Abstract
Background/Purpose
During pandemics like SARS-CoV-2, healthcare providers' well-being and morale are in particular at stake. Burnout may substantially hinder the well-being and morale of healthcare providers, challenging our efforts at disease containment. This study investigated the relationship between perceived COVID-19 stigma and burnout symptoms among physicians and nurses. We further aimed to identify potential factors that may moderate this relationship, including profession, clinical contact with COVID-19 patients, and prior experience with 2003 SARS-CoV-1.
Methods
We used a web-based, structured survey from March 12th to 29th, 2020 to collect cross-sectional, self-reported data. Participants were provided with a link to the survey which took them on average 5-8 minutes. Survey consisted of demographic characteristics, clinical experiences, perceived COVID-19 related stigma, and burnout symptoms. Linear regression with bootstrapping techniques was adopted to test the relations between stigma and burnout, as well as other potential moderators, while adjusting for demographic and clinical factors.
Results
Of the 1421 consented respondents, 357 identified as physicians while 1064 identified as nurses. Participants reported some levels of stigma, and noticeable burnout symptoms. Burnout symptoms were positively correlated with COVID-19 stigma, profession, and currently care for confirmed/suspected COVID-19 patients. The interaction between stigma and profession (Stigma × Nurses) but no other interaction terms reached the significance level, suggesting that the slope for nurses was flatter than the slope for physicians.
Conclusion
The study results suggest that COVID-19 stigma may contribute to burnout among physicians and nurses, and this relation may not vary across clinical roles and experiences but profession.
Keywords: Burnout, COVID-19, Healthcare providers, Pandemics, Social stigma
Introduction
Frontline healthcare providers (HCPs), in particular physicians and nurses who provide care to confirmed or suspected patients with COVID-19, are critical to the containment of the pandemic of SARS-CoV-2. It is imperative for healthcare systems and organizations to support and maintain the well-being and morale of frontline staff during this worldwide crisis.
Burnout may substantially hinder the well-being and morale of HCPs, challenging our efforts at disease containment. Burnout is defined as “prolong occupational stress that presents as emotional exhaustion, depersonalization and diminished personal accomplishment.“ 1 Burnout among healthcare workers has been linked to loss of empathy, poor care quality, medical errors, malpractice risk, impaired job performance, and premature termination of their positions and careers 2, 3, 4; factors which further compromise patient safety and deplete human resources in the time of a pandemic. Additionally, as burnout is associated with medical errors and patient safety incidents, HCPs experiencing burnout may be less likely to comply with safety guidelines,5 , 6 exposing themselves and patients to greater risk of SARS-CoV-2 infection. Given the significance of burnout, there is a growing literature documenting the reported burnout among HCPs during the global pandemic. It is estimated that about 22%–51% of the surveyed HCPs display symptoms of burnout.7, 8, 9, 10, 11, 12
Given the serious implications of burnout among HCPs, studies have identified factors that may positively or negatively impact burnout, ranging from individual characteristics to institutional practices.13 In the COVID-related literature predictors for burnout mainly included demographic backgrounds, work conditions and locations, perceived preparedness, clinical contacts, social support, leaderships in the organizations, among others.7, 8, 9, 10, 11 However, this research largely overlooks stigma and its impact on HCPs’ burnout, with the exception of HIV/AIDS14, 15, 16 and mental health literature.17 , 18 Stigma refers to an “attribute that is deeply discrediting”, connecting specific discernible traits with negative social evaluations and leading to reduced “life chances.“ 19 The mechanisms through which stigma impacts individuals often include public stigma (e.g. cultural norms that devalue certain traits), enacted stigma (e.g. experiences of discrimination), anticipated stigma (e.g. expectations of discrimination) and internalized stigma (e.g. acceptance of negative social evaluations).20 , 21 Indeed, lessons from these fields indicate that healthcare providers who care for patients with mental illness or HIV/AIDS may be stigmatized, which in turn can increase their mental health distress and burnout symptoms. Similarly, stigma has been identified as a risk factor for diminished psychological well-being among frontline health care workers during previous outbreaks of novel viruses.22
While celebrations in honor of COVID-19 frontline health care workers have been widely publicized,23 some HCPs have experienced stigma as a result of their perceived close proximity to the patients and the virus. Reported stigma experiences have included social exclusion24 blockades to their residential buildings,25 denial of housing rentals,26 and physical assault,27 among others. In April 2020 alone, the World Health Organization documented more than 35 COVID-related attacks on HCPs across 11 countries. As a result, some HCPs are advised avoid wearing their uniforms on the street to protect themselves and their families.28 Experience of COVID-19 stigma among healthcare workers may be quite widespread: more than a quarter of 3551 non-healthcare survey respondents in Canada and the U.S. indicated that healthcare providers should have strict restrictions on their freedom,29 and about 8% of 7441 HCPs from 173 countries reported that they or their family members ever experienced COVID-related stigmatization, such as harassment or bullying.30 These experiences of stigma may have important consequences for HCPs’ mental health. Indeed, a recent review summarizing over 200 studies on psychological risks among healthcare prfgoviders has concluded that COVID-related stigma and their experiences of different forms of stigmatization (e.g. victimization, expressed fear, and avoidance) may be linked to their mental well-being.31
To address the pressing issue of HCP burnout and to promote clinician well-being, Dzau, Kirch, and Nasca have proposed a strategy which explicitly includes stigma as a component.32 However, limited evidence exists on the relation between stigma and HCP burnout, thereby limiting efforts to develop psychosocial interventions to serve frontline HCPs during the SARS-CoV-2 pandemic. Therefore, our objective is to study the relationship between burnout symptoms and perceived COVID-19 stigma among a sample of physicians and nurses. We further aim to identify potential factors that may moderate this relationship, including type of profession (physicians vs. nurses), contact with COVID-19 (did not contact any case vs. provided care to suspected cases vs. provided care to confirmed cases), and prior experience with SARS-CoV-1 in 2003 (did not provided care to confirmed cases vs. ever provided care to confirmed cases). We hypothesized that the relationship between burnout and stigma may differ between physicians and nurses because they have different types and levels of contact with the patients. This relationship may also be moderated by their perceived proximity to the virus given their clinical contact with the patients. Finally, this relationship may also differ across HCPs with or without prior similar experiences because those who have experiences with SARS-CoV-1 in 2003 and remained in clinical practice, according to the post-traumatic growth theory, may have developed coping skills to manage COVID-19 related stigma.33 , 34
Methods
Study design and participants
This study protocol was reviewed and approved by the Research Ethics Committee of the National Taiwan Normal University (no. 202003HS002). A cross-sectional, web-based anonymous survey was implemented from March 12th to 29th, 2020, during which the local incident rates remained zero with all confirmed cases imported from abroad. Intentional social distancing acts in this context may be of lower utilities as a daily precaution measure, yet conveying a message that the targeted individuals were considered, and treated, as contaminated.
Snowballing sampling procedures were used to recruit the participants. The study invitations were sent out through e-mails and social networks sites, i.e. Facebook, Line groups of physicians and nurses, to circulate the survey link among HCPs in the hospitals designated as the treatment centres for patients with COVID-19 in Taiwan. The invitation asked the HCP to share their experiences in working in close proximity with COVID-19. The detailed explanations of study purposes and procedures were provided at the front page of our survey. If potential respondents were interested in our study, they can review the debriefing information and consent to the study by clicking the ‘continue’ button to proceed to our survey. When participants anonymously completed the survey, they were encouraged to disseminate the survey link to their professional contacts. The participants were informed that their participation was voluntary, and consent was implied through their completion of the questionnaire. Local experts in the fields of psychology, psychiatry, medicine and public health validated the content of the questionnaire, after which it was pilot tested to determine the psychometric properties of the measurements.
Measures
Demographic factors included age, sex and education (1: high school or below, 2: college, 3: graduate and above). Healthcare provider variables included years of clinical practice, profession (1: physicians, 2: nurses), division (1: Emergency and Internal Medicine, 2: All the others), clinical contact with suspected or confirmed COVID-19 patients (1: did not contact any case, 2: provided care to suspected cases, 3: provided care to confirmed cases), and prior experience with SARS-CoV-1 patients (1: did not provided care to confirmed cases, 2: ever provided care to confirmed cases). Emergency and internal medicine are the most common sources for (or sites of) initial medical care for Taiwanese patients with suspected COVID-19 symptoms.
Burnout was assessed using a single item developed with 5404 primary care providers35 and results showed this assessment had strong psychometric validity and good sensitivity (83.2%) and specificity (87.4%).35 The question asked “Overall, based on your definition of burnout, how would you rate your level of burnout?” The response options had 5 categories, with 1: I enjoy my work. I have no symptoms of burnout, 2: Occasionally I am under stress, and I don't always have as much energy as I once did, but I don't feel burned out, 3: I am definitely burning out and have one or more symptoms of burnout, such as physical and emotional exhaustion, 4: The symptoms of burnout that I'm experiencing won't go away. I think about frustration at work a lot, and 5: I feel completely burned out and often wonder if I can go on. I am at the point where I may need some changes or may need to seek some sort of help. We followed the convention and further dichotomized the responses into 0 (did not burnout, including 1 and 2) and 1 (Burned out, including 3, 4, and 5).8 , 36, 37, 38
Perceived COVID-19 Stigma Items were designed based on the Bogardus Social Distance Scale39 to measure social distance and has been widely used to indicate the stigma associated with psychiatric illness.40 Respondents were asked how willing they perceived others would be to 1) take public transportation with you, 2) shop with you, 3) have a conversation with you, 4) shake hands with you, 5) go out for a meal with you, 6) kiss you, 7) discriminate with crowd out, and 8) do something violent against you, because of their professions and positions in the COVID-19 designed medical centres. Response options included 0: not at all, 1: not likely, 2: I don't know, 3: somewhat likely, and 4: very likely. Item 7 and 8 were reverse coded. A summary score was created that averaged the scores across the eight items. The reliability coefficient (Cronbach's α) was .781.
Statistical analysis
Univariate statistics were employed to gain an overall picture of the sample regarding the distribution of the selected variables. Next, bivariate statistics were applied to compare physicians and nurses in relation to their demographic and clinical characteristics, as well as their levels of stigma and burnout. Finally, logistic regression was used to test the relationship with demographic factors and clinical experiences adjusted between stigma and burnout. The analysis resulted in five statistical models. Model 1 included all the selected variables as main effects. Model 2 included a squared term of stigma to capture potential non-linear relations between stigma and burnout. Model 3 added an interaction term between stigma and profession to estimate the moderating effect of profession on the relationship between stigma and burnout. Model 4, incorporated an additional interaction term to estimate the moderating effect of clinical contact on the relation between stigma and burnout. Finally, Model 5 added an interaction term to estimate the moderating effect of prior clinical experience with SARS-CoV-1 on the relationship between stigma and burnout. Bootstrapping techniques were employed with an additional 3000 samples for statistical inferences. All statistical analyses were conducted in a commercial software package, Stata 16.
Results
Of the 1421 Taiwanese healthcare providers included in the sample, 357 identified as physicians while 1064 identified as nurses. The average age of participants was 36.6 years-old (SD = 8.1). Roughly 82% of the sample was female, and 87% had obtained a bachelor's degree. Participants had an average of 12 years (SD = 7.9) of practice experience; about half of whom worked in emergency and internal medicine departments. Just over 1/3 (35%) of participants had provided care to suspected COVID-19 cases while 4% had provided care to confirmed cases and about 16% had prior experience with the 2003 SARS-CoV-1 outbreak. Participants reported relatively low levels of stigma (mean = 2.0, SD = .6). Noticeably, 41% of the participants reported burnout symptoms. Comparing the two professions, physicians were more likely to be younger, male, with higher levels of educational attainment, and clinical contact with suspected or confirmed COVID-19 cases, but fewer years of practice, and less likely to report burnout. Table I summarizes the univariate and bivariate statistics for this sample.
Table 1.
Characteristics of the sample and bivariate analysis between professions and selected factor.
| All Sample (N = 1421) |
Physicians (N = 357) |
Nurses (N = 1064) |
p | ||||
|---|---|---|---|---|---|---|---|
| Burnout (n, %) | 586 | 41.24 | 110 | 30.81 | 476 | 44.74 | <.001 |
| Stigma (mean, SD) | 2.04 | .62 | 2.08 | .65 | 2.03 | .62 | .188 |
| Demographic Factors | |||||||
| Age (mean, SD) | 36.64 | 8.13 | 38.27 | 8.68 | 36.09 | 7.86 | <.001 |
| Sex (n, %) | <.001 | ||||||
| Male | 262 | 18.44 | 230 | 64.43 | 32 | 3.01 | |
| Female | 1159 | 81.56 | 127 | 35.57 | 1032 | 96.99 | |
| Education (n, %) | <.001 | ||||||
| Below Bachelor Degree | 6 | .42 | 0 | 0 | 6 | .56 | |
| Bachelor Degree | 1237 | 87.05 | 276 | 77.31 | 961 | 90.32 | |
| Graduate Degrees | 178 | 12.53 | 81 | 22.69 | 97 | 9.12 | |
| Clinical Experiences | |||||||
| Years of Services (mean, SD) | 12.68 | 7.89 | 11.38 | 8.00 | 13.12 | 7.81 | <.001 |
| Division (n, %) | .815 | ||||||
| High risk divisions | 685 | 48.21 | 174 | 48.74 | 511 | 48.03 | |
| Others | 736 | 51.79 | 183 | 51.26 | 553 | 51.97 | |
| Clinical Contact (n, %) | <.001 | ||||||
| Never with COVID patients | 861 | 60.59 | 170 | 47.62 | 691 | 64.94 | |
| With suspected cases | 501 | 35.26 | 163 | 45.66 | 338 | 31.77 | |
| With confirmed cases | 59 | 4.15 | 24 | 6.72 | 35 | 3.29 | |
| Prior Experiences with SARS (n, %) | .147 | ||||||
| No | 1187 | 83.53 | 307 | 85.99 | 880 | 82.71 | |
| Yes | 234 | 16.47 | 50 | 14.01 | 184 | 17.29 | |
Table 2 summarizes the results of the linear regression models. Please note, all the estimations were adjusted for the selected covariates in Table 2 . In model 1 stigma (adjusted O.R. = 1.78, 95%CI: 1.53–2.07, p < .001) was associated with burnout symptoms; nurses had higher burnout symptoms than physicians (adjusted O.R. = 2.22, 95%CI: 1.52–3.27, p < .001); and healthcare providers providing care to suspected (adjusted O.R. = 1.76, 95%CI: 1.37–2.25, p < .001) and confirmed (adjusted O.R. = 2.53, 95%CI: 1.39–4.60, p < .001) cases had higher burnout symptoms than those who did not have clinical contact with COVID-19 cases. In model 2, 3, and 4 where an additional interaction term was entered into the model, only the interaction between stigma and profession (Stigma × Nurses) reached the .05 significance level (adjusted O.R. = .68, 95%CI: .47–.98, p < .05), suggesting that the slope for nurses was flatter than the slope for physicians.
Table 2.
Results of logistic regression models with burnout as the outcome (N = 1421).
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|||||
|---|---|---|---|---|---|---|---|---|
| a.O.R. | (95% CI) | a.O.R. | (95% CI) | a.O.R. | (95% CI) | a.O.R. | (95% CI) | |
| Stigma | 1.78∗∗ | (1.53, 2.07) | 2.41∗∗ | (1.73, 3.37) | 1.66∗∗ | (1.36, 2.02) | 1.79∗∗ | (1.51, 2.13) |
| Profession | ||||||||
| Nurses (vs. Physicians) | 2.22∗∗ | (1.52, 3.27) | 4.34∗∗ | (2.02, 9.33) | 2.21∗∗ | (1.50, 3.25) | 2.23∗∗ | (1.52, 3.27) |
| Clinical Contact | ||||||||
| With suspected cases (vs. Never) | 1.76∗∗ | (1.37, 2.25) | 1.78∗∗ | (1.39, 2.29) | 1.50 | (.85, 2.67) | 1.76∗∗ | (1.37, 2.26) |
| With confirmed cases (vs. Never) | 2.53∗∗ | (1.39, 4.60) | 2.50∗∗ | (1.36, 4.57) | .66 | (.12, 3.64) | 2.54∗∗ | (1.40, 4.61) |
| Prior Experiences in SARS | ||||||||
| Yes (vs. No) | 1.03 | (.73, 1.46) | 1.04 | (.74, 1.47) | 1.01 | (.71, 1.44) | 1.10 | (.50, 2.45) |
| Stigma × Profession | ||||||||
| Stigma × Nurses (vs. Physicians) | .68∗ | (.47, .98) | ||||||
| Stigma × Clinical Contact | ||||||||
| Stigma × To suspected cases (vs. Never) | 1.10 | (.79, 1.54) | ||||||
| Stigma × To confirmed cases (vs. Never) | 2.39 | (.74, 7.72) | ||||||
| Stigma × Prior Experiences with SARS | ||||||||
| Stigma × Yes (vs. No) | .96 | (.64, 1.45) | ||||||
All the estimated coefficients were further adjusted for demographic factors and clinical experiences as listed in Table 1; a.O.R.: adjusted Odd Ratio; †p < .10; ∗p < .05; ∗∗p < .01.
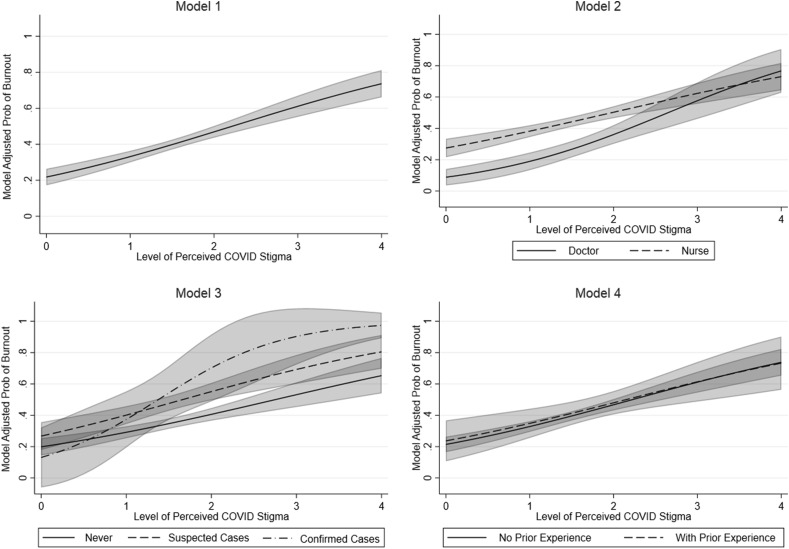
To assist in interpretation, the marginal probabilities of burnout across levels of perceived stigma were computed using the fitted models, as illustrated in Fig. 1 . As shown, the probability of burnout was steadily increased when level of perceived COVID stigma increased in Model 1. In Model 2, nurses displayed higher probability of burnout when stigma was low, yet the increase in burnout probability was steeper among physicians across level of stigma, so that the two professions did not differ in their probability of burnout when stigma level was high. In Model 3, although the healthcare providers who had clinical contact with confirmed cases had a rapid increase in their burnout probability when perceived stigma increased, as the confidence interval was wider the difference in the slopes was not statistically significant.
Figure 1.
Marginal probabilities of burnout across levels of perceived stigma by profession, clinical contact of COVID-19 and prior experiences in SARS.
Discussion
To our knowledge, this is one of the first studies to document the relationship between stigma and burnout among healthcare providers responding to the SARS-CoV-2 pandemic. In this study, stigma was positively associated with burnout symptoms among health care providers. Our data further support that physicians had steeper increase in their burnout when compared with nurses in their response to stigma. However, our data did not support the moderating role of clinical contacts with COVID-19 cases and prior experiences with SARS-CoV-1, in the relationship between stigma and burnout.
Our main study finding, that healthcare provider stigma experiences are correlated with burnout symptoms, is consistent with another study conducted in Italy with a smaller sample size of 273 healthcare providers drawn from a hospital.41 The possibility exists that those healthcare providers who have greater stigma may self-isolate and are less likely to seek out help when they are in need of emotional support to cope with their exhaustion and distress that come with their care duties.16 , 42 Additionally, healthcare providers often require extra psychological resources to manage stigma, leading to further depletion of their already limited mental energy.43 As a consequence, healthcare providers who experience COVID-19 stigma may feel lonely and emotional strained, or burnout, when providing care to patients with or without SARS-CoV-2. Notably, a similar study conducted in Canada found that healthcare providers' stigma can marginally predict their long-term burnout two years after the end of SARS-CoV-1 outbreak.44 Our significant findings on the relation between stigma and burnout may reflect potential immediate effects of stigma on healthcare providers' burnout symptoms at the peak of the early outbreak, which may be overridden later by other factors, such as coping strategies. We also found support for the relationships between burnout symptoms and two other key factors, specifically, profession and providing care to suspected or confirmed cases. These findings are also consistent with other similar studies on HCP's burnout symptoms during the SARS-CoV-2 pandemic. Specifically, HCP who provided care to suspected or confirmed cases displayed higher levels of burnout symptoms as compared with their colleagues who did not involve in direct care delivery.10 , 12 The relationships between burnout symptoms and professions were also documented in different studies, yet the directions remained inconclusive.45, 46, 47
Our data supported the moderating role of profession in the stigma–burnout relationship. More specifically, physicians may display higher sensibility to negative impacts of stigma on their burnout as compared with nurses. Yet, this may also be partly due to the fact that nurses had higher probabilities of burnout even when level of stigma was low, leaving smaller room for increases in burnout as a function of stigma. It is speculated that in Taiwan as nurses enjoy lower occupational prestige as compared with physicians, yet often assume the leadership roles in implementing physicians’ orders and delivering care, nurses may experience higher levels of burnout even in absence of stigma. However, as the result of working in such high demanding environments nurses may develop some coping strategies that may also assist them in managing the impacts of stigma. Our data, however, did not support the moderating role of clinical contact and prior experience with infectious diseases. This suggests that the relationship between health care provider burnout and stigma experiences may not vary greatly by levels of clinical contact, or by prior experience with infectious diseases. However, given the magnitude of the estimated odds ratios and the confidence intervals of the interaction term between stigma and clinical contact, it was also possible that this result may be attributed to insufficient power in our study. At the time of study implementation, there were only 363 confirmed cases of COVID-19 reported in Taiwan, thereby curtailing the available sample of healthcare providers who had provided care to COVID 19 patients. However, as the recent outbreak of COVID-19 in Taiwan (May, 2021) has reached nearly 10,000 cases, more healthcare providers would have clinical contacts with the confirmed cases.
These study results should be interpreted within the contexts of study limitations. First, our sample was drawn from selected medical centers using snowballing techniques, rendering our conclusions not readily generalizable to the overall population of Taiwanese physicians and nurses who have been working on the frontline of the pandemic. Second, we used a cross-sectional, online survey to collect data, which inevitably limits our capacity to identify causal relations between stigma and burnout symptoms. Third, the instrument used in this study can only measure a particular mechanism of stigma, namely, enacted stigma. Future studies should consider following a representative cohort of healthcare providers to obtain a more robust estimate of the impact of stigma on their burnout symptoms over a period of time. A more comprehensive evaluation of stigma experiences may also help to identify how different mechanisms may link to healthcare providers’ burnout symptoms. Nevertheless, this study represents one of the earliest efforts to document the stigma–burnout relation among healthcare providers during the SARS-CoV-2 pandemic.
Clinical implication
During pandemics like SARS-CoV-2, healthcare providers’ well-being and morale are in particular at stake. Healthcare systems and organizations should provide support to prevent their clinical staff from burnout. When providing mental health services to staff members, stigma may be a critical topic to be addressed during the sessions, so that healthcare providers can have opportunities to reflect upon how their COVID-19 stigma may contribute to their sense of burnout, and learn new skills to cope with stigma as well as its negative impact on their well-beings.
Funding
This study was subsidized by the National Taiwan Normal University. The funder plays no role in study design, data collection, analysis, interpretation and in the writing of the report.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
We gratefully appreciate all physicians and nurses who agreed to fill in the survey during the era of pandemic.
References
- 1.Buckley L., Berta W., Cleverley K., Medeiros C., Widger K. What is known about paediatric nurse burnout: a scoping review. Hum Resour Health. 2020;18(1):9. doi: 10.1186/s12960-020-0451-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pospos S., Young I.T., Downs N., Iglewicz A., Depp C., Chen J.Y., et al. Web-based tools and mobile applications to mitigate burnout, depression, and suicidality among healthcare students and professionals: a systematic review. Acad Psychiatr. 2018;42(1):109–120. doi: 10.1007/s40596-017-0868-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Axisa C., Nash L., Kelly P., Willcock S. Burnout and distress in Australian physician trainees: evaluation of a wellbeing workshop. Australas Psychiatr. 2019;27(3):255–261. doi: 10.1177/1039856219833793. [DOI] [PubMed] [Google Scholar]
- 4.Hall L.H., Johnson J., Watt I., Tsipa A., O'Connor D.B. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS One. 2016;11(7) doi: 10.1371/journal.pone.0159015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Gerven E., Vander Elst T., Vandenbroeck S., Dierickx S., Euwema M., Sermeus W., et al. Increased risk of burnout for physicians and nurses involved in a patient safety incident. Med Care. 2016;54(10):937–943. doi: 10.1097/MLR.0000000000000582. [DOI] [PubMed] [Google Scholar]
- 6.Garcia C.L., Abreu L.C., Ramos J.L.S., Castro C.F.D., Smiderle F.R.N., Santos J.A.D., et al. Influence of burnout on patient safety: systematic review and meta-analysis. Medicina (Kaunas). 2019;55(9) doi: 10.3390/medicina55090553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang H.L., Chen R.C., Teo I., Chaudhry I., Heng A.L., Zhuang K.D., et al. A survey of anxiety and burnout in the radiology workforce of a tertiary hospital during the COVID-19 pandemic. J Med Imaging Radiat Oncol. 2021;65(2):139–145. doi: 10.1111/1754-9485.13152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Civantos A.M., Byrnes Y., Chang C., Prasad A., Chorath K., Poonia S.K., et al. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: National study. Head Neck. 2020;42(7):1597–1609. doi: 10.1002/hed.26292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelker H., Yoder K., Musey P., Harris M., Johnson O., Sarmiento E., et al. Prospective study of emergency medicine provider wellness across ten academic and community hospitals during the initial surge of the COVID-19 pandemic. BMC Emerg Med. 2021;21(1):1–12. doi: 10.1186/s12873-021-00425-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galanis P.A., Vraka I., Fragkou D., Bilali A., Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. medRxiv. 2020;77(8):3286–3302. doi: 10.1111/jan.14839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moerdler S, Steinberg DM, Jin Z, Cole PD, Levy AS, Rosenthal SL. Well-being of pediatric hematology oncology providers and staff during the COVID-19 pandemic in the New York and New Jersey epicenter. . JCO Oncology Practice, . 2021(OP-20.). [DOI] [PubMed]
- 12.Magnavita N., Chirico F., Garbarino S., Bragazzi N.L., Santacroce E., Zaffina S. SARS/MERS/SARS-CoV-2 outbreaks and Burnout Syndrome among healthcare workers. An umbrella systematic review. Int J Environ Res Publ Health. 2021;18(8):4361. doi: 10.3390/ijerph18084361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patel R.S., Bachu R., Adikey A., Malik M., Shah M. Factors related to physician burnout and its consequences: a review. Behav Sci. 2018;8(11) doi: 10.3390/bs8110098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hayter M. Burnout and AIDS care-related factors in HIV community clinical nurse specialists in the North of England. J Adv Nurs. 1999;29(4):984–993. doi: 10.1046/j.1365-2648.1999.00973.x. [DOI] [PubMed] [Google Scholar]
- 15.Roomaney R., Steenkamp J., Kagee A. Predictors of burnout among HIV nurses in the Western Cape. Curationis. 2017;40(1):e1–e9. doi: 10.4102/curationis.v40i1.1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ha P.N., Chuc N.T., Hien H.T., Larsson M., Pharris A. HIV-related stigma: impact on healthcare workers in Vietnam. Global Publ Health. 2013;8(Suppl 1):S61–S74. doi: 10.1080/17441692.2013.799217. [DOI] [PubMed] [Google Scholar]
- 17.Verhaeghe M., Bracke P. Associative stigma among mental health professionals: implications for professional and service user well-being. J Health Soc Behav. 2012;53(1):17–32. doi: 10.1177/0022146512439453. [DOI] [PubMed] [Google Scholar]
- 18.Yanos P.T., DeLuca J.S., Salyers M.P., Fischer M.W., Song J., Caro J. Cross-sectional and prospective correlates of associative stigma among mental health service providers. Psychiatr Rehabil J. 2020;43(2):85–90. doi: 10.1037/prj0000378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goffman E. Prentice-Hall; Englewood Cliffs, N.J.: 1963. Stigma: notes on the management of spoiled identity. [Google Scholar]
- 20.Earnshaw V.A., Chaudoir S.R. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scambler G. Re-framing stigma: felt and enacted stigma and challenges to the sociology of chronic and disabling conditions. Soc Theor Health. 2004;2(1):29–46. [Google Scholar]
- 22.Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Verma S., Mythily S., Chan Y.H., Deslypere J.P., Teo E.K., Chong S.A. Post-SARS psychological morbidity and stigma among general practitioners and traditional Chinese medicine practitioners in Singapore. Ann Acad Med Singapore. 2004;33(6):743–748. [PubMed] [Google Scholar]
- 24.Katanuma M., Reynolds I. The Japan Times; 2020. (Children of nurses in Japan excluded from day care over virus fears). 04/25. [Google Scholar]
- 25.Sheridan M.B., Masih N., Cabato R. The Washington Post; 2020. As coronavirus fears grow, doctors and nurses face abuse, attacks. [Google Scholar]
- 26.Amin M. 2020. NSW healthcare workers struggling to keep families safe from coronavirus. ABC.net.au. [Google Scholar]
- 27.Holmes E. 2020. Man attacks nurse on CTA bus after accusing her of trying to spread COVID-19. ABC7chicago.com. April 3, 2020. [Google Scholar]
- 28.Nguyen K. 2020. NSW nurses told not wear scrubs outside of hospital due to abuse over coronavirus fears. ABC.net. Apr. 5, 2020. [Google Scholar]
- 29.Taylor S., Landry C.A., Rachor G.S., Paluszek M.M., Asmundson G.J.G. Fear and avoidance of healthcare workers: an important, under-recognized form of stigmatization during the COVID-19 pandemic. J Anxiety Disord. 2020;75:102289. doi: 10.1016/j.janxdis.2020.102289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dye T.D., Alcantara L., Siddiqi S., Barbosu M., Sharma S., Panko T., et al. Risk of COVID-19-related bullying, harassment and stigma among healthcare workers: an analytical cross-sectional global study. BMJ Open. 2020;10(12) doi: 10.1136/bmjopen-2020-046620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Franklin P., Gkiouleka A. A scoping review of psychosocial risks to health workers during the covid-19 pandemic. Int J Environ Res Publ Health. 2021;18(5) doi: 10.3390/ijerph18052453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dzau V.J., Kirch D., Nasca T. Preventing a parallel pandemic - a national strategy to protect clinicians’ well-being. N Engl J Med. 2020;383:513–515. doi: 10.1056/NEJMp2011027. [DOI] [PubMed] [Google Scholar]
- 33.Chen R., Sun C., Chen J.J., Jen H.J., Kang X.L., Kao C.C., et al. A large-scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID-19 pandemic. Int J Ment Health Nurs. 2021;30(1):102–116. doi: 10.1111/inm.12796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tamiolaki A., Kalaitzaki A.E. That which does not kill us, makes us stronger": COVID-19 and Posttraumatic Growth. Psychiatr Res. 2020;289:113044. doi: 10.1016/j.psychres.2020.113044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dolan E.D., Mohr D., Lempa M., Joos S., Fihn S.D., Nelson K.M., et al. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med. 2015;30(5):582–587. doi: 10.1007/s11606-014-3112-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Waddimba A.C., Nieves M.A., Scribani M., Krupa N., Jenkins P., May J.J. Predictors of burnout among physicians and advanced-practice clinicians in Central New York. J Hosp Adm. 2015;4(6):21–30. [Google Scholar]
- 37.De Marchis E., Knox M., Hessler D., Willard-Grace R., Olayiwola J.N., Peterson L.E., et al. Physician burnout and higher clinic capacity to address patients’ social needs. J Am Board Fam Med. 2019;32(1):69–78. doi: 10.3122/jabfm.2019.01.180104. [DOI] [PubMed] [Google Scholar]
- 38.Wolf C., Schwarz J., Thurstone C., Rylander M. Agreement between a single, self-defined burnout item and the ProQOL burnout subscale for behavioural health staff. Int J Ment Health Nurs. 2021;30(1):326–333. doi: 10.1111/inm.12788. [DOI] [PubMed] [Google Scholar]
- 39.Bogardus E.S. Measurement of personal-group relations. Sociometry. 1947;10(4):306–311. [Google Scholar]
- 40.General Social Survey. NORC at University of Chicago; 1972-2018. https://gss.norc.org/. Accessed the GSS Data Explorer website at gssdataexplorer.norc.org.
- 41.Ramaci T., Barattucci M., Ledda C., Rapisarda V. Social Stigma during COVID-19 and its impact on HCWs outcomes. Sustainability. 2020;12(9):3834. [Google Scholar]
- 42.Sofolahan Y., Airhihenbuwa C., Makofane D., Mashaba E. I have lost sexual interest ..."-challenges of balancing personal and professional lives among nurses caring for people living with HIV and AIDS in Limpopo, South Africa. Int Q Community Health Educ. 2010;31(2):155–169. doi: 10.2190/IQ.31.2.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hatzenbuehler M.L., Phelan J.C., Link B.G. Stigma as a fundamental cause of population health inequalities. Am J Publ Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S., et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chor W.P.D., Ng W.M., Cheng L., Situ W., Chong J.W., Ng L.Y.A., et al. Burnout amongst emergency healthcare workers during the COVID-19 pandemic: a multi-center study. Am J Emerg Med. 2021;46:700–702. doi: 10.1016/j.ajem.2020.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Çelmeçe N., Menekay M. The effect of stress, anxiety and burnout levels of healthcare professionals caring for COVID-19 patients on their quality of life. Front Psychol. 2020;11:3329. doi: 10.3389/fpsyg.2020.597624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Torrente M., Sousa P.A., Sanchez-Ramos A., Pimentao J., Royuela A., Franco F., et al. To burn-out or not to burn-out: a cross-sectional study in healthcare professionals in Spain during COVID-19 pandemic. BMJ Open. 2021;11(2) doi: 10.1136/bmjopen-2020-044945. [DOI] [PMC free article] [PubMed] [Google Scholar]