Abstract
Willingness to donate hair samples is a rate-limiting step for assaying antiretroviral (ARV) concentrations in hair, an emerging technique for HIV prevention and treatment monitoring. We surveyed ethnically diverse Nigerians to determine their willingness to donate hair for biomedical research. A cross-sectional survey of people living with HIV on ARV therapy (ART) was conducted at the HIV clinic of Nigerian Institute of Medical Research, using systematic sampling. The researcher-administered questionnaire was designed to capture sociodemographic data, length of time on ART, and willingness to donate hair. Univariate analysis was performed on sociodemographic characteristics, and independent-samples t-test and chi-square tests were used for bivariate analysis. Multivariable logistic regression analysis was performed to assess factors associated with willingness to donate hair samples, with a significance level of 0.05. Of the 398 participants enrolled in the study, 258 (64.8%) were female, the average age was 40 years (±9.8), and the average time spent on ART was 7.3 years (±4.2). More than half (64.8%) of the respondents were willing to donate hair samples for biomedical research and they were 1.5 times more likely to donate hair than blood. For one-third of the participants, the anticipated benefit from the eventual research findings was the primary motivation to donate hair samples. Fear of use of hair for rituals was the most common stated reason for unwillingness to donate hair samples (21.2%). In an ethnically diverse, urban-based Nigerian study population, nearly two-thirds of the participants were willing to donate hair samples for biomedical research. These findings support the feasibility of hair sampling for future HIV clinical research conducted within Nigeria.
Keywords: antiretroviral therapy, acceptability rate, ARV concentration, hair ARV level, hair collection, HIV treatment monitoring, predominantly female
Background
HIV is currently managed as a chronic illness by using antiretroviral therapy (ART) to achieve established treatment matrics.1 The main goal of HIV treatment is to achieve sustained virologic suppression, measured clinically by plasma RNA. Therefore, plasma is the most frequently collected biological sample in laboratory HIV testing. However, due to the expense of performing frequent HIV RNA levels, other methods to assess adherence to ART, such as examining drug levels in urine2 and hair,3 have been explored as alternative lower-cost techniques to predict virologic suppression.
Hair has been used as a biological sample as far back as the early 1970s to 1980s to determine systemic levels of mercury, arsenic, opiates, and trace metals in humans.4–6 Analyzing hair antiretroviral (ARV) concentrations as a predictor of virologic suppression was first reported more than a decade ago.7 This technique of analyzing ARVs in hair is now an evolving field of study that is being used to determine toxicity, exposure, and adherence to ARVs for both HIV prevention and treatment.8–10 Unlike drug levels in blood, urine, or other biological samples that give information over a snapshot of time, hair levels of ARVs can provide information on adherence or exposure over weeks to months.9,11 Hair levels of tenofovir have been established as an inexpensive, easy-to-collect biomarker for measuring adherence to pre-exposure prophylaxis12; concentrations of lopinavir, ritonavir, and efavirenz in the hair of neonates have been linked to in utero transfer of ARVs from maternal consumption to the fetus.13 The ARV hair levels as biomarkers of adherence are strongly associated with ART outcomes, including HIV viral RNA load.8 Finally, in this era of individualized medicine, hair can be a useful sample for pharmacogenomic studies.14
Hair has several advantages over other biological samples used in biomedical research. First, drug is deposited in hair from the systemic circulation over weeks to months, allowing hair levels to serve as metrics of adherence over long periods, compared with 2–4 days with blood or urine.9 Drug levels in hair are more stable than in blood and other biological samples,9 so hair samples can be analyzed for medications or poisons decades later. Moreover, segmental hair analysis allows for the assessment of adherence at various time points over the past months depending on the segment of hair that is analyzed,9,15 for example, analyzing narcotics in sequential segments from the scalp demonstrates the history of narcotic use over time.11 The collection of hair sample is easy, non-invasive, cheap, and does not require use of sterile equipment.11 Hair can be stored for more than 5 years at room temperature.16 Finally, concentrations of ARVs in hair samples collected at home by research participants correlate with samples collected at research study sites.17 With the advantages of hair as a biological sample, hair could be a useful tool for monitoring ART in resource-limited settings such as Nigeria.
Assessments to determine willingness to donate hair samples have been carried out in various settings before collection of hair samples for research. Willingness to donate hair varies widely across different study populations worldwide: An Indian study reported 100% willingness to donate hair samples3; Kenyan and Ugandan studies reported rates of 95% and 84%, respectively18,19; and studies in the United States reported a wide range, from 3.4% to 84.3%,20,21 with improved knowledge about the process being a key factor influencing the willingness of research participants to donate hair samples.
In earlier work by our group, 51.4% of participants from an ethnically homogenous population in southwest Nigeria were willing to donate hair for research.22 To better understand acceptance of this technology, we assessed factors associated with willingness to donate hair and biological samples in a more ethnically diverse and urban-based population of Nigeria.
Methods
Study design, study site, and study population
This was a cross-sectional study design; the study site was the Outpatients HIV Clinic, Nigerian Institute of Medical Research, Lagos. The study population was people living with HIV (PLWH) (≥18 years) and on ART for more than 3 months. Pregnant women and adolescents younger than 18 years were excluded from this study, because their drug pick-up days did not fall within the days of the week for data collection in this study.
Sample size and sampling procedure
A calculated sample size of 398 was determined for assessing a single proportion by using a cross-sectional design.23 An estimated proportion of 51.4% in willingness to donate hair from our earlier study22 was used in the calculation. Assumptions made in the sample size calculation are: 5% precision, 5% type 1 error, and population size <15,000.
Our sampling method was systematic; every fifth patient who arrived at the pharmacy for ARV pick up on Mondays, Tuesdays, and Thursdays were offered enrollment and those who agreed to participate and signed an informed consent were enlisted. The next person on the queue was offered enrollment when the fifth person declined participation. The study period was from November 2019 to January 2020.
Study instrument and data collection
The study instrument was adapted from the questionnaire used in our prior study by Nwogu et al.22 Additions to the questionnaire included length of time on ART, and willingness to donate other biological samples, which included saliva, stool, and urine. The participant's length of time on ART was verified from the pharmacy records. The question on willingness to donate hair required a “yes” or “no” response, whereas the question on other biological samples required the selection of each sample type that respondents were willing to donate for research. There was also a question, where the respondent could indicate the desire to donate none of the listed biological samples, including hair; if the answer to this last question contradicted the response to the initial two questions, it was likely due to misunderstanding and was, therefore, excluded from data analysis. Other questions in the questionnaire provided multiple options, as reasons for the respondent for agreeing or declining to donate hair and other biological samples. The questionnaire was either self-administered by those who could read or administered by research assistants in English, Pidgin English, Yoruba, Ibo, or Hausa, depending on the participant's level of literacy.
Data analysis
Data from the questionnaire were transcribed to a database software, SPSS version 26 (IBM, Chicago, IL) and analyzed. Univariate analysis was performed on sociodemographic characteristics by using descriptive statistics. Independent-sample t tests and chi-square tests were used for bivariate analysis. Logistic regression was performed for a multivariable analysis of factors that influenced willingness to donate hair samples. Significance level was set at 0.05.
Ethics statement
Ethical approval (IRB-19-051) was obtained from the Institutional Review Board (IRB) of the Nigerian Institute of Medical Research. Informed consent was presented in written English language for the literate participants to read and sign before responding to the questionnaire. Informed consent was read out aloud in English language, Pidgin English, Yoruba, Ibo, or Hausa for those participants who could not read.
Results
Sociodemographic characteristics
Overall, 398 participants consented to be enrolled into the study over the study period. More than half of the respondents—258 out of (64.8%)—were female; average age was 40 years (±9.8), and the average time spent on ART was 7.3 years (±4.2). All three major ethnic groups in Nigeria, Hausa, Ibo, and Yoruba, and some minority tribes (Bini, Ibibio, Tiv, etc.) were represented in the sample. Other sociodemographic characteristics of the respondents are shown in Table 1.
Table 1.
Sociodemographic Characteristics of Respondents
| N = 398 | n (%) |
|---|---|
| Sex | |
| Female | 258 (64.8) |
| Male | 140 (35.2) |
| Age | |
| Mean (SD) | 40.9 (9.8) |
| Time on ART (years) | |
| Mean (SD) | 7.33 (4.19) |
| Marital status, N = 396 (100%) | |
| Married | 250 (63.1) |
| Not married | 146 (36.9) |
| Religion | |
| Christianity | 346 (86.9) |
| Islam | 52 (13.1) |
| Education, N = 394 (100%) | |
| <Tertiary | 214 (54.3) |
| ≥Tertiary | 180 (45.7) |
| Ethnicity, N = 397(100%) | |
| Hausa | 25 (6.3) |
| Ibo | 180 (45.3) |
| Yoruba | 123 (31.0) |
| Idoma/Igala/Tiv | 16 (4.0) |
| Edo/Delta | 23 (5.8) |
| Ibibio/Efik | 28 (7.1) |
| Non-Nigerian | 2 (0.5) |
ART, antiretroviral therapy; SD, standard deviation.
Willingness to donate hair and other biological samples
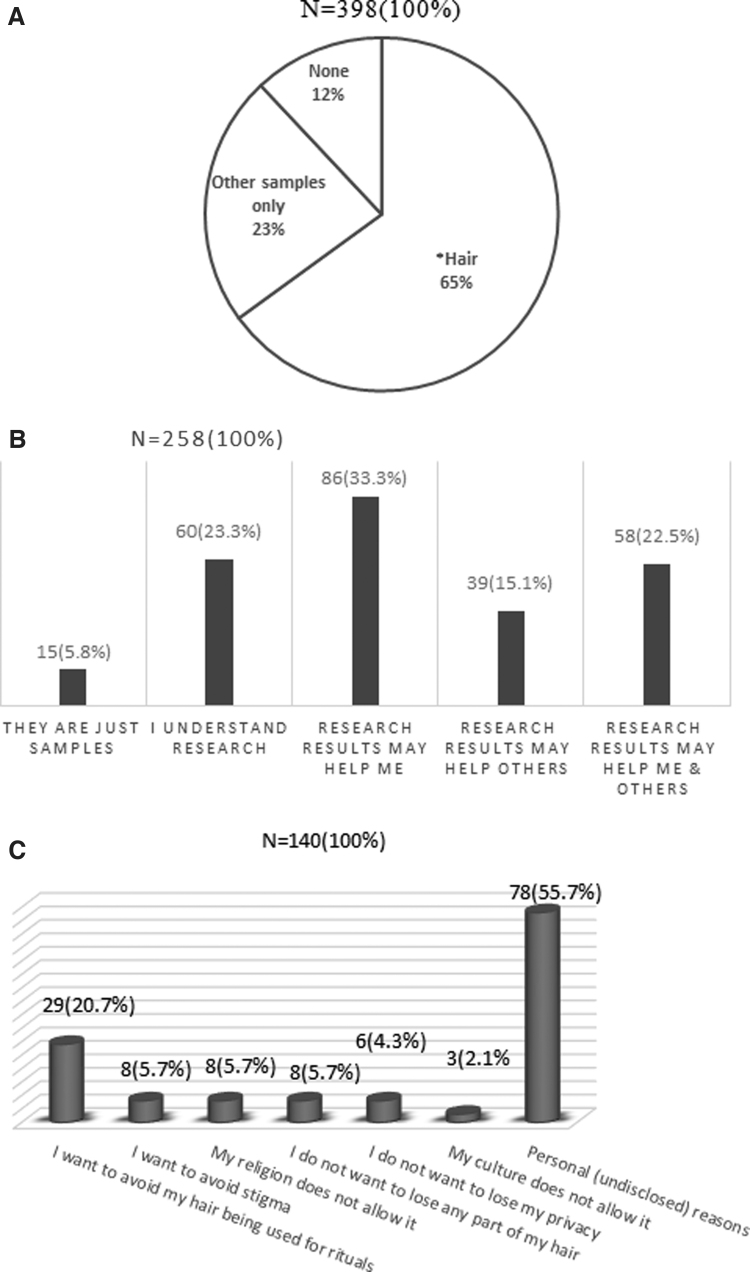
Overall, 258 (64.8%) respondents in this study were willing to donate hair samples for biomedical research. On an average, respondents in this study were 1.5 times more likely to donate hair than blood, urine, saliva, or stool for research (p < .001). A minority of individuals, specifically 48 (12%), indicated unwillingness to donate any of the listed biological samples; the majority, 350 (88%), expressed willingness to donate at least one biological sample for research (Fig. 1A).
FIG. 1.
(A) Willingness to donate biological samples for research. *121 (47%) of those who will donate hair, will also donate at least one other biological samples. (B) Reasons for willingness to donate hair for biomedical research. (C) Reasons for unwillingness to donate hair for research.
Motivation and factors associated with willingness to donate hair samples for biomedical research
Anticipated benefits from eventual research findings were the motivation for a third of the respondents, 86 (33%), to donate hair samples for research (Fig. 1B). In bivariate analyses, factors that were statistically significantly associated with willingness to donate hair for research included having a tertiary (university) education or higher, being on ART for >6 years, and willingness to donate at least one biological sample (Table 2). These statistically significant variables at bivariate analyses were pooled together in a logistic regression model for multivariable analysis.
Table 2.
Factors Associated with Participants' Willingness to Donate Hair Samples for Biomedical Research
| Cross-tabulation |
Logistic regression |
||||
|---|---|---|---|---|---|
| Independent variables | Willingness to donate hair | p | Exp (B) | 95% CI for Exp(B) | p |
| Gender | .779 | ||||
| Female | 166 | ||||
| Male | 92 | ||||
| Age (years) | .085 | ||||
| ≤30 | 42 | ||||
| 31–40 | 79 | ||||
| 41–50 | 99 | ||||
| ≥51 | 38 | ||||
| Religion | .688 | ||||
| Christianity | 223 | ||||
| Islam | 35 | ||||
| Education | .006* | 0.658 | 0.475–0.910 | .012* | |
| ≤Primary | 25 | ||||
| Secondary | 99 | ||||
| ≥Tertiary | 131 | ||||
| Marital status | .141 | ||||
| Married | 169 | ||||
| Not married | 88 | ||||
| Time on ART (years) | .045* | 0.578 | 0.343–0.975 | .040* | |
| <6 | 67 | ||||
| ≥6 | 178 | ||||
| Willingness to donate at least one biological sample | <.001* | 6.332 | 3.086–12.992 | <.001* | |
| No | 22 | ||||
| Yes | 219 | ||||
Statistically significant p values.
The best fit logistic regression model was obtained by including marital status, religion, and age to the earlier mentioned three factors as independent variables, and “willingness to donate hair sample for biomedical research” as the dependent variable. The logistic regression model was statistically significant, χ2 (6) = 44.920, p < .001. Three independent variables—education (p = .012), time on ART (p = .040), and willingness to donate at least one biological sample (p < .001)—contributed significantly to the model.
Reasons for unwillingness to donate hair samples for research
Out of the 137 participants who provided reasons for unwillingness to donate hair samples, 75 (54.7%) indicated personal reasons, whereas 29 (21.1%) wanted to “avoid their hair being used for rituals.” Other reasons given are shown in Figure 1C.
Discussion
Our study indicates that nearly two-thirds of PLWH in an urban center in Nigeria are willing to donate hair samples for biomedical research. Since hair samples can assess ART adherence over time, it may be measured in between HIV RNA levels as an adherence matrix and can be analyzed in laboratories in low-income settings.3 This high acceptability of hair collection could, therefore, help in treatment monitoring in the setting.
The proportion of PLWH willing to donate hair samples for HIV research in our study (64.8%) was higher than that reported from an earlier study conducted by our group in Ibadan, Nigeria, where a 51.3% willingness was reported.22 Respondents in this current study are more ethnically diverse and are residing in a more urban environment, which could explain the difference. Of note, 65% of our sample was female, which was representative of the clinic population, thereby increasing generalizability.24 Though this study was conducted in Southwest Nigeria, only 31% of respondents were Yoruba, the major tribe in Southwest Nigeria, unlike the Ibadan-based study where 79.5% of participants were Yoruba. The Igbo and other tribes of Southern Nigeria, which make up 52% of the Nigerian population,25 constitute 62% of our study population. Another likely reason for the difference in proportions between both studies could be that participants in our study are more exposed to biomedical research. The HIV Treatment Center at the Nigerian Institute of Medical Research, the site for this study, was established in 2002 as a clinical research center for the National HIV Treatment Programme,26 resulting in the conduct of multiple research studies involving PLWH since its establishment. The rate reported in our study is, however, lower than the rates reported from India, Kenya, and Uganda.3,18,19 Higher rates in these studies could be explained by the participants' active involvement in existing research, whereas in our study, the survey was administered in anticipation of a future study.
Anticipated personal benefit from the research was the primary motivation to donate hair in this study. These findings are consistent with a report by Goldenberg et al., which showed that a potential benefit to an ethnic group was a factor associated with the decision to donate samples for genetic research.27,28
Several reports show a significant association between education or knowledge and willingness to donate human biological samples or solid organs.29–33 Educational interventions have been reported to significantly improve willingness to donate biological samples.34,35 This study reports a significant association between higher (tertiary) level of education and willingness to donate hair. Although other studies also reported similar findings,22,27 this stands in contrast to our earlier work in Ibadan, Nigeria22 where less educated participants were more willing to donate hair. This discrepancy could be attributed to their understanding of the processes and benefit of research, as reported by Babatunde et al.27 where participants who were health care professionals (with tertiary education) were well versed in the research and willing to donate biological samples. Moreover, pharmacy records showed that the mean time on ART by participants in this study was 7 years, and 69% of those willing to donate hair had been on ART for at least 6 years. Those willing to donate hair may, therefore, have been more familiar with the medical system compared with those who were not, which could have generated trust.
Respondents in this study were more willing to donate hair than blood, urine, saliva, and stool; this finding is consistent with a report from a South African qualitative study, where participants indicated preference to donate hair compared with blood, due to the fear of pain from phlebotomy required in collecting blood specimens.36 Fear of their cut hair being used in rituals was the highest stated reason for unwillingness to donate hair. African cultural views and superstitious beliefs about hair are likely to play into reduced acceptability in certain African populations for hair donation.22,37
Study limitations and strengths
Our study has some limitations. The factors associated with willingness to donate other biological samples were not studied; the inclusion of these factors to future studies may provide better insight into the factors influencing willingness to donate hair for research compared with other biological samples. Moreover, asking participants about their intent to donate biological samples is not the same thing as assessing acceptability of actual hair collection in an ongoing study. An additional limitation is that those who came to the clinic to be offered study participation might inherently be more adherent to care. Therefore, our findings are limited to those who are in care and not poorly adherent and out of care.
In terms of strengths, this survey was conducted in an ethnically diverse Nigerian population of PLWH. Though Yoruba is the major ethnic group in Lagos, South-west Nigeria, most participants in this study had ethnic origins from other regions of South Nigeria, making the study generalizable across urban regions and southern Nigeria. The participants in this survey were predominantly female (64.8%), which is a true representation of the clinic population (66% female), and in contrast to the low female representation (19.2%) in many other HIV clinical studies, as reported in a systematic review by Curno et al.24
Conclusion
In conclusion, our research shows that nearly two-thirds of PLWH in an ethnically diverse, urban center in Nigeria were willing to donate hair samples for biomedical research. Our study population was predominantly female and ART-experienced, generalizable to the PLWH in the region. The implication of our findings is that studies involving hair collection for ARV monitoring in both HIV treatment and prevention should be feasible to conduct in Nigeria.
Acknowledgments
The authors acknowledge the counselors, pharmacists, and physicians at the Nigerian Institute of Medical Research who assisted in the project. They thank the H.O.D, Clinical Sciences Department, and the Director-General, Nigerian Institute of Medical Research for their support. They also acknowledge Ms. Hannah Nicol for reviewing the article for English Language structure.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Authors' Contributions
All listed authors contributed significantly to the conception, design, data acquisition, data analysis and interpretation, article drafting, article revision for intellectual and technical content, and approval of the final version. All authors agree to be accountable for all aspects of the work.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
Research training for this publication is supported by the Fogarty International Center of the National Institutes of Health under Award no. D43TW010934 for E.C.H. and D43TW009608 for J.N.N. Further support comes from NIAID/NIH 2RO1AI098472 (M.G.) and 5K23-AI124913 (C.D.L.).
References
- 1. World Health Organization (WHO): Consolidated Guidelines on the Use of Antiretroviral Drugs for Treatment and Prevention of HIV Infection. Recommendation for a Public Health Approach-Second edition. Available at apps.who.int/iris/bitstream/handle/10665/10665/208825/9789241549684_eng.pdf (2016), accessed August19, 2020
- 2. Gandhi M, Bacchetti P, Spinelli MA, et al. : Brief report: Validation of a urine tenofovir immunoassay for adherence monitoring to PrEP and ART and establishing the cutoff for a point-of-care test. J Acquir Immune Defic Syndr 2019;81:72–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gandhi M, Devi S, Bacchetti P, et al. : Measuring adherence to antiretroviral therapy via hair concentrations in India. J Acquir Immune Defic Syndr 2019;81:202–206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McDowell MA, Dillon CF, Osterloh J, et al. : Hair mercury levels in US children and women of childbearing age: Reference range data from NHANES 1999–2000. Environ Health Perspect 2004;112:1165–1171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hammer DI, Finklea JF, Hendricks RF, Shy CM, Horton RJM: Hair trace metal levels and environmental exposure. J Epidemiol 1971;93:84–92 [DOI] [PubMed] [Google Scholar]
- 6. Puschel K, Thomasch P, Arnol W: Opiate levels in hair. Forensic Sci Int 1981;21:181–186 [DOI] [PubMed] [Google Scholar]
- 7. Gandhi M, Ameli N, WIHS, et al.: Protease inhibitor levels in hair samples strongly predict virologic response to HIV treatment. AID 2009;23:471–478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gandhi M, Ameli N, Bacchetti P, et al. : Atazanavir concentration in hair is the strongest predictor of outcomes on antiretroviral therapy. Clin Infect Dis 2011;52:1267–1275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Usman M, Naseer A, Baig Y, Jamshaid T, Shahwar M, Khurshuid S: Forensic toxicological analysis of hair: A review. Egypt J Forensic Sci 2019;9:1–12 [Google Scholar]
- 10. Gandhi M, Glidden D, Mayer K, et al. : Association of age, baseline kidney function and medication exposure with declines in creatinine clearance on pre-exposure prophylaxis: An observational cohort study. Lancet HIV 2016;3:e521–e528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kintz P: Analysis in forensic toxicology: An updated review with a special focus on pitfalls. Currr Pharm Design 2017;23:5480–5486 [DOI] [PubMed] [Google Scholar]
- 12. Koss CA, Hosek SG, Bacchetti P, et al. : Comparison of measures of adherence to human immunodeficiency virus preexposure prophylaxis among adolescent and young men who have sex with men in the United States. Clin Infect Dis 2018;66:213–219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gandhi M, Mwesigwa J, Aweek F, et al. : Hair and plasma data show that lopinavir, ritonavir and efavirenz all transfer from mother to infant in utero, but only efavirenz transfer via breastfeeding. J Acquir Immune Defic Syndr 2013;63:578–584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gandhi M, Greenblatt RM, Bacchetti P, et al. : A single nucleotide polymorphism in CYP2B6 leads to >3-fold increases in efavirenz concentrations in intensive PK curves and hair samples in HIV-infected women. J Infect Dis 2012;206:1453–1461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cohen SE, Sachdev D, Lee SA, et al. : Acquisition of tenofovir-susceptible emtricitabine-resistant HIV despite high adherence to daily pre-exposure prophylaxis: A case report. Lancet HIV 2019;6:e43–e50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kerrigan S: Sampling, storage and stability. In: Clarke's Analytical Forensic Toxicology, 2nd ed. (Negrusz A, Cooper G, eds.) Pharmaceutical Press, London, UK, 2013, Ch. 13, p. 343 [Google Scholar]
- 17. Saberi P, Torsten B, Ming K, Johnson MO, Kuncze CA, Gandhi M: Strong correlation between concentrations of antiretrovirals in home-collected and study-collected hair samples: Implications for adherence monitoring. J Acquir Immune Defic Syndr 2017;76:101–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hickey MD, Salmen CR, Tessler RA, et al. : Antiretroviral concentrations in small hair samples as a feasible marker of adherence in rural Kenya. J Acquir Immune Defic Syndr 2014;66:311–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Koss CA, Natureeba P, Mwesigwa J, et al. : Hair concentrations of antiretrovirals predict viral suppression in HIV-infected pregnant and breastfeeding Ugandan women. AIDS (London, England) 2015;29:825–830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Palamar JJ, Salomone A, Cleland CM, Sherman S: Willingness to provide a hair sample for drug testing among electronic dance music party attendees. Subst Abus 2019;40:116–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tong EK, Fung LC, Stewart SL, Paterniti DA, Dang JH, Chen MS Jr: Impact of a biospecimen collection seminar on willingness to donate biospecimens among Chinese Americans: Results from a randomized, controlled community-based trial. Cancer Epidemiol Biomarkers Prev 2014;23:392–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nwogu JN, Babalola CP, Berzins B, et al. : Willingness to donate hair samples for research among people living with HIV/AIDS attending a tertiary health facility in Ibadan, Nigeria. AIDS Res Hum Retroviruses 2019;35:642–648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Select Statistical Services. Available at https://select-statistics.co.uk/calculators/sample-size-calculator-population-proportion/, accessed February20, 2020
- 24. Curno MJ, Rossi S, Hodges-Mameletzis L, et al. : A systematic review of the inclusion (or exclusion) of women in HIV research. J Acquir Immune Defic Syndr 2016;71:181–188 [DOI] [PubMed] [Google Scholar]
- 25. Wikipedia, the free encyclopedia: Demographics of Nigeria. Available at https://en.wikipedia.org/wiki/Demographics_of_Nigeria, accessed August11, 2020
- 26. Idigbe EO, Adewole TA, Eisen G, et al. : Management of HIV-1 infection with a combination of nevirapine, stavudine, and lamivudine. J Acquir Immune Defic Syndr 2005;40:65–69 [DOI] [PubMed] [Google Scholar]
- 27. Babatunde OA, Elegbede OE, Ayodele LM, et al. : Workers willingness to donate human biological sample for future research in a South Western Nigerian Tertiary Health Center. J Asian Sci Res 2013;3:57 [Google Scholar]
- 28. Goldenberg AJ, Hull SC, Wilfond BS, Sharp RR: Patient perspectives on group benefits and harms in genetic research. Public Health Genomics 2011;14:135–142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Boima V, Ganu V, Yorke E, et al. : Knowledge and willingness to donate kidneys for transplantation in Ghana: A cross-sectional survey. Transplant Proc 2020;52:2883–2889 [DOI] [PubMed] [Google Scholar]
- 30. Iliyasu Z, Abubakar IS, Lawan UM, Abubakar M, Adamu B: Predictors of public attitude toward living organ donation in Kano, northern Nigeria. Saudi J Kidney Dis Transpl 2014;25:196–205 [DOI] [PubMed] [Google Scholar]
- 31. Pule PI, Rachaba B, Magafu MG, Habte D: Factors associated with intention to donate blood: Sociodemographic and past experience variables. J Blood Transfus 2014;2014:571678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Akinyemi RO, Akinyemi JO, Olorunsogbon OF, Uvere E, Jegede AS, Arulogun OS: Gender and educational attainment influence willingness to donate organs among older Nigerians: A questionnaire survey. Pan Afr Med J 2020;36:288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lewis C, Clotworthy M, Hilton S, et al. : Public views on the donation and use of human biological samples in biomedical research: A mixed methods study. BMJ Open 2013;3:e003056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Plana NM, Kimberly LL, Parent B, et al. : The public face of transplantation: The potential of education to expand the face donor pool. Plast Reconstr Surg 2018;141:176–185 [DOI] [PubMed] [Google Scholar]
- 35. Park UJ, Han SY, Han KH, et al. : Effects of phased education on attitudes toward organ donation and willingness to donate after brain death in an Asian country. Asian J Surg 2019;42:256–266 [DOI] [PubMed] [Google Scholar]
- 36. Coetzee B, Kagee A, Tomlinson M, Warnich L, Ikediobi O: Reactions, beliefs and concerns associated with providing hair specimens for medical research among a South African sample: A qualitative approach. Future Virol 2012;7:1134–1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rosado SD: No Nubian Knots or Nappy Locks: Discussing the politics of hair among women of African decent in the diaspora. A report on research in progress. Transform Anthropol 2004;11:60–63 [Google Scholar]