Abstract
Background:
A number of motor abnormalities have been reported in psychotic disorders, including dyskinesia and psychomotor slowing. There is also evidence for many of the same motor abnormalities in biological first-degree relatives, and accruing evidence for motor abnormalities in bipolar disorder. In addition to motor dysfunction, there are also shared symptom domains amongst these populations.
Objectives:
We explored the associations of (1) current and lifetime psychosis and mood symptom domains and (2) domains of psychosis proneness with various domains of motor function in a transdiagnostic sample (n=149).
Method:
Individuals with schizophrenia, schizoaffective disorder, or bipolar disorder, biological first-degree relatives of individuals with a psychotic disorder, and controls completed measures of psychomotor speed and movement fluidity, and neural activity related to motor preparation (stimulus-locked lateralized readiness potential, S-LRP) and execution (response-locked LRP) was assessed using EEG. All participants completed the Brief Psychiatric Rating Scale; patients were additionally assessed for lifetime psychosis and mood episode symptoms, and relatives and controls completed the Chapman psychosis proneness scales.
Results:
Multiple regression revealed levels of current negative symptoms and mania were significantly positively associated with psychomotor slowing even after accounting for current antipsychotic medication dosage and duration of illness. S-LRP onset latency was significantly positively associated with magical ideation.
Conclusion:
Domains of motor function are associated with various mood and psychosis symptom domains in a transdiagnostic sample, which may provide insight into brain abnormalities relevant to the expression of symptoms across disorders.
Keywords: psychomotor slowing, dyskinesia, lateralized readiness potential, psychosis, bipolar disorder
Introduction
Empirical evidence of motor abnormalities in the psychosis spectrum has steadily accrued over the past few decades. The term “motor abnormalities” is intentionally broad, reflecting the diverse array of disturbances and dysfunction that have been reported in this population. These motor abnormalities range from involuntary movements (i.e., spontaneous dyskinesia [1,2]), to disturbances in the execution of voluntary movement (e.g., disruptions in motor coordination and sequencing [3], slowness of movement [4]), and also include spontaneous Parkinsonism [1,2] and the heterogeneous syndrome catatonia [5] (see Walther and Strik [6] and van Harten and colleagues [7] for reviews). It is important to note that all voluntary motor actions involve varying degrees of non-motor processes; therefore, “psychomotor abnormalities” is a more accurate descriptor for most of the motor abnormalities outlined above (see Morrens and colleagues [4] for discussion). The identification of motor abnormalities in the psychosis spectrum has highlighted specific brain regions that may be relevant to the pathophysiology of the disorder (e.g., cerebellar dysfunction [8]), and dyskinesia appears to have prognostic value for the development of a psychotic disorder [9,10].
Motor function has also been studied in biological first-degree relatives of individuals with schizophrenia, who carry genetic liability for the disorder. Abnormalities in a number of domains of motor behavior have been reported in this population, suggesting that motor abnormalities may be an endophenotype reflecting genetic contributions to psychosis. For example, meta-analyses have indicated the presence of motor abnormalities in first-degree relatives that include spontaneous dyskinesia [2] (see also Koning and colleagues [11], but see Kent and colleagues [12]), spontaneous Parkinsonism [2] (see also Koning and colleagues [11] and Kamis and colleagues [13]), and neurological soft signs [14,15]. Also, meta-analyses of cognitive and neuropsychological function have revealed psychomotor slowing in first degree relatives [16,17].
Outside of the psychomotor disturbances characteristic of mood states (i.e., psychomotor retardation and agitation; increased and decreased activity levels [18,19]), relatively little attention has been paid to motor function in bipolar disorder. While there is less work examining motor function in bipolar disorder than first-degree relatives of individuals with schizophrenia, there are data to suggest that similar motor abnormalities exist in this population, although the extent to which each motor domain has been studied varies considerably. For example, a meta-analysis of euthymic individuals with bipolar disorder revealed psychomotor slowing in this population, though medication confounds complicated the interpretation of these results [20] (see also Correa-Ghisays and colleagues [21]). Neurological soft signs have been reported in bipolar disorder (see Hirjak and colleagues [22] and Peralta and Cuesta [23] for reviews), including in currently psychotic individuals [24,25], individuals with no history of psychosis [26], and euthymic individuals [27]. Bolbecker and colleagues [28] reported balance impairments in euthymic individuals with bipolar disorder during a static task, while Kang and colleagues [29] reported impaired balance in depressed but not euthymic individuals with bipolar disorder during a dynamic task. Dyskinesia has also been reported in bipolar disorder [30,31], including one study of euthymic individuals [32], as has Parkinsonism [30].
Findings of motor abnormalities in bipolar disorder are especially interesting when various similarities between bipolar disorder and schizophrenia are considered. Bipolar disorder and schizophrenia have been shown to share genetic risk factors [33]. In addition, there is substantial symptom overlap between psychotic and bipolar disorders. This is most apparent in schizoaffective disorder, wherein both mood and psychotic symptoms are prominent features, and the psychotic features that can be present during mood episodes in bipolar disorder. However, both mood symptoms and episodes also occur in schizophrenia [18], and the status of schizoaffective disorder as a distinct nosological entity has been called into question (see for example Peralta and Cuesta [34]). Given that symptom domains and motor abnormalities are shared by psychotic disorders and bipolar disorder, it would be informative to understand whether specific symptom domains are associated with particular motor abnormalities in a transdiagnostic sample. A relationship between a specific motor abnormality and transdiagnostic clinical phenotype could provide insight into the nature of the transdiagnostic occurrence of the motor dysfunction, and may indicate shared neural substrates, which could enhance our understanding of the underlying neural bases of various symptom domains.
A related question arises when considering subthreshold symptom expression in biological first-degree relatives. In addition to carrying genetic liability for psychosis, as a group these individuals display greater schizotypal symptoms than controls that are similar in content, but not in severity, to domains of symptomatology seen in psychosis (see for example Calkins and colleagues [35]). It is therefore of interest to examine if motor abnormalities in this population are associated with schizophrenia spectrum symptomology.
The current study aimed to investigate the mapping of different motor abnormalities onto dimensions of psychotic and mood symptomatology. As discussed above, there are many aspects of (psycho)motor functioning that have been investigated in the context of psychosis, and a comprehensive investigation including each type of motor abnormality that has been studied in psychosis is out of the scope of the current paper. In this study, we examined two aspects of motor behavior (movement fluidity and psychomotor speed) which we hypothesized to be related to specific symptom domains for associations with various psychotic, mood, and subthreshold psychosis symptom dimensions in transdiagnostic samples. We did the same in a more exploratory capacity for EEG measures of neural activity preceding action. Specifically, we examined the relationship of lifetime occurrence of mood and psychotic symptom domains to these motor variables in a sample of individuals with schizophrenia, schizoaffective disorder, or bipolar disorder. We also examined the relationship of four domains of subthreshold psychotic symptomology (magical ideation, perceptual aberrations, social anhedonia, and physical anhedonia) to motor variables in controls and first-degree biological relatives of individuals with a psychotic disorder. Finally, the relationship of these motor variables to current levels of psychotic and mood symptom domains was explored across all participants.
It should be noted that unipolar depression is also associated with various psychomotor abnormalities (e.g., see Sobin and Sackeim [19] and Peralta and Cuesta [23] for reviews; see also Lohr and colleagues [36]). The associations between depression as a symptom domain and motor variables will be explored in the current study. However, given that the focus of this study is on the schizophrenia/schizoaffective disorder/bipolar disorder spectrum, individuals with unipolar depression are not included as a patient group.
Our hypotheses regarding which symptom domains would be predictive of motor function were grounded in the literature specific to each motor domain investigated. There have been studies demonstrating the association of psychomotor slowing with negative symptoms in schizophrenia (see Morrens and colleagues [4] for review; see also Norman and colleagues [37], Docx and colleagues [38], and Bervoets and colleagues [39]). It has been hypothesized that psychomotor slowing is one motor component of a “negative syndrome” [38]. In addition, psychomotor slowing is a symptom of depression [18], and an association between depressive symptoms and psychomotor slowing has been reported in schizophrenia ([40]; see Morrens and colleagues [4] for review). The possibility that psychomotor slowing (and other deficits) could have the same neural and psychological substrates in individuals with psychotic disorders experiencing depression as those in individuals with depression has been suggested [40]. Therefore, we hypothesize that the negative symptoms and depression symptom domains will be associated with psychomotor slowing.
Dyskinesia results from basal ganglia abnormalities [41,42], and striatal hyperdopaminergia is a possible contributing mechanism [42]. Striatal hyperdopaminergia has been hypothesized to be an important mechanism in the development of psychosis, particularly positive symptoms [43]. Given this possible shared mechanism, we hypothesize that only the positive symptoms of psychosis will be related to dysfluent movement. Importantly, the movement fluidity data reported here represent a secondary analysis of data previously published. In Kent and colleagues [12], we reported significantly increased movement dysfluency in a group of individuals with both schizophrenia and schizoaffective disorder (compared to both controls and relatives), but no difference in movement fluency between controls and relatives. Given the possible shared mechanism discussed above, it is possible that increased dysfluency would only be expected in non-proband participants experiencing subthreshold “positive” symptoms. We therefore hypothesize that such symptoms (i.e., magical ideation and perceptual aberrations) will be associated with more dysfluent movement in the combined control and relative sample (note: these Chapman scales provide a richer characterization of these symptoms in comparison to the schizotypal personality questionnaire utilized in Kent and colleagues [12]).
Neural activity preceding action was investigated using the lateralized readiness potential (LRP). The LRP is calculated by subtracting EEG activity recorded from electrodes on opposite sides of the motor strip during a window preceding a response, with activity specific to the contralateral cortex believed to reflect processes related to motor preparation and execution [44,45]. The LRP can be measured in relation to stimulus presentation or to response execution. The onset latency of the stimulus-locked LRP (S-LRP) reflects the time between stimulus presentation and the activation of motor preparatory processes, while the onset latency of the response-locked LRP (R-LRP) (measured in milliseconds before the response) reflects the time required for response execution once motor preparatory processes have been initiated [46]. Several studies have reported S-LRP onset latency delays in schizophrenia [46–49], while the literature examining R-LRP onset latency in schizophrenia has been mixed [46–50]. Here again, we are conducting a secondary analysis on data that we have previously published [51]. In Van Voorhis and colleagues [51], we reported significantly later S-LRP onset latency in both (1) individuals with schizophrenia or schizoaffective disorder and (2) individuals with bipolar disorder compared to first-degree relatives of individuals with a psychotic disorder, but not controls; there were no differences between groups in R-LRP onset latency. We do not have any specific hypotheses regarding which symptoms will be associated with variance in S-LRP onset latency, however given that relatives and controls were not significantly different from each other in Van Voorhis and colleagues [51], we hypothesize that subthreshold psychotic symptomology will be associated with S-LRP onset latency in these groups (i.e., any attenuated abnormality might only show up in individuals displaying some degree of subthreshold symptoms). Given the mixed findings regarding R-LRP onset latency in the literature, these analyses are considered exploratory.
Materials and Methods
1. Participants
The sample was composed of 149 individuals from the following groups: 32 individuals with schizophrenia (mean age = 40.31 years, SD = 11.44 years; 22 male), 14 individuals with schizoaffective disorder (10 with bipolar type, 4 with depressive type; mean age = 45.07 years, SD = 10.05 years; 9 male), 17 individuals with bipolar I disorder (mean age = 47.12 years, SD = 11.10 years; 14 male), 43 biological first-degree relatives of individuals with either schizophrenia or schizoaffective disorder (mean age = 45.86 years, SD = 10.96 years; 18 male), and 43 controls (mean age = 45.42 years, SD = 11.56 years; 24 male).
Three individuals in the schizophrenia group also had diagnoses of bipolar disorder not otherwise specified, and 9 individuals had other current or lifetime mood disorder diagnoses (n = 2 with major depressive disorder; n = 7 with depressive disorder not otherwise specified). Thirteen individuals with bipolar I disorder had a history of psychotic features during a mood state. Current mood states for the individuals with bipolar I disorder at the time of participation in this study were n = 4 depressed, n = 12 euthymic, and n = 1 unknown. All individuals in the patient groups were outpatients, and diagnoses were determined via clinical interview by trained psychodiagnosticians and subsequent review of these materials by doctoral students or doctoral-level staff (see Procedures section below for details).
One relative had a diagnosis of psychotic disorder not otherwise specified, one had a diagnosis of bipolar I disorder (current mood state euthymic, no history of psychotic features), and 12 had lifetime unipolar mood disorder diagnoses (n = 8 with major depressive disorder; n = 2 with depressive disorder not otherwise specified; n = 1 with a mood disorder due to a general medical condition; n = 1 with a substance-induced mood disorder). Two relatives (including one who had a unipolar mood disorder diagnosis) had Axis II Cluster A diagnoses (n = 1 with schizoid personality disorder; n = 1 with paranoid personality disorder).
Control participants had no current or past Axis I mood or psychotic disorders, no Axis II Cluster A personality disorders, and denied a family history of psychotic disorders. No participants had current alcohol or substance abuse or dependence diagnoses, and no participants in the patient groups were taking anti-Parkinsonian medications. In the patient groups, 54 individuals were taking antipsychotic medication (n = 5 taking typical antipsychotics); 33 individuals were taking mood stabilizers (n = 7 taking Lithium, n = 24 taking divalproex sodium, and n = 7 taking other mood stabilizers); 27 individuals were taking antidepressants (n = 10 taking SSRIs, n = 1 taking an MAOI, and n = 17 taking other antidepressants); and 8 individuals were taking benzodiazepines. Of the relatives carrying diagnoses described above, 6 were taking antidepressants, and 1 was taking an atypical antipsychotic medication. Chlorpromazine equivalent dosages (CPZ) were computed for individuals with complete antipsychotic medication dosage data [52].
Not all participants completed every motor task and clinical assessment. Table 1 provides the sample for each motor and clinical measure for each diagnostic group, as well as means and standard deviations. As discussed in the introduction, a portion of the data presented in this study is a secondary analysis of previously published data. Specifically, the movement fluidity data from the individuals with schizophrenia or schizoaffective disorder, relatives, and controls were presented in Kent and colleagues [12]. Movement fluidity data from the participants with bipolar I disorder have not been previously published. The participants with LRP data in this study are subsamples of the schizophrenia/schizoaffective disorder, depressive type, bipolar disorder, relative, and control samples reported in Van Voorhis and colleagues [51], and reflect participants for whom both LRP and movement fluidity data were available. LRP data from individuals with schizoaffective disorder, bipolar type and an additional 6 relatives have not been previously published.
Table 1.
Sample size, mean, and standard deviation for demographic, cognitive, clinical, and motor measures for each group.
| Schizophrenia | Schizoaffective Disorder | Bipolar Disorder | Relative | Control | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | n | Mean | SD | n | Mean | SD | n | Mean | SD | ||
| BPRS | Positive Symptoms | 32 | 2.48 | 1.11 | 14 | 2.36 | 0.93 | 17 | 1.45 | 0.77 | 43 | 1.17 | 0.38 | 42 | 1.11 | 0.23 |
| Negative Symptoms | 32 | 2.05 | 1.19 | 14 | 1.76 | 1.09 | 17 | 1.57 | 0.94 | 43 | 1.19 | 0.38 | 42 | 1.17 | 0.36 | |
| Disorganization | 32 | 1.85 | 0.82 | 14 | 1.95 | 0.79 | 17 | 1.60 | 0.49 | 43 | 1.29 | 0.32 | 42 | 1.23 | 0.31 | |
| Mania | 32 | 1.39 | 0.94 | 14 | 1.48 | 0.91 | 17 | 1.47 | 0.70 | 43 | 1.17 | 0.46 | 42 | 1.10 | 0.22 | |
| Depression | 32 | 2.01 | 0.80 | 14 | 2.79 | 1.13 | 17 | 2.61 | 1.23 | 43 | 1.71 | 0.78 | 42 | 1.59 | 0.65 | |
|
| ||||||||||||||||
| OPCRIT | Mania | 26 | 1.12 | 2.36 | 10 | 4.75 | 1.83 | 10 | 5.63 | 1.07 | ||||||
| Reality Distortion | 26 | 2.42 | 1.22 | 10 | 2.25 | 1.14 | 10 | 0.86 | 1.18 | |||||||
| Depression | 26 | 1.75 | 1.93 | 10 | 4.84 | 0.37 | 10 | 3.55 | 2.19 | |||||||
| Disorganization | 26 | 2.03 | 1.12 | 10 | 2.19 | 1.43 | 10 | 1.43 | 1.32 | |||||||
| Negative Symptoms | 26 | 1.01 | 0.74 | 10 | 1.13 | 0.67 | 10 | 0.62 | 0.62 | |||||||
|
| ||||||||||||||||
| Chapman Scales | Perceptual Aberrations | 22 | 2.09 | 4.97 | 36 | 1.17 | 1.46 | |||||||||
| Physical Anhedonia | 22 | 10.69 | 5.91 | 36 | 9.17 | 4.72 | ||||||||||
| Magical Ideation | 22 | 4.14 | 4.39 | 36 | 2.71 | 2.81 | ||||||||||
| Social Anhedonia | 22 | 9.19 | 6.74 | 36 | 7.18 | 4.70 | ||||||||||
|
| ||||||||||||||||
| Trails A (sec) | 17 | 29.76 | 8.48 | 10 | 25.70 | 7.27 | 10 | 27.40 | 6.88 | 43 | 22.67 | 6.03 | 28 | 22.57 | 5.85 | |
| Average log(ANJ) | 32 | 1.41 | 0.24 | 14 | 1.45 | 0.33 | 12 | 1.30 | 0.17 | 43 | 1.25 | 0.22 | 43 | 1.24 | 0.21 | |
| RLRP Onset Latency (ms) | 25 | −123.28 | 59.84 | 12 | −108.40 | 52.83 | 14 | −109.10 | 54.33 | 35 | −122.99 | 48.21 | 37 | −121.62 | 41.27 | |
| SLRP Onset Latency (ms) | 23 | 200.07 | 53.30 | 12 | 206.71 | 45.60 | 14 | 207.87 | 60.32 | 34 | 174.06 | 38.52 | 37 | 178.74 | 37.57 | |
| Age | 32 | 40.31 | 11.44 | 14 | 45.07 | 10.05 | 17 | 47.12 | 11.10 | 43 | 45.86 | 10.96 | 43 | 45.42 | 11.56 | |
| Estimated IQ | 30 | 89.50 | 11.25 | 14 | 100.50 | 14.06 | 14 | 99.64 | 14.66 | 43 | 107.51 | 13.99 | 43 | 106.74 | 14.07 | |
| CPZ (mg) | 26 | 538.46 | 323.21 | 13 | 446.15 | 443.69 | 16 | 85.31 | 184.98 | 43 | 0.29 | 1.91 | 43 | 0 | 0 | |
2. Procedures
Clinical and cognitive assessment.
Procedures were approved by institutional review boards from the Minneapolis VA Health Care System and the University of Minnesota. Data collection occurred as a part of a larger study of individuals with a psychotic disorder or bipolar disorder and their biological first-degree relatives (see Docherty and Sponheim [53] for recruitment procedures). After an informed consent process, participants were administered the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I [54]) and the Brief Psychiatric Rating Scale (BPRS [55]). IQ was estimated using the Vocabulary and Block Design subtests of the Wechsler Adult Intelligence Scale [56]. Diagnoses (or lack thereof) were determined for each participant through review of all clinical research assessments by advanced clinical psychology graduate students or postdoctoral researchers in consultation with clinical psychologists, and a minimum of two such individuals reached consensus on all diagnoses.
The Operational Criteria Checklist for Psychotic and Affective Illness (OPCRIT) [57] was additionally completed for individuals with a psychotic or bipolar disorder. The OPCRIT records information on the lifetime presence and severity of various psychotic and mood episode symptoms. Controls and relatives of individuals with a psychotic disorder additionally completed the Chapman psychosis proneness scales measuring magical ideation [58], perceptual aberrations [59], physical anhedonia [60], and social anhedonia [61].
Assessments of motor function.
To assess psychomotor speed, participants were administered the Trail Making Test Part A (Trails A) [62], with time (in seconds) serving as the dependent variable.
As stated in the introduction, this study represents a secondary analysis of the movement fluidity data presented in Kent et al. [12], wherein details regarding data collection and processing are outlined. Briefly, participants completed a handwriting task using a non-inking pen and a Wacom Intuos 3 digitizing tablet (Wacom, Saitama, Japan) connected to a computer. For the task, participants wrote “lleellee” in cursive in 1 cm, 2 cm, and 4 cm size conditions, completing five trials of each condition in random order. Each participant had a minimum of three acceptable trials (trials with too few strokes or that were interrupted were discarded), and the first eight strokes of each trial were subjected to movement fluidity analysis.
MovAlyzeR software (Neuroscript, LLC, Tempe, AZ) was used to sample pen movements and for data processing and analysis. Data processing steps and additional analysis details are described in Caligiuri and colleagues [63] and Kent and colleagues [12]. Briefly, average normalized jerk (ANJ) was calculated [64] as an index of movement smoothness [65]. Jerk, the third time derivative, is calculated and normalized for vertical stroke size and duration (resulting in a unit-free value) [64], and averaged across strokes and trials. ANJ, which reflects changes in acceleration during movement, has been used previously to quantify dysfluent movement, or dyskinesia (indicated by higher ANJ values) [12,63,64,66,67]. Because our previous work demonstrated no main effect or interactions involving the size condition [12], we averaged ANJ across size conditions for the current secondary analysis.
Similarly, we are conducting a secondary analysis of LRP data for the current study. Data were collected as a part of a stop signal task (SST) paradigm, which was used to investigate the neural correlates of motor inhibition [51]. The SST comprised a Go Only condition and a Go/Stop condition. The current secondary analysis only examined data from the Go Only condition, wherein participants responded to an X replacing either the left or the right crosshair in a row of three crosshairs by pushing a button with their corresponding thumb as quickly as possible. In the Go/Stop condition, a stop signal appeared after a variable delay on 20% of trials, requiring participants to inhibit their responses. The SST had five blocks, each consisting of 20 Go Only trials, followed by 120 Go/Stop trials, and then 20 Go Only trials; there were never any stop trials during the Go Only trials.
Additional task details and full description of EEG data collection, processing, and analysis are provided in Van Voorhis and colleagues [51]. Briefly, EEG data were collected with either 64- or 128-channel Ag/AgCl electrode arrays and a Biosemi ActiveTwo system (1024 Hz sampling rate, single earlobe reference signal). Data were re-referenced to linked earlobes, filtered (0.5 Hz high-pass filter, 256 Hz low-pass filter), and de-noised via visual inspection and independent component analysis (ICA) decomposition [68] and removal of noise ICs. Reconstituted de-noised data were average head re-referenced and epoched and averaged to form event-related potentials (ERPs) for various conditions [51].
The current analysis examines S-LRP and R-LRP onset latencies from the Go Only condition. As described in detail in Van Voorhis and colleagues [51], LRPs were calculated by low-pass filtering (8 Hz), baseline correcting, and then averaging waveforms for electrodes C3 and C4 for both left and right hand responses. Next, subtraction waveforms were computed to reflect LRP activity corresponding to both left and right hand responses and then averaged. See Van Voorhis and colleagues [51] for details regarding LRP onset latency calculations, as well as criteria for inclusion of LRP data for each participant.
Statistical Analysis.
As an index of current psychotic and mood symptom severity, we averaged BPRS item ratings corresponding to each of the five factors identified by Wilson & Sponheim [69] (positive symptoms, negative symptoms, disorganization, mania symptoms, and depression/anxiety symptoms). As an index of lifetime psychotic and mood symptom expression, we multiplied binary (i.e., symptom coded as present or not present) OPCRIT items by their respective factor loadings [70], which were then summed according to the five factors identified by Dikeos and colleagues [70] (mania, reality distortion, depression, disorganization, and negative symptoms). Total number of pathological items endorsed was summed for each of the four Chapman scales.
Multiple regression models were used to investigate the association between the domains of each of the three symptom measures (BPRS, OPCRIT, and Chapman Scales) and each of the motor indices (Trails A, ANJ, and LRP). There was a significant pairwise correlation observed between R-LRP and S-LRP onset latency (r=0.42, p<0.001), prompting the use of multivariate multiple regression with two dependent variables (S-LRP onset latency, R-LRP onset latency) for all models predicting LRP onset latency. In all models, age and sex were included as covariates due to their observed association with the outcome variables (age associated with S-LRP [p<0.001] and Trails A [p=0.019]; sex associated with ANJ [p=0.001] and S-LRP [p=0.005]). Number of errors was included as a covariate for all models predicting Trails A completion time. Each model included only participants who completed both of the relevant measures; the number of participants from each group included in each model is listed in table 2.
Table 2.
Number of participants from each group who have both a given motor and clinical measure.
| Schizophrenia | Schizoaffective Disorder | Bipolar Disorder | Relative | Control | |
|---|---|---|---|---|---|
| BPRS-Trails A | 17 | 10 | 10 | 42 | 26 |
| OPCRIT-Trails A | 12 | 6 | 6 | ||
| Chapman-Trails A | 21 | 21 | |||
| BPRS-ANJ | 32 | 14 | 12 | 43 | 42 |
| OPCRIT-ANJ | 26 | 10 | 7 | ||
| Chapman-ANJ | 22 | 36 | |||
| BPRS-RLRP | 25 | 12 | 14 | 35 | 36 |
| OPCRIT-RLRP | 19 | 10 | 8 | ||
| Chapman-RLRP | 17 | 32 | |||
| BPRS-SLRP | 23 | 12 | 14 | 34 | 36 |
| OPCRIT-SLRP | 17 | 10 | 8 | ||
| Chapman-SLRP | 16 | 32 |
For models involving the patient groups that yielded significant effects, we conducted follow-up analyses to explore and account for possible effects of antipsychotic medication and duration of illness on the variables of interest. Specifically, models were re-run including only patients for whom complete antipsychotic medication dosage data were available, and then these new models were run again including chlorpromazine equivalent dosages and duration of illness as covariates.
Results
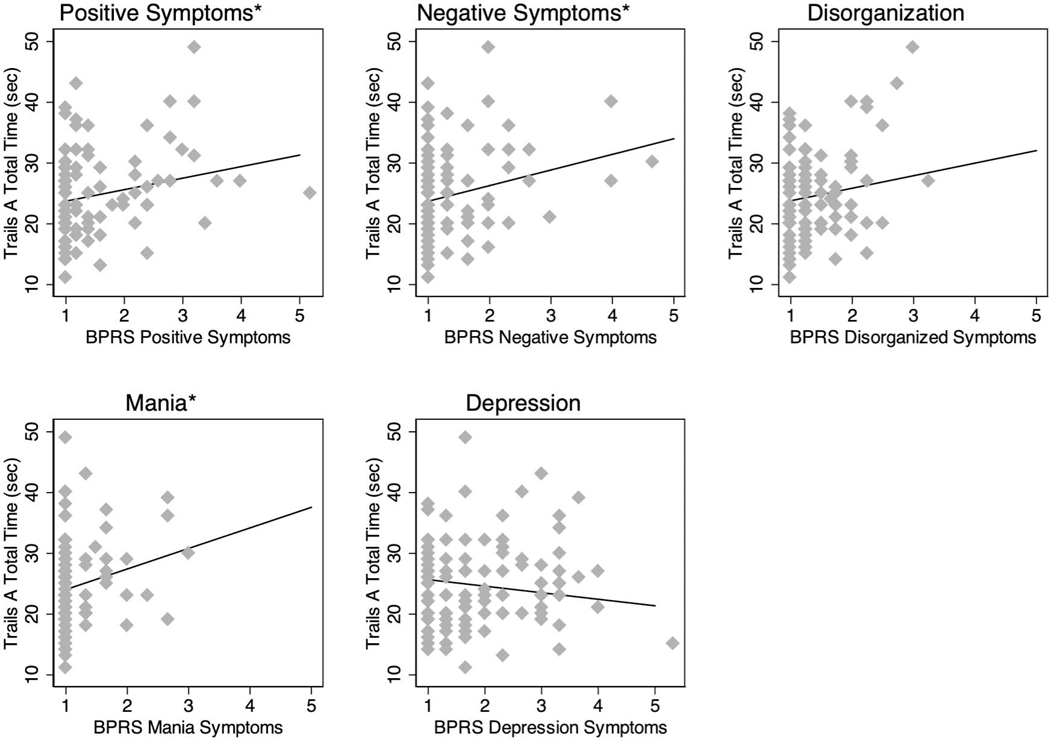
The model investigating the relationship between current symptom severity, measured using the BPRS, and Trails A performance yielded several significant associations (see figure 1). Time to complete Trails A was significantly associated with positive symptoms (β=0.22, t=2.09, p=0.040), mania (β=0.20, t=2.02, p=0.047), and negative symptoms (β=0.24, t=2.33, p=0.022) (full model statistics: F(8,96)=4.44, p=0.0001, adjusted R-squared=0.21). All associations were in the positive direction, meaning that increased symptoms were associated with increased time to complete Trails A. There was no significant association between BPRS factor severity and ANJ (all p>0.1). There was no significant association between BPRS factor severity and either of the LRP indices (all p>0.1).
Figure 1.
Associations between BPRS symptom factors and Trails A (* = p<0.05).
Amongst the lifetime symptom factors in patients, measured using the OPCRIT, there was a trend-level association between reality distortion (delusions and hallucinations) and Trails A completion time (β=0.45, t=1.87, p=0.081) (full model statistics: F(8,15)=1.14, p=0.3952, adjusted R-squared=0.05). The direction of this association indicates that greater lifetime reality distortion symptoms was associated with longer Trails A completion time. However, this result stems from a markedly smaller sample than the previously reported BPRS findings (n=24, vs. n=105 in the BPRS analysis). Reality distortion showed a significant association with S-LRP onset latency (β=−0.37, t=−2.36, p=0.026) (full model statistics for S-LRP: F(7,27)=3.27, p=0.0120, adjusted R-squared=0.32). The negative association in this reality distortion finding suggests that these symptoms were related to faster S-LRP onset latency when accounting for all other OPCRIT symptom factors, however it is important to note that the sample for this analysis was also quite small (n=35). There was no significant association between OPCRIT factors and the other motor indices (all p>0.1).
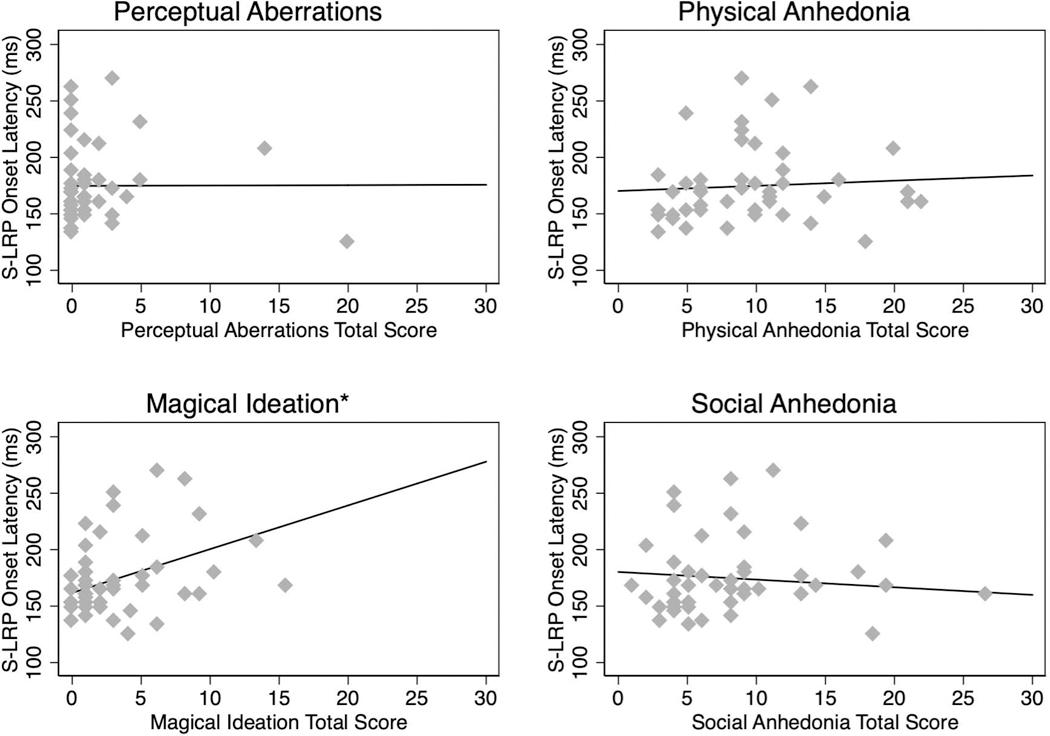
Subthreshold symptom severity, measured using the Chapman scales, was not associated with Trails A or ANJ (all p>0.1). However, there was a significant association between the magical ideation score and S-LRP onset latency (β=0.42, t=2.99, p=0.005) (full model statistics for S-LRP: F(6,41)=4.22, p=0.0021, adjusted R-squared=0.29) (figure 2). The positive direction of this association indicates that greater magical ideation was associated with longer S-LRP onset latency. This analysis did not include the two relatives with psychotic disorder not otherwise specified and bipolar disorder diagnoses due to lack of Chapman data from these participants. β, t, and p values for all models are listed in table 3.
Figure 2.
Associations between the Chapman scales and S-LRP onset latency (* = p<0.01).
Table 3.
Statistics for all models.
| Trails A | ANJ | S-LRP | R-LRP | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measure | Factor/Symptom | n | β | T | p | n | β | T | p | n | β | T | p | n | β | T | p |
| BPRS | Positive Symptoms | 105 | 0.215 | 2.090 | 0.040 | 143 | 0.127 | 1.320 | 0.188 | 119 | 0.011 | 0.110 | 0.915 | 122 | 0.107 | 0.940 | 0.350 |
| Negative Symptoms | 105 | 0.245 | 2.330 | 0.022 | 143 | 0.130 | 1.490 | 0.139 | 119 | 0.099 | 1.030 | 0.303 | 122 | 0.014 | 0.130 | 0.897 | |
| Disorganization | 105 | 0.144 | 1.190 | 0.235 | 143 | 0.174 | 1.460 | 0.148 | 119 | 0.067 | 0.550 | 0.584 | 122 | −0.051 | −0.370 | 0.709 | |
| Mania | 105 | 0.198 | 2.020 | 0.047 | 143 | 0.072 | 0.700 | 0.487 | 119 | 0.058 | 0.530 | 0.597 | 122 | −0.034 | −0.280 | 0.782 | |
| Depression | 105 | −0.144 | −1.370 | 0.173 | 143 | −0.028 | −0.310 | 0.760 | 119 | 0.116 | 1.200 | 0.232 | 122 | 0.046 | 0.430 | 0.667 | |
|
| |||||||||||||||||
| OPCRIT | Mania | 24 | 0.053 | 0.200 | 0.846 | 43 | 0.121 | 0.600 | 0.556 | 35 | 0.187 | 1.160 | 0.254 | 37 | 0.210 | 1.060 | 0.296 |
| Reality Distortion | 24 | 0.448 | 1.870 | 0.081 | 43 | −0.069 | −0.390 | 0.701 | 35 | −0.373 | −2.360 | 0.026 | 37 | 0.022 | 0.110 | 0.912 | |
| Depression | 24 | −0.267 | −1.070 | 0.302 | 43 | −0.059 | −0.310 | 0.757 | 35 | −0.091 | −0.570 | 0.573 | 37 | −0.035 | −0.180 | 0.858 | |
| Disorganization | 24 | −0.206 | −0.760 | 0.459 | 43 | −0.071 | −0.400 | 0.691 | 35 | 0.009 | 0.050 | 0.960 | 37 | −0.215 | −1.060 | 0.297 | |
| Negative Symptoms | 24 | 0.186 | 0.690 | 0.498 | 43 | 0.082 | 0.470 | 0.643 | 35 | 0.067 | 0.450 | 0.657 | 37 | 0.156 | 0.850 | 0.401 | |
|
| |||||||||||||||||
| Chapman scales | Perceptual Aberrations | 42 | 0.262 | 1.360 | 0.182 | 58 | 0.163 | 1.050 | 0.300 | 48 | 0.004 | 0.020 | 0.981 | 49 | −0.018 | −0.100 | 0.917 |
| Physical Anhedonia | 42 | 0.062 | 0.260 | 0.794 | 58 | −0.003 | −0.020 | 0.987 | 48 | 0.071 | 0.420 | 0.678 | 49 | −0.014 | −0.070 | 0.947 | |
| Magical Ideation | 42 | −0.015 | −0.090 | 0.932 | 58 | 0.050 | 0.330 | 0.744 | 48 | 0.419 | 2.990 | 0.005 | 49 | 0.208 | 1.240 | 0.222 | |
| Social Anhedonia | 42 | 0.042 | 0.170 | 0.867 | 58 | −0.161 | −0.830 | 0.408 | 48 | −0.108 | −0.590 | 0.559 | 49 | 0.059 | 0.280 | 0.780 | |
p<0.1 p<0.05 p<0.01
Follow-up analyses
When the BPRS-Trails A model was re-run including only those participants for whom complete antipsychotic medication dosage data were available (n=102, 3 fewer participants), the significant associations between Trails A and negative symptoms (β=0.28, t=2.54, p=0.013) and mania (β=0.24, t=2.28, p=0.025) persisted, and the association between Trails A and positive symptoms dropped to β=0.17, t=1.63, p=0.106 (full model statistics: F(8,93)=3.69, p=0.0009, adjusted R-squared=0.18). When chlorpromazine equivalent dosage and duration of illness were entered into the model, both negative symptoms (β=0.30, t=2.71, p=0.008) and mania (β=0.21, t=2.02, p=0.046) were still significantly associated with Trails A (positive symptom association p=0.419). Chlorpromazine equivalent dosage was not significantly associated with Trails A (p = 0.858), and there was a trend-level association wherein longer duration of illness was associated with longer Trails A time (β=0.22, t=1.73, p=0.087) (full model statistics: F(10,91)=3.35, p=0.0009, adjusted R-squared=0.19).
When the OPCRIT-S-LRP model was re-run including only those participants for whom complete antipsychotic medication dosage data were available (n=30, 5 fewer participants), the significant association between reality distortion and S-LRP onset latency persisted (β=−0.42, t=−2.53, p=0.019) (full model statistics: F(7,22)=3.19, p=0.0173, adjusted R-squared=0.35). When chlorpromazine equivalent dosage and duration of illness were entered into the model, the significant association between reality distortion and S-LRP onset latency persisted (β=−0.42, t=−2.44, p=0.024). Neither chlorpromazine equivalent dosage (p=0.615) nor duration of illness (p=0.623) were significantly associated with S-LRP onset latency (full model statistics: F(9,20)=2.37, p=0.0516, adjusted R-squared=0.30).
In order to further examine the counterintuitive positive association between mania and Trails A, we conducted an exploratory analysis wherein status regarding taking divalproex sodium, a mood stabilizer with possible parkinsonian motor side effects [71], was included as a binary (i.e., taking or not taking divalproex sodium) covariate in the model already including chlorpromazine equivalent dosage and duration of illness as covariates. In this model, negative symptoms (β=0.26, t=2.30, p=0.024) were still significantly associated with Trails A, and the association between mania and Trails A dropped to the trend level (β=0.18, t=1.79, p=0.076). Neither chlorpromazine equivalent dosage (p = 0.844) nor duration of illness (p=0.422) were significantly associated with Trails A in this model, but there was a trend-level association wherein taking divalproex sodium was associated with longer Trails A time (β=0.22, t=1.86, p=0.066) (full model statistics: F(11,90)=3.45, p=0.0005, adjusted R-squared=0.21).
Discussion
Our examination of the association of deviations in motor function with symptomatology across psychotic and bipolar disorders revealed that multiple domains of current symptom severity are associated with psychomotor slowing. When current antipsychotic medication dosage and duration of illness were included in the model the relationships of negative symptoms and mania with psychomotor slowing are robust. While the association between negative symptoms and slower psychomotor activity is consistent with hypotheses and previous research (see introduction), the finding of increased mania being associated with slower psychomotor activity is unexpected given the psychomotor features characteristic of mania. While exploratory post-hoc medication analysis suggested that this relationship could be partially accounted for by mood stabilizing medication (though see below in the discussion for important caveats), the persistence of this relationship at the trend level is notable. Like all psychomotor tasks [4], Trails A involves non-motor processes. While speculative, it is possible that the association between Trails A completion time and mania severity reflects the impact of mania symptoms on the non-motor processes recruited (e.g., attention, goal directedness) by this task. It is important to note that variability in completion time associated with Trails A errors was accounted for in the models.
The finding of an association between magical ideation and S-LRP onset latency was broadly consistent with our hypothesis, indicating that S-LRP onset latencies more similar to those seen in psychosis are associated with more subthreshold psychosis symptoms. This finding compliments existing literature showing delayed S-LRP onset latency in individuals with psychosis [46–49], and suggests that S-LRP onset latency abnormalities in non-psychotic individuals are associated with intermediate symptom expression rather than genetic liability per se [51]. Longer S-LRP onset latency is reflective of delayed response selection and initiation of response preparation. However, to better understand what this abnormality associated with schizophrenia spectrum symptoms reflects, these findings must be considered in the context of the task. In a similar task, Kappenman and colleagues [46] demonstrated that task-relevant (i.e., responding as quickly and accurately as possible) higher-order processes affecting response selection and motor preparation explained S-LRP onset delays in individuals with schizophrenia. In addition, fMRI studies of speeded responding have implicated the basal ganglia, pre-SMA (supplementary motor area), and frontal areas [72–74].
It is difficult to know how to interpret the relationship between lifetime reality distortion symptoms and S-LRP onset latency in patients, as this relationship is in the opposite direction as that in controls and relatives. The smaller sample size for this analysis may be an important factor, and future work examining the relationship of motor function to indices of lifetime symptoms should include larger samples.
There are several limitations of the current study that must be addressed. First, antipsychotic medications have known motor side effects, and the fact that the majority of the patients in this study were taking antipsychotic medication poses a major confound for the study of motor function. We have attempted to account for effects related to current antipsychotic medication dosage and approximate duration of antipsychotic treatment by re-running all models with significant effects with chlorpromazine equivalent dosages and duration of illness included. However, motor side effects of antipsychotic medication are certainly related to more than simply current dosage, and while we have attempted to account for duration of treatment with antipsychotics by including duration of illness as a covariate as well, this is a very rough proxy and of course reflects additional factors. Furthermore, there is also the issue of shared variance between such covariates and diagnosis/symptoms, with this also being a serious concern for the exploratory analysis including on versus off divalproex sodium, making it difficult to draw firm conclusions regarding variance accounted for by medication. In summary, we have attempted to understand the effects that some medications may be having on our dependent variables, but this study is not designed to interrogate these questions.
In addition to the possibility of motor side effects, psychotropic medications impact symptoms as well, and therefore future research should study the relationship between symptom domains and motor function in medication-naïve samples. An additional limitation of this study relates to sample size. Because not all measures were administered to all participants, some models had smaller sample sizes than others, with the model examining the relationship of lifetime symptomology to psychomotor slowing in patients particularly underpowered, as previously noted.
A final limitation concerns the scope of the current study and of the particular motor measures used. Indeed, we have only been able to begin interrogating the broader question of the relationships between transdiagnostic motor dysfunction and clinical phenomenology. This is reflected in both the fact that we only included measures of three aspects of motor function, and in the limitations inherent to the specific measures we used. For example, Trails A assesses both motor speed and visual search [75], and it is therefore possible that the relationship between Trails A performance and symptoms reflects the relationship between visual search ability and symptoms to some degree. Importantly, while visual search ability could be considered a confound in the context of the current study given the nature of the Trails A task, it is essential to remember that all psychomotor functioning involves a variety of motor (e.g., speed, coordination) and non-motor processes (e.g., visuospatial monitoring, higher-order processes) [4]. Attempts to separate motor and non-motor processes are futile and given that non-motor processes are indeed essential to motor behavior [4], any such attempts, even if possible, would be of limited utility. In addition, as we have previously discussed [12], handwriting fluency is a less demanding neuromuscular control task than force stability maintenance; it is therefore possible that a different measure of dyskinesia could have been more sensitive to more subtle levels of dyskinesia. Finally, as discussed above, task parameters have been shown to affect group differences in S-LRP onset latency [46], thereby circumscribing the generalizability of our findings.
In conclusion, the results of the present study demonstrate the relationship between psychotic and mood symptom domains and domains of motor dysfunction in a transdiagnostic sample. Both mania and negative symptoms were associated with psychomotor slowing. In addition, a relationship between variability in psychomotor processes and subthreshold symptomology was demonstrated for S-LRP onset latency, which was related to magical ideation. It is possible that the pattern regarding which symptom domains are associated with various motor indices may highlight particular neural substrates as being potentially relevant for the expression of certain symptoms. Furthermore, investigation of the relationship of transdiagnostic symptom domains with motor function may aid in further identifying motor abnormalities relevant to psychopathology, which dovetails with the recent addition of a sensorimotor domain to the National Institute of Mental Health’s Research Domain Criteria framework.
Acknowledgement
We are grateful to Seung Suk Kang and Mallory Skorheim for assistance with EEG and handwriting data analysis, respectively.
Funding Sources
This research was supported by a Merit Review Award #I01CX000227 from the U.S. Department of Veterans Affairs, Clinical Sciences Research and Development Research Program and award number U01MH108150 from the National Institute of Mental Health to SRS. JSK was supported by a Ruth L. Kirschstein National Research Service Award (award number F32MH112334) from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the views of the Department of Veterans Affairs or the National Institutes of Health. These funding sources played no role in preparation of data or the manuscript.
Footnotes
Statement of Ethics
All participants gave written informed consent, and the study protocol was approved by the Minneapolis VA Health Care System and the University of Minnesota IRBs. This research was conducted in accordance with the Declaration of Helsinki.
Disclosure Statement
The authors have no conflicts of interest to declare.
References
- 1.Pappa S, Dazzan P: Spontaneous movement disorders in antipsychotic-naive patients with first-episode psychoses: a systematic review. Psychological medicine 2009;39:1065–1076. [DOI] [PubMed] [Google Scholar]
- 2.Koning JP, Tenback DE, van Os J, Aleman A, Kahn RS, van Harten PN: Dyskinesia and parkinsonism in antipsychotic-naive patients with schizophrenia, first-degree relatives and healthy controls: a meta-analysis. Schizophrenia bulletin 2010;36:723–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bombin I, Arango C, Buchanan RW: Significance and meaning of neurological signs in schizophrenia: two decades later. Schizophrenia bulletin 2005;31:962–977. [DOI] [PubMed] [Google Scholar]
- 4.Morrens M, Hulstijn W, Sabbe B: Psychomotor slowing in schizophrenia. Schizophrenia bulletin 2007;33:1038–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walther S, Strik W: Catatonia. CNS spectrums 2016;21:341–348. [DOI] [PubMed] [Google Scholar]
- 6.Walther S, Strik W: Motor symptoms and schizophrenia. Neuropsychobiology 2012;66:77–92. [DOI] [PubMed] [Google Scholar]
- 7.van Harten PN, Walther S, Kent JS, Sponheim SR, Mittal VA: The clinical and prognostic value of motor abnormalities in psychosis, and the importance of instrumental assessment. Neuroscience and biobehavioral reviews 2017;80:476–487. [DOI] [PubMed] [Google Scholar]
- 8.Andreasen NC, Pierson R: The role of the cerebellum in schizophrenia. Biological psychiatry 2008;64:81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Callaway DA, Perkins DO, Woods SW, Liu L, Addington J: Movement abnormalities predict transitioning to psychosis in individuals at clinical high risk for psychosis. Schizophrenia research 2014;159:263–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mittal VA, Walker EF: Movement abnormalities predict conversion to Axis I psychosis among prodromal adolescents. Journal of abnormal psychology 2007;116:796–803. [DOI] [PubMed] [Google Scholar]
- 11.Koning JP, Kahn RS, Tenback DE, van Schelven LJ, van Harten PN: Movement disorders in nonpsychotic siblings of patients with nonaffective psychosis. Psychiatry research 2011;188:133–137. [DOI] [PubMed] [Google Scholar]
- 12.Kent JS, Caligiuri MP, Skorheim MK, Lano TJ, Mittal VA, Sponheim SR: Instrument-based assessment of motor function yields no evidence of dyskinesia in adult first-degree biological relatives of individuals with schizophrenia and schizoaffective disorder. Psychiatry research 2019;272:135–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kamis D, Stratton L, Calvo M, Padilla E, Florenzano N, Guerrero G, Molina Rangeon B, Molina J, de Erausquin GA: Sex and laterality differences in parkinsonian impairment and transcranial ultrasound in never-treated schizophrenics and their first degree relatives in an Andean population. Schizophrenia research 2015;164:250–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan RC, Xu T, Heinrichs RW, Yu Y, Gong QY: Neurological soft signs in non-psychotic first-degree relatives of patients with schizophrenia: a systematic review and meta-analysis. Neuroscience and biobehavioral reviews 2010;34:889–896. [DOI] [PubMed] [Google Scholar]
- 15.Neelam K, Garg D, Marshall M: A systematic review and meta-analysis of neurological soft signs in relatives of people with schizophrenia. BMC psychiatry 2011;11:139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sitskoorn MM, Aleman A, Ebisch SJ, Appels MC, Kahn RS: Cognitive deficits in relatives of patients with schizophrenia: a meta-analysis. Schizophrenia research 2004;71:285–295. [DOI] [PubMed] [Google Scholar]
- 17.Snitz BE, Macdonald AW 3rd, Carter CS: Cognitive deficits in unaffected first-degree relatives of schizophrenia patients: a meta-analytic review of putative endophenotypes. Schizophrenia bulletin 2006;32:179–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA, American Psychiatric Association, 2013. [Google Scholar]
- 19.Sobin C, Sackeim HA: Psychomotor symptoms of depression. Am J Psychiatry 1997;154:4–17. [DOI] [PubMed] [Google Scholar]
- 20.Bora E, Yucel M, Pantelis C: Cognitive endophenotypes of bipolar disorder: a meta-analysis of neuropsychological deficits in euthymic patients and their first-degree relatives. Journal of affective disorders 2009;113:1–20. [DOI] [PubMed] [Google Scholar]
- 21.Correa-Ghisays P, Balanza-Martinez V, Selva-Vera G, Vila-Frances J, Soria-Olivas E, Vivas-Lalinde J, San Martin C, Borras AM, Ayesa-Arriola R, Sanchez-Moreno J, Sanchez-Ort J, Crespo-Facorro B, Vieta E, Tabares-Seisdedos R: Manual motor speed dysfunction as a neurocognitive endophenotype in euthymic bipolar disorder patients and their healthy relatives. Evidence from a 5-year follow-up study. Journal of affective disorders 2017;215:156–162. [DOI] [PubMed] [Google Scholar]
- 22.Hirjak D, Meyer-Lindenberg A, Fritze S, Sambataro F, Kubera KM, Wolf RC: Motor dysfunction as research domain across bipolar, obsessive-compulsive and neurodevelopmental disorders. Neuroscience and biobehavioral reviews 2018;95:315–335. [DOI] [PubMed] [Google Scholar]
- 23.Peralta V, Cuesta MJ: Motor Abnormalities: From Neurodevelopmental to Neurodegenerative Through “Functional” (Neuro)Psychiatric Disorders. Schizophrenia bulletin 2017;43:956–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whitty P, Clarke M, McTigue O, Browne S, Gervin M, Kamali M, Lane A, Kinsella A, Waddington J, Larkin C, O’Callaghan E: Diagnostic specificity and predictors of neurological soft signs in schizophrenia, bipolar disorder and other psychoses over the first 4 years of illness. Schizophrenia research 2006;86:110–117. [DOI] [PubMed] [Google Scholar]
- 25.Nasrallah HA, Tippin J, McCalley-Whitters M: Neurological soft signs in manic patients. A comparison with Schizophrenic and control groups. Journal of affective disorders 1983;5:45–50. [DOI] [PubMed] [Google Scholar]
- 26.Zhao Q, Ma YT, Lui SS, Liu WH, Xu T, Yu X, Tan SP, Wang ZR, Qu M, Wang Y, Huang J, Cheung EF, Dazzan P, Chan RC: Neurological soft signs discriminate schizophrenia from major depression but not bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry 2013;43:72–78. [DOI] [PubMed] [Google Scholar]
- 27.Chrobak AA, Siwek GP, Siuda-Krzywicka K, Arciszewska A, Starowicz-Filip A, Siwek M, Dudek D: Neurological and cerebellar soft signs do not discriminate schizophrenia from bipolar disorder patients. Prog Neuropsychopharmacol Biol Psychiatry 2016;64:96–101. [DOI] [PubMed] [Google Scholar]
- 28.Bolbecker AR, Hong SL, Kent JS, Klaunig MJ, O’Donnell BF, Hetrick WP: Postural control in bipolar disorder: increased sway area and decreased dynamical complexity. PloS one 2011;6:e19824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kang GE, Mickey BJ, Krembs BS, McInnis MG, Gross MM: The effect of mood phases on balance control in bipolar disorder. J Biomech 2019;82:266–270. [DOI] [PubMed] [Google Scholar]
- 30.Lohr JB, Caligiuri MP: Abnormalities in motor physiology in bipolar disorder. The Journal of neuropsychiatry and clinical neurosciences 2006;18:342–349. [DOI] [PubMed] [Google Scholar]
- 31.Crespo Y, Ibanez A, Soriano MF, Iglesias S, Aznarte JI: Handwriting movements for assessment of motor symptoms in schizophrenia spectrum disorders and bipolar disorder. PloS one 2019;14:e0213657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lage GM, Malloy-Diniz LF, Neves FS, Gallo LG, Valentini AS, Correa H: A kinematic analysis of manual aiming control on euthymic bipolar disorder. Psychiatry research 2013;208:140–144. [DOI] [PubMed] [Google Scholar]
- 33.Purcell SM, Wray NR, Stone JL, Visscher PM, O’Donovan MC, Sullivan PF, Sklar P: Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 2009;460:748–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peralta V, Cuesta MJ: Exploring the borders of the schizoaffective spectrum: a categorical and dimensional approach. Journal of affective disorders 2008;108:71–86. [DOI] [PubMed] [Google Scholar]
- 35.Calkins ME, Curtis CE, Grove WM, Iacono WG: Multiple dimensions of schizotypy in first degree biological relatives of schizophrenia patients. Schizophrenia bulletin 2004;30:317–325. [DOI] [PubMed] [Google Scholar]
- 36.Lohr JB, May T, Caligiuri MP: Quantitative assessment of motor abnormalities in untreated patients with major depressive disorder. Journal of affective disorders 2013;146:84–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Norman RM, Malla AK, Cortese L, Diaz F: Aspects of dysphoria and symptoms of schizophrenia. Psychological medicine 1998;28:1433–1441. [DOI] [PubMed] [Google Scholar]
- 38.Docx L, Morrens M, Bervoets C, Hulstijn W, Fransen E, De Hert M, Baeken C, Audenaert K, Sabbe B: Parsing the components of the psychomotor syndrome in schizophrenia. Acta Psychiatr Scand 2012;126:256–265 [DOI] [PubMed] [Google Scholar]
- 39.Bervoets C, Docx L, Sabbe B, Vermeylen S, Van Den Bossche MJ, Morsel A, Morrens M: The nature of the relationship of psychomotor slowing with negative symptomatology in schizophrenia. Cogn Neuropsychiatry 2014;19:36–46. [DOI] [PubMed] [Google Scholar]
- 40.Holthausen EA, Wiersma D, Knegtering RH, Van den Bosch RJ: Psychopathology and cognition in schizophrenia spectrum disorders: the role of depressive symptoms. Schizophrenia research 1999;39:65–71. [DOI] [PubMed] [Google Scholar]
- 41.Obeso JA, Rodriguez-Oroz MC, Stamelou M, Bhatia KP, Burn DJ: The expanding universe of disorders of the basal ganglia. Lancet 2014;384:523–531. [DOI] [PubMed] [Google Scholar]
- 42.Alexander GE, Crutcher MD, DeLong MR: Basal ganglia-thalamocortical circuits: parallel substrates for motor, oculomotor, “prefrontal” and “limbic” functions. Progress in brain research 1990;85:119–146. [PubMed] [Google Scholar]
- 43.Howes OD, Kapur S: The dopamine hypothesis of schizophrenia: version III--the final common pathway. Schizophrenia bulletin 2009;35:549–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Coles MG: Modern mind-brain reading: psychophysiology, physiology, and cognition. Psychophysiology 1989;26:251–269. [DOI] [PubMed] [Google Scholar]
- 45.Smulders FTY, Miller JO: The Lateralized Readiness Potential; in Kappenman ES, Luck SJ (eds): The Oxford Handbook of Event-Relaed Potential Components. New York, NY, Oxford University Press, 2011 [Google Scholar]
- 46.Kappenman ES, Luck SJ, Kring AM, Lesh TA, Mangun GR, Niendam T, Ragland JD, Ranganath C, Solomon M, Swaab TY, Carter CS: Electrophysiological Evidence for Impaired Control of Motor Output in Schizophrenia. Cerebral cortex (New York, NY : 1991) 2016;26:1891–1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kappenman ES, Kaiser ST, Robinson BM, Morris SE, Hahn B, Beck VM, Leonard CJ, Gold JM, Luck SJ: Response activation impairments in schizophrenia: evidence from the lateralized readiness potential. Psychophysiology 2012;49:73–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Karayanidis F, Nicholson R, Schall U, Meem L, Fulham R, Michie PT: Switching between univalent task-sets in schizophrenia: ERP evidence of an anticipatory task-set reconfiguration deficit. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology 2006;117:2172–2190. [DOI] [PubMed] [Google Scholar]
- 49.Luck SJ, Kappenman ES, Fuller RL, Robinson B, Summerfelt A, Gold JM: Impaired response selection in schizophrenia: evidence from the P3 wave and the lateralized readiness potential. Psychophysiology 2009;46:776–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kieffaber PD, O’Donnell BF, Shekhar A, Hetrick WP: Event related brain potential evidence for preserved attentional set switching in schizophrenia. Schizophrenia research 2007;93:355–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Van Voorhis AC, Kent JS, Kang SS, Goghari VM, MacDonald AW 3rd, Sponheim SR: Abnormal neural functions associated with motor inhibition deficits in schizophrenia and bipolar disorder. Hum Brain Mapp 2019;40:5397–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Andreasen NC, Pressler M, Nopoulos P, Miller D, Ho BC: Antipsychotic dose equivalents and dose-years: a standardized method for comparing exposure to different drugs. Biological psychiatry 2010;67:255–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Docherty AR, Sponheim SR: Anhedonia as a phenotype for the Val158Met COMT polymorphism in relatives of patients with schizophrenia. Journal of abnormal psychology 2008;117:788–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I). Arlington, American Psychiatric Publishing Incorporated, 1997. [Google Scholar]
- 55.Ventura J, Lukoff D, Nuechterlein KH, Liberman RP, Green MF, Shaner A: Manual for the Expanded Brief Psychiatric Rating Scale. International Journal of Methods in Psychiatric Research 1993;3:227–244. [Google Scholar]
- 56.Wechsler D: WAIS-III: Wechsler Adult Intelligence Scale (3rd ed.) Administration and Scoring Manual. San Antonio, TX, Psychological Corporation//Harcourt Brace, 1997. [Google Scholar]
- 57.McGuffin P, Farmer A, Harvey I: A polydiagnostic application of operational criteria in studies of psychotic illness. Development and reliability of the OPCRIT system. Archives of general psychiatry 1991;48:764–770. [DOI] [PubMed] [Google Scholar]
- 58.Eckblad M, Chapman LJ: Magical ideation as an indicator of schizotypy. Journal of consulting and clinical psychology 1983;51:215–225. [DOI] [PubMed] [Google Scholar]
- 59.Chapman LJ, Chapman JP, Raulin ML: Body-image aberration in Schizophrenia. Journal of abnormal psychology 1978;87:399–407. [DOI] [PubMed] [Google Scholar]
- 60.Chapman LJ, Chapman JP, Raulin ML: Scales for physical and social anhedonia. Journal of abnormal psychology 1976;85:374–382. [DOI] [PubMed] [Google Scholar]
- 61.Mishlove M, Chapman LJ: Social anhedonia in the prediction of psychosis proneness. Journal of abnormal psychology 1985;94:384–396. [DOI] [PubMed] [Google Scholar]
- 62.Reitan RM, Wolfson D: The Halstead-Reitan Neuropsychological Test Battery: Theory and Clinical Interpretation, ed 2nd. Tuscon, AZ, Neuropsychology Press, 1993. [Google Scholar]
- 63.Caligiuri MP, Teulings HL, Dean CE, Lohr JB: A quantitative measure of handwriting dysfluency for assessing tardive dyskinesia. Journal of clinical psychopharmacology 2015;35:168–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Teulings HL, Contreras-Vidal JL, Stelmach GE, Adler CH: Parkinsonism reduces coordination of fingers, wrist, and arm in fine motor control. Experimental neurology 1997;146:159–170. [DOI] [PubMed] [Google Scholar]
- 65.Hogan N, Flash T: Moving gracefully: quantitative theories of motor coordination. Trends in Neurosciences 1987;10:170–174. [Google Scholar]
- 66.Caligiuri MP, Teulings HL, Dean CE, Niculescu AB 3rd, Lohr JB: Handwriting movement kinematics for quantifying extrapyramidal side effects in patients treated with atypical antipsychotics. Psychiatry research 2010;177:77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dean DJ, Teulings HL, Caligiuri M, Mittal VA: Handwriting analysis indicates spontaneous dyskinesias in neuroleptic naive adolescents at high risk for psychosis. Journal of visualized experiments : JoVE 2013:e50852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hyvarinen A, Oja E: Independent component analysis: algorithms and applications. Neural networks : the official journal of the International Neural Network Society 2000;13:411–430. [DOI] [PubMed] [Google Scholar]
- 69.Wilson S, Sponheim SR: Dimensions underlying psychotic and manic symptomatology: Extending normal-range personality traits to schizophrenia and bipolar spectra. Comprehensive psychiatry 2014;55:1809–1819. [DOI] [PubMed] [Google Scholar]
- 70.Dikeos DG, Wickham H, McDonald C, Walshe M, Sigmundsson T, Bramon E, Grech A, Toulopoulou T, Murray R, Sham PC: Distribution of symptom dimensions across Kraepelinian divisions. The British journal of psychiatry : the journal of mental science 2006;189:346–353. [DOI] [PubMed] [Google Scholar]
- 71.Brugger F, Bhatia KP, Besag FM: Valproate-Associated Parkinsonism: A Critical Review of the Literature. CNS Drugs 2016;30:527–540. [DOI] [PubMed] [Google Scholar]
- 72.Forstmann BU, Dutilh G, Brown S, Neumann J, von Cramon DY, Ridderinkhof KR, Wagenmakers EJ: Striatum and pre-SMA facilitate decision-making under time pressure. Proceedings of the National Academy of Sciences of the United States of America 2008;105:17538–17542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.van Veen V, Krug MK, Carter CS: The neural and computational basis of controlled speed-accuracy tradeoff during task performance. Journal of cognitive neuroscience 2008;20:1952–1965. [DOI] [PubMed] [Google Scholar]
- 74.Ivanoff J, Branning P, Marois R: fMRI evidence for a dual process account of the speed-accuracy tradeoff in decision-making. PloS one 2008;3:e2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bowie CR, Harvey PD: Administration and interpretation of the Trail Making Test. Nature protocols 2006;1:2277–2281. [DOI] [PubMed] [Google Scholar]