Abstract
Object.
Enlargement of the subarachnoid spaces has been theorized as a risk factor for the development of subdural hemorrhage (SDH). As the finding of unexplained SDH in children often raises suspicion for nonaccidental trauma, the possibility of increased risk of SDH in children with enlargement of the subarachnoid spaces has important clinical, social, and legal implications. Therefore, the authors evaluated the frequency of SDH in a cohort of children with enlargement of the subarachnoid spaces.
Methods.
The authors identified children younger than 2 years of age who were diagnosed with enlargement of the subarachnoid spaces on MRI or CT scanning in a large primary care network between July 2001 and January 2008. The authors excluded children who had enlargement of the subarachnoid spaces diagnosed on imaging performed for trauma or developmental delay, as well as children with a history of prematurity, diagnosis of intracranial pathology, or metabolic or genetic disorders. Chart review recovered the following data: patient demographics, head circumference, history of head trauma, and head imaging results. For the subset of children with SDH, information regarding evaluation for other injuries, including skeletal survey, ophthalmological examination, and child protection team evaluation, was abstracted.
Results.
There were 177 children with enlargement of the subarachnoid spaces who met the inclusion criteria. Subdural hemorrhage was identified in 4 (2.3%) of the 177 children. All of the children with SDH underwent evaluations for suspected nonaccidental trauma, which included consultation by the child protection team, skeletal survey, and ophthalmological examination. Additional injuries (healing rib fractures) were identified in 1 of 4 patients. None of the 4 children had retinal hemorrhages. Only the child with rib fractures was reported to child protective services due to concerns for abuse.
Conclusions.
Only a small minority of the patients with enlargement of the subarachnoid spaces had SDH. Evidence of additional injuries concerning for physical abuse were identified in a quarter of the children with enlargement of the subarachnoid spaces and SDH, suggesting that an evaluation for suspected nonaccidental trauma including occult injury screening should be performed in cases of SDH with enlargement of the subarachnoid spaces. In the absence of additional injuries, however, the presence of an unexplained SDH in the setting of enlargement of the subarachnoid spaces may be insufficient to support a diagnosis of nonaccidental trauma.
Keywords: subdural hemorrhage, child abuse, vascular disorders, benign enlargement of the extraaxial space, benign external hydrocephalus, abusive head trauma
Enlargement of the extraaxial spaces in developmentally normal children younger than 2 years of age historically has been described as a benign self-limiting physiological process.1,3 This radiological finding has been described using a variety of names, including benign external hydrocephalus, idiopathic external hydrocephalus, benign extraaxial collections of infancy, and benign enlargement of extraaxial fluid; we will use the term enlargement of the subarachnoid spaces specifically to focus on the radiological findings and to acknowledge that SDH in association with enlargement of the subarachnoid spaces should not necessarily be considered “benign.” Macrocephaly, particularly benign familial macrocephaly, is frequently associated with enlargement of the extraaxial spaces.1 In fact, BESS is often diagnosed based on imaging performed to evaluate macrocephaly or a rapidly increasing head circumference.
The typical clinical pattern of BESS begins with a rapid increase in head circumference first noted at 2–3 months of age. The rate of head circumference growth often stabilizes by 10–18 months of life but usually results in head circumferences above the 95th percentile for age.3 Typical radiographic findings include widening of the frontal subarachnoid spaces, anterior interhemispheric fissure, and sylvian fissures without significant ventriculomegaly, all of which resolve by 2 years of age.3,11,16 Transient developmental delay, particularly gross motor delay, has been reported in children with BESS but has been found to resolve by 2 years of life, supporting a “benign” clinical course.1,6 Others have suggested possible longer-term effects from enlargement of the subarachnoid spaces.20 The etiology of enlargement of the subarachnoid spaces is still unknown. Hypothesized causes have included altered CSF dynamics due to delayed maturation of the arachnoid villi3 and a response to enlargement of the brain and gyral development.11
Several case reports and case series have suggested a possible association between enlargement of the subarachnoid spaces and the development of spontaneous SDH.2,13,18,19 The mechanism by which enlargement of the subarachnoid spaces may predispose young children to develop SDH is not clear. It has been hypothesized that the enlarged subarachnoid space may stretch the bridging veins draining into the sagittal sinus, increasing the risk for rupture of the bridging veins either spontaneously or following minor trauma.14 Others, however, have disputed this theory and have claimed that increased CSF collections would lead to a decreased risk of SDH because of a damping effect on the relative motion between the brain and skull during a rotational event.17 Despite the controversy regarding the possible mechanism, an association between enlargement of the subarachnoid spaces and increased risk of SDH has continued to be proposed in the literature.
The possibility of an increased risk of SDH in children with enlargement of the subarachnoid spaces has important medical, social, and legal implications. Subdural hemorrhage in children younger than 2 years can lead to developmental delay, seizure disorders, focal neurological deficits, or, on rare occasions, death.7,15 If enlargement of the subarachnoid spaces predisposes young children to the development of SDH with minimal or no trauma, clinicians need to consider a history of enlargement of the subarachnoid spaces when evaluating young head-injured children or those with symptoms suggestive of an intracranial hemorrhage. The presence of enlarged subarachnoid spaces might account for an otherwise unexplained SDH, lessening the concern for abusive trauma. However, the leading cause of SDH in children is head trauma, and the majority of traumatic SDHs in young children are a result of child abuse.12 Unrecognized abusive head trauma has dangerous and even fatal outcomes.8
Given the uncertainty regarding an association between enlargement of the subarachnoid spaces and development of SDH, we performed a retrospective study of a large cohort of pediatric patients younger than 2 years with enlargement of the subarachnoid spaces documented on head imaging. The primary objective of this study was to describe the cohort of children with enlargement of the subarachnoid spaces and to determine the percentage and characteristics of children who develop SDH.
Methods
Data Sources
The data source for this study was the electronic health record system for a large pediatric primary care network and the affiliated urban tertiary care children’s hospital. The network spans large areas of 3 mid-Atlantic states and includes practices in urban, suburban, and semirural communities.
The primary care network clinicians documented medical visits via the Epic electronic medical record system (Epic Systems Corporation), which was abstracted as part of this study. Additional information was abstracted using ChartMaxx (Care360), which stores the scanned paper versions of medical records and radiology reports from departments not yet transitioned to electronic record keeping, including inpatient hospital records. Radiological images were reviewed using the Department of Radiology’s picture archiving and communication system. This study was approved by the CHOP Institutional Review Board.
Study Population
As part of a prior study evaluating head circumference distribution in children, Daymont et al.5 identified a cohort of 75,412 patients in the primary care network with at least 2 visits and 1 head circumference measurement documented in the electronic medical record between August 2001 and January 2008. Children with a birth weight less than 1500 g and gestational age younger than 33 weeks were excluded. Additionally, children who at the time of discharge from the hospital after birth had a known diagnosis of hydrocephalus, intraventricular hemorrhage, SDH, tumor, spina bifida, neurofibromatosis, and other metabolic and genetic conditions known to be related to head size were excluded.
From this larger cohort we identified children younger than the age of 2 years who were diagnosed with enlarged extraaxial spaces on imaging performed to evaluate macrocephaly or enlarging head circumference. Only children younger than 2 years were included due to the physiological resolution of BESS by this age3 and the decreased risk of abusive head trauma in children older than 2 years.9 Since we were interested in the occurrence of SDH in children with enlarged extraaxial spaces without apparent acute trauma or underlying medical disorders, we excluded children who underwent head imaging due to acute trauma, seizures, genetic disorders, or structural abnormalities. Children whose primary indication for head imaging was developmental delay were also excluded, but children who underwent imaging because of macrocephaly and a minor developmental concern were included. Additionally, only children who underwent CT scanning or MRI were included because of concerns regarding the reliability of ultrasonography to accurately diagnose SDH.4
Measures
All variables were collected via chart review by a solitary physician reviewer (H.M.). The complete outpatient medical record for the visit at which the imaging was ordered was reviewed in addition to all injury-related outpatient visits, all emergency department visits, all social work notes, and all radiological reports for head imaging. The birth history, medical history, and problem list recorded in the electronic medical record was also reviewed for each patient when available. Demographic data including age at time of head imaging, family-reported race, and insurance status were obtained. Additional variables included the following: history of prior trauma, indication for imaging, imaging modality, and imaging results, and any medical or surgical treatment related to enlargement of the subarachnoid spaces. Assessment for a history of prior trauma included review of the inpatient and outpatient medical records for any trauma-related medical visits, documentation of a history of birth trauma (vacuum or forceps related), and review of nontrauma-related medical visits for documentation of household trauma not requiring medical attention.
The subset of children with intracranial bleeding on imaging underwent further chart review and abstraction, which included results from the following evaluations: child protection team consult, social work consult, skeletal survey, and pediatric ophthalmology consult. A diagnosis of nonaccidental trauma was determined based on the opinion documented in the child protection team consult. The child protection team is made up of 4 board-certified child abuse pediatricians, child abuse pediatrician fellows, and a social worker. If completed, documentation of any reports filed with child protective services was also reviewed.
In all cases in which the original head imaging report documented an SDH or any other abnormality that might be suggestive of an SDH (dural thickening, subdural effusion, or subdural collection), the imaging studies were reviewed separately by a board-certified pediatric neuroradiologist (A.N.P.) to confirm the presence of an SDH or other extraaxial abnormality, and to obtain additional details regarding the findings. The specific location of the hemorrhage, maximum width of both the subarachnoid spaces and the SDH measured from the gyrus at the point of maximum width, density characteristics of the hemorrhage, and any other abnormalities identified were recorded.
Statistical Analysis
Demographic information and clinical characteristics were summarized by frequencies and percentages for categorical variables (for example, sex and race) and by mean, standard deviation, and median for continuous variables (for example, age). The prevalence of SDH among children with enlargement of the subarachnoid spaces was calculated with 95% confidence intervals. The demographic characteristics of the included patients and the patients excluded because they only underwent head ultrasonography imaging were compared using the chi-square test for categorical variables or the Fisher exact test when any category had fewer than 10 participants, and the nonparametric Wilcoxon rank-sum test for age as a continuous variable. Statistical analyses were conducted using Stata 11.0 software (Stata Press).
Results
Study Population
Two hundred sixty-seven children younger than 2 years with enlargement of the subarachnoid spaces diagnosed on imaging were identified. Of these, 57 children were excluded because they underwent imaging for an indication other than macrocephaly or increasing head circumference (Fig. 1). An additional 33 children with enlargement of the subarachnoid spaces diagnosed via ultrasonography alone were excluded, resulting in a final cohort of 177 children. Three of the children excluded on the basis of imaging indication had SDH: 1 underwent imaging because of acute trauma and 2 infants with a history of vacuum-assisted birth underwent imaging because of concern for structural facial/skull abnormalities.
Fig. 1.
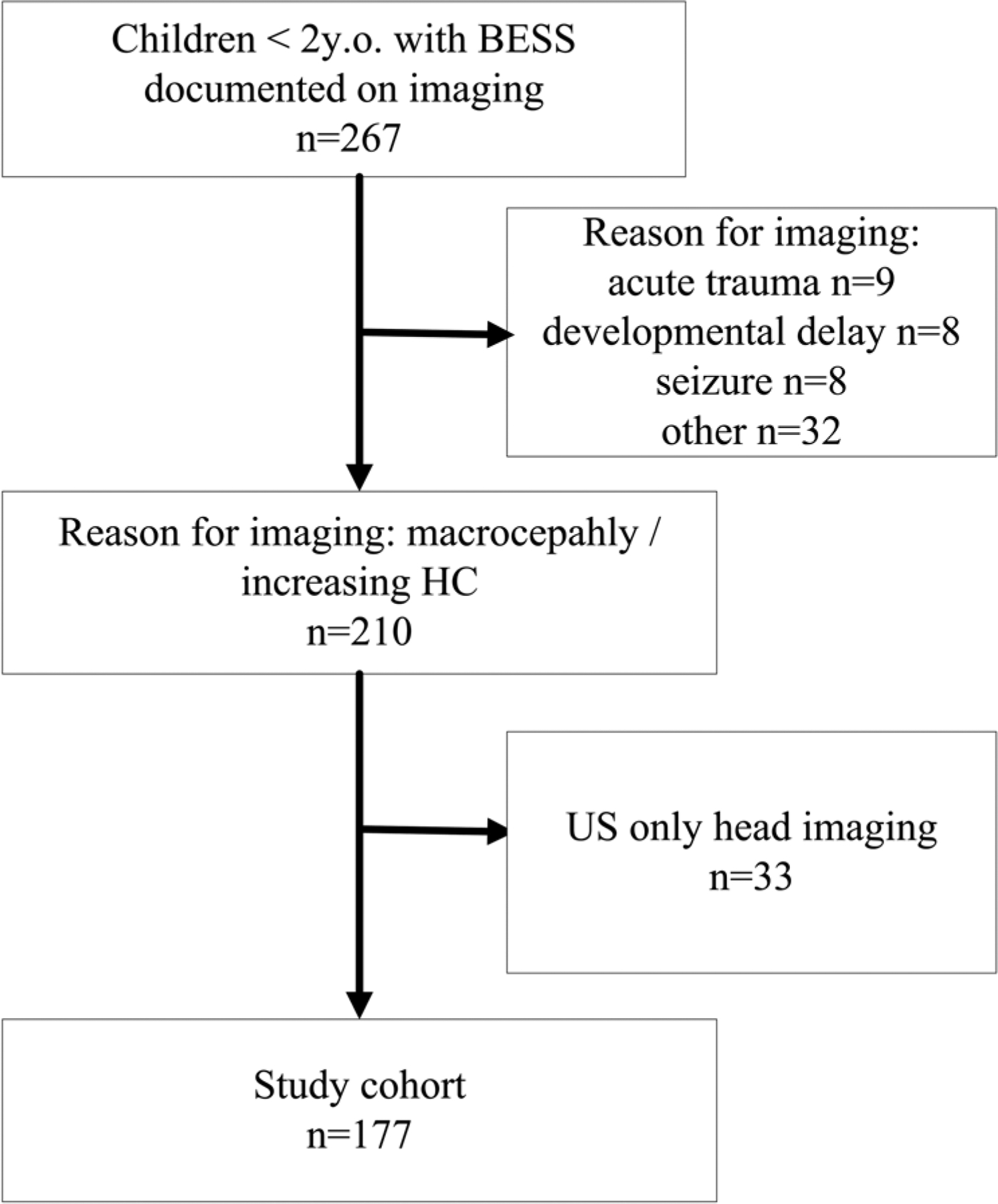
Assembly of study cohort. HC = head circumference; US = ultrasonography; y.o. = years old.
The 33 children who were excluded due to imaging with ultrasonography only were younger at time of imaging with a mean age of 143 ± 65 days (range 20–371 days, p < 0.001) and were more likely to be female (48% male, p = 0.05) than the included children who underwent MRI or CT scanning (Table 1). Minor race and insurance status differences were not statistically significant. None of the children excluded on the basis of ultrasound imaging alone had a documented SDH.
TABLE 1:
Characteristics of the study cohort
| Characteristic | Imaging via MRI or CT* |
|---|---|
| age in days | |
| mean ± SD | 288 ± 109 |
| median | 282 |
| range | 41–622 |
| sex | |
| male | 118 (67) |
| female | 59 (33) |
| race | |
| African American | 70 (40) |
| Asian | 5 (3) |
| Caucasian | 88 (50) |
| other | 14 (8) |
| insurance | |
| private | 74 (42) |
| public | 94 (53) |
| self-pay | 9 (5) |
Values are the number of patients (%) unless indicated otherwise.
The cohort was racially diverse, with 88 Caucasian patients (50%), 70 African American patients (40%), 5 Asian patients (3%), and 14 patients who were described as other by their families (8%), similar to the demographic composition of the primary care network described by Daymont et al.5 There were 118 male (67%) and 59 female (33%) patients. Ages at the time of imaging ranged from 41 to 622 days (mean age 288 days, median age 282 days). Forty-two percent (74 patients) of our cohort had private insurance, and 58% (103 patients) had either public or no insurance. One hundred sixty-four children (93%) qualified as having macrocephaly or a head circumference greater than the 95th percentile for age based on the standard Centers for Disease Control and Prevention curves in use at the time the children were evaluated; the remaining 7% had head circumferences in the normal range.
Subdural Hemorrhages: Incidence and Evaluations for Medical and Traumatic Etiologies
Four (2.26% [95% CI 0.05%–4.47%]) of the 177 children with enlarged subarachnoid spaces had evidence of SDH on head CT or MRI. Inclusion of the children who only underwent ultrasonography would result in a decrease of the percentage of children with enlargement of the subarachnoid spaces and SDH to 1.9% (95% CI 0.04%–3.8%). Patient demographics, description of the hemorrhage, and width of the subarachnoid spaces of the 4 patients with SDH are provided in Table 2. In 3 of the 4 patients, enlargement of the subarachnoid spaces and SDH was diagnosed concurrently on images obtained at a single point in time. In a single case (Case 4), enlarged subarachnoid spaces were initially diagnosed on head CT scanning performed at 14 months of life, and a repeat head CT scan obtained at 18 months demonstrated both enlargement of the subarachnoid spaces and SDH. Description of clinical presentations and complications are outlined in Table 2.
TABLE 2:
Demographics and measurements of SDH in children with enlargement of the extraaxial spaces*
| Case No. | Age at Imaging (mos), Sex | Presenting Symptoms | Imaging Modality | Location of SDH | Nature of SDH | Width of SDH in mm† | Width of SAS in mm† | Results of Evaluation for Suspected Abuse | Neurosurgical Intervention |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 8, F | macrocephaly | CT | bilat | hyperdense | 12.3 (rt), 7.6 (lt) | 13.3 (rt), 10.6 (lt) | negative | drainage of SDH via bur hole |
| 2 | 5, M | macrocephaly | CT | bilat, frontal | mildly hyperdense | 13.5 (rt), 14.1 (lt) | 11.9 (rt), 7.1 (lt) | negative | lost to neurosurgical follow-up |
| 3 | 6, M | increasing HC | MRI | lt | slightly hyperdense | 5.1 (lt) | 14.5 (rt), 14.1 (lt) | negative | none |
| 4 | 14, M | emesis, lethargy | CT | none | NA | NA | 9.2 (rt), 8.4 (lt) | NA | none |
| 18, M | increasing HC | CT | bilat, rt holohemi-spheric | hyperdense | 26.7 (rt), 16.2(lt) | 11.1 (rt), 12.8 (lt) | multiple healing posterior & lat rib fractures; upper-extremity fracture | none |
HC = head circumference; NA = not applicable; SAS = subarachnoid space.
Measured from the gyral surface at the point of maximum SDH width.
The 4 children with SDH were evaluated by the inpatient child protection team. The child protection consults included physical examination, skeletal survey, pediatric ophthalmological examination, and social work evaluation for each child. These 4 children also had normal findings on baseline coagulation studies (prothrombin time and partial thromboplastin time). Based on clinical presentation, additional laboratory workup varied and included 1 or more of the following: urine organic acids, serum acylcarnitine profile, fibrinogen, factor VIII, factor XIII, von Willebrand activity, and antigen levels. All coagulation and metabolic findings evaluated in these patients were normal. Due to the absence of additional findings suggestive of nonaccidental trauma, the child protection team determined that there was insufficient evidence to support a diagnosis of abuse in Cases 1–3.
In addition to the SDH documented on head CT scanning, 2 healing posterior rib fractures and a distal radius fracture were identified on skeletal survey in Case 4. Bone health laboratory results were completed, including parathyroid hormone (39.9 pg/ml), 25-OH vitamin D (34.5 ng/ml), calcium (10.7 mg/dl), and phosphorous (6.2 mg/dl), and all values were within normal limits. Alkaline phosphatase (2513 U/L) was elevated and, after consultation with the endocrine department, this was thought to be a transient elevation and benign in nature. Further re-review of abdominal radiographs obtained for vomiting and altered mental status 4.5 months prior to the presentation with SDH identified multiple healing rib fractures. Rib fracture locations on the initial abdominal radiographs were as follows: 2 posterior (ongoing healing noted on later films during presentation with SDH), 1 anterolateral, and 2 anterior. Based on the presence of fractures in multiple locations in various stages of healing without a history of accidental trauma to explain the injuries, a report was made to child protective services for injuries concerning for inflicted trauma.
History of Remote Trauma and Relation to SDH
Eight of the 177 patients had documented historical trauma 1 week to 3 months prior to head imaging. These traumas included the following: facial/nasal trauma, chronic head banging, a 9- to 10-ft fall, a shelf falling onto a child, fall from a wagon to the garage floor, fall forward while sitting on a toy, large birth-related cephalohematomas following instrument-assisted vaginal birth, and fall from the arms of a 7-year-old sibling (Case 4). Only 1 (12.5%) of 8 children with a remote history of trauma had evidence of SDH; this child (Case 4) also had additional skeletal injury leading to a diagnosis of physical child abuse.
Neurosurgical Interventions
Two of the children with enlargement of the subarachnoid spaces underwent neurosurgical procedures; one underwent surgical drainage of SDH via bur hole at 8 months of life (Case 1) and the other without SDH underwent placement of a subdural shunt at 10 months of age for enlarged ventricles.
Discussion
We have described a large cohort of pediatric patients younger than 2 years with documented enlargement of the extraaxial spaces on head imaging. Subdural hemorrhages were uncommon in our study cohort, occurring in only 2.3% of the patients. In the majority of the patients with SDH, a thorough evaluation did not reveal any additional signs of trauma, and the SDH was thought to have occurred spontaneously or due to routine household trauma in the setting of enlarged subarachnoid spaces. However, 1 in 4, or 25%, of our patients with SDH and enlargement of the subarachnoid spaces was believed to be a victim of abuse. Thus, screening for occult injuries, including skeletal survey and ophthalmological evaluation, is needed in children with an SDH regardless of the presence of enlarged extraaxial spaces. It must be noted that the child in Case 4 had a reported history of previous head trauma (fall from the arms of a 7-year-old sibling, no head imaging performed) in the setting of documented enlarged extraaxial spaces 3 months prior to presentation for increasing head circumference. The diagnosis of nonaccidental trauma in this child was based on the identification of multiple fractures and lack of accidental trauma or metabolic condition to explain the etiology of these fractures. The finding of an SDH in constellation with the unexplained fractures serves to increase the concern for inflicted trauma and cause speculation as to whether the SDH in this child was also a result of an abusive etiology. Although limited in number, there were 7 additional patients with enlargement of the subarachnoid spaces and documented closed head injury in the months prior to their head imaging for macrocephaly who did not have an SDH.
Our study is not without limitations. The radiological diagnosis of enlargement of the subarachnoid spaces is subjective, and there may be variability among neuroradiologists in diagnosis. We chose to acknowledge this variability and did not have a separate neuroradiological reviewer confirm each diagnosis of enlargement of the subarachnoid spaces. The department within CHOP that was responsible for reading all images in this study is a tertiary pediatric neuroradiology department with extensive experience. For the reasons mentioned above regarding the subjective nature of the radiographic diagnosis of enlargement of the subarachnoid spaces combined with the variability within the radiologists in the department of neuroradiology at CHOP, under- or overdiagnosis could be possible in this study. Our findings may also be limited by the retrospective nature of the study. As a retrospective chart review study, the study was prone to misclassification bias because of inaccuracies in the medical record.
Our study findings add to the growing body of literature documenting cases of SDH in children with enlarged subarachnoid spaces, although these findings do not prove causation. In 3 of the 4 cases, enlargement of the subarachnoid spaces and SDH were diagnosed concurrently. This leads to the question of which occurred first in these children, the SDH or the enlargement of the subarachnoid spaces? Stretching of the bridging veins in children with enlargement of subarachnoid spaces has been postulated to increase the risk of SDH. Changes in the physiology of CSF absorption following traumatic SDH, however, has also been postulated to lead to bifrontal enlargement of the subarachnoid spaces. Cases of children without any prior history of enlarged spaces who develop abnormal CSF flow dynamics following intracranial hemorrhage have been documented in the literature.10 Thus, while it is possible that enlargement of the subarachnoid spaces may have predisposed the children to develop SDH, it is also possible that in 3 of the 4 cases the SDH predisposed the children to develop enlarged extraaxial spaces or that the enlarged spaces and SDH were unrelated.
Conclusions
This study highlights both the possibility of SDH developing in the absence of a history of significant trauma in children with enlargement of the subarachnoid spaces but also the rarity of this complication. The identification of abusive fractures in 1 of 4 children with enlarged subarachnoid spaces and SDH necessitates that an evaluation for possible nonaccidental trauma be performed in children with SDH and enlargement of the extraaxial spaces. Clinicians should not assume that children with benign enlargement of the subarachnoid spaces cannot also be victims of abusive head trauma. In the absence of other findings suggestive of abusive injury, however, a diagnosis of abuse and referral to child protective services may not be warranted.
Disclosure
Dr. Christian provides legal consultation in child abuse cases. Dr. Wood has received salary funding from the National Institute of Child Health and Human Development (Grant No. 1K23HD071967-01).
Abbreviations used in this paper:
- BESS
benign enlargement of the subarachnoid spaces
- CHOP
Children’s Hospital of Philadelphia
- SDH
subdural hemorrhage
Footnotes
Portions of this work were presented in poster form at the Pediatric Academic Societies Annual Meeting, Boston, Massachusetts, April 29, 2012.
References
- 1.Alvarez LA, Maytal J, Shinnar S: Idiopathic external hydrocephalus: natural history and relationship to benign familial macrocephaly. Pediatrics 77:901–907, 1986 [PubMed] [Google Scholar]
- 2.Amodio J, Spektor V, Pramanik B, Rivera R, Pinkney L, Fefferman N: Spontaneous development of bilateral subdural hematomas in an infant with benign infantile hydrocephalus: color Doppler assessment of vessels traversing extra-axial spaces. Pediatr Radiol 35:1113–1117, 2005 [DOI] [PubMed] [Google Scholar]
- 3.Barkovich A: Pediatric Neuroimaging, ed 4. Philadelphia: Lippincott Williams & Wilkins, 2005, pp 686–689 [Google Scholar]
- 4.Datta S, Stoodley N, Jayawant S, Renowden S, Kemp A: Neuroradiological aspects of subdural haemorrhages. Arch Dis Child 90:947–951, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daymont C, Hwang WT, Feudtner C, Rubin D: Head-circumference distribution in a large primary care network differs from CDC and WHO curves. Pediatrics 126:e836–e842, 2010 [DOI] [PubMed] [Google Scholar]
- 6.Hellbusch LC: Benign extracerebral fluid collections in infancy: clinical presentation and long-term follow-up. J Neurosurg 107 (2 Suppl):119–125, 2007 [DOI] [PubMed] [Google Scholar]
- 7.Jayawant S, Parr J: Outcome following subdural haemorrhages in infancy. Arch Dis Child 92:343–347, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jenny C, Hymel KP, Ritzen A, Reinert SE, Hay TC: Analysis of missed cases of abusive head trauma. JAMA 281:621–626, 1999 [DOI] [PubMed] [Google Scholar]
- 9.Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF, Sinal SH: A population-based study of inflicted traumatic brain injury in young children. JAMA 290:621–626, 2003 [DOI] [PubMed] [Google Scholar]
- 10.Kleinman PK: Diagnostic Imaging of Child Abuse, ed 2. St. Louis: Mosby, 1998, p 312 [Google Scholar]
- 11.Kleinman PK, Zito JL, Davidson RI, Raptopoulos V: The subarachnoid spaces in children: normal variations in size. Radiology 147:455–457, 1983 [DOI] [PubMed] [Google Scholar]
- 12.Matschke J, Voss J, Obi N, Görndt J, Sperhake JP, Püschel K, et al. : Nonaccidental head injury is the most common cause of subdural bleeding in infants <1 year of age. Pediatrics 124: 1587–1594, 2009 [DOI] [PubMed] [Google Scholar]
- 13.McNeely PD, Atkinson JD, Saigal G, O’Gorman AM, Farmer JP: Subdural hematomas in infants with benign enlargement of the subarachnoid spaces are not pathognomonic for child abuse. AJNR Am J Neuroradiol 27:1725–1728, 2006 [PMC free article] [PubMed] [Google Scholar]
- 14.Papasian NC, Frim DM: A theoretical model of benign external hydrocephalus that predicts a predisposition towards extra-axial hemorrhage after minor head trauma. Pediatr Neurosurg 33:188–193, 2000 [DOI] [PubMed] [Google Scholar]
- 15.Parent AD: Pediatric chronic subdural hematoma: a retrospective comparative analysis. Pediatr Neurosurg 18:266–271, 1992 [DOI] [PubMed] [Google Scholar]
- 16.Prassopoulos P, Cavouras D, Golfinopoulos S, Nezi M: The size of the intra- and extraventricular cerebrospinal fluid compartments in children with idiopathic benign widening of the frontal subarachnoid space. Neuroradiology 37:418–421, 1995 [DOI] [PubMed] [Google Scholar]
- 17.Raul JS, Roth S, Ludes B, Willinger R: Influence of the benign enlargement of the subarachnoid space on the bridging veins strain during a shaking event: a finite element study. Int J Legal Med 122:337–340, 2008 [DOI] [PubMed] [Google Scholar]
- 18.Ravid S, Maytal J: External hydrocephalus: a probable cause for subdural hematoma in infancy. Pediatr Neurol 28:139–141, 2003 [DOI] [PubMed] [Google Scholar]
- 19.Vinchon M, Delestret I, DeFoort-Dhellemmes S, Desurmont M, Noulé N: Subdural hematoma in infants: can it occur spontaneously? Data from a prospective series and critical review of the literature. Childs Nerv Syst 26:1195–1205, 2010 [DOI] [PubMed] [Google Scholar]
- 20.Zahl SM, Egge A, Helseth E, Wester K: Benign external hydrocephalus: a review, with emphasis on management. Neurosurg Rev 34:417–432, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]


