Abstract
Ankle arthritis is a major source of morbidity impacting a younger working age population than hip and knee arthritis. Unlike the hip and knee, more than 70% of ankle arthritis cases are post-traumatic, with the remainder being inflammatory or primary arthritis. Nonoperative treatment begins with lifestyle and shoe-wear modifications and progresses to bracing, physical therapy, anti-inflammatory medications, and intra-articular injections. Ankle arthrodesis and total ankle arthroplasty are the 2 main surgical options for end-stage ankle arthritis, with debridement, realignment osteotomy, and distraction arthroplasty being appropriate for limited indications.
Level of Evidence:
Level V, expert opinion.
Keywords: arthritis, ankle arthritis, ankle arthrodesis, total ankle replacement, ankle
Introduction
Unlike the arthritides of the hip and knee, ankle arthritis is primarily post-traumatic (70%) and most often from rotational ankle fractures. 102 The remaining 30% are from chronic ligamentous instability, malalignment, inflammatory conditions, neuropathy, systemic medical conditions such as hemophilia, or idiopathic. 102 In addition, end-stage ankle arthritis has significant effects on function, 1 with similar morbidity, pain, and loss of function as hip arthritis. 42 Surgical treatment has been shown to improve unemployment rates and be cost-effective on a societal level. 38
Ankle arthritis is increasingly recognized as a major source of morbidity, impacting younger adults in their most societally and monetarily productive years (age 55 for fusions and 63 for replacements 130 ). This cohort of 55-year-olds likely have 10 more productive work years prior to retirement as compared to hip or knee arthritis patients who are already in their retirement years (65 in total hip arthroplasty and 66 in total knee arthroplasty 106 ). Although less prevalent than in the hip or knee, 24 ankle arthritis can lead to a greater societal impact by detrimentally affecting vocational abilities and resulting in loss of employment productivity, because of the younger age of onset. 38
Patient Assessment
Assessment of ankle pain begins with a thorough history of the presenting symptoms and attention paid to the area of maximal discomfort and pain. Ankle arthritis typically presents with activity-related anterior, lateral, or medial ankle pain and stiffness with a history of ankle trauma or instability (Table 1). Relevant additional history includes previous lower limb trauma, ankle sprains, known alignment issues, systemic medical conditions, and prior surgeries. Relevant systemic symptoms, such as fever, chills, rigors, or pain, heat, and swelling in multiple joints, should be inquired about for possible infections or inflammatory causes. It is important to ask how the ankle pain impacts the patient’s activities of daily living and occupational duties, as this can dictate which treatment is most appropriate once a firm diagnosis is established.
Table 1.
Typical History and Physical Examination Findings in Ankle Arthritis.
| History | Physical Examination | |
|---|---|---|
| Soft tissues | Activity-related swelling Recurrent ankle sprains |
Swelling/ankle effusion Ankle inverter and everter tendons may be weak and/or tender. Deltoid and lateral ligament complex may be deficient/incompetent |
| Pain | Activity-related pain—may be limited to anterior, medial, lateral posterior, or central, but frequently anterior | Tenderness around the ankle: medially, laterally, anteriorly |
| Ankle motion | Stiffness | Decreased range of motion |
| Hindfoot alignment | Possible change with time | Varus/valgus/neutral/pronated/supinated |
| Forefoot alignment | Abduction/adduction/neutral | |
| Medial longitudinal arch | Cavus/planus/neutral | |
| Anatomical axis (coronal) | Possible long-standing deformity |
Varus/valgus/neutral alignment of the hip/femur/knee/tibia Is the ankle deformity compensatory for a hip/knee deformity? Is the ankle joint concentric? |
| Anatomical axis (sagittal) | Recurvatum/procurvatum/neutral to the femur/knee/tibia | |
| Adjacent joints | Foot pain if arthritic | If arthritic, swelling/tenderness/stiffness to subtalar, talonavicular, calcaneocuboid, or other joints in the foot |
Focused examination of the ankle assesses lower limb alignment, surface, and bony anatomy. Standing hindfoot alignment should be assessed with attention to varus or valgus deformity. Localization of tender points indicate the origin of articular or bony pathology surrounding the ankle, such as in the talonavicular joint, calcaneocuboid joint, naviculocuneiform joint, subtalar joint, or sinus tarsi. Range of motion (ROM) should be assessed, both of the ankle joint (dorsiflexion and plantarflexion), and the subtalar, talonavicular, and calcaneocuboid triple joint complex (eversion and inversion), with attention paid to ROM in each component. Restriction in ROM can indicate arthritic changes. Examinations should be performed bilaterally and also include observation of hip and knee alignment, gait, and neurovascular function.
Examination of ligamentous stability and associated muscles and tendons is also necessary. A positive anterior drawer test and varus stress test can indicate possible injury to the anterior talofibular ligament or calcaneofibular ligament, respectively, which are also potential etiologies of ankle arthritis. Ankle assessment should also include the peroneal tendons laterally, with palpation along their course and strength testing with resisted ankle plantarflexion/eversion. Similarly, assessment of the posterior tibial tendon should be done with palpation along its course and resisted ankle plantarflexion/inversion. Finally, it is also important to note previous surgical incisions as this may influence the surgical plan.
Radiographic classification for assessment of ankle osteoarthritis (OA) is not standardized in the literature. The definition of ankle OA is generally based on joint space narrowing, osteophytes, and subchondral sclerosis, which makes up the basis of the Kellgren-Lawrence classification system, 17 but the authors prefer to use the Canadian Orthopaedic Foot and Ankle Society (COFAS) system 69 which incorporates the presence of a tight heel cord, intra- and juxta-articular deformity, as well as adjacent joint OA (Table 2). The radiographic technique for the assessment of the ankle in OA is also variable in the literature but authors generally base their assessment on weightbearing anteroposterior, mortise, lateral and hindfoot alignment views. Weightbearing views are generally considered more reliable for assessment of ankle OA. 31
Table 2.
Canadian Orthopaedic Foot and Ankle Society (COFAS) Preoperative Classification System for End-Stage Ankle Arthritis.a
| Type 1 | Type 2 | Type 3 | Type 4 | |
|---|---|---|---|---|
| Preoperative classification | Isolated ankle arthritis | Ankle arthritis with intra-articular deformity, ankle instability, and/or a tight heel cord | Ankle arthritis with hindfoot deformity, tibial malunion, midfoot ab- or adductus, supinated midfoot, plantarflexed first ray, etc | Types 1-3 plus subtalar, calcaneocuboid, or talonavicular arthritis |
| Potential concurrent procedures with total ankle replacement or ankle arthrodesis | None, hardware removal | Deltoid ligament release, ligament reconstruction, tendo-Achilles lengthening, gastrocnemius recession, tendon transfer, capsule release, forefoot reconstruction, metatarsal osteotomy, dissection of neurovascular structures, plantar fascia release, syndesmosis reconstruction | Fibular osteotomy, calcaneal osteotomy, tibial osteotomy, midtarsal arthrodesis | Arthrodesis: triple, subtalar, talonavicular, or calcaneocuboid |
aAdapted from Krause et al, 2012. 69
Any osseous or joint deformity should be assessed above, at, and below the tibiotalar joint level. Supramalleolar alignment is assessed in coronal and sagittal planes using the medial distal tibial and anterior distal tibial angles respectively. 65,113 Inframalleolar hindfoot alignment can be assessed on the hindfoot alignment view of Saltzman and El-Khoury. 101 The patient stands on a 6-inch platform facing the x-ray cassette placed at 20 degrees to the vertical, leaning away from the patient. The x-ray tube is positioned behind the patient perpendicular to the cassette, with the beam centered at the ankle joint. The mean moment arm as described by Saltzman is –3.2 mm (standard deviation 7.2 mm). 101
Advanced imaging modalities including computed tomography (CT), weight-bearing CT, single-photon emission CT (SPECT), and magnetic resonance imaging (MRI) contribute additional information in the workup of ankle arthritis. CT assessment in end-stage ankle OA is useful for demonstrating bone loss, cysts, and presence and extent of peri-talar OA, 126 which may be useful for preoperative planning. Weight-bearing CT is a relatively new modality that enables assessment of ankle alignment in the physiologic position.
Single-photon emission CT (SPECT-CT) combines a nuclear medicine detector with a CT scanner. This enables accurate localization of the part of the tibiotalar joint most affected by OA as well as demonstrate OA in adjacent joints. 66,87 Abnormal activity in a joint indicates a high likelihood of a positive response to image-guided joint injection in the presence of joint pain. MRI is particularly useful for assessment of the ankle soft-tissue envelope and cartilage pathology, 49 which may be relevant in reconstruction cases. Imaging is essential for planning treatment in ankle osteoarthritis, enabling assessment of severity, osseous deformity, alignment, adjacent joint disease, and the status of the soft tissue envelope.
Nonoperative Treatment
Nonsurgical treatment of ankle arthritis can allow preservation of mobility and function of the patient, while averting, or at least delaying, ankle surgery. As many patients are of working age and have occupational duties, taking time off for surgery and rehabilitation may be difficult. Nonoperative cornerstones include activity modification, weight loss, shoe modification, bracing, gait aids, physical therapy, nonsteroidal anti-inflammatory medications (NSAIDs), and joint injections. Bracing, as a noninvasive means of immobilizing the ankle, can be accomplished by a variety of nonarticulated ankle-foot orthoses (AFOs) or lace-up braces, both off-the-shelf and custom-made. The vast number of options leads to a paucity of strong literature for any single brace in the context of ankle arthritis. Shoe modifications, such as a rocker-bottom and cushioned soles, can assist in the mechanics of a stiff ankle or a braced ankle to allow enhanced forward propulsion and more normal gait. However, these devices can be expensive, and patient compliance is critical to success. Patients may not be able to comply given their financial and social situations. Activity modification and gait aids such as a cane can be effective but not always feasible depending on the patient’s occupational requirements. Education on expectations is crucial for success. NSAIDs can provide pain relief by their anti-inflammatory effect and, in the authors’ experience, the best results come from consistent use over a 6-week period. Prescribers should counsel patients about side effects such as gastrointestinal ulcers and nephrotoxicity. Joint injections are another option but have variable results. Common injections include corticosteroids, hyaluronic acid viscosupplements, or the less-proven platelet-rich plasma (PRP). A Cochrane review on the use of hyaluronic acid products in ankle arthritis was inconclusive especially compared with placebo. 127 Corticosteroid injections provide low-cost and accessible symptomatic relief with an unpredictable duration of effect. 124 Currently, newer therapies such as PRP or stem cell therapy are lacking sufficient evidence to recommend. The nonsurgical regimen should be selected based on patient and physician factors, such as patient preference, level of compliance, availability of modalities, and financial cost.
Surgical Treatment
Presently, surgery for ankle arthritis is predominantly ankle arthrodesis or total ankle arthroplasty (TAA) with increasing utilization of joint-preservation realignment osteotomies and less commonly, distraction techniques. Of those, ankle arthrodesis is performed far more frequently than TAA; however, there is a trend toward increasing numbers of arthroplasty, particularly in academic centers. 94 The authors use the COFAS pre- and postoperative classification system to guide management. 69
Ankle Arthrodesis
Ankle arthrodesis, or fusion, involves the tibiotalar joint and can include the subtalar joint for a complete hindfoot fusion. Arthrodesis is a mainstay of ankle arthritis treatment since being described by Albert in 1879. 3 Developments in the technique have been aimed at improving fusion rates and reducing invasiveness of surgery to improve overall patient outcomes.
The primary indication for ankle arthrodesis in arthritis is end-stage disease with failure of nonoperative treatment. Other indications include arthrosis from previous infection, talar avascular necrosis, 59 neuropathy, inflammatory arthropathy 121 including hemophilia, 11 salvage of failed arthroplasty, 57 and rarely primary treatment following severe ankle trauma. 2,112 Many techniques have been described for ankle fusion, and they broadly fall into 2 categories: open arthrotomy and minimally invasive. One major concern of arthrodesis is the acceleration of adjacent joint arthritis, which has been shown to be present in the triple joint complex, naviculocuneiform, tarsometatarsal, and first metatarsophalangeal joints after ipsilateral ankle fusion at 22-year follow-up. 22 Patients should be counseled about this natural history following ankle fusion. One should consider preserving some motion with a total ankle replacement in the presence of a stiff hindfoot or midfoot.
Open Arthrotomy Techniques
Several techniques have been described for open ankle arthrodesis. Laterally based approaches typically involve osteotomizing or excising the distal fibula for access to the ankle joint, such as in the classic transfibular technique described by Mann 78 in which he describes both excising and incorporating the distal fibula into the fusion. The addition of an anteromedial arthrotomy can help with medial ankle access. After preparation of the articular surfaces, the foot is neutrally positioned (detailed later) to the contralateral limb, followed by internal fixation under compression. Compression fixation was introduced by Charnley in 1951 using an external fixator. 18 Variations on the approach could include fibular-sparing techniques such as that described by Smith et al 107 and others. 5,72,114 Sparing the fibula is important with the increasing popularity of TAA as it can make future conversion easier. The anterior approach can be used with various forms of fixation and compression, including transarticular screws, anterior compression plates, or both. 20,99,125 Anterior approaches allow easier visualization of the joint surface and preservation of the fibula. It is also frequently used in trauma and may be ideal in post-traumatic osteoarthritis cases with prior anterior incisions. The use of an anterior plate is indicated with poor bone quality and strength of screw purchase if the surgeon feels screw fixation alone is inadequate. Intact posterior structures can enhance stability and compression with the anterior plating technique. An anterior plate, particularly with locking screw constructs, can increase the strength of fixation and compression in patients with poor bone quality, such as in osteopenia or rheumatoid arthritis compared with screws alone. 29,104,118 In addition, locking plates can help hold large deformity correction cases aligned if there are concerns for potential subsidence. In cases with poor anterior soft tissues such as with previous trauma, posterior approaches can be performed instead. This also allows visualization of both the tibiotalar and subtalar joint in the same exposure, making it a convenient technique for fusing both of these joints when indicated. There are precontoured posterior plates available for both ankle and tibiotalocalcaneal (TTC) arthrodesis.
In all cases, the joint surfaces for fusion are prepared by removing all remaining articular cartilage and preparing subchondral bone with instruments such as high speed burrs, curettes, saws, and osteotomes under direct visualization. One can preserve the tibiotalar joint shape, but beware this makes talar translation difficult. If this is desired, then creating flat fusion surfaces allows more talar translation, especially posteriorly at the cost of some shortening. Fenestration of the remaining subchondral bone surfaces is common practice using either drills, burrs, Kirschner wires, or osteotomes. Bone graft, either autogenous or substitute product, is then applied to the fusion surfaces where needed. In recent years, there has been interest in orthobiologics in foot and ankle surgery, particularly with ankle fusions, but more research is needed before one product is recommended. 75 The indications for bone graft are not clearly defined; however, there are some factors generally agreed upon as requiring it, such as prior nonunion and avascular necrosis. 8 Attempts have been made to develop a risk assessment model for nonunion 120 but there is still inadequate information to develop formal guidelines on when to use bone graft product. One must also consider the cost-benefit ratio as some products are expensive.
Correct alignment of the arthrodesis is required. Ideally, ankle dorsiflexion is neutral with rotation to match the contralateral side. Coronal alignment should allow about 5 degrees of hindfoot valgus, which occurs naturally through the subtalar joint in normal individuals. Thus, the tibiotalar surfaces should be well-apposed and parallel to the talar dome in the coronal plane. The talus should be posteriorly translated relative to the tibia, effectively shortening the lever arm of the foot and reducing the torque through the midfoot and fusion site with load-bearing. This is a commonly held belief and, in the authors’ experience, helps with foot progression, but high-quality evidence is lacking and this is expert opinion. Beware of excessive posterior translation, which reduces available talar bone stock for plate fixation. Kirschner wires may be used for provisional fixation prior to definitive fixation, and attention must be paid to compressing across the fusion site to maintain the desired position. Typically cannulated larger screws are used (such as 6.5-mm or 7.3-mm partially threaded variety) or solid smaller screws (such as 3.5-mm “small fragment” screws). The appropriate screw trajectory can be challenging to find, and one risks larger bone loss with misplaced larger screws (and associated screw tract) that need to be replaced, hence the utility of obtaining the correct trajectory with much thinner guidewires and passing the larger cannulated screws only once. Compression is achieved via headed partially threaded screws or headless variable pitch screws with various configurations previously described. 48,53,78,84 If an anterior plate is utilized, then locking constructs may be selected for enhanced fixation, and compression can also be achieved with compression plating techniques. Constructs with lateral plating 12 and blade plating 109 have also been described. The objective in all cases is adequately debrided fusion surfaces free of cartilage, well apposed and compressed with stable rigid fixation.
Postoperatively, the ankle is immobilized and kept non–weight bearing for a minimum of 6 weeks but up to 12 weeks in patients with higher-risk comorbidities such as diabetes mellitus. Knee scooters to facilitate non–weight bearing are easier to use than crutches or wheelchairs. Some authors advocate for earlier weight bearing and have demonstrated good results. 16 Sutures are removed at approximately 2 weeks or when the wounds have healed. After the immobilization period, weight bearing is initiated as tolerated in a protective walker boot. Patients may continue to benefit from shoe modifications such as a well-cushioned rocker sole to accommodate the resultant stiff hindfoot after fusion. Physical therapy may commence for strengthening, balance, gait training, and overall mobility. Routine radiographs are taken to assess for bony union and any fixation complications, typically at 2, 6, and 12 weeks, then 6 months and 1 year, if needed. However, it can be difficult to determine if a fusion is successful based on plain radiographs alone, and studies have attempted to define the best method. 30,41 Plain radiographs are useful, however, for assessing the maintenance of the fusion position and if the selected fixation is still intact. CT scans can be used to assess percentage of fusion or to guide mobility, with 25% fusion mass indicative of a clinically successful fusion, although more fusion is shown to be beneficial. 41 Time to union has been reported to average 14.5 weeks with open arthrodesis. 82
Minimally invasive techniques
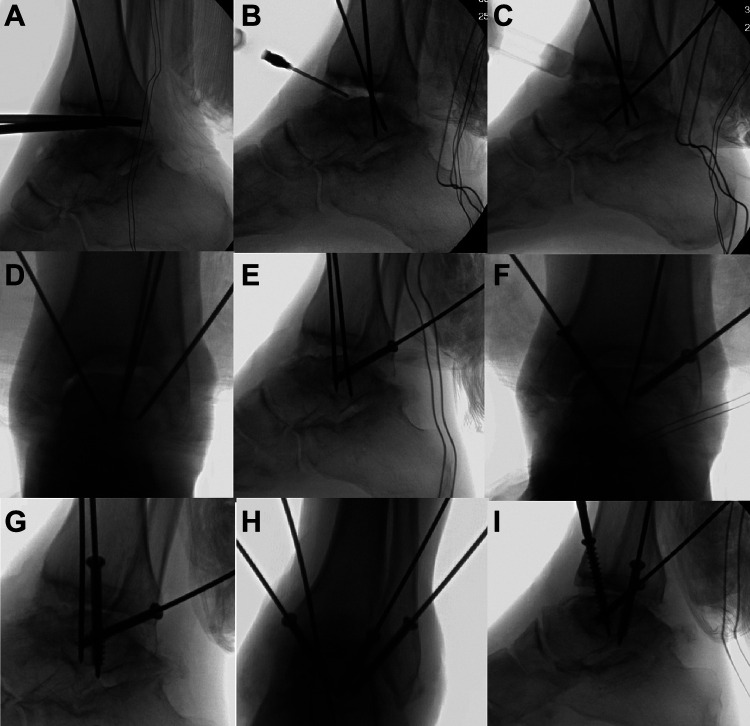
Arthroscopic techniques for arthrodesis have grown in popularity to avoid the large incisions and dissections associated with open techniques and the associated wound complications. In addition, there is less soft-tissue stripping and therefore less disruption of vascular supply to bone. Large coronal plane deformities beyond 15 degrees 35 may be a contraindication because of the limited ability to correct the deformity, although this has recently been called into question. 103 Conventionally, the arthroscopic joint preparation is performed through standard anteromedial and anterolateral portals; however, posterior arthroscopic fusion techniques have been described with good results. 73 Tourniquet use is surgeon preference and has the advantages of a bloodless surgical field. Tourniquet time is a limitation, and if placed on the calf, then the gastrocnemius-soleus complex is mechanically tethered and limits ankle range of motion, which may make arthroscopy more difficult. Scope size is surgeon preference; the authors recommend using 2.9- to 4.0-mm-diameter arthroscopes with a 30-degree angle. The larger the scope, the larger the field of view and flow of arthroscopic fluid, but this may increase the difficulty of maneuvering around the joint. Conversely, a smaller scope is easier to maneuver but will provide a smaller field of view, with a lower rate of flow. The arthroscope is used to visualize the joint surface to remove all cartilage. The patient is generally positioned supine with the hip and knee slightly flexed on a bolster of choice, and traction can be applied to the foot to increase the available joint space for arthroscopy. Standard anteromedial and anterolateral portals are established, and a diagnostic arthroscopy is performed. Visualization is improved by shaving synovial tissue and removing marginal osteophytes with an arthroscopic burr. With adequate debridement, the entire tibiotalar joint can be visualized for joint preparation. A combination of arthroscopic shaver and burr is effective in removing articular cartilage (Figures 1 and 2). Standard curettes are often simpler instruments to navigate the tight contours of the ankle joint. To aid in reaching the posterior ankle, additional posterior portals and accessory portals can be established to access the otherwise inaccessible portions of the joint depending on patient anatomy. The authors’ practice also includes use of a low-speed minimally invasive burr (MICA Instruments; Wright Medical, Memphis, TN) as an alternative to traditional arthroscopic burrs for fusion site preparation. Joint preparation along the articular surface makes posterior talar translation difficult as a result of the posterior malleolus. The authors address this by burring the posterior malleolus arthroscopically. The addition of a gastrocnemius recession can further improve posterior translation if tight. Burrs can be used to fenestrate the subchondral bone (Figures 3 and 4) in the same manner via the arthroscopic portals, and then all fluid is evacuated from the joint followed by insertion of bone graft product. Arthroscopy without fluid is used to direct and verify bone graft product placement. The traction is then removed, followed by the same positioning and fixation as above with screws.
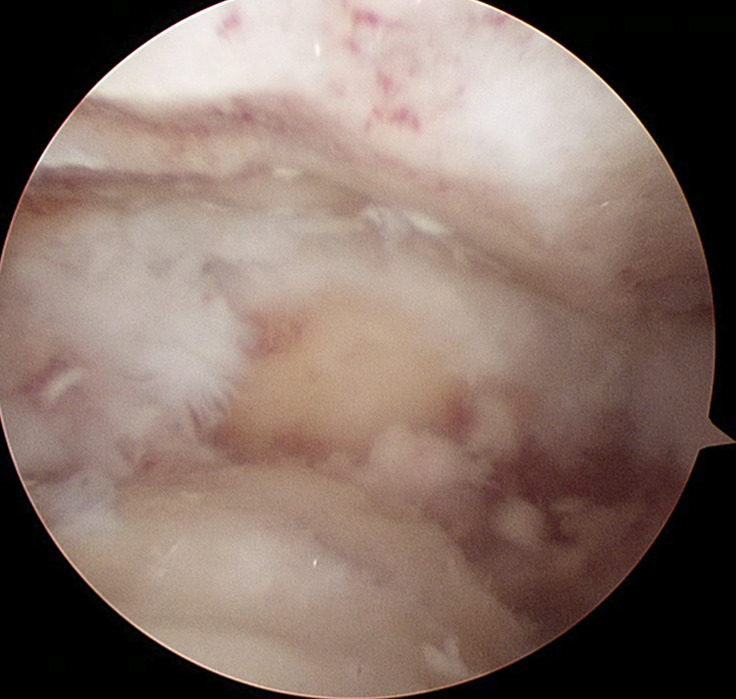
Figure 1.
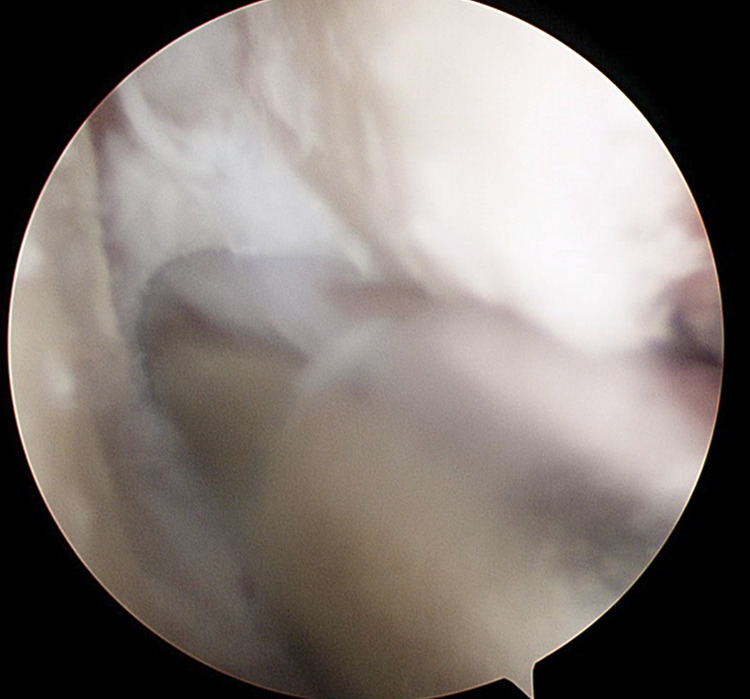
Arthroscopic view of the medial gutter of a right ankle from the anteromedial portal. A shaver is debriding articular cartilage and fibrous tissue via an accessory inferior medial portal.
Figure 2.
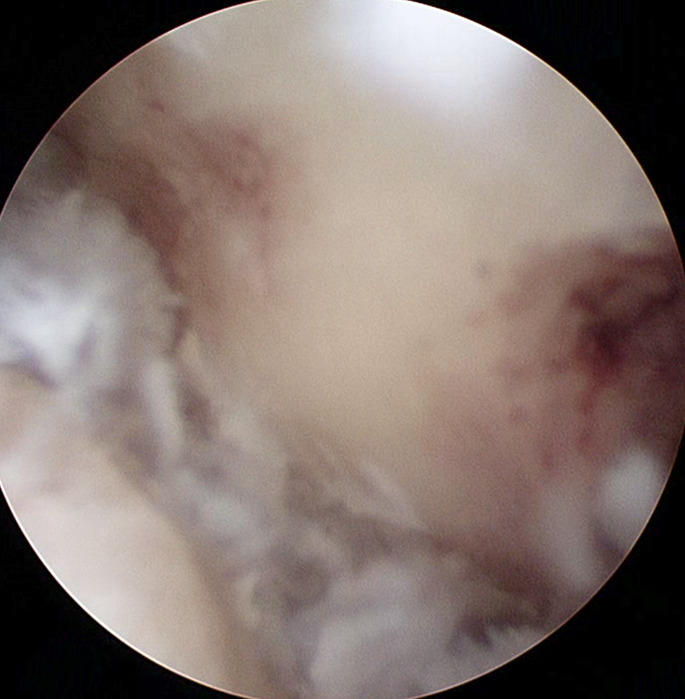
Arthroscopic view of the medial gutter of a right ankle from the anteromedial portal after debridement.
Figure 3.
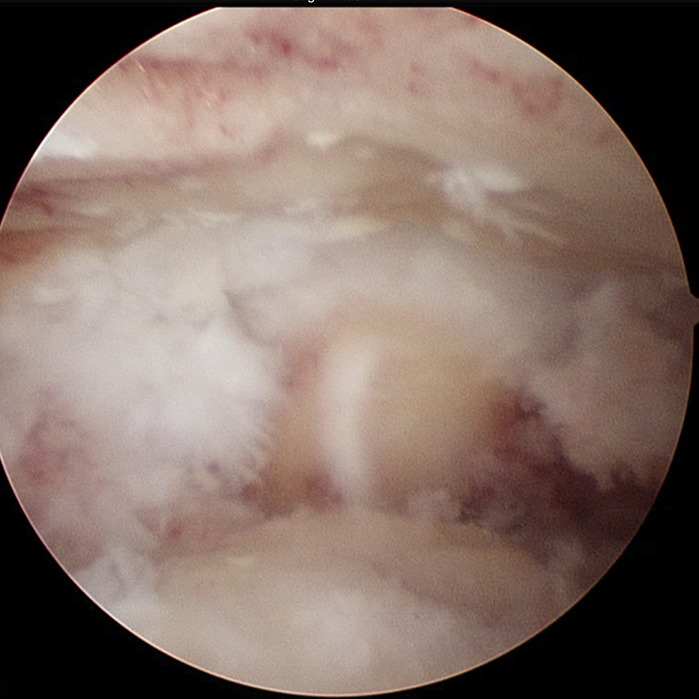
Arthroscopic view from the anteromedial portal of a right ankle looking laterally over the talar dome at the fibula and lateral gutter. Articular cartilage has been removed.
Figure 4.
Arthroscopic view from the anteromedial portal of a right ankle looking laterally over the talar dome at the fibula and lateral gutter. Further debridement of fibrous tissue has been performed and bare subchondral bone has been fenestrated with an arthroscopic burr.
Screw fixation configurations can be done much in the same way but percutaneously rather than through open incisions. As with arthroscopy portals, care must be taken to avoid damaging both subcutaneous and deep neurovascular structures when creating percutaneous screw tracts; only the skin is incised sharply and careful blunt dissection is used through the deeper layers. Contrasting with open techniques, plate fixation cannot be performed. The author’s preferred fixation construct is 3 large cannulated transarticular screws, either 6.5-mm headed or variable-pitch headless. The first screw is inserted either through the lateral or medial tibial cortex into the talar body under compression, depending on the intra-articular deformity correction desired (Table 3). The next screw is inserted as fully threaded for fixation through the remaining side. The third and final screw is the “home-run” screw as previously described, 53 inserted posterolaterally from the posterior malleolus into the talar body in line with the talar neck. Alternate screw trajectories and screw insertion order can be used depending on the deformity correction that is required in combination with manual manipulation (Table 3 and Figures 5 –12).
Table 3.
Sample Screw Configuration Variations for Ankle Fusions and Associated Intra-articular Deformity Correction Strategies.a
| Intra-articular ankle deformity | Varus | Valgus | Neutral |
|---|---|---|---|
| First screw crosses the ankle joint in the:b | Lateral half of the joint, in compression to correct varus | Medial half of the joint, in compression to correct valgus | Both lateral or medial, in any sequence, with balanced compression to maintain neutral alignment |
| Second screw crosses the ankle joint in the:b | Medial half of the joint, under compression | Lateral half of the joint, under compression | |
| Third screw crosses the ankle joint:c | Posteriorly, in line with the long axis of the talar neck, under compression. | ||
aStrategies vary depending on the deformity.
bLateral and medial screws can be inserted from their respective sides or both from the medial side under compression, with careful attention paid to where the screw crosses the joint.
cSome surgeons do not routinely use a third screw whereas some use more than 3.
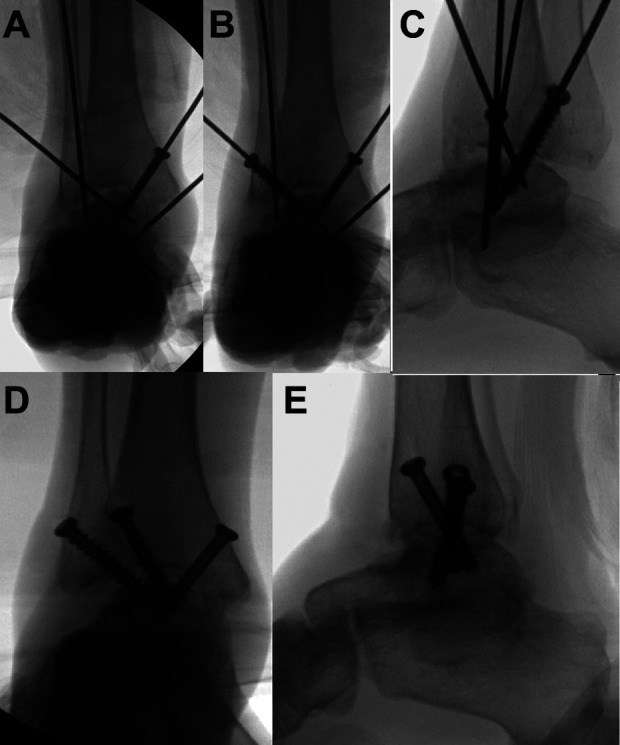
Figure 5.
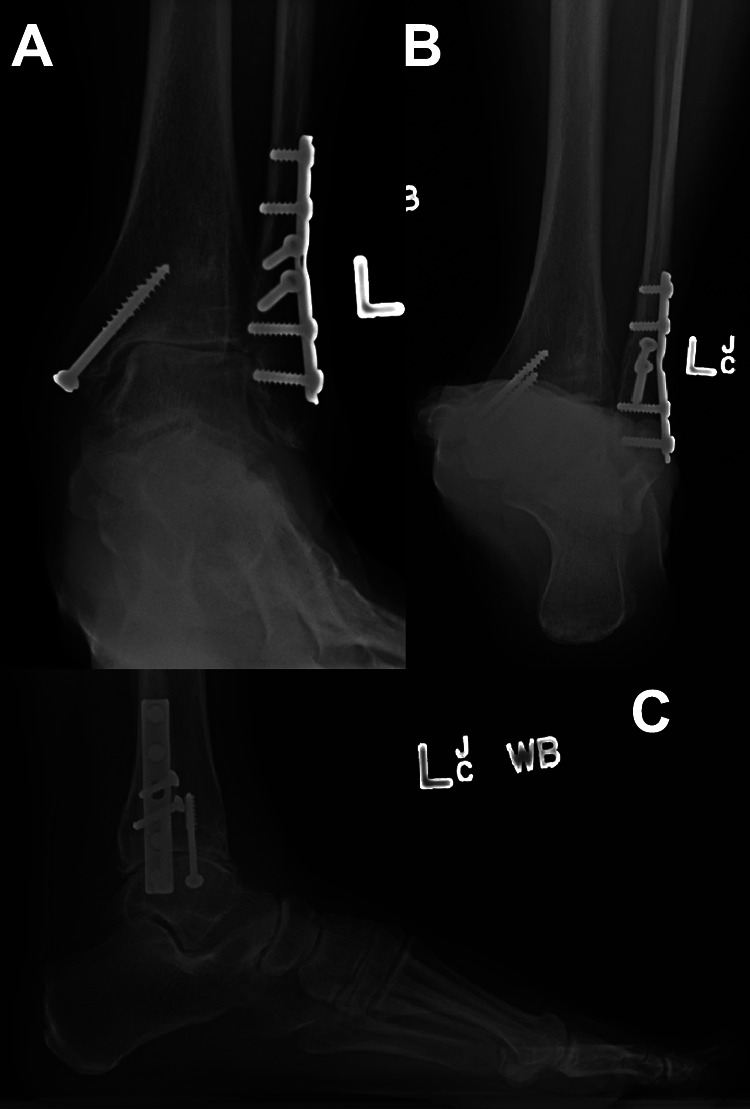
Case 1. Varus nonconcentric post-traumatic ankle arthritis weightbearing preoperative radiographs. Note the previous bimalleolar ankle fracture fixation. (A) Anteroposterior view; (B) hindfoot alignment view; (C) lateral view.
Figure 6.
Case 1. Varus nonconcentric ankle arthritis weightbearing radiographs after arthroscopic fusion with percutaneous screw fixation. Note that the previous medial malleolar fracture fixation was removed. The lateral screw was inserted first under compression to reduce the varus talar tilt, followed by the medial screw, and finally the posterior screw. (A) Anteroposterior view; (B) hindfoot alignment view; (C) lateral view.
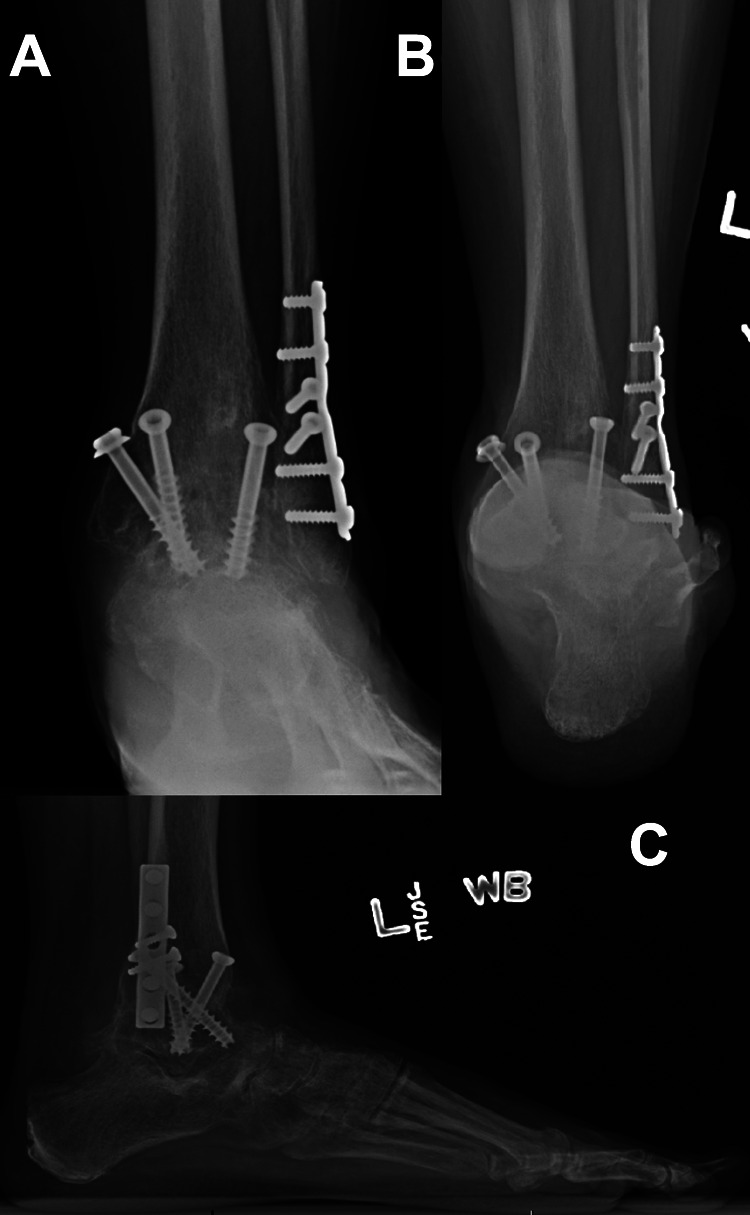
Figure 7.
Case 2. Valgus concentric ankle arthritis with ball-and-socket deformity and planovalgus foot. Weightbearing preoperative radiographs. (A) Anteroposterior view; (B) hindfoot alignment view; (C) lateral view.
Figure 8.
Case 2. Intraoperative fluoroscopic images of arthroscopic ankle fusion of valgus concentric ankle arthritis with ball-and-socket deformity after joint preparation and gastrocnemius recession to enhance deformity reduction. The ball-and-socket articulation allows simple angular reduction via screw placement. (A) Reduction of valgus alignment performed manually followed by K-wire placement to hold. Medial screw inserted first under compression to further reduce out of valgus. (B, C) Anteroposterior view of second screw inserted as full-threaded strut to prevent collapse back into valgus. (D, E) Third screw inserted anterolaterally under compression to obtain appropriate ankle dorsiflexion.
Figure 9.
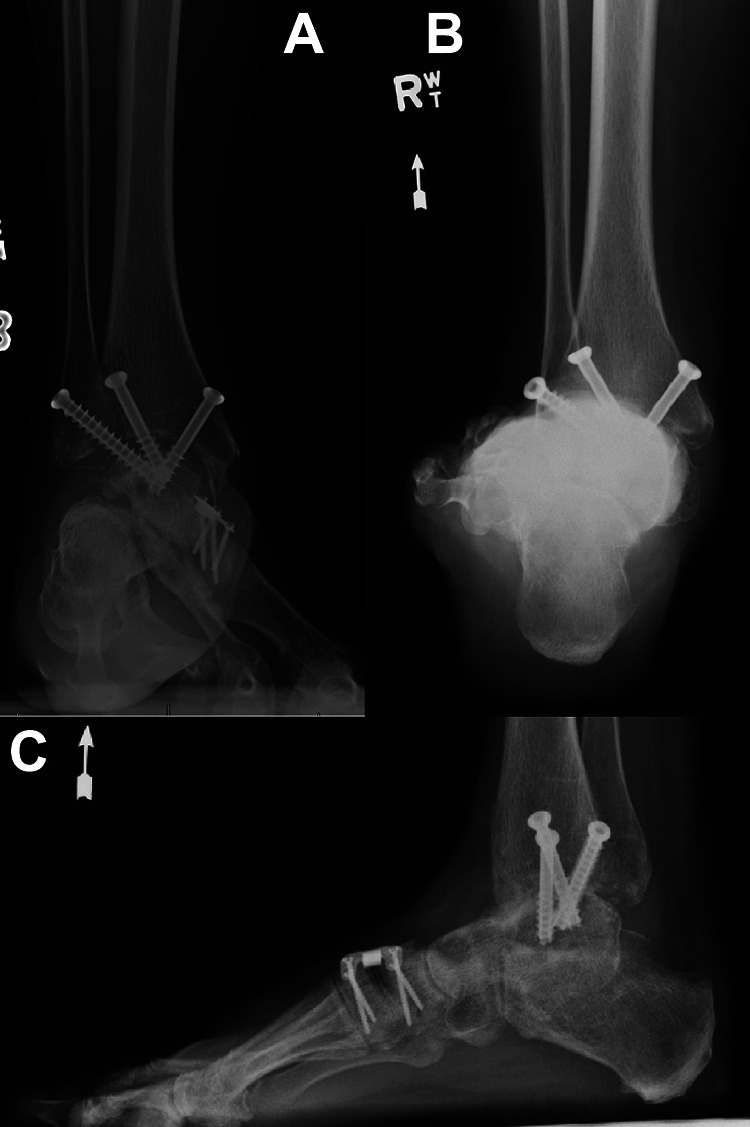
Case 2. Valgus concentric ankle arthritis with ball-and-socket deformity. Weightbearing postoperative radiographs after arthroscopic fusion with percutaneous screw fixation. Also note the concomitant medial cuneiform dorsal opening wedge osteotomy for correction of a dorsiflexed first ray. (A) Anteroposterior view; (B) hindfoot alignment view; (C) lateral view.
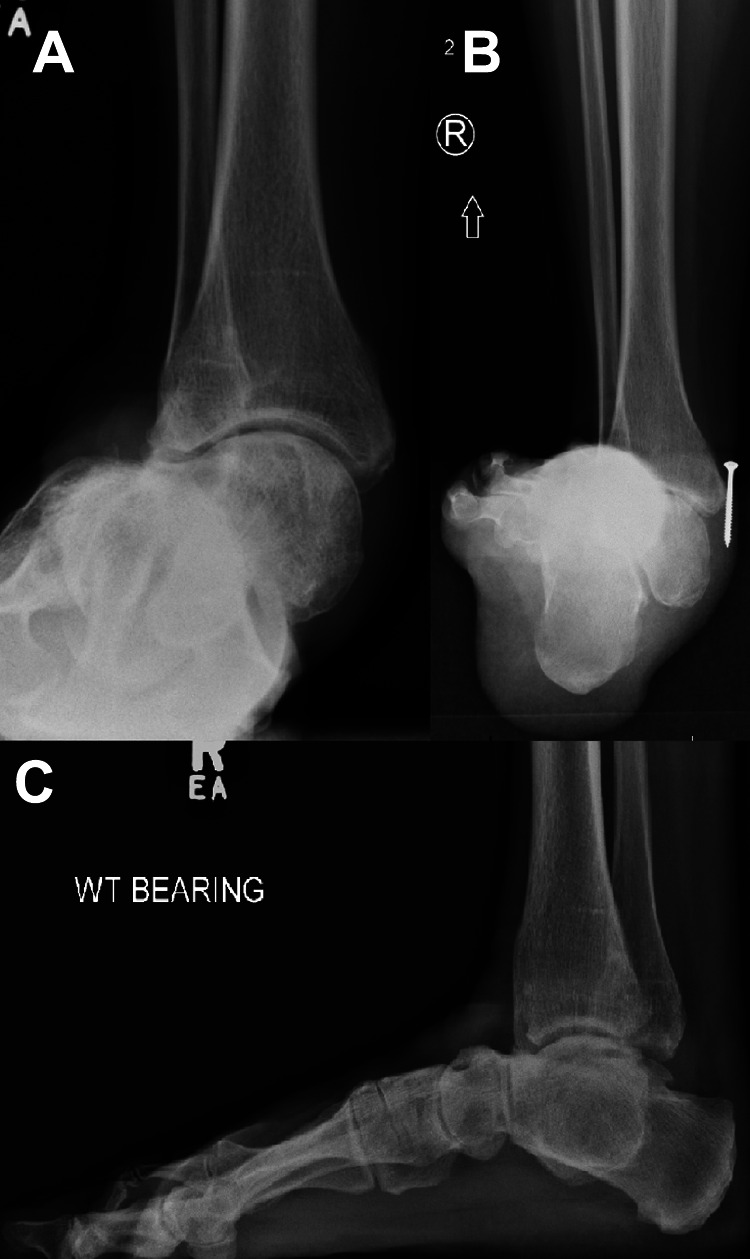
Figure 10.

Case 3. Anteriorly translated varus nonconcentric ankle arthritis preoperative weightbearing radiographs. Note the previous medial malleolar fracture screw fixation. (A) Anteroposterior view. (B) Lateral view.
Figure 11.
Case 3. Intraoperative fluoroscopic images of arthroscopic ankle fusion of case 3 after joint preparation and gastrocnemius recession to enhance posterior translation. (A) The posterior plafond is burred to allow more posterior translation. (B-C) Platelet-derived growth factor bone graft substitute is inserted into the anterior void (panel b) followed by demineralized bone matrix (panel c). (D) Ankle is manually reduced and provisionally fixed with K-wires. (E) First screw is inserted posterolaterally to reduce the anterior translation and varus talar tilt. (F, G) Second screw is inserted medially to compress medial side of joint. (H, I) Third screw is inserted anterolaterally as a fully threaded strut to avoid drifting back anteriorly. A fourth posteromedial screw is inserted under compression as well (not shown).
Figure 12.

Case 3. Postoperative weightbearing radiographs of case 3. A circumferential cast is applied due to patient noncompliance. (A) Anteroposterior view. (B) Hindfoot alignment view. (C) Lateral view. Note that a concomitant first metatarsal dorsiflexion osteotomy was performed to help create a plantigrade foot.
A miniarthrotomy technique has been described 81,89 that is a variation on the arthroscopic approach. Working portals are created like anterolateral and anteromedial arthroscopic ankle portals, but with larger incisions. Distractors are inserted to open the ankle joint space and the fusion surface is prepared like in open arthrotomy techniques with the same instruments via the established small incisions. The benefit is to minimize soft-tissue dissection and stripping and therefore wound complications much like arthroscopic techniques but also have more power to correct coronal plane deformities. The degree of correction is less reliable though, according to some authors. 48
The hindfoot nail
A hindfoot nail is a salvage device used to fuse the ankle joint in conjunction with the subtalar joint (tibiotalocalcaneal [TTC] arthrodesis). TTC arthrodeses need not be performed with the nail, but this device is useful in cases of severe deformities such as in Charcot arthropathy, rheumatoid arthritis, or with substantial degeneration of both joints. It is also used in severe talar bone loss, such as in trauma, for TTC fusion with structural bone graft or a direct tibiocalcaneal fusion. 96 The hindfoot nail is inserted through minimal incisions and is a particularly good complement to posterior arthroscopic arthrodesis that allows preparation of both the ankle and subtalar joint. However, it can also be used with traditional open approaches as well, and provides a load-sharing construct like a tibial or femoral nail. The trend with hindfoot nail fusions is to use lateral/perifibular approaches with separate medial approaches as needed, such as to correct a valgus deformity with medial malleolar shortening osteotomy, as opposed to a traditional direct anterior approach. Straight nails may have a higher risk of lateral plantar neurovascular injury and causing difficulty with maintaining normal hindfoot valgus and thus curved nails were introduced with a more lateral start point and promising results. 15 However, complication rates are reported as high as 40%, 71 with potential nonunion rates up to 15.8%. 96 Given this and the fusion of the subtalar joint, this procedure’s purpose should be a salvage to provide a stable plantigrade foot that can be walked upon while allowing pain relief and not for routine ankle arthrodesis.
External fixation
Ankle arthrodesis with external fixation such as the Ilizarov technique using circular frames have also been described with some success. 9,47,55 Cases where traditional internal fixation is not ideal, such as with active infections, poor bone quality for screw purchase, or open wounds at high risk of infection, are good candidates for external fixation while also allowing early weight bearing. 33 This technique is also a powerful tool for deformity correction using specialized ring-fixator constructs based on the technique of Ilizarov, and it allows adjustment outside the operating theater although specialized expertise is required. This has been used in severe deformity cases such as in Charcot arthropathy, leg length discrepancy, and other complex comorbidities with satisfactory union rates. 36 Given the nature of external frames, the disadvantages include having the bulky external frame for prolonged periods, open pin sites requiring care, and a compliant patient who can look after the frame. Therefore, this technique is best used as a salvage in specific indications such as challenging revision cases, possibly with infection, severe deformity or a poor soft-tissue envelope rather than a routine option in ankle arthrodesis.
Results
Several studies have reported good outcomes with ankle arthrodesis. Ankle fusion patients tended to remain active but often opt for less demanding sports, while having adequate functional outcomes and pain relief 60 with an improved gait. 13 Historically, complication rates were high and included non-union, malunion, infection, or amputation. 50,76,117 Reported nonunion rates ranged from 0% to 36%, averaging around 8% with open techniques, with more recent series showing better results according to a recent review. 128 Many modern series tend to focus on arthroscopic fusions, which have demonstrated improved fusion rates and lower complications 34,56,93 and better functional outcomes. 122 A recent systematic review demonstrated improved clinical outcome scores, lower complication rates, lower length of hospital stay and lower blood loss with arthroscopic fusions compared to open fusions; however, union rate, reoperation rate, and surgical time were similar. 90 Other studies demonstrated faster union with arthroscopic fusions. 83 A recent systematic review showed arthroscopic arthrodesis to yield improved fusion rates, lower tourniquet time, and lower length of stay but surgical time, infection, and complication rates were similar. 54
Total Ankle Arthroplasty
Total ankle replacement (TAA) as an alternative to arthrodesis is attractive for preservation of ankle joint motion and to better replicate normal gait while still relieving pain. Indications for TAA were classically limited to end-stage arthritis, more commonly inflammatory than post-traumatic in the older low-demand patient, with contraindications including Charcot arthropathy, active infection, obesity, poor vascular status, poorly controlled diabetes, and multiplanar foot or ankle deformities. 26,123 However, indications are expanding as surgical expertise and implant design improves. TAA has the potential benefits of offloading adjacent joints and potentially delaying the progress of adjacent joint degeneration that may diminish outcomes, and thus should be considered when there is concomitant ipsilateral subtalar stiffness or arthritis. Multiplanar deformities should be corrected prior to TAA or during the same surgery. Critical patient factors to consider include activity level and age given the limited longevity of TAAs. A recent review of international registry data shows revision rates between 4.6% and 17% at 5 years, and between 18.4% and 31% at 10 years. 115 Reports on specific implants frequently demonstrate survival over 80% at 10 years. 115
Treating ankle arthritis with arthroplasty rather than fusion began with Eloesser’s report of allograft joint transplantation in 1913 32 and ankle hemiarthroplasty in 1962 by Larson. 44 The first generation of prostheses was generally 2-component cemented designs that poorly replicated ankle kinematics and had unacceptably high failure rates with potentially poor bony incorporation characteristics. 121 However, interest in TARs increased with the ongoing success of total hip and knee arthroplasty, leading to the second generation of TAA implants. These are typically uncemented 2-component designs with a modular ultrahigh-molecular-weight polyethylene bearing (UHMWPE) fixed to the tibial component with a separate talar component, or 3-component designs utilizing a mobile UHMWPE bearing. The “third generation” includes mobile bearing designs borrowed from the same principle in mobile-bearing knee arthroplasty designs meant to allow high congruity of articulating components to best distribute load, while still minimizing constraint and therefore load transmission to the fixed components leading to failure. 44 Limitations in FDA requirements in the United States led to development of the current implants (sometimes considered the “fourth generation”) with fixed-bearing prostheses and a modular UHMWPE liner that attaches to the tibial component. The newest frontier of TAA is patient-specific implant placement guides thought to allow more accurate and predictable implant placement, but more data are warranted. 97
Balancing the ankle
It is critical to address concomitant lower limb deformities in ankle arthritis to allow a balanced TAA, 19,40 but it is unclear how much deformity is still tolerable. Deformities can be classified into intra-articular (ie, varus or valgus malalignment of the talus relative to the tibia causing incongruence) or extra-articular (ie, proximal or distal to the ankle joint); these are not mutually exclusive and can coexist.
Deformities in the hip, femur, knee, and tibia all affect overall mechanical axis alignment in the lower limbs. The deformities are ideally corrected from proximal to distal as smaller changes proximally will be magnified more distally. Treatment of these deformities begins with thorough assessment and imaging of complete lower limb alignment and may include corrective osteotomies or arthroplasty of the hip and knee. Similarly, foot deformities should be corrected as well. A planovalgus or cavovarus deformity should be treated as if there was no ankle arthritis. Assessment of degenerative and/or unstable joints can help determine which joints to fuse. Hindfoot valgus or varus can be treated with medializing or lateralizing calcaneal osteotomies, respectively. Triple fusion is a reasonable foot deformity correction option in patients with extensive degeneration, severe deformity, and advanced age prior to TAA. Other deformity patterns should be treated accordingly. These procedures can be done as a staged procedure with TAA or in the same setting depending on surgeon preferences and experience. If staged, then the deformity correction should be performed prior to TAA, or very shortly after TAA, to minimize potential eccentric loading through the arthroplasty. In any case, the ultimate goal is the same: to achieve a stable plantigrade foot to support a TAA.
An incongruent ankle joint is associated with failure of TAA. 46,98 Conversely, TAA after correction of coronal plane malalignment has been shown to be similarly successful to those with minimal preoperative deformity. 61 Thus, these deformities must also be corrected to avoid edge-loading after TAA implantation. Intra-articular varus or valgus deformity of the ankle can be corrected concomitantly with the TAA. In both cases, thorough removal of osteophytes should be performed, which can help with implantation of the TAA and decrease tension in the surrounding soft tissues. Minor attenuations in the lateral or medial ligamentous structures can be accommodated by increasing the UHMWPE liner thickness. The varus ankle may require medial release of the deltoid ligament for adequate correction. Alternatively, a medial malleolar osteotomy can be performed for a similar effect while preserving deltoid ligament bony attachments but requires internal fixation. 28 A varus ankle with a deficiency in the lateral ligamentous complex can be supplemented by a lateral ligament repair or reconstructive procedure in addition to the TAA. The valgus ankle is approached with similar principles. Classically a deltoid ligament deficiency in a valgus ankle was a contraindication for TAA. 26 However, deltoid advancement can be performed with sufficient residual tissue or formal allograft/autograft reconstructive procedures without 40 and thus surgeons should be ready to address this at time of TAA as needed or afterwards as a staged procedure. The intention is to maintain the medial restraint to talar alignment within the ankle mortise allowing congruent loading through the prosthesis. The deltoid is certainly important in TAA, such as in concomitant grade 4 posterior tibial tendon insufficiency, while the treatment is up for debate. 27
Results
First-generation TAAs had an unacceptably high failure rate 63,119,121 thought to be from the large bone resection required, poor ability to replicate ankle kinematics, and lack of understanding of soft tissue balancing and ankle alignment. 121 The Agility prosthesis (DePuy, Warsaw, IN) is the most commonly reported 2-component TAA but it was plagued with a high complication rate 23,80,110 despite having reasonable survival compared with other TAAs 95 and similar patient-reported outcomes. 74 Failure was often associated with a syndesmosis nonunion. 64 Newer designs, combined with a better understanding of foot deformity correction with TAA, 27,79 have led to improved clinical results and survival. The high variability in quality of the published data make interpretation of TAA results difficult. 131 Haddad et al in a systematic review reported a TAA 10-year survival of 77% whereas Brunner et al reported a Scandinavian TAA (STAR; Stryker, Mahwah, NJ) survival of 70.7% at 10 years and 45.6% at 14 years. 14 More recently, Daniels et al reported a 12% metal component revision rate with the STAR at a mean of 4.3 years. 25 Newer still is a 15-year reported metal-component survival of 63.6% to 73% 68,88 and 19-year survival of 55%. 37 Other implants showed similar results, such as the Salto Talaris with approximately 95% survival at 5 years. 52,111 The newer Infinity TAA (Wright Medical, Memphis, TN) has limited published data; short-term results are promising 92,100 but have been contested. 21 The benefits of a fixed bearing vs mobile bearing are unclear; one study comparing these 2 designs failed to show a difference. 39 Despite recent advances and understanding of ankle kinematics, TAA still does not normalize gait. 58
Comparing Arthrodesis to TAA
An early systematic review demonstrated similar outcomes between TAA and ankle arthrodesis. 45 However, the data then were not of high quality and the authors were unable to make strong conclusions. A paper by the COFAS group in 2014 reviewed 321 ankle arthritis cases treated with fusion or TAA with a mean follow-up of 5.5 years and showed similar outcome scores between the 2 procedures. However, TAA resulted in higher complication rate (7% arthrodesis vs 19% TAA) and reoperation rate (7% arthrodesis vs 17% TAA). 25 Newer literature demonstrated increased complications and reoperations with TAA compared with arthrodesis, but both achieved similar clinical outcomes. 62,77 Another study showed that TAA patients have improved motion, pain control, and perceived outcomes postoperatively. 91 However, both have poorer outcomes if swelling is significant. 129 Level I evidence for TAA compared with fusion is still lacking, and hence the justification for the in-progress multicenter randomized trial of total ankle replacement vs arthrodesis (TARVA) based in the United Kingdom. 43
Joint-Preservation Strategies
Aside from arthrodesis and TAA, there exists other recognized but less common surgical treatments. Joint preservation strategies are ideal for the younger population and have been of interest in the hip, knee, and ankle as an alternative to arthroplasty or arthrodesis. In the ankle, these include simple debridement, realignment osteotomies, distraction arthroplasty, and other less common procedures.
Joint debridement
The purpose of debridement in ankle arthritis is primarily removal of marginal impinging osteophytes to relieve both the impingement causing pain and associated stiffness in cases of mild arthritis. This treatment can be performed via open surgical approaches, but is frequently done arthroscopically with improved results. 105 The technique involves performing a diagnostic arthroscopy, identifying the impinging osteophytes, and removal with burrs, curettes, and rongeurs. Impingement can be a result of malalignment, and in these cases, consideration should be given to correction of this malalignment in addition to addressing the osteophytes, such as in planovalgus deformities. Debridement is not appropriate for moderate or severe cases of arthritis; by removing osteophytes and increasing range of motion through arthritic articular surfaces, this can cause increased pain and poor outcomes. 4,85
Realignment osteotomies
In patients with ankle arthritis affecting only a portion of the joint surface, realignment of the mechanical axis such that weight-bearing shifts to the preserved portion of the joint can be performed with osteotomies. The ideal candidate is a younger, active individual who does not want a joint-sacrificing procedure such as fusion or arthroplasty. Conceptually, this is akin to the high tibial osteotomy for varus knee medial osteoarthritis to preferentially load a preserved lateral compartment. Physical examination findings can suggest a role for realignment prior to any imaging. For example, a planovalgus deformity with tenderness in the lateral gutter and sinus tarsi is consistent with a valgus pattern of ankle arthritis and possible preservation of the medial side of the joint. If this diagnosis is confirmed on imaging, realignment surgery may be possible instead of ankle fusion or replacement. The obvious prerequisite is eccentric wear with some remaining articular cartilage to load through after realignment, ideally 50% or more. 51 In cases of underlying foot deformity and asymmetrical ankle arthritis, such as a planovalgus foot with primarily lateral ankle arthritis or cavovarus foot with primarily medial ankle arthritis, correction of the foot deformity may also realign the mechanical axis enough to relieve pain. The commonly reported supramalleolar osteotomy is a powerful technique that affords a higher degree of angular correction for this purpose as it occurs more proximally and can be done in combination with foot deformity correction. The end goal is to restore neutral talar alignment within the mortise both in the sagittal and coronal planes, and slight overcorrection is sometimes advocated. 51 In varus ankle arthritis, a medial opening wedge osteotomy with bone graft is typically done, although a lateral closing wedge osteotomy is also an option. Similarly, valgus ankle arthritis can be treated with medial closing wedge supramalleolar osteotomies or lateral opening wedge osteotomies. In either case, fixation is usually with plates and screws but external fixation is also an option, and deformity correction can be done with adjustable ring fixator systems. Angular corrections over 10 degrees may require concomitant fibular osteotomies, 7 and large opening wedge osteotomies will cause lengthening. One must be cautious of lengthening to the surrounding soft tissues such as tendons and nerves, and dome osteotomies should be considered instead to minimize this. Many series have been published with good results. 6,67,86,116 This technique has potential use with appropriate patient selection, but current literature is still insufficient to recommend broadly. 70
Distraction arthroplasty
This technique involves the application of a ring external fixator to the ankle to apply distraction across the tibiotalar joint to unload it, relieving pain and possibly delay or reverse osteoarthritis. 10 The frame can be fixed but is usually hinged at the ankle to allow motion, and the patient is permitted to weight bear. 70 The ideal candidate is one who is not suitable for other joint-preservation techniques, but does not want joint-sacrificing surgery such as fusion or arthroplasty. Indications and technique are well described, 10 but the mechanism of action is still unclear, results confounded by concomitant procedures, and scientific evidence to support its general use in ankle arthritis is insufficient, according to several reviews. 10,70,108
Other procedures
There has been some interest in other even less common procedures, such as interpositional arthroplasty and osteochondral allograft transplantation, but current evidence is lacking to recommend them. 70
Conclusion
Although less common than that of the hip or knee, ankle arthritis is a significant disease of variable etiology affecting a younger working-age group with an increasing number of reliable surgical and nonsurgical treatments. Proper treatment of these conditions depends on meticulous patient evaluation both of the ankle pathology as well as systemic medical issues and lower limb alignment. The invasive nature of surgical treatments warrant exhausting nonoperative measures first and delaying the index procedure. However, failure of nonsurgical treatments would merit surgery in an appropriate candidate. Arthroscopic ankle arthrodesis, although still less commonly performed in the United States compared with open techniques, can be the superior fusion technique in experienced hands in patients with limited coronal plane deformity because of its inherent minimally invasive nature. In the future, more durable TARs may allow usage in younger patients in addition to the gold standard of ankle arthrodesis for end-stage ankle arthritis. Better understanding of ankle anatomy and biomechanics may increase the prevalence of joint-preservation techniques such as supramalleolar osteotomy in this unique population.
Supplemental Material
Supplemental Material, FAO852931-ICMJE for Ankle Arthritis by Vu Le, Andrea Veljkovic, Peter Salat, Kevin Wing, Murray Penner and Alastair Younger in Foot & Ankle Orthopaedics
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Vu Le, MD, FRCSC, reports personal fees from Purdue Pharma (Canada), outside the submitted work. Andrea Veljkovic, MD, MPH, FRCSC, reports grants from Acumed, from AIC, from Therapia, personal fees from Arthrex, grants from Zimmer, outside the submitted work. Kevin Wing, MD, FRCSC, reports grants from Acumed, grants and personal fees from Wright medical, grants from Ferring, grants from Zimmer, grants from Synthes, grants from Bioventus, outside the submitted work. Murray Penner, MD, FRCSC, reports grants and personal fees from Wright medical, grants from Zimmer, grants from Synthes, grants and personal fees from Springer, grants from Arthrex, other from Cdn. Orthop. Foot & Ankle society, other from Intl. Federation of Foot & Ankle societies, outside the submitted work. Alastair Younger, MB, ChB, MSc, ChM, FRCSC, reports grants and personal fees from Acumed, grants and personal fees from Wright medical, grants and personal fees from Ferring, grants and personal fees from Zimmer, grants from Synthes, grants and personal fees from Bioventus, outside the submitted work. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Vu Le, MD, FRCSC,  https://orcid.org/0000-0003-1625-4200
https://orcid.org/0000-0003-1625-4200
References
- 1. Agel J, Coetzee JC, Sangeorzan BJ, Roberts MM, Hansen ST. Functional limitations of patients with end-stage ankle arthrosis. Foot Ankle Int. 2005;26(7):537–539. [DOI] [PubMed] [Google Scholar]
- 2. Al-Ashhab ME. Primary ankle arthrodesis for severely comminuted tibial pilon fractures. Orthopedics. 2017;40(2):e378–e381. [DOI] [PubMed] [Google Scholar]
- 3. Albert E. Zur resection des kniegelenkes [For the resection of the knee joint]. Wien Med Press. 1879;20:705–708. [Google Scholar]
- 4. Amendola A, Petrik J, Webster-Bogaert S. Ankle arthroscopy: outcome in 79 consecutive patients. Arthroscopy. 1996;12(5):565–573. [DOI] [PubMed] [Google Scholar]
- 5. Balaji S, Selvaraj V, Devadoss S, Devadoss A. Transfibular ankle arthrodesis: a novel method for ankle fusion—a short term retrospective study. Indian J Orthop. 2017;51(1):75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Barg A, Barg K, Schneider SW, et al. Thrombembolic complications after total ankle replacement. Curr Rev Musculoskelet Med. 2013;6(4):328–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barg A, Pagenstert GI, Horisberger M, et al. Supramalleolar osteotomies for degenerative joint disease of the ankle joint: indication, technique and results. Int Orthop. 2013;37(9):1683–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baumhauer JF, Pinzur MS, Daniels TR, et al. Survey on the need for bone graft in foot and ankle fusion surgery. Foot Ankle Int. 2013;34(12):1629–1633. [DOI] [PubMed] [Google Scholar]
- 9. Bek D, Demiralp B, Kürklü M, Ateşşalp AS, Başşbozkurt M. Ankle arthrodesis using an Ilizarov external fixator in patients wounded by landmines and gunshots. Foot Ankle Int. 2008;29(2):178–184. [DOI] [PubMed] [Google Scholar]
- 10. Bernstein M, Reidler J, Fragomen A, Rozbruch SR. Ankle distraction arthroplasty: indications, technique, and outcomes. J Am Acad Orthop Surg. 2017;25(2):89–99. [DOI] [PubMed] [Google Scholar]
- 11. Bluth BE, Fong YJ, Houman JJ, Silva M, Luck JV. Ankle fusion in patients with haemophilia. Haemophilia. 2013;19(3):432–437. [DOI] [PubMed] [Google Scholar]
- 12. Braly WG, Baker JK, Tullos HS. Arthrodesis of the ankle with lateral plating. Foot Ankle Int. 1994;15(12):649–653. [DOI] [PubMed] [Google Scholar]
- 13. Brodsky JW, Kane JM, Coleman S, Bariteau J, Tenenbaum S. Abnormalities of gait caused by ankle arthritis are improved by ankle arthrodesis. Bone Joint J. 2016;98-B(10):1369–1375. [DOI] [PubMed] [Google Scholar]
- 14. Brunner S, Barg A, Knupp M, et al. The Scandinavian total ankle replacement: long-term, eleven to fifteen-year, survivorship analysis of the prosthesis in seventy-two consecutive patients. J Bone Joint Surg Am. 2013;95(8):711–718. [DOI] [PubMed] [Google Scholar]
- 15. Budnar VM, Hepple S, Harries WG, Livingstone JA, Winson I. Tibiotalocalcaneal arthrodesis with a curved, interlocking, intramedullary nail. Foot Ankle Int. 2010;31(12):1085–1092. [DOI] [PubMed] [Google Scholar]
- 16. Cannon LB, Brown J, Cooke PH. Early weight bearing is safe following arthroscopic ankle arthrodesis. Foot Ankle Surg. 2004;10(3):135–139. [Google Scholar]
- 17. Carroll GJ, Breidahl WH, Bulsara MK, Olynyk JK. Hereditary hemochromatosis is characterized by a clinically definable arthropathy that correlates with iron load. Arthritis Rheum. 2011;63(1):286–294. [DOI] [PubMed] [Google Scholar]
- 18. Charnley J. Compression arthrodesis of the ankle and shoulder. J Bone Joint Surg Br. 1951;33(2):180–191. [PubMed] [Google Scholar]
- 19. Choi WJ, Kim BS, Lee JW. Preoperative planning and surgical technique: how do I balance my ankle? Foot Ankle Int. 2012;33(3):244–249. [DOI] [PubMed] [Google Scholar]
- 20. Clare MP, Sanders RW. The anatomic compression arthrodesis technique with anterior plate augmentation for ankle arthrodesis. Foot Ankle Clin. 2011;16(1):91–101. [DOI] [PubMed] [Google Scholar]
- 21. Cody EA, Taylor MA, Nunley JA, Parekh SG, DeOrio JK. Increased early revision rate with the INFINITY total ankle prosthesis. Foot Ankle Int. 2019;40(1):9–17. [DOI] [PubMed] [Google Scholar]
- 22. Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am. 2001;83(2):219–228. [DOI] [PubMed] [Google Scholar]
- 23. Conti SF, Wong YS. Complications of total ankle replacement. Foot Ankle Clin. 2002;7(4):791–807, vii. [DOI] [PubMed] [Google Scholar]
- 24. Cushnaghan J, Dieppe P. Study of 500 patients with limb joint osteoarthritis, I: Analysis by age, sex, and distribution of symptomatic joint sites. Ann Rheum Dis. 1991;50(1):8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Daniels TR, Younger ASE, Penner M, et al. Intermediate-term results of total ankle replacement and ankle arthrodesis: a COFAS multicenter study. J Bone Joint Surg Am. 2014;96(2):135–142. [DOI] [PubMed] [Google Scholar]
- 26. Deorio JK, Easley ME. Total ankle arthroplasty. Instr Course Lect. 2008;57(2):383–413. [PubMed] [Google Scholar]
- 27. Dodd A, Daniels TR. Total ankle replacement in the presence of talar varus or valgus deformities. Foot Ankle Clin. 2017;22(2):277–300. [DOI] [PubMed] [Google Scholar]
- 28. Doets HC, van der Plaat LW, Klein JP. Medial malleolar osteotomy for the correction of varus deformity during total ankle arthroplasty: results in 15 ankles. Foot Ankle Int. 2008;29(2):171–177. [DOI] [PubMed] [Google Scholar]
- 29. Dohm MP, Benjamin JB, Harrison J, Szivek JA. A biomechanical evaluation of three forms of internal fixation used in ankle arthrodesis. Foot Ankle Int. 1994;15(6):297–300. [DOI] [PubMed] [Google Scholar]
- 30. Dorsey ML, Liu PT, Roberts CC, Kile TA. Correlation of arthrodesis stability with degree of joint fusion on MDCT. Am J Roentgenol. 2009;192(2):496–499. [DOI] [PubMed] [Google Scholar]
- 31. Ellis SJ, Deyer T, Williams BR, et al. Assessment of lateral hindfoot pain in acquired flatfoot deformity using weightbearing multiplanar imaging. Foot Ankle Int. 2010;31(5):361–371. [DOI] [PubMed] [Google Scholar]
- 32. Eloesser L. Implantation of joints. Cal State J Med. 1913;11(12):485–491. [PMC free article] [PubMed] [Google Scholar]
- 33. Eylon S, Porat S, Bor N, Leibner ED. Outcome of Ilizarov ankle arthrodesis. Foot Ankle Int. 2007;28(8):873–879. [DOI] [PubMed] [Google Scholar]
- 34. Ferkel RD, Hewitt M. Long-term results of arthroscopic ankle arthrodesis. Foot Ankle Int. 2005;26(4):275–280. [DOI] [PubMed] [Google Scholar]
- 35. Fitzgibbons TC. Arthroscopic ankle debridement and fusion: indications, techniques, and results. Instr Course Lect. 1999;48:243–248. [PubMed] [Google Scholar]
- 36. Fragomen AT, Borst E, Schachter L, Lyman S, Rozbruch SR. Complex ankle arthrodesis using the Ilizarov method yields high rate of fusion foot and ankle. Clin Orthop Relat Res. 2012;470(10):2864–2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Frigg A, Germann U, Huber M, Horisberger M. Survival of the Scandinavian Total Ankle Replacement (STAR): results of ten to nineteen years follow-up. Int Orthop. 2017;41(10):2075–2082. [DOI] [PubMed] [Google Scholar]
- 38. Gagné OJ, Veljkovic A, Glazebrook M, et al. Prospective cohort study on the employment status of working age patients after recovery from ankle arthritis surgery. Foot Ankle Int. 2018;39(6):657–663. [DOI] [PubMed] [Google Scholar]
- 39. Gaudot F, Colombier JA, Bonnin M, Judet T. A controlled, comparative study of a fixed-bearing versus mobile-bearing ankle arthroplasty. Foot Ankle Int. 2014;35(2):131–140. [DOI] [PubMed] [Google Scholar]
- 40. Gauvain TT, Hames MA, McGarvey WC. Malalignment correction of the lower limb before, during, and after total ankle arthroplasty. Foot Ankle Clin. 2017;22(2):311–339. [DOI] [PubMed] [Google Scholar]
- 41. Glazebrook M, Beasley W, Daniels T, et al. Establishing the relationship between clinical outcome and extent of osseous bridging between computed tomography assessment in isolated hindfoot and ankle fusions. Foot Ankle Int. 2013;34(12):1612–1618. [DOI] [PubMed] [Google Scholar]
- 42. Glazebrook M, Daniels T, Younger A, et al. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J Bone Joint Surg Am. 2008;90(3):499–505. [DOI] [PubMed] [Google Scholar]
- 43. Goldberg AJ, Zaidi R, Thomson C, et al. Total Ankle Replacement Versus Arthrodesis (TARVA): protocol for a multicentre randomised controlled trial. BMJ Open. 2016;6(9):e012716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gougoulias N, Maffulli N. History of total ankle replacement. Clin Podiatr Med Surg. 2013;30(1):1–20. [DOI] [PubMed] [Google Scholar]
- 45. Haddad SL, Coetzee JC, Estok R, Fahrbach K, Banel D, Nalysnyk L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis: a systematic review of the literature. J Bone Joint Surg Am. 2007;89(9):1899. [DOI] [PubMed] [Google Scholar]
- 46. Haskell A, Mann RA. Ankle arthroplasty with preoperative coronal plane deformity: short-term results. Clin Orthop Relat Res. 2004;424:98–103. [DOI] [PubMed] [Google Scholar]
- 47. Hawkins BJ, Langerman RJ, Anger DM, Calhoun JH. The Ilizarov technique in ankle fusion. Clin Orthop Relat Res. 1994;303;217–225. [PubMed] [Google Scholar]
- 48. Hayes BJ, Gonzalez T, Smith JT, Chiodo CP, Bluman EM. Ankle arthritis: you can’t always replace it. J Am Acad Orthop Surg. 2016;24(2):29–38. [DOI] [PubMed] [Google Scholar]
- 49. Haygood TM. Magnetic resonance imaging of the musculoskeletal system: part 7. The ankle. Clin Orthop Relat Res. 1997;336:318–336. [DOI] [PubMed] [Google Scholar]
- 50. Helm R. The results of ankle arthrodesis. J Bone Jt Surg Br. 1990;72(1):141–143. [DOI] [PubMed] [Google Scholar]
- 51. Hintermann B, Knupp M, Barg A. Supramalleolar osteotomies for the treatment of ankle arthritis. J Am Acad Orthop Surg. 2016;24(7):424–432. [DOI] [PubMed] [Google Scholar]
- 52. Hofmann KJ, Shabin ZM, Ferkel E, Jockel J, Slovenkai MP. Salto talaris total ankle arthroplasty clinical results at a mean of 5.2 years in 78 patients treated by a single surgeon. J Bone Joint Surg Am. 2016;98(24):2036–2046. [DOI] [PubMed] [Google Scholar]
- 53. Holt ES, Hansen ST, Mayo KA, Sangeorzan BJ. Ankle arthrodesis using internal screw fixation. Clin Orthop Relat Res. 1991;268:21–28. [PubMed] [Google Scholar]
- 54. Honnenahalli Chandrappa M, Hajibandeh S, Hajibandeh S. Ankle arthrodesis—open versus arthroscopic: a systematic review and meta-analysis. J Clin Orthop Trauma. 2017;8(suppl 2):S71–S77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Johnson EE, Weltmer J, Lian GJ, Cracchiolo A. Ilizarov ankle arthrodesis. Clin Orthop Relat Res. 1992;280:160–169. [PubMed] [Google Scholar]
- 56. Jones CR, Wong E, Applegate GR, Ferkel RD. Arthroscopic ankle arthrodesis: a 2-15 year follow-up study. Arthroscopy. 2018;34(5):1641–1649. [DOI] [PubMed] [Google Scholar]
- 57. Kamrad I, Henricson A, Magnusson H, Carlsson Å, Rosengren BE. Outcome after salvage arthrodesis for failed total ankle replacement. Foot Ankle Int. 2016;37(3):255–261. [DOI] [PubMed] [Google Scholar]
- 58. Kane JM, Coleman S, Brodsky JW. Kinematics and function of total ankle replacements versus normal ankles. Foot Ankle Clin. 2017;22(2):241–249. [DOI] [PubMed] [Google Scholar]
- 59. Kendal AR, Cooke P, Sharp R. Arthroscopic ankle fusion for avascular necrosis of the talus. Foot Ankle Int. 2015;36(5):591–597. [DOI] [PubMed] [Google Scholar]
- 60. Kerkhoff YRA, Keijsers NLW, Louwerens JWK. Sports participation, functional outcome, and complications after ankle arthrodesis: midterm follow-up. Foot Ankle Int. 2017;38(10):1085–1091. [DOI] [PubMed] [Google Scholar]
- 61. Kim BS, Choi WJ, Kim YS, Lee JW. Total ankle replacement in moderate to severe varus deformity of the ankle. J Bone Joint Surg Br. 2009;91(9):1183–1190. [DOI] [PubMed] [Google Scholar]
- 62. Kim HJ, Suh DH, Yang JH, et al. Total ankle arthroplasty versus ankle arthrodesis for the treatment of end-stage ankle arthritis: a meta-analysis of comparative studies. Int Orthop. 2017;41(1):101–109. [DOI] [PubMed] [Google Scholar]
- 63. Kitaoka HB, Patzer GL, Ilstrup DM, Wallrichs SL. Survivorship analysis of the Mayo total ankle arthroplasty. J Bone Joint Surg Am. 1994;76(7):974–979. [DOI] [PubMed] [Google Scholar]
- 64. Knecht SI, Estin M, Callaghan JJ, et al. The Agility total ankle arthroplasty: seven to sixteen-year follow-up. J Bone Joint Surg Am. 2004;86(6):1161–1171. [PubMed] [Google Scholar]
- 65. Knupp M, Ledermann H, Magerkurth O, Hinterman B. The surgical tibiotalar angle: a radiologic study. Foot Ankle Int. 2005;26(9):713–716. [DOI] [PubMed] [Google Scholar]
- 66. Knupp M, Pagenstert GI, Barg A, Bolliger L, Easley ME, Hintermann B. SPECT-CT compared with conventional imaging modalities for the assessment of the varus and valgus malaligned hindfoot. J Orthop Res. 2009;27(11):1461–1466. [DOI] [PubMed] [Google Scholar]
- 67. Knupp M, Stufkens SAS, Bolliger L, Barg A, Hintermann B. Classification and treatment of supramalleolar deformities. Foot Ankle Int. 2011;32(11):1023–1031. [DOI] [PubMed] [Google Scholar]
- 68. Koivu H, Kohonen I, Mattila K, Loyttyniemi E, Tiusanen H. Long-term results of scandinavian total ankle replacement. Foot Ankle Int. 2017;38(7):723–731. [DOI] [PubMed] [Google Scholar]
- 69. Krause FG, Di Silvestro M, Penner MJ, et al. The postoperative COFAS end-stage ankle arthritis classification system: interobserver and intraobserver reliability. Foot Ankle Spec. 2012;5(1):31–36. [DOI] [PubMed] [Google Scholar]
- 70. Labib SA, Raikin SM, Lau JT, et al. Joint preservation procedures for ankle arthritis. Foot Ankle Int. 2013;34(7):1040–1047. [DOI] [PubMed] [Google Scholar]
- 71. Lee BH, Fang C, Kunnasegaran R, Thevendran G. Tibiotalocalcaneal arthrodesis with the hindfoot arthrodesis nail: a prospective consecutive series from a single institution. J Foot Ankle Surg. 2018;57(1):23–30. [DOI] [PubMed] [Google Scholar]
- 72. Lee HJ, Min WK, Kim JS, Yoon SD, Kim DH. Transfibular ankle arthrodesis using burring, curettage, multiple drilling, and fixation with two retrograde screws through a single lateral incision. J Orthop Surg. 2016;24(1):101–105. [DOI] [PubMed] [Google Scholar]
- 73. de Leeuw PAJ, Hendrickx RPM, van Dijk CN, Stufkens SS, Kerkhoffs GMMJ. Midterm results of posterior arthroscopic ankle fusion. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1326–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Lefrancois T, Younger A, Wing K, et al. A prospective study of four total ankle arthroplasty implants by non-designer investigators. J Bone Joint Surg Am. 2017;99(4):342–348. [DOI] [PubMed] [Google Scholar]
- 75. Lin SS, Montemurro NJ, Krell ES. Orthobiologics in foot and ankle surgery. J Am Acad Orthop Surg. 2016;24(2):113–122. [DOI] [PubMed] [Google Scholar]
- 76. Lynch AF, Bourne RB, Rorabeck CH. The long-term results of ankle arthrodesis. J Bone Joint Surg Br. 1988;70(1):113–116. [DOI] [PubMed] [Google Scholar]
- 77. Maffulli N, Longo UG, Locher J, Romeo G, Salvatore G, Denaro V. Outcome of ankle arthrodesis and ankle prosthesis: a review of the current status. Br Med Bull. 2017;124(1):91–112. [DOI] [PubMed] [Google Scholar]
- 78. Mann RA, Van Manen JW, Wapner K, Martin J. Ankle fusion. Clin Orthop Relat Res. 1991;268(July):49–55. [PubMed] [Google Scholar]
- 79. Mayich DJ, Daniels TR. Total ankle replacement in ankle arthritis with varus talar deformity: pathophysiology, evaluation, and management principles. Foot Ankle Clin. 2012;17(1):127–139. [DOI] [PubMed] [Google Scholar]
- 80. McCollum G, Myerson MS. Failure of the agility total ankle replacement system and the salvage options. Clin Podiatr Med Surg. 2013;30(2):207–223. [DOI] [PubMed] [Google Scholar]
- 81. Miller SD, Paremain GP, Myerson MS. The miniarthrotomy technique of ankle arthrodesis: a cadaver study of operative vascular compromise and early clinical results. Orthopedics. 1996;19(5):425–430. [DOI] [PubMed] [Google Scholar]
- 82. Myerson MS, Quill G. Ankle arthrodesis. A comparison of an arthroscopic and an open method of treatment. Clin Orthop Relat Res. 1991;268:84–95. [PubMed] [Google Scholar]
- 83. Nielsen KK, Linde F, Jensen NC. The outcome of arthroscopic and open surgery ankle arthrodesis. A comparative retrospective study on 107 patients. Foot Ankle Surg. 2008;14(3):153–157. [DOI] [PubMed] [Google Scholar]
- 84. Ogilvie-Harris DJ, Fitsialos D, Hedman TP. Arthrodesis of the ankle. A comparison of two versus three screw fixation in a crossed configuration. Clin Orthop Relat Res. 1994;304:195–199. [PubMed] [Google Scholar]
- 85. Ogilvie-Harris DJ, Sekyi-Otu A. Arthroscopic debridement for the osteoarthritic ankle. Arthroscopy. 1995;11(4):433–436. [DOI] [PubMed] [Google Scholar]
- 86. Pagenstert G, Knupp M, Valderrabano V, Hintermann B. Realignment surgery for valgus ankle osteoarthritis. Oper Orthop Traumatol. 2009;21(1):77–87. [DOI] [PubMed] [Google Scholar]
- 87. Pagenstert GI, Barg A, Leumann AG, et al. SPECT-CT imaging in degenerative joint disease of the foot and ankle. J Bone Joint Surg Br. 2009;91(9):1191–1196. [DOI] [PubMed] [Google Scholar]
- 88. Palanca A, Mann RA, Mann JA, Haskell A. Scandinavian total ankle replacement: 15-year follow-up. Foot Ankle Int. 2018;39(2):135–142. [DOI] [PubMed] [Google Scholar]
- 89. Paremain GD, Miller SD, Myerson MS. Ankle arthrodesis: results after the miniarthrotomy technique. Foot Ankle Int. 1996;17(5):247–252. [DOI] [PubMed] [Google Scholar]
- 90. Park JH, Kim HJ, Suh DH, et al. Arthroscopic versus open ankle arthrodesis: a systematic review. Arthroscopy. 2017;34(3):988–997. [DOI] [PubMed] [Google Scholar]
- 91. Pedowitz DI, Kane JM, Smith GM, Saffel HL, Comer C, Raikin SM. Total ankle arthroplasty versus ankle arthrodesis: a comparative analysis of arc of movement and functional outcomes. Bone Joint J. 2016;98(5):634–640. [DOI] [PubMed] [Google Scholar]
- 92. Penner M, Davis WH, Wing K, Bemenderfer T, Waly F, Anderson RB. The infinity total ankle system: early clinical results with 2- to 4-year follow-up. Foot Ankle Spec. 2019;12(2):159–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Quayle J, Shafafy R, Khan MA, Ghosh K, Sakellariou A, Gougoulias N. Arthroscopic versus open ankle arthrodesis. Foot Ankle Surg. 2018;24(2):137–142. [DOI] [PubMed] [Google Scholar]
- 94. Raikin SM, Rasouli MR, Espandar R, Maltenfort MG. Trends in treatment of advanced ankle arthropathy by total ankle replacement or ankle fusion. Foot Ankle Int. 2014;35(3):216–224. [DOI] [PubMed] [Google Scholar]
- 95. Raikin SM, Sandrowski K, Kane JM, Beck D, Winters BS. Midterm outcome of the agility total ankle arthroplasty. Foot Ankle Int. 2017;38(6):662–670. [DOI] [PubMed] [Google Scholar]
- 96. Rammelt S, Pyrc J, Ågren PH, et al. Tibiotalocalcaneal fusion using the hindfoot arthrodesis nail: a multicenter study. Foot Ankle Int. 2013;34(9):1245–1255. [DOI] [PubMed] [Google Scholar]
- 97. Reb CW, Berlet GC. Experience with navigation in total ankle arthroplasty. Is it worth the cost? Foot Ankle Clin. 2017;22(2):455–463. [DOI] [PubMed] [Google Scholar]
- 98. Reddy SC, Mann JA, Mann RA, Mangold DR. Correction of moderate to severe coronal plane deformity with the STARTM ankle prosthesis. Foot Ankle Int. 2011;32(7):659–664. [DOI] [PubMed] [Google Scholar]
- 99. Rowan R, Davey KJ. Ankle arthrodesis using an anterior AO T plate. J Bone Joint Surg Am. 1999;81(1):113–116. [DOI] [PubMed] [Google Scholar]
- 100. Saito GH, Sanders AE, de Cesar Netto C, O’Malley MJ, Ellis SJ, Demetracopoulos CA. Short-term complications, reoperations, and radiographic outcomes of a new fixed-bearing total ankle arthroplasty. Foot Ankle Int. 2018;39(7):787–794. [DOI] [PubMed] [Google Scholar]
- 101. Saltzman CL, El-Khoury GY. The hindfoot alignment view. Foot Ankle Int. 1995;16(9):572–576. [DOI] [PubMed] [Google Scholar]
- 102. Saltzman CL, Salamon ML, Blanchard GM, et al. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44–46. [PMC free article] [PubMed] [Google Scholar]
- 103. Schmid T, Krause F, Penner MJ, Veljkovic A, Younger ASE, Wing K. Effect of preoperative deformity on arthroscopic and open ankle fusion outcomes. Foot Ankle Int. 2017;38(12):1301–1310. [DOI] [PubMed] [Google Scholar]
- 104. Scranton PE, Fu FH, Brown TD. Ankle arthrodesis: a comparative clinical and biomechanical evaluation. Clin Orthop Relat Res. 1980;151:234–243. [PubMed] [Google Scholar]
- 105. Scranton PE, McDermott JE. Anterior tibiotalar spurs: a comparison of open versus arthroscopic debridement. Foot Ankle. 1992;13(3):125–129. [DOI] [PubMed] [Google Scholar]
- 106. Senay A, Trottier M, Delisle J, et al. Incidence of symptomatic venous thromboembolism in 2372 knee and hip replacement patients after discharge: data from a thromboprophylaxis registry in Montreal, Canada. Vasc Health Risk Manag. 2018;14:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Smith JT, Chiodo CP, Singh SK, Wilson MG. Open ankle arthrodesis with a fibular-sparing technique. Foot Ankle Int. 2013;34(4):557–562. [DOI] [PubMed] [Google Scholar]
- 108. Smith NC, Beaman D, Rozbruch SR, Glazebrook MA. Evidence-based indications for distraction ankle arthroplasty. Foot Ankle Int. 2012;33(8):632–636. [DOI] [PubMed] [Google Scholar]
- 109. Sowa DT, Krackow KA. Ankle fusion: a new technique of internal fixation using a compression blade plate. Foot Ankle. 1989;9(5):232–240. [DOI] [PubMed] [Google Scholar]
- 110. Spirt AA, Assal M, Hansen ST. Complications and failure after total ankle arthroplasty. J Bone Joint Surg Am. 2004;86(6):1172–1178. [DOI] [PubMed] [Google Scholar]
- 111. Stewart MG, Green CL, Adams SB, DeOrio JK, Easley ME, Nunley JA. Midterm results of the salto talaris total ankle arthroplasty. Foot Ankle Int. 2017;38(11):1215–1221. [DOI] [PubMed] [Google Scholar]
- 112. Stiehl JB, Dollinger B. Primary ankle arthrodesis in trauma: report of three cases. J Orthop Trauma. 1988;2(4):277–283. [DOI] [PubMed] [Google Scholar]
- 113. Stufkens SA, Barg A, Bolliger L, Stucinskas J, Knupp M, Hintermann B. Measurement of the medial distal tibial angle. Foot Ankle Int. 2011;32(3):288–293. [DOI] [PubMed] [Google Scholar]
- 114. Sung W, Greenhagen RM, Hobizal KB, Burns PR, Wukich DK. Technical guide: transfibular ankle arthrodesis with fibular-onlay strut graft. J Foot Ankle Surg. 2010;49(6):566–570. [DOI] [PubMed] [Google Scholar]
- 115. Syed F, Ugwuoke A. Ankle arthroplasty. EFORT Open Rev. 2018;3(6):391–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Takakura Y, Takaoka T, Tanaka Y, Yajima H, Tamai S. Results of opening-wedge osteotomy for the treatment of a post-traumatic varus deformity of the ankle. J Bone Joint Surg Am. 1998;80(2):213–218. [DOI] [PubMed] [Google Scholar]
- 117. Takakura Y, Tanaka Y, Sugimoto K, Akiyama K, Tamai S. Long-term results of arthrodesis for osteoarthritis of the ankle. Clin Orthop Relat Res. 1999;361:178–185. [DOI] [PubMed] [Google Scholar]
- 118. Tarkin IS, Mormino MA, Clare MP, Haider H, Walling AK, Sanders RW. Anterior plate supplementation increases ankle arthrodesis construct rigidity. Foot Ankle Int. 2007;28(2):219–223. [DOI] [PubMed] [Google Scholar]
- 119. Thermann H, Hufner T, Roehler A, Tscherne H. Screw arthrodesis of the ankle joint. Technique and outcome [in German]. Orthopade. 1996;25(2):166–176. [PubMed] [Google Scholar]
- 120. Thevendran G, Wang C, Pinney SJ, Penner MJ, Wing KJ, Younger ASE. Nonunion risk assessment in foot and ankle surgery. Foot Ankle Int. 2015;36(8):901–907. [DOI] [PubMed] [Google Scholar]
- 121. Thomas RH, Daniels TR. Ankle arthritis. J Bone Joint Surg Am. 2003;85(5):923–936. [DOI] [PubMed] [Google Scholar]
- 122. Townshend D, Di Silvestro M, Krause F, et al. Arthroscopic versus open ankle arthrodesis: a multicenter comparative case series. J Bone Joint Surg Am. 2013;95(2):98–102. [DOI] [PubMed] [Google Scholar]
- 123. Trumble TE, Salas P, Barthel T, Robert KQ. Management of scaphoid nonunions. J Am Acad Orthop Surg. 2003;11(6):380–391. [DOI] [PubMed] [Google Scholar]
- 124. Ward ST, Williams PL, Purkayastha S. Intra-articular corticosteroid injections in the foot and ankle: a prospective 1-year follow-up investigation. J Foot Ankle Surg. 2008;47(2):138–144. [DOI] [PubMed] [Google Scholar]
- 125. Wiewiorski M, Barg A, Schlemmer T, Valderrabano V. Ankle joint fusion with an anatomically preshaped anterior locking plate. J Foot Ankle Surg. 2016;55(2):414–417. [DOI] [PubMed] [Google Scholar]
- 126. Wiewiorski M, Hoechel S, Anderson AE, et al. Computed tomographic evaluation of joint geometry in patients with end-stage ankle osteoarthritis. Foot Ankle Int. 2016;37(6):644–651. [DOI] [PubMed] [Google Scholar]
- 127. Witteveen AG, Hofstad CJ, Kerkhoffs GM. Hyaluronic acid and other conservative treatment options for osteoarthritis of the ankle. Cochrane Database Syst Rev. 2015;10:CD010643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Yasui Y, Hannon CP, Seow D, Kennedy JG. Ankle arthrodesis: a systematic approach and review of the literature. World J Orthop. 2016;7(11):700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Younger AS, Daniels TR, Wing K, et al. Swelling results in poor outcome after ankle arthritis surgery. Foot Ankle Orthop. 2016;1(1):1-1. doi: 10.1177/2473011416S00285. [Google Scholar]
- 130. Younger ASE, Glazebrook M, Veljkovic A, et al. A coding system for reoperations following total ankle replacement and ankle arthrodesis. Foot Ankle Int. 2016;37(11):1157–1164. [DOI] [PubMed] [Google Scholar]
- 131. Zaidi R, Cro S, Gurusamy K, et al. The outcome of total ankle replacement: a systematic review and meta-analysis. Bone Joint J. 2013;95B(11):1500–1507. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO852931-ICMJE for Ankle Arthritis by Vu Le, Andrea Veljkovic, Peter Salat, Kevin Wing, Murray Penner and Alastair Younger in Foot & Ankle Orthopaedics