because of the biomechanical interaction between IOL and the capsular bag after cataract surgery, it is reasonable to hypothesize that IOL position is significantly affected by crystalline lens geometry and the position of the capsular bag.4 In addition, several studies have demonstrated that the magnitude and direction of tilt of postoperative IOLs were strongly correlated with the tilt of preoperative crystalline lens.5,6 Therefore, the tilt and decentration of crystalline lens can be used to predict postoperative IOL position.5 However, few data are available regarding the distributions of crystalline lens biometry in age-related cataract eyes and about their correlations.
Several devices have already been developed to measure the tilt and decentration of the natural crystalline lens in human eyes, such as Scheimpflug photography, Purkinje images, MRI 3D image reconstruction, and anterior segment optical coherence tomography (AS-OCT).7–9 However, these devices were often complicated to operate and required combination with image processing software and other measurement methods. AS-OCT is a popular method for measuring anterior segment parameters of the eye at present, such as lens geometry or anterior chamber angle. Nevertheless, previous OCT including CASIA1 (Tomey GmbH) could not clearly image the posterior surface and measure the tilt and decentration of crystalline lens automatically. As a result, these methods were difficult to use in clinical practice. CASIA2 (Tomey GmbH) is a new second-generation AS-OCT with faster scanning speed, deeper scanning depth, and higher resolution, allowing the quantification of parameters related to crystalline lens geometry, including lens front and back curvature radius and lens equator diameter. In particular, it is able to automatically measure tilt and decentration of crystalline lens and IOLs used the corneal topographic axis as a reference with high repeatability.10,11
In this study, we aimed to describe the distribution of natural crystalline lens tilt and decentration in a large sample of age-related cataract using CASIA2 and then analyzed their characteristics and identified the systemic and ocular factors associated with them.
METHODS
Study Population
This was a prospective, single-center, cross-sectional study that included 1097 eyes of 1097 patients with age-related cataract who were going to undergo phacoemulsification and IOL implantation at Zhongshan Ophthalmic Center (Guangzhou, China) from August 2019 to June 2020. Inclusion criteria were an age-related cataract including nuclear, cortical, and subcapsular, age 50 years or older, axial length of 26 mm or less, no previous intraocular surgeries or laser treatments, no history of ocular diseases and ocular trauma, and no history of corticoid use. If both eyes were ready for surgery and met the inclusion criteria, the most recently operated eye for analysis was selected. Ethics committee approval was obtained from Zhongshan Ophthalmic Center (Guangzhou, China) Institutional Review Board, and all study procedures adhered to the tenets of the Declaration of Helsinki. All participants were fully informed before examinations and signed a written informed consent form.
Study Procedures
All participants underwent a complete ophthalmic examination in the following order: visual acuity and refraction, slitlamp biomicroscopy, analysis by IOLMaster, lens opacity grading, and AS-OCT imaging. The data of age, sex, and medical history were obtained by inquiring general anamnesis of each patient. Axial length (AL) was measured by IOLMaster 700 (Carl Zeiss Meditec AG) in a dark room. For cataract opacity grading and AS-OCT imaging, tropicamide and phenylephrine eyedrops were administered every 5 minutes for 3 times to dilate the pupil 30 minutes before the examinations were taken. Nuclear, cortical, and subcapsular posterior opacity were graded by 2 ophthalmologists (X.Y.-C., X.X.-G.) according to Lens Opacities Classification System III.
AS-OCT Imaging
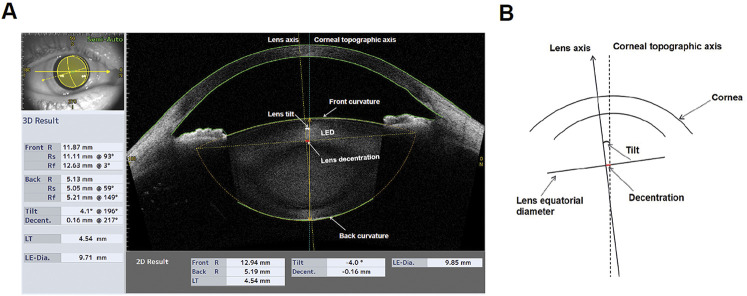
All subjects underwent mydriatic AS-OCT imaging of both eyes before cataract phacoemulsification and IOL implantation surgery using CASIA2 Two consecutive scans were performed using Corneal Topography and Lens Biometry modes. For Lens Biometry mode, CASIA2 produced 3D OCT images by generating 16 distinct AS-OCT images from 16 different angles of crystalline lens (0- to 180-degree, 11- to 191-degree, 23- to 203-degree, 4- to 214-degree, 45- to 225-degree, 56- to 236-degree, 68- to 248-degree, 79- to 259-degree, 90- to 270-degree, 101- to 281-degree, 113- to 293-degree, 124- to 304-degree, 135- to 315-degree, 146- to 326-degree, 158- to 338-degree, and 169- to 349-degree meridians). Six parameters about crystalline lens geometry, including lens thickness (LT), front curvature radius (FCR), back curvature radius (BCR), tilt, decentration, and lens equator diameter (LED), were quantitatively providing from the built-in software (v. SS2000). The anterior chamber depth and the anterior chamber width describing the anterior chamber were also obtained. An example of 3D results of anterior chamber and crystalline lens obtained from CASIA2 and the diagram descripting the definitions of tilt and decentration are shown in Figure 1.
Figure 1.
The measurements of anterior segment and crystalline lens tilt and decentration using CASIA2. A: The representative image showing the 3D result of a crystalline lens. The axis of the crystalline lens (yellow dotted line) and the corneal topographic axis (blue dotted line) were automatically generated by the built-in software. B: The diagram showing the definitions of the tilt and decentration of crystalline lens. The corneal topographic axis is a reference line connecting the fixation point in the topographer to the vertex normal on the cornea. Tilt is the angle of lens axis against the corneal topographic axis, and decentration is the vertical distance from the center of lens equatorial diameter to the corneal topographic axis. Back R = radius of curvature for the lens back surface; Decent. = decentration; Front R = front radius of curvature for the lens front surface; LE-Dia. = lens equatorial diameter; LT = lens thickness; R = radius of curvature; Rs = steep radius of curvature; Rf = flat radius of curvature
Statistical Analysis
Statistical analysis was performed using StataSE15 software (v. 15.0; Stata Corp LP). A P value less than 0.05 was considered statistically significant. All continuous variables were expressed as mean ± SD, and categorical variables were expressed as counts and percentages. One-way analysis of variance was performed to assess the differences in the tilt and decentration between different age, AL, and cataract types groups. Univariate and multivariate regression analysis were performed to determine the correlations of tilt and decentration of crystalline lens with related factors. To avoid multicollinearity, LED and BCR were not included in the multivariate regression analysis.
RESULTS
Patients
A total of 1097 patients (1097 eyes) were enrolled in this study. The mean patient age was 69.00 ± 8.34 years, and 46.95% (515) of the participants was men. Six hundred seventy-nine patients (61.90%) had nuclear cataract, 301 patients (27.44%) cortical cataract, and 117 patients (10.66%) subcapsular posterior cataract. The mean AL was 23.53 ± 0.91 mm, and the mean LT was 4.56 ± 0.45 mm. The basic characteristics of patients are summarized in Table 1.
Table 1.
Characteristics of Enrolled Participants.
| Characteristic | Value |
| Patients, n | 1097 |
| Age (y), mean (SD) | 69.00 (8.34) |
| Male sex, n (%) | 515 (46.95) |
| Diabetes, n (%) | 201 (18.32) |
| Hypertension, n (%) | 406 (37.01) |
| Right eye, n (%) | 650 (59.25) |
| Nuclear opacity grading score (LOCS III), mean (SD) | 3.79 (1.37) |
| Cortical opacity grading score (LOCS III), mean (SD) | 2.89 (1.33) |
| Anterior chamber depth (mm), mean (SD) | 2.72 (0.43) |
| Lens thickness (mm), mean (SD) | 4.56 (0.45) |
| Axial length (mm), mean (SD) | 23.53 (0.91) |
| Front curvature radius (mm), mean (SD) | 9.73 (1.36) |
| Back curvature radius (mm), mean (SD) | 5.49 (0.70) |
| Lens equator diameter (mm), mean (SD) | 9.81 (0.83) |
| Anterior chamber width (mm), mean (SD) | 11.48 (0.46) |
| Cataract types | |
| Age-related nuclear cataract | 679 (61.90) |
| Age-related cortical cataract | 301 (27.44) |
| Subcapsular posterior cataract | 117 (10.66) |
Distribution of Crystalline Lens Tilt and Decentration
The distributions of crystalline lens tilt and decentration are summarized in Table 2 and Figure 2. As illustrated in Figure 2, crystalline lenses tilted mainly toward the inferotemporal direction and decentered toward the temporal side in both eyes.
Table 2.
Distribution of the Tilt and Decentration.
| Crystalline lens tilt | Crystalline lens decentration | ||
| Mean (°) (SD) | 5.16 ± 1.65 | Mean (mm) (SD) | 0.22 ± 0.13 |
| <5°, n (%) | 510 (46.49) | <0.20 mm, n (%) | 560 (51.05) |
| 5-7°, n (%) | 468 (42.66) | 0.2, 0.4 mm, n (%) | 448 (40.84) |
| ≥7°, n (%) | 119 (10.85) | ≥0.4 mm, n (%) | 89 (8.11) |
Figure 2.
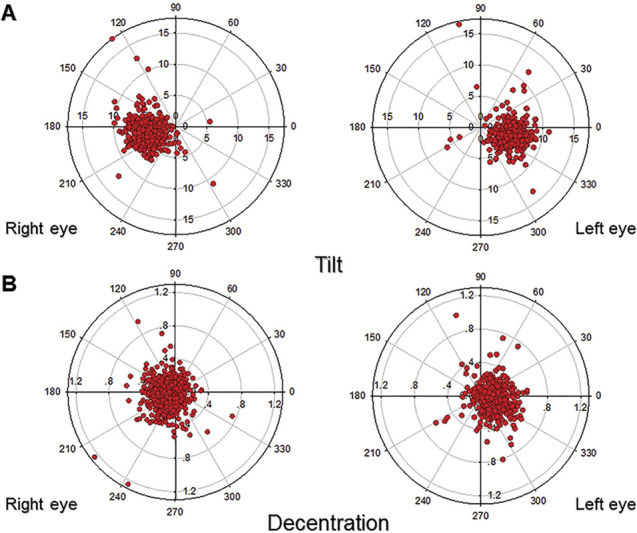
The distributions of tilt and decentration of the crystalline lenses in both eyes. A: Coordinate graphics showing the orientations and values of crystalline lenses tilt in the both eyes. B: Coordinate graphics showing the orientations and values of crystalline lens decentration in the both eyes.
Table 3 summarizes the increase in decentration of crystalline lenses with age. The decentration was obviously larger in patients aged 70 years or older (P = .003). Although no statistical significance in tilt of crystalline lenses with different ages was found, it was slightly larger in patients aged 70 years or older. In addition, there were statistically significant differences in the tilt and decentration between the groups with different AL. Longer AL had a lower tilt and decentration (P < .001 and P = .004, respectively). Moreover, the decentration increased with the tilt. The greater the tilt of the crystalline lens was, the larger the decentration of it was and vice versa (P < .001 and P < .001, respectively). However, there was no statistical significance difference in tilt and decentration of crystalline lenses with different types of cataract (P = .363 and P = .041, respectively).
Table 3.
Tilt and Decentration According to Age, AL, and Cataract Type.
| Groups | Patients, n (%) | Tilt (°), mean (SD) | Decentra (mm), mean (SD) |
| Age (y) | |||
| 50-59 | 143 (13.04) | 5.06 (1.72) | 0.20 (0.14) |
| 60-69 | 447 (40.75) | 5.08 (1.47) | 0.20 (0.11) |
| 70-79 | 372 (33.91) | 5.17 (1.82) | 0.23 (0.15) |
| ≥80 | 135 (12.31) | 5.47 (1.66) | 0.24 (0.13) |
| P value | .089 | .003 | |
| AL (mm) | |||
| <22 | 45 (4.10) | 5.71 (1.64) | 0.25 (0.19) |
| 22-24 | 754 (68.73) | 5.31 (1.58) | 0.22 (0.13) |
| 24-26 | 298 (27.16) | 4.69 (1.74) | 0.20 (0.12) |
| P value | <.001 | .004 | |
| LT (°) | |||
| <5 | 510 (46.49) | — | 0.17 (0.10) |
| 5-7 | 468 (42.66) | — | 0.23 (0.10) |
| ≥7 | 119 (10.85) | — | 0.38 (0.20) |
| P value | — | <.001 | |
| LD (mm) | |||
| <0.20 | 560 (51.05) | 4.48 (1.21) | — |
| 0.2-0.4 | 448 (40.84) | 5.60 (1.35) | — |
| ≥0.4 | 89 (8.11) | 7.14 (2.73) | — |
| P value | <.001 | — | |
| Cataract type | |||
| Cortical | 301 (27.44) | 5.04 (1.51) | 0.20 (0.12) |
| Nuclear | 679 (61.90) | 5.20 (1.69) | 0.22 (0.13) |
| SP | 117 (10.66) | 5.21 (1.77) | 0.22 (0.15) |
| P value | .363 | .041 |
AL = axial length; LD = lens decentration; LT = lens tilt; SP = subcapsular posterior
Association Between the Tilt and Decentration of Crystalline Lens With General and Ocular Parameters
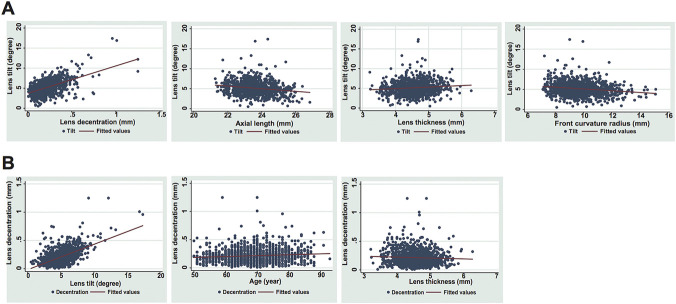
The results of univariate and multivariate analysis of regression models for crystalline lens tilt and decentration are summarized in Table 4. In the multivariate analysis for crystalline lens tilt, larger degree tilt was positively associated with larger decentration and thicker lens (P < .001, P = .007), whereas it was negatively associated with longer AL (P = .006) and larger FCR (P = .003) (Figure 3, A). For every 1 mm increase in lens decentration, tilt increased by 6.869 degrees, and for 1 mm increase in axial length, tilt decreased by 0.328 degrees. However, age, sex, and the presence of diabetes were not significantly associated with crystalline lens tilt. These findings indicated that larger decentration, thicker lens, and shorter AL and FCR are strongly correlated with greater crystalline lens tilt.
Table 4.
Univariate and Multivariate Analyses of Associations Between the Tilt and Decentration and Related Factors.
| Factor | Crystalline lens tilt | Crystalline lens decentration | ||||||
| Univariate analysis | Multivariate analysis | Univariate analysis | Multivariate analysis | |||||
| b (95% CI) | P value | b (95% CI) | P value | b (95% CI) | P value | b (95% CI) | P value | |
| Age (y) | 0.015 (0.003, 0.027) | .013 | 0.000 (−0.010, 0.010) | .987 | 0.002 (0.001, 0.003) | .001 | 0.001 (0.001, 0.002) | .001 |
| Sex, F | −0.169 (−0.365, 0.026) | .090 | −0.102 (−0.267, 0.062) | .223 | −0.001 (−0.017, 0.014) | .863 | 0.010 (−0.003, 0.023) | .130 |
| Hypertension | −0.046 (−0.249, 0.157) | .657 | −0.078 (−0.250, 0.094) | .373 | 0.003 (−0.014, 0.019) | .733 | 0.000 (−0.013, 0.015) | .900 |
| Diabetes | 0.064 (−0.189, 0.317) | .618 | 0.053 (−0.158, 0.263) | .624 | 0.001 (−0.019, 0.022) | .910 | −0.003 (−0.020, 0.013) | .703 |
| LT (mm) | 0.383 (0.167, 0.599) | .001 | 0.289 (0.077, 0.502) | .008 | −0.015 (−0.033, 0.002) | .083 | −0.039 (−0.056, −0.022) | <.001 |
| AL (mm) | −0.328 (−0.434, −0.221) | <.001 | −0.136 (−0.235, −0.038) | .006 | −0.015 (−0.024, −0.006) | .001 | −0.004 (−0.012, 0.004) | .334 |
| FCR (mm) | −0.220 (−0.290, −0.149) | <.001 | −0.109 (−0.181, −0.036) | .003 | −0.004 (−0.009, 0.002) | .200 | 0.000 (−0.005, 0.007) | .785 |
| Decentr (mm) | 6.869 (6.257, 7.481) | <.001 | 6.934 (6.308, 7.560) | <.001 | — | — | — | — |
| Tilt (°) | — | — | — | — | 0.045 (0.041, 0.049) | <.001 | 0.044 (0.040, 0.048) | <.001 |
AL = axial length; b = regression coefficient; FCR = front curvature radius; LT = lens thickness
Figure 3.
Correlations between the tilt and decentration of crystalline lens and associated factors. A: Scattergrams showing the relationships between crystalline lens tilt and decentration, axial length, lens thickness, and front curvature radius of lens. B: Scattergrams showing the relationships between crystalline lens decentration and tilt, age, and lens thickness.
In the multivariate analysis for crystalline lens decentration, greater crystalline lens decentration was positively associated with age (P < .001) and tilt (P < .001) and negatively associated with LT (P < .001) (Figure 3, B). For every 1 degree increase in lens tilt, decentration increased by 0.045 mm, and for 1 mm decrease in LT, decentration decreased by 0.015 mm. Sex, the presence of diabetes, AL, and FCR were not significantly associated with crystalline lens decentration. In other words, greater crystalline lens tilt, and thinner and older lens result in larger decentration.
DISCUSSION
The tilt and decentration of postoperative IOLs were strongly correlated with the position of preoperative crystalline lens. A better understanding of the characteristics of preoperative crystalline lens position and associated factors will improve IOL performance. Therefore, it is important to quantify the tilt and decentration of natural crystalline lens objectively and efficiently. Nevertheless, no device is able to image and analyze the complete crystalline lens biometry currently. To the authors' knowledge, CASIA2 is the first with high-quality image lens morphology and automatically measures lens front and back curvature radius, lens equator diameter, tilt, and decentration of crystalline lens and IOLs.
This cross-sectional study of 1097 participants is the first, to our knowledge, to investigate the multiaspect important factors for crystalline lens tilt and decentration in age-related cataract. We found that the crystalline lenses showed a mean tilt of 5.16 degrees toward the inferotemporal direction and a mean decentration of 0.22 mm toward the temporal direction. One hundred nineteen eyes (10.85%) had a tilt greater than 7 degrees, and 89 eyes (8.11%) had a decentration more than 0.4 mm. We further demonstrated that larger decentration, thicker lens, short AL, and short FCR were associated with greater crystalline lens tilt. Moreover, greater tilt and older and thinner lens were correlated with decentration.
In previous studies, Purkinje images, Scheimpflug analyzer, and swept-source OCT (IOLMaster 700) have been used to measure the lens geometry, and they all found that the crystalline lens was not aligned perfectly along the visual axis.6,12–14 Schaeffel et al. reported that the crystalline lenses tilted about 4.6 degrees toward the temporal side and decentered approximately 0.3 mm downward relative to the pupil center using Purkinje images.13 Findings in another study showed that crystalline lenses decentered 0.25 mm toward the temporal direction and tilted 2.85 degrees toward the inferotemporal direction using Scheimpflug analyzer.12 Other studies using IOLMaster 700 reported that the mean tilt of crystalline lens was 3.36 to 4.3 degrees toward the nasal direction in both eyes.6,14 However, these methods have relatively poor image resolution and cannot quantitatively measure the tilt and decentration of lens because of technical problems. As a result, previous studies of lens biometric parameters produced inconsistent results. Kimura et al. were the first to use CASIA2 to measure the tilt and decentration of crystalline lenses and IOLs.10 They found that crystalline lenses had a inferotemporal tilt of 4.22 to 5.30 degrees and a temporal decentration of 0.03 to 0.12 mm.10 There was a mirror symmetry between the right eyes and the left eyes.10 Another study also reported that the crystalline lens tilted about 4.9 ± 1.0 degrees toward the inferotemporal direction.11 The results in our study accorded closely with those of Kimura et al. and Wang et al.10,11
A previous study has demonstrated that AL is negatively correlated with crystalline lens and IOL tilt.6,15 In this study, we also found that AL was negatively associated with the tilt of natural crystalline lens in age-related cataract patients, which means that crystalline lenses are more prone to tilt in patients with short AL. The possible cause of this phenomenon is that the crystalline lenses may be more likely to tilt in the crowded intraocular space. Nevertheless, we also found that AL was not significantly associated with crystalline lens decentration.
So far, to our knowledge, no report has been published the correlations about crystalline lens tilt with lens thickness and front curvature radius. Although myopic subjects exhibited thinner crystalline lens and lower lens power compared with emmetropic subjects, the effect of lens thickness on tilt may be induced by AL.16,17 However, we found that even after adjustment for age, sex, and AL by the multivariate regression model, LT was still positively associated with lens tilt. In addition, we also reported that the increased FCR was also negatively correlated with crystalline lens tilt. These results suggested that the shorter the lens FCR and the thicker the lens, the greater tilt the lens is.
Furthermore, we observed that the extent of lens decentration is becoming larger along with age. The well-centered position of the lens depends on the equal tension of zonular fibers, which weakens with age, thus the decentration of lens are probably related with the zonular weakness. Moreover, we found that LT was negatively associated with lens decentration. These results indicated that the thinner the lens, the easier it shifts, however, the thicker the lens, the easier it tilts.
As the definition of tilt and decentration, the greater the tilt of the crystalline lens is, the larger the decentration of it is. Tilt is the angle of lens axis against the reference (corneal topographic axis), and decentration is the vertical distance from lens center to the reference. Thus, a greater lens tilt results in a larger lens decentration. More attention should be paid to the patients with greater lens tilt or decentration before cataract surgery. The using of a toric and multifocal IOL should be prudent since these IOLs are more dependent on alignment with visual axis to achieve the best visual quality. In addition, our previous study has found that larger capsulorhexis size with bad coverage of IOL edge is significantly correlated with IOL decentration.15 Thus, appropriate capsulorhexis size that covers IOL edge perfectly should be warranted in patients with larger preoperative lens decentration.
Finally, we also validated the measurements of CASIA2 using model eye (OEMI-7; Ocular Instruments). This model eye consists of a cornea and crystalline lens both of which are made of poly(methyl methacrylate) with a refractive index of 1.485. The anterior chamber and vitreous chamber were filled with saline solution. As shown in Supplementary Table 1 (http://links.lww.com/JRS/A347), we found CASIA2 could accurately measure the anterior segment parameters of model eye with good repeatability, including radius curvature of cornea, anterior chamber depth, lens thickness, and lens equator diameter. The measurements of lens radius curvature obtained from CASIA2 are consistently smaller than the actual values of model eye. We speculate that it is attributed to the custom-developed algorithm that calculates the lens radius curvature using the central part of lens surface with a diameter of 3 mm. However, as a systemic error, it would not affect our conclusion.
This study has several limitations. First, optical imaging instruments are subject to geometrical and optical distortion, so optical distortion correction of CASIA2 still requires further research using model eyes.18,19 Second, lens opacities and asymmetric distribution of the refraction index may affect the results of lens parameters from CASIA2, especially in patients with cataract. Further studies are necessary to explore the relationships of lens opacity and refractive index or constant, and the measurement should be adjusted according to the different refractive index or constant. Third, the agreements of lens tilt and decentration obtained by CASIA2 and other devices such as Purkinje-like images and Scheimpflug imaging still need to be validated as previous study.20
In conclusion, our study demonstrated that the natural crystalline lenses tilted about 5.16 degrees toward the inferotemporal direction and decentered about 0.22 mm toward the temporal direction in age-related cataract. Larger decentration of crystalline lens, shorter AL and FCR, and thicker lens were significantly associated with greater crystalline lens tilt. In addition, greater tilt, older and thinner lens contributed to larger crystalline lens decentration. Our findings indicated that CASIA2 can be used to measure the biometry of crystalline lenses before cataract surgery, combined with age and AL, so as to predict the tilt and decentration of postoperative IOLs.
WHAT WAS KNOWN
Crystalline lens is not aligned perfectly along the visual axis.
CASIA2 AS-OCT is the first with high-quality image lens morphology that automatically measures lens front and back curvature radius, lens equator diameter, tilt, and decentration of crystalline lens and IOLs.
WHAT THIS PAPER ADDS
10.85% of patients with age-related cataract had a tilt greater than 7 degrees, and 8.11% had a decentration more than 0.4 mm.
The greater tilt of the crystalline lens, the larger decentration and vice versa.
Larger crystalline lens decentration, thicker lens, shorter axial length, and front curvature radius were significantly correlated with greater crystalline lens tilt.
Greater crystalline lens tilt, thinner lens, and older age resulted in larger decentration.
Footnotes
X. Chen and X. Gu contributed equally to this work.
Supported by the National Natural Science Foundation of China (81770905 and 81873675), the Pearl River Nova Program of Guangzhou (201806010167), the Natural Science Foundation of Guangdong Province (2017A030313802), and the Construction Project of High-Level Hospitals in Guangdong Province (303020102).
First author:
Xiaoyun Chen, MD, PhD
State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou, Guangdong, China
Disclosures: None reported.
Contributor Information
Xiaoyun Chen, Email: chenxiaoyun@gzzoc.com.
Xiaoxun Gu, Email: guxiaoxun01@163.com.
Wei Wang, Email: will.wong@qq.com.
Guangming Jin, Email: jingm@mail2.sysu.edu.cn.
Lanhua Wang, Email: wanglanhua666666@126.com.
Enen Zhang, Email: 472523530@qq.com.
Jingmin Xu, Email: 2587246302@qq.com.
Zhenzhen Liu, Email: liuzhenzhen@gzzoc.com.
Yizhi Liu, Email: yzliu62@yahoo.com.
REFERENCES
- 1.Lawu T, Mukai K, Matsushima H, Senoo T. Effects of decentration and tilt on the optical performance of 6 aspheric intraocular lens designs in a model eye. J Cataract Refract Surg 2019;45:662–668 [DOI] [PubMed] [Google Scholar]
- 2.Taketani F, Matuura T, Yukawa E, Hara Y. Influence of intraocular lens tilt and decentration on wavefront aberrations. J Cataract Refract Surg 2004;30:2158–2162 [DOI] [PubMed] [Google Scholar]
- 3.Fujikado T, Saika M. Evaluation of actual retinal images produced by misaligned aspheric intraocular lenses in a model eye. Clin Ophthalmol 2014;8:2415–2423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olsen T. Prediction of the effective postoperative (intraocular lens) anterior chamber depth. J Cataract Refract Surg 2006;32:419–424 [DOI] [PubMed] [Google Scholar]
- 5.Hirnschall N, Buehren T, Bajramovic F, Trost M, Teuber T, Findl O. Prediction of postoperative intraocular lens tilt using swept-source optical coherence tomography. J Cataract Refract Surg 2017;43:732–736 [DOI] [PubMed] [Google Scholar]
- 6.Wang L, Guimaraes de Souza R, Weikert M, Koch D. Evaluation of crystalline lens and intraocular lens tilt using a swept-source optical coherence tomography biometer. J Cataract Refract Surg 2019;45:35–40 [DOI] [PubMed] [Google Scholar]
- 7.Rosales P, Marcos S. Phakometry and lens tilt and decentration using a custom-developed Purkinje imaging apparatus: validation and measurements. J Opt Soc Am A 2006;23:509–520 [DOI] [PubMed] [Google Scholar]
- 8.Tabernero J, Benito A, Nourrit V, Artal P. Instrument for measuring the misalignments of ocular surfaces. Opt Express 2006;14:10945–10956 [DOI] [PubMed] [Google Scholar]
- 9.Rosales P, Wendt M, Marcos S, Glasser A. Changes in crystalline lens radii of curvature and lens tilt and decentration during dynamic accommodation in rhesus monkeys. J Vis 2008;8:18.1–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kimura S, Morizane Y, Shiode Y, Hirano M, Doi S, Toshima S, Fujiwara A, Shiraga F. Assessment of tilt and decentration of crystalline lens and intraocular lens relative to the corneal topographic axis using anterior segment optical coherence tomography. PLoS One 2017;12:e0184066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang X, Chen X, Tang Y, Wang J, Chen Y, Sun X. Morphologic features of crystalline lens in patients with primary angle closure disease observed by CASIA 2 optical coherence tomography. Invest Ophthalmol Vis Sci 2020;61:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hu C, Jian J, Cheng Y, Hsu H. Analysis of crystalline lens position. J Cataract Refract Surg 2006;32:599–603 [DOI] [PubMed] [Google Scholar]
- 13.Schaeffel F. Binocular lens tilt and decentration measurements in healthy subjects with phakic eyes. Invest Ophthalmol Vis Sci 2008;49:2216–2222 [DOI] [PubMed] [Google Scholar]
- 14.Lu Q, He W, Qian D, Lu Y, Zhu X. Measurement of crystalline lens tilt in high myopic eyes before cataract surgery using swept-source optical coherence tomography. Eye Vis (Lond) 2020;7:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen X, Gu X, Wang W, Xiao W, Jin G, Wang L, Dai Y, Zhang E, Ruan X, Liu Z, Luo L, Liu Y. Characteristics and factors associated with intraocular lens tilt and decentration after cataract surgery. J Cataract Refract Surg 2020;46:1126–1131 [DOI] [PubMed] [Google Scholar]
- 16.Muralidharan G, Martinez-Enriquez E, Birkenfeld J, Velasco-Ocana M, Perez-Merino P, Marcos S. Morphological changes of human crystalline lens in myopia. Biomed Opt Express 2019;10:6084–6095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mutti DO, Mitchell GL, Sinnott LT, Jones-Jordan LA, Moeschberger ML, Cotter SA, Kleinstein RN, Manny RE, Twelker JD, Zadnik K, Grp CS. Corneal and crystalline lens dimensions before and after myopia onset. Optom Vis Sci 2012;89:251–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Castro A, Rosales P, Marcos S. Tilt and decentration of intraocular lenses in vivo from Purkinje and Scheimpflug imaging. Validation study. J Cataract Refract Surg 2007;33:418–429 [DOI] [PubMed] [Google Scholar]
- 19.Ortiz S, Siedlecki D, Grulkowski I, Remon L, Pascual D, Wojtkowski M, Marcos S. Optical distortion correction in optical coherence tomography for quantitative ocular anterior segment by three-dimensional imaging. Opt Express 2010;18:2782–2796 [DOI] [PubMed] [Google Scholar]
- 20.Sun M, de Castro A, Ortiz S, Perez-Merino P, Birkenfeld J, Marcos S. Intraocular lens alignment from an en face optical coherence tomography image Purkinje-like method. Opt Eng 2014;53:061704 [Google Scholar]