Abstract
Purpose: To assess psychological state of women who experienced postponement of ART care during the first COVID-19 wave in a French public ward of reproductive medicine.
Methods: An online anonymous survey was emailed between July and August 2020 to all women whose infertility care, including the first consultation for infertility, have been delayed at the beginning of the COVID-19 pandemic. Anxiety, depression, and stress were assessed using Hospital Anxiety and Depression Scale (HADS) and Perceived Stress Scale (PSS-10). Feelings about COVID-19 outbreak, lockdown and suspension of fertility care were assessed by Multiple-Choice Questions and Visual Analog Scales.
Results: 435 women answered to the survey (response rate 34.6%). Mean levels of the HADS-A (anxiety), HADS-D (depression) and PSS10 were respectively 7.58(±3.85), 4.51(±3.48), and 27(±6.75). Prevalence of stress was 50.8% and almost half of women presented clear or suggestive anxiety symptoms (respectively 21.6% and 25.7%). Stress and anxiety rates were much higher than those expected in infertile population. Increased stress was observed in women above 35 years and those stopped ‘in cycle’ or during pre-treatment for in-vitro fertilization or frozen embryo transfer. Patient with history of depression or anxiety had a higher prevalence of perceived stress (p = 0.0006). Postponement was perceived as ‘unbearable’ for women experiencing stress (p = 0.0032). After the first wave of pandemic, pregnancy desire remained the same and 84.3% of women wanted to resume fertility care as soon as possible.
Conclusion: Stopping fertility care during the COVID-19 pandemic had a significant psychological impact on women with an increase of stress, and anxiety. Psychological counseling should always be offered especially during this difficult period.
Keywords: Anxiety, Stress; COVID-19; Infertility; ART; Psychological effect; Mental health
Introduction
At the end of December 2019, a new disease emerged in China named the 2019-coronavirus disease (COVID-19) [1]. This disease due to a severe acute respiratory coronavirus 2 (SARS-CoV-2) was highly contagious. It spread out in the entire world in a few weeks. On March 11th, 2020, the World Health Organization (WHO) declared COVID-19 outbreak a pandemic [2].
In France, during the first wave, 90 778 patients infected with COVID-19 were hospitalized with 19% of them requiring intensive care [3]. Therefore, intensive care units were overwhelmed with a lack of bed, equipment, paramedical and medical staff. To limit the strain on the health care system, French authorities set up containment and delayed non-emergency care [4].
According to stress and coping theory, stress reaction results from an imbalance between the perception of a threat and the ability to cope with it [5]. People facing disasters generally experienced more stress than usual however are often able to show resilience and finally recover. Some groups could be more vulnerable than others to the psychosocial effects of pandemics [6]. Early epidemiological studies related to COVID-19 pandemic indicate a psychological impact in general population all around the world [7], [8], [9], [10], [11], [12], [13], [14]. Isolation, the fear of being contaminated and the absence of perspective increased stress and anxiety.
In France, one in eight couples encounters difficulties to conceive [15]. The diagnosis and treatments of infertility with uncertain results is often felt as a burden [16]. Infertile couples are at risk of psychosocial problems, especially anxiety and depression [17], [18], [19], [20]. These symptoms appear to be higher than in general population [21] and women are more exposed than men [17,19,20].
Following the recommendations of the European Society of Human Reproduction and Embryology (ESHRE) [22], the Biomedicine Agency (Agence de la Biomédecine) and the American Society for Reproductive Medicine (ASRM) [23], infertility treatments suddenly stopped all around the world although infertility is recognized by the WHO as a ‘disease’ for which the ‘time variable is critical’ [24]. Main recommendations included suspension of new fertility treatments –ovulation induction, intrauterine insemination (IUI), and in vitro fertilization (IVF)– as well as non-urgent gamete cryopreservation, cancellation of all embryo transfers, whether fresh or frozen. Moreover, elective surgery and non-urgent diagnostic procedures were postponed.
With COVID-19 pandemic and suspension of Assisted Reproductive Treatments (ART), it is highly likely that psychic symptoms of anxiety, stress and depression may have appeared or worsened in women waiting for their first infertility consultation or undergoing infertility treatment.
In Turocy et al., cancellation of fertility treatment upset infertile couples [25]. Regarding the COVID-19 studies, in different countries, an increase of emotional distress and anxiety were found in infertile couple [26,27], especially in women [28].
The aim of the study was to assess psychological state of women who experienced postponement of ART care during the first COVID-19 wave in one of the largest French public ART centers.
Materials and methods
Study design
This cross-sectional study was performed in a French public Reproductive Center at the ‘Femme, Mère, Enfant’ Hospital (HFME). An online survey was e-mailed to the participants from a dedicated mailing box. Women treated for infertility were recruited if they had consultation, surgery or ART treatment delayed due to the COVID-19 pandemic. Survey was completely anonymous and voluntary.
HADS and PSS-10 scales were used to assess anxiety, depression, and stress.
Survey characteristic
Survey was developed by a team of gynecologist and psychologists.
There were three main sections: 1) questions related to demography, socioeconomic situation, fertility history, mental health history and specific feelings related to the COVID-19 pandemic, 2) Hospital Anxiety and Depression Scale (HADS) questionnaire for anxiety and depression assessment, 3) Perceived Stress Scale (PSS-10) questionnaire for stress assessment. Both scales are worldwide validated, with a French version and used in recent ART and COVID19’s research [29], [30], [31], [32], [33]. Clinical translation of HADS and PSS-10 scores are resume in Table 1 .
Table 1.
Clinical signification of HADS and PSS-10 scores.
| HADS-Anxiety | HADS-Depression | PSS-10 | Mood disorder |
|---|---|---|---|
| 0–7 | 0–7 | 0–13 | Absence |
| 8–10 | 8–10 | 14–26 | Suggestive/Doubtful |
| 11–21 | 11–21 | 27–40 | Presence |
HADS: Hospital Anxiety and Depression Scale; PSS10: Perceived Stress Scale.
Patient background
Demographic variables including age, marital status, work status, number of children, anxiety or depression history and treatment were asked. Specific items related to ART were added: infertility duration, length of fertility cares, previous ART treatment. We asked for the feeling about stopping ART care, fear of being pregnant during outbreak, desire of pregnancy and starting again ART procedure. Regarding COVID-19, we asked some specific questions: “Did the news about COVID-19 in the media increase anxiety?”, “Did the COVID-19 pandemic prevent you from seeing your doctor/ going to the hospital?”, “How did you assess your stress compared to the period before the lockdown?”, “At what step of ART procedure were you at the beginning of lockdown?” “Did you personally think about stopping ART treatment during the outbreak?”, “Did you experience any mood change during lockdown?”, “Did you notice any change within your relationship during the lockdown?”. It was assessed either with visual analog scales (VAS) (1 to 10 / −5 to 5) or MCQ.
HADS scale
Hospital Anxiety and Depression Scale is a 14 items scale, assessing separately anxiety (7 items) and depression (7 items). All items were scored on a four-point Likert scale ranging from 0 to 3. It results in a score of 0 to 21 for both anxiety and depression. The subscales, anxiety (HADS-A) and depression (HADS-D), were independent measures. Score of 0 to 7 was regarded as normal range, score of 11 or higher indicates probable presence of mood disorder and score of 8 to 10 was suggestive. Despite the world ‘hospital’, HADS was validated in community setting.
PSS-10 scale
Perceived Stress Scale (PSS-10) was a 10 items scale, graded on a five-point (0–4) Likert scale, examining participant's level of perceived stress over the last month. Four items (4, 5, 7, and 8) were positively stated items and require reverse coding. Total score was between 0 and 40. Score ranging from 0–13 would be considered low stress, 14–26 moderate stress, 27–40 high perceived stress.
Recruitments
Women who had consultation (face-to-face, remote, scheduled or canceled) between 1st of January et 11th of May 2020 were contacted. Email addresses were found in the ART software used in the department. Online survey was sent between July and August, to 1300 women.
Inclusion criteria were age between 18 and 42 years and 12 months, all causes of infertility. Exclusion criteria were non-French speakers or readers, no email address found in the medical file, need for oocyte donation or fertility preservation. We chose to exclude oocyte donation and fertility preservation patients because these journeys engage other specific psychic process.
All the women received a consent form and gave their agreement to use the survey data. Clinical research and innovation department of HCL (Hospices Civils de Lyon) and regional Personal Protection Committee (CPP) approved the study on 30th of June 2020 (Ref: 2020-A01760-39). The trial was registered in ClinicalTrials.gov (NCT04496869).
Objectives
The aim of the study was to understand psychological response among women who had infertility care, including the first consultation for infertility, postponed because of the COVID-19 pandemic and the need of psychological counseling. We also wanted to assess anxiety and depression with already known scales in infertile women.
Statistical analysis
The quantitative variables were described using the mean and the standard deviation or using the quartiles and the minimum and maximum values, depending on the shape of the distribution. The qualitative variables were described using the number and percentage in each category.
Patients’ characteristics were compared between the PPS10 stress <27 and the PPS10 stress ≥ 27 using Student t-test or Mann-Whitney according to the distribution for quantitative characteristics and chi-square test or Fisher exact test for qualitative characteristics with a two-sided significance level of 5%. No comparisons were performed for the HADS scale.
All statistical analyses were performed using SAS® Software version 9.4 in a Windows environment.
Results
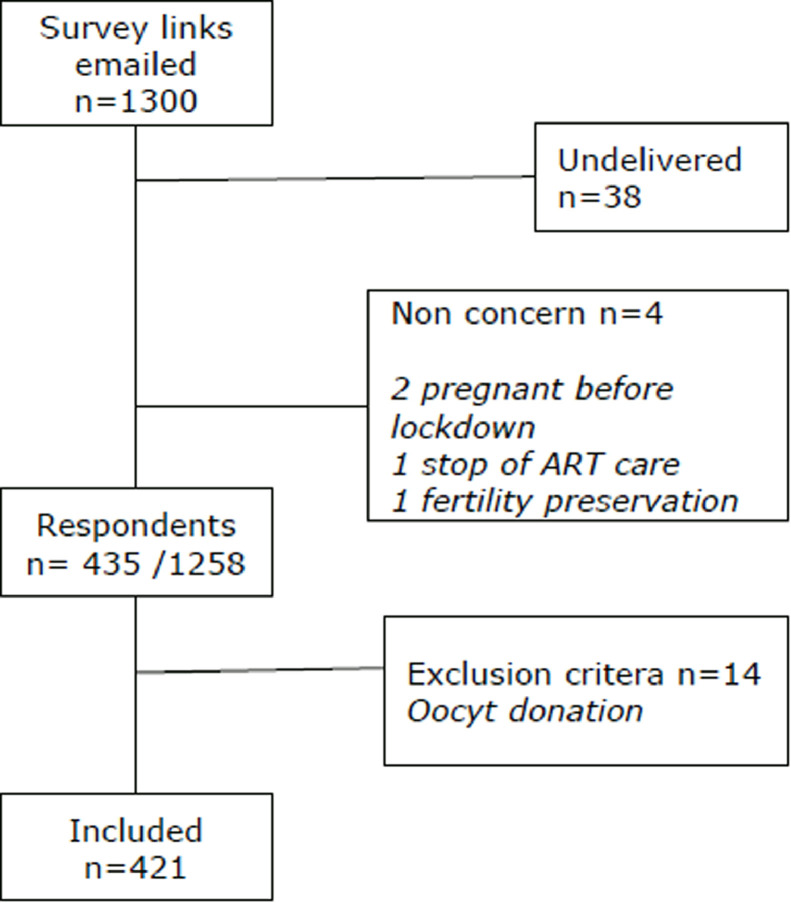
One thousand and three hundred emails with survey links were sent. Thirty-eight email addresses were wrong, and four women were excluded before answering survey (ART treatment stopped, pregnancy before the lock down, fertility preservation). Finally, 435 women completed the survey and 14 were excluded (oocyte donation). The response rate was 34.6% (n = 435/1258) (Fig. 1 ).
Fig. 1.
PsyCovART flowchart.
Mean age of the participant was 34 years (±4.6). More than half of the participants were married (53.2%). One quarter of participants already had children with their current partner. In our population, mean duration of infertility was 4.8 years (±3.1) and mean time before consulting for infertility care was 2 years (±1.9). Two-thirds of the participants were in the middle of IVF treatment, or frozen embryo transfer (FET) (n = 262 / 62.2%), 28 ovulation inductions (clomiphene citate or gonadotrophin) (6.7%), 36 intrauterine inseminations (8.6%) and 91 women were not undergoing any treatment (22.6%). All the participants experienced the sudden stop of ART care on 16th March 2020. Some women were “in-cycle”, and decision was made to perform oocytes pick up and froze all embryos (18.5%). Ovulation stimulation (9.5%) IVF and FET pretreatments (19.9%) were stopped. Some of them were between two consultations (45.6%), other were waiting for the first fertility appointment (6.4%) (Table 2 ).
Table 2.
Characteristics of the patients.
| Characterisis | Women (n = 421) |
|---|---|
| Age, years (mean±std) | 34 ± 4,6 |
| Marital statut n(%) | |
| Married | 224 (53,2) |
| Common-law | 197 (46,8) |
| Occupation during lockdown n(%) | |
| No | 60 (14,3) |
| Yes | 321 (76,2) |
| Face-to-face Work | 140 (43,6) |
| Teleworking | 148(46,1) |
| Other | 40 (9,5) |
| Anxiety history n(%) | 89(21,1) |
| Number of children n(%) | |
| None | 318 (75,5) |
| With current partner | 104(24,7) |
| One | 90(87,4) |
| Two | 9(8,7) |
| Three | 5(4,9) |
| With a precedent partner | 21(0,5) |
| Partner's child | 43(10,2) |
| Children living at home during lockdown | |
| None | 278(66) |
| One | 120(28,5) |
| Two | 17(4) |
| Three | 6(1,4) |
| Infertility characteristics | |
| Duration of infertility, years (mean±std) | 4,8 ±3,1 |
| Time before consulting, years (mean±std) | 2 ±1,9 |
| Treatment phase n(%) | |
| IVF or FET | 262(62,2) |
| Oral ovulation induction | 5(1,2) |
| Gonadotrophine induction ovulation | 23(5,5) |
| Intrauterine insemination | 36(8,6) |
| No treatement | 95(22,6) |
| Care process stage when ART was suspended n(%) | |
| "In-cycle" | 78(18,5) |
| Ovulation stimulation | 40(9,5) |
| Pre-treatment of IVF ou FET | 84(19,9) |
| Between two consultations | 192(45,6) |
| Wainting for the first appointment | 27(6,4) |
ART: Assisted Reproductive Treatment; IVF: In Vitro Fertilization; FET: Freezing Embryo Transfer.
Anxiety and depression history in our population was 21.1% (n = 89). Thirty-nine (43.8%) of them were treated by anxiolytics and 38 (42.7%) by antidepressants. The majority experienced psychological counseling (n = 54 – 60.7%) and 20.2% (n = 18) alternative medicine.
Thirty spontaneous pregnancies were reported during the lockdown (7.1%).
Mean levels of the HADS-A (anxiety), HADS-D (depression) and PSS10 were respectively 7.58 (± 3.85), 4.51 (±3.48), and 27 (±6.75) (Table 3 ). Presence of stress was clearly identified in 50.8% of our patients (PSS10 ≥ 27: n = 214). Anxiety also seemed to be present with 21.6% of symptomatic women and 25.6% with suggestive symptoms. No tendency to depression was found.
Table 3.
HADS-A, HADS-D and PSS-10 scores among infertile women.
| Mood disorder |
||||
|---|---|---|---|---|
| Absence | Suggestive | Presence | ||
| Mean ± Std | n(%) | n(%) | n(%) | |
| PSS10 score | 27 ± 6,75 | 76 (18,1) | 131 (31,1) | 214 (50,8) |
| HADS-A score | 7,58 ± 3,85 | 222 (52,7) | 108 (25,7) | 91 (21,6) |
| HADS-D score | 4,51 ± 3,48 | |||
HADS-A: Hospital Anxiety and Depression Scale - anxiety part; HADS-D: Hospital Anxiety and Depression Scale - depression part; PSS10: Perceived Stress Scale; Std: standard deviation.
Among the patients, only 112 (26.6%) imagined suspending ART procedures for themselves. Suspension of ART care during the lockdown felt logical for 45.8% of them and surmountable for 27.3%. It was unbearable for a significant part (n = 85 – 20.2%). Most of the women wanted to resume treatments as soon as possible (n = 355 – 84,3%). Desir of pregnancy did not decrease, and patients did not seem to be afraid of getting pregnant during the COVID-19 pandemic (Table 4 ).
Table 4.
Specific questions of the survey and answers about ART care.
| Has your desire of pregnancy been exacerbated or decreased compared to the period before COVID-19? VAS −5/5 | Were you afraid of being pregnant during the COVID-19 pandemic? VAS 1/10 |
| 1,3 ± 2,4 | 1 [1] |
| Have you noticed any change within your relationship during the lockdown? MCQ | Have you personally imagine stopping ART treatment during the outbreak? MCQ |
| if yes, in good way 29(37,7%) | |
| if yes, in bad way34(44,2%) | |
| The postponement of your ART care seemed to you: MCQ | Would you like to resume your follow-up? MCQ |
 |
Results = n(%) or median [IQR] or mean ± std.
VAS: Visual Analog Scale; MCQ: multiple-choice question.
Women reported that they did not feel more stressed during lockdown, while they experienced mood changes and 18,3% noticed changes in their relationship. COVID-19 media news appeared to be worrisome, and fear of COVID-19 seemed to prevent them from going to hospital (Table 5 ).
Table 5.
Specific questions about COVID-19 experience.
| VAS | Mean±std | |
|---|---|---|
| How do you assess your stress compared to the period before the lockdown? | −5/5 | 0,8 ± 2,1 |
| Have you experienced any mood change during lockdown? | 1/10 | 4,1 ± 3 |
| Did the COVID-19 media news seem anxious to you? | 1/10 | 6,5 ± 2,9 |
| Did the COVID-19 pandemic prevent you, for fear, from seeing your doctor? | 1/10 | 2,9 ± 2,7 |
| Did the COVID-19 pandemic prevent you, for fear, from going to hospital? | 1/10 | 3,6 ± 3,1 |
VAS: visual analog scale; std: standard deviation.
Stress and anxiety were assessed according to sociodemographic and clinical characteristics of the sample. Results are presented in Tables 6 and 7 . Previous parity, infertilty duration, desir of pregnancy did not have a significative impact on the prevalence of anxiety or stress. However, women stopped ‘in cycle’ or during pre-treatement for IVF or FET seemed to be more stressed, as well as women over 35 years old and those who consulted earlier for difficulty getting pregnant (not statistically significant).
Table 6.
Comparison of PSS-10 according to sociodemographic and clinical parameters.
|
PSS10 Stress |
||||
|---|---|---|---|---|
|
n(%) or Mean±Std |
||||
| <27 | ≥ 27 | |||
| n = 421 | 207(49,2) | 214(50,8) | ||
| Age | p | |||
| ≤35 years | n = 260 | 132 (50,8) | 128 (49,2) | 0,5384 |
| > 35 years | n = 161 | 75 (46,6) | 86 (53,4) | |
| Infertility duration (year) | ||||
| 4,9±3,3 | 4,7±2,9 | 0,6029 | ||
| Time before consulting in ART (year) | ||||
| 2,5±2,5 | 2,1±2,1 | 0,1807 | ||
| Children with current partner | ||||
| Yes | n = 103 | 53 (51,5) | 50 (48,5) | 0,647 |
| Non | n = 318 | 154 (48,4) | 164 (51,6) | |
| Anxiety history | ||||
| Yes | n = 89 | 22 (24,7) | 67 (75,3) | 0,0006 |
| No | n = 332 | 185 (55,7) | 147 (44,3) | |
| Support stage when ART stopped | ||||
| "In-cycle" | n = 78 | 35 (44,9) | 43 (55,1) | 0,7129 |
| Ovulation stimulation | n = 40 | 19 (47,5) | 21 (52,5) | |
| Pre-treatment of IVF/FET | n = 84 | 38 (45,2) | 46 (54,8) | |
| Between two consultations | n = 192 | 101 (52,6) | 91 (47,4) | |
| Wainting for the first appointment | n = 27 | 14 (51,9) | 13 (48,1) | |
| Desire of pregnancy (VAS −5/5) | ||||
| 1,3±2,1 | 1,3±2,7 | |||
| Feeling about postponement | ||||
| Logical | n = 193 | 117 (60,6) | 76 (39,4) | 0,0006 |
| Sumontable | n = 115 | 51 (44,3) | 64 (55,7) | 0,3861 |
| Unbearable | n = 85 | 28 (32,9) | 57 (67,1) | 0,0032 |
| Normal | n = 93 | 50 (53,8) | 43 (46,2) | 0,473 |
| Dont'know | n = 16 | 4 (25) | 12 (75) | 0,1461 |
| Resuming ART follow-up | ||||
| Yes, as soon as possible | n = 355 | 174 (49) | 181(51) | |
| Yes, in a while | n = 20 | 10 (50) | 10 (50) | |
| Not yet | n = 28 | 18 (64,3) | 10 (35,7) | |
| Don't know | n = 18 | 5 (27,8) | 13 (72,2) | |
IVF: In Vitro Fertilization; FET: Freezing Embryo Transfer; VAS: Visual Analog Scale.
Table 7.
Comparison of HADS anxiety score according to sociodemographic and clinical parameters.
|
HADS anxiety |
|||
|---|---|---|---|
|
n(%) or mean±std |
|||
| <11 | ≥ 11 | ||
| n = 421 | 330(78,4) | 91(21,6) | |
| Age | |||
| ≤35 years | n = 260 | 202 (77,7) | 58 (22,3) |
| > 35 years | n = 161 | 128 (79,5) | 33 (20,5) |
| Infertility duration (year) | |||
| 4,8±3,1 | 4,7±3 | ||
| Time before consulting in ART (year) | |||
| 2,3±2,4 | 2,1±2,1 | ||
| Children with current partner | |||
| Yes | n = 103 | 83 (80,6) | 20 (19,4) |
| Non | n = 318 | 247 (77,7) | 71 (22,3) |
| Anxiety history | |||
| Yes | n = 89 | 63 (70,8) | 26 (29,2) |
| No | n = 332 | 267 (80,4) | 65 (19,6) |
| Support stage when ART stopped | |||
| "In-cycle" | n = 78 | 63 (80,8) | 15 (19,2) |
| Ovulation stimulation | n = 40 | 30(75) | 10 (25) |
| Pre-treatment of IVF/FET | n = 84 | 65 (77,4) | 19 (22,6) |
| Between two consultations | n = 192 | 150 (78,1) | 42 (21,9) |
| Wainting for the first appointment | n = 27 | 22 (81,5) | 5 (18,5) |
| Desire of pregnancy (VAS −5/5) | |||
| 1,2±2,3 | 1,6±2,9 | ||
| Feeling about postponement | |||
| Logical | n = 193 | 164 (84,9) | 29 (15,1) |
| Sumontable | n = 115 | 90 (78,3) | 25 (21,7) |
| Unbearable | n = 85 | 56 (65,9) | 29 (34,1) |
| Normal | n = 93 | 78 (83,9) | 15 (16,1) |
| Dont'know | n = 16 | 13 (81,3) | 3 (18,7) |
| Resuming ART follow-up | |||
| Yes, as soon as possible | n = 355 | 280 (78,9) | 75 (21,1) |
| Yes, in a while | n = 20 | 14 (70) | 6 (30) |
| Not yet | n = 28 | 24 (85,7) | 4 (14,3) |
| Don't know | n = 18 | 12 (66,6) | 6 (33,3) |
IVF: In Vitro Fertilization; FET: Freezing Embryo Transfer; VAS: Visual Analog Scale.
Patient with an history of depression or anxiety had a higher prevalence of percieved stress (75.3% vs. 44.3%, p = 0.0006).
Concerning emotional aspect, postponement was significatively more likely to be perceived as ‘unberable’ by women under stress (67.1% vs. 32.9%, p = 0.0032). While women without psycological distress were more prone to consider it as ‘logical’ (60.6% vs. 39.4% p=0.0006).
Discussion
To our knowledge, this is the first study assessing the psychological effect of COVID-19 pandemic among a whole population of infertile women by using standardized survey. This study revealed that COVID-19 pandemic had a psychological impact with a clear prevalence of stress. Fifty percent of women had a PSS-10 score above 27 classifying them directly with a symptomatic mood disorder. Almost half of the women presented clear or suggestive symptoms of anxiety (respectively 21.6% and 25.7%). Compared to those usually expected in infertile population, stress and anxiety rates were higher.
Validated scales, either in general or infertile population, were used in this study. Lesage et al. assessed PSS-10 in a French cohort, finding a woman mean score of 15.9 +/- 6.7 with no difference related to parental or marital status [31]. In another study, same scores were found in women attempting to conceive outside of any fertility investigations (PSS:14.8 −17.8) [32]. Concerning HADS scale: women scores were respectively 6,6 and 3,5 for HADS-A and HADS-D in a group of French workers [34]. Similar scores were found in a population of infertile women attempting for IVF (HADS-A=6,8 – HADS-D=3) [29]. In both scale (HADS and PSS10), items were balanced with positive and negative statements to minimize the response set effect. Comparatively to our finding, these scores confirmed an increase of stress in our cohort and a tendency towards anxiety during this period. Moreover, in a meta-analysis conducted in 2020, authors estabished the rate of anxiety at 36.17% in infertile women, based on 13 international publications [35]. This rate was greater than the prevalence of this condition in a general and healthy women population [36]. In comparison, in the departement, prevalence of stress was 50.8% and the tendancy to anxiety was 47.2%. These high rates support the idea that suppension of ART care increased the psychological consequences of infertilty.
Interviewing only women was a deliberate choice, because they are known to be more vulnerable. Indeed, the unabilty to conceive is often a topic of discussion within family and among friends. Social pressure about parenthood remains mainly on women's shoulders. Previous investigations indicated a difference in prevalence of psychological disorders within the couple, with women psychologically more affected than men by the burden of infertilty [17,37,38]. This observation was also found in the latest studies about ART during the COVID-19 pandemic. Indeed, emotional distress, anxiety and depression were more observed among women. As a consequence they feel more concerned within the couple and seem more prone to answer to psychological surveys [26,39]. This might be explained by the weight of fertility treatments often injectable and usually with side effects like mood disorders, asthenia, nausea, weight gain or ovarian hyperstimulation syndrome [40]. These tedious protocols are given to all women, regardless the origin of infertility. Moreover, uncertainty about whether it will be successful or not increase the distress of these women. It was already shown that women who felt to have a poor control over the course of their fertility problem displayed higher levels of stress and anxiety [41]. Boivin et al. reported that women also suffered from the fact that their medical care was not considered essential and therefore, find their condition denigrated and minimized [39].
It must be underlined that psychological distress highlighted in this study could be due to multiple causes. Part of stress due to the pandemic and the one due to the closure of fertility center are difficult to assess. Containment measures, including self-isolation and social distancing, had a strong impact on population's daily life and may have negatively affected psychological well-being [42]. Surveys on COVID-19 have been recently conducted in general population in Italy [7], Spain [8], France [10] and China [11,12,14]. Those have shown an increase in psychological issue because of the COVID-19 pandemic. However, it is noteworthy that it did not reach a pathological level. As reported by Qiu et al.: only 5% of the population suffered from severe distress and 29% from mild or moderate distress [12]. Therefore, the symptomatic level of psychological disorder reported in this study seems to be, even more, in connection with the interruption of ART.
According to the characteristics of the population, a higher rate of stress seemed to be observed among women whose treatment was stopped before oocyte retrieval or embryo transfer. The sudden stop was experienced as a lost chance and a failure of treatment, which did not lead to the expected result: pregnancy. Previous treatment failures are known to be an important element reducing the ability to cope and thus increasing stress [43]. Stress symptoms were also more frequent in patient above 35 years old. Same trend was found in infertile Turkish women [28]. Advanced maternal age is known to have a significant impact on reproductive outcomes with the physiological decrease of ovarian reserve over time. Women above 35 years old might be more concerned about the diminished chances of pregnancy. This is consistent with Tokgoz et al. results which showed that women with a diminished ovarian reserve had a higher level of anxiety during the outbreak [28]. 21% of the participant had an history of anxiety or depression before the outbreak. It was a normal rate for an infertile women population [35]. As expected, this subgroup of women significatively experienced more stress (PSS score >27 for 75.3% of them). Women who had consulted earlier for infertility also appeared to be more prone to stress during the pandemic. For both groups, imbalance between the perception of the threat (stopping treatment) and the personal resources to cope with (pre-existing psychological vulnerability) leads to a stress reaction.
One in four women had spontaneously thought of stopping ART care because of the pandemic. This concern about fertility and getting pregnant despite the pandemic is not specific to our sample. Vaughan et al. pointed out that infertility remained a top stressor in America, before the COVID-19 during the first wave [44]. For half of the women, stopping ART care was acceptable. However, for 20% of them, it was felt to be unbearable. COVID-19 became an additional burden on top of what patients had already experienced due to infertility or past disappointment (miscarriage, treatment failures).
The first aim of ART ward closure was to limit the spread of the disease (by bringing people to hospital), to avoid additional stress on healthcare systems and free some needs (human and material redeployment) to help in COVID centers [39]. Secondly, stopping ART care seemed to be necessary because of uncertain effects of COVID on fertility [45,46], pregnancy and newborn's health [47], [48], [49] at the beginning of the pandemic. It was therefore, understood by most of the patients.
Nevertheless, women were not afraid of getting pregnant and 84.3% wanted to resume treatments as soon as possible. This is slightly more than in the US and Italy where respectively 52% and 64% of the patients indicated that they would have chosen to resume an IVF cycle despite the pandemic [25,26].
The spontaneous pregnancy rate during this period reflected that desire for parenthood was still there. In addition, lockdown allowed couple to spend more time together at home. Some patients reported positive changes in their relationship, with better communication, greater complicity, and increased libido. Others experienced a deterioration in relationships. Most of them reported tension related to confinement and the appearance of unusual behavior (stress, irritability, moroseness) in their partner. Having marital tension and a stressed partner contributes to increased women psychological distress [27,43]. This may have contributed to intensify stress in this group.
The media were also identified as a source of anxiety and stress by women. Like our research, Barra et al. demonstrated that the occurrence of stress or anxiety feeling was associated with the time per day spent on COVID-19 related news (>1 h) [27]. Despite this, in general population as well among infertility subgroup, regular update information was perceived to be helpful in some other studies [9,39].
Other international studies have been carried out and most of them only included women undergoing IVF or IIU [26,28]. From our perspective, it was important to assess state of mind of all patients who received care, and particularly those waiting to start treatment. Women who underwent IVF represented only 38% of the active file when the lockdown started. Focusing only on them would have made us neglected most of the patients. With our results that included all women, it was obvious that psychological impact of COVID-19 pandemic occurred regardless the stage of the ART care process.
This is the first French study assessing the psychological status of women who experienced postponement of ART care due to the COVID-19 pandemic. One of the strengths of this work was to use standardized measures of anxiety, depression, and stress. It will allow us to repeat survey, assess evolution of emotional distress and follow up of our patient. Another strength was the inclusion of all consecutive women at different stages of the care process. In addition, our sample is relatively large and the response rate for online survey is satisfying and consistent with same-topic studies [26,28,39,44].
Limitations of our study include inherent constraints of self-report measures of psychological distress which maybe not always aligned with assessment by mental health professionals. It is possible that there was a selection bias of participants with women experiencing less anxiety and stress choosing not to enroll. Due to the survey anonymity, characteristics about the non-responders were not available. The urgency of this work required a quick turnaround of surveys. The absence of control group is a regret but establishing a suitable one with these deadlines was complex. Moreover, our results can be easily compared with the literature regarding the validated scale. Another bias might be a recall bias because the survey has been done after the end of the lockdown. Emotional distress may have been underestimated. Gradual return to work, increasing numbers of people recovering from COVID-19 and improvement of infection knowledge gave the population some confidence. The psychological distress due to quarantine could have decreased [48] as well as the one due to the suspension of the infertility care [50]. Another limit could be the monocentric nature of the investigation, which focuses on a community in a relatively affluent urban area. The incidence of COVID-19 was high in our area and healthcare system has been seriously threatened. Our population might have been more aware of the pandemic severity. Participants might have experienced more stress and anxiety than people in other region. Moreover, our infertility center is a public hospital where ART care costs are covered. Impact of COVID-19 economic issues on our patients might be minimized.
Our study is in line with the extensive psychological research following the COVID-19 pandemic and responds to the call made by Holmes et al. (Lancet Psychiatry): to collect collaboratively and multidisciplinary data on the effect of the COVID-19 pandemic on mental health across the whole population and vulnerable groups [51]. Our findings help to identify some of the most sensitive patients.
In June 2020, thanks to a partial control of the pandemic, authorities allowed the resumption of ART cares. Initially with medical restrictions, then reproductive treatment resumed as before. However, couples are still experiencing uncertainty about a new postponement of treatment, fear of being contaminated, the risk of delaying or even interrupting again the procedure. A psychological follow-up has been initiated in our ward to monitor anxiety and stress throughout the COVID-19 pandemic. The mood impact of the closure of ART centers will be reassessed with new surveys and with the aim of identifying protective and resilience factors to offer an optimal counselling strategy. More than ever, psychological counseling must be offered to the patient in all reproductive medicine department.
Trial registration
ClinicalTrials.gov NCT04496869 on 15th of June 2020. Clinical research and innovation department of HCL (Hospices Civils de Lyon) and regional Personal Protection Committee (CPP) approved the study on 30th of June 2020 (Ref: 2020-A01760-39).
Conclusion
COVID-19 pandemic was an unprecedented situation which have changed daily life and future perspective.
According to this study, stopping ART treatments during COVID-19 lockdown contributed to increase stress and anxiety. Women aged over 35 years old and those whose treatment was interrupted before oocyte puncture or embryo transfer seemed to have a higher rate of psychological distress. Despite the lack of knowledge about the COVID-19 and the consequences on pregnancy and fetus wellbeing at the time of the survey, desire of getting pregnant and starting over ART treatments clearly showed up.
Psychological impact of COVID-19 pandemic on infertile women must not be neglected. Specific psychological counseling should be proposed to women and her partners. In the light of our findings, a new suspension of ART care should be avoided, as far as possible.
Declaration of Competing Interest
Authors reported no potential conflict of interest.
Acknowledgments
The authors acknowledge the support of the HCL Covid Task Force.
References
- 1.WHO. WHO | Novel Coronavirus – China [Internet]. WHO. World Health Organization; 2020. Available from: http://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/
- 2.WHO Director-General. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020 [Internet]. 2020. Available from:https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020
- 3.Golberg E (DREES/DIRECTION). Parcours hospitalier des patients atteints de la Covid-19 lors de la première vague de l’épidémie. 2020;39.
- 4.Ministère des solidarités et de la santé. PREPARATION A LA PHASE ÉPIDÉMIQUE DE Covid-19 [Internet]. 2020. Available from: https://solidarites-sante.gouv.fr/IMG/pdf/guide-covid-19-phase-epidemique-v15-16032020.pdf
- 5.Lazarus R, Folkman S. Springer; New York: 1984. Stress, appraisal, and coping. [Google Scholar]
- 6.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 7.Moccia L, Janiri D, Pepe M, Dattoli L, Molinaro M, De Martin V, et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav Immun. 2020;87:75–79. doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the Northern Spain. Cad Saude Publica. 2020;34(4) doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- 9.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020;06 doi: 10.3390/ijerph17051729. 17(5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Droit-Volet S, Gil S, Martinelli N, Andant N, Clinchamps M, Parreira L, et al. Time and Covid-19 stress in the lockdown situation: time free, «Dying» of boredom and sadness. PLoS One. 2020;15(8) doi: 10.1371/journal.pone.0236465. Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang SX, Wang Y, Rauch A, Wei F. Unprecedented disruption of lives and work: health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112958. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33(2) doi: 10.1136/gpsych-2020-100213. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112954. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu N, Zhang F, Wei C, Jia Y, Shang Z, Sun L, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112921. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.INSERM. Infertilité [Internet]. Inserm - La science pour la santé. 2019. Available from: https://www.inserm.fr/information-en-sante/dossiers-information/infertilite
- 16.Podolska MZ, Bidzan M. Infertility as a psychological problem. Ginekol Pol. 2011;82(1):44–49. Jan. [PubMed] [Google Scholar]
- 17.Baghianimoghadam MH, Aminian AH, Baghianimoghadam B, Ghasemi N, Abdoli AM, Seighal Ardakani N, et al. Mental health status of infertile couples based on treatment outcome. Iran J Reprod Med. 2013;11(6):503–510. Jun. [PMC free article] [PubMed] [Google Scholar]
- 18.Gdańska P, Drozdowicz-Jastrzębska E, Grzechocińska B, Radziwon-Zaleska M, Węgrzyn P, Wielgoś M. Anxiety and depression in women undergoing infertility treatment. Ginekol Pol. 2017;88(2):109–112. doi: 10.5603/GP.a2017.0019. [DOI] [PubMed] [Google Scholar]
- 19.Schaller MA, Griesinger G, Banz-Jansen C. Women show a higher level of anxiety during IVF treatment than men and hold different concerns: a cohort study. Arch Gynecol Obstet. 2016;293(5):1137–1145. doi: 10.1007/s00404-016-4033-x. [DOI] [PubMed] [Google Scholar]
- 20.Vikström J, Josefsson A, Bladh M, Sydsjö G. Mental health in women 20–23 years after IVF treatment: a Swedish cross-sectional study. BMJ Open. 2015 1;5(10) doi: 10.1136/bmjopen-2015-009426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramezanzadeh F, Aghssa MM, Abedinia N, Zayeri F, Khanafshar N, Shariat M, et al. A survey of relationship between anxiety, depression and duration of infertility. BMC Womens Health. 2004;4(1):9. doi: 10.1186/1472-6874-4-9. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.ESHRE. ESHRE News [Internet]. 2020. Available from: https://www.eshre.eu/Press-Room/ESHRE-News#COVID19WG
- 23.ASRM. Patient Management and Clinical Recommendations During The Coronavirus (COVID-19) Pandemic [Internet]. 2020. Available from: https://www.asrm.org/news-and-publications/covid-19/statements/patient-management-and-clinical-recommendations-during-the-coronavirus-covid-19-pandemic/
- 24.Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, et al. The International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) Revised Glossary on ART Terminology, 2009. Hum Reprod. 2009;24(11):2683–2687. doi: 10.1093/humrep/dep343. Nov 1. [DOI] [PubMed] [Google Scholar]
- 25.Turocy JM, Robles A, Hercz D, D'Alton M, Forman EJ, Williams Z. The emotional impact of the ASRM guidelines on fertility patients during the COVID-19 pandemic. Fertil Steril. 2020;114(3):e63. Sep. [Google Scholar]
- 26.Esposito V, Rania E, Lico D, Pedri S, Fiorenza A, Strati MF, et al. Influence of COVID-19 pandemic on the psychological status of infertile couples. Eur J Obstet Gynecol Reprod Biol. 2020;253:148–153. doi: 10.1016/j.ejogrb.2020.08.025. Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barra F, La Rosa VL, Vitale SG, Commodari E, Altieri M, Scala C, et al. Psychological status of infertile patients who had in vitro fertilization treatment interrupted or postponed due to COVID-19 pandemic: a cross-sectional study. J Psychosom Obstet Gynecol. 2020:1–8. doi: 10.1080/0167482X.2020.1853095. Nov 30. [DOI] [PubMed] [Google Scholar]
- 28.Tokgoz VY, Kaya Y, Tekin AB. The level of anxiety in infertile women whose ART cycles are postponed due to the COVID-19 outbreak. J Psychosom Obstet Gynaecol. 2020:1–8. doi: 10.1080/0167482X.2020.1806819. Aug 19. [DOI] [PubMed] [Google Scholar]
- 29.Massarotti C, Gentile G, Ferreccio C, Scaruffi P, Remorgida V, Anserini P. Impact of infertility and infertility treatments on quality of life and levels of anxiety and depression in women undergoing in vitro fertilization. Gynecol Endocrinol Off J Int Soc Gynecol Endocrinol. 2019;35(6):485–489. doi: 10.1080/09513590.2018.1540575. Jun. [DOI] [PubMed] [Google Scholar]
- 30.Joelsson LS, Tydén T, Wanggren K, Georgakis MK, Stern J, Berglund A, et al. Anxiety and depression symptoms among sub-fertile women, women pregnant after infertility treatment, and naturally pregnant women. Eur Psychiatry. 2017;45:212–219. doi: 10.1016/j.eurpsy.2017.07.004. Sep. [DOI] [PubMed] [Google Scholar]
- 31.Lesage F-X, Berjot S, Deschamps F. Psychometric properties of the French versions of the Perceived Stress Scale. Int J Occup Med Environ Health. 2012;25(2):178–184. doi: 10.2478/S13382-012-0024-8. [DOI] [PubMed] [Google Scholar]
- 32.Tiplady S, Jones G, Campbell M, Johnson S, Ledger W. Home ovulation tests and stress in women trying to conceive: a randomized controlled trial. Hum Reprod Oxf Engl. 2013 doi: 10.1093/humrep/des372. Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cousineau Tm, Green Tc, Corsini Ea, Barnard T, Seibring Ar. Domar Ad. Development and validation of the infertility self-efficacy scale. Fertil Steril. 2006 doi: 10.1016/j.fertnstert.2005.10.077. Jun. [DOI] [PubMed] [Google Scholar]
- 34.Bocéréan C, Dupret E. A validation study of the Hospital Anxiety and Depression Scale (HADS) in a large sample of French employees. BMC Psychiatry. 2014;14 doi: 10.1186/s12888-014-0354-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kiani Z, Simbar M, Hajian S, Zayeri F, Shahidi M, Saei Ghare Naz M, et al. The prevalence of anxiety symptoms in infertile women: a systematic review and meta-analysis. Fertil Res Pract. 2020;6(1):7. doi: 10.1186/s40738-020-00076-1. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Remes O, Brayne C, Linde R, Lafortune L. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain Behav. 2016;6(7):e00497. doi: 10.1002/brb3.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chiaffarino F, Mp B, Scarduelli C, Bommarito F, Ambrosio S, D'Orsi C, et al. Prevalence and incidence of depressive and anxious symptoms in couples undergoing assisted reproductive treatment in an Italian Infertility Department. Eur J Obstet Gynecol Reprod Biol. 2011 doi: 10.1016/j.ejogrb.2011.04.032. Oct. [DOI] [PubMed] [Google Scholar]
- 38.Kissi YE, Romdhane AB, Hidar S, Bannour S, Idrissi KA, Khairi H, et al. General psychopathology, anxiety, depression and self-esteem in couples undergoing infertility treatment: a comparative study between men and women. Eur J Obstet Gynecol Reprod Biol. 2013;167(2):185–189. doi: 10.1016/j.ejogrb.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 39.Boivin J, Harrison C, Mathur R, Burns G, Pericleous-Smith A, Gameiro S. Patient experiences of fertility clinic closure during the COVID-19 pandemic: appraisals, coping and emotions. Hum Reprod Oxf Engl. 2020 doi: 10.1093/humrep/deaa218. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Derman SG, Adashi EY. Adverse effects of fertility drugs. Drug Saf. 1994;11(6):408–421. doi: 10.2165/00002018-199411060-00003. Dec 1. [DOI] [PubMed] [Google Scholar]
- 41.Gourounti K, Anagnostopoulos F, Potamianos G, Lykeridou K, Schmidt L, Vaslamatzis G. Perception of control, coping and psychological stress of infertile women undergoing IVF. Reprod Biomed Online. 2012;24(6):670–679. doi: 10.1016/j.rbmo.2012.03.002. Jun. [DOI] [PubMed] [Google Scholar]
- 42.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet Lond Engl. 2020;14:912–920. doi: 10.1016/S0140-6736(20)30460-8. 395(10227) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gameiro S, Van den Belt-Dusebout AW, Smeenk JMJ, Braat DDM, Van Leeuwen FE, Verhaak CM. Women's adjustment trajectories during IVF and impact on mental health 11-17 years later. Hum Reprod Oxf Engl. 2016;31(8):1788–1798. doi: 10.1093/humrep/dew131. [DOI] [PubMed] [Google Scholar]
- 44.Vaughan DA, Shah JS, Penzias AS, Domar AD, Toth TL. Infertility remains a top stressor despite the COVID-19 pandemic. Reprod Biomed Online. 2020;41(3):425–427. doi: 10.1016/j.rbmo.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dutta S, Sengupta P. SARS-CoV-2 and male infertility: possible multifaceted pathology. Reprod Sci Thousand Oaks Calif. 2021;28(1):23–26. doi: 10.1007/s43032-020-00261-z. Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rong L, Tailang Y, Fang F, Qin L, Jiao C, Wang Y, et al. Potential risks of SARS-CoV-2 infection on reproductive health. Reprod Biomed Online. 2020;41(1):89–95. doi: 10.1016/j.rbmo.2020.04.018. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schwartz DA. An analysis of 38 pregnant women with COVID-19, their newborn infants, and maternal-fetal transmission of SARS-CoV-2: maternal Coronavirus infections and pregnancy outcomes. Arch Pathol Lab Med. 2020 doi: 10.5858/arpa.2020-0901-SA. Mar 17. [DOI] [PubMed] [Google Scholar]
- 48.Juan J, Gil MM, Rong Z, Zhang Y, Yang H, Poon LC. Effect of coronavirus disease 2019 (COVID-19) on maternal, perinatal and neonatal outcome: systematic review. Ultrasound Obstet Gynecol. 2020;56(1):15–27. doi: 10.1002/uog.22088. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yu N, Li W, Kang Q, Xiong Z, Wang S, Lin X, et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-centre, descriptive study. Lancet Infect Dis. 2020;20(5):559–564. doi: 10.1016/S1473-3099(20)30176-6. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yuan S, Liao Z, Huang H, Jiang B, Zhang X, Wang Y, et al. Comparison of the indicators of psychological stress in the population of Hubei province and non-endemic provinces in China during two weeks during the Coronavirus disease 2019 (COVID-19) outbreak in February 2020. Med Sci Monit Int Med J Exp Clin Res. 2020 doi: 10.12659/MSM.923767. Apr;26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]