Highlights
-
•
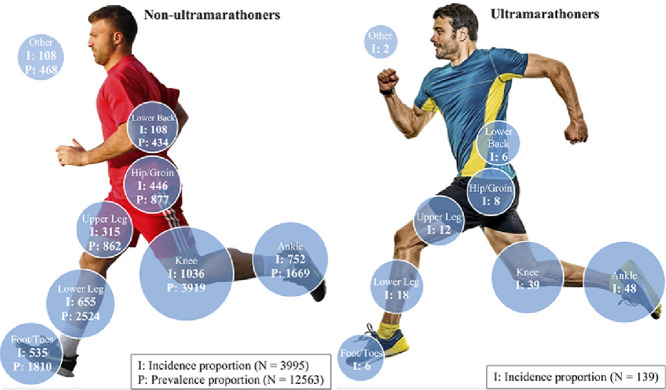
For both ultramarathoners and non-ultramarathoners, the knee and ankle regions had the highest incidence proportion of injuries.
-
•
There was no significant difference in injury incidence proportions by anatomic location between ultramarathoners and non-ultramarathoners.
-
•
For non-ultramarathoners, ankle sprains were in the top 5 injury incidence proportions but were not in the top 5 injury prevalence proportions.
-
•
Achilles tendinopathy and medial tibial stress syndrome had the highest incidence proportions in non-ultramarathoners.
-
•
Anterior compartment syndrome, patellofemoral pain syndrome and Achilles tendinopathy had the highest incidence proportions in ultramarathoners.
Keywords: Epidemiology, Injury, Injury prevention, Rehabilitation, Running
Abstract
Objective
Running-related musculoskeletal injuries (RRMIs), especially stemming from overuse, frequently occur in runners. This study aimed to systematically review the literature and determine the incidence and prevalence proportion of RRMIs by anatomic location and specific pathology.
Methods
An electronic database search with no date beginning restrictions was performed in SPORTDiscus, PubMed, and MEDLINE up to June 2020. Prospective studies were used to find the anatomic location and the incidence proportion of each RRMI, whereas retrospective or cross-sectional studies were used to find the prevalence proportion of each RRMI. A separate analysis for ultramarathon runners was performed.
Results
The overall injury incidence and prevalence were 40.2% ± 18.8% and 44.6% ± 18.4% (mean ± SD), respectively. The knee, ankle, and lower leg accounted for the highest proportion of injury incidence, whereas the knee, lower leg, and foot/toes had the highest proportion of injury prevalence. Achilles tendinopathy (10.3%), medial tibial stress syndrome (9.4%), patellofemoral pain syndrome (6.3%), plantar fasciitis (6.1%), and ankle sprains (5.8%) accounted for the highest proportion of injury incidence, whereas patellofemoral pain syndrome (16.7%), medial tibial stress syndrome (9.1%), plantar fasciitis (7.9%), iliotibial band syndrome (7.9%), and Achilles tendinopathy (6.6%) had the highest proportion of injury prevalence. The ankle (34.5%), knee (28.1%), and lower leg (12.9%) were the 3 most frequently injured sites among ultramarathoners.
Conclusion
The injury incidence proportions by anatomic location between ultramarathoners and non-ultramarathoners were not significantly different (p = 0.798). The pathologies with the highest incidence proportion of injuries were anterior compartment tendinopathy (19.4%), patellofemoral pain syndrome (15.8%), and Achilles tendinopathy (13.7%). The interpretation of epidemiological data in RRMIs is limited due to several methodological issues encountered.
Graphical abstract
1. Introduction
Running is one of the most popular and accessible sport activities enjoyed by people worldwide,1 and it has become increasingly popular in the past 50 years.2 The number of runners and running events has grown substantially over the past decades because it is of low cost and can be easily implemented with minimal equipment by a variety of people.3 More important, running is an excellent form of exercise for people seeking to achieve physical fitness and/or a healthier lifestyle because it has been linked with longevity and reduction of risk factors for cardiovascular disease.4,5
Despite these health benefits, running-related musculoskeletal injuries (RRMIs) are common among runners.6 These RRMIs are usually caused by the application of relatively small loads over many repetitive cycles.7 Various studies have examined the proportion of injuries (incidence and prevalence rates) among runners, with incidence rates ranging between 3.2% and 84.9%.8, 9, 10 This large variation may be explained by the differences in study designs, injury definitions, subjects’ characteristics, and follow-up periods, all of which can differ among studies. Both incidence and prevalence are fundamentally different but both are important in epidemiological studies. Incidence is the indication of the number occurrences of new sporting injuries. It conveys information about the risk of getting injured and is usually only available in prospective studies. Prevalence indicates how widespread the injury is in the sample population and is usually reported in retrospective studies.11 Therefore, developing effective injury prevention programs may reduce the injury incidence and, as a result, the injury prevalence.
Running is one of the most widespread activities that gives rise to overuse injuries of the lower back and lower extremities.12,13 Typically, 50% of runners experience an injury each year that prevents them from running for a period of time, and 25% of runners are injured at any given time.5 About 70%–80% of running disorders are due to overuse injuries, mainly involving the knee, ankle/foot, and shank anatomic sites.14,15 Francis et al.16 reported that patellofemoral pain syndrome is the most frequent overuse injury, whereas Lopes et al.6 stated that medial tibial stress syndrome is the most common RRMI. These 2 systematic reviews6,16 employed different methodological approaches, and this may be one of the reasons that they did not reach the same conclusion.
Some studies have reported that acute injuries are rare during running, while other studies have reported that they are very common and mainly consist of ankle sprains and muscle injuries (e.g., quadricep and hamstring strains).13,15,17 There is still no consensus whether an ankle sprain can be considered as a common injury among runners. Francis et al.16 found that ankle sprains were not in the top 10 most common RRMIs; however, Lopes et al.6 reported that ankle sprains were in the top 5 most common RRMIs. This might be because Lopes et al.6 focused on prospective studies (incidence) to find the most common RRMIs, whereas Francis et al.16 combined the number of injuries across all study designs (prevalence) to identify the most common RRMIs. This highlights again the importance of differentiating incidence (prospective studies) and prevalence (retrospective studies).
Regardless of the type of injury, RRMIs diminish pleasure in exercise and are associated with undesirable consequences, including substantial financial implications, temporary or permanent discontinuation of running, and absence from work.13 A thorough understanding of the most frequent RRMIs is an essential step in elaborating effective injury prevention programs and rehabilitation intervention strategies that can reduce the high incidence and prevalence of RRMIs, respectively.18 Systematic reviews have been conducted to identify the most common RRMIs among runners; however, the authors of these reviews used strict inclusion and exclusion criteria in an attempt to minimize the large heterogeneity in the studies reviewed.6,10,19 This resulted in a minimal amount of studies being included in the review. A recent systematic review by Francis et al.16 used broader inclusion criteria allowed the inclusion of larger populations (e.g., trail and cross-country runners) and a broader classification of injury (e.g., ankle-foot, knee, and hip). However, Francis et al.16 reported the prevalence by combining the number of injuries per anatomic region or specific pathology across all study designs. Lopes et al.6 used an alternative approach in which incidence was measured by extracting injury incidence data from prospective studies, new injury analysis, and prevalence data from retrospective and cross-sectional studies where runners reported their past injuries.
Our review utilized the same approach as Lopes et al.,6 but with broader inclusion criteria. This approach allowed for the inclusion of larger populations (e.g., trail and cross-country runners), studies that described the anatomic location of the injury, and non-intervention and intervention groups where the volume of running was not altered and did not yield a significant difference in RRMIs between the 2 groups. Our alternative approach can provide a more comprehensive understanding of the incidence and prevalence estimates for each RRMI in this larger population. It can also provide health care professionals, researchers and coaches with a foundation for the investigation of risk factors associated with running injuries, including the anatomic location or specific pathology that injury prevention measures should focus on in order to reduce the high incidence rates of RRMIs in runners, thus reducing the risk of injury.
Therefore, the primary aim of this review was to systematically review the literature on the incidence and prevalence of RRMIs per anatomic location and, where possible, per specific pathology. A secondary aim was to compare the injury incidence proportions by anatomic location between ultramarathoners and non-ultramarathoners.
2. Methods
2.1. Search strategy
This review was conducted according to the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines.20 The aim of the search strategy was to identify studies that accurately reported the proportion (incidence or prevalence) of RRMIs per anatomic location (e.g., foot, ankle, lower leg) and/or specific pathology (e.g., patellofemoral pain syndrome) of each RRMI. An electronic systematic literature search was conducted on the PubMed (January 1962 to June 2020), SPORTDiscus (January 1975 to June 2020), and MEDLINE (January 1966 to June 2020) databases without restriction on date of publication or language. Studies that were published in languages other than English were translated into English using Google Translate. The search was completed using the following keyword strings: (“Epidemiology” OR “Epidemiologic” OR “Epidemiological” OR “Survey” OR “Incidence” OR “Prevalence”) AND (“Run” OR “Runners” OR “Running” OR “Jogging” OR “Cross Country” OR “Trail runner” OR “Ultramarathon” OR “Marathon”) AND (“Injury” OR “Injuries” OR “Injured” OR “Wound”). Additionally, one of the authors of this study (NK) checked the reference lists of the included articles and the published systematic reviews within the running injury thematic literature for other potentially relevant articles that had not been identified in the electronic search strategy. All citations were imported into a reference manager software program (Mendeley Desktop Application, London, UK), and duplicates were removed by NK. The screening of eligible studies was performed in 3 steps. In Step 1, all study titles were screened by NK; In Step 2, all abstracts were evaluated independently by NK and NY (another author of this study), who selected relevant articles for inclusion; In Step 3, NK and NY read the full text of all articles identified in Step 2 and evaluated them for eligibility. In cases of disagreement between the 2 reviewers, a consensus decision-making process was followed. If no consensus could be reached, the third author of this review (DTPF) was consulted.
2.2. Inclusion and exclusion criteria
The inclusion criteria included: (1) randomized control trials and prospective cohort studies for incidence estimates and cross-sectional and retrospective studies for prevalence estimates; (2) studies that had non-intervention and intervention groups that included only runners, did not alter the running volume and did not report a significant difference in RRMI between the 2 groups; (3) studies whose subjects (regardless of age) were trail or cross-country runners, middle- or long-distance runners, or half-, full, or ultramarathon runners; (4) studies whose subjects had levels of running skills that ranged from novice to elite; (5) studies that reported quantitative data from which it was possible to extract the proportion of each RRMI; (6) studies that reported the RRMI anatomic location as the lower back or lower limbs (and that identified these injuries as not being due to other illnesses or medical conditions); (7) studies that separated RRMIs from similar injuries that occurred due to participation in sports other than running; and (8) studies that investigated shod and barefoot running injuries, but reported shod injuries separately from barefoot injuries.
The exclusion criteria included: (1) studies in which running was not the main sport or studies on sports in which non-running activities were also required (e.g., biathlon, triathlon); (2) studies that included service personnel (e.g., military recruits, police, firefighters); (3) studies in which the subjects were orienteers, hurdlers, or sprinters; (4) studies that combined the anatomic locations of lower limb RRMIs (e.g., foot/ankle); (5) studies that only described the type of injury (e.g., sprain) without reporting a clear pathology of the injury (e.g., ankle sprain); (6) studies that recruited participants with a specific pathology (e.g., Achilles tendinopathy); and (7) multiple publications for studies involving the same cohort.
2.3. Quality assessment
Recent systematic reviews that evaluated the incidence and prevalence of running injuries have adopted different tools to assess the risk of bias (ROB) of the studies.6,10,18 Researchers have frequently modified these tools to make the ROB more related to studies on running and to the specific aims of the studies. The studies included in our review were prospective, retrospective and cross-sectional. The main purpose of our review was to measure the incidence and prevalence proportion of injuries at different anatomic locations and for specific pathologies. The mechanisms causing the RRMIs were not of interest, thus minimizing the importance of methods for randomization in assessing the quality of the outcomes. Therefore, it was possible to use a single tool proposed by Lopes et al.6 to evaluate the ROB of studies with diversified research designs like those included in our review. The tool contains 10 yes/no criteria, where the total ROB score for each study is calculated by counting the number of items that were scored positive by the 2 independent reviewers (NK and NY). A score of ≥5 was deemed as low ROB. The ROB scores of both reviewers were compared and disagreements were resolved by consensus. Briefly, the criteria for assessing the ROB were as follows: (1) definition of RRMI (yes/no), (2) prospective designs that present incidence data, or retrospective and cross-sectional designs that present prevalence data (yes/no), (3) description of the population or type of runners (yes/no), (4) random sampling used (yes/no), (5) data analysis was performed on at least 80% of the population (yes/no), (6) self-reported injuries by runner or healthcare professional (yes/no), (7) same mode of data collection (yes/no), (8) diagnosis by a medical doctor (yes/no), (9) prospective studies follow-up period of at least 6 months or up to 12 months for the recall period for retrospective studies (yes/no), and (10) incidence and prevalence rates of each RRMI expressed by the number of injuries and by the exposure to running (yes/no). The detailed criteria for the ROB assessment are presented in the Electronic Supplementary Material of Lopes et al.’s article.6
2.4. Data extraction and data analysis
Data from each included article were extracted by one of the authors of this review (NK) to gain insight into the homogeneity of the study characteristics. The following information was collected: (1) the author(s) and year of publication, (2) study design, (3) description of the population of runners and sample size used, (4) time period, (5) definition of RRMI, (6) anatomical location of injury, yes/no, (7) specific type of injury, yes/no, (8) number of injured runners, (9) number of total injuries, (10) incidence by anatomical location and, where possible, specific injury, and (11) prevalence by anatomical location and, where possible, specific injury (Supplementary Table 1). Incidence proportion data were extracted from prospective studies that assessed runners who were followed over the time period of the study (new injuries analysis). Prevalence proportion data were extracted from cross-sectional and/or retrospective studies in which runners reported their past RRMIs. Due to the heterogeneity of study designs, the studies were grouped according to lower limb RRMI anatomic location and according to specific pathologies (Table 1, Table 2). The anatomic regions used to categorize the injuries were: “hip” (hip joint/groin/pelvis), “upper leg” (thigh), “knee”, “lower leg” (tibial/shank), “ankle”, “foot and toes”, and “other” (location/unclear diagnosis/upper limp/upper trunk).10 The proportion of injury incidence and prevalence data were calculated by dividing the total number of injuries per anatomic region or specific pathology by the total number of injuries reported from all anatomic locations or pathologies, respectively. Specific pathology was defined as a pathology that was medically diagnosed or accurately self-reported. The ultramarathoners were analyzed separately from the other runners because all the studies on ultramarathoners were conducted during races that lasted between 5.0 days and 8.5 days, and Lopes et al.6 showed that ultramarathoners have different injury characteristics than other runners. The total number of injuries per specific pathology was used as the main criteria to rank the most frequent diagnosis. The overall injury incidence was calculated from only the prospective studies, and it was defined as the number of injured runners divided by the total number of runners in the study. The overall injury prevalence was calculated from all studies regardless of their design, and it was defined as the number of injured runners divided by the total number of runners in the study. The overall injury incidence and prevalence estimates did not consider ultramarathon runners. Injury definitions were categorized into time-loss injuries and pain-related injuries. Time-loss injuries were defined as RRMIs that led to the reduction of training volume for at least 1 training session. Pain-related injuries were defined as those in which running-related pain was experienced despite the consequences on training volume. All descriptive analyses were conducted using Microsoft Excel (Version 16.0; Microsoft Corp., Redmond, WA, USA).
Table 1.
Injury prevalence and incidence of non-ultramarathoners and ultramarathoners categorized by different anatomic locations.
| Non-ultramarathoners |
Ultramarathoners |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Location | Prevalence proportion (n (%)) | Range (%) | Studies | Incidence proportion (n (%)) | Range (%) | Studies | Incidence proportion (n (%)) | Range (%) | Studies |
| Knee | 3919 (31.2) | 11.6–48.0 | 9,28,31,34,44,45,47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60 | 1036 (26.2) | 14.3–36.4 | 20,21,23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39 | 39 (28.1) | 19.4–41.7 | 40, 41, 42, 43 |
| Ankle | 1669 (13.3) | 6.1–34.2 | 9,28,31,34,44,47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60 | 752 (19.0) | 7.7–28.6 | 20,21,23, 24, 25,27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39 | 48 (34.5) | 28.1–48.1 | 40, 41, 42, 43 |
| Lower leg | 2524 (20.1) | 7.8–35.0 | 9,28,31,34,44,45,47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60 | 655 (16.6) | 5.1–38.8 | 20,21,23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39 | 18 (12.9) | 8.3–14.8 | 40, 41, 42, 43 |
| Foot/toes | 1810 (14.4) | 5.2–34.9 | 9,28,31,34,44,45,47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60 | 535 (13.5) | 2.9–36.1 | 20,21,23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39 | 6 (4.3) | 5.6–6.3 | 42,43 |
| Hip/groin | 877 (7.0) | 4.0–14.5 | 9,31,34,44,45,47,48,51,53, 54, 55,57, 58, 59, 60 | 446 (11.3) | 3.5–18.4 | 20,23, 24, 25, 26, 27,29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39 | 8 (5.8) | 8.3–11.1 | 40,41,43 |
| Thigh | 862 (6.9) | 1.5–32.0 | 9,28,31,34,44,45,47, 48, 49,51,53, 54, 55, 56, 57, 58, 59, 60 | 315 (8.0) | 2.0–14.3 | 20,21,23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38 | 12 (8.6) | 8.3–11.1 | 40,42,43 |
| Lower back | 434 (3.5) | 2.2–11.5 | 28,44,45,47, 48, 49,51,54,55,58, 59, 60 | 108 (2.7) | 1.5–15.2 | 20,23, 24, 25, 26, 27, 28,32,35,36,38 | 6 (4.3) | 5.6–6.3 | 42,43 |
| Other | 468 (3.7) | 2.6–47.8 | 28,34,44,51,52,55, 56, 57, 58,60 | 108 (2.7) | 2.1–19.0 | 21,23,25,26,28,32,34,36,38 | 2 (1.4) | 3.1 | 42 |
Note: The sum of the percentages is not equal to 100% due to rounding.
Table 2.
Injury prevalence and incidence of non-ultramarathoners and ultramarathoners categorized by specific pathology.
| Non-ultramarathoners |
Ultramarathoners |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Diagnosis | Prevalence proportion (n (%)) | Range (%) | Studies | Incidence proportion (n (%)) | Range (%) | Studies | Incidence proportion (n (%)) | Range (%) | Studies |
| Patellofemoral pain syndrome | 1776 (16.7) | 2.2–32.0 | 44, 45, 46, 47, 48, 49, 50, 51, 52,59 | 35 (6.3) | 1.5–10.2 | 20, 21, 22, 23 | 22 (15.8) | 7.4–41.7 | 40, 41, 42, 43 |
| Medial tibial stress syndrome | 968 (9.1) | 3.7–35.0 | 44, 45, 46, 47,50, 51, 52 | 52 (9.4) | 3.4–19.0 | 21, 22, 23,39 | 8 (5.8) | 7.8–11.1 | 41,42 |
| Plantar fasciitis | 838 (7.9) | 2.2–17.4 | 44, 45, 46, 47,49, 50, 51, 52 | 34 (6.1) | 3.9–21.6 | 20, 21, 22, 23,39 | ― | ― | ― |
| Iliotibial band syndrome | 836 (7.9) | 2.2–17.4 | 44, 45, 46, 47, 48, 49, 50,52,59 | 28 (5.1) | 3.4–15.7 | 20,22,23,39 | 3 (2.2) | 4.7 | 42 |
| Achilles tendinopathy | 705 (6.6) | 2.2–18.6 | 44, 45, 46, 47,49, 50, 51, 52 | 57 (10.3) | 7.1–15.0 | 20, 21, 22, 23,39 | 19 (13.7) | 7.8–19.4 | 40, 41, 42, 43 |
| Stress fracture/fracture (tibia, fibula, fifth metatarsal, navicular, and calcaneus) | 605 (5.7) | 1.7–16.0 | 44, 45, 46, 47, 48, 49, 50, 51, 52,59 | 22 (4.0) | 0.5–9.1 | 20,22,23,39 | ― | ― | ― |
| Ankle sprain | 603 (5.7) | 0.8–27.4 | 44, 45, 46, 47,49, 50, 51,59 | 32 (5.8) | 2.8–19.0 | 20, 21, 22, 23 | 1 (0.7) | 8.3 | 40 |
| Quadriceps/hamstring tendinopathy | 378 (3.6) | 0.7–12.7 | 44,47,51 | ― | ― | ― | 4 (2.9) | 6.3 | 42 |
| Patella tendinopathy | 305 (2.9) | 4.2–12.3 | 45, 46, 47, 48 | 19 (3.4) | 1.5–22.7 | 22,23,39 | 6 (4.3) | 2.8–18.5 | 41,43 |
| Meniscal injury | 181 (1.7) | 3.5–5.0 | 44,46,49 | 24 (4.3) | 0.5–9.1 | 22,23 | ― | ― | ― |
| Anterior knee pain | 135 (1.3) | 15.8 | 51 | 21 (3.8) | 10.2 | 23 | ― | ― | ― |
| Gluteal strain/tendinopathy | 123 (1.2) | 1.3–3.5 | 45,46 | 25 (4.5) | 1.0–9.8 | 20,22,23 | 1 (0.7) | 2.8 | 43 |
| Tibialis posterior tendinopathy | 114 (1.1) | 0.5–16.0 | 45, 46, 47,59 | 2 (0.4) | 0.5–2.0 | 20,23 | 1 (0.7) | 2.8 | 43 |
| Calf strain | 104 (1.0) | 1.3–2.2 | 45, 46, 47,49 | 23 (4.2) | 2.0–4.7 | 20,22,39 | 1 (0.7) | 3.7 | 41 |
| Quadriceps/hamstring strain | 100 (0.9) | 1.2–6.7 | 45, 46, 47,49 | 19 (3.4) | 3.1–7.8 | 20,22,23 | 7 (5.0) | 2.8–5.6 | 40,42,43 |
| Adductor strain | 69 (0.6) | 1.1–2.2 | 45, 46, 47,49 | ― | ― | ― | ― | ― | ― |
| Spinal injuries | 69 (0.6) | 2.3–11.2 | 46,48 | ― | ― | ― | ― | ― | ― |
| Calf tendinopathy | 55 (0.5) | 6.4 | 51 | ― | ― | ― | ― | ― | ― |
| Lower back pain | 44 (0.4) | 1.5–4.7 | 47,49,51,59 | 5 (0.9) | 1.0 | 23 | 4 (2.9) | 3.1–5.6 | 42,43 |
| Knee sprain | 43 (0.4) | 1.5–4.7 | 47,49,51 | ― | ― | ― | ― | ― | ― |
| Inguinal hernias | 40 (0.4) | 4.7 | 51 | ― | ― | ― | ― | ― | ― |
| Metatarsalgia | 36 (0.3) | 1.7–8.0 | 46,59 | ― | ― | ― | 2 (1.4) | 5.6 | 43 |
| Anterior compartment syndrome | 31 (0.3) | 1.4–2.2 | 46,47 | 6 (1.1) | 2.4 | 22 | 8 (5.8) | 6.3–11.1 | 42,43 |
| Trochanteric bursitis | 24 (0.2) | 0.7–1.1 | 46,47 | 4 (0.7) | 1.6 | 22 | 6 (4.3) | 3.1–8.3 | 40,42,43 |
| Sacroiliac injuries | 22 (0.2) | 1.0–4.0 | 46,59 | ― | ― | ― | ― | ― | ― |
| Knee osteoarthritis | 21 (0.2) | 1.0 | 46 | 3 (0.5) | 1.2 | 22 | ― | ― | ― |
| Iliopsoas injury | ― | ― | ― | 6 (1.1) | 0.5–2.0 | 22,23 | 3 (2.2) | 11.1 | 41 |
| Ankle dorsiflexors tendinopathy | ― | ― | ― | 5 (0.9) | 0.5–7.8 | 20,23 | ― | ― | ― |
| Adductor tendinopathy | ― | ― | ― | 5 (0.9) | 1.6–4.5 | 22,39 | ― | ― | ― |
| Pes anserinus tendinopathy | ― | ― | ― | 3 (0.5) | 1.2 | 22 | ― | ― | ― |
| Tensor fascia latae tendinopathy | ― | ― | ― | 3 (0.5) | 1.2 | 22 | ― | ― | ― |
| Retrocalcaneal bursitis | ― | ― | ― | 2 (0.4) | 9.1 | 39 | ― | ― | ― |
| Foot laceration/abrasion | ― | ― | ― | 2 (0.4) | 1.0 | 23 | ― | ― | ― |
| Anterior compartment tendinopathy | ― | ― | ― | ― | ― | ― | 27 (19.4) | 13.9–29.6 | 40, 41, 42, 43 |
| Non-specific knee pain | ― | ― | ― | ― | ― | ― | 3 (2.2) | 2.8–3.1 | 42,43 |
| Peroneal tendinopathy | ― | ― | ― | ― | ― | ― | 2 (1.4) | 3.1 | 43 |
| Sartorius strain | ― | ― | ― | ― | ― | ― | 1 (0.7) | 2.8 | 42 |
Notes: Some specific pathologies are not included in the table because of the small number of injuries and therefore the percentages do not add to 100%. However, they are included in the total figures.
2.5. Statistical analysis
The statistical analysis to compare the injury incidence proportions by anatomic location between ultramarathoners and non-ultramarathoners was conducted using Statistical Package for the Social Sciences (SPSS) (Version 25.0; IBM Corp., Armonk, NY, USA). The data were not normally distributed according to the Shapiro–Wilk test (W(8) ≥ 0.817, p ≥ 0.043). Therefore, the analysis of ultramarathon and non-ultramarathon runners was performed by the Mann–Whitney U test.
3. Results
3.1. Study characteristics
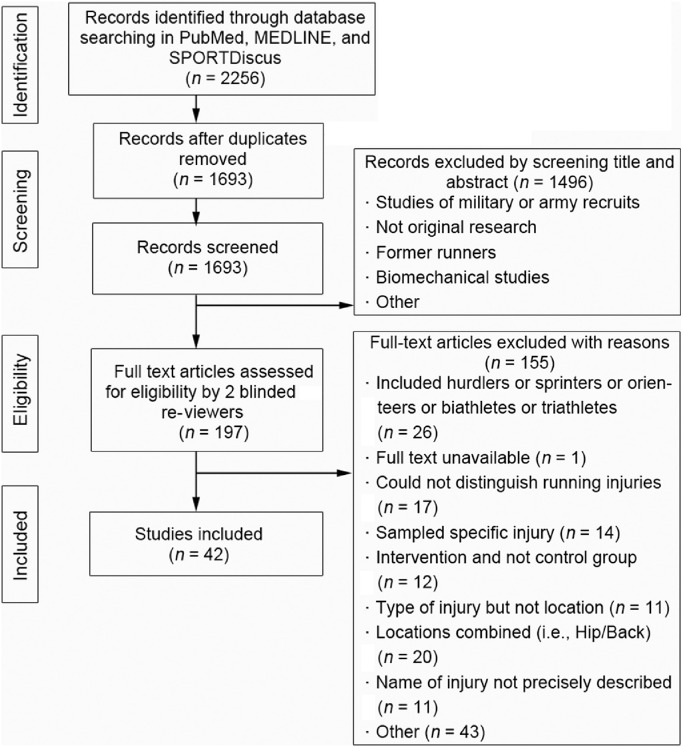
A total of 2256 articles were identified from the 3 databases. Among these articles, 563 were duplicates and were removed. After the screening of the 1693 remaining titles and abstracts, 197 potentially relevant full-text articles were retrieved and evaluated according to the inclusion and exclusion criteria. After evaluation, 155 of the 197 articles were excluded. Hence, a total of 42 studies that presented data on RRMIs met the inclusion criteria. Fig. 1 illustrates the selection process in a flowchart. Of the 42 included studies, 24 were prospective cohort studies.21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44 Of these, 3 studies included retrospective injury proportion data.29,32,35 A total of 15 articles were retrospective studies,9,45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58 and the remaining 3 articles were cross-sectional studies.59, 60, 61
Fig. 1.
Flowchart for the inclusion process of the articles in the systematic review.
A total of 5 studies presented injury proportions among cross-country runners,26,30,36,51,58 and 1 study examined trail-runners.24 For ultramarathon runners, injury proportions were reported in 4 studies,41, 42, 43, 44 5 studies examined marathon runners9,35,52,56,60 and 3 studies looked at injury proportions among half-marathon runners.32,35,52 The majority of the studies were conducted among long-distance runners,21,22,25,27,29,31, 32, 33,37,39,40,47, 48, 49,53, 54, 55,57,59,61 while middle-distance runners were studied in 10 studies.27,32,45,46,48,50,53, 54, 55,59
A total of 5 studies reported the injury occurrence in novice runners;23,28,34,35,38 16 studies in recreational runners,9,22,24, 25, 26,29,32,33,35,37,39,46,53,55,57,61 5 studies in amateur runners,40,45,47,59,60 15 studies in competitive runners,21,26,30,31,36,39,41, 42, 43, 44,50,51,53,57,58 and 7 studies in elite runners.27,43,44,48,52,58,60 Most of the studies reported both acute and chronic injuries; however, 5 studies reported only chronic injuries.25,27,28,53,54
The year of publication of the included studies ranged from 1974 to 2020. The follow-up periods for the prospective cohort studies that were used to estimate the incidence rate of the RRMIs ranged from 6 weeks to 15 years, where only 1 study had a follow-up period of more than 24 months26 and only 3 studies had follow-up periods of less than 3 months.28,36,38 The ultramarathon studies captured the RRMIs during races that varied from 5.0 days to 8.5 days. For the estimation of prevalence, the recall periods of retrospective cohort and cross-sectional studies ranged from 6 months to 17 years, with the most common recall period being 12 months. An injury definition was used in 32 studies.9,22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40,44,45,47,48,50,52, 53, 54, 55,57,58,61 A total of 24 studies used a time-loss injury definition,23,25, 26, 27, 28, 29, 30, 31, 32, 33,35, 36, 37, 38, 39, 40,47,48,53, 54, 55,57,58,61 8 studies used a pain-related definition,9,22,24,34,44,45,50,52 and the remaining 10 studies did not specify an injury definition.21,41, 42, 43,46,49,51,56,59,60
The overall injury incidence, based on 10,941 total participants, of which 3222 sustained RRMIs, was 40.2% ± 18.8% (mean ± SD). This was estimated from a total of 18 prospective studies where injured runners could be separated from the total number of runners in the studies. The overall injury prevalence, based on a total population of 22,823, of which 7671 sustained RRMIs, was 44.6% ± 18.4% (n = 31 studies).
3.2. Injury proportions by anatomic location
Table 1 shows the injury prevalence and incidence of non-ultramarathoners and ultramarathoners categorized by different anatomic locations. For non-ultramarathoners, the prevalence injury proportions were calculated from 12,563 injuries reported among 9864 runners (n = 20 studies). The knee and the lower leg regions accounted for over half of all reported injuries (6443/12,563). Foot/toes and ankle were the 3rd and 4th highest proportion of injury locations, respectively. The total number of injuries occurring at or below the knee was 9922 (79.0%). Injuries classified as “other” were of uncertain location or were upper body injuries, these locations were involved in 3.7% of the injuries.
For non-ultramarathoners, the incidences were calculated from 3955 injuries reported by 3284 runners (n = 19 studies). The most frequently injured regions were the knee, followed by the ankle, lower leg, and foot/toes. These regions accounted for 75.3% of all injuries, indicating that most of the injuries occurred at or below the knee. The injury location classified as “other” accounted for 2.7% of the total injuries (Table 1).
For ultramarathon runners, injury incidences were calculated from 139 injuries reported in 67 runners (n = 4 studies). The ankle, knee, and lower leg were the 3 most frequently injured body sites, followed by the thigh, hip/groin, foot/toes, and lower back. The injury location classified as “other” accounted for 1.4% of the total injuries. The injury incidence proportions by anatomic location between ultramarathoners and non-ultramarathoners were not significantly different (p = 0.798) (Table 1).
3.3. Injury proportions by specific pathology
Table 2 shows the injury prevalence and incidence rates and proportions for non-ultramarathoners and ultramarathoners categorized by specific pathology. For non-ultramarathoners, the prevalence data for specific pathologies were calculated from 10,640 injuries reported from 9251 runners included in 10 studies. Patellofemoral pain syndrome (16.7%) had the highest prevalence proportion of RRMI, whereas medial tibial stress syndrome (35.0%) had the highest prevalence rate reported in these studies. The most frequently reported RRMIs were patellofemoral pain syndrome and stress fractures. Furthermore, the incidence rates for specific pathologies were calculated from 554 injuries reported from 475 runners included in 5 studies. In non-ultramarathon runners, the most frequent RRMI was different from ultramarathoners. In non-ultramarathoners, the pathology with the highest incidence proportion of injuries was Achilles tendinopathy (10.3%, incidence ranging from 7.1% to 15.0%), whereas anterior compartment tendinopathy (19.4%, incidence ranging from 13.9% to 29.6%) had the highest proportion of injuries in ultramarathoners. The highest incidence rate for an RRMI reported in the studies was for patellar tendinopathy (22.7%) and in ultramarathon runners it was for patellofemoral pain syndrome (41.7%). The most frequently reported RRMIs among non-ultramarathon runners were Achilles tendinopathy and plantar fasciitis, whereas among ultramarathon runners the most frequently reported RRMIs were anterior compartment tendinopathy, patellofemoral pain syndrome, and Achilles tendinopathy (Table 2).
3.4. ROB
The results of the ROB assessment for each of the 42 studies can be found in Table 3. The overall ROB of the included studies was 58.6%, with a range of 3‒8 out of a total possible score of 10. A total of 7 articles received a ROB score lower than 5 and were classified as having high ROB.45, 46, 47,49, 50, 51,59 It is worth mentioning that all 7 articles were retrospective or cross-sectional studies. The 2 criteria from the ROB list most frequently not presented in the studies were (1) RRMIs reported by a ratio expressing the number of injuries and exposure to running and (2) whether the examination was conducted by a medical doctor.
Table 3.
Risk of bias assessment of all 42 studies included.
| Study | Risk of bias assessment of the studies |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Score | |
| Studies reporting proportion of injury incidence | |||||||||||
| Altman and Davis (2016)21 | N | Y | Y | Y | Y | Y | Y | N | Y | N | 7/10 |
| Jakobsen et al. (1994)22 | Y | Y | Y | N | Y | Y | Y | N | Y | N | 7/10 |
| Nielsen et al. (2014)23 | Y | Y | Y | Y | Y | Y | Y | N | Y | N | 8/10 |
| Hespanhol Jr et al. (2017)24 | Y | Y | Y | N | N | Y | Y | N | Y | N | 6/10 |
| Messier et al. (2018)25 | Y | Y | Y | N | Y | Y | Y | Y | Y | N | 8/10 |
| Rauh et al. (2000)26 | Y | Y | Y | Y | Y | N | Y | N | Y | Y | 8/10 |
| von Rosen et al. (2017)27 | Y | Y | Y | Y | Y | Y | Y | N | Y | N | 8/10 |
| Van Ginckel et al. (2009)28 | Y | Y | Y | Y | Y | Y | Y | N | N | N | 7/10 |
| Hespanhol Jr et al. (2016)29 | Y | Y | Y | N | Y | Y | Y | N | N | N | 6/10 |
| Ruffe et al. (2019)30 | Y | Y | Y | Y | Y | Y | Y | N | Y | N | 8/10 |
| Begizew et al. (2019)31 | Y | Y | Y | Y | Y | Y | Y | N | Y | N | 8/10 |
| van Poppel et al. (2014)32 | Y | Y | Y | Y | N | Y | Y | N | Y | N | 7/10 |
| Hespanhol Jr et al. (2013)33 | Y | Y | Y | N | Y | Y | Y | N | N | N | 6/10 |
| Fokkema et al. (2019)34 | Y | Y | Y | N | Y | Y | Y | N | Y | N | 7/10 |
| Franke et al. (2019)35 | Y | Y | Y | N | N | Y | Y | N | N | N | 5/10 |
| Rauh et al. (2014)36 | Y | Y | Y | N | Y | N | Y | N | N | Y | 6/10 |
| van der Worp et al. (2016)37 | Y | Y | Y | Y | Y | Y | Y | N | N | N | 7/10 |
| Kluitenberg et al. (2015)38 | Y | Y | Y | N | Y | Y | Y | N | N | N | 6/10 |
| Walter et al. (1989)39 | Y | Y | Y | Y | N | Y | N | N | Y | N | 6/10 |
| Pileggi et al. (2010)40 | Y | Y | Y | N | Y | Y | N | Y | Y | N | 7/10 |
| Scheer and Murray (2011a)41 | N | Y | Y | Y | Y | Y | Y | Y | N | N | 7/10 |
| Hutson (1984a)42 | N | Y | Y | Y | Y | Y | Y | Y | N | N | 7/10 |
| Fallon (1996a)43 | N | Y | Y | N | Y | Y | Y | Y | N | N | 6/10 |
| Bishop and Fallon (1999a)44 | Y | Y | Y | Y | Y | Y | Y | Y | N | N | 8/10 |
| Studies reporting proportion of injury prevalence | |||||||||||
| Van Middelkoop et al. (2008)9 | Y | N | Y | Y | N/A | Y | Y | N | Y | N | 6/9 |
| McKean et al. (2006)45 | Y | N | Y | N | N/A | Y | N | N | Y | N | 4/9 |
| Macintyre et al. (1991)46 | N | N | Y | N | N/A | Y | Y | Y | N | N | 4/9 |
| Taunton et al. (2002)47 | Y | N | N | N | N/A | N | Y | Y | N | N | 3/9 |
| Ristolainen et al. (2010)48 | Y | N | Y | Y | N/A | Y | Y | N | Y | N | 6/9 |
| Paty Jr and Swafford (1984)49 | N | N | Y | N | N/A | N | Y | Y | N/A | N | 3/8 |
| Brubaker and James (1974)50 | Y | N | Y | N | N/A | N | Y | Y | N/A | N | 4/8 |
| Tenforde et al. (2011)51 | N | N | Y | Y | N/A | Y | Y | N | N | N | 4/9 |
| Knobloch et al. (2008)52 | Y | Y | Y | N | N/A | Y | Y | N | N/A | Y | 6/8 |
| Schwellnus and Stubbs (2006)53 | Y | N | Y | Y | N/A | Y | Y | N | Y | N | 6/9 |
| Benca et al. (2020)54 | Y | N | Y | N | N/A | Y | Y | Y | Y | N | 6/9 |
| Marti et al. (1988)55 | Y | N | Y | N | N/A | Y | Y | N | Y | N | 5/9 |
| Maughan and Miller (1983)56 | N | N | Y | Y | N/A | Y | Y | N | Y | N | 5/9 |
| Jacobs and Berson (1986)57 | Y | N | Y | Y | N/A | Y | Y | N | N | N | 5/9 |
| Kerr et al. (2016)58 | Y | N | Y | N | N/A | Y | Y | N | N | Y | 5/9 |
| Williams 3rd et al. (2001)59 | N | N | Y | N | N/A | Y | N | Y | N/A | N | 3/8 |
| Ogwumike and Adeniyi (2013)60 | N | Y | Y | Y | N/A | Y | Y | Y | N/A | N | 6/8 |
| Hespanhol Jr et al. (2012)61 | Y | Y | Y | N | N/A | Y | Y | N | N/A | N | 5/8 |
Notes: 1 = injury definition; 2 = prospective study design for incidence proportion or cross-sectional for prevalence proportion; 3 = description or type of runners; 4 = random sample selection process or analyzed entire population; 5 = analysis ≥80% of sample; 6 = injury was evaluated by health professional or self-reported by the runner; 7 = same mode of data collection; 8 = medical doctor diagnosis; 9 = prospective studies follow-up period of ≥6 months and retrospective studies recall period of up to 12 months; 10 = running-related musculoskeletal injuries reported by any ratio that expresses the number of injuries and exposure of runner.
a Ultramarathon studies
Abbreviations: N = no; N/A = not applicable; Y = yes.
4. Discussion
The primary purpose of this systematic review was to present the incidence and prevalence of RRMI proportions among runners by anatomic location and specific pathology. The secondary aim was to compare the injury incidence proportions by anatomic location between ultramarathoners and non-ultramarathoners. There was sufficient literature to satisfy the aims of the study; however, the available studies significantly differed in study design, injury definitions, and type of runners studied. To minimize the heterogeneity of the studies included, the incidence proportion data for injuries were obtained from prospective studies and the prevalence proportion data were collected from retrospective and cross-sectional studies.
In agreement with previous systematic reviews, our study reported that more than 70% of all RRMIs were related to overuse. Additionally, the injuries reported in our study were predominantly at or below the knee. This may be because, during normal running, propulsion is generated mainly by the lower leg, leading to an increased biomechanical load on these structures.62 Our findings were true for both ultramarathoners and non-ultramarathoners and are consistent with previous reviews in which the most common anatomic location of injuries was at or below the knee.6,8,10,16 In non-ultramarathon runners, the knee region had a relatively greater incidence (26.2%) and prevalence (31.2%) proportion of injuries compared to the second-highest anatomic injury site, which had 19.0% and 20.1%, respectively. Francis et al.16 found that female runners had a larger proportion of knee injuries relative to their male counterparts, which may partly explain the relatively high proportion of knee injuries observed in our systematic review. This might be the result of the different lower extremity biomechanics and neuromuscular control in females arising from a greater quadriceps angle (Q angle) and reduced knee flexion angles during landing, which places abnormal loads on the lower limb.63, 64, 65, 66, 67 These gender differences also may have had an impact on the injury proportions for specific pathologies.
In ultramarathoners, the anatomic location with the highest incidence proportion of injuries was the ankle region (34.5%) followed by the knee (28.1%). This is because anterior compartment tendinopathy (19.4%) and Achilles tendinopathy (13.7%) are relatively common among ultramarathon runners during races (Table 2). Moreover, according to Hutson,42 ankle injuries among this population were almost twice as frequent as injuries to the knee. The injury incidence proportions by anatomic location between ultramarathoners and non-ultramarathoners were not significantly different (p = 0.798). In our study, the 3 most common specific pathologies among ultramarathoners were the same as those reported by Lopes et al.;6 however, the pathology with the highest incidence was different. In our study, the anterior compartment tendinopathy had the highest proportion of injury incidence among ultramarathoners, whereas Lopes et al.6 found that Achilles tendinopathy was the most common injury among this group. Anterior compartment tendinopathy (or, as it is referred to in another study, “ultramarathoner's ankle”) is not common among non-ultramarathoners, and this may indicate that this RRMI may be specific to ultramarathoners only.41
The overall injury incidence (40.2%) and prevalence (44.6%) varied greatly (10.9%–74.8%) between the studies and agree with previously reported estimates.13,16 The top injury prevalence and incidence proportions by specific pathology for non-ultramarathoners are presented in Tables 1 and 2, respectively. It has been reported that male runners have a greater proportion of ankle injuries relative to female runners, which may indicate that the incidence proportion of Achilles tendinopathy is male-biased.16 This is supported by Taunton et al.47 and Nielsen et al.,23 who found from an analysis of injuries (n = 2002 and n = 254, respectively) that males were more prone to Achilles tendinopathy and females were more prone to patellofemoral pain syndrome. The main difference observed in our study between the incidence and the prevalence proportion data for each RRMI was that ankle sprains were in the top 5 most common injuries in the incidence data but not in the top 5 in the prevalence data. Kluitenberg et al.10 has stated that prospective studies with follow-up periods are more likely to register a higher number of injuries than retrospective studies with similar recall periods. Therefore, a plausible reason ankle sprains were not in the top 5 in the prevalence data is that, in most cases, ankle sprains are not considered to be serious or severe enough and may not be memorable injuries to runners in retrospective studies where they have to report their past injuries. McKean et al.45 and Knobloch et al.52 had two of the shortest recall periods, 8 months, and 12 months, respectively, and they reported a higher prevalence of ankle sprains compared to other studies. Additionally, the sensitivity, specificity, and positive predictive values of self-reported RRMIs by runners were reported to be good for injury locations but not for specific pathologies.68 Self-reported RRMIs may have influenced the prevalence proportion of specific pathologies by affecting the validity of the retrospective studies.
Among ultramarathoners and non-ultramarathoners, the anatomic locations with the highest incidence proportion of injuries were the knee and ankle. Therefore, coaches and health professionals should focus their injury prevention programs on reducing injuries such as patellofemoral pain syndrome and Achilles tendinopathy in order to reduce the high incidence rates in these locations. Patellofemoral pain syndrome had the highest prevalence proportion of injuries in non-ultramarathoners; thus, developing effective rehabilitation programs may reduce the prevalence proportion of this condition in this population.
Evaluation of the quality of the articles showed a moderate ROB overall, where seven of 42 articles were classified as having high ROB. Although most of the studies had a definition of “injury”, the definition varied considerably across studies, and there is still no agreement about the most appropriate definition for an RRMI.6 A total of 24 studies used time-loss definitions; however, a consensus on the amount of time needed to classify a time loss from running due to an RRMI has yet to be reached. For instance, several studies did not report the amount of time, some studies used days in their definition and other studies used weeks. Additionally, the 8 studies that used a pain-related definition may have overestimated the number of injured runners since a pain-related definition may capture data from high-functioning runners who would not otherwise be considered to be injured. The impact of the definition of “injury” on running-related injury incidence or prevalence has been well established by Kluitenberg et al.,69 who reported incidences that ranged between 7.5% and 58.0%, depending on the definition of injury. This impact stresses the need for standardized injury registration methods.
Many of the articles in this review described types of runners (e.g., half- or full-marathon runners) or their training characteristics (e.g., running ≥10 miles per week) or race participation (e.g., ultramarathon). Published systematic reviews have analyzed the differences in running injuries among different levels of runners; however, the definitions given to describe a runner's level (e.g., novice, recreational, competitive) lack objective data to support their validity.10,19 A more accurate description of the runners’ level would report the volume, frequency, and intensity of running in order to make a more meaningful comparative analysis of the incidence and prevalence rates among different types of runners.
The anatomic location of injury incidence and prevalence was obtained from most of the studies included in our review, except for 2 studies that did not separately report foot and ankle injuries.23,47 The specific pathology incidence data and prevalence proportion data could only be obtained from 5 studies and 10 studies, respectively. Given the challenges in reporting an accurate diagnosis that might be expected. RRMIs should be diagnosed by a physician or general practitioner in order to minimize the ROB and misdiagnosis of the injury. An alternative approach would be to allow self-reported injuries but to also provide the source of diagnosis (e.g., medical professional, physiotherapist, coach). This would provide a crude estimate of specific pathologies and a better indication of whether the injuries were underestimated or overestimated.16 For example, injuries that have been diagnosed by the coach and self-diagnosed by the participant may lead to underestimation or overestimation of the number of injuries since the participant may or may not be considered injured if diagnosed by a physician, respectively. Moreover, there can be issues in terms of interpretation of injury definition, nature, and severity in studies that used data champions to record and submit data, leading to underreporting or overreporting of injuries.
In the studies included in our review, there were 6 prospective ones with follow-up periods of ≤3 months. Many injuries occurring during running involve overuse and are caused by repetitive microtrauma over a long period of time, leading to an overload on musculoskeletal structures.7,70 Therefore, prospective studies with longer follow-up periods are needed to examine all possible RRMIs because studies with shorter follow-up periods may have underestimate the number of overuse injuries.6 In addition, several studies included in our review did not report the total number of injured runners or the total number of injuries. Thus, this lack of clarity and consistency among studies made it difficult to obtain accurate estimates of injury incidence and prevalence proportions.
There are some limitations to our review. First, a systematic search was performed only in the 3 above-mentioned databases. It is possible that eligible studies could have been indexed in other search databases. Second, since the amount of running exposure may influence the development of RRMIs, the preferred way of reporting injury incidence is to express the total number of injuries per 1000 h of exposure to running.19,71 However, this was not possible because only a limited number of the included studies reported the incidence or prevalence ratio for each specific pathology. Therefore, a standardized expression of running-related injury data would enable comparison or pooling of data for meta-analysis.6
5. Conclusion
Broad inclusion criteria were used to estimate the incidence and prevalence proportion of RRMIs by anatomic location and specific pathologies. To our knowledge, our review is the first to take this approach. Among non-ultramarathoners, the highest proportion of injuries in both incidence and prevalence was in the knee, whereas among ultramarathoners the most injured site was the ankle. The injury incidence proportions by anatomic location between ultramarathoners and non-ultramarathoners were not significantly different (p = 0.798). In prospective studies, the top 5 pathologies with the highest incidence proportions among non-ultramarathoners were Achilles tendinopathy, medial tibial stress syndrome, patellofemoral pain syndrome, plantar fasciitis, and ankle sprain. In retrospective/cross-sectional studies, the top 5 pathologies were the same as in prospective studies except ankle sprains were replaced by iliotibial band syndrome. These findings are supported by previous research and systematic reviews conducted on the topic. For runners who participated in ultramarathon events that ranged from 5.0 days to 8.5 days, anterior compartment tendinopathy, patellofemoral pain syndrome and Achilles tendinopathy were the 3 most common RRMIs.
This systematic review provides valuable information to sports medicine specialists who are deciding on the most appropriate injury prevention measures that should be taken for a given anatomic location or specific pathology. We recommend that injury prevention measures related to the knee (e.g., patellofemoral pain syndrome) and ankle (e.g., Achilles tendinopathy) should be implemented in order to reduce the high incidence rates at these locations in the running population. Future research on injury occurrences should address the issues raised in this review.
Acknowledgments
Authors’ contributions
NK designed the study, acquired the data, analyzed and interpreted the data, drafted the manuscript, and approved the final version of the manuscript; NY analyzed and interpreted the data, and critically revised the manuscript; DTPF designed the study and critically revised and approved the final version of the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jshs.2021.04.001.
Appendix. Supplementary materials
References
- 1.van Poppel D, van der Worp M, Slabbekoorn A. Risk factors for overuse injuries in short- and long-distance running: A systematic review. J Sport Health Sci. 2021;10:14–28. doi: 10.1016/j.jshs.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vitti A, Nikolaidis P, Villiger E, Onywera V, Knechtle B. The “New York City Marathon”: Participation and performance trends of 1.2M runners during half-century. Res Sports Med. 2020;28:121–137. doi: 10.1080/15438627.2019.1586705. [DOI] [PubMed] [Google Scholar]
- 3.Bredeweg SW, Zijlstra S, Bessem B, Buist I. The effectiveness of a preconditioning programme on preventing running-related injuries in novice runners: A randomised controlled trial. Br J Sports Med. 2012;46:865–870. doi: 10.1136/bjsports-2012-091397. [DOI] [PubMed] [Google Scholar]
- 4.Buist I, Bredeweg SW, van Mechelen W, Lemmink KA, Pepping GJ, Diercks RL. No effect of a graded training program on the number of running-related injuries in novice runners: A randomized controlled trial. Am J Sports Med. 2008;36:33–39. doi: 10.1177/0363546507307505. [DOI] [PubMed] [Google Scholar]
- 5.Fields KB, Sykes JC, Walker KM, Jackson JC. Prevention of running injuries. Curr Sports Med Rep. 2010;9:176–182. doi: 10.1249/JSR.0b013e3181de7ec5. [DOI] [PubMed] [Google Scholar]
- 6.Lopes AD, Hespanhol Júnior LC, Yeung SS, Costa LO. What are the main running-related musculoskeletal injuries? A systematic review. Sports Med. 2012;42:891–905. doi: 10.1007/BF03262301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bertelsen ML, Hulme A, Petersen J. A framework for the etiology of running-related injuries. Scand J Med Sci Sports. 2017;27:1170–1180. doi: 10.1111/sms.12883. [DOI] [PubMed] [Google Scholar]
- 8.van Gent RN, Siem D, van Middelkoop M, van Os AG, Bierma-Zeinstra SM, Koes BW. Incidence and determinants of lower extremity running injuries in long distance runners: A systematic review. Br J Sports Med. 2007;41:469–480. doi: 10.1136/bjsm.2006.033548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Middelkoop M, Kolkman J, Van Ochten J, Bierma-Zeinstra SM, Koes B. Prevalence and incidence of lower extremity injuries in male marathon runners. Scand J Med Sci Sports. 2008;18:140–144. doi: 10.1111/j.1600-0838.2007.00683.x. [DOI] [PubMed] [Google Scholar]
- 10.Kluitenberg B, van Middelkoop M, Diercks R, van der Worp H. What are the differences in injury proportions between different populations of runners? A systematic review and meta-analysis. Sports Med. 2015;45:1143–1161. doi: 10.1007/s40279-015-0331-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noordzij M, Dekker FW, Zoccali C, Jager KJ. Measures of disease frequency: Prevalence and incidence. Nephron Clin Pract. 2010;115:c17–c20. doi: 10.1159/000286345. [DOI] [PubMed] [Google Scholar]
- 12.Chang WL, Shih YF, Chen WY. Running injuries and associated factors in participants of ING Taipei Marathon. Phys Ther Sport. 2012;13:170–174. doi: 10.1016/j.ptsp.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 13.van der Worp MP, ten Haaf DS, van Cingel R, de Wijer A, Nijhuis-van der Sanden MW, Staal JB. Injuries in runners; A systematic review on risk factors and sex differences. PLoS One. 2015;10 doi: 10.1371/journal.pone.0114937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hreljac A. Impact and overuse injuries in runners. Med Sci Sports Exerc. 2004;36:845–849. doi: 10.1249/01.mss.0000126803.66636.dd. [DOI] [PubMed] [Google Scholar]
- 15.Arnold MJ, Moody AL. Common running injuries: Evaluation and management. Am Fam Physician. 2018;97:510–516. [PubMed] [Google Scholar]
- 16.Francis P, Whatman C, Sheerin K, Hume P, Johnson MI. The proportion of lower limb running injuries by gender, anatomical location and specific pathology: A systematic review. J Sports Sci Med. 2019;18:21–31. [PMC free article] [PubMed] [Google Scholar]
- 17.Tenforde AS, Yin A, Hunt KJ. Foot and ankle injuries in runners. Phys Med Rehabil Clin N Am. 2016;27:121–137. doi: 10.1016/j.pmr.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 18.van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, aetiology and prevention of sports injuries. A review of concepts. Sports Med. 1992;14:82–99. doi: 10.2165/00007256-199214020-00002. [DOI] [PubMed] [Google Scholar]
- 19.Videbæk S, Bueno AM, Nielsen RO, Rasmussen S. Incidence of running-related injuries per 1000 h of running in different types of runners: A systematic review and meta-analysis. Sports Med. 2015;45:1017–1026. doi: 10.1007/s40279-015-0333-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG, Group PRISMA. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 21.Altman AR, Davis IS. Prospective comparison of running injuries between shod and barefoot runners. Br J Sports Med. 2016;50:476–480. doi: 10.1136/bjsports-2014-094482. [DOI] [PubMed] [Google Scholar]
- 22.Jakobsen BW, Krøner K, Schmidt SA, Kjeldsen A. Prevention of injuries in long-distance runners. Knee Surg Sports Traumatol Arthrosc. 1994;2:245–249. doi: 10.1007/BF01845597. [DOI] [PubMed] [Google Scholar]
- 23.Nielsen RO, Rønnow L, Rasmussen S, Lind M. A prospective study on time to recovery in 254 injured novice runners. PLoS One. 2014;9:e99877. doi: 10.1371/journal.pone.0099877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hespanhol Jr LC, van Mechelen W, Verhagen E. Health and economic burden of running-related injuries in Dutch trailrunners: A prospective cohort study. Sports Med. 2017;47:367–377. doi: 10.1007/s40279-016-0551-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Messier SP, Martin DF, Mihalko SL. A 2-year prospective cohort study of overuse running injuries: The runners and injury longitudinal study (TRAILS) Am J Sports Med. 2018;46:2211–2221. doi: 10.1177/0363546518773755. [DOI] [PubMed] [Google Scholar]
- 26.Rauh MJ, Margherita AJ, Rice SG, Koepsell TD, Rivara FP. High school cross country running injuries: A longitudinal study. Clin J Sport Med. 2000;10:110–116. doi: 10.1097/00042752-200004000-00005. [DOI] [PubMed] [Google Scholar]
- 27.von Rosen P, Floström F, Frohm A, Heijne A. Injury patterns in adolescent elite endurance athletes participating in running, orienteering, and cross-country skiing. Int J Sports Phys Ther. 2017;12:822–832. [PMC free article] [PubMed] [Google Scholar]
- 28.Van Ginckel A, Thijs Y, Hesar NG. Intrinsic gait-related risk factors for Achilles tendinopathy in novice runners: A prospective study. Gait Posture. 2009;29:387–391. doi: 10.1016/j.gaitpost.2008.10.058. [DOI] [PubMed] [Google Scholar]
- 29.Hespanhol Jr LC, de Carvalho AC, Costa LO, Lopes AD. Lower limb alignment characteristics are not associated with running injuries in runners: Prospective cohort study. Eur J Sport Sci. 2016;16:1137–1144. doi: 10.1080/17461391.2016.1195878. [DOI] [PubMed] [Google Scholar]
- 30.Ruffe NJ, Sorce SR, Rosenthal MD, Rauh MJ. Lower quarter-and upper quarter y balance tests as predictors of running-related injuries in high school cross-country runners. Int J Sports Phys Ther. 2019;14:695–706. [PMC free article] [PubMed] [Google Scholar]
- 31.Begizew DM, Grace JM, van Heerden HJ. Lower-extremity running-related injuries among 10,000-meter long distance runners in Ethiopia. J Hum Sport Exerc. 2019;14:358–373. [Google Scholar]
- 32.van Poppel D, Scholten-Peeters GG, van Middelkoop M, Verhagen AP. Prevalence, incidence and course of lower extremity injuries in runners during a 12-month follow-up period. Scand J Med Sci Sports. 2014;24:943–949. doi: 10.1111/sms.12110. [DOI] [PubMed] [Google Scholar]
- 33.Hespanhol Jr LC, Pena Costa LO, Lopes AD. Previous injuries and some training characteristics predict running-related injuries in recreational runners: A prospective cohort study. J Physiother. 2013;59:263–269. doi: 10.1016/S1836-9553(13)70203-0. [DOI] [PubMed] [Google Scholar]
- 34.Fokkema T, Burggraaff R, Hartgens F. Prognosis and prognostic factors of running-related injuries in novice runners: A prospective cohort study. J Sci Med Sport. 2019;22:259–263. doi: 10.1016/j.jsams.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 35.Franke TPC, Backx FJG, Huisstede BMA. Running themselves into the ground? Incidence, prevalence, and impact of injury and illness in runners preparing for a half or full marathon. J Orthop Sports Phys Ther. 2019;49:518–528. doi: 10.2519/jospt.2019.8473. [DOI] [PubMed] [Google Scholar]
- 36.Rauh MJ. Summer training factors and risk of musculoskeletal injury among high school cross-country runners. J Orthop Sports Phys Ther. 2014;44:793–804. doi: 10.2519/jospt.2014.5378. [DOI] [PubMed] [Google Scholar]
- 37.van der Worp MP, de Wijer A, van Cingel R, Verbeek AL, Nijhuis-van der Sanden MW, Staal JB. The 5- or 10-km Marikenloop Run: A prospective study of the etiology of running-related injuries in women. J Orthop Sports Phys Ther. 2016;46:462–470. doi: 10.2519/jospt.2016.6402. [DOI] [PubMed] [Google Scholar]
- 38.Kluitenberg B, van Middelkoop M, Smits DW. The NLstart2run study: Incidence and risk factors of running-related injuries in novice runners. Scand J Med Sci Sports. 2015;25:e515–e523. doi: 10.1111/sms.12346. [DOI] [PubMed] [Google Scholar]
- 39.Walter SD, Hart LE, McIntosh JM, Sutton JR. The Ontario cohort study of running-related injuries. Arch Intern Med. 1989;149:2561–2564. [PubMed] [Google Scholar]
- 40.Pileggi P, Gualano B, Souza M. Incidence and risk factors of lower limb injury in runners: A prospective cohort study (Incidência e fatores de risco de lesões osteomioarticulares em corredores: Um estudo de coorte prospectivo) Rev Bras Educ Fís Esporte. 2010;24:453–462. [In Portuguese] [Google Scholar]
- 41.Scheer BV, Murray A. Al Andalus Ultra Trail: An observation of medical interventions during a 219-km, 5-day ultramarathon stage race. Clin J Sport Med. 2011;21:444–446. doi: 10.1097/JSM.0b013e318225b0df. [DOI] [PubMed] [Google Scholar]
- 42.Hutson MA. Medical implications of ultra marathon running: Observations on a six day track race. Br J Sports Med. 1984;18:44–45. doi: 10.1136/bjsm.18.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fallon KE. Musculoskeletal injuries in the ultramarathon: The 1990 Westfield Sydney to Melbourne run. Br J Sports Med. 1996;30:319–323. doi: 10.1136/bjsm.30.4.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bishop GW, Fallon KE. Musculoskeletal injuries in a six-day track race: Ultramarathoner's ankle. Clin J Sport Med. 1999;9:216–220. doi: 10.1097/00042752-199910000-00006. [DOI] [PubMed] [Google Scholar]
- 45.McKean KA, Manson NA, Stanish WD. Musculoskeletal injury in the masters runners. Clin J Sport Med. 2006;16:149–154. doi: 10.1097/00042752-200603000-00011. [DOI] [PubMed] [Google Scholar]
- 46.Macintyre JG, Taunton JE, Clement DB, Lloyd-Smith DR, McKenzie DC, Morrell RW. Running injuries: A clinical study of 4173 cases. Clin J Sport Med. 1991;1:81–87. [Google Scholar]
- 47.Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36:95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ristolainen L, Heinonen A, Turunen H. Type of sport is related to injury profile: A study on cross country skiers, swimmers, long-distance runners and soccer players. A retrospective 12-month study. Scand J Med Sci Sports. 2010;20:384–393. doi: 10.1111/j.1600-0838.2009.00955.x. [DOI] [PubMed] [Google Scholar]
- 49.Paty Jr JG, Swafford D. Adolescent running injuries. J Adolesc Health Care. 1984;5:87–90. doi: 10.1016/s0197-0070(84)80004-2. [DOI] [PubMed] [Google Scholar]
- 50.Brubaker CE, James SL. Injuries to runners. J Sports Med. 1974;2:189–198. doi: 10.1177/036354657400200402. [DOI] [PubMed] [Google Scholar]
- 51.Tenforde AS, Sayres LC, McCurdy ML, Collado H, Sainani KL, Fredericson M. Overuse injuries in high school runners: Lifetime prevalence and prevention strategies. PM R. 2011;3:125–131. doi: 10.1016/j.pmrj.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 52.Knobloch K, Yoon U, Vogt PM. Acute and overuse injuries correlated to hours of training in master running athletes. Foot Ankle Int. 2008;29:671–676. doi: 10.3113/FAI.2008.0671. [DOI] [PubMed] [Google Scholar]
- 53.Schwellnus MP, Stubbs G. Does running shoe prescription alter the risk of developing a running injury? Int Sport Med J. 2006;7:138–153. [Google Scholar]
- 54.Benca E, Listabarth S, Flock FKJ. Analysis of running-related injuries: The Vienna Study. J Clin Med. 2020;9:438. doi: 10.3390/jcm9020438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marti B, Vader JP, Minder CE, Abelin T. On the epidemiology of running injuries. The 1984 Bern Grand-Prix study. Am J Sports Med. 1988;16:285–294. doi: 10.1177/036354658801600316. [DOI] [PubMed] [Google Scholar]
- 56.Maughan RJ, Miller JD. Incidence of training-related injuries among marathon runners. Br J Sports Med. 1983;17:162–165. doi: 10.1136/bjsm.17.3.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jacobs SJ, Berson BL. Injuries to runners: A study of entrants to a 10,000 meter race. Am J Sports Med. 1986;14:151–155. doi: 10.1177/036354658601400211. [DOI] [PubMed] [Google Scholar]
- 58.Kerr ZY, Kroshus E, Grant J. Epidemiology of national collegiate athletic association men's and women's cross-country injuries, 2009–2010 through 2013–2014. J Athl Train. 2016;51:57–64. doi: 10.4085/1062-6050-51.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Williams 3rd DS, McClay IS, Hamill J. Arch structure and injury patterns in runners. Clin Biomech (Bristol, Avon) 2001;16:341–347. doi: 10.1016/s0268-0033(01)00005-5. [DOI] [PubMed] [Google Scholar]
- 60.Ogwumike OO, Adeniyi AF. The SPLASH/ICPC integrity marathon in Ibadan, Nigeria: Incidence and management of injuries and marathon-related health problems. BMC Sports Sci Med Rehabil. 2013;5:6. doi: 10.1186/2052-1847-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hespanhol Jr LC, Costa LO, Carvalho AC, Lopes AD. A description of training characteristics and its association with previous musculoskeletal injuries in recreational runners: A cross-sectional study. Rev Bras Fisioter. 2012;16:46–53. [PubMed] [Google Scholar]
- 62.Schache AG, Dorn TW, Williams GP, Brown NA, Pandy MG. Lower-limb muscular strategies for increasing running speed. J Orthop Sports Phys Ther. 2014;44:813–824. doi: 10.2519/jospt.2014.5433. [DOI] [PubMed] [Google Scholar]
- 63.Sigward SM, Powers CM. The influence of gender on knee kinematics, kinetics and muscle activation patterns during side-step cutting. Clin Biomech (Bristol, Avon) 2006;21:41–48. doi: 10.1016/j.clinbiomech.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 64.Wetters N, Weber AE, Wuerz TH, Schub DL, Mandelbaum BR. Mechanism of injury and risk factors for anterior cruciate ligament injury. Oper Tech Sports Med. 2016;24:2–6. [Google Scholar]
- 65.Padua DA, DiStefano LJ, Hewett TE. National Athletic Trainers' Association position statement: Prevention of anterior cruciate ligament injury. J Athl Train. 2018;53:5–19. doi: 10.4085/1062-6050-99-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fleming BC, Renstrom PA, Ohlen G. The gastrocnemius muscle is an antagonist of the anterior cruciate ligament. J Orthop Res. 2001;19:1178–1184. doi: 10.1016/S0736-0266(01)00057-2. [DOI] [PubMed] [Google Scholar]
- 67.Meyer EG, Haut RC. Anterior cruciate ligament injury induced by internal tibial torsion or tibiofemoral compression. J Biomech. 2008;41:3377–3383. doi: 10.1016/j.jbiomech.2008.09.023. [DOI] [PubMed] [Google Scholar]
- 68.Smits DW, Backx F, Van Der Worp H. Validity of injury self-reports by novice runners: Comparison with reports by sports medicine physicians. Res Sports Med. 2019;27:72–87. doi: 10.1080/15438627.2018.1492399. [DOI] [PubMed] [Google Scholar]
- 69.Kluitenberg B, van Middelkoop M, Verhagen E. The impact of injury definition on injury surveillance in novice runners. J Sci Med Sport. 2016;19:470–475. doi: 10.1016/j.jsams.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 70.Clement DB, Taunton JE, Smart GW, McNicol KL. A survey of overuse running injuries. Phys Sports Med. 1981;9:47–58. doi: 10.1080/00913847.1981.11711077. [DOI] [PubMed] [Google Scholar]
- 71.Kemler E, Blokland D, Backx F, Huisstede B. Differences in injury risk and characteristics of injuries between novice and experienced runners over a 4-year period. Phys Sports Med. 2018;46:485–491. doi: 10.1080/00913847.2018.1507410. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.