Abstract
Objectives
To determine the effect of one-click integration of a state’s prescription drug monitoring program (PDMP) on the number of PDMP searches and opioid prescriptions, stratified by specialty.
Methods
Our large health system worked with the state department of public health to integrate the PDMP with the electronic health record (EHR), which enabled providers to query the data with a single click inside the EHR environment. We evaluated Schedule II or III opioid prescriptions reported to the Massachusetts PDMP 6 months before (November 15, 2017-May 15, 2018) and 6 months after (May 16, 2018, to November 16, 2018) integration. Search counts, prescriptions, patients, morphine milligram equivalents, as well as prescriber specialty were compared.
Results
There were 3,185 unique prescribers with a record of a Schedule II and/or III opioid prescription in both study periods that met inclusion criteria. After integration, the number of PDMP searches increased from 208,684 in the pre-integration phase to 298,478 searches in the post-integration phase (+43.0%). The number of opioid prescriptions dispensed decreased by 4.8%, the number of patients receiving a prescription decreased by 5.1%, and the mean morphine milligram equivalents (MMEs) per prescriber decreased by 5.4%. There were some notable specialty-specific differences in these measures.
Conclusions
Integration of the PDMP into the EHR markedly increased the number of searches but was associated with modest decreases in opioids prescribed and patients receiving a prescription. Single click EHR integration of the PDMP, if implemented broadly, may be a way for states to significantly increase PDMP utilization.
Keywords: Prescription drug monitoring programs, Prescriptions, Opioids
Introduction
Prescription drug monitoring programs (PDMPs) have been identified as a tool in addressing prescription opioid abuse/misuse, which over time may help stem the opioid overdose epidemic, although research on their effectiveness at preventing opioid overdose has provided mixed results [1]. One reason for lack of effectiveness is that providers are simply not using them, even when states implement programs aimed at increasing provider registration in the program [2]. In response, states have begun mandating that prescribers register and/or conduct patient searches when prescribing controlled medications [3]. A study in California, where registration was obligatory, found only modest gains in use by providers who registered after a mandate was put in place [4]. Conversely, in Ohio, where providers must both register for and then query the PDMP prior to writing controlled substance prescriptions, this policy change was associated with decreases in opioid and benzodiazepine prescriptions [5].
Even with state mandates, PDMP use may be suboptimal. PDMP data are typically accessed via web portal after inputting login credentials that may vary from hospital electronic health record (EHR) login credentials. The provider then is required to enter the name and date of birth for each patient being queried and select additional states to query if applicable. This is an onerous and time-consuming task that may contribute to low utilization of PDMPs [6]. For example, one study discovered that accessing the PDMP record of a single patient took a mean of 4.22 minutes and necessitated a mean of 50.3 mouse clicks to obtain [7]. To address this concern, Massachusetts began the process of integrating PDMP information into EHRs. Massachusetts is a state that mandates PDMP queries prior to every Schedule II or III opioid prescription written. Our primary aim was to determine if PDMP integration into the EHR was associated with an increased number of PDMP searches. Secondary aims included whether there were any specialty-specific variations (e.g., between primary care, neurologists, emergency physicians, etc.) and to evaluate the overall changes in the number of Schedule II and III opioid prescriptions, number of unique patients, and morphine milligram equivalents (MMEs) in the pre- and post-integration periods.
Methods
The study design was a retrospective pre- and post-implementation analysis involving the Massachusetts online PDMP (“MassPAT”) and a large health system’s EHR. Starting in 2016, Massachusetts required a PDMP query prior to writing a prescription for Schedule II or III opioids [8]. The health system, called Mass General Brigham (formerly Partners Healthcare), is the largest in the state, providing care for over 1.5 million patients annually. The system is composed of two large academic centers, multiple community hospitals, and numerous affiliated outpatient clinics. The health system uses the Epic EHR (Verona, WI). Working in collaboration with the state, the one-click integration was implemented on May 16, 2018. With this integration, clinicians were able to access the PDMP from the patient’s EHR within 5–8 seconds. Education was provided at the site level through in-services starting immediately after the implementation and was followed up with an email to all prescribers in the system (Appendix 1). During the time of this study, providers accessed the tool through a multilevel menu, but once they selected it as a “favorite” it always appeared on their main toolbar, also explained in the Appendix. Providers could also designate delegates who could access the PDMP record of their patients, but the integrated system did not allow for delegate use; therefore, delegates were required to use the web portal in both study periods.
The pre-integration phase was the 6 months from November 15, 2017, to May 15, 2018, and the post-integration phase was the 6 months from May 16, 2018, to November 16, 2018. Providers were included in the study if they had written at least one Schedule II or III opioid prescription reported to MassPAT (i.e., the prescription was dispensed) in both the pre- and post-integration periods. The medications included are shown in Appendix 2. A list of National Provider Identifier (NPI) numbers for these prescribers was generated and provided to the state. This list of NPI numbers was linked to the PDMP database to obtain additional pertinent information (e.g., prescriber DEA number, search audit history, Schedule II and III opioid prescriptions reported for that prescriber). The Mass General Brigham Human Research Committee approved the study protocol.
Matching was completed based on prescriber DEA or NPI number. The counts of patient searches, Schedule II and III opioid prescriptions, number of unique patients, and total MME were summed for all the individual provider rows. We removed providers who appeared to be medical residents based on whether their DEA was a hospital/facility DEA number rather than an individual DEA number. The rationale for excluding medical residents for this analysis is as follows. Prescriptions by residents are problematic in PDMP data as the same DEA number may be used for multiple individuals, specialty information is often incomplete or missing, and many residents work both inside and outside of our hospital system. Therefore, if a resident only works half of their residency in the studied health system, it would skew the results toward the null hypothesis as the individual did not have access to the integration while working at external sites. To perform this data cleaning, we eliminated PDMP records associated with NPI numbers that a) had a hospital name instead of an individual name associated with it, b) had multiple DEA numbers assigned to the same NPI, and c) did not have the same specialty listed in the pre- and post-implementation periods.
Data were compiled and aggregated into specialty groups based on the prescriber’s self-reported specialty selected at the time a MassPAT account was created. Certain specialties were collapsed into smaller categories: 1) anesthesiology, pain, and physical medicine and rehabilitation; 2) nurse practitioners and midwives; 3) dentists and oromaxillofacial surgeons; 4) family medicine and general practice; 5) allergy/immunology, hospitalists, and internal medicine; and 6) colorectal surgery, neurosurgery, otolaryngology, plastic surgery, thoracic surgery, transplant surgery and urology. Psychiatry and neurology were already considered one specialty category in the PDMP data. Specialties that prescribe infrequently (dermatology, ophthalmology, podiatry, radiology) were defined as “other.” When certified nurse specialists (e.g., nurse practitioner or midwife) or physician assistants indicated a specialty when enrolling for the PDMP, they are included in that specialty. Otherwise, they are included in the category of certified nurse specialist or physician assistant. A specialty assignment of “missing” applied to prescribers who had never registered for the system. Data were analyzed in descriptive fashion using JMP v14.2 (SAS Institute, Inc, Cary, NC).
Results
Based on data from health system prescription records, there were 9,527 NPI numbers associated with at least one Schedule II and/or III opioid prescription over the course of the study. Using this list, the state PDMP identified 4,850 NPI numbers associated with at least one opioid prescription in both the pre- and post-implementation periods. Of these, 3,185 prescribers met inclusion criteria. Overall, there were 208,684 queries before and 298,478 queries (+43.0%) after integration. Table 1 demonstrates the sources of queries. Although there were 62,792 queries from the integration, the number of searches by delegates and from the web portal also increased after integration.
Table 1.
Modalities of Prescription Drug Monitoring Program queries before and after electronic health record integration
| Before Integration | After Integration | % change | |
|---|---|---|---|
| Web portal queries | 72,093 | 91,785 | 27.3 |
| Delegate queries | 136,591 | 143,901 | 5.4 |
| Integration queries | N/A | 62,792 | N/A |
| Total queries | 208,684 | 298,478 | 43.0 |
N/A = not applicable.
Of the 3,185 prescribers, 2,098 (65.8%) had an MD/DO degree, 558 (17.5%) were certified nurse specialists, 481 (15.1%) were physician assistants, 24 (0.8%) were dentists and 24 (0.8%) were podiatrists. Table 2 shows differences in searches and prescriptions by specialty/degree type. The specialties that had the largest increases in queries after integration were psychiatry & neurology (154.9%), pediatrics (140.2%), and emergency medicine (107.4%). Only dentists/oromaxillofacial surgeons had decreased numbers of queries (−29.9%). Overall, there were modest decreases in the number of prescriptions (−4.8%), patients receiving an opioid prescription (−5.1%) and total MMEs dispensed (−5.4%).
Table 2.
Comparison of Prescription Drug Monitoring Program searches before and after electronic health record integration, by specialty or professional degree
| Specialty/Professional Degree | Providers | Period | Totals Searches | Δ % Searches | Prescription Count | Δ % Rx | Patient Count | Δ % Patients | Mean MME/ prescriber | Δ % MME |
|---|---|---|---|---|---|---|---|---|---|---|
| Total | 3,185 | Pre-integration | 208,684 | 115,676 | 62,009 | 36,221 | ||||
| Post-integration | 298,478 | 43.0 | 110,066 | −4.8% | 58,853 | −5.1% | 34,255 | −5.4 | ||
| Anesthesia, pain, PM&R | 74 | Pre-integration | 7,845 | 5,862 | 1,875 | 139,445 | ||||
| Post-integration | 11,792 | 50.3 | 5,547 | −5.4% | 1,698 | −9.4% | 124,947 | −10.4 | ||
| Clinical nurse specialist | 308 | Pre-integration | 18,401 | 11,538 | 5,840 | 46,387 | ||||
| Post-integration | 31,372 | 70.5 | 11,252 | −2.5% | 5,802 | −0.7% | 44,335 | −4.4 | ||
| Dental and oromaxillofacial | 20 | Pre-integration | 4,885 | 1,456 | 1,234 | 16,836 | ||||
| post-integration | 3,423 | −29.9 | 1,537 | 5.6% | 1,306 | 5.8% | 17,040 | 1.2 | ||
| Emergency medicine | 228 | Pre-integration | 6,455 | 4,376 | 4,338 | 1,840 | ||||
| Post-integration | 13,390 | 107.4 | 4,203 | −4.0% | 4,163 | −4.0% | 1,668 | −9.3 | ||
| Family medicine | 135 | Pre-integration | 30,278 | 9,756 | 3,600 | 83,186 | ||||
| Post-integration | 39,471 | 30.4 | 9,194 | −5.8% | 3,360 | −6.7% | 80,658 | −3.0 | ||
| General surgery | 131 | Pre-integration | 2,679 | 3,037 | 2,790 | 3,925 | ||||
| Post-integration | 3,685 | 37.6 | 2,837 | −6.6% | 2,609 | −6.5% | 3,766 | −4.0 | ||
| Internal medicine | 1,124 | Pre-integration | 97,051 | 47,808 | 17,738 | 56,231 | ||||
| Post-integration | 134,653 | 38.7 | 46,855 | −2.0% | 17,668 | −0.4% | 54,121 | −3.8 | ||
| Missing/other | 265 | Pre-integration | 1,639 | 2,805 | 2,277 | 3,831 | ||||
| Post-integration | 1,784 | 8.8 | 2,649 | −5.6% | 2,115 | −7.1% | 3,719 | −2.9 | ||
| Obstetrics and gynecology | 228 | Pre-integration | 1,907 | 2,692 | 2,538 | 2,026 | ||||
| Post-integration | 2,583 | 35.4 | 2,537 | −5.8% | 2,391 | −5.8% | 1,783 | −12.0 | ||
| Orthopedic surgery | 180 | Pre-integration | 24,017 | 12,249 | 9,739 | 23,350 | ||||
| Post-integration | 30,853 | 28.5 | 10,407 | -15.0% | 8,142 | -16.4% | 18,986 | -18.7 | ||
| Pediatrics | 38 | Pre-integration | 241 | 320 | 197 | 9,961 | ||||
| Post-integration | 579 | 140.2 | 342 | 6.9% | 172 | −12.7% | 11,878 | 19.2 | ||
| Physician assistant | 121 | Pre-integration | 5,393 | 3,418 | 2,752 | 14,339 | ||||
| Post-integration | 10,982 | 103.6 | 3,133 | −8.3% | 2,503 | −9.0% | 13,245 | −7.6 | ||
| Psychiatry and neurology | 106 | Pre-integration | 3,296 | 3,196 | 771 | 53,524 | ||||
| Post-integration | 8,402 | 154.9 | 2,583 | −19.2% | 681 | −11.7% | 46,573 | −13.0 | ||
| Specialty surgery | 227 | Pre-integration | 4,597 | 7,163 | 6,320 | 7,080 | ||||
| Post-integration | 5,509 | 19.8 | 6,990 | −2.4% | 6,243 | −1.2% | 6,649 | −6.1 |
MME = morphine milligram equivalents. Δ % = percent change.
The data presented did not meet the Shapiro-Wilk test criteria for normality and therefore are presented as medians and interquartile range (IQR) and compared with the Wilcoxon rank sum test. The median number of queries per prescriber was 8 (IQR 0–43) before and 18 (IQR 1–80) after, P < .001. The median number of prescriptions written per prescriber did not change: 14 (IQR 5–38.5) before vs 13 (IQR 5–38) after, P = .211. Likewise, the median number of patients receiving a Schedule II or III prescription was similar: median 10 (IQR 4–24) before vs 9 (IQR 3–23) after, P = .227. The median number of total morphine milligram equivalents (MMEs) prescribed was also not different: 3,900 (IQR 846.3–21,207.5) before vs 3,774 (IQR 801.8–20,140) after, P = .294. Finally, the number of MMEs prescribed per patient was also similar: median 350.0 (128.2–1,726.8) before vs 352.5 (121.0–1,664.4) after, P = .409.
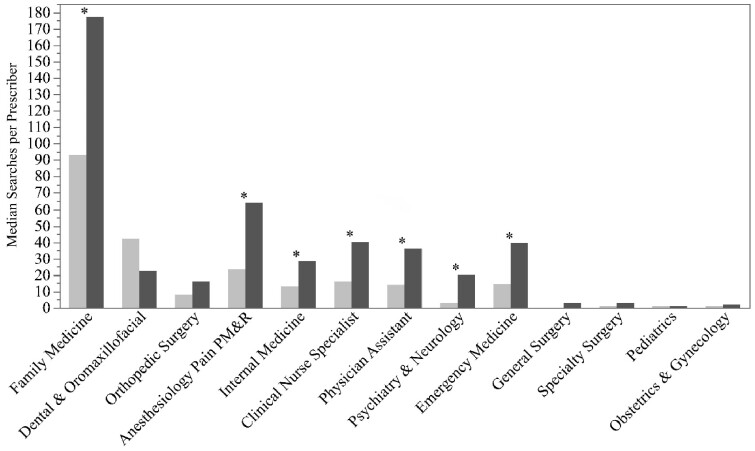
Figure 1 demonstrates the median number of queries per prescriber for the specified specialties and degrees. There were significant increases in family medicine, anesthesiology/pain/physical medicine and rehabilitation, internal medicine, psychiatry and neurology, emergency medicine, and among clinical nurse specialists and physician assistants not in a defined specialty category. Although there appears to be a decrease in the median number of queries by dentists/oromaxillofacial surgeons, the difference did not reach statistical significance.
Figure 1.
Median number of queries per prescriber for the specified specialties/professional degree groups before and after integration. * Indicates significance at P < .05.
Discussion
Our analysis showed that the introduction of a single-click PDMP integration platform to the largest health system in the state resulted in a 43% increase in the number of searches in a state that has a mandate to check the PDMP prior to prescribing every Schedule II–III opioid medication. Interestingly, although the number of queries via the integration increased, so too did queries by prescribers and delegates via the web portal. We also observed a modest decrease in opioid prescribing during this time. This, however, may be attributed to a pre-existing downward trend in opioid prescribing [9]. Based on our methodology, it is not possible to determine whether this decrease was a direct result of the PDMP integration. Still, the findings suggest that searches increased substantially but changes in opioid prescribing were small (about −5.0%) and may or may not be due to the adoption of integration.
Some possible explanations for modest changes in opioid prescribing include: 1) since potentially inappropriate prescribing (e.g., multiple provider episodes or doctor shopping as it is commonly referred to) has notably decreased in our state, the PDMP did not provide additional information to change prescriber behavior [10]; 2) EHR data interoperability is also improving, so it is possible to determine prescription history without consulting the PDMP; 3) PDMP integration only changed prescribing for the small subset of patients that had evidence of concerning behavior on their PDMP profile. This change would not be detectable with the aggregate data that we were permitted to receive from the state.
Another observation from this analysis is that the mean number of dispensed MMEs per prescriber decreased by 5.4%. There were decreases in every specialty except for dental/oromaxillofacial surgery and pediatrics. It is possible that the PDMP data influenced prescribing behavior but may also be due to more judicious prescribing of opioids for pain overall. The specialties that commonly prescribe opioids for chronic pain (anesthesiology, pain and physical medicine and rehabilitation) decreased the number of patients receiving opioid prescriptions by 9.4% and the number of dispensed MMEs by 10.4%, possibly indicative of the recent trend to deprescribe or taper opioids. Conversely, the marked increase in prescribing by pediatricians (6.9% increase in patients and 19.2% increase in MME dispensed) is concerning and warrants further study, although the total number of patients was small.
When evaluating the median searches per prescriber, there were notable increases seen across several specialties, including family medicine, anesthesiology/pain/physical medicine and rehabilitation, internal medicine, psychiatry/neurology and emergency medicine. This is reassuring given that these specialties frequently prescribe more opioids compared to other specialties [11]. Conversely, we did not see significant changes on the provider level for any of the surgical specialties. This finding may be due to the exclusion of residents from the analysis, who most commonly discharge patients in our larger academic hospitals.
There are limitations to this study. Massachusetts mandated PDMP queries during the entire study period, so the effect on opioid prescribing may differ in states without this policy. Although providers must have written at least one prescription in our system during the study period, some providers also work outside of the health system and may not have access to the integrated PDMP elsewhere. For this reason, and due to unreliable specialty data, we excluded resident physicians. By doing this we were able to evaluate differences in prescriptions at the individual provider level, but we also eliminated many providers who write opioid prescriptions, particularly at the academic medical centers. Due to limitations in data availability, we were only able to analyze total aggregate numbers in the pre- and post-intervention phase, so it was not possible to evaluate trends over time. We also were unable to include a comparison group to determine if there was a secular trend. Finally, because we did not have access to prescription-level data, it is uncertain based on these results whether overall prescribing was optimized, versus simply reduced, due to integration.
It is noteworthy that after the conclusion of this study, our system has made PDMP queries even easier. Now, providers do not need to select the PDMP tool as a “favorite” for it to appear as a default item on their EHR toolbar. Also, if a prescription for an opioid or benzodiazepine is ordered and the PDMP had not been queried, the provider is prompted with a box to either acknowledge they have checked or a button for the single-click integration. Finally, we have incorporated a check of the PDMP in a reporting tool monitoring compliance with best practices for patients on chronic opioid therapy. Integration of the PDMP in to the EHR allows such advances.
Conclusion
This research suggests that health systems which implement PDMP integration should expect a substantial increase in the number of queries. Further research is needed to determine if: 1) concurrent decreases in opioid prescribing after the integration are due to a secular trend or a function of the integration because of increased PDMP utilization and review; and 2) to determine if PDMP integration results in detection of patients with concerning prescription fill patterns.
Conflict of interest: Dr. Weiner is supported by NIH awards R01DA044167, R56AG059620, and R01HS026753. There was no additional funding for this project. None of the authors have any financial disclosures.
Opioid Prescribing After Implementation of Single Click Access to a State Prescription Drug Monitoring Program Database in a Health System’s Electronic Health Record
References
- 1. Wilson MN, Hayden JA, Rhodes E, Robinson A, Asbridge M.. Effectiveness of prescription monitoring programs in reducing opioid prescribing, dispensing, and use outcomes: A systematic review. J Pain 2019;20(12):1383–93. [DOI] [PubMed] [Google Scholar]
- 2. Deyo RA, Irvine JM, Hallvik SE, et al. Leading a horse to water: Facilitating registration and use of a prescription drug monitoring program. Clin J Pain 2015;31(9):1–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Haffajee RL, Jena AB, Weiner SG.. Mandatory use of prescription drug monitoring programs. JAMA 2015;313(9):891–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shev AB, Wintemute GJ, Cerdá M, Crawford A, Stewart SL, Henry SG.. Prescription drug monitoring program: Registration and use by prescribers and pharmacists before and after legal mandatory registration, California, 2010–2017. Am J Public Health 2018;108(12):1669–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Winstanley EL, Zhang Y, Mashni R, et al. Mandatory review of a prescription drug monitoring program and impact on opioid and benzodiazepine dispensing. Drug Alcohol Depend 2018. Jul 1;188:169–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bachhuber MA, Saloner B, LaRochelle M, et al. Physician time burden associated with querying prescription drug monitoring programs. Pain Med 2018;19(10):1952–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Poon SJ, Greenwood-Ericksen MB, Gish RE, et al. Usability of the Massachusetts prescription drug monitoring program in the emergency department: A mixed-methods study. Acad Emerg Med 2016;23(4):406–14. [DOI] [PubMed] [Google Scholar]
- 8.Commonwealth of Massachusetts. Chapter 52 of the Acts of 2016: An Act Relative to Substance Use, Treatment, Education and Prevention. Available at: https://malegislature.gov/Laws/SessionLaws/Acts/2016/Chapter52 (accessed January 2021).
- 9.IQVIA Institute. Medicine use and spending in the U.S. - A review of 2018 and outlook to 2023. IQVIA Institute for Human Data Science; 2019.
- 10.Massachusetts Department of Public Health. MA Prescription Monitoring Program County-Level Data Measures (2019 Quarter 1). Available at: https://www.mass.gov/files/documents/2019/05/15/Prescription-Monitoring-Program-PMP-Data-County-Overview-May-2019.pdf (accessed January 2021).
- 11. Weiner SG, Baker O, Rodgers AF, et al. Opioid prescriptions by specialty in Ohio, 2010–2014. Pain Med 2018;19(5):978–89. [DOI] [PubMed] [Google Scholar]