Abstract
Central nervous system (CNS) infections are rare diseases that are associated with considerable morbidity and mortality. Increased knowledge based on contemporary data is a prerequisite for improved management and prevention of these serious conditions. Yet, population-based databases of patients hospitalized with CNS infections remain scarce. The Danish Study Group of Infections of the Brain (DASGIB) has prospectively registered information on all adults ≥18 years of age admitted with CNS infections at departments of infectious diseases in Denmark since 2015. The main variables collected are baseline demographics, blood and cerebrospinal fluid tests, imaging results, and outcome using the Glasgow Outcome Scale score. To investigate important aspects for each type of CNS infections, additional variables are included specifically for bacterial meningitis, viral meningitis, encephalitis, brain abscess, neurosyphilis, and Lyme neuroborreliosis. From 2015 to 2020, a total of 3579 cases of CNS infections have been recorded in the DASGIB database. Using the unique civil registration number assigned to all Danish residents, the database can be unambiguously linked with nationwide healthcare registries at the individual level. This enables researchers to conduct detailed population-based and longitudinal observational studies of risk and prognosis of CNS infections and to compare them with matched population cohorts. The database is well-suited for epidemiological research and the DASGIB network forms a solid infrastructure for future national and international collaborations.
Keywords: CNS infections, epidemiology, database, cohort studies, bacterial meningitis, viral meningitis, encephalitis, brain abscess, cerebral abscess, neurosyphilis, syphilis, Lyme neuroborreliosis, borreliosis
Introduction
Infections of the central nervous system (CNS) may be caused by an abundance of different pathogens including bacteria, virus, fungi, and parasites.1,2 Accordingly, the clinical spectrum of disease is wide and ranges from self-limiting viral meningitis to medical emergencies such as bacterial meningitis requiring immediate treatment. The microorganisms may enter the CNS by direct invasion or by hematogenous spread. Key factors for evasion of host defense mechanisms involve defects in neuroanatomical barriers, pathogen virulence factors, and presence of immuno-compromising conditions.
The clinical presentation and prognosis of CNS infections has been examined in several high-quality cohort studies and databases, which have provided us with valuable knowledge.3–15 However, the majority of studies in CNS infections are still limited by retrospective design and small sample sizes, or they may have relied on administrative registries and microbiological databases without access to detailed clinical data.14–18 Hence, the Danish Study Group of Infections of the Brain (DASGIB) was established in 2014 and a prospective recording of all adults admitted with CNS infections at departments of infectious diseases in Denmark was initiated as of January 1, 2015.
A Historical Perspective of Research on CNS Infections
Studies of CNS infections has a longstanding tradition (Table 1). Bacterial meningitis has been studied extensively including effects of antiserum and antibiotic treatments as well as changes in epidemiological characteristics, especially after the introduction of vaccines against major pathogens such as Haemophilus influenzae type b, Neisseria meningitidis, and Streptococcus pneumoniae in childhood vaccination programs.19–23 However, viral CNS infections, neurosyphilis, and Lyme neuroborreliosis have also received considerable attention through the last century,24–37 whereas brain abscess has been studied somewhat less frequently.38–40
Table 1.
Overview of Selected Databases and Observational Cohort Studies of Central Nervous System Infections
| Type of CNS Infection | Country | Study Period | Design and Case Definition | Number of Patients |
|---|---|---|---|---|
| Bacterial meningitis | ||||
| Bijlsma et al (2016)3 | Netherlands | 2006–2014 | Ongoing prospective observational cohort study. Adults >16 years of age with community-acquired bacterial meningitis based on 1) CSF culture positive or 2) by active referral of patients with positive PCR or antigen test for Streptococcus pneumoniae or Neisseria meningitidis in CSF combined with at least one Spanos criterium. | 1412 |
| Glimåker et al (2020)4 | Sweden | 2008–2017 | National Swedish quality register. Adults ≥16 years of age with community-acquired bacterial meningitis based on clinical criteria with or without CSF analyses. | 1056 |
| Tubiana et al (2020)6 | France | 2013–2015 | Prospective multicenter cohort study. Adults ≥18 years of age with community-acquired bacterial meningitis or purpura fulminans. Bacterial meningitis was based on 1) positive CSF culture, 2) Combination of CSF pleocytosis and blood culture or PCR/antigen test for CNS pathogen, 3) Isolation of N. meningitis by culture or PCR from petechiae. | 533 |
| Viral meningitis | ||||
| McGill et al (2018)7 | United Kingdom | 2011–2014 | Prospective multicenter cohort study. Adults ≥16 years of age with suspected viral meningitis based on 1) Analyses of CSF obtained by lumbar puncture or 2) No lumbar puncture but detection of CNS pathogen by PCR or culture of blood. | 231* |
| Desmond et al (2006)64 | United States | 1999–2002 | Combined data from 2 randomized controlled trials. The studies only included males or postmenopausal/surgically sterile females >14 years of age with a positive PCR for enterovirus and >10 x 106/L leukocytes in the CSF. | 240* |
| Encephalitis | ||||
| Granerod et al (2010)9 | United Kingdom | 2005–2006 | Prospective multicenter cohort study. Patients of all ages with suspected encephalitis referred for assessment by a multi-disciplinary expert panel or identified by review of CSF analyses at pathology departments. Patients were required to have encephalopathy and ≥2 of the following: 1) Fever, 2) Seizures or focal neurological deficit, 3) CSF leukocytes >4 x 106/L, 4) EEG findings suggestive of encephalitis, or 5) Neuroimaging indicating encephalitis. | 203 |
| Britton et al (2020)42 | Australia | 2013–2016 | Prospective multicenter cohort study. Children ≤14 years of age with suspected encephalitis referred by active surveillance for assessment by a multi-disciplinary expert panel. | 287 |
| Marechal et al (2021)8 | France | 2016–2018 | Ongoing prospective multicenter cohort study. Adults ≥18 years of age with encephalitis defined as neurological symptoms (without other causes) and ≥2 of the following: 1) Fever, 2) Seizure, 3) Recent focal neurological symptoms, 4) CSF WBC ≥5 x 106/L, 5) Neuroimaging suggestive of encephalitis, or 6) EEG indicative of encephalitis. | 349 |
| Brain abscess | ||||
| Helweg-Larsen et al (2012)65 | Denmark | 1994–2009 | Single-center retrospective observational cohort study. Adults ≥16 years of age diagnosed with brain abscess by neuroimaging and either: 1) Neurosurgery, 2) Autopsy, 3) Appropriate microbiological specimen (blood culture, CSF, sputum), or 4) Clinical presentation and response to antimicrobial treatment. | 102 |
| Campioli et al (2021)66 | United States | 2009–2020 | Single-center retrospective observational cohort study. Adults ≥18 years of age diagnosed with brain abscess by neuroimaging. | 247 |
| Neurosyphilis | ||||
| Dunaway et al (2020)12 | United States | 2003–2014 | Single-center observational cohort study. Patients diagnosed with syphilis and referred due to concerns of neurosyphilis either due to 1) Clinical neurological symptoms, or 2) Other factors associated with increased risks of neurosyphilis. | 150 |
| Bettuzzi et al (2021)13 | France | 1997–2017 | Retrospective multicenter cohort study. Inclusion criteria were a positive treponemal and non-treponemal tests combined with either 1) Otic syphilis, 2) Ocular syphilis, 3) Either neurological symptom with a positive result on CSF-VDRL or CSF-PCR tests, or 4) CSF leukocytes >5 x 106/L | 208 |
| Lyme neuroborreliosis | ||||
| Obel et al (2018)15 | Denmark | 1986–2016 | Population-based cohort study using national registries. A positive Borrelia burgdorferi intrathecal antibody test and a diagnosis of Lyme neuroborreliosis in the Danish National Patient Registry. | 2067 |
Note: *Microbiologically confirmed viral meningitis.
Abbreviations: CNS, central nervous system; CSF, cerebrospinal fluid; EEG, electroencephalogram; PCR, polymerase chain reaction; VDRL, venereal disease research laboratory test.
Strategies for Studies on CNS Infections
Patients with CNS infections may be identified by retrieval of positive test results for certain pathogens in cerebrospinal fluid (CSF) or other CNS samples using electronic information systems at departments of clinical microbiology. Although this strategy allows the researcher to examine specific microorganisms and leads to a well-defined group of patients, it usually does not encompass the entire clinical spectrum of many CNS infections and determination of whether or not a pathogen is a contaminant may be difficult. Sometimes the diagnostic yield is hampered by preceding antimicrobial treatment or the pathogen may be identified in other clinically relevant samples, eg blood cultures, combined with clinical markers of CNS infection such as CSF pleocytosis or cranial imaging. Occasionally, the pathogen may be difficult to identify, eg due to decreased sensitivity of microbiological analyses at different stages of disease in patients with encephalitis or because of inaccessibility of a brain abscess.
The identification of patients with CNS infections may also be conducted by searches in healthcare registries using the World Health Organisation’s International Classification of Diseases (ICD) codes. Important limitations of this approach are that diagnosis codes may vary between different versions of ICD and that the positive predictive value, sensitivity, and specificity may be low. In addition, lack of clinical details precludes analyses based on the clinical characteristics.
In contrast, large multi-center clinical databases have the potential to include the entire range of clinical presentations of the examined CNS infections combined with detailed clinical observations. Several prospective observational studies have been conducted in bacterial meningitis in adults using different definitions ranging from CSF culture positive cases only to allowance of inclusion of patients based solely on clinical criteria.3,4,6 Other CNS infections have rarely been examined in prospective clinical registries. A few studies have investigated hospitalized adults suspected of CNS infections,7,41 whereas other databases have focused on children or adults with encephalitis.8,9,42
DASGIB – Aim and Organization
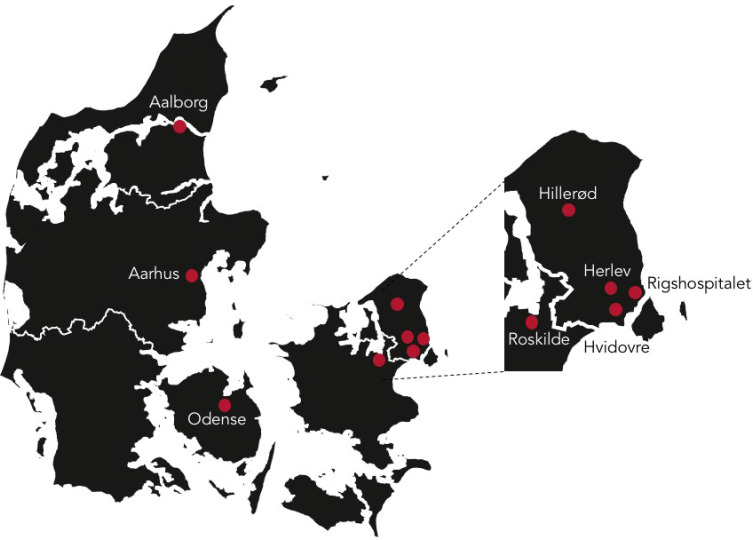
To improve research as well as quality of treatment and care of CNS infections, physicians at Danish departments of infectious diseases founded the DASGIB study group in 2014. This resulted in the establishment of the nationwide, prospective, and population-based DASGIB database of all patients admitted with community-acquired CNS infections at departments of infectious diseases in Denmark as of January 1, 2015 (Figure 1). Initially, the study group consisted of representatives from the departments of infectious diseases at hospitals in Aalborg, Aarhus, Odense, Hvidovre, Roskilde, Hillerød, and Copenhagen (Rigshospitalet). In 2018, the group was expanded to also include a member from Herlev Hospital. The DASGIB study group is managed by the secretariat located in Aalborg.
Figure 1.
The geographical distribution of the Danish Study Group of Infections of the Brain (DASGIB) study sites.
Setting and Study Population
Denmark is a welfare state and has a mixed rural and urban population totaling 4,666,625 adults ≥18 years of age (5,822,763 including children and adolescents) as of January 1, 2020 (Table 2).43 The Danish healthcare system is tax-financed and all residents are thus provided with access, free of charge at the point of delivery, to general practitioners for primary care and public hospitals for secondary and tertiary care.44 A unique civil registration number is assigned to all Danish residents at birth or immigration. This allows for unambiguous linkage across numerous nationwide registries at the individual level and for complete tracking of migration and vital status with <0.3% loss to follow-up.45 The Danish childhood vaccination program includes vaccines for potential CNS pathogens such as measles, mumps, rubella, H. influenzae type b, and Streptococcus pneumoniae (Table 3).
Table 2.
Demographics of the Adult Danish Population, Number of Hospitalizations Among Adults, and Number of Active Sites in the DASGIB Database Since Initiation on January 1, 2015
| Year | ||||||
|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | |
| Population ≥18 years of age | 4,489,821 | 4,539,791 | 4,580,547 | 4,615,690 | 4,645,697 | 4,666,625 |
| Number of hospital admissions* | 564,136 | 558,575 | 553,375 | 545,535 | – | – |
| Active sites in DASGIB | 7 | 7 | 7 | 8 | 8 | 8 |
| Number of CNS infections included | 460 | 562 | 742 | 766 | 638 | 411 |
Notes: *Not available from years 2019 through 2020 due a major change in registration of hospital admission in the Danish National Patient Registry. In addition, age categories for hospitalizations are only available in five-year intervals and are thus presented here for patients aged 20 years or older.
Abbreviations: CNS, central nervous system; DASGIB, Danish Study Group of Infections of the Brain.
Table 3.
The Danish Vaccination Program for Known Central Nervous System Pathogens
| Childhood Vaccination Programme: |
| Diphtheria-tetanus-pertussis-polio-H. influenzae and 13-valent conjugated pneumococcal vaccines are given at 3, 5, and 12 months of age. A booster of diphtheria-tetanus-pertussis-polio is administered at five years of age. |
| Measles, mumps and rubella are given at 15 months of age with a booster at four years of age. |
| Conjugated vaccination for H. influenzae was introduced in 1993. For S. pneumoniae, a 7-valent conjugated vaccine was implemented in 2007 and replaced by a 13-valent vaccine in 2010. For pneumococcal vaccinations in adults please see below. |
| Recommendations of Vaccination of Risk Groups in Denmark (Adults and Children): |
| Conjugated meningococcal vaccines (Quadrivalent A, C, Y, W-135 and lately also specific conjugated vaccine for serogroup B) are given to house-hold relatives of confirmed invasive meningococcal disease but has not been part of the Danish childhood vaccination program. |
| Since 2014, the 13-valent conjugated pneumococcal vaccine is strongly recommended to patients with asplenia, cochlear implants, before organ transplantation, dura defects, immunosuppressive conditions (eg HIV or lymphoma), or after documented invasive pneumococcal disease (eg pneumonia, meningitis, bacteremia). A second vaccination with the 23-valent polysaccharide pneumococcal vaccine is advised eight weeks after administration of the conjugate vaccine. |
| In Denmark, pneumococcal vaccination can also be considered in patients with chronic heart failure, chronic obstructive pulmonary disease, chronic liver- or kidney disease, diabetes mellitus, age> 64 years, asthma, B-cell immuno-deficiency, smokers, occupational hazards (eg welders). |
According to the Danish Board of Health, all CNS infections are to be managed at hospitals with onsite departments of infectious diseases and availability of round the clock consultation by an infectious disease specialist.46 These are located at the four tertiary care centers in Denmark (Aalborg, Aarhus, Odense, and Rigshospitalet) and at regional centers for infectious diseases at the hospitals at Roskilde, Hvidovre, Hillerød and Herlev-Gentofte.
Currently, departments of neurosurgery and neurocritical care are limited to the four tertiary care centers in Denmark. Nucleic acid amplification tests (NAAT) have been available at all departments of clinical microbiology since the start of the DASGIB database, either as in-house tests (pathogen specific and/or as syndromic panel testing using FilmArray or comparable techniques) or by centralized services provided by Statens Serum Institute (eg 16s DNA amplification or next-generation sequencing). National guidelines for treatment of bacterial and viral meningitis, encephalitis, and Lyme neuroborreliosis are provided by the Danish Infectious Diseases Society.47
Definitions of CNS Infections
Inclusion criteria of CNS infections often vary between studies. The definitions used in the DASGIB database are based on results of lumbar puncture in all patients (except for brain abscess patients) combined with a relevant clinical presentation, microbiological investigations, and cranial imaging (Table 4). Furthermore, CNS infection has to be considered the most probable diagnosis after taking into account all available information from the index and any other relevant hospitalizations at time of medical record review and as assessed by a specialist in infectious diseases. For patients with suspected encephalitis, adherence to the criteria of the International Encephalitis Consortium (year 2013) is generally encouraged but not mandatory since this definition may not capture all conceivable presentations of encephalitis.48,49 Patients with proven or suspected autoimmune encephalitis are excluded. Likewise, patients with nosocomial CNS infections are excluded defined as those occurring during hospitalization for other causes, previous neurosurgery within 30 days of admission, or indwelling hardware in the CNS (eg ventriculo-peritoneal shunts or deep-brain stimulators). In all cases of doubt, patients are discussed with the DASGIB secretary (JB) or at bi-annual DASGIB meetings.
Table 4.
Definitions for Central Nervous System Infections Used in the DASGIB Database
| Criteria | |
|---|---|
| Bacterial meningitis | A clinical presentation suggestive of bacterial meningitis (eg headache, neck stiffness, fever, altered mental status) and either of the following criteria: i)Positive culture or bacterial DNA/antigen analysis of CSF ii)Positive blood culture and CSF leukocytes >10 x 106/L iii)CSF leukocytes >10 x 106/L and seroconversion or 4-fold increase in meningococcal antibody titer within 4 weeks of admission iv)CSF leukocytes >10 x 106/L and no other diagnosis considered more likely given all available information |
| Viral meningitis | A clinical presentation suggestive of viral meningitis (eg headache, neck stiffness, fever, photophobia) and either of the following criteria: i)Positive viral DNA/RNA analysis of CSF ii)CSF leukocytes >10 x 106/L and positive intrathecal antibody index for HSV/VZV iii)CSF leukocytes >10 x 106/L and serology suggestive of acute infection with a known CNS pathogen, eg Tick-borne encephalitis virus, or positive PCR from other relevant samples, eg influenza in the respiratory tract iv)CSF leukocytes >10 x 106/L and no other diagnosis considered more likely given all available information |
| Encephalitis/myelitis | A clinical presentation suggestive of encephalitis (eg impaired consciousness >24 hours, headache, neurological deficit) and either of the following criteria: i)Positive viral DNA/RNA analysis of CSF ii)Positive intrathecal antibody index for HSV/VZV iii)CSF leukocytes >10 x 106/L and serology suggestive of acute infection with a known CNS pathogen, eg Tick-borne encephalitis virus, or positive PCR from other relevant samples, eg influenza in the respiratory tract iv)Fulfillment of the encephalitis criteria from the International Encephalitis Consortium48 v)CSF leukocytes >10 x 106/L and/or CNS imaging suggestive of encephalitis/myelitis and no other diagnosis considered more likely given all available information |
| Brain abscess | A clinical presentation suggestive of brain abscess (eg headache, neurological deficit, fever) and either of the following criteria: i)Aspirated or excised pus from brain abscess with or without detection of pathogen(s) by microbiological or histopathological examinations ii)Cranial imaging combined with bacteremia or identification of a relevant pathogen from a normally sterile sample site or positive serology for toxoplasmosis in a HIV positive patient iii)Cranial imaging and no other diagnosis considered more likely given all available information |
| Neurosyphilis | A clinical presentation suggestive of neurosyphilis (eg meningitis, headache, cranial nerve palsies, impaired vision or hearing, cerebral vasculitis, general paresis, tabes dorsalis, or dementia) combined with positive blood and/or CSF serological nontreponemal and treponemal tests. Asymptomatic neurosyphilis as well as ocular and auditory syphilis is also included. |
| Neuroborreliosis | A clinical presentation of Lyme neuroborreliosis (eg facial palsy or radiculitis) combined with CSF leukocytes >10 x 106/L and a positive Borrelia intrathecal antibody index. Patients without a positive Borrelia intrathecal antibody index are also included if the duration of symptoms is <3 weeks and no other diagnosis is considered more likely given all available information |
Abbreviations: CSF, cerebrospinal fluid; DASGIB, Danish Study Group of Infections of the Brain; DNA, deoxyribonucleic acid; HIV, human immunodeficiency virus; HSV, herpes simplex virus; PCR, polymerase chain reaction; RNA, ribonucleic acid; VZV, varicella zoster virus.
Whenever possible, the pathogen is determined, but inclusion of patients with unknown microbiological etiology is allowed to ensure that the entire clinical spectrum of disease is covered. This is important as the pathogen remains unknown for a substantial part of patients with CNS infections which may infer considerable uncertainty among patients and physicians. Hence, increased knowledge on the prognosis of these patients is crucial.
Data Collection and Variables
Data Sources
The primary data sources used for data collection consist of the electronic medical records including ambulance records, doctor’s records, nurse’s charts, laboratory results of blood and CSF analyses, radiological examinations, microbiological analyses, electronic medication records, intensive care unit observation charts, outpatient visits, and any subsequent hospital admissions. However, if patients are treated directly by the local investigator, further information may be obtained by ad hoc personal interviews.
Informatics
An online case report form developed by the IT services at North Denmark Region was used until July 1, 2016 when it was replaced by a more user-friendly and detailed database using REDcap.50 Data are extracted from the medical records by each local DASGIB representative who is a specialist in infectious diseases or by specially trained research assistants. A standard operating procedure for retrieval and entering of data is provided (Supplementary Material) and consultation with the DASGIB secretary is encouraged on a case-to-case basis if in doubt. The database is continuously updated and queries for missing values and outliers are sent to local DASGIB representatives by the DASGIB secretary. Completeness of inclusion of cases with CNS infection is ensured by annual searches at each department of infectious diseases using ICD-10 diagnosis codes or medical record review of all patients with CSF leukocytosis (Supplementary Table 1).
Variables
General information on baseline demographics, blood and CSF tests, imaging results, and outcome for all included cases are recorded in the database (Please see the Supplementary Material for the full case report form). Additional sets of disease-specific variables have been tailored to capture important traits and aspects for each type of CNS infection, ie bacterial meningitis, viral meningitis, encephalitis, brain abscess, neurosyphilis, and Lyme neuroborreliosis.
Main variables registered include date, time, and place of admission; referral and admission diagnoses; duration of symptoms; travel history; pre-existing comorbidities and functional level; exposures; symptoms and signs of relevance for each CNS infection; date and time of antimicrobial treatment, lumbar puncture, and cranial imaging when performed; complications during admission including admission to the intensive care unit and neurocritical care; and Glasgow Outcome Scale51 score at discharge and at 1-, 3-, and 6-months after discharge (Table 5). Concomitant foci of infection are determined according to clinical practice and may rely on microbiological investigations of samples outside the CNS, imaging results, consultations by ear-nose-throat specialists, and echocardiography.
Table 5.
Study Variables and Data Sources Used in the DASGIB Database
| Variable | Data Sources |
|---|---|
| Baseline demographics (civil registration number, age, sex) | Medical records |
| Time of admission | Prioritized order: Ambulance records, first triage at admission (ie measurement of blood pressure, pulse rate, temperature, respiratory rate, oxygen saturation, and Glasgow Coma Scale score), or administrative notation of admission by secretary |
| Referral and admission diagnoses | Ambulance and medical records |
| Duration of symptoms | Medical records |
| Travel history (30 days) | Medical records |
| Pre-existing comorbidities | Medical records and electronic medication records |
| Pre-morbid functional level | Medical records |
| Exposures (occupational, recreative, animal) | Medical records |
| Symptoms and signs at admission of relevance for each CNS infection | Medical records |
| First triage at admission (ie measurement of blood pressure, pulse rate, temperature, respiratory rate, oxygen saturation, and Glasgow Coma Scale) | Medical records and nurse’s charts. If Glasgow Coma Scale is not registered in these data sources, the last observation from the ambulance records is noted. |
| Date and time of antimicrobial treatment | Prioritized order: Electronic medication records, nurse’s charts, and doctor’s notes |
| Date and time of lumbar puncture | Electronic laboratory files of the Department of Clinical Biochemistry |
| Date and time of cranial imaging | Electronic files of the Department of Radiology |
| Blood tests and cell counts of cerebrospinal fluid | Electronic laboratory files of the Department of Clinical Biochemistry |
| Microbiological analyses | Electronic files of the Department of Clinical Microbiology and Statens Serum Institut |
| Observations during neurocritical care and intensive care units (eg intracranial pressure measurements) | Observational charts at intensive care units |
| Outpatient visits and subsequent hospitalizations | Medical records |
| Dates of discharge and death | Medical records |
Abbreviation: DASGIB, Danish Study Group of Infections of the Brain.
Time of hospital admission is used as reference for computations of time to antimicrobial therapy, lumbar puncture, cranial imaging, hospital discharge, and death. Time of empirical antimicrobial treatment is defined as first administration of a drug in dosages recommended for treatment of the specific CNS infection in question,47,52–54 whereas targeted treatment denotes adjustments according to pathogen identification and antimicrobial susceptibility. Occasionally, patients may switch antimicrobial regimens during prolonged treatment in which case the drug used for the majority of treatment is registered. Vital status is obtained from the electronic medical records which are synchronized with the Danish Civil Registration System on a daily basis.44,45
Biobank
Thus far, blood and CSF samples have been collected from 361/3579 (10%) patients with CNS infections at some DASGIB sites (Aalborg, Hvidovre, Skejby, and Rigshospitalet). These samples are stored according to local protocols in freezers at −80° Celsius and can be used for research purposes after obtainment of government approval according to Danish law.
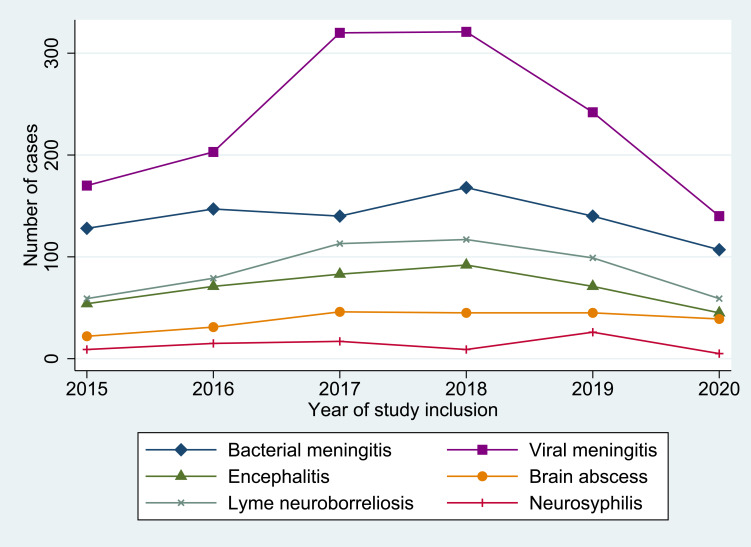
Time Period
All adults hospitalized with a CNS infection at department of infectious diseases in Denmark have been included in the DASGIB database yielding a total of 3579 cases from January 1, 2015 through December 31, 2020 (Figure 2). This included patients ≥16 years of age until June 30, 2016 when changes in hospital visitation practices of all adolescents to pediatric departments were implemented and since then only adults ≥18 years of age have been registered. An outbreak of enterovirus meningitis in years 2017 and 2018 caused a temporary increase in the annual number of included cases of CNS infections.55
Figure 2.
Annual number of central nervous system infections included in the Danish Study Group of Infections of the Brain (DASGIB) database.
Methodological Aspects
Strengths and Weaknesses
A major strength of the DASGIB database is the ongoing inclusion of longitudinal and prospectively collected detailed clinical data on all adults treated for CNS infections at Danish departments of infectious diseases for six years by now. Although CNS infections are relatively rare, this has resulted in an exceptionally large sample size that is unique on a global scale. Moreover, the nationwide and population-based design with virtually complete follow-up for subsequent hospital contacts and mortality adds to the importance of the DASGIB database. The database was developed and is maintained by infectious diseases clinicians, which may help to keep focus on clinically relevant dilemmas and challenges in the management of patients with CNS infections. Another advantage of the database is that the quality and completeness of the recorded information is continuously monitored, and great efforts are made to constantly improve data collection.
The individual civil registration number assigned to all Danish residents also allows for unambiguous linkage of DASGIB data with other nationwide healthcare and socioeconomic registries. This may include the Danish National Patient Registry which holds information on all hospital admissions since 1977 and outpatient visits since 1995;56 the Danish Civil Registration System that contains data on vital and migration status of all Danish residents;45 the Danish Laboratory Database which includes results of most major biochemical laboratories in Denmark corresponding to approximately 80% of the Danish population;57 and the Danish National Prescription Registry that comprises key information on reimbursable drugs dispensed from Danish pharmacies since 1994.58 Combining the DASGIB database with these resources makes it possible to examine large cohorts of CNS infection patients with complete hospitalization history and comorbidities as well as long-term follow-up. The Danish Civil Registration System also allows for the formation of matched cohort and case-control studies by selection of controls from the underlying source population using density sampling.
Importantly, the DASGIB study group comprises representatives from all departments of infectious diseases in Denmark and may thereby coordinate and facilitate a concerted effort of research in CNS infections. This will hopefully continue to foster a synergistic effect that may improve the quality and clinical impact of the planned research projects.
The main limitation is that some patients with relatively non-severe forms of CNS infections such as viral meningitis or Lyme neuroborreliosis may occasionally be treated at regional hospitals or at departments of neurology. In addition, some patients with severe hematological diseases or solid-organ transplants may be managed at other departments without assistance of infectious diseases specialists and thereby missed inclusion into the DASGIB database. This may lead to selection bias if such patients differ substantially from the included patients and an underestimation of incidence using the DASGIB database. However, we expect this bias to be limited given the directive from the Danish Board of Health that all CNS infections should be managed by infectious diseases specialists.46 Another limitation is the lack of uniform procedures for post-discharge patient contact for addressing missing values from the index admission. Finally, local protocols for obtainment and pre-analytic processing of blood and CSF samples are not yet standardized.
Research from the Database
Research from the DASGIB study group has thus far primarily focused on descriptive studies of the clinical presentation and outcome of community-acquired CNS infections. The first study highlighted the usefulness of CSF lactate for the diagnosis of bacterial meningitis in patients with suspected CNS infection.59 CSF lactate is an inexpensive test that can easily be analyzed within minutes after lumbar puncture and is readily available at almost all hospitals. The study showed that CSF lactate had the best diagnostic value for bacterial versus viral meningitis with an area under the curve of 0.976 (95% CI 0.966–0.997) using a cut-off of 3.5 mmol/L. The second study reported the epidemiological trends in meningitis (bacterial and viral) and encephalitis during the first 1.5 years of the DASGIB database. The predominant pathogen in bacterial meningitis was S. pneumoniae, whereas N. meningitidis and Listeria monocytogenes were infrequent compared with other settings.3,4,6 Of note, S. aureus and ß-hemolytic streptococci were the second and third most common causes of bacterial meningitis in the DASGIB cohort during this study period. Viral meningitis was mainly due to Varicella zoster virus and enterovirus, and Herpes simplex virus 1 was the primary pathogen among cases of encephalitis.
Next, two studies have examined the management of Lyme neuroborreliosis in Denmark. One study found that cranial imaging was often performed in elderly comorbid patients to rule out other diagnoses, whereas the second study observed that a substantial diagnostic delay and prolonged antibiotic treatment beyond 14 days was frequent in these patients.60,61
Another study analyzed risk factors and prognosis of seizures in bacterial meningitis using a retrospective derivation cohort and subsequently validating the findings in the DASGIB cohort.62 Risk factors for seizures consisted of pneumococcal etiology, immuno-compromise, and abnormal cranial imaging (mainly stroke), and seizures at any time during illness predicted both in-hospital mortality and unfavorable outcome at discharge. Using the DASGIB cohort, a case series provided a valuable and detailed clinical description of 12 patients with normocellular bacterial meningitis.63 The diagnosis was confirmed by culture (S. pneumoniae, n=10; S. aureus, n=1) or polymerase chain reaction (N. meningitidis, n=1) of the CSF. Importantly, none of the patients had serious immuno-compromising conditions and the overall case-fatality rate was 25%.
A large study on Varicella zoster virus encephalitis highlighted the complexity of the diagnosis and treatment challenges of this life-threatening disease. Predisposing immunocompromising conditions were frequent (39%) and the main symptoms were confusion (76%), headache (56%), nausea (45%), gait disturbance (42%), and personality changes (41%). A diagnosis of cerebral vasculitis was not uncommon (16%) and encephalitic abnormalities (13%) had a predilection for the brainstem and other deep brain structures. Unfavorable outcome at discharge was observed in 69% and was associated with increasing age, vasculitis, and Glasgow Coma Scale score <15.
Finally, the largest study to date on enteroviral meningitis in adults (n=419 cases) showcased a 2017–2018 national epidemic attributable to Echovirus 30.55 Admission diagnoses included CNS infection in 62%, other neurological conditions in 22%, and cerebrovascular diseases accounted in 8%. A polymorphonuclear predominance in the CSF was frequent if lumbar puncture was performed within 3 days of onset of symptoms. Cranial imaging preceded lumbar puncture in 30% of patients and was associated with a delay in time to lumbar puncture from median 1.5 hours (IQR 0.8–2.8) to 4.8 hours (IQR 3.4–7.9; p<0.001 for comparison). A GOS score of 4 was observed in 24% at discharge and was associated with female sex and less frequent in Echovirus 30.
Permissions and Access for Other Researchers
The DASGIB database is approved by the legal department at the North Denmark Region (record numbers 2008-58-0028 with local ID 2017-241 for the database and 2013-41-2502 for the biobank) and the Danish Board of Health (record numbers 3-3013-2579/1 and 3-3013-3168/1). Patient consent or permission from an ethical committee is not required for this type of study in Denmark. All data is managed in compliance with relevant data protection and privacy regulations and in accordance with the Helsinki declaration. The DASGIB study group encourages multidisciplinary collaborations and is very interested in working together with other Danish and international researchers after obtainment of proper approvals. Potential collaborators are invited to contact the corresponding author.
Perspectives
Knowledge on the epidemiology, clinical presentation, and outcome of CNS infections is paramount for identifying and determining research priorities and for allocation of healthcare resources. Unfortunately, high-quality and contemporary data on fundamental characteristics of most CNS infections are scarce and much remains to be explored. Nationwide and population-based studies improve the confidence in incidence estimates, risk factors, and prognosis due to the well-defined catchment area and completeness of follow-up. The large study population of approximately 4.6 million adult Danish residents also provides researchers with the opportunity to examine rare CNS infections and may contribute to detection of emerging pathogens. The DASGIB study group is dedicated to future multidisciplinary research projects that may involve clinical microbiologists, neurologists, neurosurgeons, radiologists, engineers, molecular biologists, and clinical epidemiologists with the hope of gaining new insights into changes in the etiology, risk- and prognostic factors, and treatment of CNS infections.
Already, the DASGIB study group is active in several international research projects including sponsoring an investigator-initiated large randomised non-inferiority trial on early transition to oral treatment of brain abscess that is conducted in Denmark, Sweden, France, the Netherlands, and Australia (ORAL study; EudraCT 2019-002845-39). This international study has triggered a number of other research collaborations with the hope of advancing management of CNS infections further. Finally, the DASGIB infrastructure provides an essential framework for future international clinical trials on CNS infections in Denmark.
Funding Statement
There is no funding to report.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
No funding was obtained for this study and all authors report no conflicts of interests.
References
- 1.Bennett JE, Dolin R, Blaser MJ. Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases. 8 ed. Philadelphia, US: Elsevier Health Sciences; 2015. [Google Scholar]
- 2.Michael SW, Whitley RJ, Marra CM. Infections of the Central Nervous System. 4 ed. Philadelphia US: Lippincott Williams & Wilkins; 2014. [Google Scholar]
- 3.Bijlsma MW, Brouwer MC, Kasanmoentalib ES, et al. Community-acquired bacterial meningitis in adults in the Netherlands, 2006-14: a prospective cohort study. Lancet Infect Dis. 2016;16(3):339–347. doi: 10.1016/S1473-3099(15)00430-2 [DOI] [PubMed] [Google Scholar]
- 4.Glimåker M, Naucler P, Sjölin J. Etiology, clinical presentation, outcome and the effect of initial management in immunocompromised patients with community acquired bacterial meningitis. J Infect. 2020;80:291–297. doi: 10.1016/j.jinf.2019.12.019 [DOI] [PubMed] [Google Scholar]
- 5.Bodilsen J, Storgaard M, Larsen L, et al. Infectious meningitis and encephalitis in adults in Denmark: a prospective nationwide observational cohort study (DASGIB). Clin Microbiol Infec. 2018;24(10):1102.e1–1102.e5. doi: 10.1016/j.cmi.2018.01.016 [DOI] [PubMed] [Google Scholar]
- 6.Tubiana S, Varon E, Biron C, et al. Community-acquired bacterial meningitis in adults: in-hospital prognosis, long-term disability and determinants of outcome in a multicentre prospective cohort. Clin Microbiol Infec. 2020;26(9):1192–1200. doi: 10.1016/j.cmi.2019.12.020 [DOI] [PubMed] [Google Scholar]
- 7.McGill F, Griffiths MJ, Bonnett LJ, et al. Incidence, aetiology, and sequelae of viral meningitis in UK adults: a multicentre prospective observational cohort study. Lancet Infect Dis. 2018;18(9):992–1003. doi: 10.1016/S1473-3099(18)30245-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maréchal ML, Mailles A, Seigneurin A, Tattevin P, Stahl J-P, Épaulard O. A prospective cohort study to identify clinical, biological, and imaging features that predict the etiology of acute encephalitis. Clin Infect Dis. 2020;73(2):264–270. [DOI] [PubMed] [Google Scholar]
- 9.Granerod J, Ambrose HE, Davies NW, et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis. 2010;10(12):835–844. doi: 10.1016/S1473-3099(10)70222-X [DOI] [PubMed] [Google Scholar]
- 10.Herlin LK, Hansen KS, Bodilsen J, et al. Varicella Zoster Virus encephalitis in Denmark from 2015 to 2019- a nationwide prospective cohort study. Clin Infect Dis. 2020;72(7):1192–1199. doi: 10.1093/cid/ciaa185 [DOI] [PubMed] [Google Scholar]
- 11.Glaser CA, Gilliam S, Schnurr D, et al. In search of encephalitis etiologies: diagnostic challenges in the California Encephalitis Project, 1998–2000. Clin Infect Dis. 2003;36(6):731–742. doi: 10.1086/367841 [DOI] [PubMed] [Google Scholar]
- 12.Dunaway SB, Maxwell CL, Tantalo LC, Sahi SK, Marra CM. Neurosyphilis treatment outcomes after intravenous penicillin G versus intramuscular procaine penicillin plus oral probenecid. Clin Infect Dis. 2019;71(2):267–273. doi: 10.1093/cid/ciz795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bettuzzi T, Jourdes A, Robineau O, et al. Ceftriaxone compared with benzylpenicillin in the treatment of neurosyphilis in France: a retrospective multicentre study. Lancet Infect Dis. 2021. doi: 10.1016/S1473-3099(20)30857-4 [DOI] [PubMed] [Google Scholar]
- 14.Bodilsen J, Dalager-Pedersen M, van de Beek D, Brouwer MC, Nielsen H. Long-term mortality and epilepsy in patients after brain abscess: a nationwide population-based matched cohort study. Clin Infect Dis. 2019;71(11):2825–2832. doi: 10.1093/cid/ciz1153 [DOI] [PubMed] [Google Scholar]
- 15.Obel N, Dessau RB, Krogfelt KA, et al. Long term survival, health, social functioning, and education in patients with European Lyme neuroborreliosis: nationwide population based cohort study. BMJ. 2018;361:k1998. doi: 10.1136/bmj.k1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bubba L, Broberg EK, Jasir A, et al.; collaborators E study. Circulation of non-polio enteroviruses in 24 EU and EEA countries between 2015 and 2017: a retrospective surveillance study. Lancet Infect Dis. 20;2019:350–361. doi: 10.1016/S1473-3099(19)30566-3 [DOI] [PubMed] [Google Scholar]
- 17.Omland LH, Vestergaard HT, Dessau RB, et al. Characteristics and long-term prognosis of Danish patients with varicella zoster virus detected in cerebrospinal fluid compared with the background population. J Infect Dis. 2021;224:850–859. doi: 10.1093/infdis/jiab013 [DOI] [PubMed] [Google Scholar]
- 18.Roed C, Omland LH, Skinhoj P, Rothman KJ, Sorensen HT, Obel N. Educational achievement and economic self-sufficiency in adults after childhood bacterial meningitis. JAMA. 2013;309(16):1714. doi: 10.1001/jama.2013.3792 [DOI] [PubMed] [Google Scholar]
- 19.Flexner S. The results of the serum treatment in thirteen hundred cases of epidemic meningitis. J Exp Med. 1913;17(5):553–576. doi: 10.1084/jem.17.5.553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Swartz MN. Bacterial meningitis–a view of the past 90 years. N Engl J Med. 2004;351(18):1826–1828. doi: 10.1056/NEJMp048246 [DOI] [PubMed] [Google Scholar]
- 21.Swartz MN, Dodge PR. Bacterial meningitis — a review of selected aspects — general clinical features, special problems and unusual meningeal reactions mimicking bacterial meningitis. N Engl J Med. 1965;272(17):898–902. doi: 10.1056/NEJM196504292721707 [DOI] [PubMed] [Google Scholar]
- 22.Meads M, Harris HW, Samper BA, Finland M, Wilcox C. Treatment of meningococcal meningitis with penicillin. N Engl J Med. 1944;231(15):509–517. doi: 10.1056/NEJM194410122311501 [DOI] [Google Scholar]
- 23.de Gans J, van de Beek D; Investigators ED in ABMS. Dexamethasone in adults with bacterial meningitis. N Engl J Med. 2002;347(20):1549–1556. doi: 10.1056/NEJMoa021334 [DOI] [PubMed] [Google Scholar]
- 24.Meyer HM, Johnson RT, Crawford IP, Dascomb HE, Rogers NG. Central nervous system syndromes of “viral” etiology A study of 713 cases. Am J Med. 1960;29(2):334–347. doi: 10.1016/0002-9343(60)90029-2 [DOI] [PubMed] [Google Scholar]
- 25.Whitley RJ, Soong SJ, Dolin R, Galasso GJ, Ch’ien LT, Alford CA. Adenine arabinoside therapy of biopsy-proved herpes simplex encephalitis. National Institute of Allergy and Infectious Diseases collaborative antiviral study. N Engl J Med. 1977;297(6):289–294. doi: 10.1056/NEJM197708112970601 [DOI] [PubMed] [Google Scholar]
- 26.Whitley RJ, Alford CA, Hirsch MS, et al. Vidarabine versus Acyclovir therapy in herpes simplex encephalitis. N Engl J Med. 1986;314(3):144–149. doi: 10.1056/NEJM198601163140303 [DOI] [PubMed] [Google Scholar]
- 27.Sköldenberg B, Alestig K, Burman L, et al. Acyclovir versus vidarabine in Herpes simplex encephalitis. Lancet. 1984;324(8405):707–711. doi: 10.1016/S0140-6736(84)92623-0 [DOI] [PubMed] [Google Scholar]
- 28.Ghanem KG. REVIEW: neurosyphilis: a historical perspective and review. Cns Neurosci Ther. 2010;16(5):e157–e168. doi: 10.1111/j.1755-5949.2010.00183.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moore JE, Hopkins HH. Asymptomatic neurosyphilis: VI. The prognosis of early and late asymptomatic neurosyphilis. J Amer Med Assoc. 1930;95(22):1637–1641. doi: 10.1001/jama.1930.02720220007003 [DOI] [Google Scholar]
- 30.Clark EG, Danbolt N. The Oslo study of the natural history of untreated syphilis An epidemiologic investigation based on a restudy of the Boeck-Bruusgaard material a review and appraisal. J Chron Dis. 1955;2(3):311–344. doi: 10.1016/0021-9681(55)90139-9 [DOI] [PubMed] [Google Scholar]
- 31.White RM. Unraveling the Tuskegee study of untreated syphilis. Arch Intern Med. 2000;160(5):585–598. doi: 10.1001/archinte.160.5.585 [DOI] [PubMed] [Google Scholar]
- 32.Hopkins HH. Treatment of neurosyphilis: review of results in six hundred and eighty patients. Arch Intern Med. 1933;52(1):66–75. doi: 10.1001/archinte.1933.00160010073007 [DOI] [Google Scholar]
- 33.Ryberg B. Bannwarth’s syndrome (lymphocytic meningoradiculitis) in Sweden. Yale J Biol Med. 1984;57(4):499–503. [PMC free article] [PubMed] [Google Scholar]
- 34.Ryberg B, Nilsson B, Burgdorfer W, Barbour AG. Antibodies to Lyme-disease spirochaete in European lymphocytic meningoradiculitis (Bannwarth’s syndrome). Lancet. 1983;322(8348):519. doi: 10.1016/S0140-6736(83)90552-4 [DOI] [PubMed] [Google Scholar]
- 35.Sköldenberg B, Gårde A, Carlström A, Stiernstedt G, Kolmodin G, Nord CE. Chronic meningitis caused by a penicillin-sensitive microorganism? Lancet. 1983;322(8341):75–78. doi: 10.1016/S0140-6736(83)90061-2 [DOI] [PubMed] [Google Scholar]
- 36.Steere AC, Grodzicki RL, Kornblatt AN, et al. The spirochetal etiology of Lyme disease. N Engl J Med. 1983;308(13):733–740. doi: 10.1056/NEJM198303313081301 [DOI] [PubMed] [Google Scholar]
- 37.Steere AC, Malawista SE, Snydman DR, et al. An epidemic of oligoarticular arthritis in children and adults in three Connecticut communities. Arthrit Rheumat. 1977;20(1):7–17. doi: 10.1002/art.1780200102 [DOI] [PubMed] [Google Scholar]
- 38.Canale DJ. William Macewen and the treatment of brain abscesses: revisited after one hundred years. J Neurosurg. 1996;84(1):133–142. doi: 10.3171/jns.1996.84.1.0133 [DOI] [PubMed] [Google Scholar]
- 39.Weeds J. Case of cerebral abscess. Nashville J Med Surg. 1872;9:156–171. [Google Scholar]
- 40.Brouwer MC, Coutinho JM, van de Beek D. Clinical characteristics and outcome of brain abscess: systematic review and meta-analysis. Neurology. 2014;82(9):806–813. doi: 10.1212/WNL.0000000000000172 [DOI] [PubMed] [Google Scholar]
- 41.Khatib U, van de Beek D, Lees JA, Brouwer MC. Adults with suspected central nervous system infection: a prospective study of diagnostic accuracy. J Infect. 2017;74(1):1–9. doi: 10.1016/j.jinf.2016.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Britton PN, Dale RC, Blyth CC, et al. Causes and clinical features of childhood encephalitis: a multicenter, prospective cohort study. Clin Infect Dis. 2019;70(12):2517–2526. doi: 10.1093/cid/ciz685 [DOI] [PubMed] [Google Scholar]
- 43.Statistics Denmark website. Available from: https://statbank.dk/statbank5a/default.asp?w=2560. Accessed May 5, 2021.
- 44.Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563–591. doi: 10.2147/CLEP.S179083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schmidt M, Pedersen L, Sørensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi: 10.1007/s10654-014-9930-3 [DOI] [PubMed] [Google Scholar]
- 46.The Danish Board of Health website. Gældende specialeplan - Sundhedsstyrelsen (Danish)[Overall organisation of medical specialties in Denmark]. Available from: https://www.sst.dk/da/viden/specialeplanlaegning/gaeldende-specialeplan. Accessed May 5, 2021.
- 47.Danish Society of Infections Diseases website. Guidelines og retningslinier (Danish) [Guidelines and recommendations]. Available from: http://www.infmed.dk/guidelines. Accessed May 5, 2021.
- 48.Venkatesan A, Tunkel AR, Bloch KC, et al. Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the international encephalitis consortium. Clin Infect Dis. 2013;57(8):1114–1128. doi: 10.1093/cid/cit458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jackson AC. Problems With Case Definitions and a Need for Revisions by the International Encephalitis Consortium. Clin Infect Dis. 2015;61(2):293. doi: 10.1093/cid/civ313 [DOI] [PubMed] [Google Scholar]
- 50.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McMillan T, Wilson L, Ponsford J, Levin H, Teasdale G, Bond M. The Glasgow Outcome Scale — 40 years of application and refinement. Nat Rev Neurol. 2016;12(8):477–485. doi: 10.1038/nrneurol.2016.89 [DOI] [PubMed] [Google Scholar]
- 52.van de Beek D, Cabellos C, Dzupova O, et al. ESCMID guideline: diagnosis and treatment of acute bacterial meningitis. Clin Microbiol Infec. 2016;22:1–26. doi: 10.1016/j.cmi.2016.01.007 [DOI] [PubMed] [Google Scholar]
- 53.Bodilsen J, Brouwer MC, Nielsen H, Beek DVD. Anti-infective treatment of brain abscess. Expert Rev Anti Infe. 2018;16(7):565–578. doi: 10.1080/14787210.2018.1489722 [DOI] [PubMed] [Google Scholar]
- 54.Nau R, Sorgel F, Eiffert H. Penetration of drugs through the blood-cerebrospinal fluid/blood-brain barrier for treatment of central nervous system infections. Clin Microbiol Rev. 2010;23(4):858–883. doi: 10.1128/CMR.00007-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bodilsen J, Mens H, Midgley S, et al. Enterovirus meningitis in adults: a prospective nationwide population-based cohort study. Neurology. 2021;97:e454–e463. doi: 10.1212/WNL.0000000000012294 [DOI] [PubMed] [Google Scholar]
- 56.Schmidt M, Schmidt SAJ, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi: 10.2147/CLEP.S91125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Trier-Poulsen D. Dokumentation af Labdatabasens Forskertabel [Documentation of the Danish Laboratory Database]. Available from: https://sundhedsdatastyrelsen.dk/da/registre-og-services/om-de-nationale-sundhedsregistre/doedsaarsager-og-biologisk-materiale/laboratoriedatabasen. Accessed May 5, 2021.
- 58.Kildemoes HW, Sørensen HT, Hallas J. The Danish national prescription registry. Scand J Public Health. 2011;39(7 Suppl):38–41. doi: 10.1177/1403494810394717 [DOI] [PubMed] [Google Scholar]
- 59.Buch K, Bodilsen J, Knudsen A, et al. Cerebrospinal fluid lactate as a marker to differentiate between community-acquired acute bacterial meningitis and aseptic meningitis/encephalitis in adults: a Danish prospective observational cohort study. Infect Dis Nor. 2018;50(7):1–8. [DOI] [PubMed] [Google Scholar]
- 60.Ørbæk M, Bodilsen J, Gynthersen RMM, et al. CT and MR neuroimaging findings in patients with lyme neuroborreliosis: a national prospective cohort study. J Neurol Sci. 2020;419:117176. doi: 10.1016/j.jns.2020.117176 [DOI] [PubMed] [Google Scholar]
- 61.Nordberg CL, Bodilsen J, Knudtzen FC, et al. Lyme neuroborreliosis in adults: a nationwide prospective cohort study. Ticks Tick Borne Dis. 2020;11(4):101411. doi: 10.1016/j.ttbdis.2020.101411 [DOI] [PubMed] [Google Scholar]
- 62.Larsen FTBD, Brandt CT, Klastrup L, et al. Risk factors and prognosis of seizures in adults with community-acquired bacterial meningitis in Denmark: observational cohort studies. BMJ Open. 2019;9(7):e030263. doi: 10.1136/bmjopen-2019-030263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vestergaard HH, Larsen L, Brandt C, et al. Normocellular community-acquired bacterial meningitis in adults: a nationwide population-based case series. Ann Emerg Med. 2021;77(1):11–18. doi: 10.1016/j.annemergmed.2020.05.041 [DOI] [PubMed] [Google Scholar]
- 64.Desmond RA, Accortt NA, Talley L, Villano SA, Soong S-J, Whitley RJ. Enteroviral meningitis: natural history and outcome of pleconaril therapy. Antimicrob Agents Ch. 2006;50(7):2409–2414. doi: 10.1128/AAC.00227-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Helweg-Larsen J, Astradsson A, Richhall H, Erdal J, Laursen A, Brennum J. Pyogenic brain abscess, a 15 year survey. Bmc Infect Dis. 2012;12(1):332. doi: 10.1186/1471-2334-12-332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Campioli CC, Almeida NEC, O’Horo JC, et al. Bacterial brain abscess: an outline for diagnosis and management. Am J Med. 2021. doi: 10.1016/j.amjmed.2021.05.027 [DOI] [PubMed] [Google Scholar]