Abstract
Background: Racial-ethnic disparities in diabetes technology use are well documented in young adults (YA) with type 1 diabetes (T1D), but modifiable targets for intervention still need to be identified. Our objective was to explore YA perspectives on technology access and support in routine clinical care.
Materials and Methods: Participants were YA with T1D of Hispanic or non-Hispanic Black race-ethnicity from pediatric and adult endocrinology clinics in the Bronx, NY. We conducted semistructured individual interviews to explore how health care and personal experiences affected technology use. Interviews were audio-recorded and transcribed for analysis. We used a modified inductive coding approach with two independent coders and iterative coding processes to improve data reliability and validity.
Results: We interviewed 40 YA with T1D: mean age 22 years; 62% female; 72% Medicaid insured; 72% Hispanic; 28% non-Hispanic Black; and mean hemoglobin A1C 10.3%. Themes were categorized into potentially exacerbating and alleviating factors of racial-ethnic disparities in technology use. Exacerbating factors included perceptions that providers were gatekeepers of information and prescription access to technology, providers did not employ shared decision making for use, and YA biases against technology were left unaddressed. Alleviating factors included provider optimism and tailoring of technology benefits to YA needs, and adequate Medicaid insurance coverage.
Conclusions: Our results reveal potential intervention targets at the provider level to increase technology uptake among underrepresented YA with T1D. Diabetes health care providers need to be aware of inadvertent withholding of information and prescription access to technology. Provider approaches that address YA technology concerns and promote shared decision making help to mitigate racial/ethnic disparities in technology use.
Keywords: Continuous glucose monitor, Type 1 diabetes, Young adults, Health care disparities, Insulin pump technology
Introduction
Young adults (YA) (18–25 years of age) belonging to underrepresented racial/ethnic groups are the largest growing population with type 1 diabetes (T1D) in the United States1 and disproportionately suffer from the worst outcomes, including higher rates of hospitalizations and premature death.2 Therapeutic regimens involving diabetes technologies such as insulin pumps and continuous glucose monitors (CGM) decrease hemoglobin A1C (HbA1c) levels among youth and YA with T1D, with potential to positively impact long-term outcomes, including complications and mortality.3–6 Nevertheless, use of technology remains low among YA, especially from underrepresented groups, which may be contributing to long-term inequity in outcomes.7–10
Data from the type 1 diabetes exchange demonstrated that non-Hispanic Black children and adults with T1D use insulin pumps and CGM at 50% of the rate of Whites, regardless of socioeconomic status (SES) and insurance coverage.9,11 More alarming is that use has stagnated or decreased over time despite increased technology options and expanded insurance coverage.9
We found in a national population of YA with T1D that insulin pump and CGM use were fourfold higher in White YA than in Black YA, and twofold higher than in Hispanic YA.7 Moreover, we found that socioeconomic status was not the sole driver of disparities in technology use among YA with T1D, and additional demographic (social position, neighborhood poverty, and health literacy), health care (care setting and clinic attendance), and diabetes self-management (diabetes numeracy, self-monitoring of blood glucose, and adherence) factors also did not explain disparities, especially between Black and White YA.8
While disparities in diabetes technology access and use are well documented, there is very limited understanding of diverse patient experiences with technology access and support in routine clinical care. As with disparities in use of other medications and therapies,12,13 there may be prescribing differences and pervasive negative patient-provider interactions that affect use. For example, several studies have shown that provider bias is associated with less individualized or in-depth conversations with minority versus White patients and facilitated fewer new care plans.14,15 In addition, minority patients disclosed less psychosocial and lifestyle information and asked fewer medical questions of providers who they perceived to be biased.15
On the patient side, given different historical and cultural contexts of people from underrepresented minority groups, there may be unique biases that influence technology use; however, these preferences are largely unknown. There is a critical need for research that elicits the patient perspective in the context of disparities in technology use, including discussions of technology in routine diabetes care and patient-level factors influencing use.
The goal of this study was to explore patient perceptions of access to diabetes technology and influences on decisions to start or continue technology use in Hispanic and non-Hispanic Black YA with T1D. While health care insurance is a considerable barrier to use of diabetes technology among underserved populations with T1D in the United States, we were interested in identifying more modifiable barriers, especially since our prior work shows wide disparities in technology use, despite insurance coverage.8 Examination of patient- and provider-level factors contributing to diabetes technology use from the patient perspective has potential to identify sources of racial/ethnic disparities and define modifiable targets for intervention that curb ongoing inequity in outcomes for underrepresented racial/ethnic groups.
Materials and Methods
This analysis is part of a larger qualitative study conducted to understand the lived experience and health care encounters of YA with T1D from underrepresented racial/ethnic groups. Institutional review board approval was obtained from the Albert Einstein College of Medicine for this study.
Participants and setting
YA participants (18–25 years of age) were recruited from May to December 2019 at the adult and pediatric diabetes centers at the Fleischer Institute for Diabetes and Metabolism at Montefiore Medical Center and Children's Hospital at Montefiore in the Bronx, NY. Participants needed to have had T1D for at least 1 year and could not have had a developmental disability that would have precluded tolerating an in-depth interview. Participants could have been English or Spanish speaking and did not have to be users of diabetes technology. T1D diagnosis was confirmed by medical records during the screening process and by the patient during consent. We did not systematically exclude participants who had not showed to scheduled diabetes visits within the last year.
Procedures
Participants were consented and enrolled either in person or over phone, as per patient preference. We conducted individual semistructured interviews in person or telephonically, in English or Spanish. During interviews, participants were asked to self-report their race-ethnicity using standardized categories from the U.S. Census.16
Interview guides were developed based on prior literature of YA with T1D and clinical expertise of the study team (S.A., G.C.R, and V.M.). Overall interview goals included exploration of lived experiences with T1D in underserved communities, diabetes self-management, and technology experiences. Questions focusing on diabetes technology included the following domains: (1) information access to technology (”Where did you get information on insulin pumps or CGM for type 1 diabetes management?”); (2) health care provider conversations about diabetes technology in the health care encounter (“How did your healthcare provider introduce insulin pump or continuous glucose monitor to you?”); and (3) young adult (YA) factors in decision making to use technology (“What made you decide for or against using an insulin pump or continuous glucose monitor?”).
Coding and analysis
Pilot interviews were conducted for the first two participants to ensure clarity of interview questions, after which the guide was modified once to improve verbiage and include more patient-level questions on perceived influence of race-ethnicity. Pilot interview data were included in the final analysis. Interviews were audio-recorded, transcribed, cleaned, and uploaded into NVivo17 for coding and analysis.
We used a modified inductive coding approach to develop the codebook and analyze the data.18,19 Because data are limited in this area, we used traditional content analysis instead of applying a fixed analytic scheme to the data. The first five transcripts were read several times by G.C.R. and S.A. to identify themes and categories. After discussion, a coding frame was developed between G.C.R, S.A., and V.A.M. and all transcripts were coded by G.C.R., with S.A. independently coding 20% of the sample (n = 8). If new codes emerged, the coding framework was changed and transcripts were re-read using the new coding structure. Through the coding process, categories were gathered from the data, which were further discussed and conceptualized into broader themes. Themes were categorized into potentially exacerbating and alleviating factors of racial/ethnic disparities in diabetes technology use and then further subdivided into provider-, patient-, and system-level factors.
Reliability of data was addressed by the parallel concept of dependability.20–22 Coding discrepancies were resolved by logging and discussing differences among the authors; reasons for the discrepancy were examined, interpretation of data was informed, and analytic procedures were refined. An audit trail of recorded materials, transcripts, meeting minutes, decisions logs, and memos was kept to document how data were generated, coded, analyzed, and interpreted. Toward the end of the study, no new theme emerged, thus indicating that all major themes had been identified and thematic saturation had been achieved.
Results
Sixty-two participants were approached for the study and 53 agreed to participate, resulting in a response rate of 85%. In total, 40 YA participants who self-reported Hispanic or non-Hispanic Black race-ethnicity were interviewed (10 unable to be scheduled after consent; 3 non-Hispanic White YA enrolled and completed the study but were not included in this analysis). There was little difference in response rate by race-ethnicity or sex (responders (n = 40)-Hispanic:NH Black 60:40%; females:males 40:60%; nonresponders (n = 9)-Hispanic:NH Black 40:60%; females:males 43:57%).
Mean age was 21.5 years (±2.2); proportion female was 62% (n = 25); and proportion insured by Medicaid was 72% (n = 29). Proportion Hispanic was 72% (n = 29) and non-Hispanic Black was 28% (n = 11). Mean HbA1c was 10.3% (±2.3%). At the time of interview, 33% (n = 13) were not on technology, 37% (n = 15) were on insulin pump, and 20% (n = 8) were on CGM, and 10% were on insulin pump and CGM (n = 4). Fifty percent of the patients on insulin pump or CGM (n = 14) had been initiated on technology within the past year due to being in a specialized YA T1D clinic.
YA participants described lived and health care experiences with T1D, and barriers and facilitators to adopting and continuing use of diabetes technology. All responses were coded and organized into factors that may exacerbate or alleviate racial-ethnic disparities in technology use (Fig. 1). Responses spanned provider-, patient-, and system-level factors.
FIG. 1.
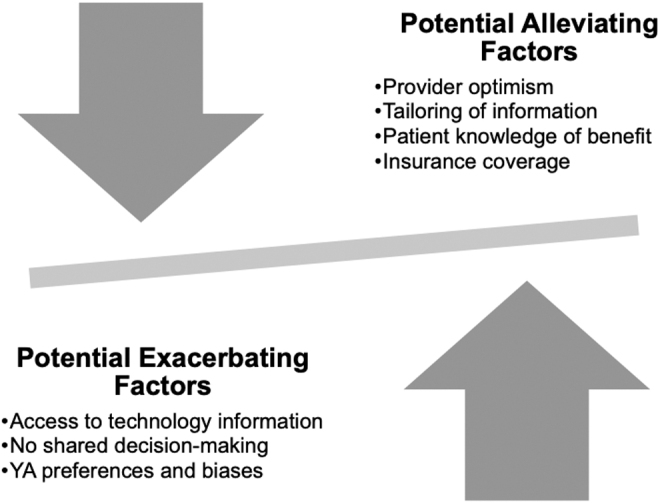
Provider-, patient-, and system-level factors, which potentially exacerbate and alleviate racial-ethnic disparities in diabetes technology use among YA with T1D from underrepresented racial/ethnic groups. T1D, type 1 diabetes; YA, young adults.
Potential exacerbating factors of racial-ethnic disparities in technology use
Provider level
Access to technology information and shared decision making in initiation
Majority of the YA participants stated that the only information they received on technology was from health care providers. Of those who had heard of technology before, most described being told about it, but not being offered it. Participants reported only hearing about insulin pump and CGM technology during the study interview or within the past year of care in a specialized YA T1D clinic, despite having had T1D for more than 10 years.
“I've never had it [insulin pump] mentioned to me or brought up.”
“I've heard about it [CGM] but was never offered until I met with my recent doctor.”
“Yeah. I just got offered that recently when I went to my doctor on Wednesday.
Never before, and I've had it for a year and a half. I didn't know the technology existed.”
Participants explained that health care providers unilaterally decided on technology use for them, for or against use. Many YA described that providers restricted their technology options based on their glycemic control or lack of self-monitoring of blood glucose. In contrast, some YA were told that they had to be on diabetes technology because their blood glucose values were not in range. Overall, YA reiterated that there was an overall lack of detailed discussion about technology options.
“I didn't really have a choice as to why I didn't get it [CGM and insulin pump]. I couldn't have it because my blood sugar was always high.”
“He [the doctor] just said if I was a bit more responsible, if I'm getting my numbers under control, then he would see if I should get the pump or not. But then in my mind I'm like, Wouldn't you want me to get the pump anyway so I can control my diabetes and so my numbers can get better?”
“They just sent it [CGM] to my house. They told me about it, they sent it to my house and like, ‘There's your last resort whether you will accept it or not’.”
Patient level
Regardless of whether YA were given a choice about use of diabetes technology, when asked whether YA would like to use the devices if offered, they described a variety of reasons for preferring not to adopt or continue device use. Some mentioned specific unfavorable experiences they had with technology, while others anticipated issues. Reasons are noted below:
Mistrust in accuracy of technology
“I used it twice [the CGM], and it just never worked with me, like it would tell me my blood sugar was low when it wasn't; it would ring and say it was high, and it was fine…like it wasn't working…So, it just always had problems and became more of a hassle than a help, so I just would stop using them.”
Hassles and alarms
“They had mentioned it [CGM], but I never was interested in it. Because I thought it was just gonna be a lotta work.”
“It stressed me out the fact that I was getting a lot of alerts of my blood sugars every two to three minutes. So, I would much rather stick myself and check my sugar instead of getting so many alerts on my phone, on the meter, and on the pump. It was just too much for me, so I didn't want it [insulin pump and CGM] to continue.”
Interference with daily activities
“I like playing basketball or whatever, I could be swimming, yeah, but if someone knocks it [insulin pump] out, I would have to deal with that.”
Attachment issues
“So, basically, the doctor was telling me that, if I get the pump, I wouldn't have to inject myself. But I would have something attached to my body, and then I would have a monitor attached to that, too. She said it was better than just checking your blood sugar, and taking shots, but I don't want a thing attached to my body.”
Stigma of diabetes
“I was always ashamed of saying I was diabetic when I was a child. When I was a child, I didn't like anyone to know about it. So, in thinking I'd have a pump on me, I would be embarrassed if a person would see it. That's why.”
Potential alleviating factors of racial-ethnic disparities in technology use
While participants mentioned many challenges in obtaining and choosing devices, they also described certain provider approaches and benefits of devices that may have facilitated technology uptake.
Provider level
Health care provider optimism
Participants mentioned that when health care providers communicated with optimism, they became excited about technology and were more willing and open to new technology options.
“The doctor was amazing. She just gave me a lot of hope. The whole process of the machine [CGM] feels exciting to know that there's something out there like that. I wish we had more things to catch our lows and catch our highs before it happens. That's amazing to me. So, having a machine like that is pretty awesome.”
“I was seeing one endocrinologist, and then she passed me on to a different endocrinologist because she had more knowledge about the insulin pump. At the time, I wasn't really taking care of it [my diabetes] as much, so it was kind of hard for her to work with me. So, they passed me on to another endocrinologist. I've really got a good grip on it [my diabetes] with this endocrinologist because she knows more about the pump, but then she's also very understanding about my situation, and she also supports me with trying to work on it and she shows that she believes in me.”
Provider tailoring of information
When health care providers explained and contextualized the benefits of technology to the individual patient's needs, YA were more likely to accept and use technology.
“They just basically told me the benefits of having the insulin pump over the needles that I used to use before then. So, they were pretty much just telling me that it would be a lot easier to just put in the needle once every three days and just monitor my blood sugars and monitor the amount of carbs that are going in rather than using the pen over and over again. And I think that's, more or less, what got me into using the insulin pump.”
“They offered it to me because I don't check my sugars at all. A normal field [for me] is from 200 to 400. I can't tell my body at this point. When I'm at a good level, I [feel] low. When I'm at a high level, I [feel] normal. The doctor told me it would be a good way to really learn and see what my body is really processing and how fast the [blood sugar rises after] foods that I eat. The machine is gonna be able to let me know, “you're eating this; your sugar's going up…give yourself insulin,” or “your sugar's going down.” I'm gonna realize how I really feel…I'm gonna get to learn more about my body at this point.”
Patient level
Patient knowledge of benefits of technology
When patients were knowledgeable about the beneficial aspects of technology, it allowed them to become self-advocates for technology use, in addition to assuming the decision-making role for use.
“I just really want my numbers to go down because I've really been doing bad habits over the years and it's really been destroying my body. So, having constant high blood sugars is not really good for any diabetic and I'm tired of going to the hospital just because I'm going into DKA. So, I think with the CGM, I think I could manage my diabetes a lot better and get back on track before anything tragic happens.”
System level
Medicaid coverage
Finally, the overwhelming majority of participants stated that with Medicaid plan coverage, they had no issues obtaining technology with regard to cost.
“Well, I was grateful enough to have good [Medicaid] insurance that allowed me to get the pump. I know other people that they don't have good insurance or their insurance does not cover the pump, so they have to take the injection needles, which for me, is a big thing…so, if it wasn't for having the good insurance and being able to have the pump, I don't even know what I would be doing because I know for a fact that the injection needles don't work for me.”
Discussion
In this qualitative study with Black and Hispanic YA with T1D, we found that YA perceived health care providers to be the major gatekeeper of access to both information and prescriptions for diabetes technology. Importantly, YA commented on an overall lack of shared decision making with regard to technology initiation, noting that the health care provider decided on use or nonuse for them. YA also had important concerns and biases against technology, which remained unaddressed and influenced decisions on initial use and continuation.
Nevertheless, we found that certain provider approaches alleviated patient-specific barriers to use, including provider optimism and tailoring of benefits of technology to YA needs. We also found in this primarily publicly insured sample that insurance coverage alleviated barriers to use. Our results demonstrate that there may be modifiable targets at the patient-provider level, which can increase uptake of diabetes technology use among underrepresented YA with T1D.
Many participants reported that they were never offered diabetes technology, despite having had T1D for many years. In addition, those who knew about diabetes technology at the time of the interview stated that they had rarely been offered the technology themselves. We found this to be surprising as these YA had interfaced with multiple endocrinologists during their T1D course. Whether these acts of omission of information or unwillingness to offer technology were overt or subconscious cannot be determined in this study. Nor can it be determined whether YA's recall of information from visits may be influenced by the low quality of visits.23 However, multiple studies have shown that well-meaning health care providers have unconscious racial biases,14 making self-awareness an important priority in starting to change provider behavior.
Provider offering of information on the existence of these technologies should be a priority of care at the least, regardless of their own perceptions of patient interests or barriers.24 Implicit bias training has had mixed results in the past, but may be useful.14,25 In addition, empowering YA with knowledge and allowing them to become advocates in their own care support their assumption of independence in diabetes self-management and provide tangible goals of care that could increase engagement. Promotion of diabetes technology may provide new ways to interact with patients and importantly break therapeutic inertia, which is apparent in all diabetes care, especially among patients with longstanding diabetes history and high HbA1c levels, and of racial/ethnic minority.26–28
We also found that even when diabetes technology was offered to YA, they noted a lack of shared decision making for initiation and use. Lack of shared decision making in our sample could be associated with less sustained use of technology, given that YA did not have the option to choose devices that were best for them or have frank discussions about the shortcomings of technology. Our results demonstrated strong YA preferences regarding wearability and utility of technology.
In addition, our data indicate that YA were not prepared for issues related to general hassles or interference with daily activities associated with technology, which could result in issues with initiation or sustained use of technology. YA should be involved in in-depth conversations about technology features and expectations from the beginning to enhance uptake and continued use, with conversations tailored to match the developmental needs of YA. Miller et al. showed that when youth with T1D were involved in the decision process of CGM initiation, they were more likely to have sustained use of CGM, which was mediated by higher reports of self-efficacy.29
Shared decision making is a powerful tool to inform patients of their therapeutic options, make joint care goals, build trust between patients and providers, and empower patients to take ownership of their care.30,31 As a care technique, shared decision making is easily employed and has been shown to improve patient outcomes.29,30,32 Nevertheless, our results demonstrate that YA often do not perceive engagement in shared decision making in the context of diabetes technology. Efforts to emphasize shared decision making in the training of diabetes health care providers and allowances of extra visit time to put skills into practice will be important to affect technology and glycemic outcomes in YA from underrepresented minority groups. Overall, shared decision making can be a potent tool in the care of underrepresented minorities, to equalize inequities in well-established disparities in health care interactions and quality of care received.33
To address patient-level exacerbating factors outside of modifying provider approaches, device companies and health care clinics should provide anticipatory guidance to prospective technology users. Introductory materials and onboarding training are needed, which preemptively address potential device hassles and alarms, provide guidance on CGM accuracy, and offer ways to manage daily activities. Involving and educating a designated support person for YA on technology may also help address hesitation to start or continue devices.
In addition, hiring patient representatives from similar racial/ethnic backgrounds and age groups to interact with YA, who are hesitant to start or continue technology may help address diabetes stigma and device attachment issues, provide creative ways to avoid interference with daily activities, and increase trust in technology. A recent study evaluating a peer mentor program pairing college students with underserved teens with T1D to support mental health and diabetes self-management showed improvement in glycemic control and teen hope for the future.34 Although not directly related to technology, this and other peer-led approaches may be particularly effective for YA with T1D.35–37
Equally important to identifying factors that likely exacerbated disparities in diabetes technology use was identifying factors that may have alleviated disparities. The quality of patient-provider interactions, including health care provider optimism and tailoring of information, was an essential component in promoting YA interest in diabetes technology. YA participants stated that when diabetes technology was discussed by providers with optimistic messages of hope for improvement in glycemic control and quality of life, they were more likely to initiate use. In addition, provider tailoring of the information to their situation and contextualizing the particular benefits of that technology were powerful tools to overcome biases or fears in starting new therapies.
Given how modifiable communication is and how efficiently it can be adopted, health care providers should modify their approaches to introducing technology in a positive way and to offer information about what the technology can specifically do to YA and how it can alter diabetes care and alleviate burden of self-management.38 A recent body of evidence has also shown that improving communication through patient-centered care can improve patient satisfaction, adherence to disease self-management, and outcomes.39,40 Helpful strategies to improve communication quality and outcomes include shared decision making, cultural sensitivity, empathy, spending quality time with patients, and addressing patients' uncertainties about their health.39,41
This study has several limitations. We only included a single center from a geographical area where Medicaid insurance covers diabetes technology, which may not be representative of the general population of YA from underrepresented minority groups. It also could have been relevant to collect insurance data from periods of time before the interview, given insurance coverage lapses during the YA period. Nevertheless, with this study sample, we were able to identify key exacerbating and alleviating factors of disparities in technology use beyond insurance and cost that will continue to be relevant after insurance coverage for these technologies is expanded.
Another limitation of this work is its qualitative and hypothesis-generating nature, which cannot provide conclusive evidence of associations between patient-perceived factors and outcomes. However, our study identified multiple new potential targets for intervention that open new avenues of research where larger and more definitive studies can be performed.
Conclusion
In conclusion, this study identified potential exacerbating and alleviating factors of racial/ethnic disparities in diabetes technology use among Hispanic and Black YA with T1D. The findings underscore the central role that the health care provider plays in information access and prescription of diabetes technology. For YA with T1D, certain provider communication styles such as shared decision making, optimism, and tailoring of information may help overcome perceived barriers to technology use. Health care providers involved in diabetes care need to be aware of their influence on diabetes technology use for YA with T1D.
Equal information access and patient-centered practices regarding diabetes technology should be prioritized, as well as early initiation of goal setting on technology initiation. Further work must be done to assess whether modification of health care provider behaviors to introduce diabetes technology early in the YA patient-provider relationship has potential to increase technology uptake among underrepresented minority groups and curb the continuation of racial/ethnic inequity into adulthood.
Acknowledgments
The authors greatly appreciate the time and insight provided by participants of this study.
Authors' Contributions
S.A. conceptualized the study, analyzed and researched the data, and wrote the article. G.C.R. analyzed the data and reviewed and edited the article. J.A.L. reviewed and edited the article. V.A.M. conceptualized the study, researched the data, contributed to the discussion, and reviewed and edited the article. S.A. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author Disclosure Statement
S.A. has done health care disparities advising for Medtronic.
Funding Information
#K23DK115896 (S.A.) and #P30DK111022 (S.A.)
References
- 1. Pettitt DJ, Talton J, Dabelea D, et al. : Prevalence of diabetes in U.S. Youth in 2009: the SEARCH for diabetes in youth study. Diabetes Care 2014;37:402–408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Saydah S, Imperatore G, Cheng Y, et al. : Disparities in diabetes deaths among children and adolescents—United States, 2000–2014. MMWR Morb Mortal Wkly Rep 2017;66:502–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group, Tamborlane WV, Beck RW, et al. Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med 2008;359:1464–1476 [DOI] [PubMed] [Google Scholar]
- 4. Beck RW, Riddlesworth T, Ruedy K, et al. : Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections the diamond randomized clinical trial. JAMA 2017;317:371–378 [DOI] [PubMed] [Google Scholar]
- 5. Laffel LM, Kanapka LG, Beck RW, et al. : Effect of continuous glucose monitoring on glycemic control in adolescents and young adults with type 1 diabetes: a randomized clinical trial. JAMA 2020;323:2388–2396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pratley RE, Kanapka LG, Rickels MR, et al. : Effect of continuous glucose monitoring on hypoglycemia in older adults with type 1 diabetes: a randomized clinical trial. JAMA 2020;323:2397–2406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Agarwal S, Kanapka LG, Raymond JK, et al. : Racial-ethnic inequity in young adults with type 1 diabetes. J Clin Endocrinol Metab 2020;105:e2960–e2969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Agarwal S, Schechter C, Gonzalez J, Long J: Racial-ethnic disparities in diabetes technology use among young adults with type 1 diabetes. Diabetes Technol Ther Published online 2020:DOI: 10.1089/dia.2020.0338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Foster NC, Beck RW, Miller KM, et al. : State of type 1 diabetes management and outcomes from the T1D exchange in 2016–2018. Diabetes Technol Ther 2019;21:66–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mark A Clements Anke Schwandt Kim C Donaghue Kellee Miller Ursula Lück Jennifer J Couper Nicole Foster Carmen Schröder Helen Phelan David Maahs Nicole Prinz Maria E Craig on behalf of the Australasian Diabetes Data Network (ADDN) Study Group, the T1D Exch and the GD (DPV) initiative. Five heterogeneous HbA1c trajectories from childhood to adulthood in youth with type 1 diabetes from three different continents—a group-based modeling approach. Pediatr Diabetes 2019;20:920–931 [DOI] [PubMed] [Google Scholar]
- 11. Willi S, Miller K, DiMeglio L, et al. : Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics 2015;135:424–434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Johansen ME, Hefner JL, Foraker RE: Antiplatelet and statin use in US patients with coronary artery disease categorized by race/ethnicity and gender, 2003 to 2012. Am J Cardiol 2015;115:1507–1512 [DOI] [PubMed] [Google Scholar]
- 13. Cook BL, Carson NJ, Kafali EN, et al. : Examining psychotropic medication use among youth in the U.S. by race/ethnicity and psychological impairment. Gen Hosp Psychiatry 2011;45:32–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hall WJ, Chapman M V., Lee KM, et al. : Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health 2015;105:e60–e76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lowe C, Beach MC, Roter DL: Individuation and implicit racial bias in genetic counseling communication. Patient Educ Couns 2020;103:804–810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. The United States Census Bureau. The United States Census Bureau: Race. https://www.census.gov/topics/population/race/about.html (accessed April7, 2018)
- 17. QSR International Pty Ltd. (2020) NVivo (released in March 2020), https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- 18. MacQueen KM, McLellan E, Kay K, Milstein B: Codebook development for team-based qualitative analysis. Field Methods 1998;10:31–36 [Google Scholar]
- 19. Thomas DR: A general inductive approach for analyzing qualitative evaluation data. Am J Eval 2006;27:237–246 [Google Scholar]
- 20. Ryan GW, Bernard HR: Techniques to identify themes. Field Methods 2003;15:85–109 [Google Scholar]
- 21. Erlandson DA, Harris EL, Skipper BL, Allen SD: Doing Naturalistic Inquiry: A Guide to Methods. Thousand Oaks, CA: Sage Publications, 1993 [Google Scholar]
- 22. Lincoln YS, Guba EG: Naturalistic Inquiry. Thousand Oaks, CA: Sage Publications, 1995 [Google Scholar]
- 23. Peddecord KM, Wang W, Wang L, et al. : Adolescents' self-reported recall of anticipatory guidance provided during well-visits at nine medical clinics in San Diego, California, 2009–2011. J Adolesc Health 2016;58:267–275 [DOI] [PubMed] [Google Scholar]
- 24. Tanenbaum ML, Adams RN, Lanning MS, et al. : Using cluster analysis to understand clinician readiness to promote continuous glucose monitoring adoption. J Diabetes Sci Technol 2018;12:1108–1115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sukhera H, Michael W, Milne A, et al. : Implicit bias and the feedback paradox: exploring how health professionals engage with feedback while questioning its credibility. Acad Med 2019;94:1204–1210 [DOI] [PubMed] [Google Scholar]
- 26. Gabbay RA, Kendall D, Beebe C, et al. : Addressing therapeutic inertia in 2020 and beyond: a 3-year initiative of the American Diabetes Association. Clin Diabetes 2020;38:371–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cunningham A, Crittendon D, Konys C, et al. : Critical race theory as a lens for examining primary care provider responses to persistently-elevated HbA1c. J Natl Med Assoc 2020;DOI: 10.1016/j.jnma.2020.11.012 [DOI] [PubMed] [Google Scholar]
- 28. Corathers SD, DeSalvo DJ: Therapeutic inertia in pediatric diabetes: challenges to and strategies for overcoming acceptance of the status quo. Diabetes Spectr 2020;33:22–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Miller VA, Xiao R, Slick N, et al. : Youth involvement in the decision to start CGM predicts subsequent CGM use. Diabetes Care 2020;43:2355–2361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Serrano V, Rodriguez-Gutierrez R, Hargraves I, et al. : Shared decision-making in the care of individuals with diabetes. Diabet Med 2016;33:742–751 [DOI] [PubMed] [Google Scholar]
- 31. Funnell MM: Patient empowerment: what does it really mean? Patient Educ Couns 2016;99:1921–1922 [DOI] [PubMed] [Google Scholar]
- 32. Tamhane S, Rodriguez-Gutierrez R, Hargraves I, Montori VM: Shared decision-making in diabetes care. Curr Diab Rep 2015;15:112. [DOI] [PubMed] [Google Scholar]
- 33. Flores G: Technical report—racial and ethnic disparities in the health and health care of children. Pediatrics 2010;125:e979–e1020 [DOI] [PubMed] [Google Scholar]
- 34. Walker AF, Haller MJ, Gurka MJ, et al. : Addressing health disparities in type 1 diabetes through peer mentorship. Pediatr Diabetes 2020;21:120–127 [DOI] [PubMed] [Google Scholar]
- 35. Raymaekers K, Prikken S, Oris L, et al. : A person-centered perspective on the role of peer support and extreme peer orientation in youth with type 1 diabetes: a longitudinal study. Ann Behav Med 2020;54:893–903 [DOI] [PubMed] [Google Scholar]
- 36. Lu Y, Pyatak EA., Peters AL, et al. : Patient perspectives on peer mentoring: type 1 diabetes management in adolescents and young adults. Diabetes Educ 2014;41:59–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wu N, Brazeau A-S, Nakhla M, et al. : Type 1 diabetes mellitus virtual patient network as a peer support community: protocol for social network analysis and content analysis. JMIR Res Protoc 2020;9:e18714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fisher L, Polonsky WH, Hessler D, Potter MB: A practical framework for encouraging and supporting positive behaviour change in diabetes. Diabet Med 2017;34:1658–1666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hagiwara N, Elston Lafata J, Mezuk B, et al. : Detecting implicit racial bias in provider communication behaviors to reduce disparities in healthcare: challenges, solutions, and future directions for provider communication training. Patient Educ Couns 2019;102:1738–1743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pérez-Stable EJ, El-Toukhy S: Communicating with diverse patients: how patient and clinician factors affect disparities. Patient Educ Couns 2018;101:2186–2194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Spooner KK, Salemi JL, Salihu HM, Zoorob RJ: Disparities in perceived patient-provider communication quality in the United States: trends and correlates. Patient Educ Couns 2016;99:844–854 [DOI] [PubMed] [Google Scholar]


