Abstract
Objectives:
Computed tomography (CT), the reference standard for diagnosis of intraabdominal injury (IAI), carries risk including ionizing radiation. CT-sparing clinical decision rules for children have relied heavily on physical examination, but they did not include focused assessment with sonography for trauma (FAST), which has emerged into widespread use during the past decade. We sought to determine the independent associations of physical examination, laboratory studies, and FAST with identification of IAI in children and to compare the test characteristics of these diagnostic variables. We hypothesized that FAST may add incremental utility to a physical examination alone to more accurately identify children who could forgo CT scan.
Methods:
We reviewed a large trauma database of all children with blunt torso trauma presenting to a freestanding pediatric emergency department during a 20-month period. We used logistic regression to evaluate the association of FAST, physical examination, and selected laboratory data with IAI in children, and we compared the test characteristics of these variables.
Results:
Among 354 children, 50 (14%) had IAI. Positive FAST (odds ratio [OR] = 14.8, 95% confidence interval [CI] = 7.5 to 30.8) and positive physical examination (OR = 15.2, 95% CI = 7.7 to 31.7) were identified as independent predictors for IAI. Physical examination and FAST each had sensitivities of 74% (95% CI = 60% to 85%). Combining FAST and physical examination as FAST-enhanced physical examination (exFAST) improved sensitivity and negative predictive value (NPV) over either test alone (sensitivity = 88%, 95% CI = 76% to 96%) and NPV of 97.3% (95% CI = 94.5% to 98.7%).
Conclusions:
In children, FAST and physical examinations each predicted the identification of IAI. However, the combination of the two (exFAST) had greater sensitivity and NPV than either physical examination or FAST alone. This supports the use of exFAST in refining clinical predication rules in children with blunt torso trauma.
Trauma is the leading cause of death and disability in children1 and unrecognized injury from blunt torso trauma is the third most common cause of preventable death in children sustaining blunt trauma.2 Computed tomography (CT) remains the reference standard for diagnosis of intraabdominal injury (IAI), but carries risk, including ionizing radiation.3 In the past 25 years, there has been a dramatic increase in the number of CT scans performed on children.4-8 However, the prevalence of IAI in children undergoing CT scan is only 6% to 15%,9-11 making many of these studies potentially avoidable by using safer screening methods12.
Evidence-based clinical decision rules have been created to limit CT scans in children with blunt torso trauma.10 These rules use medical history, clinical findings, and diagnostic testing to identify children with blunt torso trauma who have low risk for IAI and could safely avoid CT scans. However, the two most rigorous and recent prediction rules were developed without the focused assessment with sonography for trauma (FAST) examination, because many study sites were lacking expertise and a standard implementation pathway.10,13,14
Focused assessment with sonography for trauma is a bedside sonographic evaluation performed within minutes of the patient’s arrival by the treating provider, in conjunction with the physical examination, to rapidly identify intraperitoneal traumatic hemorrhage.15 FAST has been successfully integrated into the management of injured adult patients where it improves clinical outcomes including reducing CT scan usage.16 FAST has the potential to be an ideal diagnostic test in the evaluation of IAI in children given its portability, cost efficiency, lack of ionizing radiation, and rapid performance.17 However, previous studies have shown variability in the test characteristics of FAST in children, with reported sensitivities of 20% to 80%18-20 and specificities of 77% to 100%.19,21 There are several reasons for this variability in test characteristics including age of patient, injury type, timing of study, provider expertise in image acquisition and interpretation, confidence, and lack of implementation pathways.22,23 However, in the past decade there has been substantial improvement in the availability, education, and overall expertise in the use of pediatric-specific point-of-care ultrasound applications including FAST. With the increase in expertise of providers using pediatric emergency ultrasonography during the past decade, we believe FAST may have increasing utility and deserves a reevaluation in the assessment of children with blunt torso trauma as a strategy to reduce the use of CT scans. Therefore, we sought to determine the incremental independent associations of physical examination, laboratory studies, and FAST in predicting IAI in children presenting with blunt torso trauma and to compare the test characteristics of these predictors. We hypothesized that adding FAST would enhance the ability to predict IAI in the diagnostic approach in children with blunt torso trauma.
MATERIALS AND METHODS
Study Design and Population
We performed a retrospective chart review of the trauma database and EMRs of children younger than 18 years of age presenting to an academic, urban, freestanding Level I pediatric trauma center during a 20-month period from November 1, 2013, to July 31, 2015, when FAST was routinely used for children presenting with blunt torso trauma. This study was performed at a tertiary referral center for Northern California with an annual census of approximately 50,000 visits. The pediatric emergency department (ED) is staffed by board-certified pediatric emergency providers and has a full complement of specialists providing pediatric and trauma care. The hospital is an American College of Surgeons verified Level I trauma center. The UCSF Benioff Children’s Hospital Oakland institutional review board approved this study.
Trauma Database.
As part of the quality improvement program for trauma services, all patients regardless of disposition requiring a pediatric trauma evaluation in the ED were included in a database. Using this database, we included children younger than 18 years of age who met institutional trauma activation criteria and who also had a FAST performed. Children who had two or more trauma visits during the study period were included only once, and their first visit was selected. Mechanism of injury and International Classification of Disease, Ninth Revision (ICD-9) codes were obtained from the trauma database. Patients with penetrating injury or those who were transferred from a referring institution were excluded. Penetrating trauma was defined as any child with a presenting complaint related to penetrating injury (i.e., stab wound, gunshot wound) or final ICD-9 diagnosis of penetrating injury (see Data Supplement S1, available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1111/acem.13959/ full). The trauma database was then linked to the electronic medical record (EMR) and subsequently reviewed by two independent expert reviewers (AK, JF) using a standard data abstraction document. Any disagreement between the reviewers was given to a third independent expert for review (CN). Chart abstraction included patient demographics, physical examination findings, laboratory tests, radiographic findings, and the study’s primary and secondary outcomes.
Predictor and Outcome Variables.
Demographic and clinical information was collected, including age, sex, weight, mechanism of injury, Injury Severity Score, ED vital signs (respiratory rate, pulse rate, mean blood pressure), Glasgow Coma Score (GCS), ED disposition, ED length of stay (hours), and hospital length of stay (days). Predictor variables included physical examination findings, ED laboratory results, and FAST. Outcome variables collected included CT scan report, hospital course, procedures performed (ICD-9), and final diagnosis (ICD-9).
All physical examination findings of blunt torso trauma, including thoracic wall trauma, abdominal wall trauma, or abdominal tenderness, as documented by the emergency and trauma providers, were included in the analysis. An abnormal examination was defined a priori as outlined by Holmes et al.10 as evidence of thoracic wall injury (erythema, abrasion, ecchymosis, subcutaneous air, or laceration to the anterior or posterior chest wall; chest auscultation for absent or decreased breath sounds; thoracic tenderness; costal margin tenderness), abdominal injury (erythema, abrasion, ecchymosis, laceration, seat belt sign to the abdominal wall; abdominal tenderness; abdominal distention; abdominal auscultation for bowel sounds; peritoneal irritation; flank tenderness), or pelvic injury (pelvic bone tenderness or instability on palpation). Data were collected using a standardized data collection sheet. A physical examination was considered positive if any of the above findings were recorded as positive. Missing or omitted physical examinations were considered as negative. If data points were conflicting or ambiguous, they were reviewed by our third blinded author to reach consensus (CN).
Elevated liver enzymes were defined as abnormal if either serum aspartate aminotransferase (AST) was >200 IU/L or serum alanine aminotransferase (ALT) was >125 IU/L. Elevated pancreatic enzymes were defined as abnormal if there was an elevation of the serum lipase ≥100 IU/L.
Focused assessment with sonography for trauma examinations were performed and interpreted by the treating providers. Bedside interpretations by the treating provider were used as the study’s FAST interpretation. All providers participating in this study had undergone formalized didactic training and hands-on instruction. Completeness of FAST was based on the guideline published by the American College of Emergency Physicians.24 Treating providers performed standard FAST including views of the right upper quadrant, the splenorenal fossa, the long and short axis of the pelvis, and cardiac subxyphoid views. All FAST images were uploaded and backed up on a server for routine quality assurance (overread review), by the emergency ultrasound director asynchronously. Agreement between the bedside provider and the overread was measured with a Cohen’s kappa coefficient (j, 95% CI) for interrater agreement. In addition, we reviewed the CT scan interpretations for children with IAI who had both negative physical examination and FAST.
Outcome Measures
The primary outcome measure was the presence of IAI. The secondary outcome was the presence of IAI requiring acute intervention. The reference standard included CT scan or review of the medical record. CT scan results were those from the final interpretation by attending radiologist. The trauma database and hospital EMR were also reviewed for IAI. IAI has been defined by Holmes at al.10 as any radiographically or surgically apparent injury to the spleen, liver, urinary tract, gastrointestinal tract, pancreas, gallbladder, adrenal gland, intraabdominal vascular structure, or traumatic fascial defect. Similarly, the trauma database and the EMR of hospitalized patients were reviewed to identify patients who had IAI requiring acute intervention, defined as any IAI requiring blood transfusion for anemia resulting from hemorrhage, surgery, angiographic embolization, or intravenous fluids for 2 or more nights in patients with pancreatic or gastrointestinal injury.10
Data Analysis
For reporting the characteristics of the patient population, continuous variables were reported as median and interquartile ranges and categorical variables were presented as frequency and proportions. Predictor variables for univariate regression were chosen based on theoretical and previously demonstrated clinical significance. We determined a priori that 50 positive FAST studies could allow as many as five predictor variables to be included in our multivariate analysis.25 Univariate regression was used to evaluate each variable’s association with identification of IAI in the present study. Multivariate logistic regression modeling was used to further assess the association of each predictor with IAI. Variables that showed an association with a p-value of <0.2 were considered for multivariate logistic regression and included or eliminated using backward stepwise selection. We used an adjusted alpha level of <0.01 for the multivariate regression analysis. All continuous covariates were reviewed for influential data points and transformed or normalized as appropriate. Patients missing laboratory data were not included in the multivariate analysis. Measurement of goodness of fit was evaluated using Hosmer-Lemeshow test. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and positive and negative likelihood ratios (LR+/LR−) of included examinations were calculated using conventional definitions. All other statistical tests were two-sided with a p-value of <0.05 considered significant. Analyses were performed using SAS 9.4 (SAS Institute).
RESULTS
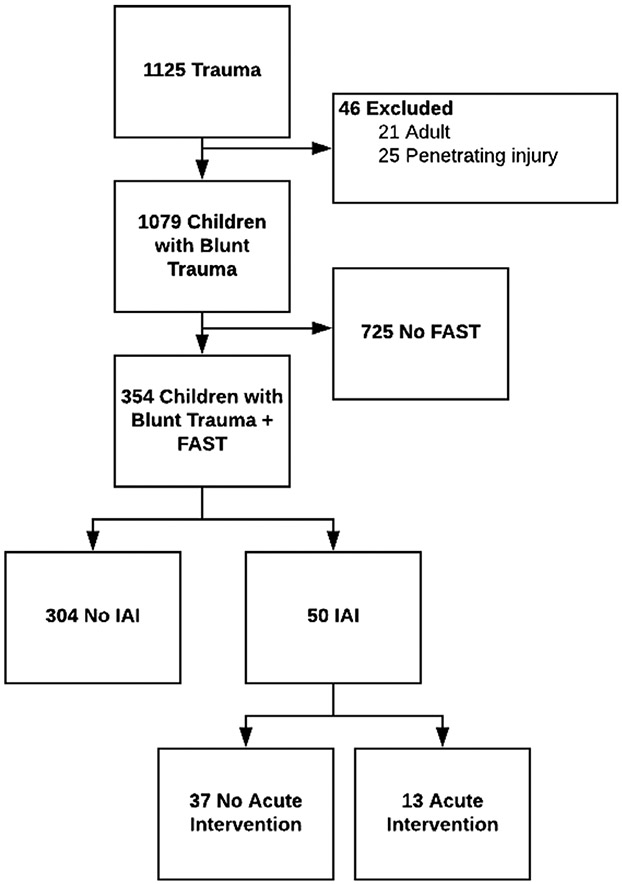
We identified 1,125 unique initial encounters from November 1, 2013, to July 31, 2015 (Figure 1). We excluded 21 patients (2%) older than 18 years of age and 25 patients (2%) who sustained penetrating injuries. Of the remaining children with blunt torso trauma, 725 patients (67%) did not receive a FAST because of lack of expertise or because FAST images were not available for review. Of the 354 remaining patients who were included in the analysis, more than 70% were younger than 12 years of age (Table 1). Nearly 70% of the sample were boys, and the majority had a mechanism of injury of either vehicle collision (motorized or nonmotorized) or fall from height. The majority of children in this cohort were admitted to the hospital, 287 patients (81%). There were 254 patients (72%) had full results for ALT and AST in addition to the examination data.
Figure 1.
Flow diagram. FAST = focused assessment with sonography for trauma.
Table 1.
Demographics and Characteristics of All Eligible Patients Without and With IAI
| Characteristics | Total (N = 354) |
No IAI (n = 304) |
IAI (n = 50) |
|---|---|---|---|
| Age (years) | 8 (4–12) | 8 (4–12) | 8 (6–11) |
| Age category (years) | |||
| 0–2 | 50 (14.1) | 47 (15.5) | 3 (6.0) |
| 3–6 | 93 (26.3) | 83 (27.3) | 10 (20.0) |
| 7–11 | 107 (30.2) | 81 (26.6) | 26 (52.0) |
| 12–15 | 102 (28.8) | 91 (29.9) | 11 (22.0) |
| 16–17 | 2 (0.6) | 2 (0.7) | 0 (0) |
| Male | 245 (69.2) | 207 (68.1) | 38 (76.0) |
| Weight (kg) | 30 (18–49) | 30 (17–50) | 30 (20–43) |
| ED GCS | 15 (15–15) | 15 (15–15) | 15 (15–15) |
| ISS | 4 (1–9) | 4 (1–9) | 11 (6–17) |
| Cause of injury | |||
| Vehicle collision (motorized and nonmotorized) | 182 (51.4) | 161 (53.0) | 21 (42.0) |
| Fall | 143 (40.4) | 118 (38.8) | 25 (50.0) |
| Hit | 14 (4.0) | 12 (4.0) | 3 (6.0) |
| Other | 15 (4.2) | 13 (4.3) | 1 (2.0) |
| ED disposition (%) | |||
| ICU | 78 (22) | 51 (16.8) | 27 (54.0) |
| Operating room | 20 (5.6) | 17 (5.6) | 3 (6.0) |
| Ward | 189 (53.4) | 169 (55.6) | 20 (40.0) |
| Home | 66 (18.6) | 66 (21.7) | 0 (0) |
| Transfer | 1 (0.3) | 1 (0.3) | 0 (0) |
Data are reported as median (IQR) or n (%).
IAI = intraabdominal injury; ICU = intensive care unit; IQR, interquartile range; ISS = Injury Severity Score; GCS = Glasgow coma score.
Fifty patients (14% of the cohort) had IAI while 304 patients (86%) did not. The age, sex, weight and GCS were similar between those groups with and without IAI (Table 1).
We identified the following variables as associated with the identification of IAI in children with blunt torso trauma: physical examination, FAST, liver enzymes, and lipase. Univariate analysis (Table 2) showed that FAST, physical examination, and abnormal liver enzymes were each associated with the identification of IAI in children with blunt torso trauma. Lipase, however, was not considered a good candidate variable for this model as it demonstrated multi-collinearity with liver enzymes and its values were missing for 37% of the population. In the multivariate regression model incorporating FAST, physical examination, and AST and ALT test results, only a positive FAST and physical examination continued to be significantly associated with identification of IAI in children with blunt torso trauma (Table 2). The overall model performance showed Hosmer and Lemeshow of χ2 = 1.52, p-value of 0.68, which indicates acceptable goodness of fit. We did not find significant outliers in any of the model covariates. Based on this analysis, we created a composite variable, FAST-enhanced physical examination (exFAST). If both FAST and physical examination were negative, the exFAST was negative. If at least one of the two variables were positive, the exFAST was positive.
Table 2.
Univariate and Multivariate Analysis for IAI in Children With Blunt Torso Trauma
| OR (95% CI) | AOR (95% CI) | |
|---|---|---|
| FAST | 14.8 (7.5–30.8) | 10.2 (3.9–29.3) |
| Physical examination | 15.2 (7.7–31.7) | 16.4 (6.3–48.3) |
| Abnormal AST | 15.3 (5.8–43.8) | 2.1 (0.1–32.9) |
| Abnormal ALT | 18.6 (7.5-49.8) | 5.4 (0.4-81.7) |
ALT = alanine enzymes; AOR = adjusted odds ratio; AST = aspartate enzymes; FAST = focused assessment with sonography for trauma.
We then determined the test characteristics of the exFAST for identifying IAI in children. Of those patients with an IAI, 44 (88%) were detected by the exFAST and six (12%) were missed (Table 3). Of the patients without IAI, 87 (29%) had positive and 217 (71%) had negative exFAST. The sensitivity of the exFAST was 88% (95% CI = 75.7 to 95.5), specificity was 71% (95% CI = 65.9 to 76.4), PPV was 33.6% (95% CI = 10.7 to 18.2), and NPV was 97.3% (95% CI = 94.5 to 98.7). The LR+ was 3.07 and the LR− was 0.17. Of the 50 patients with IAI, 30 (60%) had a physical examination and FAST that were positive. Seven patients (14%) were only positive on FAST and an additional seven patients (14%) were only positive on physical examination.
Table 3.
Test Characteristics of Independent Predictors for Identification of IAI in Children
| exFAST | Physical Examination Alone | FAST Examination Alone | exFAST for IAI Requiring Acute Intervention | |
|---|---|---|---|---|
| Sensitivity | 88% (76%–96%) | 74% (60%–85%) | 74% (60%–85%) | 100% (75%–100%) |
| Specificity | 71% (66%–76%) | 84% (65%–75%) | 84% (65%–75%) | 70% (65%–75%) |
| PPV | 33% (29%–38%) | 43% (10%–13%) | 43% (10%–13%) | 11% (10%–13%) |
| NPV | 97% (95%–99%) | 95% (92%–97%) | 95% (92%–97%) | 100% |
| LR | 3.1 (2.5–3.8) | 4.6 (3.4–6.2) | 4.6 (3.4–6.2) | 3.4 (2.9–4.0) |
| LR− | 0.2 (0.1–0.4) | 0.3 (0.2–0.5) | 0.3 (0.2–0.5) | 0 |
exFAST = FAST-enhanced physical examination; FAST = focused assessment with sonography for trauma; IAI = intraabdominal injury; LR+ = positive likelihood ratio; LR− = negative likelihood ratio; NPV = negative predictive value; PPV = positive predictive value.
Six patients (12%) had IAI not identified by the exFAST, of whom none had a IAI requiring acute intervention, but all had some amount of intraperitoneal fluid on CT (Table 4). Four of these patients had erroneously negative bedside FAST, which were subsequently overread FAST as positive. These four children also had intraperitoneal fluid identified on CT scan. When recalculating the exFAST test characteristics using the overread FAST, the sensitivity of the test improved to 96% (95% CI = 86.3 to 99.5), the specificity was 78% (95% CI = 73.2 to 82.8), the PPV 42.1% (95% CI = 36.8 to 47.6), and the NPV was 99.2% (95% CI = 96.8 to 99.8). The interrater reliability for provider and overread FAST was fair (κ = 0.40, 95% CI = 0.29 to 0.51; Table 4).
Table 4.
List of Characteristics and Findings of the Children With IAI That Would Be Missed by the Compound Variable Physical Examination and Focused Assessment With Sonography for Trauma
| Age (years) | Sex | Mechanism | FAST overread* |
CT Free Fluid | Hospital Length of Stay (Days) |
ICU | Procedure | IAI - I | Injury |
|---|---|---|---|---|---|---|---|---|---|
| 3 | F | MVC | Positive | Yes | 6 | No | No | No | Grade 1 liver laceration |
| 5 | M | Fall | Positive | Yes | 3 | No | No | No | Grade 1 liver laceration |
| 8 | M | MVC | Positive | Yes | 4 | No | No | No | Grade 1 liver laceration |
| 2 | M | NAT | Positive | Yes | 12 | Yes† | Craniotomy | No | Subdural hematoma; grade 2 splenic laceration |
| 7 | F | MVC | Negative | Yes | 2 | No | No | No | Concussion; pancreatic tail contusion |
| 13 | M | Fall | Negative | Yes | 4 | No | No | No | Distal radius fracture, Grade 1 Liver laceration |
FAST = focused assessment with sonography for trauma; IAI-I = intraabdominal injury requiring acute intervention; ICU = intensive care unit; MVC = motor vehicle collision; NAT = nonaccidental trauma.
Cohen kappa coefficient: (κ = 0.40, 95% CI = 0.29 to 0.51).
ICU admission for traumatic brain injury.
One of the two patients with a negative exFAST and negative overread was a 7-year-old girl with a pancreatic tail contusion seen on CT scan. CT scan revealed scant intraperitoneal fluid though the overread FAST was also negative. She remained clinically stable and began eating without difficulty within 24 hours of arrival to the ED. The second patient was a 13-year-old boy with a grade 1 liver laceration who did not require acute intervention. He stayed in the hospital for 4 days for surgical repair of a displaced radius fracture. Neither his FAST nor his overread FAST showed intraperitoneal fluid; however, CT scan revealed scan intraperitoneal fluid.
Thirteen of the 50 children with IAI (26%) had IAI that required acute intervention. The exFAST did not miss any children with an IAI requiring acute intervention, resulting in a sensitivity of 100% (95% CI = 75.3 to 100), specificity of 65.4% (95% CI = 60.1 to 70.4), PPV of 9.92 (95% CI = 8.69-11.31), NPV of 100, and LR+ and LR− of 2.89 (2.5 to 3.34) and 0, respectively (Table 3).
DISCUSSION
We found that physical examination and FAST were both independent predictors of IAI in children with blunt torso trauma. However, in combination, the exFAST outperformed either diagnostic approach alone. A positive exFAST had a positive likelihood ratio of 3.1. The pretest probability of our study cohort for having an IAI was 14.1%. If the result of an exFAST were positive in this study cohort, it would increase the posttest probability for IAI from 14.1% to 43%. Similarly, the negative likelihood ratio of the exFAST was 0.2. If the results of exFAST were negative, the probability of IAI would decrease from 14.1% to 2.4%. Using the risk criteria describe by Menaker et al.,26 a negative exFAST may reduce a provider’s level of suspicion from a high to low likelihood of IAI.
Investigators have long sought CT-sparing risk stratification strategies for children with blunt torso trauma and have focused on patient history, physical examination criteria,27-29 and laboratory values.30-32 There are two large multicenter studies that derived clinical decision rules for risk stratifying children with possible IAI, the Pediatric Emergency Care Applied Research Network (PECARN, 2013)10 and the Pediatric Surgery Research Collaborative (PSRC, 2017).14 The PECARN study included 12,044 children from which it derived a prediction rule of seven variables to identify children at very low risk of IAI requiring acute intervention. The variables in descending order of importance were evidence of abdominal wall trauma, GCS less than 14, abdominal tenderness, evidence of thoracic wall trauma, complaints of abdominal pain, decreased breath sounds, and vomiting. The PECARN prediction rule has a NPV of 98.9% (95% CI = 98.5% to 99.1%) and a sensitivity of 92.5% (95% CI = 90.4% to 94.3%) for the identification of IAI. The PSRC study included 2,188 children and derived a prediction rule of five variables to identify children at very low risk of IAI, including complaints of abdominal pain, abdominal wall trauma/tenderness/ distention, abnormal chest radiography, elevated AST, and abnormal pancreatic enzymes. The PSRC rule has a NPV of 99.4% (95% CI = 99.2% to 99.6%), sensitivity of 98.4% (95% CI = 97.8 to 98.8), and LR− of 0.04 (0.03-0.06) for the identification of IAI. However, it is important to note that FAST was not included in these studies because of low utilization and lack of standardization across research sites. In fact, only a minority of children in both the PECARN and the PSRC studies received a FAST, 935 children (8.6%) in PECARN and 829 children (37.9%) in PSRC, because FAST expertise during this era was still emerging. However, with the growth of point-of-care ultrasound within the discipline of pediatric emergency medicine, FAST has become widespread in usage with consequent improved user quality of image acquisition and interpretation. For these reasons, these prediction algorithms may need to be reconsidered.
Historically, FAST had limited utility for children because of the mixed reported results. In a systematic review and meta-analysis that included 2,135 patients from eight studies, there was a pooled sensitivity of 35% (95% CI = 29% to 40%) and pooled specificity of 96% (95% CI = 95% to 97%).33 However, in a retrospective secondary analysis of PECARN study children who received FAST, patients with low to moderate clinical suspicion for IAI were less likely to receive a CT scan if they had a negatively interpreted FAST.26 This study laid the groundwork for a single-center randomized clinical trial of 925 children by Holmes et al.34 of FAST in children with blunt torso trauma. The authors found that a negative FAST successfully and safely reduced physician suspicion for IAI, but did not translate into lower rates of CT scans. There were multiple editorials in response to this single-center study, suggesting that the FAST should not be used alone, but instead combined with other variables in the context of a clinical decision rule.22-23,35
In contrast to injured adults, the use of FAST for injured children remains controversial and there is no standard method of application for its use. FAST has been successfully implemented into a consistent pathway for the management of injured adult patients in which a hemodynamically unstable adult patient with a positive FAST can forgo advanced diagnostic imaging and be directed for emergent surgical exploration. This adult pathway has improved patient and hospital-centered outcomes, including decreasing CT scan use.16 In contrast, there has not been a consistent pathway for the implementation of FAST in children with blunt torso trauma. For this reason, we have sought to evaluate the ability of FAST to rule out IAI in combination with other readily available predictor variables in children.
Our results suggest an opportunity to improve the accuracy of real-time provider FAST at the bedside. Four of the six patients who had an erroneously read study (Table 4) had a positive FAST overread on expert review and on CT scan, suggesting opportunity to improve the sensitivity of the test. These erroneous studies most likely represent errors made early in the FAST learning curve, because they all occurred within the first year that FAST was introduced to the study site. If we instead presume that these four erroneously read FAST were correctly identified, we would have improved the test characteristics of the exFAST from a sensitivity of 88% to 96% and the NPV from 97.3% to 99.2%. Similarly, we would have improved the specificity, from 71% to 78%, and PPV, from 34% to 42%, using the overread for exFAST. The agreement between provider and overread exFAST accounts for the fair interrater agreement (κ = 0.4, 95% CI = 0.29 to 0.51), which was similar to a single-center randomized controlled trial of pediatric FAST (κ = 0.45, 95% CI = 0.30 to 0.60).34 Therefore, through educational intervention, experience, and technologic advancement, we would expect the sensitivity of FAST to improve.
LIMITATIONS
There are intrinsic limitations for FAST in children. In this study, two children in whom FAST and overread FAST were negative, scant intraperitoneal fluid was noted on CT scan interpretation (Table 4). The first possible reason for the discrepancy in FAST and CT scan interpretation was the passage of time. FAST and CT scan are performed in succession. FAST may have been performed too early to detect intraperitoneal fluid. The second possible reason was that CT scan was more sensitive than FAST for detecting small volumes of intraperitoneal fluid.36 Therefore, like adult FAST,37 there may be a minimal fluid threshold below in which pediatric FAST cannot detect intraperitoneal fluid. Third, there are IAIs that may not cause intraabdominal hemorrhage and, therefore, cannot be detected on FAST.
Our study has several important limitations that predominantly stem from the retrospective design. First, our inclusion sampling of only children who received a FAST may have led to sampling bias. There were 725 children who did not receive a FAST, which could bias the results of the study. However, the cohort of patients included in our study appears to be representative of previous reports. The incidence of IAI in this cohort was 14%, which was similar to the 10% to 15% rate of IAI in other studies,9,38,39 but different than the rate reported by Holmes et al.,10 6.3%. Importantly, in this study, the choice to perform a FAST was left to the discretion of the treating provider, and we believe that children who did not receive a FAST may have had a lower suspicion for injury than those who did. Assuming that other factors remain constant, the NPV of a test improves with a lower prevalence. Therefore, we believe that this potential sampling bias could have led to an underestimate of the NPV. Second, the study’s retrospective design may have led to classification errors. We sought to minimize errors in classification by defining variables a priori40 and resolving discrepancies between two reviewers. In addition, the data set did not include a category of indeterminate for FAST. Third, although we report demographic, frequency, and accuracy data using all available patients, in computing the ORs for IAI we included only records that had complete data for physical examination and liver enzymes. This could lead to overestimation bias. Fourth, contemporary publications evaluating children with blunt torso trauma focus on identifying children with IAI requiring acute intervention. Our small sample size was not powered to evaluate children with IAI requiring acute intervention. However, the incidence of IAI requiring intervention was 26% of those with IAI, which was similar to previous studies.10,41 Furthermore, the exFAST did not have any false-negative studies when considering IAI requiring acute intervention. Although this study was underpowered to truly evaluate IAI requiring acute intervention, we believe that this is hypothesis generating and may lead to future evaluation of this approach as a CT-sparing technique for children with blunt torso trauma. Our study found that the physical examination and the FAST were each significantly and independently associated with the IAI outcome. However, it is important to note that these variables may be interdependent clinically because the person who performed the physical examination also performed the FAST. Knowledge of other elements of the examination, including the ultrasound transducer on the patient’s abdomen, may have influenced the performance and provider interpretation of FAST. However, our analysis indicates that addition of FAST to the physical examination significantly improved the accuracy in detection and exclusion of IAI.
The results of study are significant because the exFAST offers an advantageous CT-sparing strategy, the capability of the clinician to deploy and interpret the test without relying on a specialty service, the ability to obtain results within minutes of the patient’s arrival, and the ease of conducting serial examinations without the patient leaving the resuscitation bay. Similarly, FAST has become ubiquitous in pediatric EDs. Therefore, we believe that the exFAST has desirable test characteristics, including its NPV, which may help clinicians risk stratify patients and identify those who may not require CT scan. Furthermore, the exFAST may offer promising refinement to new or existing clinical decision rules.
CONCLUSION
We conclude that physical examination and focused assessment with sonography for trauma are both independent predictors associated with the identification of intraabdominal injury in children with blunt torso trauma. Furthermore, the combination of physical examination combined with focused assessment with sonography for trauma may have adequate negative predictive value to decrease the need for computed tomography scan in certain low- to moderate-risk populations of children with blunt torso trauma and may be used in conjunction with new or existing clinical decision rules. Further testing is warranted to determine extent of computed tomography sparing that can be achieved using the focused assessment with sonography for trauma–enhanced physical examination.
Supplementary Material
Data Supplement S1. Final International Classification of Disease, Ninth Revision (ICD-9) diagnosis of penetrating injury.
Footnotes
Presented at the Society for Academic Emergency Medicine Annual Meeting, Las Vegas, NV, May 17, 2019.
The authors have no relevant financial information or potential conflicts to disclose.
Supporting Information
The following supporting information is available in the online version of this paper available at http://onlinelibrary.wiley.com/doi/10.1111/acem.13959/full
REFERENCES
- 1.Heron M Deaths: leading causes for 2015. Natl Vital Stat Rep 2017;66:1–76. [PubMed] [Google Scholar]
- 2.Kenefake ME, Swarm M, Walthall J. Nuances in pediatric trauma. Emerg Med Clin North Am 2013;31:627–52. [DOI] [PubMed] [Google Scholar]
- 3.Miglioretti DL, Johnson E, Williams A, et al. The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr 2013;167:700–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Broder J, Fordham LA, Warshauer DM. Increasing utilization of computed tomography in the pediatric emergency department, 2000–2006. Emerg Radiol 2007;14:227–32. [DOI] [PubMed] [Google Scholar]
- 5.Smith-Bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996–2010. JAMA 2012;307:2400–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Korley FK, Pham JC, Kirsch TD. Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998–2007. JAMA 2010;304:1465–71. [DOI] [PubMed] [Google Scholar]
- 7.Hussein W, Mullins PM, Alghamdi K, Sarani B, Pines JM. Trends in advanced computed tomography use for injured patients in United States emergency departments: 2007–2010. Acad Emerg Med 2015;22:663–9. [DOI] [PubMed] [Google Scholar]
- 8.Shahi V, Brinjikji W, Cloft HJ, Thomas KB, Kallmes DF. Trends in CT utilization for pediatric fall patients in US emergency departments. Acad Radiol 2015;22:898–903. [DOI] [PubMed] [Google Scholar]
- 9.Letton RW, Worrell V; APSA Committee on Trauma Blunt Intestinal Injury Study Group. Delay in diagnosis and treatment of blunt intestinal injury does not adversely affect prognosis in the pediatric trauma patient. J Pediatr Surg 2010;45:161–5. [DOI] [PubMed] [Google Scholar]
- 10.Holmes JF, Lillis K, Monroe D, et al. Identifying children at very low risk of clinically important blunt abdominal injuries. Ann Emerg Med 2013;62:e2. [DOI] [PubMed] [Google Scholar]
- 11.Arbra CA, Vogel AM, Zhang J, et al. Acute procedural interventions after pediatric blunt abdominal trauma: a prospective multicenter evaluation. J Trauma Acute Care Surg 2017;83:597–602. [DOI] [PubMed] [Google Scholar]
- 12.Fenton SJ, Hansen KW, Meyers RL, et al. CT scan and the pediatric trauma patient–are we overdoing it? J Pediatr Surg 2004; 39:1877–81. [DOI] [PubMed] [Google Scholar]
- 13.Green SM. In reply. Ann Emerg Med 2014; 63:373. [DOI] [PubMed] [Google Scholar]
- 14.Streck CJ, Vogel AM, Zhang J, et al. Identifying children at very low risk for blunt intra-abdominal injury in whom CT of the abdomen can be avoided safely. J Am Coll Surg 2017; 224:e3. [DOI] [PubMed] [Google Scholar]
- 15.Richards JR, McGahan JP. Focused assessment with sonography in trauma (FAST) in 2017: what radiologists can learn. Radiology 2017;283:30–48. [DOI] [PubMed] [Google Scholar]
- 16.Melniker LA, Leibner E, McKenney MG, Lopez P, Briggs WM, Mancuso CA. Randomized controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency department: the first sonography outcomes assessment program trial. Ann Emerg Med 2006;48:227–35. [DOI] [PubMed] [Google Scholar]
- 17.Brody AS, Frush DP, Huda W, Brent RL; American Academy of Pediatrics Section on Radiology. Radiation risk to children from computed tomography. Pediatrics 2007;120:677–82. [DOI] [PubMed] [Google Scholar]
- 18.Fox JC, Boysen M, Gharahbaghian L, et al. Test characteristics of focused assessment of sonography for trauma for clinically significant abdominal free fluid in pediatric blunt abdominal trauma. Acad Emerg Med 2011;18:477–82. [DOI] [PubMed] [Google Scholar]
- 19.Thourani VH, Pettitt BJ, Schmidt JA, Cooper WA, Rozycki GS. Validation of surgeon-performed emergency abdominal ultrasonography in pediatric trauma patients. J Pediatr Surg 1998;33:322–8. [DOI] [PubMed] [Google Scholar]
- 20.Holmes JF, Gladman A, Chang CH. Performance of abdominal ultrasonography in pediatric blunt trauma patients: a meta-analysis. J Pediatr Surg 2007;42:1588–94. [DOI] [PubMed] [Google Scholar]
- 21.Scaife ER, Rollins MD, Barnhart DC, et al. The role of focused abdominal sonography for trauma (FAST) in pediatric trauma evaluation. J Pediatr Surg 2013;48:1377–83. [DOI] [PubMed] [Google Scholar]
- 22.Kessler DO. Abdominal ultrasound for pediatric blunt trauma: FAST is not always better. JAMA 2017;317: 2283–5. [DOI] [PubMed] [Google Scholar]
- 23.Marin JR, Fields JM, Tayal VS. The FAST examination for children with abdominal trauma. JAMA 2017;318:1394. [DOI] [PubMed] [Google Scholar]
- 24.American College of Emergency Physicians. Emergency ultrasound guidelines. Ann Emerg Med 2009;53:550–70. [DOI] [PubMed] [Google Scholar]
- 25.Moons KG, de Groot JA, Bouwmeester W, et al. Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Med 2014;11:e1001744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Menaker J, Blumberg S, Wisner DH, et al. Use of the focused assessment with sonography for trauma (FAST) examination and its impact on abdominal computed tomography use in hemodynamically stable children with blunt torso trauma. J Trauma Acute Care Surg 2014;77:427–32. [DOI] [PubMed] [Google Scholar]
- 27.Acker SN, Stewart CL, Roosevelt GE, Partrick DA, Moore EE, Bensard DD. When is it safe to forgo abdominal CT in blunt-injured children? Surgery 2015;158:408–12. [DOI] [PubMed] [Google Scholar]
- 28.Cotton BA, Beckert BW, Smith MK, Burd RS. The utility of clinical and laboratory data for predicting intraabdominal injury among children. J Trauma 2004;56:1068–74; discussion 1074–5. [DOI] [PubMed] [Google Scholar]
- 29.Taylor GA, O’Donnell R, Sivit CJ, Eichelberger MR. Abdominal injury score: a clinical score for the assignment of risk in children after blunt trauma. Radiology 1994;190:689–94. [DOI] [PubMed] [Google Scholar]
- 30.de Jong WJ, Stoepker L, Nellensteijn DR, Groen H, El Moumni M, Hulscher JB. External validation of the Blunt Abdominal Trauma in Children (BATiC) score: ruling out significant abdominal injury in children. J Trauma Acute Care Surg 2014;76:1282–7. [DOI] [PubMed] [Google Scholar]
- 31.Karam O, Sanchez O, Chardot C, La Scala G. Blunt abdominal trauma in children: a score to predict the absence of organ injury. J Pediatr 2009;154:912–7. [DOI] [PubMed] [Google Scholar]
- 32.Holmes JF, Sokolove PE, Brant WE, et al. Identification of children with intra-abdominal injuries after blunt trauma. Ann Emerg Med 2002;39:500–9. [DOI] [PubMed] [Google Scholar]
- 33.Liang T, Roseman E, Gao M, Sinert R. The utility of the focused assessment with sonography in trauma examination in pediatric blunt abdominal trauma: a systematic review and meta-analysis. Pediatr Emerg Care 2019. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 34.Holmes JF, Kelley KM, Wootton-Gorges SL, et al. Effect of abdominal ultrasound on clinical care, outcomes, and resource use among children with blunt torso trauma: a randomized clinical trial. JAMA 2017;317:2290–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moore C, Liu R. Not so FAST-let’s not abandon the pediatric focused assessment with sonography in trauma yet. J Thorac Dis 2018;10:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Emery KH, McAneney CM, Racadio JM, Johnson ND, Evora DK, Garcia VF. Absent peritoneal fluid on screening trauma ultrasonography in children: a prospective comparison with computed tomography. J Pediatr Surg 2001;36:565–9. [DOI] [PubMed] [Google Scholar]
- 37.Von Kuenssberg Jehle D, Stiller G, Wagner D. Sensitivity in detecting free intraperitoneal fluid with the pelvic views of the FAST exam. Am J Emerg Med 2003;21:476–8. [DOI] [PubMed] [Google Scholar]
- 38.Streck CJ, Vogel AM, Zhang J, et al. Identifying children at very low risk for blunt intra-abdominal injury in whom CT of the abdomen can be avoided safely. J Am Coll Surg 2017;224:e3. [DOI] [PubMed] [Google Scholar]
- 39.Gaines BA. Intra-abdominal solid organ injury in children: diagnosis and treatment. J Trauma 2009;67:S135–9. [DOI] [PubMed] [Google Scholar]
- 40.Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: reducing bias in emergency medicine chart review studies. Ann Emerg Med 2014;64:292–8. [DOI] [PubMed] [Google Scholar]
- 41.Streck CJ Jr, Jewett BM, Wahlquist AH, Gutierrez PS, Russell WS. Evaluation for intra-abdominal injury in children after blunt torso trauma: can we reduce unnecessary abdominal computed tomography by utilizing a clinical prediction model? J Trauma Acute Care Surg 2012;73:371–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. Final International Classification of Disease, Ninth Revision (ICD-9) diagnosis of penetrating injury.