Abstract
Problem
Birth satisfaction is an important health outcome that is related to postpartum mood, infant caretaking, and future pregnancy intention.
Background
The COVID-19 pandemic profoundly affected antenatal care and intrapartum practices that may reduce birth satisfaction.
Aim
To investigate the extent to which pandemic-related factors predicted lower birth satisfaction.
Methods
2341 women who were recruited prenatally in April–May 2020 and reported a live birth between April–October 2020 were included in the current analysis. Hierarchical linear regression to predict birth satisfaction from well-established predictors of birth satisfaction (step 1) and from pandemic-related factors (step 2) was conducted. Additionally, the indirect associations of pandemic-related stress with birth satisfaction were investigated.
Findings
The first step of the regression explained 35% of variance in birth satisfaction. In the second step, pandemic-related factors explained an additional 3% of variance in birth satisfaction. Maternal stress about feeling unprepared for birth due to the pandemic and restrictions on companions during birth independently predicted lower birth satisfaction beyond the non-pandemic variables. Pandemic-related unpreparedness stress was associated with more medicalized birth and greater incongruence with birth preference, thus also indirectly influencing birth satisfaction through a mediation process.
Discussion
Well-established contributors to birth satisfaction remained potent during the pandemic. In addition, maternal stress and restriction on accompaniment to birth were associated with a small but significant reduction in birth satisfaction.
Conclusion
Study findings suggest that helping women set flexible and reasonable expectations for birth and allowing at least one intrapartum support person can improve birth satisfaction.
Abbreviations: COVID-19, coronavirus 2019; PREPS, Pandemic-Related Pregnancy Stress Scale; WHO, World Health Organization
Keywords: Patient satisfaction, COVID-19 pandemic, Stress, Psychological, Birth experience, Birth preferences, Pandemic-related pregnancy stress
Statement of significance
Problem or issue
The COVID-19 pandemic changed the lives of pregnant women, disrupted antenatal care practices, and affected intrapartum protocols. Yet, the unique contribution of the pandemic to birth satisfaction are unknown.
What is already known
Intrapartum complications, mode and place of birth, unmet birth expectations, positive appraisals, and social support are known contributors to birth satisfaction.
What this paper adds
Maternal stress and restriction on birth companions are associated with a small but significant decrease in birth satisfaction. Stress regarding being unprepared for birth due to the pandemic was associated with birth satisfaction directly and through its association with more medicalized birth and incongruence with birth preference.
1. Introduction
Birth satisfaction has been shown to predict lower risk for disordered postpartum mood, more favourable attitudes toward obstetric care providers, better infant caretaking, and future pregnancy intention. The novel Coronavirus (COVID-19) pandemic has profoundly affected antenatal care and intrapartum practices which may decrease birth satisfaction. Very little is known regarding whether and how pandemic-related restrictions and perception influenced women’s satisfaction with their birth experience. In the current longitudinal study, we investigated the extent to which pandemic-related factors predicted lower birth satisfaction beyond the impact of non-pandemic-related factors.
1.1. Birth satisfaction
Giving birth is a psychologically complex experience influenced by a variety of perceptions. These perceptions can include constructs such as pain, interpersonal communication, emotional responses, fear, and birth satisfaction. Birth satisfaction refers to the overall cognitive appraisal of birth as a fulfilling, positive, and gratifying experience [1]. Birth satisfaction can have profound immediate and long-lasting effects on mothers, families, and society. Evidence suggests that birth dissatisfaction may increase the risk for postpartum mood disorders (e.g., depression, post-traumatic stress) [[2], [3], [4]], mother-infant adjustment difficulties (e.g., maternal caretaking, breastfeeding, bonding) [5], and changes to future fertility plans (e.g., maternal requested caesarean birth, postponing next pregnancy) [6]. Therefore, much research has been conducted in the past decades on identifying contributors to birth satisfaction.
Birth satisfaction has been linked to various sociodemographic, psychological and obstetric factors [7,8]. Sociodemographic factors such as younger age, lack of social support, and belonging to a socially marginalized group (e.g., racial, ethnic, or sexual minoritized identity, financial insecurity) have been linked to more negative birth experiences. Birth related psychological constructs such as optimism and positive appraisals are associated with greater birth satisfaction [9]. By and large, the most frequently studied factors related to birth satisfaction are obstetric factors, mainly birth-related factors. Mode and place of birth as well as their congruence with preferred birth have been linked to birth experience and birth satisfaction. Consistent research documents that women experience out-of-hospital births or community births (i.e., home birth, birth centres) more favourably compared to in-hospital births [10]. Among hospital births, greater amounts of intervention during birth are linked to lower birth satisfaction [11] — women who have unassisted vaginal births report greater levels of birth satisfaction compared to those who have instrumental vaginal births, and unplanned caesarean births are usually rated most negatively compared to other types of birth [12,13]. At the same time, evidence suggests that while mode and place of birth are strong contributors to birth satisfaction, their congruence with birth preferences are equally important [14,15]. Pregnant women often have desires and preferences regarding having a certain mode and type of birth and the extent to which these expectations are fulfilled must be accounted for when examining the contribution of mode and place of birth to birth satisfaction. For example, epidural pain analgesia uptake itself is not as influential to birth satisfaction as the fulfilment of the wish to have a medicated or unmedicated birth [16,17]. Maternal and infant complications during birth such as postpartum haemorrhage, vaginal lacerations, and low Apgar scores have also been found to increase negative appraisals of birth [12,18]. Accompaniment by a supportive person of choice is another intrapartum factor that can improve birth satisfaction [19,20]. Finally, parity is a major contributor to birth satisfaction such that nulliparous women often have lower levels of birth satisfaction than multiparas.
1.2. The COVID-19 pandemic and its impact on pregnant women
In March 2020, COVID-19 was declared a global pandemic by the World Health Organization [21]. The rapid growth in numbers of infected individuals led many nations, including the U.S., to quickly implement restrictive measures to mitigate virus transmission. For pregnant women, these circumstances created an unparalleled confluence of stressors related to social isolation, disruptions to medical care, and potential threats to self and baby. The pandemic greatly affected obstetric care practices as new protocols had to be developed to keep mothers, babies and staff safe [22]. Necessary alterations to antenatal care (e.g., cancellation of appointments, changes to schedules, shifts to telehealth, termination of hospital tours) caused women to feel less prepared for birth and more stressed and anxious [23]. Limiting companions during birth, and forbidding postpartum in-hospital visitations was another cause for concern for birthing mothers who feared they might not get the intrapartum support they desired [24]. At the pandemic onset, expectations regarding birth swiftly changed and uncertainty is likely to have caused great distress since women were concerned about birthing without their loved ones, wearing a mask, or having an obstetric team clad in a hazmat suit [[25], [26], [27]]. Women expressed worries regarding being unprepared for birth due to pandemic-related restrictions which increased the risk of clinically significant anxiety symptoms [28] and unplanned operative deliveries [29]. Pandemic-related restrictions along with concerns regarding perinatal infection led to a possible shift in women’s preferences regarding out-of-hospital births [30,31].
The COVID-19 pandemic undoubtedly changed maternity care practices and affected women’s stress and their expectations of birth, and preliminary evidence suggest it adversely affected birth satisfaction [4]. Recent evidence regarding women’s experiences giving birth during the pandemic implicates the effects of pandemic-related restrictions on birth satisfaction. A recent study from the UK indicates that in the early stages of the pandemic, many women had to change their birth plans including place of birth (from out-of-hospital to in hospital), were not able to have their support persons with them during birth, and were not able to have the mode of birth they desired [32]. Similarly, in Hong Kong, women giving birth in the early pandemic period were not able to have the same levels of intrapartum support or use birthing aids (e.g., birthing ball) compared to the pre-pandemic period [33]. In the U.S., data indicates that women giving birth during the pandemic had higher rates of acute stress and that this stress was subsequently related to higher rates of postpartum post-traumatic stress, overall bonding problems, and breastfeeding problems [34]. In Spain, women who gave birth during the pandemic reported greater levels of stress during childbirth compared to women who gave birth before the pandemic [35]. Further work is needed in order to understand the unique impact of the COVID-19 pandemic on women’s birth satisfaction [36].
1.3. Hypothesis and guiding questions
The purpose of the current study was to investigate the unique effects of pandemic-related factors on birth satisfaction while controlling for non-pandemic-related, established contributors. We hypothesized that non-pandemic-related known contributors to birth satisfaction such as parity, mode and place of birth, incongruence between preferred birth and actual birth, social support, and maternal and infant intrapartum complications would explain much of the variance in birth satisfaction. We aimed to identify the degree to which prenatal pandemic-related perceptions and pandemic-related antenatal and intrapartum practices would contribute to birth satisfaction. Finally, because evidence suggests that pandemic-related unpreparedness stress is associated with higher rates of unplanned operative births [29], we explored mediating processes related to the association between unpreparedness stress and birth satisfaction.
2. Participants, ethics and methods
2.1. Procedure and setting
Data for the current report are from the Stony Brook COVID-19 Pregnancy Experiences (SB-COPE) Study, a longitudinal study on the effects of prenatal stress during the COVID-19 pandemic. In April–May 2020, pregnant women across the U.S. at least 18 years of age were recruited to participate in the SB-COPE Study through targeted Facebook advertisements (95% of participants) and invitations posted on pregnancy-related social media groups and pages (Facebook, Instagram, & Reddit). After reviewing study purposes and requirements and providing informed consent (including providing details on how to be contacted), participants completed an online questionnaire using Qualtrics software. To avoid fraudulent responses, we excluded participants who completed the survey in less than five minutes or who had not completed the entire survey. Participants were entered into a raffle with a 1/100 chance to win a $100 gift card for each completed questionnaire. The SB-COPE Study included follow-ups every 3–4 months to assess stress levels, perinatal, and postpartum outcomes (including reinviting participants who missed a time point). The current report focuses on participants who reported a live birth during a follow-up assessment. The study was approved by the Institutional Review Board of Stony Brook University. Participants’ data were de-identified to ensure confidentiality and stored in password protected computers that were accessible only to study team members who were trained in human subjects protection.
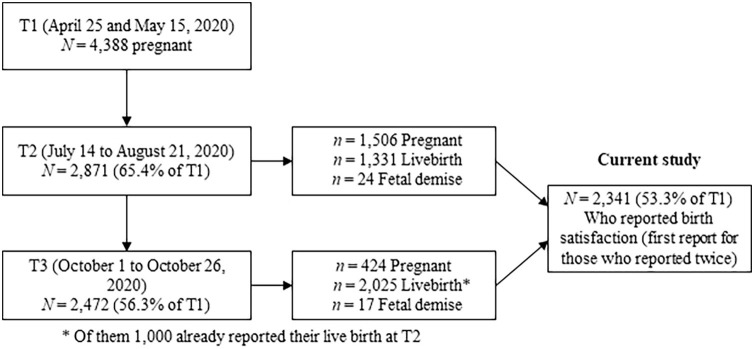
Between April 25 and May 15, 2020 (T1), 4388 pregnant women were enrolled into the SB-COPE Study and completed the study questionnaire. Three months later, follow-up questionnaires were sent to all participants (T2; July 14 to August 21, 2020). Overall, 2871 participants completed T2 surveys, some of whom were still pregnant, some who lost their pregnancy, and some postpartum (65.4% retention rate). Three months after T2, additional follow-up surveys were sent to all participants (T3; October 1 to October 26, 2020). Overall, 2472 participants completed the third study questionnaire, some of whom were still pregnant, some who lost their pregnancy, and some postpartum (56.3% retention rate). The current analysis focuses on 2341 SB-COPE Study participants who reported a live birth at either T2 or T3 (53.3% of the T1 study sample), and excluded those who were still pregnant or that reported a pregnancy loss (Fig. 1 ). The SB-COPE Study was supported by a Stony Brook University Office of the Vice President for Research and Institute for Engineering-Driven Medicine COVID-19 Seed Grant which did not have bearing on the collection of data, its analysis and interpretation, or the approval or disapproval of publication.
Fig. 1.
Participation timepoints and current study sample.
2.2. Measures
Psychosocial factors were assessed at T1 and included Age, Race and Ethnicity, Relationship Status, Financial Status (perceived and grouped as below average vs. average/above average), and Social Support. Women were asked to rate the help or support they received from their partner/spouse and the help or support they received from family and friends on an ordinal scale ranging from 1 = very little to 5 = very much. The score for Social Support was calculated as the average of the ‘partner/spouse’ and ‘family and friends’ items.
Obstetric factors were assessed at T1, T2, and T3 and included Parity, Preterm Birth (based on reported gestational age at birth less than 37 weeks), Place and Mode of Birth, Birth Preference Incongruence, Intrapartum Maternal Complications, and Intrapartum Infant complications. Women were asked about their Place and Mode of Birth with the following options: 1 = emergency caesarean birth (hospital), 2 = planned caesarean birth (hospital), 3 = instrumental birth (hospital), 4 = unassisted vaginal birth with epidural (hospital), 5 = unassisted vaginal birth without epidural (hospital), 6 = unassisted vaginal birth at natural birth centre, and 7 = unassisted vaginal birth at home. Place and Mode of Birth options were reverse coded and used as an ordinal variable ranging from natural to medical based on a previously validated scale [15]. Building on a previously validated measure [15], Birth Preference Incongruence was calculated based on women’s Prenatal Birth Preferences assessed at T1 (which included the same options as Place and Mode of Birth, except for unplanned caesarean birth and instrumental birth) and their Place and Mode of Birth assessed at T2/T3. The absolute value of the gap between Prenatal Birth Preference and Place and Mode of Birth was calculated and ranged from 0 to 6 with greater scores indicating greater Birth Preference Incongruence. Intrapartum Maternal Complications and Intrapartum Infant Complications were reported at T2/T3 (No/Yes).
Pandemic-related prenatal perceptions were assessed at T1 using the Pandemic-Related Prenatal Stress Scale (PREPS) that has been validated in the U.S. and elsewhere [[37], [38], [39], [40]]. The PREPS includes three distinct factors: PREPS-Preparedness, PREPS-Infection, and PREPS-Positive Appraisal. PREPS-Preparedness (pandemic-related unpreparedness stress) measures the extent to which women feel stressed about being unprepared for birth or postpartum due to the pandemic with 7 items such as “I am worried that the pandemic could ruin my birth plans”. PREPS-Infection (pandemic-related perinatal infection stress) refers to concerns related to COVID-19 infection to oneself or the foetus/baby and is comprised of 5 items such as “I am worried that my baby could get COVID-19 at the hospital after birth”. PREPS-Positive Appraisal (pandemic-related positive appraisal) measures the extent to which positive perceptions about pregnancy during the pandemic are helping women cope using 3 items such as “I feel that being pregnant is giving me strength during the pandemic”. Women rate their agreement with the statements on a 1–5 Likert scale. Scores were derived by calculating the average item response. All three PREPS factors were internally consistent with Cronbach’s alphas ranging between 0.69 and 0.85.
Pandemic-related obstetric factors were assessed at T1, T2, and T3. Participants were asked at T1 whether the pandemic has caused Appointment Alterations to their prenatal care (cancellations or appointment change) (No/Yes). Intrapartum Mask Wearing was assessed by asking women if they were required to wear a mask during the birth (No/Yes, some of the time/Yes, all the time). Intrapartum Accompaniment was assessed by asking “Other than medical personnel, who was in the room with you during the delivery?”. The number of different persons was counted and stratified into three ordinal answers: none/one/two or more. Timing of Birth from Pandemic Announcement was a calculation of elapsed weeks between March 10, 2020, when COVID-19 was announced a global pandemic by the World Health Organization [21], and the date of giving birth.
Birth satisfaction was assessed at T2 and T3 using the Childbirth Satisfaction Scale which has been used in various studies in the U.S. and elsewhere and is both reliable and valid [41]. The scale measures women’s subjective general satisfaction with the birth experience using 8 items such as “I am satisfied with the way I delivered”. Women rate their agreement with the statements on a 1–5 Likert scale. Scores were derived by calculating the average item response. The scale was unifactorial and internally consistent with Cronbach’s alphas of 0.95 at both T2 and T3.
2.3. Statistical analysis
First, we used descriptive statistics to present the study sample and the distribution of study variables. Second, we assessed univariate associations between study variables and Birth Satisfaction. To assess the unique contribution of pandemic-related factors to birth satisfaction, we conducted a hierarchical linear regression. In the first step of the regression, we included non-pandemic-related factors hypothesized to predict birth satisfaction and in the second step, pandemic-related factors were added. Finally, we used mediation path analysis to assess the direct and indirect associations of PREPS-Preparedness with Birth Satisfaction via Mode and Place of Birth and Birth Preference Incongruence. Analyses were performed using SPSS 27 and PROCESS Macro for SPSS. p values of <0.05 were considered significant.
Of the 2341 women who reported a live birth at either T2 or T3, 1000 completed the Birth Satisfaction Scale at both T2 and T3. The correlation between the two assessments was r = 0.90, p < 0.001. In order to increase homogeneity of timing, the first assessment was used in analyses if more than one assessment was completed. Missing values of items ranged from 0.0% to 1.5% and were missing completely at random (Little’s MCAR test χ2(158) = 186.99, p = 0.057), therefore, pairwise (univariate) or listwise (multivariate) deletion was used.
3. Results
3.1. Psychosocial and obstetric characteristics
The final study sample included 2341 women who were on average 31.5 ± 4.4 years old and 30.0 ± 6.2 weeks pregnant when they enrolled into the SB-COPE Study (T1; April 25, 2020–May 15, 2020). Additional sample characteristics can be seen in Table 1 . Women gave birth between April 27, 2020 and October 23, 2020 (6–32 weeks from when COVID-19 was announced as a global pandemic). As can be seen in Table 2 , the most common Mode and Place of Birth was unassisted vaginal birth with use of epidural in a hospital (n = 1,093, 46.7%), followed by planned caesarean birth (n = 432, 18.5%). A little over half of the participants gave birth as they had prenatally preferred (n = 1,249, 53.7%) and 40.2% (n = 935) had a more medicalized birth than they preferred with an average Birth Preference Incongruence rating of 0.91 ± 1.24 (Table 2). Close to a quarter of participants reported Intrapartum Maternal Complications during birth (n = 668, 28.5%), a third reported Intrapartum Infant Complications (n = 762, 32.6%), and 7.2% (n = 168) reported Preterm Birth (Table 1). On average, women were moderately satisfied with their births as indicated by the overall mean of 3.72 on a 1–5 scale which corresponds to mostly agreeing with the descriptions of birth as a satisfying experience.
Table 1.
Categorical variables distributions and their associations with Birth Satisfaction (N = 2341).
| n (%) | M ± SD | t/F | ||
|---|---|---|---|---|
| Psychosocial factors | Race/Ethnicity | t = 1.85, p = 0.07 | ||
| Non-Hispanic White | 1985 (84.8) | 3.74 ± 1.04 | ||
| Non-White and/or Hispanic/Latino | 356 (15.2) | 3.63 ± 1.03 | ||
| Relationship Status | t = −2.20, p = 0.03 | |||
| Married or cohabiting | 2205 (94.2) | 3.73 ± 1.04 | ||
| No relationship or serious relationship | 136 (5.8) | 3.53 ± 1.00 | ||
| Financial Status | t = 2.25, p = 0.03 | |||
| Below average | 302 (13.0) | 3.58 ± 1.12 | ||
| Average or Above average | 2038 (87.0) | 3.74 ± 1.02 | ||
| Non-pandemic-related obstetrics factors | Parity | t = 8.61, p < 0.001 | ||
| Nullipara | 1149 (49.1) | 3.53 ± 1.06 | ||
| Multipara | 1192 (50.9) | 3.90 ± 0.98 | ||
| Maternal Complications | t = 19.98, p < 0.001 | |||
| No | 1673 (71.5) | 3.99 ± 0.90 | ||
| Yes | 668 (28.5) | 3.05 ± 1.07 | ||
| Infant Complications | t = 8.22, p < 0.001 | |||
| No | 1579 (67.4) | 3.85 ± 0.99 | ||
| Yes | 762 (32.6) | 3.46 ± 1.09 | ||
| Preterm Birth | t = 5.58, p < 0.001 | |||
| No | 2171 (92.7) | 3.75 ± 1.02 | ||
| Yes | 168 (7.3) | 3.25 ± 1.12 | ||
| Pandemic-related obstetric factors | Appointment Alterations | t = 4.43, p < 0.001 | ||
| No alteration | 1031 (44.0) | 3.83 ± 0.99 | ||
| Yes alteration | 1310 (56.0) | 3.64 ± 1.07 | ||
| Intrapartum Mask Wearing | F = 8.98, p < 0.001 | |||
| No | 1041 (44.5) | 3.82 ± 1.03a | ||
| Yes, some of the time | 805 (34.4) | 3.64 ± 1.04b | ||
| Yes, all of the time | 494 (21.1) | 3.63 ± 1.04b | ||
| Intrapartum Accompaniment | F = 33.55, p < 0.001 | |||
| No one | 50 (2.2) | 2.72 ± 1.19a | ||
| One person | 2152 (91.9) | 3.72 ± 1.02b | ||
| Two or more people | 139 (5.9) | 4.10 ± 0.92c |
Note: different superscript letters indicate mean difference between the groups that were compared in an ANOVA (post hoc Scheffe test p < 0.05).
Table 2.
Birth Preference Incongruence score and frequencies (N = 2325).
 |
Note. An incongruence score was calculated for each participant by computing the absolute value of the difference between their Preferred Birth (T1) and Place and Mode of Birth (T2) [15]. Values of Preferred Birth and Place and Mode of Delivery are indicated in the column and row headers. For example, the score for a woman who planned a home birth (7) and had a vaginal birth with an epidural (4) would be 3 (7−4 = 3). A score for a woman who planned a caesarean birth (2) and had an instrumental vaginal birth (3) would be 1 (2−3=|1|). Scores ranged from 0 to 6 with greater scores indicating greater Birth Preference Incongruence. Bold numbers represent the incongruence score; darker shade represents greater incongruence; numbers in parentheses are the number of women with that combination of Preferred Birth and Place and Mode of Birth.
In univariate analyses examining non-pandemic related factors, nulliparity, having below average Financial Status, and not having a married or cohabiting Relationship Status were associated with lower levels of Birth Satisfaction (Table 1). Greater Social Support was associated with higher levels of Birth Satisfaction (Table 3 ). Maternal and Infant Intrapartum Complication as well as Preterm Birth were associated with lower Birth Satisfaction (Table 1). Greater Birth Preference Incongruence and more medicalized Place and Mode of Birth were also significantly correlated with lower Birth Satisfaction (Table 3).
Table 3.
Central tendencies of continuous variables (means and standard deviations) and their univariate associations (using Pearson’s correlations coefficients) (N = 2341).
| M ± SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 31.5 ± 4.4 | --- | |||||||
| 2. Social Support | 4.23 ± 0.80 | −0.11*** | --- | ||||||
| 3. Place and Mode of Birth (natural-(natural–medical) | 3.49 ± 1.44 | 0.10*** | 0.08*** | --- | |||||
| 4. Birth Preference Incongruence | 0.91 ± 1.24 | −0.02 | 0.05* | 0.64*** | --- | ||||
| 5. PREPS-Preparedness | 3.42 ± 0.84 | −0.13*** | −0.13*** | 0.12*** | 0.11*** | --- | |||
| 6. PREPS-Infection | 3.23 ± 0.97 | −0.02 | −0.07*** | 0.09*** | 0.01 | 0.56*** | --- | ||
| 7. PREPS-Positive Appraisal | 2.23 ± 0.88 | −0.13*** | 0.13*** | 0.02 | 0.07*** | 0.03 | 0.07** | --- | |
| 8. Timing of Birth from Pandemic Start | 16.22 ± 5.98 | 0.27 | 0.02 | 0.02 | 0.05* | −0.00 | 0.04 | 0.07** | --- |
| 9. Birth Satisfaction | 3.72 ± 1.04 | −0.03 | 0.10*** | −0.43*** | −0.49*** | −0.23*** | −0.12** | 0.04 | −0.02 |
Note: PREPS- Pandemic-Related Pregnancy Stress Scale.
p < 0.05.
p < 0.01.
p < 0.001.
3.2. Pandemic related factors and childbirth satisfaction
As can be seen in Table 3 which included Pearson’s Correlations Coefficients, women who were more stressed prenatally about being unprepared for birth (PREPS-Preparedness) and those who reported more stress about perinatal infection (PREPS-Infection) had slightly lower Birth Satisfaction. Pandemic-related pregnancy positive appraisal (PREPS-Positive Appraisal) and Timing of Birth from Pandemic Announcement were not significantly associated with Birth Satisfaction (Table 3).
As can be seen in Table 1, over half of the participants reported Appointment Alterations to their prenatal care due to the pandemic, which was associated with lower Birth Satisfaction. 94.1% of participants did not have more than one person accompany them during the birth and a linear effect of Intrapartum Accompaniment on Birth Satisfaction was observed. The fifty women who had no accompaniment to their birth had significantly lower levels of Birth Satisfaction than other women and Birth Satisfaction for the former group was on average below 3. Over half of the participants reported Intrapartum Mask Wearing some or all of the time during their birth, and these women had significantly lower birth satisfaction than those who did not wear a mask.
3.3. Multivariate modelling
Hierarchical linear regression indicated that non-pandemic related factors explained most of the variance in Birth Satisfaction and the pandemic-related factors explained a small but significant amount of variance beyond non-pandemic factors (Table 4 ). In the first step, below average Financial Status, nulliparity, more medicalized Place and Mode of birth, greater Birth Preference Incongruence, Maternal and Infant Complications, and Preterm Birth uniquely predicted less Birth Satisfaction while greater Social Support uniquely predicted greater Birth Satisfaction. The first step explained 35% of the variance in Birth Satisfaction. In the second step, the added factors explained another 3% of the variance in Birth Satisfaction; greater PREPS-Positive Appraisal and having more companions during birth (Intrapartum Accompaniment) uniquely predicted higher Birth Satisfaction whereas greater PREPS-Preparedness uniquely predicted lower Birth Satisfaction.
Table 4.
Hierarchical linear regression predicting Birth Satisfaction during the COVID-19 pandemic (N = 2290).
| Step 1 |
Step 2 |
|||
|---|---|---|---|---|
| β | 95% CI | β | 95% CI | |
| Age | −0.02 | (−0.01, 0.00) | −0.03 | (−0.02, 0.00) |
| Racial or ethnic minority identity | −0.01 | (−0.14, 0.06) | −0.01 | (−0.13, 0.07) |
| Not married or cohabiting | −0.01 | (−0.20, −0.12) | −0.01 | (−0.18, −0.13) |
| Lower Financial Status | −0.04* | (−0.23, −0.01) | −0.03 | (−0.20, 0.02) |
| Social Support | 0.12*** | (0.12, 0.21) | 0.09*** | (0.07, 0.17) |
| Nulliparity | −0.06** | (−0.19, −0.04) | −0.05** | (−0.18, −0.03) |
| Place and Mode of Birth (natural–medical) | −0.18*** | (0.10, 0.17) | −0.14*** | (0.07, 0.13) |
| Birth Preference Incongruence | −0.27*** | (−0.26, −0.19) | −0.28*** | (−0.27, −0.20) |
| Maternal Complications | −0.24*** | (−0.63, −0.47) | −0.23*** | (−0.61, −0.45) |
| Infant Complications | 0.07*** | (−0.22, −0.07) | 0.06* | (−0.20, −0.05) |
| Preterm Birth | −0.04* | (−0.31, −0.04) | −0.04* | (−0.29, −0.02) |
| PREPS-Preparedness | −0.13*** | (−0.19, −0.10) | ||
| PREPS-Infection | 0.00 | (−0.04, 0.05) | ||
| PREPS-Positive Appraisal | 0.06*** | (0.03, 0.10) | ||
| Appointment Alterations | −0.02 | (−0.11, 0.02) | ||
| Intrapartum Mask Wearing | −0.02 | (−0.11, 0.03) | ||
| Intrapartum Accompaniment | 0.09*** | (0.19, 0.44) | ||
| Timing of Birth from Pandemic Start | −0.01 | (−0.01, 0.00) | ||
| F = 112.16*** | F = 76.90*** | |||
| R2 = 0.35 (ΔR2 = 0.35) | R2 = 0.37 (ΔR2 = 0.03) | |||
Note: PREPS- Pandemic-Related Pregnancy Stress Scale.
p < 0.05.
p < 0.01.
p < 0.001.
3.4. Mediation analyses
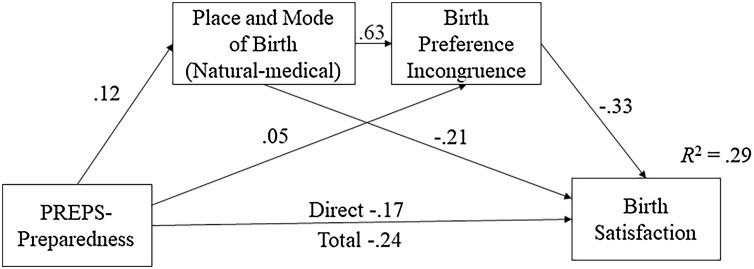
Because PREPS-Preparedness, Place and Mode of Birth, Birth Preference Incongruence, and Birth Satisfaction were all associated, and since previous work indicates that PREPS-Preparedness is associated with higher risk of unplanned operative births [29] (which are by definition incongruent with preferred birth), a path model was explored. As can be seen in Fig. 2 , PREPS-Preparedness was both directly associated with Birth Satisfaction and indirectly associated with Birth Satisfaction via Place and Mode of Birth, which was strongly associated with Birth Preference Incongruence.
Fig. 2.
Direct and indirect associations of PREPS-Preparedness with Birth Satisfaction (N = 2306).
Note: all paths are standardized beta coefficients. All paths were significant at p < 0.05. PREPS- Pandemic-Related Pregnancy Stress Scale.
4. Discussion
The COVID pandemic significantly affected the life of pregnant women, as evident by their increased stress levels partially attributable to restrictions related to intrapartum care [[25], [26], [27]]. To some degree, these have affected how satisfied women are with their birth. While intrapartum events are the major contributors to women’s birth satisfaction, several pandemic-related factors also influenced women’s experience, above and beyond non-pandemic contributors. Prenatal concerns regarding being unprepared for birth due to the pandemic, positive appraisals of pregnancy during the pandemic, and the number of support persons at the birth, were found to be related to levels of birth satisfaction.
Our hypothesis that non-pandemic-related known contributors to birth satisfaction such as nulliparity, mode and place of birth, incongruence between preferred birth and actual birth, social support, and maternal and infant intrapartum complications, would explain much of the variance in birth satisfaction was supported. Previous research on the deleterious emotional impacts of maternal and infant complications and of highly medicalized/ high intervention births were corroborated by our findings [[11], [12], [13]]. Yet, beyond these intrapartum events, the degree to which women’s expectations were met was pivotal to their satisfaction. Birth preferences are often not met due to the unpredictable nature of birth. In the current study, close to half of the participants did not give birth the way they prenatally preferred. While the causes for the incongruence are unknown, it is likely that these high rates of unmet birth expectation were related to the pandemic. During the COVID-19 pandemic, restrictions on intrapartum practices affected women’s ability to access their preferred place and mode of birth and caused alterations to birth preferences [30,31]. Decreased access to alternative pain relief methods such as a birthing ball or water birth, and to home births have recently been documented [33].
Study findings corroborate the importance of social support — prenatally and during birth — to women’s birth satisfaction. Perceived social support has previously been linked with better birth experiences and yet support availability was reduced by the COVID-19 pandemic for many women. One of the frequently reported repercussions of pandemic-related restrictions, especially during the early months of the pandemic where lockdown measures were in place in many U.S. states, was isolation and lack of social support [24,26]. In our study, prenatal perceptions of social support (from partner and family or friends) were positively associated with birth satisfaction.
The number of support persons during birth was also associated with birth satisfaction, even after controlling for other variables. This finding substantiates previous studies on the importance of companions during birth [19]. In an effort to contain the spread of SARS-COV-2, many hospitals restricted the number of companions allowed during birth. These restrictions were some of the main concerns mentioned by pregnant women during the pandemic who feared they would give birth alone or without the persons they were expecting to accompany them [42]. For some women, these fears were realized, as in our study, 50 women had no companion, and 94% had no more than one.
Prenatal perceptions related to pregnancy and the pandemic are unique cognitive constructs that arose because of unprecedented conditions. Among these perceptions, concerns about being unprepared for birth due to the pandemic and positive appraisals about being pregnant during the pandemic, were found to be related to birth satisfaction. Unpreparedness stress, which has previously been linked to higher rates of general anxiety symptoms and greater risk for unplanned emergency births (i.e., instrumental birth and unplanned caesarean birth) [29,43] was both directly and indirectly associated with birth satisfaction. The direct association of unpreparedness stress may be related to women’s self-fulfilling negative perceptions — believing that they are unprepared and therefore more likely to experience and remember what occurred during the birth unfavourably. Unpreparedness stress was also related to having a more medicalized birth and to greater incongruence between preferred and actual birth. Special attention needs to be given to help women feel more prepared for birth during major public health crises such as a pandemic, especially for nulliparae who are more likely to feel unprepared [23].
The association between positive appraisal and birth satisfaction could be attributable to underlying coping skills and personality traits that are known to contribute to greater birth satisfaction [9]. Positive appraisal of pregnancy and the pandemic are likely reflections of optimistic dispositions and adaptive coping mechanisms which are associated with more positive birth experiences [44].
4.1. Limitations
The current study is an in-depth investigation of factors related to birth satisfaction during the COVID-19 pandemic. The study is, however, limited by its reliance on a self-selected cohort that was racially and socioeconomically relatively homogeneous. Volunteer recruitment through social media was necessitated by pandemic-related constraints on in-person research enrolment and it allowed us to recruit a large cohort in a short amount of time. Another sample-related limitation stems from attrition of 46% of participants that could bias the results. While some of the baseline study participants were not included in the current analysis because they had not reported a live birth at T2 or T3 (e.g., they reported pregnancy loss or were still pregnant; Fig. 1), it is possible that some who failed to complete these assessments possessed characteristics associated with birth satisfaction (e.g., pandemic-related stress, social support). In addition, women reported maternal and infant complications whose accuracy cannot be confirmed, and which may have included “perceived” complications (e.g., intermittent fetal heart rate changes) that had no effect on overall labour process or put women or their infant in real danger. Although there is evidence that women have good recollection of birth events [45], future studies should directly measure perinatal outcomes through medical record data extraction and include additional variables that could influence birth satisfaction such as duration of labour. In conclusion, some of these limitations may affect the generalisability of the findings and therefore, additional research in various cultural contexts and study designs is recommended. Finally, more research should be conducted to explore the birth experiences of COVID-19 positive women who likely experienced greater isolation, unmet expectations, and more stress during pregnancy and while giving birth [42,46].
4.2. Clinical implications
Our results have several prenatal, intrapartum, and postpartum clinical implications that could help improve women’s birth satisfaction, during times of pandemic and otherwise. During the prenatal period, providers can help better prepare women for their upcoming birth, particularly first-time mothers. Education regarding the birth process and hospital procedures is likely to benefit women who feel unprepared, especially women who have had alterations to their prenatal care, are unable to go to a hospital tour, or attend a prenatal class [23]. Such preparation could be conducted even with pandemic related restrictions. For example, virtual prenatal education has become increasingly common, and has shown preliminary efficacy in reducing anxiety and fear of birth [47], and virtual hospital tours are available. Increasing preparedness, including encouraging flexibility regarding expectations and modifying birth preferences, will likely help women have the birth they desire and be less dissatisfied if it is not [48]. Women can be specifically educated near their due date regarding what the birth process is expected to be like and the positive features of health and safety precautions. For example, limitations on hospital visitors can be framed as both a means to decrease infection spread and also a chance to recuperate after giving birth and not have to entertain visitors [24]. Our findings regarding the protective qualities of positive appraisal suggest the value of interventions to increase adaptive coping with stress that could be implemented prenatally. Fostering constructive cognitions that focus on the positive aspects of a major life event such as giving birth, even during troublesome times, could increase women’s birth satisfaction and improve their overall well-being.
During birth, special attention needs to be given to women who are unable to have the companionship they desire. When continuous support through the birth by a midwife or companion is not possible or not available, having an in-house support person or doula is likely to improve women’s birth experience [20]. Now more than ever, birth attendants need to be communicative with birthing mothers throughout the labour, with positive language and clear explanations, this can help improve inter-personal communication during birth and reduce misinterpretations of birth events that are not “true complications” as dangerous, thus improving birth satisfaction [49].
After the birth, several practices could improve the birth satisfaction. Encouraging skin-to-skin contact immediately after birth can also moderate the negative effects of operative births on birth satisfaction [50]. Support and council should be offered to women who had adverse events during birth or who had a different birth than preferred, especially since the negative effects of unplanned operative deliveries on birth satisfaction can linger for many years. A recent study found increased incidents of acute stress when comparing COVID-19 positive women who had visitor restrictions and those who did not [42,46]. Therefore, special attention should be given to women who have an infectious condition during birth and might be adversely affected by hospital restrictions.
4.3. Conclusion
Well-established contributors to birth satisfaction including social support and maternal expectations remained relevant and potent during the COVID-19 pandemic. In addition, pandemic-related disruptions to usual antenatal and intrapartum practices created maternal stress and were associated with a small but significant reduction in birth satisfaction. Study findings suggest that allowing at least one intrapartum support person and helping women set flexible and reasonable expectations for birth could improve birth satisfaction during a major public health crisis such as a pandemic and hence protect against adverse consequences of patient dissatisfaction with this pivotal life event.
Ethical statement
The study was approved by the Institutional Review Board at Stony Brook University on April 21, 2020 (#IRB2020-00227).
Funding
Funding for this study was provided by a Stony Brook University Office of the Vice President for Research and Institute for Engineering-Driven Medicine COVID-19 Seed Grant. The funding did not have any role in study design, in the collection, analysis and interpretation of data, in the writing of the report or in the decision to submit the article for publication.
Conflict of interest
Brittain Mahaffey received support from the National Institutes of Health Grant K23HD092888 during preparation of this article. Heidi Preis received support from National Institutes of Health Grant R21DA049827 during preparation of this article. Otherwise, the authors report no conflicts of interest.
CRediT authorship contribution statement
Heidi Preis: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing - original draft. Brittain Mahaffey: Funding acquisition, Investigation, Writing - review & editing. Cassandra Heiselman: Investigation, Writing - review & editing. Marci Lobel: Conceptualization, Funding acquisition, Investigation, Methodology, Supervision, Validation, Writing - review & editing.
Acknowledgments and disclosures
Funding for this study was provided by Stony Brook University Office of the Vice President for Research and Institute for Engineering-Driven Medicine COVID-19 Seed Grant. Brittain Mahaffey received support from NIH Grant K23HD092888 during preparation of this article and Heidi Preis received support from NIH Grant R21DA049827 during preparation of this article. Authors have no other conflicts of interest to disclose.
References
- 1.Karlström A., Nystedt A., Hildingsson I. The meaning of a very positive birth experience: focus groups discussions with women. BMC Pregnancy Childbirth. 2015;15:1–8. doi: 10.1186/s12884-015-0683-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.MacKinnon A.L., Yang L., Feeley N., et al. Birth setting, labour experience, and postpartum psychological distress. Midwifery. 2017;50:110–116. doi: 10.1016/j.midw.2017.03.023. [DOI] [PubMed] [Google Scholar]
- 3.Bell A.F., Andersson E. The birth experience and women’s postnatal depression: a systematic review. Midwifery. 2016;39:112–123. doi: 10.1016/j.midw.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 4.Janevic T., Maru S., Nowlin S., et al. Pandemic birthing: childbirth satisfaction, perceived health care Bias, and postpartum health during the COVID-19 pandemic. Matern. Child Health J. 2021;25:860–869. doi: 10.1007/s10995-021-03158-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bell A.F., Andersson E., Goding K., Vonderheid S.C. The birth experience and maternal caregiving attitudes and behavior: a systematic review. Sex. Reprod. Healthc. 2018;16:67–77. doi: 10.1016/j.srhc.2018.02.007. [DOI] [PubMed] [Google Scholar]
- 6.Preis H., Tovim S., Mor P., et al. Fertility intentions and the way they change following birth-a prospective longitudinal study. BMC Pregnancy Childbirth. 2020;20:1–11. doi: 10.1186/s12884-020-02922-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waldenström U., Hildingsson I., Rubertsson C., Rådestad I. A negative birth experience: prevalence and risk factors in a national sample. Birth. 2004;31:17–27. doi: 10.1111/j.0730-7659.2004.0270.x. [DOI] [PubMed] [Google Scholar]
- 8.Hamm R.F., Srinivas S.K., Levine L.D. Risk factors and racial disparities related to low maternal birth satisfaction with labor induction: a prospective, cohort study. BMC Pregnancy Childbirth. 2019;19:1–9. doi: 10.1186/s12884-019-2658-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Catala P., Peñacoba C., Carmona J., Marin D. Do maternal personality variables influence childbirth satisfaction? A longitudinal study in low-risk pregnancies. Women Health. 2020;60:197–211. doi: 10.1080/03630242.2019.1613473. [DOI] [PubMed] [Google Scholar]
- 10.Overgaard C., Fenger-Grøn M., Sandall J. The impact of birthplace on women’s birth experiences and perceptions of care. Soc. Sci. Med. 2012;74:973–981. doi: 10.1016/j.socscimed.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 11.Çalik K.Y., Karabulutlu Ö, Yavuz C. First do no harm-interventions during labor and maternal satisfaction: a descriptive cross-sectional study. BMC Pregnancy Childbirth. 2018;18:1–10. doi: 10.1186/s12884-018-2054-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Falk M., Nelson M., Blomberg M. The impact of obstetric interventions and complications on women’s satisfaction with childbirth a population based cohort study including 16,000 women. BMC Pregnancy Childbirth. 2019;19:494. doi: 10.1186/s12884-019-2633-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alderdice F., Henderson J., Opondo C., et al. Psychosocial factors that mediate the association between mode of birth and maternal postnatal adjustment: findings from a population-based survey. BMC Womens Health. 2019;19:1–12. doi: 10.1186/s12905-019-0738-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goodman P., Mackey M.C., Tavakoli A.S. Factors related to childbirth satisfaction. J. Adv. Nurs. 2004;46:212–219. doi: 10.1111/j.1365-2648.2003.02981.x. [DOI] [PubMed] [Google Scholar]
- 15.Preis H., Lobel M., Benyamini Y. Between expectancy and experience: testing a model of childbirth satisfaction. Psychol. Women Q. 2019;43:105–117. [Google Scholar]
- 16.Orbach-Zinger S., Landau R., Harousch A.B., et al. The relationship between women’s intention to request a labor epidural analgesia, actually delivering with labor epidural analgesia, and postpartum depression at 6 weeks: a prospective observational study. Anesth. Analg. 2018;126:1590–1597. doi: 10.1213/ANE.0000000000002501. [DOI] [PubMed] [Google Scholar]
- 17.Soliday E., Sayyam J., Tremblay K. Pathways to violated expectations of epidural uptake. J. Reprod. Infant Psychol. 2013;31:413–425. [Google Scholar]
- 18.Briley A.L., Silverio S.A., Singh C., Sandall J., Bewley S. “It’s like a bus, going downhill, without a driver”: a qualitative study of how postpartum haemorrhage is experienced by women, their birth partners, and healthcare professionals. Women Birth. 2021 doi: 10.1016/j.wombi.2020.12.002. (in press) [DOI] [PubMed] [Google Scholar]
- 19.Bruggemann O.M., Parpinelli M.A., Osis M.J.D., Cecatti J.G., Neto A.S.C. Support to woman by a companion of her choice during childbirth: a randomized controlled trial. Reprod. Health. 2007;4:5. doi: 10.1186/1742-4755-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hodnett E.D., Gates S., Hofmeyr G.J., Sakala C. Continuous support for women during childbirth. Issue. Cochrane Database of Systematic Reviews. 2013;(7) doi: 10.1002/14651858.CD003766.pub5. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization . Geneva, Switzerland; 2020. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. [Google Scholar]
- 22.Ross-Davie M., Brodrick A., Randall W., Kerrigan A., McSherry M. Labour and birth. Best Pract. Res. Clin. Obstet. Gynaecol. 2021;73:91–103. doi: 10.1016/j.bpobgyn.2021.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Preis H., Mahaffey B., Heiselman C., Lobel M. Vulnerability and resilience to pandemic-related stress among U.S. women pregnant at the start of the COVID-19 pandemic. Soc. Sci. Med. 2020;266 doi: 10.1016/j.socscimed.2020.113348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vasilevski V., Sweet L., Bradfield Z., et al. Receiving maternity care during the COVID-19 pandemic: experiences of women’s partners and support persons. Women Birth. 2021 doi: 10.1016/j.wombi.2021.04.012. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peahl Af, Powell A., Berlin H., et al. Patient and provider perspectives of a new prenatal care model introduced in response to the coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. 2021;224:381–384. doi: 10.1016/j.ajog.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meaney S., Leitao S., Olander E.K., Pope J., Matvienko-Sikar K. The impact of COVID-19 on pregnant womens’ experiences and perceptions of antenatal maternity care, social support, and stress-reduction strategies. Women Birth. 2021 doi: 10.1016/j.wombi.2021.04.013. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Karavadra B., Stockl A., Prosser-Snelling E., Simpson P., Morris E. Women’s perceptions of COVID-19 and their healthcare experiences: a qualitative thematic analysis of a national survey of pregnant women in the United Kingdom. BMC Pregnancy Childbirth. 2020;20:600. doi: 10.1186/s12884-020-03283-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hessami K., Romanelli C., Chiurazzi M., Cozzolino M. COVID-19 pandemic and maternal mental health: a systematic review and meta-analysis. J. Matern. Neonatal Med. 2021 doi: 10.1080/14767058.2020.1843155. (in press) [DOI] [PubMed] [Google Scholar]
- 29.Preis H., Mahaffey B., Pati S., Heiselman C., Lobel M. Adverse perinatal outcomes predicted by prenatal maternal stress among U.S. women at the COVID-19 pandemic onset. Ann. Behav. Med. 2021;55:179–191. doi: 10.1093/abm/kaab005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Preis H., Mahaffey B., Lobel M. The role of pandemic-related pregnancy stress in preference for community birth during the beginning of the COVID-19 pandemic in the U.S. Birth. 2021;48:242–250. doi: 10.1111/birt.12533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gildner T.E., Thayer Z.M. Maternity care preferences for future pregnancies among United States childbearers: the impacts of COVID-19. Front. Sociol. 2021;6 doi: 10.3389/fsoc.2021.611407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vazquez-Vazquez A., Dib S., Rougeaux E., Wells J.C., Fewtrell M. The impact of the Covid-19 lockdown on the experiences and feeding practices of new mothers in the UK: preliminary data from the COVID-19 New Mum Study. Appetite. 2021;156 doi: 10.1016/j.appet.2020.104985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hui P., Ma G., Seto M.T., Cheung K. Effect of COVID-19 on delivery plans and postnatal depression scores of pregnant women. Hong Kong Med. J. 2020;26:113–117. doi: 10.12809/hkmj208774. [DOI] [PubMed] [Google Scholar]
- 34.Buitelaar J.K., Huizink A.C., Mulder E.J., de Medina P.G.R., Visser G.H.A. Prenatal stress and cognitive development and temperament in infants. Neurobiol. Aging. 2003;24:53–60. doi: 10.1016/s0197-4580(03)00050-2. [DOI] [PubMed] [Google Scholar]
- 35.Mariño‐Narvaez C., Puertas‐Gonzalez J.A., Romero‐Gonzalez B., Peralta‐Ramirez M.I. Giving birth during the COVID‐19 pandemic: the impact on birth satisfaction and postpartum depression. Int. J. Gynecol. Obstet. 2021;153:83–88. doi: 10.1002/ijgo.13565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Berthelot N., Lemieux R., Garon‐Bissonnette J., et al. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstet. Gynecol. Scand. 2020;99:848–855. doi: 10.1111/aogs.13925. [DOI] [PubMed] [Google Scholar]
- 37.Preis H., Mahaffey B., Lobel M. Psychometric properties of the pandemic-related pregnancy stress scale (PREPS) J. Psychosom. Obstet. Gynecol. 2020;41:191–197. doi: 10.1080/0167482X.2020.1801625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schaal N.K., La Marca-Ghaemmaghami P., Preis H., et al. The German version of the pandemic-related pregnancy stress scale: a validation study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021;256:40–45. doi: 10.1016/j.ejogrb.2020.10.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ilska M., Kołodziej-Zaleska A., Brandt-Salmeri A., Preis H., Lobel M. Pandemic-related pregnancy stress assessment–psychometric properties of the Polish PREPS and its relationship with childbirth fear. Midwifery. 2021;96 doi: 10.1016/j.midw.2021.102940. [DOI] [PubMed] [Google Scholar]
- 40.Yirmiya K., Yakirevich-Amir N., Preis H., et al. Women’s depressive symptoms during the COVID-19 pandemic: the role of pregnancy. Int. J. Environ. Res. Public Health. 2021;18:4298. doi: 10.3390/ijerph18084298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Graham J.E., Lobel M., DeLuca R.S. Anger after childbirth: an overlooked reaction to postpartum stressors. Psychol. Women Q. 2002;26:222–233. [Google Scholar]
- 42.Fumagalli S., Ornaghi S., Borrelli S., Vergani P., Nespoli A. The experiences of childbearing women who tested positive to COVID-19 during the pandemic in northern Italy. Women Birth. 2021 doi: 10.1016/j.wombi.2021.01.001. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Preis H., Mahaffey B., Heiselman C., Lobel M. Pandemic-related pregnancy stress and anxiety among women pregnant during the COVID-19 pandemic. Am. J. Obstet. Gynecol. Matern. Fetal Med. 2020;2 doi: 10.1016/j.ajogmf.2020.100155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Handelzalts J.E., Zacks A., Levy S. The association of birth model with resilience variables and birth experience: home versus hospital birth. Midwifery. 2016;36:80–85. doi: 10.1016/j.midw.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 45.Bat-Erdene U., Metcalfe A., McDonald S.W., Tough S.C. Validation of Canadian mothers’ recall of events in labour and delivery with electronic health records. BMC Pregnancy Childbirth. 2013;13 doi: 10.1186/1471-2393-13-S1-S3. S3–S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mayopoulos G.A., Ein-Dor T., Li K.G., Chan J., Dekel S. COVID-19 positivity associated with traumatic stress response to childbirth and no visitors and infant separation in the hospital. Scientific Reports. 2021;11:1–8. doi: 10.1038/s41598-021-92985-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Aksoy Derya Y., Altiparmak S., AkÇa E., GÖkbulut N., Yilmaz A.N. Pregnancy and birth planning during COVID-19: the effects of tele-education offered to pregnant women on prenatal distress and pregnancy-related anxiety. Midwifery. 2021;92 doi: 10.1016/j.midw.2020.102877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Afshar Y., Mei J.Y., Gregory K.D., Kilpatrick S.J., Esakoff T.F. Birth plans—impact on mode of delivery, obstetrical interventions, and birth experience satisfaction: a prospective cohort study. Birth. 2018;45:43–49. doi: 10.1111/birt.12320. [DOI] [PubMed] [Google Scholar]
- 49.Gregory K.D., Korst L.M., Saeb S., et al. Childbirth-specific patient-reported outcomes as predictors of hospital satisfaction. Am. J. Obstet. Gynecol. 2019;220 doi: 10.1016/j.ajog.2018.10.093. 201.e201. [DOI] [PubMed] [Google Scholar]
- 50.Kahalon R., Preis H., Benyamini Y. Who benefits most from skin-to-skin mother-infant contact after birth? Survey findings on skin-to-skin and birth satisfaction by mode of birth. Midwifery. 2021;92 doi: 10.1016/j.midw.2020.102862. [DOI] [PubMed] [Google Scholar]