Abstract
OBJECTIVES:
To understand physician organization (PO) responses to financial incentives for quality and total cost of care among POs that were exposed to a statewide multipayer value-based payment (VBP) program, and to identify challenges that POs face in advancing the goals of VBP.
STUDY DESIGN:
Semistructured qualitative interviews and survey.
METHODS:
We drew a stratified random sample of 40 multispecialty California POs (25% of the POs that were eligible for incentives). In-person interviews were conducted with physician leaders and a survey was administered on actions being taken to reduce costs and redesign care and to discuss the challenges to improving value. We performed a thematic analysis of interview transcripts to identify common actions taken and challenges to reducing costs.
RESULTS:
VBP helps to promote care delivery transformation among POs, although efforts varied across organizations. Investments are occurring primarily in strategies to control hospital costs and redesign primary care, particularly for chronically ill patients; specialty care redesign is largely absent. Physician payment incentives for value remain small relative to total compensation, with continued emphasis on productivity. Challenges cited include the lack of a single enterprisewide electronic health records platform for information exchange, limited ability to influence specialists who were not exclusive to the organization, lack of payer cost and utilization data to manage costs, inability to recoup care redesign investments given the small size of VBP incentives, and lack of physician cost awareness.
CONCLUSIONS:
Transformation could be advanced by strengthening financial incentives for value; engaging specialists in care redesign and delivering value; enhancing partnerships among POs, hospitals, and payers to align quality and cost actions; strengthening information exchange across providers; and applying other strategies to influence physician behavior.
Policy makers and payers are implementing new provider payment models to incentivize improvements in value, and they are experimenting with different approaches to determine how best to design provider incentives to achieve desired effects.1–10 Applying incentives is intended to serve as a catalyst for change to close large gaps in quality performance.11 However, studies examining the association between pay-for-performance (P4P) incentives and quality improvement in ambulatory care have found mixed results and modest improvements.12–14 Despite many P4P interventions failing to show desired effects, little qualitative research has explored provider responses to incentives, whether they are making the changes needed to affect quality and costs, and factors that may explain why there has been small or no improvement in performance. The lack of evidence is notable given substantial investments in a new generation of payment initiatives that incentivize providers for both cost and quality.
Examining responses to value-based payment (VBP) can help determine whether programs are functioning as intended, motivating providers to redesign care delivery to improve value.15,16 Further, identifying challenges that providers are encountering could be used to refine VBP program design, increasing the prospect that value-based care transformations succeed. Our research objectives were to examine care delivery changes among physician organizations (POs) exposed to the California Integrated Healthcare Association (IHA)’s Value Based Pay for Performance (VBP4P) program, one of the nation’s largest VBP programs, and to identify challenges that POs are encountering in working to improve value. Examining California’s VBP experiment is important because California has served as a national bellwether for healthcare organization and delivery innovation, including fostering the development of health maintenance organizations (HMOs) and preferred provider organizations, creating quality and cost transparency tools for consumers, and pioneering the use of performance-based payments.6,17
METHODS
The IHA VBP4P Program
IHA implemented VBP4P starting in 2013, reconfiguring its quality-based P4P program, which began in 2003.6,18 VBP4P is composed of public reporting, public recognition awards, and value-based incentives.19 Using common measures, VBP4P aligns performance measurement across California’s 9 largest commercial HMO and point-of-service plans. These plans represent 180 multispecialty medical groups and independent practice associations (IPAs) (approximately 35,000 physicians), which care for 95% of California’s commercial HMO/point-of-service enrollees. The POs receive population-based payments under full or professional risk capitation arrangements, reflective of a category 4 payment model.20
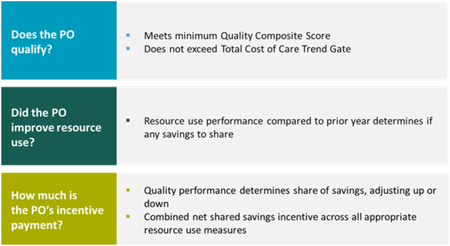
POs earn shared savings based on quality, total cost of care (TCC), and resource utilization. To earn shared savings, a PO must (1) meet performance thresholds for quality and TCC trend and (2) reduce resource utilization over the prior year (Figure 1).21 For high-performing POs with little ability to demonstrate year-over-year improvement, IHA added attainment thresholds in 2016 for maintaining excellent resource management. The 2013 TCC trend was the consumer price index (CPI) plus 3% as the standard threshold and CPI plus 1% for high-cost POs. Earned savings are quality adjusted; quality multipliers range from 0.65 to 1.35, corresponding to a PO earning from 33.0% to 68.0% of generated savings. In 2015, plans paid $23.4 million in incentive payments (across plans, between $9 and $41 per member per month).
FIGURE 1.
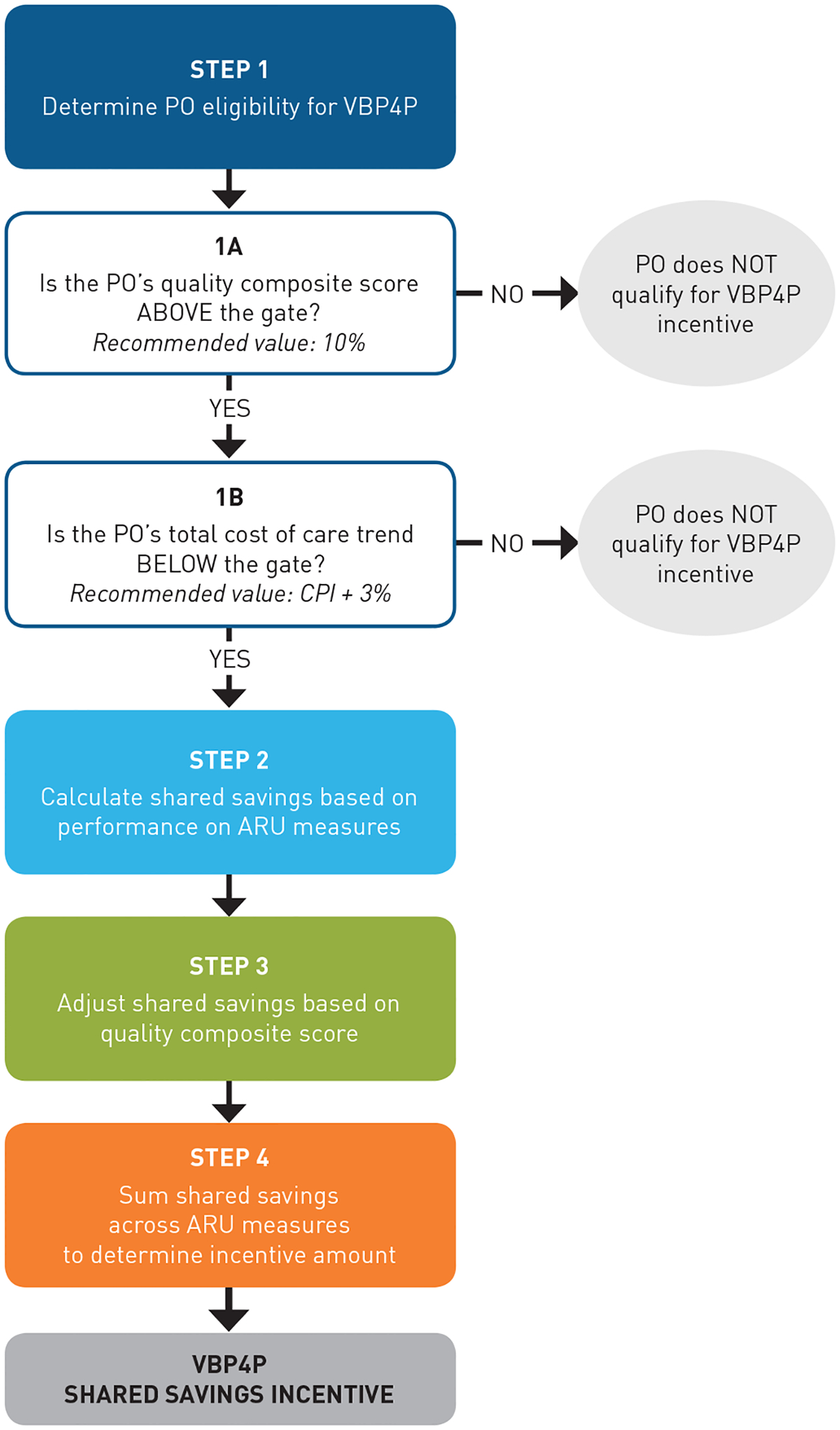
IHA VBP4P Description10
ARU indicates appropriate resource use; CPI, Consumer Price Index; IHA, Integrated Healthcare Association; PO, physician organization; VBP4P, Value Based Pay for Performance.
Source: Reproduced10 (with minor style edits) with permission from IHA.
Quality measures included 25 clinical measures (Healthcare Effectiveness Data and Information Set), 6 patient experience measures (Clinician and Group Consumer Assessment of Healthcare Providers and Systems survey), and meaningful use of health information technology (IT).22 In 2014, IHA shifted from meeting CMS Meaningful Use standards to the ability to submit electronic clinical quality measures from the electronic health record (EHR) (ie, for blood pressure, screening for depression).
The TCC measure included average total annual payments to all providers who care for patients, including hospital, ambulatory, prescription drug, and ancillary services, and administrative payments and adjustments. Each PO’s TCC is computed and aggregated across plans to generate the average TCC per PO, adjusting for patient mix (using the concurrent DxCG Relative Risk Score [Sightlines DxCG Risk Solutions software, version 3.1.0 (Verscend Technologies; Waltham, Massachusetts)]) and geography (using the Medicare hospital wage index geographic adjustment factor).23,24
Resource utilization measures included inpatient bed days per 1000 member-years, all-cause readmissions, emergency department (ED) visits per 1000 member-years, outpatient procedures in preferred facility, and generic prescribing.
Sample Selection
We randomly sampled 40 POs from 156 POs eligible to earn shared savings in 2014 (with complete 2013 quality and TCC data), stratifying by geography to capture variation in market competition, capitation rates, and cost performance to examine a range of PO experiences. We hypothesized that differences in competition, capitation rates, and cost performance might affect PO responses to VBP4P. The 156 POs were stratified into 6 cost groups based on their absolute 2010 TCC level and 3-year TCC trend (2010–2012) prior to VBP implementation. We excluded 1 cost group (n = 8 POs) with unstable multiyear cost trend estimates (suggesting data completeness/quality issues) and very small POs (<5000 enrollees) with large year-to-year variation (n = 39 POs), leaving 108 POs for sampling.25
We sampled proportional to the number of POs in each cost group, with at least 3 POs from each of 5 regions. We replaced nonrespondents (n = 14) with POs from the same region and cost group; when no replacement was available, we drew a replacement from the same cost group, or, if no replacement was available from the same cost group, from the same region. The 40 sampled POs were not significantly different from the 108 POs eligible for sampling (Table). RAND’s Human Subjects Protection Committee approved the study.
TABLE.
Descriptive Characteristics of California POs in Study Sample, IHA VBP4P Program, 2013
| POs in IHA VBP4P (n = 108) | n | POs Interviewed (n = 40) | n | P a | |
|---|---|---|---|---|---|
| Mean number of members enrolled | |||||
| <10,000 (small) | 43.5% | 47 | 47.5% | 19 | .071 |
| 10,000–24,999 (medium) | 29.6% | 32 | 30.0% | 12 | |
| ≥25,000 (large) | 26.9% | 29 | 22.5% | 9 | |
| PO model type | |||||
| Medical group | 38.0% | 41 | 45.0% | 18 | .248 |
| IPA | 62.0% | 67 | 55.0% | 22 | |
| Health system affiliation | |||||
| PO is part of a larger health system | 41.1% | 44 | 45.0% | 18 | .529 |
| Region | |||||
| Bay Area/Sacramento | 21.3% | 23 | 20.0% | 8 | .693 |
| Central Valley/Coast | 13.0% | 14 | 10.0% | 4 | |
| Riverside, San Bernardino (Inland Empire) | 13.9% | 15 | 20.0% | 8 | |
| Los Angeles | 29.6% | 32 | 27.5% | 11 | |
| Orange County/San Diego | 22.2% | 24 | 22.5% | 9 | |
| Performance on VBP4P measures | |||||
| Mean total cost of careb | $3731.39 | 108 | $3701.92 | 40 | .650 |
| Quality composite (0–100) | 61.80 | 108 | 64.63 | 40 | .085 |
IHA indicates Integrated Healthcare Association; IPA, independent practice association; PO, physician organization; VBP4P, Value Based Pay for Performance.
Based on χ2 goodness-of-fit test comparing the sample of 40 POs with the universe of 108 POs eligible for sampling in the VBP4P program.
Total cost of care is risk and geography adjusted.
Source: Data collected as part of the IHA VBP4P program and by the authors as part of the program evaluation.
Data Collection and Analysis
Between January 2015 and January 2016, we completed in-person, 2-hour, semistructured interviews with 1 or more senior leaders of each of the 40 POs. Participants included chief executive officers, chief medical officers, medical directors, and other leaders with a deep understanding of the VBP4P program and their organizations’ efforts to improve quality and total costs. Respondents also completed a brief survey on actions to reduce costs, reduce variation in care, and redesign primary care (eAppendix [available at ajmc.com]). Interviews were recorded, and we conducted a thematic analysis of transcribed interviews to identify common actions taken and challenges encountered. For survey and categorical response items, we computed counts and proportions.
Interview topics addressed (1) cost reduction targets and actions taken to reduce costs, (2) primary and specialty care redesign efforts, (3) strategies used to reduce practice variation, (4) physician incentives and alternative payment models (APMs), and (5) challenges to moderating costs and improving value.
RESULTS
Actions to Reduce Costs
Nearly all PO leaders reported taking some action to reduce costs in response to VBP4P. Reducing hospital-related costs (admissions, readmissions, and length of stay) was reported by 39 of 40 POs as their most important cost reduction target, followed by ED use (n = 22), use of specialty drugs (n = 14), generic drug substitution (n = 8), chronic disease management (n = 8), use of ambulatory surgery centers (n = 7), and use of complex imaging (n = 5).
PO leaders reported that accountability under VBP4P is driving greater organizational investments to reduce costs. Actions taken to reduce costs (Figure 2) focused heavily on reducing hospital utilization through improved ambulatory care access, tighter management of high-risk patients, and strengthening care transitions. PO leaders reported redirecting patients from the ED to ambulatory settings, using risk-prediction tools to identify patients at risk of hospitalization, strengthening case management, using multidisciplinary care teams, off-loading primary care physician (PCP) management of complex patients by centralizing their care in specialized clinics, and using ambulatory surgery centers. While most (n = 30/40) reported having a “preferred” hospital, few POs selected hospitals based on cost (n = 4) or quality (n = 4). Geographic convenience, health system affiliation, or participation in the plan network were cited as more important decision factors. POs reported lacking hospital cost information to steer patients to lower-cost facilities.
FIGURE 2.
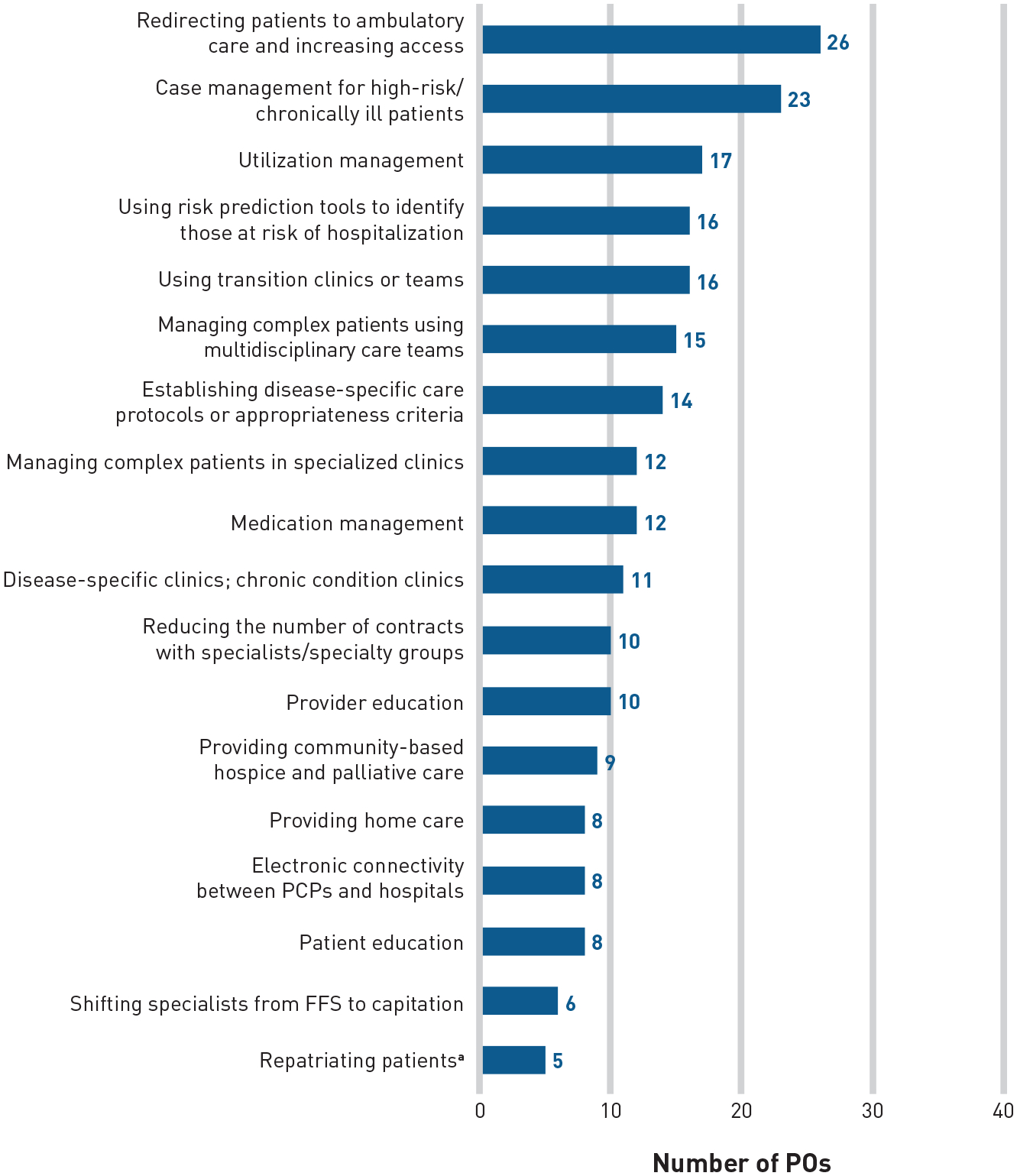
Actions That California PO Leaders Reported Taking to Reduce Total Cost of Care, 2016
FFS indicates fee-for-service; PCP, primary care physician; PO, physician organization.
aRepatriating patients refers to the practice by POs of moving their enrolled patients who have been admitted to hospitals outside their system back to their system’s hospital, in order to better manage and coordinate the care they receive.
Source: Data collected by the authors during interviews with 40 PO leaders, 2016.
POs noted that depression, chronic pain, and medication reconciliation are important drivers of hospitalizations, ED visits, and primary care costs; many POs reported that they have embedded, or plan to embed, behavioral health and pharmacy professionals within their ambulatory practices (results not shown). Other cost reduction actions taken include changing specialty care payment away from fee-for-service (FFS) to capitation and reducing the number of contracted specialists and specialty groups.
Actions to Redesign Primary Care
Most POs (n = 29/40) reported redesigning primary care. Substantial experimentation and variation exist among POs in their redesign efforts, with some having scaled care redesign across their organizations, whereas others were conducting small-scale pilots. Redesign focused mostly on managing chronically ill patients, often deploying elements of the patient-centered medical home model. PO leaders reported a range of activities to improve access, better track patients, and provide information support to frontline physicians (Figure 3).
FIGURE 3.
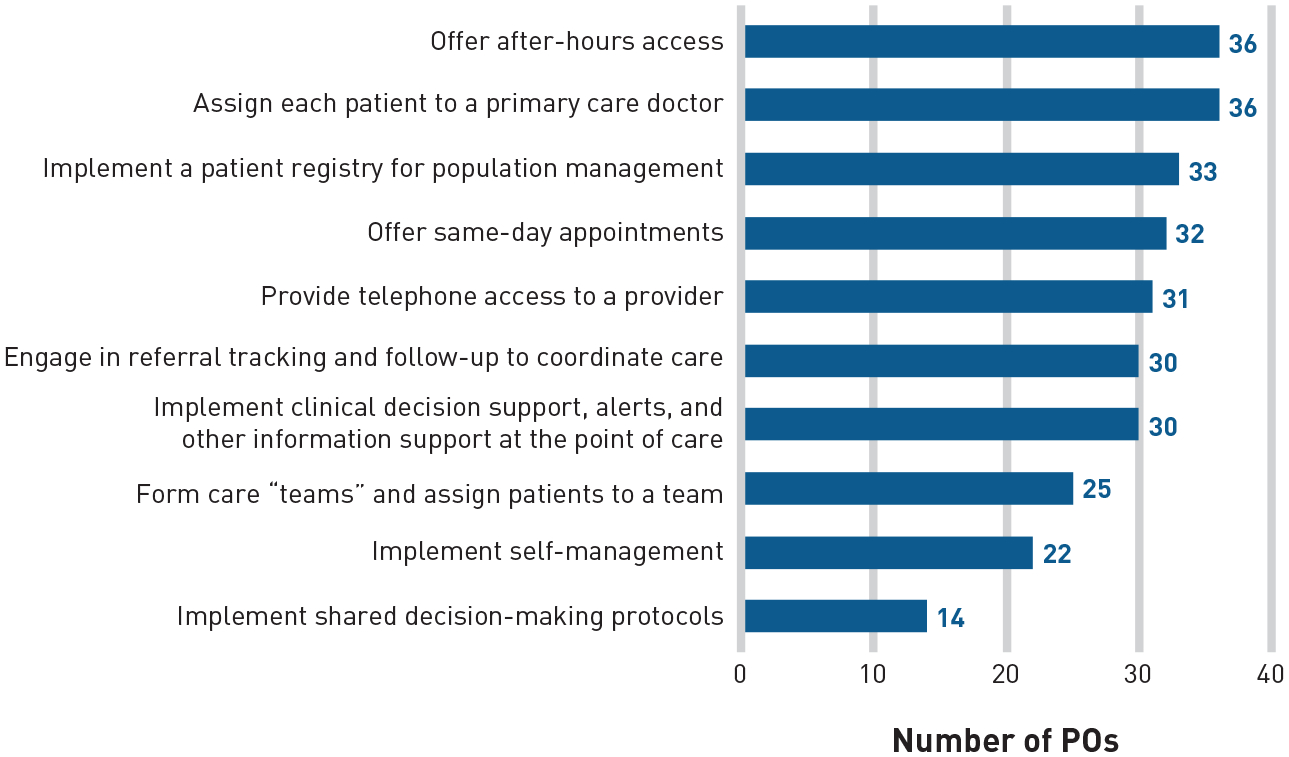
Actions That California PO Leaders Reported Taking to Redesign Primary Care, 2016
PCP indicates primary care physician; PO, physician organization.
Source: Data collected by the authors in the structured survey of 40 PO leaders, 2016.
Actions to Redesign Specialty Care
Specialty care redesign was reported less often (n = 22/40), although most POs acknowledged the need for redesign. When reported, efforts focused on areas of costly specialty care use (eg, oncology, use of pharmaceuticals and cardiology, anticoagulation clinics). PO leaders cited challenges with specialty care redesign because specialists frequently were nonexclusive or not employed by and integrated into a PO’s organizational strategies, EHR platform, and management system.
Actions to Reduce Practice Variation
Most POs (n = 36/40) worked to reduce practice variation to lower spending, although the intensity of efforts varied (Figure 4). Most reported applying traditional approaches (ie, utilization management, physician education and coaching). Fewer than half reported having embedded clinical decision support (CDS) tools or appropriateness criteria into their EHRs to reduce variation and overuse of low-value services. Only a handful routinely conducted data analysis and profiled physicians to identify and reduce practice variation, commenting that it requires sophisticated analytical capabilities and is cost prohibitive for small organizations. Most PO leaders described their efforts as modest, acknowledging that more could be done.
FIGURE 4.
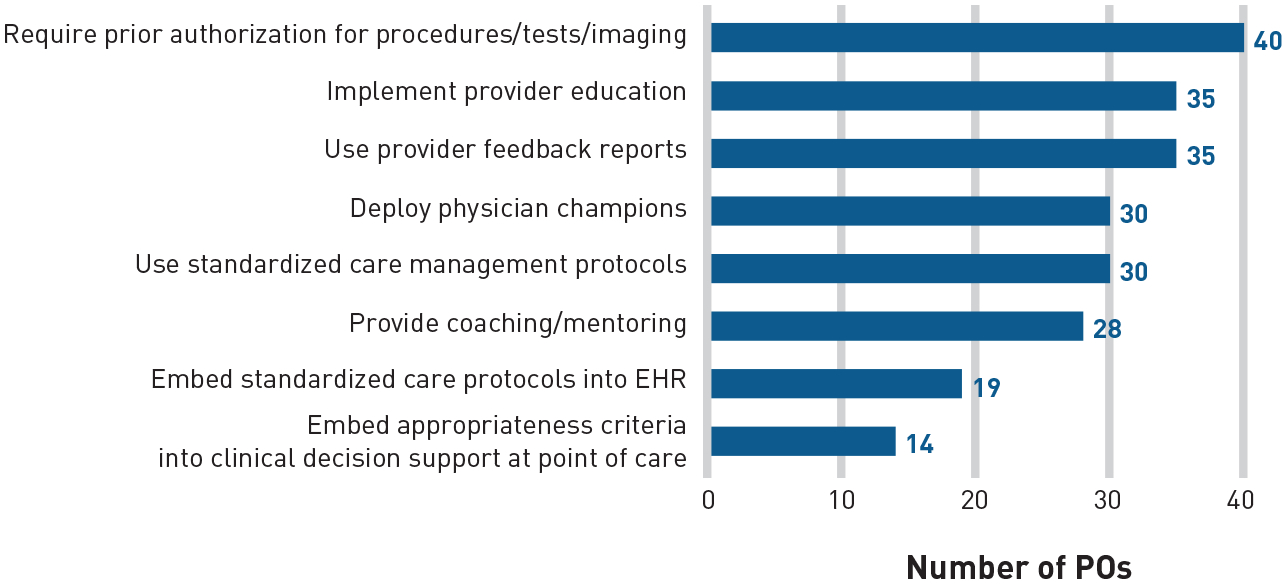
Actions That California PO Leaders Reported Taking to Reduce Practice Variation, 2016
EHR indicates electronic health record; PO, physician organization.
Source: Data collected by the authors in the structured survey of 40 PO leaders, 2016.
A majority of POs (n = 37/40; all except for 3 small IPAs) provided physician-level quality performance feedback; fewer (n = 18/40) provided cost/utilization feedback. Some POs reported shifting to electronic dashboards in the EHR (n = 19/37) to show physicians real-time performance on a broad set of measures, which leaders viewed as more useful for improvement than annual/quarterly profiles.
Frontline Physician Incentives and APMs
Most PO leaders reported that their PCPs are salaried employees or receive capitated payments, with a few paying PCPs on an FFS basis. In contrast, most specialists were paid on an FFS basis and many worked across multiple POs.
Most POs financially incentivized PCPs, focusing on quality and patient satisfaction (n = 36/40), resource use (n = 19/40), Medicare Hierarchical Condition Category Risk Adjustment Factor coding and annual senior wellness visits (n = 18/40), and panel size or productivity (ie, billable relative value units) (n = 9/40). Some POs cited liability concerns (n = 3/40) associated with undertreatment as a reason for not tying incentives to costs/utilization. POs most often reported financially incentivizing physicians for VBP4P, Medicare Advantage star ratings, and Physician Quality Reporting System measures.
The average overall PCP performance-based incentive (which could include quality, patient experience, cost/resource use, and other) represented less than 5%, on average, of total compensation (range, <1%–30%). Incentives tied specifically to clinical quality and patient experience performance ranged from less than 1% to 25% of total compensation (mean, 8.25%), whereas incentives for resource utilization ranged from less than 1% to 10% (mean, 3.5%). In some POs, PCPs were also eligible for annual revenue-sharing incentives based on the organization’s profitability. In one case, revenue sharing represented up to 30% of total compensation.
Fewer POs financially incentivized specialists for performance on quality (n = 17/40) or resource use (n = 15/40). When incentivized, the POs typically incentivized only a few specialties (eg, cardiology, ophthalmology) and the magnitude was similar to PCP incentives: quality (range, <1%–30%; mean, 7.6%) and resource use (range, <1%–10%; mean, 4.6%).
Many POs participated in APMs, although efforts typically were limited in scope, applying to a small subgroup of patients with a certain clinical condition (bundled payments) or a small fraction of the PO’s total patient population.
Challenges
Although most leaders (n = 28/40) reported that their PO has some influence over TCC, they highlighted challenges to reducing costs. Although hospital costs are a large component of the total costs, POs rarely had any role in selecting the hospitals in a plan’s network and lacked hospital cost information needed to steer patients to lower-cost facilities.
PO leaders also cited health IT challenges, especially among IPAs. Many POs lacked an enterprisewide EHR for all affiliated physicians to promote information exchange and facilitate performance monitoring. Few POs reported electronic connectivity between their PCPs and affiliated hospital(s) (n = 8/40), creating obstacles to sharing real-time patient information on admissions and facilitating postdischarge care. When a common EHR was present, PO leaders reported that it increased data sharing between PCPs and specialists, preventing unnecessary referrals and duplicate testing. POs also credited data sharing as facilitating the formation of clinically integrated networks, facilitating performance monitoring, enabling POs to identify outlier providers to reduce variation, and determining where to focus redesign efforts. Many leaders reported that their EHR included CDS functionalities, but the CDS frequently targeted only a few conditions and focused mainly on reducing gaps in care (eg, preventive screening). Less than half (n = 19/40) reported having embedded standardized care protocols into their EHRs.
Nearly all PO leaders cited data challenges, including the absence of real-time patient utilization information from plan partners on ED, hospital, and pharmacy use and inadequate internal data infrastructure for real-time quality monitoring and frontline care delivery.
PO leaders reported difficulty securing resources to proactively and intensively manage high-risk patients and expressed concerns about recouping their clinical and health IT investments to support care redesign, given small VBP incentives. POs also cited cultural challenges and a lack of physician cost awareness that affected their ability to make changes necessary to improve quality and cost performance.
DISCUSSION
Our study of a representative sample of California POs reveals that accountability for total cost and quality is transforming care delivery, although with varying intensity and reach across POs in the changes being deployed. Reform is uneven for a variety of reasons, including resource constraints, differing organizational structures (ie, IPA vs medical group) that affect the extent of integration (particularly around shared data systems and information exchange), and the amount of influence that a PO can exert on physician behavior when physicians are not exclusive to the PO. The ability to engage in data-driven work to reduce variations is hampered by a lack of resources and analytic expertise, as well as challenges in pulling together data from multiple EHR platforms.
Redesign efforts focus almost exclusively on primary care, are incremental in nature, address only a limited number of clinical conditions, and often have not been scaled organization-wide. Specialty care redesign remains rare despite specialty care costs being a large component of total costs. Specialty care redesign is more difficult because specialists are not typically integrated into the POs’ organizational strategies, EHR platforms, and management systems, given nonexclusive employment arrangements. Our findings are consistent with those of a 2016 study on how healthcare organizations are attempting to manage cost of care.26 With hospital services representing one-third (34%) of total costs,27 PO actions to manage costs focused heavily on hospital spending.26,28 Among POs not financially integrated with hospitals, focusing on averting inpatient utilization offers the benefit of achieving savings without threatening PO profitability.
Incentives to frontline physicians for cost and quality performance remain small; productivity incentives remain key drivers of behavior. Liability concerns about undertreatment related to incentivizing physicians for cost/utilization reductions highlight a barrier to the effectiveness of using financial incentives to reduce low-value care. APMs were being tested, although efforts remain small-scale. For most POs in our study, Medicare and commercially insured FFS patients still represent a substantial share of patient volume, minimizing organizational incentives to change care delivery.
Some employers and plans are using cost sharing to steer patients to lower-cost hospitals.29–31 However, we did not find evidence that POs are similarly engaged. Besides lacking the requisite cost data, significant obstacles exist to POs steering patients to less costly hospitals, specifically the geographic convenience of hospitals to patients and physicians, pressure to use the health system–affiliated hospital (when the PO is in a health system), and a lack of control by the PO over which hospital a patient can elect to use, which is determined by their insurance coverage.
Policy Implications
Our study highlights 4 important issues that policy makers and providers should consider to further transform care delivery.
Increase attention on specialty care.
To achieve greater impact on quality and spending, VBP programs should strive to include specialists in performance measurement and accountability. The dearth of specialty care measures highlights needed investments to develop measures to enable payers and PO leaders to provide performance feedback and hold specialists accountable for quality and controlling spending. Additionally, POs should consider addressing structural barriers resulting from the lack of specialist exclusivity and integration with POs (eg, creating the ability to share information across different EHR platforms to facilitate delivery of high-quality, efficient care).
Strengthen incentives for change.
Because payment redesign is evolving slowly, it remains a significant barrier to innovation. Moving a larger fraction of a PO’s overall revenue stream away from FFS to risk-based payments will strengthen signals for care redesign and foster better integration and coordination between PCPs and multiple specialists involved in a patient’s care.
Develop partnerships among POs, plans, and hospitals to integrate care delivery and manage costs.
Incentives and payment structures that foster partnerships for integrated care delivery, rather than care delivered by independent actors, as currently occurs, could promote further improvements. POs will need to partner with health plans and hospitals to manage patient populations, as they are limited in what they alone can do to slow the upward cost trend.
Strengthen the health IT infrastructure.
Addressing gaps in the health IT infrastructure of POs could support value improvements, particularly the sharing of clinical information across physicians within POs and between POs and hospitals through a single enterprisewide EHR platform; increase the use of CDS to promote delivery of evidence-based care and reduce practice variation; and provide real-time point-of-care access to information and performance feedback.32
Limitations
The 40 POs studied varied in size, market, group type, and performance. Because all of the POs were multispecialty POs with risk-based contracting experience, the findings may not generalize to POs in other states. However, physicians in other regions are increasingly consolidating into multispecialty POs and accepting risk-based contracts. Because payers across the United States are implementing similar VBP programs with physicians, we believe that responses of POs in other regions would be similar.
CONCLUSIONS
Early indications suggest that value-based incentives are leading to changes; however, incentives remain small, potentially limiting their effectiveness in driving the significant changes needed to derive large improvements in performance.5,33–35 Payers and PO leaders have been slow to increase the size of incentives to make them more impactful, and payment reform that would apply greater pressure for care redesign is difficult and slow going.5 What, then, might help advance the goal of improving value in healthcare in the near term?
Drawing from the field of behavioral economics, POs may be able to make structural changes to the practice environment by changing the “choice architecture” for frontline physicians in ways that would improve quality and reduce costs.36 For example, POs could leverage an improved health IT infrastructure, creating defaults in the EHR to enhance the likelihood that physicians take the preferred action (eg, ordering the first-line medication) and reduce the frequency of undesired actions (eg, creating a “hard stop” on imaging for low back pain absent justification), as well as structuring complex choices between alternative treatments, particularly when the evidence on what to do is less certain.36,37 By facilitating delivery of appropriate care, such structural supports may help POs achieve larger improvements in performance than have been achieved with small financial incentives.5,35
TAKEAWAY POINTS.
Value-based payment (VBP) is promoting care delivery transformation among California physician organizations (POs).
Investments are occurring primarily in strategies to control hospital costs and redesign primary care.
Few POs reported addressing specialty care redesign, practice variation, and low-value care, which are important cost drivers.
Advancing the goals of VBP further may require strengthening financial incentives for value; engaging specialists in care redesign and delivering value; enhancing partnerships among POs, hospitals, and payers to align quality and cost actions; strengthening information exchange across providers; and applying other strategies to influence physician behavior.
Acknowledgments
The authors thank the POs that contributed their time to participate in the study. They appreciate the helpful comments on the draft manuscript provided by Dolores Yanagihara from the Integrated Healthcare Association, Susan Paddock from RAND, and Jose Escarce from University of California at Los Angeles.
Source of Funding:
This work was supported through grant funding from the National Institutes of Health (NIH) Common Fund (5R33AG044252-04) and a cooperative agreement from the Agency for Healthcare Research and Quality (AHRQ) (1U19HS024067-01) to RAND’s Center of Excellence on Health System Performance. The content and opinions expressed in this publication are solely the responsibility of the authors and do not reflect the official position of NIH, AHRQ, or HHS.
Technical Appendix. Are Value-based Incentives Driving Behavior Change to Improve Value?
Appendix Exhibit A1: Integrated Healthcare Association Value-based P4P program Description
Source: Integrated Healthcare Association, www.iha.org, 2017.
Description of Total Cost of Care (TCC) Measure
Total cost of care (TCC) measures the average total annual payment to providers to care for a patient, including hospital, ambulatory, prescription drug, and ancillary services, as well as administrative payments and adjustments. TCC is estimated by computing the total cost per patient incurred by each of the plans and then aggregating across the plans to generate the average TCC per PO. The TCC is adjusted to account for differences across POs in patient age, gender, and health status, identified through diagnosis codes on patient claims and encounters. Patient-level relative risk scores (RRS) are computed using the DxCG Relative Risk software14. RRS is normalized so that a RRS of 1.0 represents the average risk across the population. RRS for all patients belonging to a PO are then combined to calculate PO-level RRS score. The PO-level risk score is the sum of patient-level observed costs for all patients in PO divided by the sum of patient-level expected costs for these patients, which is then multiplied by the population average cost, where expected cost for a patient equals the normalized RRS for patient multiplied by the population average cost, and where the population average cost is the sum of observed costs for all patients divided by the sum of member years enrolled for all patients. TCC is further adjusted for geographic differences in wages using the Centers for Medicare and Medicaid Services’ hospital wage index.
Description of sampling approach
We drew a stratified random sample of 40 physician organizations from the 156 POs with 2013 measurement year quality and TCC data that were eligible to earn shared savings in 2014 (15). We sampled using geographic region and cost performance, factors we hypothesized might affect PO responses to VBP4P. The 156 POs were divided into six cost groups based on their absolute 2010 TCC level and the three-year TCC trend (from 2010–2012, the time period prior to the start of VBP4P in 2013). We excluded one PO cost group (n=8 POs) from sampling because it contained unstable multi-year cost trend estimates (suggesting data completeness/quality issues) and very small POs (<5,000 HMO and POS commercial enrollees) because of low VBP4P program engagement (n=39), leaving 108 POs for sampling.1 Within each cost group, we sampled proportional to the number of POs in that group. The sample contained at least three POs from each of five geographic market regions (Los Angeles, Inland Empire, Orange County and San Diego, San Francisco/Bay Area, and the Central Valley/Coast). Exhibit A2 compares the sampled POs against the universe of POs eligible for sampling. There were no significant differences between the sample and the universe of POs.
Appendix Exhibit A2. Interview Topics and Questions
| Interview Topics | Questions |
|---|---|
| Cost Reduction Targets and Activities |
|
| Attempts to Address Hospital Costs |
|
| Redesigning Care Delivery |
|
| Participation in Alternative Payment and Service Delivery Models |
|
| Reduction of Variation in Practice |
|
| Use of Data for Physician Performance Profiling |
|
| Use of Performance Incentives for Physicians |
|
| Attitude Toward IHA Value-Based P4P Program |
|
Appendix Exhibit A3. Structured Survey Questions
-
Is your PO currently participating in any alternative payment or service delivery models, such as Accountable Care Organizations (ACOs), bundled payment arrangements, global payments?
Which insured populations do these involve?Yes/No Type of Innovation (e.g., ACO, bundled payment, global payment) Include upside risk only (yes/no) Include downside risk (yes/no) Commercial HMO contracts Commercial PPO contracts Medicare FFS population Medicare Advantage population Medicaid population Does PO bear full financial risk (for professional, hospital, and pharmacy) in any commercial HMO contract? (YES/NO)
Does your PO bear full financial risk for any Medicare Advantage contracts? (YES/NO)
Does your PO bear full financial risk for any Medi-cal contracts? (YES/NO)
For what percentage of your total book of business do you estimate you are at full risk? (please estimate) __________________
For what percentage of your total book of business do you estimate you are at partial risk, that is for professional services only (please estimate)? ___________________
- Is your PO taking any specific actions to reduce the total cost of care? (YES/NO)
Actions implemented YES/NO Steering patients to lower cost hospitals Steering patients to lower cost specialists Performing a greater fraction of all surgeries in ambulatory surgery centers Using risk prediction tools to identify and more closely manage high risk patients Use of hospitalists Administrative—changes in staffing Administrative—closing or consolidating the number of practice locations Administrative—group purchasing for equipment/devices Administrative—IT solutions, such as e-scheduling Implementing the ABIM’s Choosing Wisely recommendations or other efforts to reduce the use of “low value” services? Other (please specify) - Is your PO making any specific changes to primary care?
Actions implemented YES/NO Assigned each patient to primary care doctor (patient empanelment) Access: Offer same day appointments Access: Provide telephone access to a provider Access: Offer after-hours access Care coordination: Engage in referral tracking and follow-up Continuous team-based healing relationships: Formed care “teams” and assigned patients to a team Data systems: Implemented a patient registry (for population management) Data systems: Implemented Clinical Decision Support (CDS), alerts, and other information support at the point of care Patient centered care interactions: Implemented shared-decision-making protocols Patient centered care interactions: Implemented self-management Quality improvement: Engage in quality measurement and feedback to primary care physicians Other (please specify) - Is your PO taking any specific actions to reduce variation in practice?
Actions implemented YES/NO Require prior authorization for certain procedures/tests/imaging Implemented provider education Deploy physician champions Use provider feedback reports Provide coaching/mentoring Use standardized care management protocols Embed standardized care protocols into EHR (alerts/reminders, CDS) Embed appropriateness criteria into clinical decision support tools at point of care Other (please specify)
Footnotes
Prior Presentation: Preliminary findings from this work were presented at the June 2016 AcademyHealth annual meeting in Boston, MA.
Author Disclosures: Dr Damberg is a nonvoting, noncompensated member (liason member) of the IHA Board; IHA itself is a convening entity and has no financial interest in the subject matter. The remaining authors report no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter of this article.
Burgette et al. Optimizing Sample Selection in the Face of Design Constraints: Use of Clustering to Define Sample Strata for Qualitative Research. 2017. Under review.
REFERENCES
- 1.Medicare Access and CHIP Reauthorization Act of 2015, 42 USC §1305 (2015).
- 2.Berwick DM. Launching accountable care organizations—the proposed rule for the Medicare Shared Savings Program. N Engl J Med. 2011;364(16):e32. doi: 10.1056/NEJMp1103602. [DOI] [PubMed] [Google Scholar]
- 3.Burwell SM. Setting value-based payment goals—HHS efforts to improve U.S. health care. N Engl J Med. 2015;372(10):897–899. doi: 10.1056/NEJMp1500445. [DOI] [PubMed] [Google Scholar]
- 4.Quality Payment Program overview. CMS; website. qpp.cms.gov/about/qpp-overview. Accessed December 18, 2017. [Google Scholar]
- 5.Damberg CL, Sorbero ME, Lovejoy SL, Martsolf GR, Raaen L, Mandel D. Measuring success in health care value-based purchasing programs: findings from an environmental scan, literature review, and expert panel discussions. Rand Health Q. 2014;4(3):9. [PMC free article] [PubMed] [Google Scholar]
- 6.Damberg CL, Raube K, Teleki SS, Dela Cruz E. Taking stock of pay-for-performance: a candid assessment from the front lines. Health Aff (Millwood). 2009;28(2):517–525. doi: 10.1377/hlthaff.28.2.517. [DOI] [PubMed] [Google Scholar]
- 7.Japsen B Anthem Blue Cross nears 60% value-based care spend. Forbes. April 27, 2017. forbes.com/sites/brucejapsen/2017/04/27/anthem-blue-cross-nears-60-value-based-care-spend. Accessed December 18, 2017.
- 8.Pearson SD, Schneider EC, Kleinman KP, Coltin KL, Singer JA. The impact of pay-for-performance on health care quality in Massachusetts, 2001–2003. Health Aff (Millwood). 2008;27(4):1167–1176. doi: 10.1377/hlthaff.27.4.1167. [DOI] [PubMed] [Google Scholar]
- 9.Tefera L Hospital Value-Based Purchasing (HVBP) Program. CMS; website. cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/HVBP/2013-2015-HVBP-Presentation-.pptx. Published 2015. Accessed March 7, 2018. [Google Scholar]
- 10.Yegian J, Yanagihara D. Value Based Pay for Performance in California. Integrated Healthcare Association; website. iha.org/sites/default/files/resources/issue-brief-value-based-p4p-2013.pdf. Published September 2013. Accessed April 4, 2018. [Google Scholar]
- 11.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 12.Eijkenaar F, Emmert M, Scheppach M, Schöffski O. Effects of pay for performance in health care: a systematic review of systematic reviews. Health Policy. 2013;110(2–3):115–130. doi: 10.1016/j.healthpol.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 13.Kondo KK, Damberg CL, Mendelson A, et al. Implementation processes and pay for performance in healthcare: a systematic review. J Gen Intern Med. 2016;31(suppl 1):61–69. doi: 10.1007/s11606-015-3567-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van Herck P, De Smedt D, Annemans L, Remmen R, Rosenthal MB, Sermeus W. Systematic review: effects, design choices, and context of pay-for-performance in health care. BMC Health Serv Res. 2010;10:247. doi: 10.1186/1472-6963-10-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asch B, Warner J. Incentive systems: theory and evidence. In: Lewin D, Mitchell D, Zaidi M, eds. Handbook of Human Resource Management. Stamford, CT: JAI Press; 1996:175–215. [Google Scholar]
- 16.Prendergast C The provision of incentives in firms. J Econ Lit. 1999;37(1):7–63. jstor.org/stable/2564725. [Google Scholar]
- 17.Damberg CL, Raube K, Williams T, Shortell SM. Paying for performance: implementing a statewide project in California. Qual Manag Health Care. 2005;14(2):66–79. [DOI] [PubMed] [Google Scholar]
- 18.AMP Commercial HMO. Integrated Healthcare Association; website. iha.org/our-work/accountability/value-based-p4p. Accessed November 1, 2016. [Google Scholar]
- 19.Value Based Pay for Performance (VBP4P) results & highlights measurement year (MY) 2015. Integrated Health Association; website. iha.org/sites/default/files/resources/2016-value-based-p4p-results.pdf. Published October 2016. Accessed January 7, 2019. [Google Scholar]
- 20.Alternative Payment Model Framework and Progress Tracking (APM FPT) Work Group. Alternative Payment Model (APM) Framework: final white paper. Health Care Payment Learning and Action Network; website. hcp-lan.org/workproducts/apm-whitepaper.pdf. Published January 12, 2016. Accessed January 7, 2019. [Google Scholar]
- 21.Yegian JM, Erickson L, Yanagihara D. Charting a course to value in physician group payment: key pay-for-performance design decisions. Integrated Healthcare Association; website. iha.org/sites/default/files/resources/value-based-p4p-design-issue-brief.pdf. Published November 2016. Accessed January 7, 2019. [Google Scholar]
- 22.Promoting Interoperability Programs Registration and Attestation System. CMS; website. https://ehrincentives.cms.gov/hitech/loginCredentials.action. Accessed March 1, 2018. [Google Scholar]
- 23.Wage index. CMS; website. cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/wageindex.html. Updated August 3, 2018. Accessed February 20, 2018. [Google Scholar]
- 24.Institute of Medicine. Geographic Adjustment in Medicare Payment: Phase I: Improving Accuracy. Washington, DC: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 25.Burgette LF, Escarce JJ, Paddock SM, et al. Sample selection in the face of design constraints: use of clustering to define sample strata for qualitative research [published online December 11, 2018]. Health Serv Res. doi: 10.1111/1475-6773.13100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hansen S, Stewart D. Managing cost of care: lessons from successful organizations. California Health Care Foundation; website. chcf.org/publications/2016/01/managing-cost-care. Published January 27, 2016. Accessed January 3, 2017. [Google Scholar]
- 27.Integrated Healthcare Association. Based on analyses of the aggregated plan claims data used to compute the total cost of care measure. Damberg C, ed. 2017. [Google Scholar]
- 28.Better care at lower cost: is it possible? The Commonwealth Fund; website. commonwealthfund.org/publications/health-reform-and-you/better-care-at-lower-cost. Published November 21, 2013. Accessed January 25, 2017. [Google Scholar]
- 29.Appleby J Companies steering workers to lower priced medical care. Kaiser Health News; website. khn.org/news/companies-steering-workers-to-lower-priced-medical-care. Published September 22, 2011. Accessed January 25, 2017. [Google Scholar]
- 30.Frank MB, Hsu J, Landrum MB, Chernew ME. The impact of a tiered network on hospital choice. Health Serv Res. 2015;50(5):1628–1648. doi: 10.1111/1475-6773.12291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robinson JC, MacPherson K. Payers test reference pricing and centers of excellence to steer patients to low-price and high-quality providers. Health Aff (Millwood). 2012;31(9):2028–2036. doi: 10.1377/hlthaff.2011.1313. [DOI] [PubMed] [Google Scholar]
- 32.Hussey PS, Eibner C, Ridgely MS, McGlynn EA. Controlling U.S. health care spending—separating promising from unpromising approaches. N Engl J Med. 2009;361(22):2109–2111. doi: 10.1056/NEJMp0910315. [DOI] [PubMed] [Google Scholar]
- 33.Doran T, Maurer KA, Ryan AM. Impact of provider incentives on quality and value of health care. Annu Rev Public Health. 2017;38:449–465. doi: 10.1146/annurev-publhealth-032315-021457. [DOI] [PubMed] [Google Scholar]
- 34.Hartley W, Dobosenski A. APP compensation: incremental approaches to incorporate value-based pay. American Medical Group Association; website. amga.org/docs/Meetings/AC/2017/Handouts/Dobosenski_Hartley.pdf. Published March 23, 2017. Accessed April 7, 2018. [Google Scholar]
- 35.Ogundeji YK, Bland JM, Sheldon TA. The effectiveness of payment for performance in health care: a meta-analysis and exploration of variation in outcomes. Health Policy. 2016;120(10):1141–1150. doi: 10.1016/j.healthpol.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 36.Thaler RH, Sunstein CR. Nudge: Improving Decisions About Health, Wealth and Happiness. New Haven, CT: Yale University Press; 2008. [Google Scholar]
- 37.Appropriate use criteria program. CMS website. cms.gov/medicare/quality-initiatives-patient-assessment-instruments/appropriate-use-criteria-program/index.html. Updated November 29, 2017. Accessed April 9, 2018.


