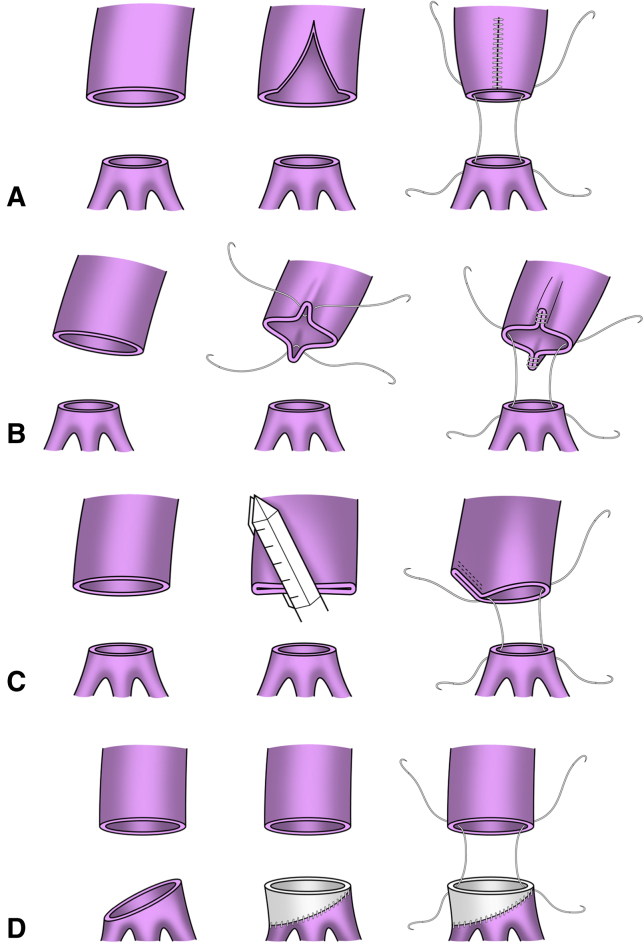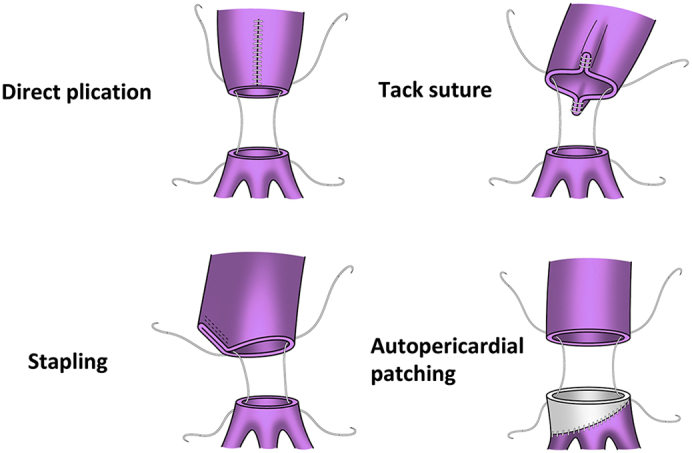
The schema of the pulmonary arterioplasty of various techniques.
Central Message.
Vessels of different calibers are often encountered when anastomosing pulmonary arteries during lung transplantation. Variants of the method we propose can be used in such situations.
See Commentaries on pages 195 and 197.
Vessels of different calibers are often encountered when anastomosing pulmonary arteries (PAs) during lung transplantation. In living-donor lobar lung transplantation (LDLLT), grafts are taken from the donor's lower lobes, and pulmonary anastomosis sometimes requires adjustment of the caliber of the blood vessels due to mismatch between the donor's and the recipient's PAs. Among the solutions to this problem, as we previously reported, is donor graft PA plasty using an autopericardial patch to preserve the donor's lingular branch if the graft's PA has a diagonal cut line.1,2 Other surgical techniques include using a tack suture or direct plication of the recipient's large PA. In cadaveric lung transplantation (CLT), a PA size mismatch could also be encountered because a giant PA can be seen in a recipient with idiopathic pulmonary hypertension.3 Herein, we reviewed the surgical techniques used in our institution along with some new surgical techniques.
Patients and Methods
Between 2008 and 2020, 263 lung transplants were performed at Kyoto University Hospital. Of these, 19 patients underwent pulmonary arterioplasty to adjust the caliber of the PA due to caliber mismatch. We used 4 different techniques to anastomose mismatched PAs during lung transplantation (Video 1). We retrospectively examined the frequency at which each technique was used and the presence of complications. This study was approved by the Kyoto University Institutional Review Board (No. R2389-1; February 24, 2021). All patients provided written informed consent before surgery, allowing for the use of their clinical data.
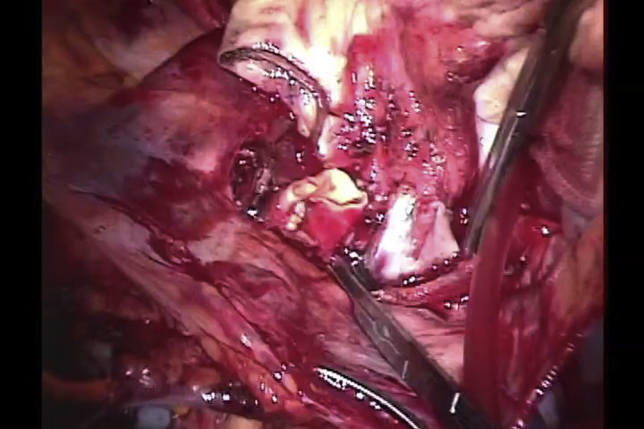
Video 1.
Videos of the 4 techniques during implantation are shown. Direct plication: The dilated wall of the recipient's pulmonary artery is incised, leaving only the healthy portion. Anastomosis is performed after suturing. Tack suture: The wall of the recipient's pulmonary artery is partially sutured and sewn in the pocket. Stapling: Half of the dilated pulmonary artery wall is stapled, and the caliber difference is matched before anastomosis. Autopericardial patching: After harvesting the pericardium, the donor's PA is patched in a back table. In this case, the edge of the pericardial patch is supported to obtain the operation view. After trimming, anastomosis is performed. Video available at: https://www.jtcvs.org/article/S2666-2507(21)00403-X/fulltext.
Surgical Techniques
Direct plication
This procedure includes incising and opening the main PA, followed by direct closure. After suturing, end-to-end anastomosis was performed (Figure 1, A).
Figure 1.
Operative techniques. The schema of the pulmonary arterioplasty of various techniques. A, Direct replication. B, Tack sutures. C, Stapling. D, Autopericardial patching.
Tack suture
Before anastomosis, 1 stitch was placed in the main PA, and the pocket was plicated. An important step in this procedure is repetitive suturing to avoid leaving a suture pocket. If caliber mismatch persists, 1 more stitch can be used to adjust the caliber mismatch (Figure 1, B).
Stapling
Before anastomosis, half of the main PA was stapled obliquely, and the remaining part was anastomosed (Figure 1, C).
Autopericardial patching
When the PA incision line of the donor graft was oblique, an autopericardial patch from the recipient was used. Intraoperatively, the stump of the graft PA was modified to ensure an optimal cuff (Figure 1, D).
Results
Patient Characteristics
The mean age of the 19 recipients was 47.5 ± 15.2 years (median age, 51 years; range, 3-64 years). Fifteen patients underwent LDLLT, and 4 patients had CLT. Only 1 patient (patient 15) underwent single lung transplantation, the other 18 patients underwent double lung transplantation (Table 1).
Table 1.
Patient characteristics
| Patient | Age/sex | Disease | Operation | PA plasty left | PA plasty right | Complication |
|---|---|---|---|---|---|---|
| 1 | 49/F | IPF | LDLLT | Direct plication | No | – |
| 2 | 44/M | OB after HSCT | LDLLT | Autopericardial patching | No | – |
| 3 | 64/M | IPF | LDLLT | Tack suture | No | Left PA kinking |
| 4 | 49/F | OB after HSCT | LDLLT | Autopericardial patching | No | – |
| 5 | 57/F | OB after HSCT | LDLLT | Autopericardial patching | Tack suture | – |
| 6 | 48/M | IPF | LDLLT | Autopericardial patching | No | – |
| 7 | 27/F | IPAH | LDLLT | Autopericardial patching | Direct plication | – |
| 8 | 58/M | IPF | LDLLT | Autopericardial patching | No | – |
| 9 | 57/F | IPH | LDLLT | Tack suture | No | – |
| 10 | 22/F | OB after HSCT | LDLLT | autopericardial patching | No | – |
| 11 | 56/F | IPF | LDLLT | Autopericardial patching | Tack suture | – |
| 12 | 64/M | IPF | LDLLT | Tack suture | Tack suture | – |
| 13 | 59/F | IPF | LDLLT | Autopericardial patch | Tack suture | – |
| 14 | 57/F | IPF | LDLLT | No | Tack suture | – |
| 15 | 3/M | PVOD | LDLLT | No | Direct plication | – |
| 16 | 45/F | IPAH | CLT | Stapling | Stapling | – |
| 17 | 35/F | ASD + Eisenmenger |
CLT | No | Direct plication | – |
| 18 | 51/M | IPAH | CLT | No | Tack suture | – |
| 19 | 52/F | IPAH | CLT | Tack suture, direct plication | Stapling, tack suture | – |
PA, Pulmonary artery; F, female; IPF, idiopathic pulmonary fibrosis; LDLLT, living-donor lobar lung transplantation; M, male; OB, bronchiolitis obliterans; HSCT, hematopoietic stem cell transplantation; IPAH, idiopathic pulmonary arterial hypertension; IPH, idiopathic pulmonary hemosiderosis; PVOD, pulmonary veno-occlusive disease; CLT, cadaveric lung transplantation; ASD, atrial septal defect.
Direct plication
This method was performed in patients 1, 7, 15, 17, and 19.
Tack suture
This procedure was performed before anastomosis in patients 3, 5, 9, 11, 12, 13, 14, 18, and 19.
Stapling
This procedure was performed on 2 patients (patients 16 and 19). Both patients had dilated pulmonary arteries due to idiopathic pulmonary hypertension.
Autopericardial patching
This procedure was performed in 9 patients for all left-side cases (patients 2, 4, 5, 6, 7, 8, 10, 11, and 13). All of these patients were LDLLT recipients.
Postoperative Complications
Twenty-four hours after transplantation, 1 patient (patient 3) presented with kinking of the PA, and a metallic stent was inserted into the main PA. The other patients had no major complications after reperfusion or transplantation. All recipients' PA were patent during follow-up CT 6 months postoperatively. At the end of 2020, no PA anastomosis-related deaths had been recorded.
Discussion
Only few reports on PA caliber mismatch during lung transplantation are available.4 In our study, 4 different methods were used when PA caliber mismatch during lung transplantation was encountered. These 4 techniques made it possible to match the caliber difference in cases where the recipient's PA is dilated or in cases of living lung transplantation. Complications related to the surgical technique used occurred in only 1 patient.5 This was caused by the abundant length of the PA after anastomosis and not by the caliber difference. The length of the PA should be carefully determined in addition to the caliber difference. Close attention should be paid to the bite and stitch because tight suturing can cause stenosis. Pulmonary vascular complications after lung transplantation are associated with high mortality rates. During LDLLT, the graft lungs are usually small, and vascular complications may be lethal. In our study, there were no other PA anastomosis-related complications and no PA anastomosis-related deaths. These indicate that our technique is safe and useful for CLT and LDLLT.
Footnotes
Disclosures: The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Supplementary Data
Videos of the 4 techniques during implantation are shown. Direct plication: The dilated wall of the recipient's pulmonary artery is incised, leaving only the healthy portion. Anastomosis is performed after suturing. Tack suture: The wall of the recipient's pulmonary artery is partially sutured and sewn in the pocket. Stapling: Half of the dilated pulmonary artery wall is stapled, and the caliber difference is matched before anastomosis. Autopericardial patching: After harvesting the pericardium, the donor's PA is patched in a back table. In this case, the edge of the pericardial patch is supported to obtain the operation view. After trimming, anastomosis is performed. Video available at: https://www.jtcvs.org/article/S2666-2507(21)00403-X/fulltext.
References
- 1.Kayawake H., Toyofumi F., Chen-Yoshikawa, Aoyama A., Date H. Pulmonary arterioplasty with end-to-end anastomosis of the lingular branch to the interlobar pulmonary artery in living-donor lobectomy. Ann Thorac Surg. 2016;102:e351–e352. doi: 10.1016/j.athoracsur.2016.03.052. [DOI] [PubMed] [Google Scholar]
- 2.Kayawake H., Chen-Yoshikawa T.F., Aoyama A., Motoyama H., Hijiya K., Menju T. Excellent outcome of donor lobectomy with various surgical techniques of the interlobar artery. Eur J Cardiothorac Surg. 2017;51:279–283. doi: 10.1093/ejcts/ezw298. [DOI] [PubMed] [Google Scholar]
- 3.Yokoyama Y., Chen F., Minakata K., Yamada T., Aoyama A., Sato M. Living-donor lobar transplantation for treatment of idiopathic pulmonary arterial hypertension with severe pulmonary arterial dilatation. Ann Thorac Surg. 2014;97:e149. doi: 10.1016/j.athoracsur.2014.02.071. [DOI] [PubMed] [Google Scholar]
- 4.Griffith B.P., Magee M.J., Gonzalez I.F., Houel R., Armitage J.M., Hardesty R.L. Anastomotic pitfalls in lung transplantation. J Thorac Cardiovasc Surg. 1994;107:743–754. [PubMed] [Google Scholar]
- 5.Chen F., Tazaki J., Shibata T. Stent angioplasty for a kink in the pulmonary artery anastomosis soon after living-donor lobar transplantation. Ann Thorac Surg. 2011;92:e105–e106. doi: 10.1016/j.athoracsur.2011.05.049. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Videos of the 4 techniques during implantation are shown. Direct plication: The dilated wall of the recipient's pulmonary artery is incised, leaving only the healthy portion. Anastomosis is performed after suturing. Tack suture: The wall of the recipient's pulmonary artery is partially sutured and sewn in the pocket. Stapling: Half of the dilated pulmonary artery wall is stapled, and the caliber difference is matched before anastomosis. Autopericardial patching: After harvesting the pericardium, the donor's PA is patched in a back table. In this case, the edge of the pericardial patch is supported to obtain the operation view. After trimming, anastomosis is performed. Video available at: https://www.jtcvs.org/article/S2666-2507(21)00403-X/fulltext.