Abstract
Objectives:
Right unilateral brief pulse (RUL-BP) ECT has been adopted as a technique for reducing the cognitive side effects of ECT relative to sine wave or bilateral treatments, but it is unknown how often patients are transitioned to alternative electrode placements. This study analyzes time in first lifetime acute course RUL-BP ECT.
Methods:
A single-center retrospective chart review was conducted of adult patients receiving a first lifetime course of ECT from 2000–2017 beginning with individualized seizure threshold determination using RUL-BP treatment parameters.
Results:
1,383 patients met study criteria and received a mean number of 9.4±3.1 treatments, of which 7.6±3.3 were utilizing RUL-BP stimuli. Only 37.5% of patients were transitioned from RUL to bilateral treatments. Younger patients and those diagnosed with bipolar disorder were more likely to transition from RUL-BP to bilateral treatments, but the overall number of treatments did not differ based on age or primary diagnosis.
Conclusions:
Among patients who begin treatment with RUL-BP ECT, more than 60% use exclusively those parameters throughout their acute course.
Keywords: electroconvulsive therapy, cohort studies, survival analysis, brief pulse
Introduction
Electroconvulsive therapy (ECT) is a safe1–4 and cost-effective5 treatment for affective and other psychiatric disorders, and its use is associated with decreased overall mortality among recipients.6 The optimal treatment parameters—in particular pulse width, with ultra-brief pulse (UBP; <0.5 ms) and brief pulse (BP; 0.5–2 ms) as the two most common treatment techniques—remains an area of active debate as treatment parameters may impact efficacy, tolerability, and duration in treatment.7–9 While prospective trials with strict criteria for treatment selection have compared different ECT montages, it is unclear in ordinary clinical practice how often patients remain in treatment with the initial prescribed parameters, and how often they are transitioned to alternative treatments. Data from large clinical cohorts which include a range of these techniques as part of usual clinical practice could help inform patients and treating physicians as to the overall likelihood of remaining in a particular treatment method, and provide evidence of differences in treatment among patents based on clinical characteristics. This study provides a descriptive analysis of patients treated with right unilateral (RUL) BP ECT at a freestanding psychiatric hospital with a high-volume ECT service. It explores how long patients remain in RUL-BP ECT, and how often they are transitioned to other treatment types. Furthermore, this study characterizes the effects of age, sex, clinical diagnosis, and initial seizure threshold on the length of a treatment course and the applied charge.
Methods
Population and Setting
This was a retrospective cohort study of patient receiving ECT at a freestanding psychiatric hospital between January 2000 and June 2017. The study population included all patients 18 or older who received a first lifetime course of ECT during the study population that began with an individualized seizure threshold determination using RUL-BP treatment parameters. Patients were followed for the duration of acute course ECT, defined to be the time until ECT discontinuation or through treatment 12, if ECT continued past that point. A wavier of informed consent for this retrospective cohort study was approved by the Partners Healthcare Institutional Review Board.
Treatment procedure
All patients had seizure threshold determination by dose titration at the time of first treatment, with subsequent treatments given three times weekly. Decisions about dosing and transition to alternative electrode placement were made by the treating psychiatrist according to clinical response. ECT was provided using a Mecta Spectrum 5000Q (Tualatin, OR). All patients received general anesthesia, most with methohexital (default dose 1 mg/kg) but etomidate, thiopental, propofol, or ketamine could be used at the discretion of the treating physicians. Succinylcholine (default dose 1 mg/kg) was used as the muscle relaxant. Seizure adequacy was assessed using both two lead bifrontal or fronto-mastoid EEG and the “cuff method” of inflating a BP cuff on one calf prior to muscle relaxant administration to observe the motor seizure.
Statistical Analysis
Kaplan-Meier analysis of duration of treatment, in terms of number of completed treatments, was performed using Prism (v 8.4, San Diego CA). For purposes of Kaplan-Meier analysis for RUL-BP ECT, patients who were transitioned from the initial unilateral electrode placement to bilateral treatments during the first 12 treatments were defined as events. In contrast, those who discontinued ECT prior to the twelfth treatment but had all treatments using a RUL-BP stimulus were defined as censored. For Kaplan-Meier analysis in ECT overall, patients who stopped treatment prior to the twelfth treatment were counted as events, while survival time included treatments utilizing any type of ECT (unilateral or bilateral). Comparisons between pairs of survival curves are made using the logrank test, and between multiple survival curves using the logrank test for trend. The eventual binary outcome of transitioning from RUL-BP treatment to bilateral treatments was analyzed using logistic regression with sex, age (z-score), diagnosis (major depressive disorder, bipolar affective disorder, other), and initial seizure threshold ≤ 40 mC as descriptor variables using R (v 3.6, Vienna, Austria). The final treatment dose was analyzed using linear regression, with male sex, age (z-score), diagnosis (major depressive disorder, bipolar affective disorder, other), and initial seizure threshold ≤ 40 mC as descriptor variables, also using R.
Results
A total of 3,860 patients began ECT during the study period, of whom 170 began with bilateral treatments and 2,307 began with right unilateral ultrabrief pulse treatments, leaving 1,383 patients who met inclusion criteria. These patients had a mean age of 49.4±16.9 years (Table 1). Men (588) made up 42.5% of the sample. Diagnoses were unipolar depression (1,008; 72.9%), bipolar disorder (211; 15.3%), other (70; 5.1%), and missing (94; 6.8%). Anesthetics used were methohexital (1,165; 85.0%), thiopental (128; 9.3%), propofol (73; 5.3%), and etomidate (5; 0.4%). Participants received a mean of 9.4±3.1 ECT treatments, of which a mean of 7.6±3.3 were RUL-BP treatments. Most patients received ECT three times a week, with the median patient receiving treatment #4 seven days after the initial treatment and treatment #7 16 days later. Later in the course there was spacing of treatments with #10 on day 28 and treatment #12 on day 40 (Table S1).
Table 1:
characteristics of the cohort, overall and based on outcome during acute course treatment. “RUL survivors” are those patients who received twelve RUL-BP treatments. “RUL censored” patients discontinued ECT prior to the twelfth treatment, but had all treatments using RUL-BP stimuli. “RUL dropouts” are the patients who transitioned from RUL-BP ECT to bilateral treatments during the acute course.
| All patients | RUL “survivors” | RUL “censored” | RUL “dropouts” | |
|---|---|---|---|---|
| N | 1383 | 298 | 567 | 518 |
| Sex = male (%) | 588 (42.5) | 124 (41.6) | 235 (41.4) | 229 (44.2) |
| Age (yrs; mean (SD)) | 49.4 (16.9) | 51.2 (17.0) | 49.8 (17.2) | 47.8 (16.3) |
| # of treatments (mean (SD)) | 9.4 (3.1) | 12 (0) | 6.7 (2.7) | 10.8 (1.9) |
| # of RUL treatments (mean (SD)) | 7.6 (3.3) | 12 (0) | 6.7 (2.7) | 6.0 (2.5) |
| Treatment #1 | Treatment #12 | Last before censoring | Last before dropout | |
| Dose (mC; mean (SD)) | 75.0 (38.4) | 406.8 (140.4) | 329.8 (151.9) | 371.1 (153.5) |
| Dose (mC; median) | 80 | 403.2 | 288 | 403.2 |
| Major depressive disorder (%) | 1008 (72.9) | 227 (76.2) | 412 (72.7) | 369 (71.2) |
| Bipolar disorder (%) | 211 (15.3) | 42 (14.1) | 75 (13.2) | 94 (18.1) |
| Other (%) | 70 (5.1) | 18 (6.0) | 25 (4.4) | 27 (5.2) |
| Missing (%) | 94 (6.8) | 11 (3.7) | 55 (9.7) | 28 (5.4) |
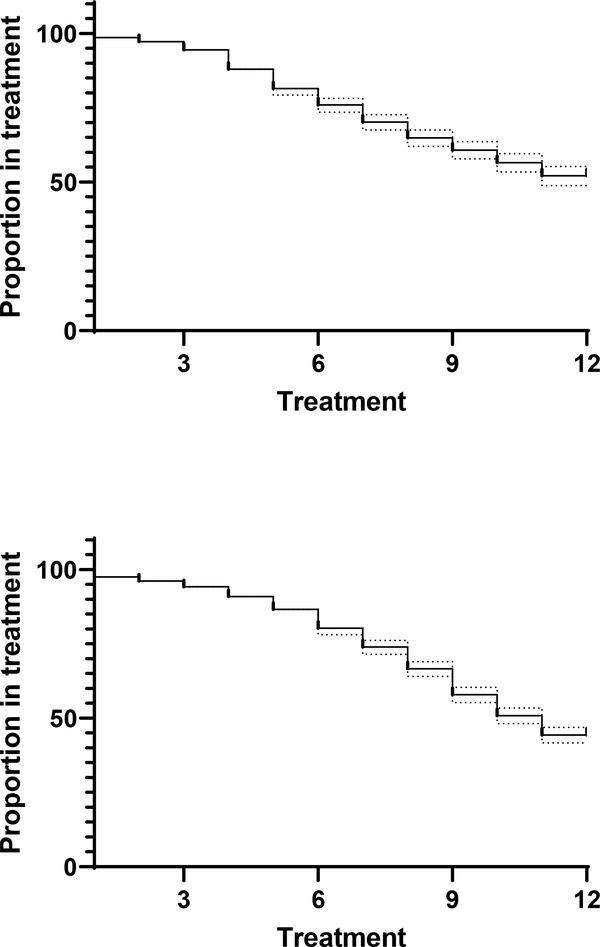
At treatment #12, 298 (21.5%) patients were still receiving RUL-BP ECT, while 567 (41.0%) discontinued treatment prior to the twelfth ECT but had all treatments using RUL-BP stimuli (mean of 6.7±2.7 treatments). A further 518 (37.5%) were transitioned from RUL-BP treatments to bilateral treatments over the course of acute ECT after having received a mean of 6.0±2.5 RUL-BP treatments. At treatment #12 613 patients (44.3%) were continuing in any type of ECT, of whom 298 were continuing to receive RUL-BP treatments. Using the Kaplan-Meier method, the proportion of patients remaining in treatment with RUL-BP parameters through treatment #12 is 52.1% (Figure 1; Figure S1).
Figure 1:
Top: Kaplan-Meier analysis for remaining in RUL-BP ECT. Patients who are transitioned to bilateral treatments before the twelfth treatment are counted as events, while those who discontinue ECT but have their last treatment with RUL-BP are censored. Proportion utilizing RUL-BP at treatment #12 is 52.1%. Bottom: Kaplan-Meier analysis for remaining in any type of ECT, with discontinuation of ECT for any reason counted as events. Proportion in any type of ECT is 44.3% at treatment #12. 95% confidence intervals for survival curves are shown as dashed lines.
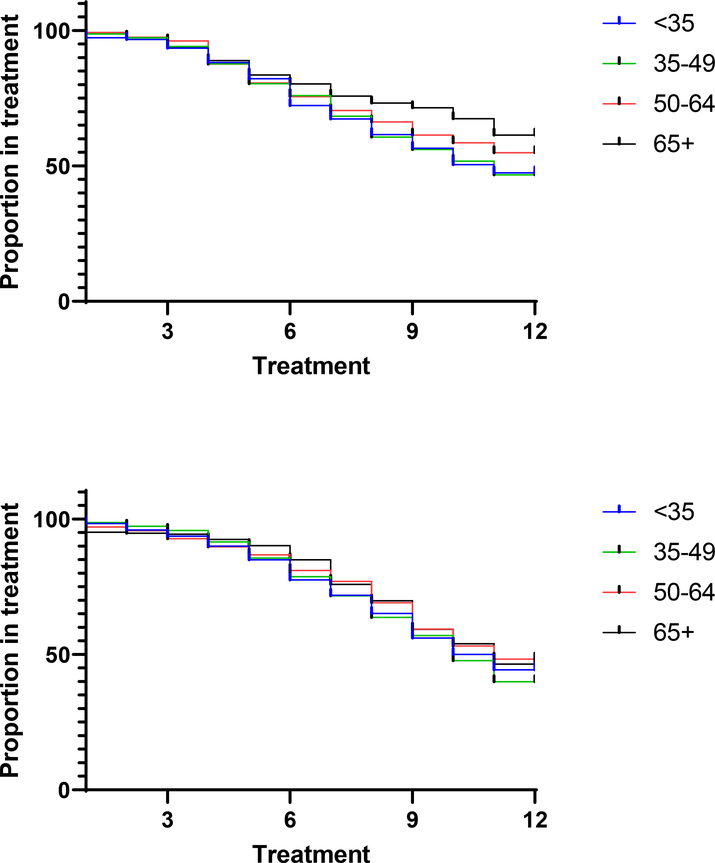
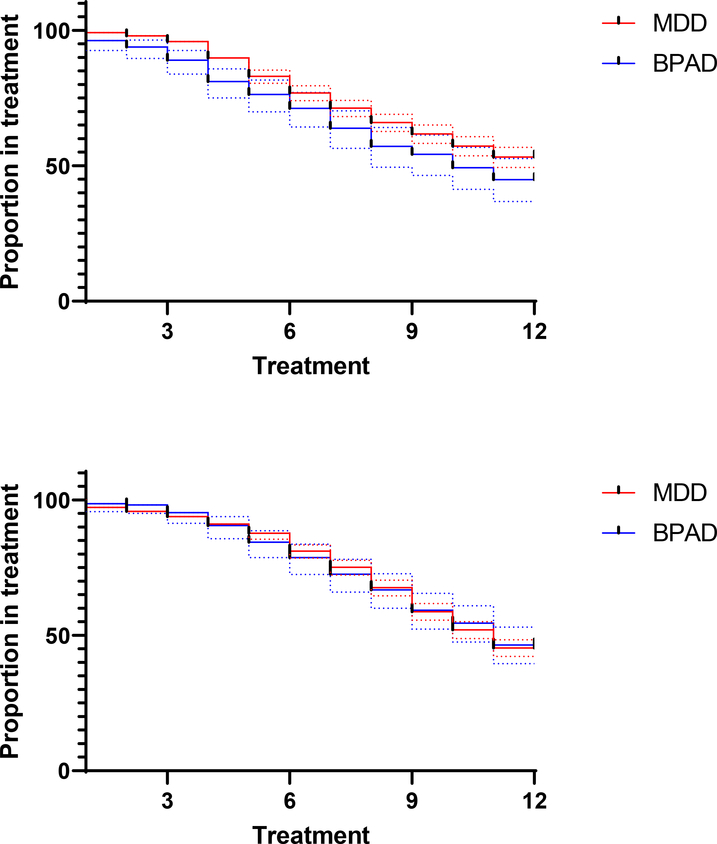
Separating patients into age cohorts (<35 years old, 35–49, 50–64, 65+), patients have differing time in RUL-BP treatment depending on their age with older patients having longer time in treatment with these parameters (χ2=10.26, p=0.0014, logrank test for trend), but have equal overall time in ECT treatment (χ2=2.42, p=0.12, logrank test for trend; Figure 2). Likewise comparing patients with major depressive disorder (1,008) and those with bipolar disorder (211), those with MDD have more RUL-BP treatments (p=0.011, logrank test) but identical numbers of overall treatments (p=0.88, logrank test; Figure 3).
Figure 2:
Top: Kaplan-Meier analysis for remaining in RUL-BP ECT, broken down by age (<35, blue; 35–49, green; 50–64, red; >65, black). Proportions remaining in RUL-BP treatments at treatment #12 differ among the 4 age buckets with older patients remaining in RUL-BP treatment for a longer time (χ2=10.26, p=0.0014, logrank test for trend). Bottom: Kaplan-Meier analysis for remaining in any type of ECT, broken down by age (<35, blue; 35–49, green; 50–64, red; >65, black). Proportion remaining in any ECT do not differ significantly among the 4 age buckets (χ2=2.42, p=0.12, logrank test for trend).
Figure 3:
Top: Kaplan-Meier analysis for remaining in RUL-UBP ECT among patients with a diagnosis of major depressive disorder (red) or bipolar disorder (blue). Patients with bipolar disorder have overall decreased time in RUL-BP treatment (p=0.011, logrank test). Bottom: Kaplan-Meier analysis for remaining in any type of ECT among patients with a diagnosis of major depressive disorder (red) or bipolar disorder (blue). Duration in ECT does not differ significantly among the two diagnoses (p=0.88, logrank test). 95% confidence intervals for survival curves are shown as dashed lines.
In a multivariable logistic model of transition from RUL-BP to other stimulus types, older age was associated with lower risk of dropout (aOR 0.78–0.98), whereas sex, age, diagnostic category, and low initial seizure threshold were not significantly associated with dropout from RUL-UBP (Table 2).
Table 2:
Logistic model of transition from RUL-BP to bilateral ECT using male sex, age (z-score), diagnosis (major depressive disorder, bipolar affective disorder, other), and initial seizure threshold ≤ 40 mC. R2=0.01.
| Predictors | Odds Ratios | CI | p |
|---|---|---|---|
| Sex (male) | 1.1 | 0.88 – 1.37 | 0.399 |
| Age (z-score) | 0.87 | 0.78 – 0.98 | 0.017 |
| Diagnosis | |||
| MDD | 1.16 | 0.82 – 1.65 | 0.415 |
| BPAD | 1.52 | 1.00 – 2.34 | 0.052 |
| Initial ST ≤ 40 mC | 0.83 | 0.34 – 1.86 | 0.653 |
RUL-BP dose changed over the course of treatment, with a mean dose at treatment #1 (the time of individual seizure threshold determination) of 75.0±38.4 mC.10 This increased to 236.3±103.1 mC for treatment #2 (3.2x initial dose). There was a further increase in dose over the duration of the acute course (Figure S2), with mean dose of 406.8±140.4 mC, or 5.4x initial dose, among the 298 patients continuing in RUL-BP at treatment #12. The 567 patients who discontinued ECT had a mean dose of 329.8±151.9 mC at last RUL-BP treatment before censoring (4.4x initial dose), compared to 371.1±153.5 mC (4.9x initial dose) for the final RUL-BP treatment in the 518 patients who transitioned to bilateral treatments. In a multivariable linear model of final RUL-BP dose male sex and older age were each associated with higher final dose whereas diagnostic categories and low initial dose were not significantly associated (Table 3).
Table 3:
Linear regression of final BP dose on sex, age (z-score), diagnosis (major depressive disorder, bipolar disorder, other), and initial seizure threshold ≤ 40 mC. R2=0.08.
| Predictors | Estimates | CI | p |
|---|---|---|---|
| Sex (male) | 32.55 | 16.86 – 48.25 | <0.001 |
| Age (z-score) | 39.69 | 31.79 – 47.58 | <0.001 |
| Diagnosis | |||
| MDD | 1.91 | −22.34 – 26.17 | 0.877 |
| BPAD | −4.08 | −34.19 – 26.03 | 0.79 |
| Initial ST ≤40 mC | −57 | −115.56 – 1.57 | 0.056 |
Discussion
Patients who began RUL-BP ECT at our study site received a mean 9.4±3.1 ECT treatments, of which a mean of 7.6±3.3 were utilizing RUL-BP stimuli. Kaplan-Meier analysis indicates the proportion remaining in RUL-BP stimuli through treatment #12 was 52.1%. In total 37.5% of patients were transitioned to bilateral treatments at some point during the acute course.
Prospective trials using prespecified criteria for selecting and modifying treatment parameters have analyzed the number of treatments required to remit from depression using ECT. The CORE trial utilized bilateral ECT and found a mean of 7.3 treatments until remission among 184 remitters,11 and an identical mean of 7.3 treatments was found among the 148 remitting patients out of 240 geriatric patients treated with RUL-UBP ECT in the PRIDE trial.12 More recently the EFFECT-Dep trial of unilateral brief pulse ECT vs bilateral ECT used an average of 7.8 RUL-BP treatments before remission among the 69 patients randomized to RUL-BP ECT.13 As our retrospective data is based on usual clinical practice without strictly-defined criteria for treatment, it cannot be directly compared to these trials. Despite this limitation, the 7.6±3.3 RUL-BP treatments in our clinical sample matches closely the values from the prospective trials.
Continued treatment using RUL-BP stimuli was lower in younger patients relative to older patients, but notably the overall average time in ECT (including RUL-BP and other stimulus types) did not differ on age. While there are numerous reasons for discontinuing ECT including disease remission, lack of efficacy, and intolerable side effects, switching from RUL-BP to bilateral treatments will generally only occur in the case of insufficient clinical response. As this is a retrospective study, treatment decisions were made by the treating psychiatrist and not algorithmically. Meta-analysis of bilateral treatments indicates equivalent efficacy in depression but worse cognitive outcomes relative to RUL ECT,14 and as a result treating psychiatrists may have been hesitant to use bilateral treatments in older patients which may partially explain the difference in dropout relative to younger patients. These results are consistent with our logistic model of transition from RUL-BP treatments to bilateral ones, in which only a small minority of the sample variance was explained by age, sex, diagnosis, or seizure threshold, and the effect size of the only significant predictive variable was small.
Similar to the effect of age, a diagnosis of bipolar disorder was associated with fewer RUL-BP treatments relative to a diagnosis of major depressive disorder but an equivalent number of overall treatments. This result is consistent with meta-analyses showing equivalent antidepressant effect of ECT in major depressive disorder and bipolar depression,15,16 but is contrary to studies showing a slightly faster response in bipolar depression as faster transition to bilateral treatments suggests less efficacy at the time of dropout, thus necessitating more intensive treatments.16
Treatment response to unilateral ECT depends significantly on dosage,17,18 and patients in this sample were initially dosed at approximately 3x initial seizure threshold, on average, increasing to approximately 5x by the end of the treatment course. This is a dose range that has been associated with less antidepressant efficacy than 6x for initial treatments. A similar trend towards increased dosing during a treatment course has been found in prospective trials. For instance, Loo et al. dosed patients receiving RUL-BP ECT initially at 4.8x seizure threshold, rising to 6.4x at the time of last treatment (mean of 7.6 treatments),19 and the EFFECT-Dep trial utilized 6x treatments initially, rising to an average of 9.9x during the treatment course.13 Our multivariable linear model of final dose found that male sex and older age were each independently associated with higher final dose, but diagnostic categories and low initial dose were not significantly associated. This model explains only a minority of the variance in dosing, and highlights as yet unexplained factors affecting dose. Notably, due to FDA limitations on maximum charge output of ECT devices in the United States limit the maximum dose to 576 mC or 7.7x seizure threshold in this sample,20–22 so the higher doses used in some trials are inaccessible to American patients.
Strengths of this study include a large sample size, wide age range of patients, and inclusion of patients with multiple different diagnoses. The single-center nature of the study assures consistency of treatment protocols and personnel but does potentially hinder generalizability to other study sites.
Limitations of the study include its retrospective observational nature without control group, which prevents determination of causality or the relative effectiveness of alternative treatments. As the study period spans 2000–2017, changes in clinical practice during the period are potential confounders. These include differences in referral patterns for ECT, increased used of ultrabrief pulse treatments, changes in pharmacotherapy, and potentially increased fear of cognitive side effects of bilateral treatment, which may have affected willingness to switch. Moreover the decision to use RUL-BP ECT initially as opposed to other treatment parameters was made by the treating physicians, who then also determined dose changes and the need to transition to alternative treatment methods. As a result, unstated clinical factors or cognitive biases on the part of the treatment team may underlie decisions about continuation vs. switching. During the study period the study site maintained different records systems for ECT and other medical records, and as a result we are unable to assess the results of changes in pharmacotherapy or other treatments that may have occurred during the study period. Furthermore, we lack information about the baseline severity of symptoms at time of treatment initiation. As the most severely ill patients may have been more likely to transition from RUL-BP treatments earlier, or even to be treated with bilateral electrode placement from the first treatment and thus excluded from this study population, the generalizability of these findings to the sickest patients may be limited. Additionally, the diagnoses analyzed here are clinical, and not based on structured interviews. This reflects usual clinical practice at most facilities but hinders comparisons to research studies utilizing different diagnostic criteria for study entry.
Conclusion
Among 1,383 patients beginning acute-course treatment using RUL-BP ECT from 2000–2017, mean number of treatments was 9.4±3.1, of which a mean of 7.6±3.3 were utilizing RUL-BP stimuli. More than 60% of patients were treated with RUL-BP exclusively.
Supplementary Material
Acknowledgments
Funding
This work was supported by the National Institute of Mental Health (R25MH094612, JL; R56MH115187 and R01MH120991, THM; 5R01MH112737-03, MEH), the National Institute on Aging (5R01AG061100-02; BPF), and the Brain and Behavior Research Foundation (NARSAD 26489; THM). The sponsors had no role in study design, writing of the report, or data collection, analysis, or interpretation.
Conflicts of Interest
THM receives research funding from the Stanley Center at the Broad Institute, the Brain and Behavior Research Foundation, National Institute of Mental Health, National Human Genome Research Institute Home, and Telefonica Alfa. Dr. Forester receives research support from the National Institute on Aging, Biogen, Lilly, the Rogers Family Foundation, and the Spier Family Foundation. He reports consulting for Biogen. The remaining authors have no disclosures to report.
Contributor Information
James Luccarelli, Department of Psychiatry, Massachusetts General Hospital, Boston, MA; Department of Psychiatry, McLean Hospital, Belmont, MA; Harvard Medical School, Boston, MA.
Thomas H. McCoy, Jr, Department of Psychiatry, Massachusetts General Hospital, Boston, MA; Harvard Medical School, Boston, MA.
Alec P. Shannon, Department of Psychiatry, Massachusetts General Hospital, Boston, MA.
Brent P. Forester, Division of Geriatric Psychiatry, McLean Hospital Harvard Medical School, Boston, MA.
Stephen J. Seiner, Department of Psychiatry, McLean Hospital, Belmont, MA; Harvard Medical School, Boston, MA.
Michael E. Henry, Department of Psychiatry, Massachusetts General Hospital, Boston, MA; Harvard Medical School, Boston, MA.
Bibliography
- 1.Blumberger DM, Seitz DP, Herrmann N, et al. Low medical morbidity and mortality after acute courses of electroconvulsive therapy in a population-based sample. Acta Psychiatr Scand. 2017;136(6):583–593. doi: 10.1111/acps.12815 [DOI] [PubMed] [Google Scholar]
- 2.Tørring N, Sanghani SN, Petrides G, Kellner CH, Østergaard SD. The mortality rate of electroconvulsive therapy: a systematic review and pooled analysis. Acta Psychiatr Scand. 2017;135(5):388–397. doi: 10.1111/acps.12721 [DOI] [PubMed] [Google Scholar]
- 3.Duma A, Maleczek M, Panjikaran B, Herkner H, Karrison T, Nagele P. Major Adverse Cardiac Events and Mortality Associated with Electroconvulsive Therapy: A Systematic Review and Meta-analysis. Anesthesiology. 2019;130(1):83–91. doi: 10.1097/ALN.0000000000002488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luccarelli J, Henry ME, McCoy TH. Quantification of fracture rate during electroconvulsive therapy (ECT) using state-mandated reporting data. Brain Stimul Basic Transl Clin Res Neuromodulation. 2020;13(3):523–524. doi: 10.1016/j.brs.2019.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ross EL, Zivin K, Maixner DF. Cost-effectiveness of Electroconvulsive Therapy vs Pharmacotherapy/Psychotherapy for Treatment-Resistant Depression in the United States. JAMA Psychiatry. 2018;75(7):713–722. doi: 10.1001/jamapsychiatry.2018.0768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Munk-Olsen T, Laursen TM, Videbech P, Mortensen PB, Rosenberg R. All-cause mortality among recipients of electroconvulsive therapy: Register-based cohort study. Br J Psychiatry. 2007;190(5):435–439. doi: 10.1192/bjp.bp.106.026740 [DOI] [PubMed] [Google Scholar]
- 7.Galletly C, Clarke P, Paterson T, Rigby A, Gill S. Practical Considerations in the Use of Ultrabrief ECT in Clinical Practice: J ECT. 2014;30(1):10–14. doi: 10.1097/YCT.0000000000000081 [DOI] [PubMed] [Google Scholar]
- 8.Spaans H-P, H. Kho K, Verwijk E, Kok RM, Stek ML. Efficacy of ultrabrief pulse electroconvulsive therapy for depression: A systematic review. J Affect Disord. 2013;150(3):720–726. doi: 10.1016/j.jad.2013.05.072 [DOI] [PubMed] [Google Scholar]
- 9.Tor P-C, Bautovich A, Wang M-J, Martin D, Harvey SB, Loo C. A Systematic Review and Meta-Analysis of Brief Versus Ultrabrief Right Unilateral Electroconvulsive Therapy for Depression. J Clin Psychiatry. 2015;76(9):e1092–1098. doi: 10.4088/JCP.14r09145 [DOI] [PubMed] [Google Scholar]
- 10.Luccarelli J, McCoy TH, Seiner SJ, Henry ME. Charge required to induce a seizure during initial dose titration using right unilateral brief pulse electroconvulsive therapy. Brain Stimul Basic Transl Clin Res Neuromodulation. 2020;13(6):1504–1506. doi: 10.1016/j.brs.2020.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kellner CH, Knapp RG, Petrides G, et al. Continuation Electroconvulsive Therapy vs Pharmacotherapy for Relapse Prevention in Major Depression: A Multisite Study From the Consortium for Research in Electroconvulsive Therapy (CORE). Arch Gen Psychiatry. 2006;63(12):1337–1344. doi: 10.1001/archpsyc.63.12.1337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kellner CH, Husain MM, Knapp RG, et al. Right Unilateral Ultrabrief Pulse ECT in Geriatric Depression: Phase 1 of the PRIDE Study. Am J Psychiatry. 2016;173(11):1101–1109. doi: 10.1176/appi.ajp.2016.15081101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Semkovska M, Landau S, Dunne R, et al. Bitemporal Versus High-Dose Unilateral Twice-Weekly Electroconvulsive Therapy for Depression (EFFECT-Dep): A Pragmatic, Randomized, Non-Inferiority Trial. Am J Psychiatry. 2016;173(4):408–417. doi: 10.1176/appi.ajp.2015.15030372 [DOI] [PubMed] [Google Scholar]
- 14.Kolshus E, Jelovac A, McLoughlin DM. Bitemporal v. high-dose right unilateral electroconvulsive therapy for depression: a systematic review and meta-analysis of randomized controlled trials. Psychol Med. 2017;47(3):518–530. doi: 10.1017/S0033291716002737 [DOI] [PubMed] [Google Scholar]
- 15.Dierckx B, Heijnen WT, van den Broek WW, Birkenhäger TK. Efficacy of electroconvulsive therapy in bipolar versus unipolar major depression: a meta-analysis. Bipolar Disord. 2012;14(2):146–150. doi: 10.1111/j.1399-5618.2012.00997.x [DOI] [PubMed] [Google Scholar]
- 16.Bahji A, Hawken ER, Sepehry AA, Cabrera CA, Vazquez G. ECT beyond unipolar major depression: systematic review and meta-analysis of electroconvulsive therapy in bipolar depression. Acta Psychiatr Scand. 2019;139(3):214–226. doi: 10.1111/acps.12994 [DOI] [PubMed] [Google Scholar]
- 17.Sackeim HA, Prudic J, Devanand DP, et al. Effects of Stimulus Intensity and Electrode Placement on the Efficacy and Cognitive Effects of Electroconvulsive Therapy. N Engl J Med. 1993;328(12):839–846. doi: 10.1056/NEJM199303253281204 [DOI] [PubMed] [Google Scholar]
- 18.Sackeim HA, Prudic J, Devanand DP, et al. A Prospective, Randomized, Double-blind Comparison of Bilateral and Right Unilateral Electroconvulsive Therapy at Different Stimulus Intensities. Arch Gen Psychiatry. 2000;57(5):425–434. doi: 10.1001/archpsyc.57.5.425 [DOI] [PubMed] [Google Scholar]
- 19.Loo CK, Sainsbury K, Sheehan P, Lyndon B. A comparison of RUL ultrabrief pulse (0.3 ms) ECT and standard RUL ECT. Int J Neuropsychopharmacol. 2008;11(07). doi: 10.1017/S1461145708009292 [DOI] [PubMed] [Google Scholar]
- 20.Sackeim HA. Are ECT Devices Underpowered? Convuls Ther. 1991;7(4):233–236. [PubMed] [Google Scholar]
- 21.Lisanby SHMD, Devanand DPMD, Nobler MSMD, Prudic JMD, Mullen LMD, Sackeim HA. Exceptionally High Seizure Threshold: ECT Device Limitations. Convuls Ther. 1996;12(3):156–164. [PubMed] [Google Scholar]
- 22.Abrams R Electroconvulsive Therapy Requires Higher Dosage Levels: Food and Drug Administration Action Is Required. Arch Gen Psychiatry. 2000;57(5):445–446. doi: 10.1001/archpsyc.57.5.445 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.