Abstract
Introduction
and importance: COVID-19 has been associated with thrombotic events in a variety of organs and systems, with pulmonary embolism being the most prevalent. Splenic infarction, renal infarction, and intestinal ischemia have all been documented recently as abdominal visceral infarctions.
Case presentation
A 59 years old female patient with a history of COVID-19 disease was admitted to our hospital due to her left upper quadrant abdominal and left flank pain. She had a history of left heel color change in few days. We perform an ultrasound and it was shown vein thrombosis. So, heparin infusion was started for her. We also performed a thoraco-abdominopelvic computed tomography (CT) with intravenous and oral contrast. Total evidence suggests a splenic system infarction. A regular clinical examination for malignancy was performed on the patient and there was no evidence of cancer. Other probable reasons were ruled out. The patient was diagnosed with splenic infarction, Due to coagulopathy caused by SARS-Cov-2 infection. Treatment with heparin was continued for 5 days and she was discharged home on day 9 with oral agents. The patient was asymptomatic when she returned. The spleen had decreased in size on the follow-up CT, and there were no clinical complications.
Discussion and conclusions
Spleen artery thrombosis is a rare complication of COVID-19. In this report, we described a 59 years old female with a history of COVID-19. She was discharged home and in follow-up, there was no evidence of thrombosis anymore.
Keywords: COVID-19, Limb ischemia, Splenic infarction, Case report
Highlights
-
•
Due to COVID-19 pandemic, it is important to report any new cases.
-
•
Splenic infarction is reported as a COVID-19 complication.
-
•
Limb ischemia simultaneously with spleen infarction is very rare.
-
•
It is important to notice coagulopathy and its treatment in COVID-19 patients.
1. Background
The COVID-19 pandemic is posing a threat to global health systems. Several problems and novel clinical manifestations connected to SARS-CoV-2 infection are published every day, despite the fact that the majority of infected individuals are asymptomatic or have mild to moderate respiratory illness [1,2]. SARS-CoV-2 infection has been associated with a pro-thrombotic condition and an elevated risk of venous and arterial thromboembolism in several studies [3,4].
COVID-19 has been associated with thrombotic events in a variety of organs and systems, with pulmonary embolism being the most prevalent. Splenic infarction, renal infarction, and intestinal ischemia have all been documented recently as abdominal visceral infarctions [5]. Also, A dramatic upsurge in instances of arterial thrombosis in COVID-19 patients has been reported in recent papers, configuring acute limb ischemia and posing a surgical urgency [6,7].
Splenic infarction is an uncommon condition that causes left-abdominal discomfort and is often caused by hypercoagulable conditions [5]. Clinical instances of COVID-19 with splenic infarction have been uncommon in the literature so far.
2. Case presentation
A 59 years old female, with a history of COVID-19 infection last month was admitted to Sina hospital, Tehran, Iran because of pain in the left upper quadrant and left flank by herself. She stated that she had also undergone a discoloration of the heel of her left lower limb three days ago, so she went to the clinic on an outpatient basis and was scheduled to undergo angiography. She also complained of nausea. She has an oral temperature of 38° centigrade. She has mild tachycardia. The respiratory rate was 25 per minute and oxygen saturation was 93%. Her blood pressure was recorded at 123/79 mmHg. In the examination she had abdominal distention and obvious tenderness in the left upper quadrant. Digital rectal examination was reported as normal fecal. Her left foot was cyanotic with mild edema. It was warm and pulses were palpable. She also had a white blood cell count of 18,500 per microliter.
She had a history of diabetes mellites, systemic hypertension, dyslipidemia and hypothyroidism. Her daily medication included Insulin, Losartan, Atorvastatin and Levothyroxine. There was no mentionable point in social and family history.
D-dimer and other coagulation parameters were normal. We perform an ultrasound to define the cause of ischemia and there was no pathologic finding. Therefore, an angiography was done that showed obstruction in the left popliteal artery. She was treated with Heparin (5000 U stat and 1000 U/h infusion) and broad-spectrum antibiotics.
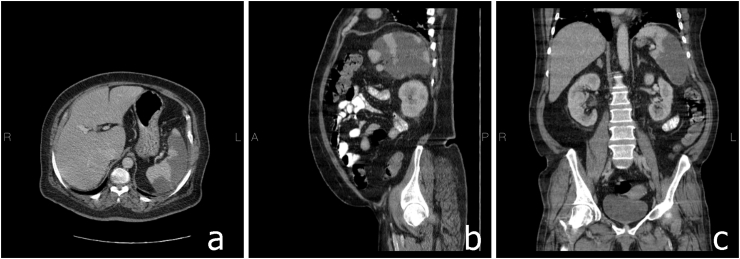
We performed a thoraco-abdominopelvic computed tomography (CT) with intravenous and oral contrast. (Fig. 1). It was reported as Multiple wedge shape hypodense areas are seen in the splenic parenchyma. A filling defect in the splenic artery is seen in the umbilicus. Total evidence suggests a splenic infarction. No free fluid was seen.
Fig. 1.
Cuts of a thoraco-abdominopelvic computed tomography (CT) with intravenous and oral contrast which suggest splenic artery thrombosis and splenic infarction (a) Axial (b) sagittal (c) coronal.
After this report hematology and Cardiology consultation was done to rule out any other reason than the COVID-19 complication. A regular clinical examination for malignancy was performed on the patient, followed by a review of the CT scans. A CT scan of the chest, abdomen, and pelvis, as well as laboratory indicators, revealed no evidence of cancer.
She had no symptoms of a gastrointestinal infection or any localized infections. Blood cultures were negative, Electrocardiogram and transthoracic echocardiography were normal, and no additional signs of endocarditis were present.
The patient was diagnosed with splenic infarction, Due to coagulopathy caused by SARS-Cov-2 infection. We chose a cautious approach, using Heparin 1000 U/h infusion for 5 days for complete anticoagulation and then change to oral Rivaroxaban, ASA and Clopidogrel.
After anticoagulation and mild analgesics, the patient's abdominal pain gradually subsided. The patient was discharged home on oral Rivaroxaban, ASA and Clopidogrel on day 9, with an outpatient follow-up in 3 months. The patient was asymptomatic when she returned. The spleen had decreased in size on the follow-up CT, and there were no clinical complications. This case report has been reported in line with the SCARE Criteria [8].
3. Discussion and Conclusions
Splenic infarction occurs when the splenic artery or its branches become occluded owing to thrombosis or embolism. Cardioembolic events, hematological and neoplastic illnesses are the most prevalent etiologies, although this event has also been linked to acute viral infections, which frequently cause states of hypercoagulability [9]. Despite the fact that thrombotic events are one of the most common symptoms of SARS-CoV-2 infection, there are few instances of splenic infarction in the literature. Because abdominal imaging tests are rarely routinely conducted and reported cases are frequently accidental findings from chest CT scans that extend to the upper abdomen, its prevalence is likely underestimated [4]. Also, the link between COVID-19 and limb arterial thrombosis has been well-documented, and it has been seen often in male patients, particularly those who are older [10].
Several researches have looked at the risk factors for COVID-19-related arterial thrombosis, including hypertension, diabetes, dyslipidemia, heart failure, heart attack history, and smoking [6,11,12].
In 184 COVID-19 patients hospitalized to the Intensive Care Unit, Klok et al. found a 31% cumulative incidence of thrombotic events. In individuals with severe COVID-19 or D-dimer levels more than 6 times the upper normal range, prophylactic dosage low-molecular-weight heparin (LMWH) has been linked to decreased mortality. In the absence of a demonstrable contraindication, society recommendations advise the administration of prophylactic anticoagulant dosages in all hospitalized COVID-19 patients [5]. However, among individuals who do not have a definite diagnosis of thromboembolism, the use of empirical full-dose anticoagulation is debatable [13].
Patients infected with COVID-19 have been observed to have abnormal coagulation parameters. Although the exact mechanism of COVID-19 coagulopathy is unclear, it is thought to be a kind of disseminated intravascular coagulation (DIC). According to recent research, infection causes a considerable number of pro-inflammatory cytokines to be released, which in certain people can result in a systemic inflammatory response syndrome defined by an increase in serum cytokines and substantial hypercoagulability [3]. Furthermore, data to date suggests that the novel coronavirus may be linked to widespread vasculopathy in many systems [2].
Multiple organs have shown thrombovascular symptoms. The most prevalent complication of COVID-19 is pulmonary thromboembolism. However, various infarctions of abdominal organs, such as splenic infarction, renal infarction, and intestinal ischemia, have lately been recorded [5]. Cases of acute abdomen in COVID-19 patients linked with vascular infarctions have risen, although being rare in the literature [13].
Anticoagulants may not help unselected individuals, according to Tang et al., however individuals with disseminated intravascular coagulation or a highly increased D-dimer may benefit from anticoagulant treatment, mostly with low molecular weight heparin. To support full-dose anticoagulation in COVID-19, further data from prospective trials is needed [14].
In another study showed acute limb ischemia is a vascular disease that is linked to embolic and thrombotic events. COVID-19 infection can lead to substantial abnormalities in coagulation processes, resulting in severe acute arterial problems such as thrombosis as the only related presentation in some individuals [15]. Since the beginning of the epidemic, investigations from Asia, Europe, and the United States have often reported venous involvement above the artery [7,16].
To our knowledge it is very rare to have limb ischemia and spleen thrombosis together. It is noticeable that venous and arterial events can occur simultaneously.
Spleen artery thrombosis is a rare complication of COVID-19. In this report, we described a 59 years old female with history of COVID-19. She presented left heel ischemia and spleen artery thrombosis as a COVID-19 complication simultaneously. Although it is controversial to use anticoagulation, we treated her with LMWH. She discharged home and in follow up, there was no evidence of thrombosis any more.
Declaration of competing interest
There is no conflict of interest.
List of abbreviations
- CT
computed tomography
Ethical approval
Due to our institution regulations, there is no need to have ethical approval for case reports.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
All authors contribute the same. All authors read and approved the final manuscript.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Registration of research studies
Name of the registry:
Unique Identifying number or registration ID:
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
Seyed Amir Miratashi Yazdi.
Address: Sina Hospital, Hassan Abad Square, Imam Khomeini Avenue, Tehran, Iran, and Po BOX: 1136746911.
Email: amiratashi@sina.tums.ac.ir.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Refrences
- 1.Karki S., Rawal S.B., Malla S., Rayamajhi J., Thapa B.B. A case report on spontaneous hemoperitoneum in COVID-19 patient. International Journal of Surgery Case Reports. 2020;75:211–213. doi: 10.1016/j.ijscr.2020.09.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mondal R., Lahiri D., Deb S., Bandyopadhyay D., Shome G., Sarkar S. COVID-19: are we dealing with a multisystem vasculopathy in disguise of a viral infection? J. Thromb. Thrombolysis. 2020;50(3):567–579. doi: 10.1007/s11239-020-02210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maiese A., Passaro G., Matteis A.D., Fazio V., Raffaele L.R., Paolo M.D. Thromboinflammatory response in SARS-CoV-2 sepsis. Med. Leg. J. 2020;88(2):78–80. doi: 10.1177/0025817220926915. [DOI] [PubMed] [Google Scholar]
- 4.Pessoa M.S.L., Lima C.F.C., Pimentel A.C.F., Costa J.C.G. Multisystemic infarctions in COVID-19: focus on the spleen. European Journal of Case Reports in Internal Medicine. 2020;7(7) doi: 10.12890/2020_001747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qasim Agha O., Berryman R. 2020. Acute Splenic Artery Thrombosis and Infarction Associated with COVID-19 Disease. Case Reports in Critical Care; p. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bellosta R., Luzzani L., Natalini G., Pegorer M.A., Attisani L., Cossu L.G. Acute limb ischemia in patients with COVID-19 pneumonia. J. Vasc. Surg. 2020;72(6):1864–1872. doi: 10.1016/j.jvs.2020.04.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Etkin Y., Conway A.M., Silpe J., Qato K., Carroccio A., Manvar-Singh P. Acute arterial thromboembolism in patients with COVID-19 in the New York City area. Ann. Vasc. Surg. 2021;70:290–294. doi: 10.1016/j.avsg.2020.08.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 9.Kranidiotis G., Efstratiadis E., Kapsalakis G., Loizos G., Bilis A., Melidonis A. Splenic infarcts as a rare manifestation of parvovirus B19 infection. IDCases. 2016;4:62–64. doi: 10.1016/j.idcr.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Organization W.H. vol. 82. 2020. (Coronavirus Disease 2019 (COVID-19): Situation Report). [Google Scholar]
- 11.Kashi M., Jacquin A., Dakhil B., Zaimi R., Mahé E., Tella E. Severe arterial thrombosis associated with Covid-19 infection. Thromb. Res. 2020;192:75. doi: 10.1016/j.thromres.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Carranza M., Salazar D.-E., Troya J., Alcázar R., Peña C., Aragón E. Aortic thrombus in patients with severe COVID-19: review of three cases. J. Thromb. Thrombolysis. 2021;51(1):237–242. doi: 10.1007/s11239-020-02219-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramanathan M., Chueng T., Fernandez E., Gonzales-Zamora J. Concomitant renal and splenic infarction as a complication of COVID-19: a case report and literature review. Inf. Med. 2020;28(4):611–615. [PubMed] [Google Scholar]
- 14.Tang N., Bai H., Chen X., Gong J., Li D., Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemostasis. 2020;18(5):1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sánchez J.B., Cuipal Alcalde J.D., Ramos Isidro R., Luna C.Z., Cubas W.S., Coaguila Charres A. Acute limb ischemia in a Peruvian cohort infected by COVID-19. Ann. Vasc. Surg. 2021;72:196–204. doi: 10.1016/j.avsg.2020.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Connors J.M., Levy J.H. COVID-19 and its implications for thrombosis and anticoagulation. Blood. The Journal of the American Society of Hematology. 2020;135(23):2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]