Abstract
Objective:
Exposure to traumatic life events is associated increased risk of posttraumatic stress disorder (PTSD) and other mental health problems such as suicidal ideation (SI), alcohol use disorder (AUD), and decreased quality of life (QOL). Mindfulness, which involves attending to the present moment, may help individuals cope with traumatic events by increasing acceptance of trauma-related experiences, and decreasing trauma-related negative affect and avoidance of trauma reminders. The current study evaluated whether mindful attention to the present moment mediated the association between number of lifetime traumas and mental health.
Method:
The sample consisted of 1,268 trauma-exposed U.S. veterans who participated in the National Health and Resilience in Veterans Study, a nationally representative study of U.S. veterans. On average, the sample was 60.6 years of age (SD=15.2, range=20–94), predominantly male (89.8%), Caucasian (75.0%), and non-combat veterans (59.2%).
Results:
Path analyses revealed that mindfulness partially mediated the relation between number of lifetime traumas and PTSD symptoms (β= −0.55), AUD (β= −0.17), and QOL (β= 0.38), and fully mediated the relation between number of lifetime traumas and SI (β= −0.36).
Conclusions:
The relationship between lifetime trauma burden and various mental health issues of relevance to U.S. veterans may be mediated by mindfulness or the ability to pay attention to the present moment. Interventions that bolster mindfulness may help mitigate the negative impact of cumulative traumas in this population.
Keywords: MINDFULNESS, VETERANS, TRAUMA EXPOSURE, MENTAL HEALTH
Exposure to traumatic life events is common among adults in the United States, with the prevalence ranging between 40% and 90% (Breslau et al., 1998; Kessler et al., 1995; Kilpatrick et al, 2013). For example, a study of 2,953 adults from the general population found that 89.7% had been exposed to a traumatic event (Kilpatrick et al., 2013) as defined by the fifth edition of the American Psychiatric Association’s (APA’s) Diagnostic and Statistical Manual (DSM-5, 2013). Trauma exposure tends to be more prevalent in certain at-risk individuals, such as Armed Forces personnel (e.g., Brunet et al., 2015) who may be exposed to combat, as well as other service-related potentially traumatic events.
Exposure to traumatic events can lead to the development of mental health problems, as well as reduced quality of life (QOL; e.g., Afifi et al., 2007; Nygaard & Heir, 2012). Some of the more common problems include posttraumatic stress disorder (PTSD), major depressive disorder, substance use disorders, and other anxiety disorders (e.g., Galatzer-Levy et al., 2013; Kessler et al., 1995). Exposure to traumatic life events may also increase risk for suicidal ideation (SI; e.g., Belik et al, 2007; Beristianos et al., 2016; Stein et al., 2010). Importantly, exposure to multiple traumatic events is common (Kilpatrick et al., 2013) and increases in the number of traumas to which one has been exposed can have a cumulatively deleterious effect on mental and physical health (e.g., Breslau, Peterson, & Schultz, 2008; Green et al., 2000; Kraaij & de Wilde, 2001).
Although the link between exposure to multiple traumatic life events and mental health problems has been clearly established, research examining possible mediators of this association is limited. Identification of such mediators is important, as not all individuals who experience trauma will go on to develop psychological problems and in fact, the majority are resilient in the face of traumatic stressors (e.g., Bonnano et al., 2006). Furthermore, knowledge of mediators of the link between trauma exposure and mental health outcomes may help inform treatment and the development of more targeted clinical interventions.
One potential mechanism that has been gaining increased attention in the literature is mindfulness, which is broadly defined as paying attention to the present moment in a non-judgmental way (Kabat-Zinn, 1990). Mindfulness has been conceptualized as a unidimensional construct that focuses primarily on one’s ability to be attentive to and aware of what is taking place in the present moment (e.g., Brown & Ryan, 2003; 2004). Mindfulness has also been conceptualized as a multidimensional construct that includes observing one’s internal and external experiences, describing one’s internal experiences with words, not judging one’s inner experiences, acting with awareness, and not reacting to those inner experiences (Baer et al., 2008).
Through mindfulness, one can cultivate awareness of their mental state and shift their attention from ruminative thought patterns to the present moment. In doing so, they may be better able to respond more flexibly in a given situation (Segal, Williams, & Teasdale, 2002). Thus, mindfulness may help individuals more effectively cope with the negative impact of traumatic events by increasing acceptance of trauma-related experiences, and decreasing negative affect related to the trauma and avoidance of trauma reminders (Schoorl et al., 2015). Mindfulness may also help a traumatized individual remain grounded and focused on the present moment, which may help in processing intrusive memories of previous traumas and mitigate emotional numbing symptoms (Boughner, Thornley, Kharlas, and Frewen, 2016). Support for the usefulness of mindfulness for trauma-exposed individuals comes from research showing that mindfulness is negatively correlated with the severity of PTSD-related avoidance (Thompson & Waltz, 2010). In addition, mindfulness-based treatments have been found to lead to improvements in PTSD symptoms, as well as depressive symptoms and QOL (see Boyd, Lanius, & McKinnon, 2018; Banks, Newman, & Saleem, 2015).
Although mindfulness may assist individuals in better coping with traumatic events by increasing awareness and acceptance of one’s experiences in the present moment, which in turn can help to decrease symptom levels, alternatively, exposure to multiple traumas may be particularly overwhelming to an individual and may make it more difficult to remain in the present moment. This may in turn, increase susceptibility to the development of psychopathology and other related outcomes including overall life satisfaction and QOL. Although studies have shown an inverse association between increases in trauma exposure and decreases in mindfulness (e.g., Boughner et al., 2016; Im & Follette, 2016), to date, no study of which we are aware has examined the potential role of mindfulness in mediating the relation between trauma exposure and mental health outcomes in military veterans.
Purpose of the Present Study
In the current study, we examined: 1) the association between trauma exposure, mindfulness, and three mental health outcomes—PTSD symptoms, alcohol use disorder (AUD), and SI—in a nationally representative sample of U.S. military veterans; and 2) how mindfulness mediates the association between exposure to cumulative trauma burden and these outcomes. The relationship between trauma exposure, mindfulness and QOL, defined as degree of satisfaction and enjoyment experienced in different areas of one’s life (Endicott et al., 1993) was also examined (see Figure 1).
Figure 1.
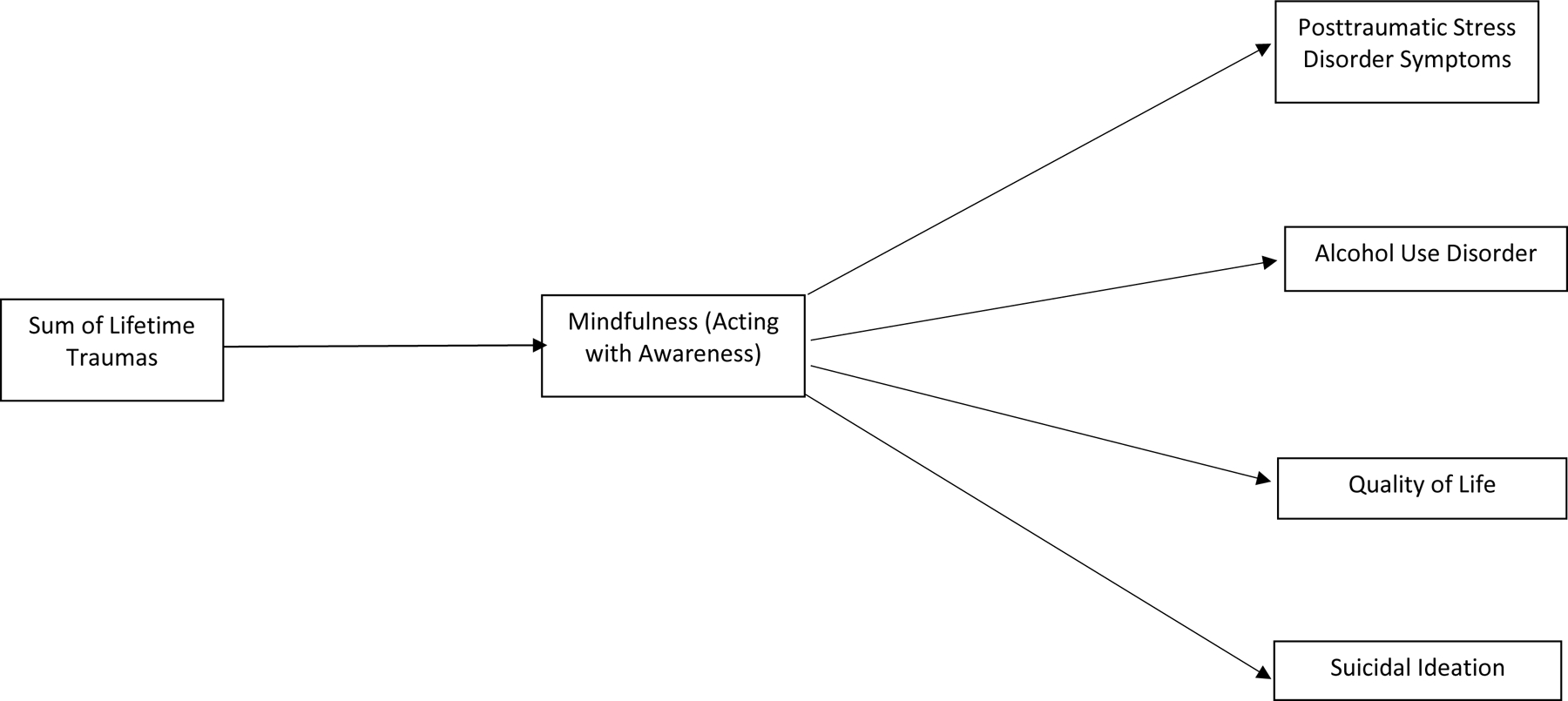
Proposed structural model examining the interrelationships between trauma exposure, mindfulness, PTSD Symptoms, alcohol use disorder, quality of life, and suicidal ideation.
We focused specifically on the aspect of mindfulness that involves the ability to be attentive to and aware of what is occurring in the present moment, as this aspect has been consistently shown to be associated with PTSD in addition to other mental health outcomes in trauma-exposed populations (e.g., An et al., 2018; Boelen & Lenferink, 2017; Chang et al., 2018; Schoorl et al., 2015). We hypothesized that a greater number of traumas would be negatively associated with one’s ability to be attentive to what is occurring in the present moment, and that this would, in turn, be associated with greater severity of PTSD symptoms, higher likelihood of AUD and SI, and decreased QOL.
Method
Participants and Procedure
The sample consisted of 1,268 trauma-exposed U.S. military veterans who participated in the National Health and Resilience in Veterans Study (NHRVS), a nationally representative survey that was conducted in 2013. On average, the sample was 60.6 years of age (SD=15.2, range=20–94), predominantly male (89.8%), Caucasian (75.0%), had some college or higher education (68.1%), and were married/cohabitating (68.9%), employed (76.5%), and non-combat veterans (59.2%).
Veterans completed a 60-minute anonymous web-based survey. The NHRVS sample was drawn from a research panel of more than 50,000 households and maintained by GfK Knowledge Networks, Inc. (now Ipsos), a survey research firm. A total of 1,602 adults responded to an initial screening question that confirmed veterans’ status, and 1,484 completed the survey, resulting in a response rate of 92.6%. To permit generalizability of study results to the entire population of US veterans, post-stratification weights were computed by GfK statisticians and applied on the basis of demographic distributions (i.e., age, gender, race/ethnicity, education, census region, and metropolitan area) from the most contemporaneous Current Population Survey (US Census Bureau, 2013). Missing data (<5%) were imputed using an iterative Markov chain Monte Carlo method. All participants provided informed consent, and the study was approved by the Human Subjects Subcommittee of the VA Connecticut Healthcare System.
Measures
Sociodemographic Characteristics.
Sociodemographic variables assessed included age, sex (male, female), marital status (not married/cohabitating, married/cohabitating), race (Caucasian, non-Caucasian), education (up to high school, some college or higher), employment status (currently employed vs. not), household income (<$60,000, $60,000 or higher), and combat exposure (yes, no).
Trauma History.
History of trauma was assessed using the Trauma History Screen (Carlson et al., 2011), a self-report measure that assesses the occurrence of 14 potentially traumatic life events. Potential traumas across the lifespan including physical or sexual assault during childhood or adulthood, traumatic events during military service, accidents and unexpected loss of loved ones were assessed. The occurrence of life-threatening illness or injury also was additionally assessed in the NHRVS. Endorsement of each traumas was summed to yield a total number of lifetime trauma exposures.
Mindful Attention.
Mindfulness was assessed using an abbreviated version of the Mindful Attention to Awareness Scale (MAAS; Brown & Ryan, 2003). The MAAS consists of 15 items designed to assess a core characteristic of mindfulness, namely open awareness of and attention to what is taking place in the present moment. In the current study, 3 items were taken from the MAAS to assess mindfulness (It seems I am running on automatic without much awareness of what I am doing, I find myself doing things without paying attention, I rush through activities without paying attention). Responses ranged from 1 (almost always) to 6 (almost never). These three items were chosen as they showed the highest item-total correlation in the original validation study of the MAAS (Brown and Ryan, 2003). Responses to each of the three items were summed to create an overall mindfulness score (Cronbach’s α=0.93).
PTSD Symptoms.
Past-month symptoms of PTSD were assessed using the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5; Weathers et al., 2013). The PCL-5 is a 20-item self-report questionnaire that assesses DSM-5 PTSD symptoms. Respondents are asked to report the extent to which they are bothered by PTSD symptoms in response to their ‘worst’ traumatic event assessed by the Trauma History Screen in the past month from 0 (not at all) to 4 (extremely). Scores on each of the items to summed to create an overall PTSD symptom score (Cronbach’s α=0.95).
Alcohol use disorder (AUD).
The presence or absence of an AUD was determined using the Alcohol Use Disorders Identification Test (AUDIT; Saunders et al., 1993). The AUDIT is a ten-item questionnaire that assesses: 1) frequency of alcohol consumption (3 items), 2) dependence (3 items), and 3) alcohol-related problems (4 items). It reliably identifies individuals who are hazardous drinkers or have active alcohol use disorders in a variety of populations. Each of the first eight questions are rated on a four-point scale (0–4) and the last two questions are scored 0, 2, or 4 for a maximum of 40 points. Cutoff scores of ≥8 are indicative of a positive screen for AUD (Cronbach’s α=0.81).
Quality of life (QOL).
QOL was assessed with the Quality of Life Enjoyment and Satisfaction Questionnaire-Short Form (Q-LES-Q-SF; Endicott et al., 1993), a 16-item measure that asks respondents about their satisfaction in the past week with various aspects of their lives (e.g, work, family). Respondents are asked to rate their satisfaction from 1 (very poor) to 5 (very good), and scores are summed for a total score (Cronbach’s α=0.94).
Suicidal ideation (SI).
SI within the past two weeks was assessed using the SI item on the Patient Health Questionnaire-9 (Kroenke & Spitzer, 2002). This item was divided into two separate questions to assess passive and active SI. Specifically, participants were asked how often over the past 2 weeks they had been (1) bothered by thoughts that they were better off dead (passive SI); and (2) thoughts of hurting themselves in some way (active SI). Response options ranged from 0 (not at all) to 3 (nearly every day). These items were combined and recoded (i.e., 0=0 (absence of passive and/or active SI in the past two weeks); 1–3=1 (presence of passive and/or active SI in past two weeks)).
Data Analysis
Structural equation modeling (SEM) was used to test the conceptual model depicted in Figure 1, which examined interrelationships between trauma exposure, mindful awareness, PTSD symptoms, AUD, QOL, and SI. Assuming power=0.80 and conservatively small alpha and beta path coefficients of 0.14, the required sample size for mediation analyses using bias-corrected bootstrap tests is 462 (Fritz & MacKinnon, 2007); thus, the current sample size of 1,268 was determined to be adequate to detect coefficients as low as 0.14. Sociodemographic variables that were found to correlate with our outcomes were included as covariates. All SEM analyses were conducted using Mplus (Version 8; Muthén & Muthén, 1998–2006). Several different fit indices were used to evaluate model fit, including the comparative fit index (CFI), the root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR). Fit indices were evaluated based on the recommendations made by Hu and Bentler (1999); specifically, cutoff values >0.95 for the CFI, <0.06 for the RMSEA, and <0.08 for the SRMR were indicative good fitting models. Models were also compared using the Bayesian Information Criterion (BIC) and Akaike Information Criterion (AIC; Ling et al., 2017), with lower values indicative of a better fitting model (i.e., BIC difference of 6–10 indicates very strong support for the model with lower BIC; Akaike, 1987; Raftery, 1995). Full-information maximum likelihood (FIML) was used to estimate parameters in model testing. An alternative model with mental health outcomes specified as mediating the relation between trauma burden and mindfulness was also evaluated.
Results
The mean number of traumas was 4.1 (SD=2.9, range=1–15) and mean number of years since index trauma was 24.0 (SD=19.1, range=0–92); the most prevalent index traumas were sudden death of close family member or friend (31.3%), life-threatening illness or injury (14.4%) and military-related trauma (8.3%). The mean PCL-5 score was 10.1 (SD=13.1) with 8.9% of veterans scoring 31 or higher, which is indicative of probable PTSD (Bovin et al., 2016). Table 1 shows Pearson correlation coefficients among the primary study variables.
Table 1.
Bivariate Correlations, Means, and Standard Deviations of Study Variables
| Variables | 2 | 3 | 4 | 5 | 6 | M | SD | |
|---|---|---|---|---|---|---|---|---|
| 1. | Trauma Exposures | −.38* | .43* | .16* | .21* | −.33* | 3.52 | 3.07 |
| 2. | MAAS-A scores | −.66* | −.39* | −.22* | .45* | 5.18 | 1.07 | |
| 3. | PCL-5 score | .46* | .22* | −.59* | 10.13 | 13.11 | ||
| 4. | PHQ-9 SI item | .09* | −.42* | .08 | .28 | |||
| 5. | AUDIT positive screen | −.14* | .12 | .33 | ||||
| 6. | Q-LES-Q-SF scores | 53.03 | 10.26 |
Note: MAAS=Mindful Attention to Awareness Scale, abbreviated; PCL-5=Posttraumatic Stress Disorder Checklist for DSM-5; PHQ-9-SI=Patient Health Questionnaire-9 suicidal ideation item; AUDIT=Alcohol Use Disorders Identification Test; Q-LES-Q-SF=Quality of Life Enjoyment and Satisfaction Questionnaire-Short Form;
p < .01
The structural model included variables for trauma exposure, mindfulness, PTSD symptoms, presence of an AUD, QOL, and SI. The baseline model also included paths from relevant demographic variables (age, sex, race, employment status, marital status, combat exposure) to each of the outcomes (PTSD symptoms, presence of an AUD, QOL, and SI). Direct paths were included from the number of lifetime traumas to mindfulness, and from mindfulness to each of the outcomes (PTSD symptoms, AUD, QOL, and SI; see Figure 1).
Results indicated that the hypothesized model provided good fit to the data: RMSEA = 0.077 (90%CI=0.058–0.097), CFI = 0.948, SRMR = 0.041, BIC=21,750.87, AIC=21,498.83). As shown in Figure 2, mindfulness partially mediated the relation between the number of lifetime traumas and PTSD symptoms, AUD, and QOL, and fully mediated the relation between number of lifetime traumas and SI. Age (β= −0.05, p=0.010), being married/partnered (β= −0.05, p=0.012), current employment (β= −0.09, p<0.001), and combat exposure (β=0.08, p<0.001) were additionally associated with PTSD symptoms; age (β= −0.06, p=0.024), female gender (β= −0.13, p<0.001), being married/partnered (β= −0.05); and current employment (β= −0.07, p=0.005) with AUD; being married/partnered with SI (β= −0.13, p<0.001); and being married/partnered (β= 0.08, p=0.001) and current employment (β= 0.10, p<0.001) with higher QOL scores.
Figure 2.
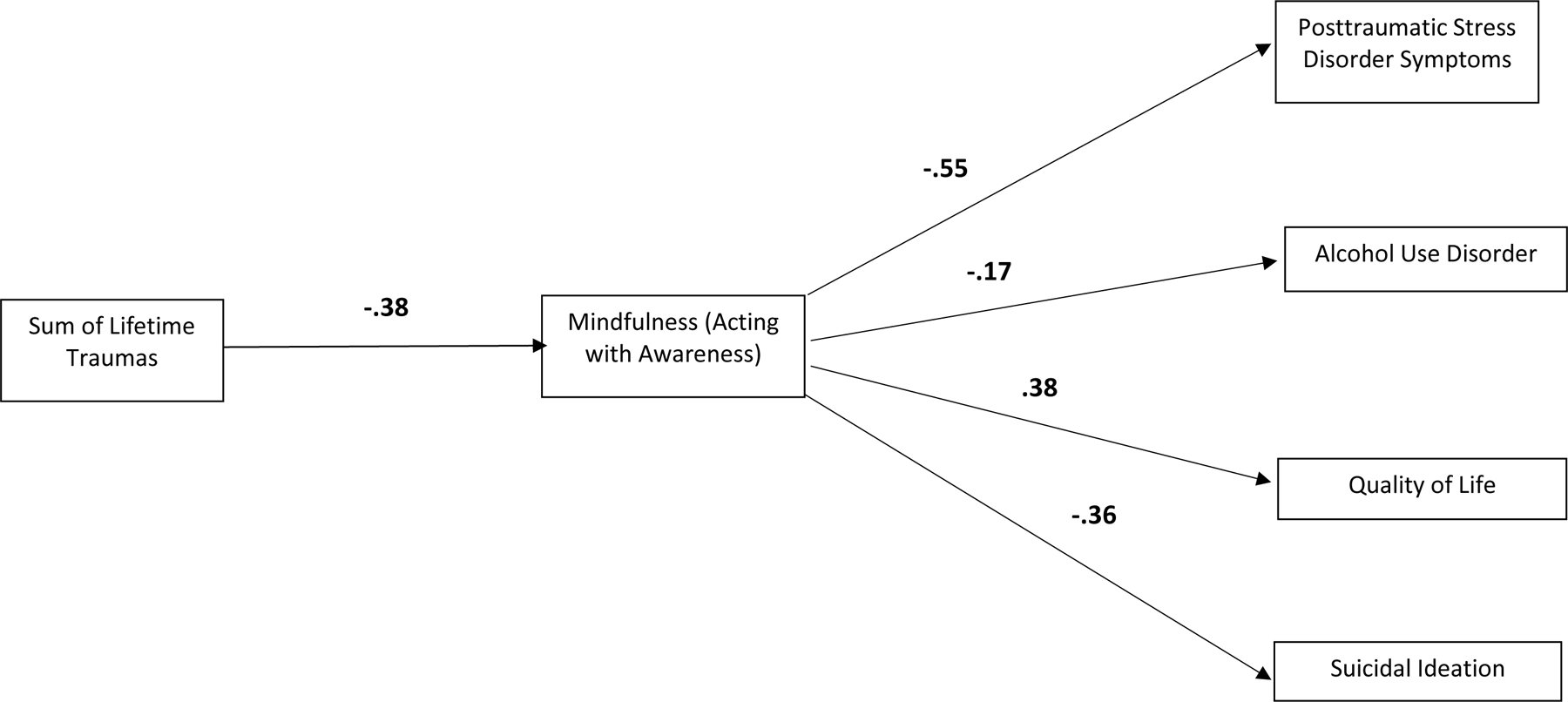
Structural model examining the interrelationships between trauma exposure, mindfulness, PTSD Symptoms, alcohol use disorder, quality of life, and suicidal ideation. Note: Coefficients are beta weights. Model paths are adjusted for sociodemographic variables (age, sex, race, employment status, marital status, combat exposure). All beta weights significant at p < .001.
An alternative model that included mental health outcomes as mediators between trauma exposure and mindfulness was also evaluated. Fit statistics revealed that the hypothesized model fit the data better than this alternate model (ΔBIC=27,952.04; ΔAIC=27,797.73; RMSEA (90%CI)=0.077 (0.058–0.097) vs. 0.217 (0.207–0.227); CFI=0.948 vs. 0.443; SRMR=0.041 vs. 0.145). This finding provides additional support for the hypothesized associations between trauma exposure, mindfulness and mental health outcomes.
Discussion
Exposure to traumatic life events is associated with a number of negative mental health outcomes, including PTSD, AUD, and SI (Galatzer-Levy et al., 2013; Kessler et al., 1995; Stein et al., 2010), as well as decreased QOL (Affifi et al., 2007). In addition, the experience of multiple traumas, which tends to be the norm in the general adult population (e.g., Kilpatrick et al., 2013), may further increase the risk for and severity of mental health problems. The goal of the current study was to consider whether mindfulness, which involves the ability to remain attentive in the present moment, may mediate the relation between number of lifetime traumas, and severity of PTSD symptoms, AUD and SI, and overall QOL in U.S. veterans, a population considered to be at greater risk of experiencing multiple traumatic events. Results revealed that enduring a greater number of traumas was associated with reduced mindfulness or ability to remain attentive to what is occurring in the present moment, which suggests that exposure to multiple traumatic life events may erode one’s ability to be mindful. The experience of multiple traumas may have a cumulative negative effect that may overwhelm an individual’s ability to cope with these events. For example, after experiencing a traumatic event, one may experience increases in affect-laden intrusive thoughts about the events and an increased desire to avoid such thoughts. This is consistent with previous research showing that greater exposure to traumatic events is associated with increases in the frequency of ruminative thinking (Im & Follette, 2016; Michael et al., 2007). Increases in ruminative thinking or intrusive thoughts, in turn, may make it more difficult to be mindful—that is to focus attention on the present moment. Furthermore, from a neurobiological perspective, when one is under mild or moderate levels of stress, catecholamines (e.g., norepinephrine) may help maintain prefrontal cortical executive functioning, including increases in levels of alertness, attention regulation, and impulse control. However, under high level of stress, particularly when it is chronic and uncontrollable (i.e., the experience of multiple traumatic life events), the prefrontal cortex becomes flooded with catecholamines, which weakens prefrontal executive functions, including attentional control (Arnsten, 2009), which may help one remain attentive to the present moment.
Consistent with previous research (Affifi et al., 2007; Galatzer-Levy et al., 2013; Kessler et al., 1995; Stein et al., 2010), mindfulness was inversely associated with PTSD symptoms, and AUD and SI. Furthermore, mindfulness showed the strongest associations with PTSD symptoms, followed by QOL, SI, and AUD. Mindfulness involves bringing one’s full attention to the present moment in addition to taking a stance of nonjudgmental acceptance to the ongoing flow of sensations, thoughts, and/or emotional states (Baer et al. 2006; Vujanovic et al., 2011). These aspects of mindfulness may make it particularly beneficial for those dealing with the negative impact of multiple traumatic events. The ability to manage these thoughts and feelings by focusing one’s attention on them, as opposed to pushing them away (i.e., avoiding them) may in turn decrease symptoms of PTSD, which is characterized by avoidance of thoughts and feelings. Furthermore, focusing one’s attention on the present moment may decrease the likelihood of engaging in maladaptive avoidance coping strategies (e.g., using drugs and alcohol, experiencing SI) as a way to distract from the present moment. Alternatively, the ability to cope in a more constructive way to multiple traumas may also help enhance one’s overall QOL.
Results of the current study also suggest that mindful attention mediated the association between number of lifetime traumas and these mental health outcomes. Specifically, mindfulness was found to be a partial mediator, such that increases in trauma exposure was associated with decreases in mindfulness, and this in turn was associated with increased severity of PTSD symptoms, AUD, and decreased QOL. Mindful attention also was shown to fully mediate the association between number of lifetime traumas and SI, such that increased trauma exposure was associated with decreases in mindfulness, which in turn was associated with increased likelihood of screening positive for SI.
Results of the current study suggest that mindfulness, specifically focusing one’s attention on the present moment, may represent a potential mechanism linking trauma exposure and negative mental health outcomes. They further suggest that mindfulness may fully mediate the link between trauma exposure and SI. The ability to be mindful and tolerate difficult internal experiences, including the experience of painful memories of traumatic events, may be important in helping to prevent the development of or mitigate the severity of PTSD symptoms and alcohol use problems, and may help to improve one’s overall QOL. Furthermore, the ability to be mindful may serve as a potentially helpful strategy for mitigating thoughts about suicide, as such thoughts may be considered the ultimate avoidance strategy, one that runs counter to the tenets of mindfulness that involve acceptance of current experiences in a non-judgmental way.
Implications for Practice
Results of the current study suggest that interventions to help bolster mindfulness may help mitigate the negative mental health impact that cumulative traumas can have on individuals, particularly for U.S. military veterans. Mindfulness-based interventions (e.g., Mindfulness Based Stress Reduction; Kabat-Zinn, 1990; Mindfulness Based Relapse Prevention; Bowen, Chawla, & Marlatt, 2010) have been shown to be effective for a number of mental health problems including PTSD, depression, and substance use problems (see Goldberg et al., 2018 for a review). Some of these interventions have also been shown to be effective in decreasing PTSD and substance use in military veterans (e.g., Polusny, et al. 2015). To the extent that mindfulness interventions could be implemented among individuals who have been exposed to multiple traumas, they may help to mitigating the risk of developing PTSD, as well as other mental health problems and overall QOL.
Limitations and Future Directions
The current findings are limited by the cross-sectional nature of the study; thus, conclusions about the temporal order of associations and causality cannot be made, particularly when testing a cross-sectional mediation model. Also, the current study relied entirely on self-report measures, which may increase the potential for response bias, and limit their validity and reliability. Furthermore, the current study utilized an abbreviated (i.e., three item) measure of mindfulness not used in prior research and an abbreviated measure of SI. Furthermore, while nationally representative, the sample consisted of predominantly older, male, Caucasian, non-combat veterans, thus potentially limiting the generalizability of the current findings to this population. Further research is needed to examine these relationships longitudinally using SEM methods to examine these associations (e.g., O’Laughlin, Martin, & Ferrer 2018). Given the multidimensionality of mindfulness, future research should also examine other facets of mindfulness in addition to present-moment awareness, such as observing (i.e., ability to notice or attend to internal and external experiences), describing (i.e., ability to label internal experiences with words), non-judging of inner experience (i.e., taking a non-evaluative stance toward thoughts and feelings), and non-reactivity to inner experience (i.e., tendency to allow thoughts and feelings to come and go, without getting caught up in or carried away by them) (Baer et al., 2008) as they may show differential associations between trauma exposure and mental health. Finally, further studies are needed to examine additional factors, such as ruminative thinking, that may mediate the association between trauma exposure and mental health outcomes in veterans and other trauma-exposed populations.
Acknowledgments
This work was supported in part by Career Development Award Number IK2 CX-001259–01 from the United States (U.S.) Department of Veterans Affairs Clinical Sciences R&D (CSRD) Service (L. Kachadourian). The National Health and Resilience in Veterans Study is supported by the U.S. Department of Veterans Affairs National Center for Posttraumatic Stress Disorder. The views and opinions expressed in this report are those of the authors and should not be construed to represent the U.S. government.
Footnotes
Clinical Impact Statement
The current study found that a higher number of traumatic life events was associated with a reduced ability to pay attention to the present moment in U.S. military veterans. Reduced ability to pay attention to the present moment, in turn, was associated with higher number of posttraumatic stress disorder (PTSD) symptoms, positive screen for alcohol use disorder, suicidal ideation, and lower quality of life. These results suggest that psychological treatments that bolster mindfulness may help mitigate the negative impact of experiencing a high number of traumatic events on negative mental health outcomes in U.S. veterans.
We have no known conflict to disclose.
References
- Afifi TO, Enns MW, Cox BJ, de Graaf R, Have M, & Sareen J (2007). Child abuse and health-related quality of life in adulthood. Journal of Nervous and Mental Disease, 195, 797–804. [DOI] [PubMed] [Google Scholar]
- Akaike H (1987). Factor analysis and AIC. Psychometrika, 52, 317–332. [Google Scholar]
- American Psychiatric Association American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders 5th ed. Arlington (VA): APA; 2013. [Google Scholar]
- An Y, Yuan G, Liu Z, Zhou Y, & Xu W (2018). Dispositional mindfulness mediates the relationships of parental attachment to posttraumatic stress dieosrder and academic burnout in adolescents following the Yancheng tornado. European Journal of Psychotraumatology, 9, 1, 1472989, [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnsten AFT (2009). Stress signaling pathways that impair prefrontal cortex structure and function. Nature Reviews Neuroscience 10, 6, 410–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer RA, Smith GA, Lykins E, Button D, et al. (2008). Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment, 15, 329–342. [DOI] [PubMed] [Google Scholar]
- Banks K, Newman E, & Saleem J (2015). An overview of the research on mindfulness-based interventions for treating symptoms of posttraumatic stress disorder: A systematic review. Journal of Clinical Psychology, 71(10), 935–963. [DOI] [PubMed] [Google Scholar]
- Belik SL, Cox BJ, Stein MB, Asmundson GJ, & Sareen J (2007). Traumatic events and suicidal behavior: Results from a national mental health survey. Journal of Nervous and Mental Disorders, 195, 4, 342–349. [DOI] [PubMed] [Google Scholar]
- Beristianos MH, Maguen S, Neylan TC, & Byers AL (2016). Trauma exposure and risk of suicidal ideation among ethnically diverse adults. Depression and Anxiety, 33, 495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein A, Tanay G, & Vujanovic AA (2011). Mindful attention and awareness and psychopathology among trauma-exposed adults: Preliminary evidence of transdiagnostic resilience. Journal of Cognitive Psychotherapy: An International Quarterly, 25, 2, 99–113. [Google Scholar]
- Boelen PA, & Lenferink LIM (2017). Experiential acceptance and trait-mindfulness as predictors of analogue post-traumatic stress. Psychology and Psychotherapy: Theory, Research and Practice, 91, 1–14. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Galea S, Bucciarelli A, & Vlahov D (2006). Psychological resilience after disaster: New York City in the aftermath of the September 11th terrorist attack. Psychological Science, 17, 3, 181–186. [DOI] [PubMed] [Google Scholar]
- Boughner E, Thornley E, Kharlas D, & Frewen P (2016). Mindfulness-related traits partially mediate the association between lifetime and childhood trauma exposure and PTSD and dissociative symptoms in a community sample assessed online. Mindfulness, 7, 672–679. [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric Properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in Veterans. Psychological Assessment, 28, 11, 1379–1391. [DOI] [PubMed] [Google Scholar]
- Boyd, Lanius, & McKinnon (2018). Mindfulness-based treatments for posttraumatic stress disorder: A review of the treatment literature and neurobiological evidence. Journal of Psychiatry and Neuroscience, 43(1), 7–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. (1998). Trauma and posttraumatic stress disorder in the community. Archives of General Psychiatry, 55, 626–632. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EW, & Schultz LR (2008). A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: A prospective epidemiological study. Archives of General Psychiatry, 65, 431–437. [DOI] [PubMed] [Google Scholar]
- Brown & Ryan, 2003 Brown KW, & Ryan RM (2003). The benefits of being present: mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84, 4, 822–848. [DOI] [PubMed] [Google Scholar]
- Brown KW, & Ryan RM (2004). Perils and promise in defining and measuring mindfulness: Observations from experience. Clinical Psychology: Science and Practice, 11, 242–248. [Google Scholar]
- Brunet A, Monson E, Liu A, & Fikretoglu D (2015). Trauma exposure and posttraumatic stress disorder in the Canadian Military. Canadian Journal of Psychiatry, 60, 11, 488–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson EB, Smith SR, Palmieri PA et al. (2011). Development and validation of a brief self-report measure of trauma exposure: The Trauma History Screen. Psychological Assessment 23, 2, 463–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang S, Banks K, Bartlett BA, San Miguel G, & Vujanovic AA (2018). Posttraumatic stress and mindfulness facets in relation to suicidal ideation severity among psychiatric inpatients. Mindfulness, 9, 761–772. [Google Scholar]
- Endicott J, Nee J, Harrison W, & Blumenthal R (1993). Quality of life enjoyment and satisfaction questionnaire: A new measure. Psychopharmacology Bulletin 29, 2, 321–326. [PubMed] [Google Scholar]
- Fritz MS, and MacKinnon DP (2007). Required sample size to detect the mediated effect. Psychological Science, 18, 3, 233–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galatzer-Levy IR, Nickerson A, Litz BT, & Marmar CR (2013). Patterns of lifetime PTSD comorbidity: a latent class analysis. Depression and Anxiety, 30, 5, 489–496. [DOI] [PubMed] [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Davidson RJ et al. (2018). Mindfulness based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green BL, Goodman LA, Krupnick JL, Corcoran CB, Petty RM, Stockton P & Stern NM (2000) Outcomes of single versus multiple trauma exposure in a screening sample. Journal of Traumatic Stress, 13, 2, 271–286. [DOI] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. [Google Scholar]
- Im S, & Follette VM (2016). Rumination and Mindfulness Related to Multiple Types of Trauma Exposure. Translational Issues in Psychological Science, 2, 4, 395–407. [Google Scholar]
- Kabat-Zinn J (1990). Full catastrophe living: using the wisdom of your mind and body to face stress, pain, and illness New York: Delta Trade. [Google Scholar]
- Kearney DJ, McDermott K, Malte C, Martinez M, & Simpson TL (2012). Association of participation in a mindfulness program with measures of PTSD, depression and quality of life in a veteran sample. Journal of Clinical Psychology, 68, 1, 101–116. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. (1995). Posttraumatic stress disorder in the National Co-morbidity Survey. Archives of General Psychiatry, 52,1048–1060. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26, 5, 537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraaij V, & de Wilde EJ (2001). Negative life events and depressive symptoms in the elderly: A life-span perspective. Aging & Mental Health, 5, 84–91. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB. (2001). The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael T, Halligan SL, Clark DM, & Ehlers A (2007). Rumination in posttraumatic stress disorder. Depression and Anxiety, 24, 307–317. [DOI] [PubMed] [Google Scholar]
- Nygaard E, & Heir T (2012). World assumptions, posttraumatic stress and quality of life after a natural disaster: A longitudinal study. Health Quality Life Outcomes, 10, 76, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Laughlin KD, Martin MJ, & Ferrer E (2018). Cross-sectional analysis of longitudinal mediation processes. Multivariate Behavioral Research, 53(3), 375–402.) [DOI] [PubMed] [Google Scholar]
- Polusny MA, Erbes CR, Thuras P, Moran A, Lamberty GJ, et al. (2015). Mindfulness based stress reduction for posttraumatic stress disorder among veterans: A randomized clinical trial. JAMA, 314, 5, 456–465. [DOI] [PubMed] [Google Scholar]
- Raftery AE (1995). Bayesian model selection in social research. Sociological Methodology, 25, 111–163. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La Fuente JR, & Grant M (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II Grant. Addiction, 88, 791–804. [DOI] [PubMed] [Google Scholar]
- Schoorl M, Van Mil-Klinkenberg L, & Van Der Does W (2015). Mindfulness skills, anxiety sensitivity, and cognitive reactivity in patients with posttraumatic stress disorder. Mindfulness, 6, 1004–1011. [Google Scholar]
- Segal, Williams, & Teasdale, 2002 Segal ZV, Williams JMG, & Teasdale JD (2002). Mindfulness Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse New York: The Guilford Press. [Google Scholar]
- Stein DJ, Chiu WT, Hwang I, Kessler RC, Sampson N, Alonso J, et al. (2010). Cross-national analysis of the associations between traumatic events and suicidal behavior: Findings from the WHO world mental health surveys. PloS One, 5, 5, e10574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson BL, & Waltz J (2010). Mindfulness and experiential avoidance as predictors of posttraumatic stress disorder avoidance symptom severity. Journal of Anxiety Disorders, 24, 409–415. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau Current Population Survey (2013). https://www.census.gov/programs-surveys/cps.html.
- Weathers FW, Litz BT, Keane TM, et al. (2013). The PTSD Checklist for DSM-5 (PCL-5) Washington, D. C.: U.S. Department of Veterans Affairs, National Center for Posttraumatic Stress Disorder. [Google Scholar]


