Abstract
The association between matrix metalloproteinases (MMPs), tissue inhibitor of metalloproteinases (TIMPs) and obesity as well as obesity-related disease including metabolic syndrome is not fully explored. Our aims are that: (i) to evaluate the plasma levels of MMP-1, MMP-2, MMP-3, MMP-9, TIMP-1, TIMP-2 and their ratios in non-obese people, overweight and obese people with or without metabolic syndrome, (ii) to investigate correlations between MMPs or TIMPs levels and several anthropometric parameters, blood pressure, endothelial function. Anthropometric and biochemical parameters were determined in 479 randomly selected participants, subdividing according to body mass index (BMI) and metabolic syndrome status. Plasma MMPs and TIMPs levels were measured. The assessment of endothelial function was characterized in people with obesity, overweight and non-obese, using laser Doppler Flowmetry. Obese people have elevated MMP-1, MMP-2, TIMP-1, TIMP-2 levels and decreased MMP-3/TIMP-1 and MMP-9/TIMP-1 ratios compared with non-obese people. MMP-1 levels and MMP-1/TIMP-1 ratio were positively correlated with BMI and waist circumference (WC) while MMP-2 levels were negatively correlated with BMI and WC values in obese people. MMP-3 levels and MMP-3/TIMP-1 ratio were positively correlated with systolic blood pressure (SBP) or diastolic blood pressure (DBP) in obese and metabolic syndrome people. Additionally, MMP-9 levels and MMP-9/TIMP-1 ratio were negatively correlated with endothelium-dependent response in obese and metabolic syndrome people. MMP-1, MMP-2, TIMP-1, TIMP-2 levels were increased in obese subjects. Significant correlations between anthropometric parameters and MMP-1 as well as MMP-1/TIMP-1 ratio supported these results. MMP-3 and -9 levels as well as their ratios with TIMP-1 were associated with blood pressure and endothelial-dependent response, respectively. In conclusion, our results demonstrated that MMP-1, MMP-3 and MMP-9 levels were correlated with several obesity-related parameters including BMI, WC, blood pressure and endothelial-dependent response. Our findings will hopefully provide new aspects for the use of MMPs and TIMPs as clinical biomarkers in obesity-related cardiovascular diseases such as metabolic syndrome and hypertension. The lack of measure of MMPs activity in plasma and relevant organs/tissues in obesity and metabolic syndrome is considered as a limitation in this report.
Subject terms: Biochemistry, Biomarkers, Cardiology, Diseases, Endocrinology, Medical research, Pathogenesis, Risk factors
Introduction
Obesity is a worldwide health problem with increasing incidence. This chronic metabolic disease is consistently and strongly associated with a higher risk of cardiovascular disease and mortality1. Furthermore, obesity leads to the risk-clustering status known as metabolic syndrome, which is characterized by the presence of any three of five factors including high waist circumference (WC), high plasma triglycerides (TG), low plasma high-density lipoprotein cholesterol (HDL-C), high fasting plasma glucose (FG), and high blood pressure2.
Matrix metalloproteinases (MMPs) are involved in physiological and pathological complications of obesity or metabolic syndrome through the degradation and remodeling of the extracellular matrix (ECM) molecules3–5. MMP family members are categorized into soluble collagenases (MMP-1, -8, -13), gelatinases (MMP-2, -9), stromelysins (MMP-3, -10, -11), matrilysins (MMP-7, -26), membrane-type MMPs (MT-MMPs) (MMP-14, -15, -16, -17, -24, -25) and elastase (MMP-12)3.
MMPs activity is regulated by their endogenous inhibitors tissue inhibitor of metalloproteinases (TIMPs): TIMP-1 inhibits MMP-1, MMP-3, MMP-7 and MMP-9, TIMP-2 inhibits especially MMP-2, TIMP-3 can inhibit MMP-2 and MMP-9, while TIMP-4 inhibits MT-1 MMP and MMP-2 activity6. Among these TIMPs, especially TIMP-1 and TIMP-2 gain importance in obesity-related cardiovascular diseases7. The balance between MMPs and TIMPs is a critical determinant of ECM integrity and function, and alterations in MMPs/TIMPs mediated proteolysis may contribute to many pathological states. Since TIMPs levels directly affect MMPs activity, changes of TIMPs levels play an important role in pathological conditions.
Several studies demonstrated altered expression of MMPs and TIMPs in obese rodent models8–11. The potential contribution of MMPs and TIMPs was also detected in mice with genetic deletion of MMPs or TIMPs12,13. In addition, mice treated with a global MMP inhibitor reduced adipose tissue weight and the total number of adipocytes when exposed to a high-fat diet14. The role of MMPs and TIMPs were also investigated in obesity-associated cardiovascular diseases including hypertension and metabolic syndrome6,15–17. Even though, several animal models demonstrated that there is a dysregulation of MMPs and TIMPs in these diseases, correlation between MMPs or TIMPs and blood pressure, several anthropometric parameters including body mass index, waist circumference is not fully examined in humans.
As well as altered MMPs, TIMPs levels, endothelial dysfunction has also been observed in obesity and metabolic syndrome18,19. Several in vivo approaches including assessment of forearm blood flow have been developed to measure the function of the endothelium in humans19. However, no previous work has studied the relationship between MMPs or TIMPs levels and endothelial dysfunction. Understanding this relationship could provide early treatment and prevention of more serious cardiovascular diseases such as atherosclerosis.
The aim of this study is to investigate the plasma levels of MMP-1, MMP-2, MMP-3, MMP-9, TIMP-1, TIMP-2 and their ratios in a large variety of study groups including overweight people and obese people with or without metabolic syndrome and non-obese healthy people with total of 479 participants. Furthermore, correlations between MMPs or TIMPs levels and endothelial function, several anthropometric parameters, blood pressure were performed.
Materials and methods
Study subjects
In the present study, we recruited 479 randomly selected Tunisian subjects, included 227 healthy lean (non-obese) people with BMI between 18.5 and 25 kg/m2, 67 overweight people with 25 ≤ BMI < 30 kg/m2, and 185 obese people with BMI ≥ 30 kg/m2. We followed the diagnostic criteria for metabolic syndrome defined according to the National Cholesterol Education Program's-Third Adult Treatment Panel (NCEP-ATPIII) which included the following factors: (1) increased WC (> 102 cm in men and > 88 cm in women); (2) elevated TG (≥ 150 mg/dL); (3) reduced HDL-C (< 1.03 mmol/L in men and < 1.29 mmol/L in women); (4) elevated blood pressure (≥ 130 mm Hg for SBP or ≥ 85 mm Hg for DBP); (5) elevated fasting glucose (FG) ≥ 6.1 mmol/L20. The presence of defined abnormalities in presence of three or more of the measures constitutes a diagnosis of the metabolic syndrome.
Depending on metabolic syndrome status, people with obesity were divided into two groups: 87 metabolic syndrome obese (MetsO) and 77 metabolic healthy obese (MHO). The study was approved by Farhat Hached Hospital Ethics Committee for research on humans in Tunisia. All research was performed in accordance with relevant guidelines/regulations, and informed consent was obtained from all participants and/or their legal guardians. This study has been performed in accordance with the Declaration of Helsinki. Information on each participant’s lifestyle and health status was obtained through an interview, including questions regarding smoking history, prescription medicines for diseases such as dyslipidemia, hypertension or cardiovascular diseases. Subjects with a history of cardiovascular, liver, renal, or thyroid disease, smoking habit, malignancy, diseases responsible for microvasculopathy and participants using medications that might affect lipid and glucose metabolism or alter the endothelial or smooth muscle dependent responses were excluded from the study. Other exclusion criteria were women in the menstrual cycle and pregnant women.
Anthropometric measurements, biochemical analyses, and microvascular reactivity assessment
Participants were first examined anthropometrically. Height (m) and weight (kg) were taken with participants dressed in lightweight clothing without shoes and BMI was calculated (kg/m2). The WC was measured at the midway point between the lower rib margin and the crest of the ileum in a horizontal plane at standing position (cm), and the hip circumference (HC) was measured by placing a tape measure around the patient's hips at the level of the prominences over the greater trochanters of both femurs (cm); after, we calculated the waist-to-hip ratio (WHR) and the waist-to-height ratio (WHtR). Blood pressure was also measured using a mercury sphygmomanometer with an appropriately sized cuff and stethoscope after the subject has been seated for 5 min.
Blood samples were collected from subjects in tubes after 12 h overnight fast, the blood was maintained at 4 °C then centrifuged (4000g for 10 min). Plasma was distributed in aliquots and stored at − 80 °C until the batched measurements of parameters. FG was measured by the glucose oxidase method (Biomaghreb, Tunisia). Total cholesterol (TC) and TG were determined by the cholesterol oxidase and the glycerol oxidase methods (Elitech Diagnostic, France). HDL-C was measured by the immune-inhibition method (Elitech Diagnostic, France) and low-density lipoprotein cholesterol (LDL-C) concentrations were calculated with the Friedwald formula21. High-sensitivity C-reactive protein (hsCRP) concentrations were also measured. All biochemical parameters were determined on an automated Synchron CX7 Clinical System (Beckman, Fullerton, CA).
Microvascular reactivity and endothelial function assessments
Microvascular reactivity parameters were determined as previously described22. Endothelial function was explored by assessing the forearm microvascular cutaneous vasoreactivity using laser Doppler flowmeter coupled with iontophoresis (Periflux System 5000, Perimed, Jarfalla Sweden). Endothelium-dependent vasodilation was evaluated by stimulation with 2% acetylcholine chloride (ACh) (Sigma Aldrich, Switzerland). Briefly, cutaneous blood flow was recorded at rest for 2 min and during the functional exploration. Three doses of ACh were delivered using an anodal current (0.1 mA for 10 s) at 2-min intervals. Data were expressed as cutaneous vascular conductance (CVC), which represents the ratio between the cutaneous blood flow and mean arterial pressure values, to take into account variations in blood pressure between subjects. The endothelium-dependent response was calculated as the difference between the peak CVC upon ACh stimulation (i.e., the CVC after the third dose of ACh) and the baseline CVC (ΔACh-CVC).
BioPlex luminex and enzyme-linked immunosorbent assays
Firstly, as a preliminary study 9 MMPs (-1, -2, -3, -7, -8, -9, -10, -12, -13), TIMP-1, and TIMP-2 plasma levels were measured in non-obese and people with overweight and obesity by BioPlex Luminex (BioRad; 2 lasers, 3 colors, High-Throughput System for multiplex cytometric bead arrays). From the preliminary results given by this technique we have chosen to focus on MMP (-1, -2, -3 and -9) and TIMP-1 and TIMP-2. Then, MMP (-1, -2, -3 and -9) and TIMP-1 and TIMP-2 levels were determined by Enzyme-Linked Immunosorbent Assays (ELISA) using commercially available kits, human MMP-1 (DYS901), human MMP-2 (DY902), human MMP-3 (DY513), human MMP-9 (DY911), human TIMP-1 (DY970) and human TIMP-2 (DY971) (DUOSET®ELISA, R&D systems), respectively, according to the manufacturer's instructions.
Statistical analysis
SPSS® 20.0 software (SPSS Inc., Chicago, IL, USA) and Graph Pad 7.0 software (La Jolla, CA, USA) were used for statistical analysis. The comparison of non-parametric quantitative variables was performed by the Mann Whitney test or the Kruskal–Wallis test. P values were adjusted for age, gender, systolic blood pressure, LDL-C, TC and FG (Table 2). The correlation study was carried out using the Spearman correlation coefficient. The β coefficient was determined by linear regression and binary logistic regression. A p-value less than 0.05 is considered significant.
Table 2.
MMPs and TIMPs levels of the study population.
| Parameters | Non-obese (18.5 ≤ BMI < 25) | Overweight (25 ≤ BMI < 30) | Obese (BMI ≥ 30) | MHO | MetsO |
|---|---|---|---|---|---|
| MMPs | |||||
| MMP-1 (ng/ml) | 1.18 (0.04–9.97) | 1.28 (0.08–5.8) | 2.5 (0.08–22.5)* | 2.7 (0.11–14.17) | 1.84 (0.08–22.15) |
| MMP-2 (ng/ml) | 100.65 (47.56–211.43) | 117.67 (73.65–231.75)*** | 113.26 (43.98–260)* | 116.77 (43.98–260) | 110.46 (56.12–206) |
| MMP-3 (ng/ml) | 6.22 (1.28–29.66) | 9.42 (2.14–31.32) | 7.46 (1.4–33) | 7.95 (1.84–32.98) | 7.91 (1.4–23.6) |
| MMP-9 (ng/ml) | 63.02 (16.38–231.77) | 54.19 (19.76–211.34) | 66.28 (12.34–215.34) | 67.2 (15.21–215.34) | 65.72 (13.65–205.14) |
| TIMPs | |||||
| TIMP-1 (ng/ml) | 141.05 (53.34–446.21) | 173.28 (36.06–292.1) | 193.32 (53.6–487.2)***# # | 194.03 (53.62.76–413) | 184.94 (70.54–487.22) |
| TIMP-2 (ng/ml) | 90.26 (48.75–158.76) | 103.72 (77.78–190.76)** | 96.12 (65.93–268)** | 97.99 (72.44–268) | 94.47 (65.93–139.16) § |
| MMPs/TIMPs | |||||
| MMP-1/TIMP-1 | 0.007 (0.003–0.01) | 0.01 (0.005–0.01) | 0.012 (0.006–0.02) | 0.01 (0.007–0.02) | 0.01 (0.005–0.02) |
| MMP-2/TIMP-2 | 1.11 (0.56–2.5) | 1.11 (0.57–1.83) | 1.15 (0.42–1.95) | 1.12 (0.42–1.81) | 1.19 (0.54–1.95) |
| MMP-3/TIMP-1 | 0.05 (0.02–0.09) | 0.04 (0.02–0.09) | 0.03 (0.02–0.07)*** | 0.04 (0.02–0.08) | 0.04 (0.02–0.07) |
| MMP-9/TIMP-1 | 0.42 (0.09–8.61) | 0.38 (0.03–2.09) | 0.35 (0.05–1.69)* | 0.34 (0.05–1.30) | 0.39 (0.06–1.69) |
Data are presented as median (interquartile range). Statistical differences were obtained with adjusted values for age, gender, systolic blood pressure, LDL-C, TC and FG. *P < 0.05 vs non-obese. **P < 0.01 vs non-obese. ***P < 0.001 vs non-obese. #P < 0.05 vs overweight. ##P < 0.01 vs overweight. §P < 0.05 MetsO vs MHO.
MetsO Metabolic syndrome obese, MHO Metabolic healthy obese, MMP matrix metalloproteinase, TIMP tissue inhibitors of MMP.
Ethical approval and informed consent
This study was approved by the local Ethical Committee of Farhat Hached Hospital (Sousse, Tunisia).
Results
Characteristics of the study population
The demographic and clinical characteristics of the participants are summarized in Table 1. Non-obese, overweight and obese groups had comparable gender distribution. However, obese and overweight people were older than non-obese people (P < 0.001 and 0.004, respectively; Table 1). In order to avoid the contribution of age, our results were adjusted for age. As expected, BMI and central obesity markers (WC, WHR, and WHtR) were higher in both overweight and obese people when compared to non-obese people (P < 0.001 for all; Table 1). Moreover, BMI, WC, WHR, and WHtR were significantly higher in people with obesity when compared to overweight people (Table 1). DBP was significantly increased in both overweight and obese people when compared to non-obese people (P < 0.001 for both groups, Table 1). Besides, SBP was significantly increased in obese when compared to non-obese people (P < 0.001, Table 1).
Table 1.
Anthropometric, biochemical parameters and microvascular function of the study subjects according to obesity status.
| Parameters | Non-obese (n = 227) (18.5 ≤ BMI < 25) |
Overweight (n = 67) (25 ≤ BMI < 30) |
Obese (n = 185) (BMI ≥ 30) |
Pϛ value | MHO (n = 87) | MetsO (n = 77) | Pϛϛ value |
|---|---|---|---|---|---|---|---|
| Demographic parameters | |||||||
| Gender (males/females) | 101/126 | 34/33 | 92/93 | 0.42 | 37/40 | 48/39 | 0.23 |
| Age (years) | 34.81 ± 0.73 | 39.52 ± 1.53** | 41.79 ± 0.81*** | 0.000 | 40.38 ± 1.30 | 43.10 ± 1.13 | 0.000 |
| Anthropometric parameters | |||||||
| BMI (kg/m2) | 22.87 ± 0.13 | 28.12 ± 0.12*** | 37.69 ± 0.50***### | 0.000 | 35.93 ± 0.70 | 38.52 ± 0.78§§ | 0.000 |
| WC (cm) | 79.93 ± 0.71 | 97.64 ± 1.05*** | 115.63 ± 1.06***### | 0.000 | 110.64 ± 1.51 | 118.98 ± 1.48§§§ | 0.000 |
| HC (cm) | 95.07 ± 0.72 | 107.64 ± 0.91*** | 123.31 ± 1.12***### | 0.000 | 120.79 ± 1.68 | 123.88 ± 1.63 | 0.000 |
| WHR | 0.84 ± 0.08 | 0.91 ± 0.01*** | 0.93 ± 0.006***### | 0.000 | 0.91 ± 0.01 | 0.96 ± 0.008§§ | 0.000 |
| WHtR | 0.47 ± 0.004 | 0.57 ± 0.006*** | 0.70 ± 0.006***### | 0.000 | 0.67 ± 0.01 | 0.72 ± 0.009§§ | 0.000 |
| SBP (mmHg) | 116.2 ± 0.6 | 122.8 ± 3.0 | 126.4 ± 0.13*** | 0.000 | 119.1 ± 1.6 | 133.0 ± 1.8 §§§ | 0.000 |
| DBP (mmHg) | 76.7 ± 0.4 | 81.3 ± 1.5*** | 81.8 ± 0.07*** | 0.000 | 77.5 ± 1.0 | 85.3 ± 1.0 §§§ | 0.000 |
| Biochemical parameters | |||||||
| hs-CRP (mg/dl) | 1.28 ± 0.18 | 6.36 ± 1.01*** | 5.79 ± 0.42*** | 0.000 | 5.61 ± 0.6 | 5.90 ± 0.64 | 0.000 |
| FG (mmol/l) | 5.18 ± 0.11 | 5.32 ± 0.17 | 5.91 ± 0.12***### | 0.000 | 5.30 ± 0.12 | 6.46 ± 0.19§§§ | 0.000 |
| TG (mmol/l) | 1.14 ± 0.05 | 1.55 ± 0.16*** | 1.62 ± 0.06*** | 0.000 | 1.57 ± 0.08 | 1.51 ± 0.11 | 0.000 |
| TC (mmol/l) | 4.45 ± 0.08 | 4.73 ± 0.13 | 4.98 ± 0.07***# | 0.000 | 4.92 ± 0.10 | 5.15 ± 0.11 | 0.000 |
| HDL-C (mmol/l) | 1.26 ± 0.03 | 1.21 ± 0.04 | 1.11 ± 0.02*** | 0.000 | 1.26 ± 0.04 | 1.01 ± 0.02§§§ | 0.000 |
| LDL-C (mmol/l) | 2.67 ± 0.07 | 2.83 ± 0.11 | 3.16 ± 0.07***# | 0.000 | 3.10 ± 0.11 | 3.25 ± 0.11 | 0.000 |
| LDL-C/HDL-Cratio | 2.37 ± 0.07 | 2.54 ± 0.15 | 3.05 ± 0.11***# | 0.000 | 2.68 ± 0.15 | 3.37 ± 0.17§§ | 0.000 |
| TC/HDL-Cratio | 3.76 ± 0.10 | 4.11 ± 0.17 | 4.63 ± 0.13***# | 0.000 | 4.03 ± 0.16 | 5.17 ± 0.20§§§ | 0.000 |
| Microvascular function |
Non-obese (n = 35) (18.5 ≤ BMI < 25) |
Overweight (n = 13) (25 ≤ BMI < 30) |
Obese (n = 38) (BMI ≥ 30) |
Pϛ value | MHO (n = 17) | MetsO (n = 19) | Pϛϛ value |
| Basal CVC (PU/mm Hg) | 0.09 ± 0.01 | 0.08 ± 0.02 | 0.056 ± 0.003** | 0.01 | 0.06 ± 0.005 | 0.05 ± 0.004§ | 0.01 |
| Peak ACh-CVC (PU/ mm Hg) | 0.48 ± 0.04 | 0.43 ± 0.08 | 0.3 ± 0.03** | 0.02 | 0.37 ± 0.05 | 0.27 ± 0.04§ | 0.03 |
Data are presented as mean ± SEM. Pϛ indicates statistical differences intergroups (non-obese, overweight and obese subjects). Pϛϛ indicates statistical differences intergroups (non-obese, MHO and MetsO). *P < 0.05 vs non-obese. **P < 0.01 vs non-obese. ***P < 0.001 vs non-obese. #P < 0.05 vs overweight. ###P < 0.001 vs overweight. §P < 0.05 vs MHO. §§P < 0.01 vs MHO. §§§P < 0.001 vs MHO.
Ach acetylcholine, ApoA1 apolipoprotein A1, ApoB apolipoprotein B, BMI body mass index, CVC Cutaneous vascular conductance, DBP diastolic blood pressure, FG fasting glucose, HC hip circumference, HDL-C high density lipoprotein cholesterol, hsCRP high sensitivity C reactive protein, LDL-C low density lipoprotein cholesterol, MetsO Metabolic syndrome obese, MHO Metabolic healthy obese, SBP systolic blood pressure, TC total cholesterol, TG triglycerides, WC waist circumference, WHR waist to hip ratio, WHtR waist to height ratio. The sum does not add up to the total (MetsO/MHO) because of a few missing criteria in obese people.
Additionally, hs-CRP levels were significantly increased among obese and overweight people when compared to non-obese people (P < 0.001 for both groups, Table 1). FG levels were significantly increased in people with obesity when compared to non-obese and overweight people (P < 0.001, Table 1). As shown in Table 1, TG was significantly increased in both obese and overweight people when compared to non-obese people (P < 0.001 and < 0.001, respectively). The other lipid parameters (TC, LDL-C, LDL-C/HDL-C, and TC/HDL-C) were significantly increased in people with obesity when compared to overweight people (P < 0.05, for all; Table 1) and non-obese people (P < 0.001, for all; Table 1). On the contrary, HDL-C was significantly decreased in people with obesity when compared to non-obese people (P < 0.001; Table 1).
In our study, we have also categorized obese people according to metabolic status (MHO/MetsO). As shown in Table 1, non-obese, MHO, and MetsO groups had comparable gender distribution. No significant difference was found in the age when the MetsO and the MHO group were compared (P > 0.05, Table 1). Higher BMI values were found among MetsO when compared to MHO (P = 0.006, Table 1). Moreover, central obesity markers (WC, WHR, and WHtR) were significantly higher among MetsO when compared to MHO (P < 0.001, = 0.002 and 0.003 respectively, Table 1). SBP, DBP, and FG levels were significantly higher in MetsO than in MHO (P < 0.001 for all; Table 1). Lipid parameters TC/HDL-C and LDL-C/HDL-C were also significantly increased among MetsO when compared to MHO (P < 0.001 and 0.003, respectively; Table 1), while HDL-C was significantly decreased among MetsO when compared to MHO (P < 0.001, Table 1).
The association of microvascular endothelial function with obesity status was also performed. Basal CVC as well as peak ACh-CVC values were decreased in people with obesity when compared to non-obese people (p = 0.003 and = 0.005, respectively; Table 1). When subjects were categorized as metabolic syndrome status, we found a significant decrease in both basal CVC and peak ACh-CVC among MetsO group when compared to non-obese people (p = 0.012 and = 0.015, respectively; Table 1).
Plasma levels of MMPs and TIMPs among study subjects
As shown in Table 2, plasma MMP-1 levels were significantly higher in the obese group than non-obese group (P = 0.015). Additionally, the levels of MMP-2 were markedly higher in the overweight and obese group than non-obese group (P < 0.001; P = 0.045, respectively, Table 2). In contrast, no significant difference was found in MMP-3 and MMP-9 levels when compared to the non-obese, overweight and obese groups (P = 0.15; P = 0.13, respectively, Table 2). Significantly increased levels of TIMP-1 were found in people with obesity when compared to non-obese people (P < 0.001, Table 2). In addition, a significant difference was found in TIMP-1 levels in obese people when compared to people with overweight (P = 0.008, Table 2). Similarly, the plasma concentration of TIMP-2 was significantly higher in the obese and overweight group than non-obese group (P = 0.008 and P = 0.006, respectively; Table 2).
As shown in Table 2, no significant difference was found in MMP-1/TIMP-1 and MMP-2/TIMP-2 ratios when compared to the non-obese, overweight and obese groups (P > 0.05, for all; Table 2). In contrast, we had revealed a significant difference in MMP-9/TIMP-1 and MMP-3/TIMP-1 ratios when comparing the obese group with non-obese people (P = 0.04, P < 0.001, respectively; Table 2).
Subdividing the obese group into MetsO and MHO, a significant difference was found in TIMP-2 levels when comparing MetsO to MHO (P = 0.02, Table 2).
Binary logistic regression setting obesity and metabolic syndrome status as dependent variables and MMP (-1, -2, -3 and -9), TIMP (-1 and -2) and MMP/TIMP ratios (MMP-1/TIMP-1, MMP-2/TIMP-2, MMP-3/TIMP-1 and MMP-9/TIMP-1) as independent variables revealed a significant association of MMP-2, TIMP (-1 and -2) and MMP-2/TIMP-2 ratio when obesity status was considered as a dependent variable (Supplementary Table 1). However, no significant association was found when setting metabolic syndrome status as dependent variable (Supplementary Table 1). Bêta coefficient (β) for valences indicates the direction of the relationship between the predicted variable and the independent variables. In this regard, the probabilities of MMP-2, TIMP (-1 and -2) levels and MMP-2/TIMP-2 ratio have been increased in obese subjects (Supplementary Table 1).
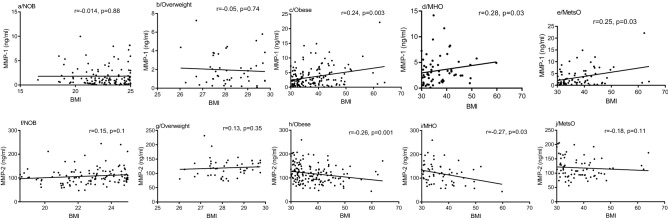
Spearman correlation of MMP-1 and MMP-2 plasma levels with anthropometric parameters (BMI and WC)
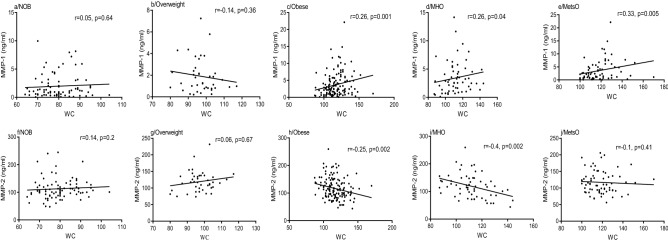
MMP-1 levels and MMP-1/TIMP-1 ratio were positively correlated with BMI in obese people (r = 0.24, p = 0.003, Fig. 1c; r = 0.19, p = 0.016, Supplementary Table 2), however, no significant correlation was found among non-obese and overweight people (r = 0.014, p = 0.88; r = 0.05, p = 0.74, Fig. 1a and 1b). Subdividing people with obesity into MetsO and MHO, a positive correlation was also detected between MMP-1 and BMI values in both MetsO (r = 0.25, p = 0.03, Fig. 1e) and MHO (r = 0.28, p = 0.03, Fig. 1d). In addition, we found a positive correlation between MMP-1/TIMP-1 ratio and BMI in MetsO (r = 0.26, p = 0.023, Supplementary Table 2). Similarly, MMP-1 levels and MMP-1/TIMP-1 ratio were positively correlated with central adiposity (WC) in obese (r = 0.26, p = 0.001, Fig. 2c r = 0.18, p = 0.03, Supplementary Table 2), however, no significant correlation was noted among non-obese and overweight people (r = 0.05, p = 0.64; r = 0.14, p = 0.36, Fig. 2a,b, respectively). A positive correlation was also detected between MMP-1 levels and WC values in both MetsO (r = 0.33, p = 0.005, Fig. 2e) and MHO (r = 0.26, p = 0.04, Fig. 2d).
Figure 1.
Spearman Rank correlation between BMI and MMP-1 and MMP-2 plasma levels respectively, according to obesity status. Regression coefficient (r) and statistical significance (p) are reported for each test. p-value < 0.05 is significant. BMI Body Mass Index, NOB non-obese, MHO metabolic healthy obese, MetsO metabolic syndrome obese.
Figure 2.
Spearman Rank correlation between WC and MMP-1 and MMP-2 plasma levels respectively, according to obesity status. Regression coefficient (r) and statistical significance (p) are reported for each test. p-value < 0.05 is significant. NOB non-obese, MHO metabolic healthy obese, MetsO metabolic syndrome obese, WC waist circumference.
Conversely, MMP-2 levels were negatively correlated with BMI values among obese (r = − 0.26, p = 0.001, Fig. 1h) and MHO group (r = − 0.27, p = 0.03, Fig. 1i). However, no significant correlation was found among MetsO (r = − 0.18, p = 0.11; Fig. 1j), overweight (r = 0.13, p = 0.35, Fig. 1g) and non-obese people (r = 0.15, p = 0.1, Fig. 1f). MMP-2 levels were negatively correlated with WC values among obese (r = − 0.25, p = 0.002, Fig. 2h) and MHO (r = − 0.4, p = 0.002, Fig. 2i), however, no correlation was found among MetsO (r = − 0.10, p = 0,41, Fig. 2j), overweight (r = 0.06, p = 0.67, Fig. 2g) and non-obese people (r = 0.14, p = 0.2, Fig. 2f). MMP-3, MMP-9, TIMP-1 and TIMP-2 levels were not correlated with BMI or WC (Supplementary Table 2).
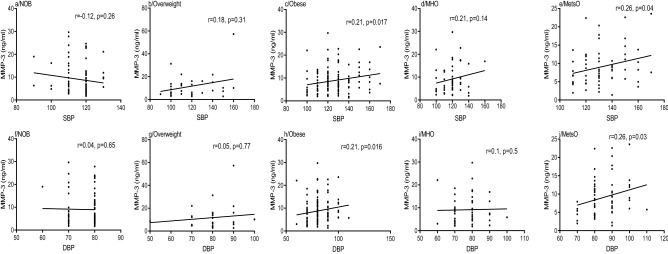
Spearman correlation between MMP-3 plasma levels, SBP and DBP
As shown in Fig. 3, MMP-3 levels were positively correlated with SBP in people with obesity (r = 0.21, p = 0.017, Fig. 3c), however, no significant correlation was noted among non-obese and overweight people (r = 0.12, p = 0.26; r = 0.18, p = 0.31, Fig. 3a,b, respectively).
Figure 3.
Spearman Rank correlation between MMP-3 plasma levels, SBP and DBP respectively, according to obesity status. Regression coefficient (r) and statistical significance (p) are reported for each test. p-value < 0.05 is significant. DBP diastolic blood pressure, SBP systolic blood pressure, NOB non-obese, MHO metabolic healthy obese, MetsO metabolic syndrome obese.
Additionally, a positive correlation was found between MMP-3 levels and SBP in MetsO (r = 0.26, p = 0.04, Fig. 3e), however, no correlation was found among MHO (r = 0.21, p = 0.14, Fig. 3d). MMP-3 levels showed no correlation with DBP among MHO (r = 0.1, p = 0.5, Fig. 3i), overweight (r = 0.05, p = 0.77, Fig. 3g) and non-obese people (r = 0.04, p = 0.65, Fig. 3f). While, like MMP-3/TIMP-1 ratio (r = 0.29, p = 0.01, Supplementary Table 2), MMP-3 levels were positively correlated with DBP in MetsO (r = 0.26, p = 0.03, Fig. 3j) and obese people (r = 0.21, p = 0.016, Fig. 3h). In addition, TIMP-1 levels were negatively correlated with DBP among obese group (r = − 0.2, p = 0.027; Supplementary Table 2), however, no correlation was found among other groups (Supplementary Table 2).
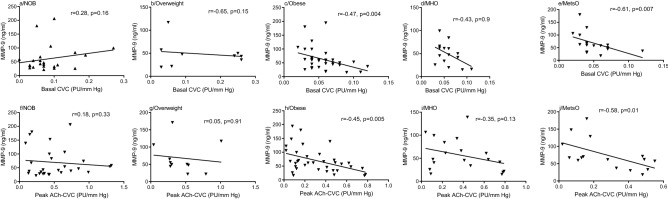
Spearman correlation between MMPs or TIMPs plasma levels and microvascular reactivity parameters (Basal CVC, Peak Ach CVC)
As shown in Fig. 4, MMP-9 levels were negatively correlated with basal CVC in people with obesity (r = − 0.47, p = 0.004, Fig. 4c), however, no correlation was found among non-obese and overweight people (r = 0.28, p = 0.16; r = 0.65, p = 0.15, Fig. 4a,b, respectively). Additionally, a negative correlation was found between MMP-9 levels and basal CVC in MetsO (r = − 0.61, p = 0.007, Fig. 4e), however, no correlation was found among MHO (r = − 0.43, p = 0.9, Fig. 4d). MMP-9 levels and MMP-9/TIMP-1 ratio showed no correlation with peak Ach-CVC among MHO (r = − 0.35, p = 0.13, Fig. 4i; r = − 0.24, p = 0.31, Supplementary Table 2), overweight (r = 0.05, p = 0.91, Fig. 4g; r = 0.08, p = 0.84, Supplementary Table 2) and non-obese people (r = 0.18, p = 0.33, Fig. 4f; r = 0.17, p = 0.34, Supplementary Table 2). While MMP-9 levels and MMP-9/TIMP-1 ratio were negatively correlated with peak Ach-CVC in obese (r = − 0.45, p = 0.005, Fig. 4h; r = − 0.46, p = 0.004, Supplementary Table 2) and MetsO subjects (r = − 0.58, p = 0.01, Fig. 4j; r = − 0.53, p = 0.03, Supplementary Table 2). In addition, MMP-2 levels and MMP-2/TIMP-2 ratio were positively correlated with Peak Ach-CVC among MetsO group (r = 0.55, p = 0.02; r = 0.6, p = 0.01; Supplementary Table 2), however, no correlation was found among other groups (Supplementary Table 2).
Figure 4.
Spearman Rank correlation between MMP-9 plasma levels and microvascular parameters according to obesity status. Regression coefficient (r) and statistical significance (p) are reported for each test. p-value < 0.05 is significant. Ach acetylcholine, CVC cutaneous vascular conductance, NOB non-obese, MHO metabolic healthy obese, MetsO metabolic syndrome obese.
Linear regression analysis also identified that the MMP-9/TIMP-1 ratio is an independent variable affecting Peak-Ach-CVC in obese, MHO and MetsO subjects (Supplementary Table 3). Additionally, MMP-1, MMP-9, and MMP-1/TIMP-1 ratio were considered as independent variables affecting Peak Ach-CVC in MetsO subjects (Supplementary Table 3).
The Bêta coefficient (β) for valences indicates the direction of the relationship between the predicted variable and the independent variables. In this regard, the probabilities of impaired endothelial function in obese subjects increase when the parameters MMP-9, MMP-1, MMP-1/TIMP-1, and MMP-9/TIMP-1 ratios increase in obese or in MetsO subjects (Supplementary Table 3).
Spearman correlation between MMPs or TIMPs plasma levels and CRP
MMP-1 and TIMP-1 levels were positively correlated with CRP in obese people (r = 0.21, p = 0.045; r = 0.2, p = 0.025, Supplementary Table 2), however, no significant correlation was found among non-obese and overweight people (Supplementary Table 2).
Subdividing people with obesity into MetsO and MHO, a negative correlation was also detected between MMP-2 levels, MMP-2/TIMP-2 ratio and CRP values in MetsO (r = − 0.26, p = 0.03, r = − 0.27, p = 0.03, respectively, Supplementary Table 2). However, no significant correlation was found among MHO subjects (Supplementary Table 2).
Discussion
The main findings of the present study are that: (i) obese people have elevated MMP-1, MMP-2, TIMP-1, TIMP-2 levels and decreased MMP-3/TIMP-1, MMP-9/TIMP-1 ratios compared with non-obese people (ii) MMP-1 levels and MMP-1/TIMP-1 ratio were positively while MMP-2 levels were negatively correlated with BMI and WC values in people with obesity (iii) MMP-3 levels and MMP-3/TIMP-1 ratio were positively correlated with SBP and/or DBP in obese or metabolic syndrome people (iv) MMP-9 levels and MMP-9/TIMP-1 ratio were negatively correlated with the endothelium-dependent response in obese or metabolic syndrome people.
In the present study, we demonstrated higher circulating levels of MMP-1 in obese people as compared to non-obese people (Table 2). Since MMP-1 activity is regulated by TIMP-1, we have calculated MMP-1/TIMP-1 ratio. There was an increase of MMP-1/TIMP-1 ratio in obese people but this increase did not reach any significance (Table 2). There was no difference in MMP-1 levels and MMP-1/TIMP-1 ratio between obese people with or without metabolic syndrome (Table 2). The association of MMP-1 levels and obesity was also verified by significant positive correlations between MMP-1 levels or MMP-1/TIMP-1 ratio and BMI/WC values in people with obesity (Figs. 1c and 2c, Supplementary Table 2). It has been suggested that macrophage accumulation in adipose tissue play important role for the stimulation of MMP-1 production by preadipocytes, mediated by pro-inflammatory mediators23. Our results demonstrated that the levels of CRP, mediator of inflammation, is increased in obesity (Table 1). Inflammation observed in obesity could be stimulant of MMP-1 levels and could be involved in adipose tissue remodeling during adipose tissue expansion in obesity23. Positive correlation observed between MMP-1 and CRP levels supported this hypothesis (Supplementary Table 2). Similar results were obtained24 and discussed in our previous studies22,24. On the other hand, studies performed on relatively small numbers of participants (n = 54–102) showed that there is no difference in MMP-1 levels between obese and non-obese people25,26. It should be noted that our recent study indicated that MMP-1 levels were increased only in obese women, not in obese men24. This result suggested that sex hormones could participate in MMP-1 regulation in obesity. The contribution of MMP-1 on obesity development was also demonstrated in studies including ours showing an association between polymorphisms of the MMP-1 gene and BMI values22,27. Another study demonstrated an association of MMP-1 genotypes/ haplotypes with MMP-1 levels predominantly in non-obese subjects28. Despite the contradictory effect of MMP-1 on obesity, the majority of studies indicated increased levels of MMP-1 in obesity.
Our results exhibited that MMP-2 levels were markedly higher in obese or overweight subjects than non-obese people (Table 2). Interestingly, there is a small reduction in obese people versus overweight people even though it did not reach significance. This probably leads to a significant negative correlation between MMP-2 levels and BMI/WC values in people with obesity however this correlation was not observed in overweight or non-obese people (Fig. 1f–h and Fig. 2f–h, respectively). This result suggests that MMP-2 levels were increased in the development of obesity while in obese people MMP-2 levels were decreased gradually depending on obesity severity that could be a compensatory mechanism.
MMP-2 activity is regulated by TIMP-2. The interaction between TIMP-2 and pro-MMP-2 is also part of activation process of pro-MMP, because it allows the binding of the complex MMP-2/TIMP-2 a key step in the generation of the active form of MMP-2. At higher levels of TIMP-2, pro-MMP-2 activation is prevented29,30. Our results showed obese people with or without metabolic syndrome exhibited no difference in MMP-2 levels as well as MMP-2/TIMP-2 ratio (Table 2). Several studies demonstrated that plasma MMP-2 levels or MMP-2 gene expression in visceral adipose tissue were not modified in obese or metabolic syndrome people31–35. Furthermore, in morbidly obese women, serum MMP-2 concentration was not affected by significant weight loss after bariatric surgery36. On the other hand, some studies exhibited either increase or decrease in MMP-2 levels or activity in obese or metabolic syndrome37–42. Limitations of these studies were their small sample size which may affect the power of their analysis. Furthermore, it is possible that gender or methodological differences have affected the results. It is worth mentioning that our study included 479 participants and age, gender, systolic blood pressure, LDL-C, TC and FG adjustments have been performed.
In the present study, we demonstrated that there is no difference in circulating levels of MMP-3 between obese, overweight, and non-obese people (Table 2). Furthermore, no difference was found in obese people with and without metabolic syndrome (Table 2). In agreement with our results, there was no difference in MMP-3 levels of obese subjects with metabolic syndrome34. Furthermore, MMP-3 levels were not affected by significant weight loss people with obesity31,36–40,43. On the other hand, Traurig et al. demonstrated that MMP-3 levels were downregulated in preadipocytes/stromal vascular cells from obese subjects, and real-time PCR showed that MMP-3 expression levels are negatively correlated with percent body fat44. Similarly, genetic deletion of MMP-3 gene in mice resulted in increased body weight8. Another study demonstrated that, high fat diet decreased MMP-3 activity in female mice45. In line with these results, we have obtained decreased MMP-3/TIMP-1 ratio in obese people (Table 2).
Although obesity plays a key role in the development of hypertension, the mechanism underlying this effect has not been fully evaluated. Our results demonstrated a significant positive correlation between MMP-3 levels or MMP-3/TIMP-1 ratio and SBP/DBP in obese people (Fig. 3c,h). In line with our results, serum levels of MMP-3 were positively associated with arterial stiffness46,47 which is the primary cause of isolated systolic hypertension48. Moreover, the polymorphism of MMP-3 was associated with blood pressure and arterial stiffness49,50. Overall, MMP-3 gene variant seems to contribute to the development of hypertension by affecting arterial stiffness51. Another study group suggested that MMP-3 polymorphism could be beneficial in predicting risk for hypertension52.
Our results demonstrated that there is no difference in MMP-9 levels between obese, overweight, metabolic syndrome people, and non-obese people (Table 2). There are conflicting results regarding MMP-9 levels in obesity and metabolic syndrome. Several studies exhibited greater MMP-9 levels34,37,38,53–55 whereas others demonstrated either no difference33,39 or decreased MMP-9 levels in obese or metabolic syndrome9. In our results, we have found decreased MMP-9/TIMP-1 ratio in obese people (Table 2). There are several methodological discrepancies between studies, such as differences in gender distribution, age, species, and samples from which measurements were performed. Furthermore, several studies indicated a lack of association between adipose tissue and plasma levels of MMP-9, suggesting that this tissue is not a major contributor to circulating MMP-9 levels56,57.
Even though MMP-9 levels were not affected by obesity status, they are negatively correlated with endothelium-dependent response measured by forearm blood flow (Fig. 4). We have obtained similar results with MMP-9/TIMP-1 ratio (Supplementary Table 2). Endothelial dysfunction is one of the early determinants for obesity-related diseases including hypertension. Although the association between MMP-9 levels and hypertension was detected in several studies7,58, the mechanism underlying this effect was not investigated. Our results emphasized that MMP-9 levels or MMP-9/TIMP-1 ratio could be predictive for endothelial dysfunction. We suggest that more serious diseases related to endothelial dysfunction such as coronary artery disease could be prevented by measuring MMP-9 levels.
Our results exhibited that TIMP-1 levels were markedly and gradually increased in people with obesity as compared to overweight and non-obese people (Table 2). In line with our results, several studies demonstrated increased TIMP-1 levels either in adipose tissue or plasma-derived from people with obesity or experimental animals9,10,26,37,59–62. Compared with these studies, our results by stratifying obese population into different groups based on BMI and metabolic syndrome status further investigate TIMP-1 levels. Our results demonstrated that there is a progressive increase in TIMP-1 levels depending on obesity status. The increase in TIMP-1 levels in people with overweight could be an early predictor for obesity and obesity-related cardiovascular diseases. The role of TIMP-1 in obesity development was also supported by experimental studies. TIMP-1 increased the accumulation of lipid during differentiation of 3T3-L1 adipocytes63 and protection from obesity was observed in mice lacking TIMP-1 gene64. Similary, obese Zucker mice demonstrated increased TIMP-1 protein and activity11. On the other hand, there are some contradictory results regarding on TIMP-1 levels in obesity. Two studies performed on relatively low number of patients demonstrated that there was no change in TIMP-1 levels between obese and lean people65. Another study demonstrated that obesity was observed in mice with deletion of TIMP-1 gene12,66.
Our results exhibited that TIMP-2 levels were significantly increased in people with obesity and overweight compared to non-obese people (Table 2). In support of our findings, obese children and adolescents had greater TIMP-2 levels33. However, another study performed on premenopausal obese women exhibited no differences in TIMP-2 levels37. These conflicting results suggested a contribution of sex hormones in the regulation of TIMP-2 levels in obesity. Our results demonstrated that there was a significant difference in TIMP-2 levels between obese people with and without metabolic syndrome and greater levels of TIMP-2 in those groups versus non-obese subjects were observed. In accordance with our results, higher TIMP-2 levels were detected in patients with metabolic syndrome versus non-obese people54,67.
One of limitations is that MMPs activity is not investigated in our study. MMPs activity is also largely determined by MMPs/TIMPs balance and in this study we present our results as MMP/TIMP ratios. Since in literature there is a lack of information about MMPs activity in humans, the implication of MMPs activity in obesity, metabolic syndrome and endothelial dysfunction should be evaluated in future studies. Other limitation is that plasma levels of MMPs and TIMPs did not represent alterations in several organs and tissue including adipose tissue, heart or blood vessels compromised in obesity or metabolic syndrome. In our recent study we demonstrated that adipose tissue and blood vessels released large amount of MMPs and TIMPs which are regulated by inflammation24. Other study showed that perivascular adipose tissue derived from obese rats thoracic-aorta had increased MMP-9 activity, which was associated with increased stiffness68. Further studies to investigate MMPs activity in plasma and other organs and tissues in humans are necessary.
In conclusion, our results demonstrated that increased levels of MMP-1, MMP-2, TIMP-1, TIMP-2 and decreased ratios of MMP-3/TIMP-1 and MMP-9/TIMP-1 were detected in obese people while there was no difference in MMP-3 and MMP-9 levels. Significant correlations between anthropometric parameters and MMP-1 as well as MMP-2 levels supported these results. Furthermore, our results showing the correlations between MMP-3, -9, their ratios with TIMP-1 and blood pressure as well as endothelial-dependent response could be beneficial for the prevention of obesity-related cardiovascular diseases such as hypertension or atherosclerosis. Our findings will hopefully provide new aspects for the use of MMPs and TIMPs as clinical biomarkers in obesity-related cardiovascular diseases.
Supplementary Information
Acknowledgements
This work was supported by the Tunisian Ministry of High Education, Scientific Research and INSERM (Institut National de la Santé et de la Recherche Médicale) Paris U1148. The authors are especially thankful to the study participants.
Author contributions
S.B., K.C. and G.O. designed the study; S.B. M.J., X.N. and G.O. performed experiments; S.B., K.C., M.J, X.N. and G.O. analysed the data; S.B. and Z.T. obtained human plasma and recruitment of patients; S.B. and G.O. wrote the manuscript; S.B., K.C., Z.T., M.J., X.N. and G.O. revised manuscript.
Funding
Soumaya Boumiza, Karim Chahed, Zouhair Tabka, Marie-Paule Jacob, Xavier Norel, Gulsev Ozen declare that this study was funded by the Tunisian Ministry of Higher Education and Research and INSERM (Institut National de la Santé et de la Recherche Médicale) Paris U1148.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-99577-2.
References
- 1.Ortega FB, Lavie CJ, Blair SN. Obesity and cardiovascular disease. Circ. Res. 2016;118:1752–1770. doi: 10.1161/CIRCRESAHA.115.306883. [DOI] [PubMed] [Google Scholar]
- 2.Matsuzawa Y, Funahashi T, Nakamura T. The concept of metabolic syndrome: Contribution of visceral fat accumulation and its molecular mechanism. J. Atheroscler. Thromb. 2011;18:629–639. doi: 10.5551/jat.7922. [DOI] [PubMed] [Google Scholar]
- 3.Nagase H, Visse R, Murphy G. Structure and function of matrix metalloproteinases and TIMPs. Cardiovasc. Res. 2006;69:562–573. doi: 10.1016/j.cardiores.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 4.Chun TH, et al. Genetic link between obesity and MMP14-dependent adipogenic collagen turnover. Diabetes. 2010;59:2484–2494. doi: 10.2337/db10-0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tinahones FJ, et al. Obesity-associated insulin resistance is correlated to adipose tissue vascular endothelial growth factors and metalloproteinase levels. BMC Physiol. 2012;12:4. doi: 10.1186/1472-6793-12-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hopps E, Caimi G. Matrix metalloproteinases in metabolic syndrome. Eur. J. Intern. Med. 2012;23:99–104. doi: 10.1016/j.ejim.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Caimi G, et al. Lipid peroxidation, protein oxidation, gelatinases, and their inhibitors in a group of adults with obesity. Horm. Metab. Res. 2019;51:389–395. doi: 10.1055/a-0887-2770. [DOI] [PubMed] [Google Scholar]
- 8.Maquoi E, Demeulemeester D, Voros G, Collen D, Lijnen HR. Enhanced nutritionally induced adipose tissue development in mice with stromelysin-1 gene inactivation. Thromb. Haemost. 2003;89:696–704. doi: 10.1055/s-0037-1613586. [DOI] [PubMed] [Google Scholar]
- 9.Maquoi E, Munaut C, Colige A, Collen D, Lijnen HR. Modulation of adipose tissue expression of murine matrix metalloproteinases and their tissue inhibitors with obesity. Diabetes. 2002;51:1093–1101. doi: 10.2337/diabetes.51.4.1093. [DOI] [PubMed] [Google Scholar]
- 10.Chavey C, et al. Matrix metalloproteinases are differentially expressed in adipose tissue during obesity and modulate adipocyte differentiation. J. Biol. Chem. 2003;278:11888–11896. doi: 10.1074/jbc.M209196200. [DOI] [PubMed] [Google Scholar]
- 11.Schaefer L, et al. Differential regulation of glomerular gelatinase B (MMP-9) and tissue inhibitor of metalloproteinase-1 (TIMP-1) in obese Zucker rats. Diabetologia. 1997;40:1035–1043. doi: 10.1007/s001250050785. [DOI] [PubMed] [Google Scholar]
- 12.Gerin I, et al. Hyperphagia and obesity in female mice lacking tissue inhibitor of metalloproteinase-1. Endocrinology. 2009;150:1697–1704. doi: 10.1210/en.2008-1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pendas AM, et al. Diet-induced obesity and reduced skin cancer susceptibility in matrix metalloproteinase 19-deficient mice. Mol. Cell Biol. 2004;24:5304–5313. doi: 10.1128/MCB.24.12.5304-5313.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lijnen HR, et al. Matrix metalloproteinase inhibition impairs adipose tissue development in mice. Arterioscler. Thromb. Vasc. Biol. 2002;22:374–379. doi: 10.1161/hq0302.104522. [DOI] [PubMed] [Google Scholar]
- 15.Fontana V, Silva PS, Gerlach RF, Tanus-Santos JE. Circulating matrix metalloproteinases and their inhibitors in hypertension. Clin. Chim. Acta. 2012;413:656–662. doi: 10.1016/j.cca.2011.12.021. [DOI] [PubMed] [Google Scholar]
- 16.Marchesi C, et al. Plasma levels of matrix metalloproteinases and their inhibitors in hypertension: A systematic review and meta-analysis. J. Hypertens. 2012;30:3–16. doi: 10.1097/HJH.0b013e32834d249a. [DOI] [PubMed] [Google Scholar]
- 17.Wang X, Khalil RA. Matrix metalloproteinases, vascular remodeling, and vascular disease. Adv. Pharmacol. 2018;81:241–330. doi: 10.1016/bs.apha.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deedwania PC. Mechanisms of endothelial dysfunction in the metabolic syndrome. Curr. Diab. Rep. 2003;3:289–292. doi: 10.1007/s11892-003-0019-8. [DOI] [PubMed] [Google Scholar]
- 19.Flammer AJ, et al. The assessment of endothelial function: from research into clinical practice. Circulation. 2012;126:753–767. doi: 10.1161/CIRCULATIONAHA.112.093245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rezaianzadeh A, Namayandeh SM, Sadr SM. National cholesterol education program adult treatment panel III versus international diabetic federation definition of metabolic syndrome, which one is associated with diabetes mellitus and coronary artery disease? Int. J. Prev. Med. 2012;3:552–558. [PMC free article] [PubMed] [Google Scholar]
- 21.Sung KC, et al. Comparison of low-density lipoprotein cholesterol concentrations by direct measurement and by friedewald calculation. Am. J. Cardiol. 2020;125:866–873. doi: 10.1016/j.amjcard.2019.12.036. [DOI] [PubMed] [Google Scholar]
- 22.Boumiza S, et al. Role of MMP-1 (-519A/G, -1607 1G/2G), MMP-3 (Lys45Glu), MMP-7 (-181A/G), and MMP-12 (-82A/G) variants and plasma MMP levels on obesity-related phenotypes and microvascular reactivity in a Tunisian population. Dis. Mark. 2017;2017:6198526. doi: 10.1155/2017/6198526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O'Hara A, Lim FL, Mazzatti DJ, Trayhurn P. Microarray analysis identifies matrix metalloproteinases (MMPs) as key genes whose expression is up-regulated in human adipocytes by macrophage-conditioned medium. Pflugers Arch. 2009;458:1103–1114. doi: 10.1007/s00424-009-0693-8. [DOI] [PubMed] [Google Scholar]
- 24.Ozen G, et al. Inflammation increases MMP levels via PGE2 in human vascular wall and plasma of obese women. Int. J. Obes. (Lond.) 2019;43:1724–1734. doi: 10.1038/s41366-018-0235-6. [DOI] [PubMed] [Google Scholar]
- 25.Grzechocinska B, Dabrowski FA, Sierdzinski J, Cyganek A, Wielgos M. The association between serum metalloproteinase concentration, obesity, and hormone levels in reproductive-aged women. Endokrynol. Pol. 2019;70:49–56. doi: 10.5603/EP.a2018.0067. [DOI] [PubMed] [Google Scholar]
- 26.Papazoglou D, et al. Matrix metalloproteinase-1 and tissue inhibitor of metalloproteinases-1 levels in severely obese patients: What is the effect of weight loss? Exp. Clin. Endocrinol. Diabetes. 2010;118:730–734. doi: 10.1055/s-0030-1249671. [DOI] [PubMed] [Google Scholar]
- 27.Nho YK, et al. Matrix metalloproteinase-1 promoter is associated with body mass index in Korean population with aged greater or equal to 50 years. Clin. Chim. Acta. 2008;396:14–17. doi: 10.1016/j.cca.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 28.Huang HL, et al. Genetic variants associated with circulating MMP1 levels near matrix metalloproteinase genes on chromosome 11q21-22 in Taiwanese: Interaction with obesity. BMC Med. Genet. 2013;14:30. doi: 10.1186/1471-2350-14-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lo Presti R, Hopps E, Caimi G. Gelatinases and physical exercise: A systematic review of evidence from human studies. Medicine. 2017;96:e8072. doi: 10.1097/MD.0000000000008072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nagareddy PR, et al. Inhibition of matrix metalloproteinase-2 improves endothelial function and prevents hypertension in insulin-resistant rats. Br. J. Pharmacol. 2012;165:705–715. doi: 10.1111/j.1476-5381.2011.01583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Belo VA, et al. Increased activity of MMP-2 in hypertensive obese children is associated with hypoadiponectinemia. Obesity (Silver Spring) 2015;23:177–182. doi: 10.1002/oby.20939. [DOI] [PubMed] [Google Scholar]
- 32.Catalan V, et al. Increased interleukin-32 levels in obesity promote adipose tissue inflammation and extracellular matrix remodeling: Effect of weight loss. Diabetes. 2016;65:3636–3648. doi: 10.2337/db16-0287. [DOI] [PubMed] [Google Scholar]
- 33.Belo VA, et al. Assessment of matrix metalloproteinase (MMP)-2, MMP-8, MMP-9, and their inhibitors, the tissue inhibitors of metalloproteinase (TIMP)-1 and TIMP-2 in obese children and adolescents. Clin. Biochem. 2009;42:984–990. doi: 10.1016/j.clinbiochem.2009.03.025. [DOI] [PubMed] [Google Scholar]
- 34.Goncalves FM, et al. Increased circulating levels of matrix metalloproteinase (MMP)-8, MMP-9, and pro-inflammatory markers in patients with metabolic syndrome. Clin. Chim. Acta. 2009;403:173–177. doi: 10.1016/j.cca.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 35.Belo VA, et al. Effect of metabolic syndrome risk factors and MMP-2 genetic variations on circulating MMP-2 levels in childhood obesity. Mol. Biol. Rep. 2013;40:2697–2704. doi: 10.1007/s11033-012-2356-7. [DOI] [PubMed] [Google Scholar]
- 36.Ress C, et al. Influence of significant weight loss on serum matrix metalloproteinase (MMP)-7 levels. Eur. Cytokine Netw. 2010;21:65–70. doi: 10.1684/ecn.2009.0177. [DOI] [PubMed] [Google Scholar]
- 37.Kosmala W, et al. Matrix metalloproteinases 2 and 9 and their tissue inhibitors 1 and 2 in premenopausal obese women: Relationship to cardiac function. Int. J. Obes. (Lond.) 2008;32:763–771. doi: 10.1038/sj.ijo.0803794. [DOI] [PubMed] [Google Scholar]
- 38.Erman H, et al. The association of vascular endothelial growth factor, metalloproteinases and their tissue inhibitors with cardiovascular risk factors in the metabolic syndrome. Eur. Rev. Med. Pharmacol. Sci. 2016;20:1015–1022. [PubMed] [Google Scholar]
- 39.Miksztowicz V, et al. Increased plasma activity of metalloproteinase 2 in women with metabolic syndrome. Metabolism. 2008;57:1493–1496. doi: 10.1016/j.metabol.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 40.Glowinska-Olszewska B, Urban M, Florys B. Selected matrix metalloproteinases (MMP-2, MMP-9) in obese children and adolescents. Endokrynol. Diabetol. Chor. Przemiany Materii Wieku Rozw. 2006;12:179–183. [PubMed] [Google Scholar]
- 41.Miksztowicz V, et al. Adiponectin predicts MMP-2 activity independently of obesity. Eur. J. Clin. Invest. 2014;44:951–957. doi: 10.1111/eci.12328. [DOI] [PubMed] [Google Scholar]
- 42.Berg G, Schreier L, Miksztowicz V. Circulating and adipose tissue matrix metalloproteinases in cardiometabolic risk environments: Pathophysiological aspects. Horm. Mol. Biol. Clin. Investig. 2014;17:79–87. doi: 10.1515/hmbci-2013-0069. [DOI] [PubMed] [Google Scholar]
- 43.King LK, Henneicke H, Seibel MJ, March L, Anandacoomarasmy A. Association of adipokines and joint biomarkers with cartilage-modifying effects of weight loss in obese subjects. Osteoarthr. Cartil. 2015;23:397–404. doi: 10.1016/j.joca.2014.11.020. [DOI] [PubMed] [Google Scholar]
- 44.Traurig MT, et al. Differential expression of matrix metalloproteinase 3 (MMP3) in preadipocytes/stromal vascular cells from nonobese nondiabetic versus obese nondiabetic Pima Indians. Diabetes. 2006;55:3160–3165. doi: 10.2337/db06-0373. [DOI] [PubMed] [Google Scholar]
- 45.Wu Y, Lee MJ, Ido Y, Fried SK. High-fat diet-induced obesity regulates MMP3 to modulate depot- and sex-dependent adipose expansion in C57BL/6J mice. Am. J. Physiol. Endocrinol. Metab. 2017;312:E58–E71. doi: 10.1152/ajpendo.00128.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peeters SA, et al. Circulating matrix metalloproteinases are associated with arterial stiffness in patients with type 1 diabetes: pooled analysis of three cohort studies. Cardiovasc. Diabetol. 2017;16:139. doi: 10.1186/s12933-017-0620-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rajzer M, et al. The effect of antihypertensive treatment on arterial stiffness and serum concentration of selected matrix metalloproteinases. Arch. Med. Sci. 2017;13:760–770. doi: 10.5114/aoms.2016.58825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dart A, Silagy C, Dewar E, Jennings G, McNeil J. Aortic distensibility and left ventricular structure and function in isolated systolic hypertension. Eur. Heart J. 1993;14:1465–1470. doi: 10.1093/eurheartj/14.11.1465. [DOI] [PubMed] [Google Scholar]
- 49.Medley TL, Kingwell BA, Gatzka CD, Pillay P, Cole TJ. Matrix metalloproteinase-3 genotype contributes to age-related aortic stiffening through modulation of gene and protein expression. Circ. Res. 2003;92:1254–1261. doi: 10.1161/01.RES.0000076891.24317.CA. [DOI] [PubMed] [Google Scholar]
- 50.Beilby JP, et al. Stromelysin-1 (MMP-3) gene 5A/6A promoter polymorphism is associated with blood pressure in a community population. J. Hypertens. 2005;23:537–542. doi: 10.1097/01.hjh.0000160209.48479.ae. [DOI] [PubMed] [Google Scholar]
- 51.Huang R, et al. Associations of MMP1, 3, 9 and TIMP3 genes polymorphism with isolated systolic hypertension in Chinese Han population. Int. J. Med. Sci. 2013;10:840–847. doi: 10.7150/ijms.5728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee YH, Kim TY, Hong YM. Metalloproteinase-3 genotype as a predictor of cardiovascular risk in hypertensive adolescents. Korean Circ. J. 2009;39:328–334. doi: 10.4070/kcj.2009.39.8.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Derosa G, et al. Matrix metalloproteinase-2 and -9 levels in obese patients. Endothelium. 2008;15:219–224. doi: 10.1080/10623320802228815. [DOI] [PubMed] [Google Scholar]
- 54.Hopps E, et al. Gelatinases and their tissue inhibitors in a group of subjects with metabolic syndrome. J. Investig. Med. 2013;61:978–983. doi: 10.2310/JIM.0b013e318294e9da. [DOI] [PubMed] [Google Scholar]
- 55.Cicero AF, et al. Vascular remodeling and prothrombotic markers in subjects affected by familial combined hyperlipidemia and/or metabolic syndrome in primary prevention for cardiovascular disease. Endothelium. 2007;14:193–198. doi: 10.1080/10623320701606731. [DOI] [PubMed] [Google Scholar]
- 56.Gummesson A, et al. Adipose tissue is not an important source for matrix metalloproteinase-9 in the circulation. Scand. J. Clin. Lab Invest. 2009;69:636–642. doi: 10.3109/00365510902912747. [DOI] [PubMed] [Google Scholar]
- 57.Miksztowicz V, et al. Effect of insulin-resistance on circulating and adipose tissue MMP-2 and MMP-9 activity in rats fed a sucrose-rich diet. Nutr. Metab. Cardiovasc. Dis. 2014;24:294–300. doi: 10.1016/j.numecd.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 58.Yasmin, et al. Matrix metalloproteinase-9 (MMP-9), MMP-2, and serum elastase activity are associated with systolic hypertension and arterial stiffness. Arterioscler. Thromb. Vasc. Biol. 2005;25:372. doi: 10.1161/01.ATV.0000151373.33830.41. [DOI] [PubMed] [Google Scholar]
- 59.Kralisch S, et al. Tissue inhibitor of metalloproteinase-1 predicts adiposity in humans. Eur. J. Endocrinol. 2007;156:257–261. doi: 10.1530/eje.1.02328. [DOI] [PubMed] [Google Scholar]
- 60.Glowinska-Olszewska B, Urban M. Elevated matrix metalloproteinase 9 and tissue inhibitor of metalloproteinase 1 in obese children and adolescents. Metabolism. 2007;56:799–805. doi: 10.1016/j.metabol.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 61.Maury E, et al. Adipokines oversecreted by omental adipose tissue in human obesity. Am. J. Physiol. Endocrinol. Metab. 2007;293:E656–665. doi: 10.1152/ajpendo.00127.2007. [DOI] [PubMed] [Google Scholar]
- 62.Meissburger B, Stachorski L, Roder E, Rudofsky G, Wolfrum C. Tissue inhibitor of matrix metalloproteinase 1 (TIMP1) controls adipogenesis in obesity in mice and in humans. Diabetologia. 2011;54:1468–1479. doi: 10.1007/s00125-011-2093-9. [DOI] [PubMed] [Google Scholar]
- 63.Alexander CM, Selvarajan S, Mudgett J, Werb Z. Stromelysin-1 regulates adipogenesis during mammary gland involution. J. Cell. Biol. 2001;152:693–703. doi: 10.1083/jcb.152.4.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lijnen HR, Demeulemeester D, Van Hoef B, Collen D, Maquoi E. Deficiency of tissue inhibitor of matrix metalloproteinase-1 (TIMP-1) impairs nutritionally induced obesity in mice. Thromb. Haemost. 2003;89:249–255. doi: 10.1055/s-0037-1613439. [DOI] [PubMed] [Google Scholar]
- 65.Andrade VL, et al. Evaluation of plasmatic MMP-8, MMP-9, TIMP-1 and MPO levels in obese and lean women. Clin. Biochem. 2012;45:412–415. doi: 10.1016/j.clinbiochem.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 66.Shin YH, et al. Associations of matrix metalloproteinase (MMP)-8, MMP-9, and their inhibitor, tissue inhibitor of metalloproteinase-1, with obesity-related biomarkers in apparently healthy adolescent boys. Korean J. Pediatr. 2014;57:526–532. doi: 10.3345/kjp.2014.57.12.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yasmeen S, Khan U, Khan GM, Fatima SS. Association of tissue inhibitor of metalloproteinase 2 with non-alcoholic fatty liver disease in metabolic syndrome. Arch. Physiol. Biochem. 2019;125:441–446. doi: 10.1080/13813455.2018.1481095. [DOI] [PubMed] [Google Scholar]
- 68.DeVallance E, et al. Aortic dysfunction in metabolic syndrome mediated by perivascular adipose tissue TNFalpha- and NOX2-dependent pathway. Exp. Physiol. 2018;103:590–603. doi: 10.1113/EP086818. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.