Abstract
The combined effects of fossil fuel combustion, mass agricultural production and deforestation, industrialisation and the evolution of modern transport systems have resulted in high levels of carbon emissions and accumulation of greenhouse gases, causing profound climate change and ozone layer depletion. The consequential depletion of Earth’s natural ecosystems and biodiversity is not only a devastating loss but a threat to human health. Sustainability—the ability to continue activities indefinitely—underpins the principal solutions to these problems. Globally, the healthcare sector is a major contributor to carbon emissions, with waste production and transport systems being amongst the highest contributing factors. The aim of this review is to explore modalities by which the healthcare sector, particularly ophthalmology, can reduce carbon emissions, related costs and overall environmental impact, whilst maintaining a high standard of patient care.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40123-021-00404-8.
Keywords: Artificial intelligence, Cataracts, Peripheral hubs, Sustainability, Teleophthalmology
Key Summary Points
| The adverse health effects of climate change include spread of infectious diseases, cardiovascular and respiratory diseases secondary to wildfires, malnourishment due to droughts and flooding, and obesity, diabetes and heart disease owing to increasing motorisation and progressive agricultural activities. |
| The healthcare sector is a significant contributor to carbon emissions globally. |
| This review aims to explore methods by which the healthcare sector, particularly ophthalmology, can positively reduce waste production and carbon emissions. |
| Refinement of referral pathways, upskilling community optometrists, establishment of peripheral imaging and treatment ‘hubs’, utilisation of home devices alongside AI algorithms, and risk stratification of patients in ophthalmology outpatient settings can reduce unnecessary cost, waste production, and travel-associated carbon emissions. |
| Promoting sustainability in healthcare through acknowledgement, education (undergraduate and postgraduate medical, nursing, and optical bodies), policy development, and setting targets for carbon emissions are the next steps in the movement towards sustainable healthcare. |
Introduction
“The life of every child born today will be profoundly affected by climate change. Without accelerated intervention, this new era will come to define the health of people at every stage of their lives.”—The 2019 report of the Lancet Countdown [1].
Combustion of fossil fuels and biomass, world food production (via animal cultivation, irrigated agriculture) and mass deforestation have resulted in rapid increases in world energy production and the accumulation of heat-trapping “greenhouse gases” in the troposphere. Man-made gases from the use of halocarbons for refrigeration and insulated packaging accumulate in the stratosphere and destroy ozone, reducing shielding against harmful ultraviolet radiation. Industrialisation and the emergence of a world economy, with modern transport systems and electronic communication network, vast expansion of energy-intensive agriculture and livestock production, urban migration and increase in consumerism are all contributing to the global environmental changes. Climatologists believe that the unusual weather patterns are signalling the beginning of a long-term change in the average temperature, precipitation and patterns of weather extremities. According to the Intergovernmental Panel on Climate Change (IPCC) report, global warming is predicted to reach 1.5 °C above pre-industrial levels between the years 2030 and 2052 if it continues at the current rate [2]. Such climate change and ozone depletion impact the Earth’s natural ecosystem and biodiversity, depleting freshwater supply and the marine ecosystem that are essential to human health [3, 4].
Climate change and ozone depletion can lead to adverse health consequences. In the past 20 years, heat-related mortality in those above 65 years old has increased significantly (53.7%), reaching a total of 296,000 deaths in 2018. The negative consequences of climate change can be observed in every continent—from the ongoing spread of dengue virus across South America, the wildfires in Australia compromising cardiovascular and respiratory health, and the floods or droughts in China, Bangladesh, Ethiopia and South Africa leading to the undersupply of food and malnourishment [5]. Modern lifestyle choices, with increasing motorisation replacing active transport modalities like walking and cycling, and the increase of red meat and dairy consumption (progressive agricultural activities) have led to an increased prevalence of diabetes and obesity and their subsequent chronic health issues. This has resulted in an increased reliance on healthcare and associated costs [6]. Yu and colleagues also elaborated the potential impact on eye health including increasing incidence of trachoma infections, vitamin A deficiency eye conditions, cataracts, allergic eye diseases, glaucoma and age-related macular degeneration (AMD) as direct or indirect consequences from extreme weather conditions [7]. Poor air quality has been shown to put additional pressure on emergency services; a study by Kings College London using data from nine English cities demonstrated that on high pollution days there is an increase in ambulance calls with 673 extra out-of-hospital cardiac arrests and admissions for stroke and asthma [8].
The Lancet Commission on Health and Climate sets forth the requirement of the health sector to tackle climate change, by identifying and mitigating the risks it poses to bring about a paradigm shift in the future delivery of healthcare [9]. Climate change not only poses the biggest health ‘threat’ but also creates an ‘opportunity’ for positive change in global health [10–12].
This review aims to explore ways in which the healthcare sector, in particular ophthalmology, can reduce carbon emissions along with related costs, environmental impacts and associated mortality and morbidity, whilst maintaining the best standard of care. We will explore ‘sustainability’ in ophthalmology, the ability to meet the needs of the current generation without compromising the needs of future generations [13, 14].
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Carbon Emission in Healthcare
In 2017, the healthcare sector was responsible for 4–6% of carbon emission globally [8]. The USA spends by far the most on its healthcare system (with nearly one-fifth of GDP in 2013). After food service facilities, hospitals are the second most energy intensive commercial buildings in the USA [15]. The NHS (England’s National Health Service) employs over 1.5 million people to provide high-quality healthcare to a population of approximately 56 million people. This delivery of care contributes to 4–5% of the country’s total greenhouse gas and this value may well increase further if unchecked, with an ageing population and increasing healthcare expenditure [16]. Whilst emitting carbon, the NHS is also treating acute presentations and conditions attributed to such emissions [6]. Hence, in 2008, the Sustainable Development Unit (SDU) was created following the publication of the Climate Change Act (2008) to gain a better understanding of the association between climate change, health and healthcare. The NHS has since achieved a significant reduction in greenhouse gas emission and their associated costs whilst delivering and maintaining high standards of care.
In January 2020, the NHS England Chief Executive launched the Greener NHS campaign, aiming to make the NHS the world’s first net zero health service by 2040, with an 80% reduction by the years 2028–2032. It was noted that the NHS is “part of the problem as well as the solution.” In addition, The NHS Net Zero Expert Panel has been established to look at changes the NHS can make across the organisation both in its supply chain and wider partnerships. NHS emissions come from a number of sources, but transport contributes significantly. It is estimated that 6.7 billion road miles each year are from patients and their visitors travelling to access the healthcare sites [17, 18].
The Ophthalmology Carbon Footprint
Cataract Surgery
Ophthalmology has the highest surgical volumes and rapid turnover rates in the NHS with approximately 414,000 cataract procedures in England and 20,000 in Wales between the years 2017 and 2018 [19]. This makes cataract procedures an obvious target for reduction of carbon emissions. Morris and colleagues estimated the carbon burden accounting for 343,782 cataract procedures in England in 2011 to be at least 63,000 tonnes of CO2 equivalent (CO2eq) taking into consideration building and energy use, travel and procurement [20]. Somner et al. compared different techniques of cataract explantation [phacoemulsification vs. modified small incision cataract surgery (MSCIS)] and the environmental impact. They concluded that phacoemulsification is not only much more costly but has a significantly greater environmental impact compared to MSCIS. This is the result of disposable waste (paper and plastic) and the energy used by the phacoemulsification machine [21, 22]. In terms of cost-effectiveness, various studies carried out in India and Nepal have shown that the technique of MSICS is 1.4–4.7 times less expensive than phacoemulsification with similar visual outcomes and complication rates. It is therefore the predominant technique in developing countries and areas with limited resource but high volume and backlog [22–26]. Of course, in many developed nations there are different socioeconomic conditions and healthcare infrastructures and expectations, and larger ‘real-world’ prospective analyses would be required to assess the long-term visual outcomes of different cataract surgery techniques, their carbon footprints and cost–benefit analyses.
In developed countries, single-use disposable instruments and equipment have contributed to a mass production of clinical and non-clinical waste, and significantly to carbon emissions. Morris et al. estimated that 53.8% of these emissions were from procurement, the majority due to disposable medical equipment [19]. Goel and colleagues published data on productivity, costs, carbon emissions and waste generation for every cataract surgery performed across nine participating sites internationally, using the “Eyefficiency” cataract surgery auditing tool. Service costs range from £31.55 to £399.34, solid waste weighs between 0.19 and 4.27 kg and carbon emissions range from 41 kg CO2eq to 130 kg CO2eq for each cataract case performed. Comparing the expenditure of medical supply and waste generation between two developed countries exposes an interesting difference. New Zealand has the highest expenditure on consumables with low waste generation indicating that the supply spending could be disproportionately high. The UK spends moderately on their disposable supplies but generates twice as much waste compared to that of the next highest site, indicating that packaging and waste management could be an issue [27].
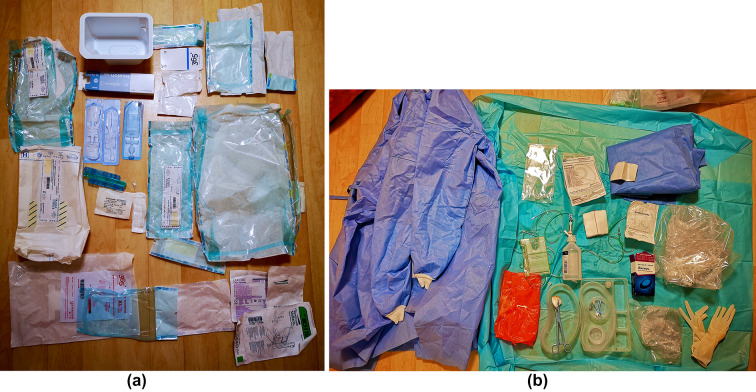
Figure 1a shows an example of non-clinical waste generated in a cataract centre in the UK in preparation for a cataract case and Fig. 1b shows an example of clinical waste generated upon completion of a cataract case. During a non-complex phacoemulsification case, a total of 2.10 kg of waste was generated. It is important to recognise the amount of waste produced from each case depends on various factors such as the complexity of case (meaning more or less surgical equipment), the use of disposable equipment and packaging, the number of saline bottles used and the remaining volume of balanced salt solution, the number of surgeons operating affecting disposable gowns and gloves used.
Fig. 1.
a Non-clinical waste generated in preparation for a phacoemulsification case. b Clinical waste generated following a phacoemulsification case
By comparing UK cataract services with the Aravind Eye Care System (AECS) in India, notable differences in carbon generated are observed. At the AECS approximately 6 kg CO2eq is generated per phacoemulsification procedure compared to approximately 130 kg CO2eq in the UK, for every case performed [20]. This significant difference is due to the Aravind’s high volume approach providing up to 1500 cataract surgeries per day, thereby minimising the environmental footprint associated with electricity and energy use. They also reuse surgical gowns, blankets and certain surgical and pharmaceutical supplies (including multiuse solutions during cataract surgery and preoperative eyedrops). Contaminated instruments (instrument trays and phacoemulsification tip) would be sterilised in between each case, whereas non-contaminated instruments (fluid collection bags, plastic protectors on phacoemulsification machines and tables, intraoperative pharmaceuticals) would be sterilised at the end of the operating day to reduce environmental impact associated with repeated sterilisation. Despite reusing surgical supplies, cleaning gloves with alcohol and chlorhexidine, and simultaneously operating on multiple patients within a single operating theatre, the rate of postoperative endophthalmitis is no higher than European norms [28, 29]. However, because of stricter infection control guidelines, implementation of the Aravind model of practice is not currently feasible in countries such as the UK.
Reduce, Reuse, Recycle, Rethink and Research
The 5 R’s of sustainability (Reduce, Reuse, Recycle, Rethink and Research) can be applied to reducing the environmental impact of ophthalmic surgery in a cumulative manner, whilst maintaining patient safety.
We can reduce energy consumption by simply turning off lights in operating theatres and switching off equipment when not in use. The use of light emitting diode (LED) lights, timer and motion detectors will also result in significant reduction in energy expenditure [30–32]. According to Kagoma and colleagues, operating theatres are almost always unoccupied up to 40% of the time over a 24-h period [33]. The Providence St. Peter Hospital, Washington reduced energy consumption by reducing its ventilation system output by 60% during unoccupied times [34].
Sensible ways to reduce the amount of waste generated should also be considered. Referring again to Fig. 1a and b, a major contributor to waste is plastic packaging, with the majority of the equipment being placed in plastic containers and double wrapped. The use of polypropylene plastic blue sterile wrap is not only damaging to the environment but will also concur a substantial disposal cost. There is an opportunity to work with industries to reduce the amount of waste derived from a single operation [33]. Understandably, ophthalmic surgeons have specific equipment they prefer for a certain surgical procedure, hence the existence of single packaging disposable surgical equipment, individually packed gloves and gowns according to size. Perhaps the creation of a surgeon-tailored pack with preferred equipment, gloves of their size and disposable gowns could reduce the amount of double packaging of each product.
Bartl [35] suggested that the reuse of materials is equally as effective at reducing waste as it avoids the side streaming of waste generated through recycling and occurs before the end-stage of material is reached. Kwakye and colleagues reported that switching from disposable to reusable surgical gowns in a single hospital led to a waste reduction of 23,000 kg of carbon, saving the hospital 60,000 USD over a 12-month period [36]. In a review article published by Guetter in 2018, decisions whether to use disposable or reusable materials such as drapes and surgical gowns are based on available scientific data and cost based on region, country, culture and customs. Data relating to infection rates is still controversial and more comparative studies are needed to look at savings and expenditures relating to reusable items [30]. Indeed, one can argue that the environmental impact of laundering of reusable textiles could potentially be more significant, especially when paired with harmful laundry chemicals and inefficient ageing hospital infrastructure (water and energy). The benefits of reuse of surgical equipment are also disputable because of the hidden costs associated with storage, damage of equipment in the process of sterilisation and instrument handling, and the risk of cross-contamination e.g. Creutzfeldt–Jakob disease (CJD), especially in vitreoretinal surgery when neural tissues are involved [37].
According to Southorn et al. [38] each operating room has the potential to produce up to 2300 kg waste every year, with almost 80% of the total waste generated preoperatively. This is variable depending on the surgical specialty, type of procedure, duration of surgery and surgeon preference of instruments and equipment. The amount of waste generated also differs from one country to another, more so in higher income countries [32]. Waste segregation is important especially in healthcare not only from an ecological standpoint but also economical one as clinical waste is the most expensive to treat [30].
As of 2013, a meaningful recycling programme has taken place in about 80% of Australian hospitals, about 50% in the USA but less than 10% in the UK [32]. This difference may be due to varying abilities to segregate waste because of strict infection control rules and fear of contamination, leading to incineration of potentially recyclable items [38]. In a survey published in 2012, only 11% (n = 780) of participating anaesthetists from Australia, New Zealand and England agreed that adequate recycling occurred in their theatre [39]. Of course, recycling also comes with its cost; the impact of carbon emissions from collection, sorting and reprocessing needs to be considered. Furthermore, a significant proportion of recycled paper, scrap metal, with approximately 70% exported to China and Hong Kong in 2016, led China to impose a ban on waste imports. This raises questions about sustainability of recycling [32, 35]. In 2015, McGain and colleagues published a cohort study reporting that recycling did not lead to additional costs and that the overall impact of recycling (although savings may be small) may be magnified if adapted by the national healthcare system [40].
‘Green initiatives, incentives or awards’ may encourage surgeons and administrators to rethink the global and financial impact of the unnecessary waste produced [31]. Perhaps ophthalmologists can be invited to participate in an innovative competition to design a surgeon-tailored instrument pack based on each subspecialty in ophthalmology to best cut down unnecessary waste and cost, whilst maintaining patient safety.
As pre-existing literature on environmental impact on current ophthalmic practices is scarce, more research and publications are needed to help map out the carbon footprint of various eye care services especially relating to cataract surgery and glaucoma care in the community [7]. More data is needed on environmental impacts of healthcare activities, life cycle analysis of materials, and cost analysis. Innovative design of devices that minimise environmental impact whilst maintaining standard of care would also be useful [33].
Restructuring Ophthalmic Delivery of Care
Ophthalmology is one of the busiest specialties in the NHS with a predicted increase in demand by 30–40% over the next 20 years [41, 42]. As of 2019, primary care referrals have increased by 12% from 2013 to 2014. In England and Wales, approximately 2.5 million people 65 years and above have visual impairment related to cataracts leading to an increasing need for outpatient services. The demand for cataract surgery is predicted to rise by 50% in the next 20 years from year 2017. Glaucoma is the most common cause of visual impairment in people over 70 years old and is predicted to rise by 44% over the next 15 years [43]. Up to 20% of new referrals are for ‘suspected glaucoma’ and the number of ‘false positive’ referrals has increased following the introduction of the first National Institute for Clinical Excellence (NICE) glaucoma guideline [44, 45]. Inappropriate referrals to the outpatient ophthalmology service are estimated to be between 20% and 65% [46–48]. This leads to unnecessary costs, capacity issues, travel-associated carbon emission, and unnecessary (clinical and non-clinical) waste production. Filtering schemes like the Manchester Glaucoma Enhanced Referral Scheme (GERS) have resulted in a 53% reduction in false positive referrals between April 2013 and November 2016, whilst maintaining clinical efficacy with no cases of missed glaucoma or non-glaucomatous pathology [49, 50].
More Local Delivery of Care
As large quantities of greenhouse gases are generated by patients travelling to access hospital-based healthcare, smaller treatment centres or screening hubs for patients with chronic eye conditions like AMD could be established peripherally in a number of locations, reducing transport-associated carbon emission. The challenge associated with delivering care in this way is the initial investment required, especially when such schemes may not offer a financial saving [51]. As the NHS moves to a population-focused planning and delivery of healthcare through the Integrated Care Systems there is an opportunity for such services at a regional level. Furthermore, an upskilled optometry workforce provides the opportunity for care to be delivered from optometry practices already located across towns, cities, and suburban areas offering convenient and closer-to-home locations. This approach again aligns with the NHS England care closer to home strategy, providing a number of benefits not least the reduction in patient miles. Many community optometrists have taken up training to provide extended care services to patients, allowing continuing professional development for particular clinical interests, whilst offering additional income generation under their NHS contracts. Nationally, optometrists who specialise in certain areas of ophthalmology and ophthalmic specialist nurses are already undertaking outpatient appointments and intravitreal injections respectively. These new models of care would provide care closer to where patients live and often located by public transport routes with opportunities to walk or cycle, thereby significantly reducing patient miles.
Teleophthalmology/Health Information Technology
The use of teleophthalmology and health information technology can help save time, energy and raw materials like paper and plastic and their subsequent impact on the environment and our planet [52]. The collaborative effort of the Teleophthalmology Network in Scotland is one example of this approach. By supporting optometric practices to utilise smartphones attached to slit lamps, enabling ocular biomicroscopic videography, ophthalmologists are able to view a patient’s examination features in real time without the patient attending, thereby streamlining the ophthalmic triaging system [53]. Purohit and colleagues published a systematic review targeting transport-associated emissions and found that the carbon footprint saved using telemedicine ranges between 0.7 and 372 kg CO2eq per consultation [54]. Sharafeldin and colleagues undertook a review on economic evaluation that supports evidence of cost-effectiveness of teleophthalmology on chronic conditions like diabetic retinopathy and glaucoma [55]. An audit carried out in Western Australia consisting of 709 patients found that they were able to correctly diagnose 95% of patients via remote consultations and saved over 10 days of outreach clinics for 287 patients with cataract seen and managed [56]. The use of teleophthalmology or virtual consultations have exponentially increased during the COVID-19 pandemic, to provide outpatient appointments in a way that usual change management cycles would have taken significantly longer to achieve. Although this was not suitable for all patients and types of appointment, it helped keep in-person hospital attendances to a minimum, whilst reducing patient miles travelled. Older patients may struggle with the not-so-traditional way of healthcare provision and the initial learning curve of telemedicine. Obtaining accurate visual acuity and clinical examination for future comparison may be difficult and is no substitute for face-to-face clinical examination. Nonetheless, with the advancement of technology, teleophthalmology offers an opportunity to deliver some suitable services remotely and provides a way to reduce the carbon footprint of services whilst allowing access to care in geographically isolated areas [57, 58].
Home Tele-screening
The emergence of a variety of home devices for the monitoring of visual acuity, visual fields, and intraocular pressure for conditions such as diabetic retinopathy, AMD, and glaucoma also present as a movement away from traditional clinic visits and towards sustainability [59–63]. In particular, ForeseeHome™ (conducts preferential hyperacuity perimetry for monitoring AMD) [64], myVisiontrack™ (uses shape discrimination hyperacuity testing in AMD and diabetic retinopathy) [65], and Alleye™ (detects neovascular AMD and distinguishes between dry and wet AMD) [66] are US Food and Drug Administration (FDA) approved platforms for monitoring patients. Integration of these applications within existing monitoring programmes could help in substantially reducing carbon footprints.
Artificial Intelligence
The application of artificial intelligence (AI) approaches such as deep learning (DL) to ophthalmic imaging, including digital fundus photographs and visual fields, has been reported to achieve high accuracy in automating the screening and diagnosis of common vision-threatening diseases including diabetic retinopathy [67–69], glaucoma [70–72], AMD [73, 74], and retinopathy of prematurity (ROP) [75]. A DL algorithm system developed by Abramoff et al., IDx-DR, has received FDA approval since 2018 for the detection of more-than-mild diabetic retinopathy in adults without physician-assisted interpretation [76]. Combining the use of ‘imaging hubs’ and AI technology would therefore be as a valuable adjunct in the mission towards improving sustainability in ophthalmology.
Promoting Environmental Sustainability
The International Agency for the Prevention of Blindness (IAPB) declared a climate emergency on the 22 April 2021 and released key resources that feature how the ‘Eye Health Sector’ can contribute to environmental sustainability. The key areas for actions which organisations can focus on to promote sustainability include acknowledging the climate emergency, the development of local and international frameworks, setting targets for carbon emission reduction, raising awareness, development of sustainable procurement policies whilst working with suppliers, reducing use of energy and water, minimising travel, reducing waste generated and finally implementing environmental sustainability in education [8, 77–79].
Both the General Medical Council (GMC) and Nursing and Midwifery Council (NMC) in the UK now require newly qualified doctors and nurses to be informed about sustainable healthcare and apply its principles and methods to their clinical practice [80, 81]. To promote this, medical schools in the UK have already begun to incorporate lectures and student-selected modules on sustainable healthcare into their curriculum [82]. Optical governing bodies including Association of Optometrists (AOP), Association of British Dispensing Opticians (ABDO), and General Optical Council (GOC) are also prioritising sustainability, evident by the organisation of the forthcoming ‘SEE Summit’ [83].
The Centre for Sustainable Healthcare has described five principles for practising sustainable healthcare. The principles comprise prevention, patient empowerment (health promotion and education), lean pathways (telecommunication), low-carbon alternatives (e.g. avoiding use of greenhouse gases such as nitrogen oxide), and operational resource use (e.g. reducing packaging and water consumption) [84]. These could be integrated into postgraduate training and education for doctors and allied health practitioners, in the form of online short courses and induction modules [85], further supporting the drive towards sustainable healthcare.
Conclusion
The use of disposable equipment and instrumentation has been increasing proportional to the increase in demand on ophthalmic services and the increase in emphasis on safety, especially in developed countries. There is action we could take to reduce the environmental impact generated from our services whilst maintaining the highest standards of safety and care to our patients. It is vital for clinicians, healthcare professionals and their managerial teams, manufacturers and pharmaceutical companies to realise the cumulative waste generated and the harmful impact they cause the environment, public health, long-term morbidity and the life of our future generations.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Funding
No funding or sponsorship was received for this study or the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Yee Ling Wong was involved in the conception and the first draft of the manuscript. Yee Ling Wong, Maha Noor, Katie L James and Tariq M Aslam contributed to the final version of the manuscript. Yee Ling Wong, Maha Noor, Katie L James and Tariq M Aslam were involved in revising, critically appraising and final approval of the manuscript.
Disclosures
Yee Ling Wong, Maha Noor and Katie L James declare that they have no personal, financial, commercial, or academic conflict of interest. Tariq M Aslam’s declarations of interest: Grant Funding, Personal fees from Bayer, Novartis, Thea Pharmaceuticals, Roche, Bausch and Laumb, Canon, Topcon, Heidelberg. Medical advisor to Give Vison. Founder and director, Clin-e-cal. Member of the Green Party.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
- 1.Watts N, Amann M, Arnell N, et al. The 2019 report of The Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394(10211):1836–1878. doi: 10.1016/S0140-6736(19)32596-6. [DOI] [PubMed] [Google Scholar]
- 2.IPCC. Global warming of 1.5 °C. An IPCC Special Report on the impacts of global warming of 1.5 °C above pre-industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of climate change, sustainable development, and efforts to eradicate poverty. Geneva: World Meteorological Organization; 2019.
- 3.McMichael AJ, Haines JA, Slooff R, et al. Climate change and human health: an assessment/prepared by a Task Group on behalf of the World Health Organization, the World Meteorological Association and the United Nations Environment Programme. Geneva: World Health Organisation; 1996. [Google Scholar]
- 4.McMichael T. Public health in Australia: a personal reflection. Aust J Public Health. 2010;17(4):295–296. doi: 10.1111/j.1753-6405.1993.tb00155.x. [DOI] [PubMed] [Google Scholar]
- 5.Watts N, Amann M, Arnell N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021;397(10269):129–170. doi: 10.1016/S0140-6736(20)32290-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Royal College of Ophthalmologists. Sustainability in ophthalmology. https://www.rcophth.ac.uk/wp-content/uploads/2014/11/2013_PROF_222_Sustainability-in-Ophthalmology-May-2013.pdf. Accessed Jul 4, 2021.
- 7.Yu M, Khan I. Climate action in eyecare. www.eyenews.uk.com. Accessed Jul 21, 2021.
- 8.King's College London. Higher air pollution days trigger cardiac arrests and hospitalisations. https://www.kcl.ac.uk/news/higher-air-pollution-days-trigger-cardiac-arrests-and-hospitalisations. Accessed Aug 5, 2021.
- 9.Landrigan PJ, Fuller R, Acosta NJR, et al. The Lancet Commission on pollution and health. Lancet. 2018;391(10119):462–512. doi: 10.1016/S0140-6736(17)32345-0. [DOI] [PubMed] [Google Scholar]
- 10.Costello A, Abbas M, Allen A, et al. Managing the health effects of climate change. Lancet. 2009;373(9676):1693–1733. doi: 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- 11.Pradyumna A, Guinto R. Climate change and health. Lancet. 2016;387(10017):430–431. doi: 10.1016/S0140-6736(16)00171-9. [DOI] [PubMed] [Google Scholar]
- 12.Lenzen M, Malik A, Li M, et al. The environmental footprint of health care: a global assessment. Lancet Planetary Health. 2020;4(7):e271–e279. doi: 10.1016/S2542-5196(20)30121-2. [DOI] [PubMed] [Google Scholar]
- 13.Holden E, Linnerud K, Banister D. Sustainable development: our common future revisited. Glob Environ Chang. 2014;26:130–139. [Google Scholar]
- 14.WCED . Our common future. World commission on environment and development. Oxford: Oxford University Press; 1987. [Google Scholar]
- 15.Eckelman MJ, Sherman J. Environmental impacts of the U.S. health care system and effects on public health. PLoS ONE. 2016;11(6):e0157014. doi: 10.1371/journal.pone.0157014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Total healthcare expenditure in the United Kingdom from 1997 to 2019. 2021. https://www.statista.com/statistics/317669/healthcare-expenditure-in-the-united-kingdom/. Accessed Sep 26, 2021.
- 17.National Health Service England, Public Health England . Reducing the use of natural resources in health and social care. London: National Health Service England; 2018. [Google Scholar]
- 18.National Health Service England. Greener NHS campaign to tackle climate ‘health emergency’. https://www.england.nhs.uk/2020/01/greener-nhs-campaign-to-tackle-climate-healthemergency/. Accessed Jul 4, 2021.
- 19.The Royal College of Ophthalmologists. National Ophthalmology Database Audit. https://www.nodaudit.org.uk/u/docs/20/urxqilwxmv/NOD%20Audit%20Annual%20Report%202019.pdf. Accessed Jul 7, 2021.
- 20.Morris DS, Wright T, Somner JEA, Connor A. The carbon footprint of cataract surgery. Eye. 2013;27(4):495–501. doi: 10.1038/eye.2013.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Somner J, Scott K, Morris D, Gaskell A, Shepherd I. Ophthalmology carbon footprint: something to be considered? J Cataract Refract Surg. 2009;35(1):202–203. doi: 10.1016/j.jcrs.2008.09.026. [DOI] [PubMed] [Google Scholar]
- 22.Venkatesh R, van Landingham SW, Khodifad AM, et al. Carbon footprint and cost-effectiveness of cataract surgery. Curr Opin Ophthalmol. 2016;27(1):82–88. doi: 10.1097/ICU.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 23.Muralikrishnan R, Venkatesh R, Prajna NV, Frick KD. Economic cost of cataract surgery procedures in an established eye care centre in Southern India. Ophthalmic Epidemiol. 2004;11(5):369–380. doi: 10.1080/09286580490888762. [DOI] [PubMed] [Google Scholar]
- 24.Gogate P, Deshpande M, Nirmalan PK. Why do phacoemulsification? Manual small-incision cataract surgery is almost as effective, but less expensive. Ophthalmology. 2007;114(5):965–968. doi: 10.1016/j.ophtha.2006.08.057. [DOI] [PubMed] [Google Scholar]
- 25.Ruit S, Tabin G, Chang D, et al. A prospective randomized clinical trial of phacoemulsification vs manual sutureless small-incision extracapsular cataract surgery in Nepal. Am J Ophthalmol. 2007;143(1):32–38.e2. doi: 10.1016/j.ajo.2006.07.023. [DOI] [PubMed] [Google Scholar]
- 26.Amitava A, Khan A, Rizvi SA, Siddiqui Z, Kumari N, Grover S. Cost-effectiveness analysis should continually assess competing health care options especially in high volume environments like cataract surgery. Indian J Ophthalmol. 2015;63(6):496. doi: 10.4103/0301-4738.162600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goel H, Wemyss TA, Harris T, et al. Improving productivity, costs and environmental impact in International Eye Health Services: using the ‘Eyefficiency’ cataract surgical services auditing tool to assess the value of cataract surgical services. BMJ Open Ophthalmol. 2021;6(1):e000642. doi: 10.1136/bmjophth-2020-000642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thiel CL, Schehlein E, Ravilla T, et al. Cataract surgery and environmental sustainability: waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg. 2017;43(11):1391–1398. doi: 10.1016/j.jcrs.2017.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chang DF. Needless waste and the sustainability of cataract surgery. Ophthalmology. 2020;127(12):1600–1602. doi: 10.1016/j.ophtha.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guetter CR, Williams BJ, Slama E, et al. Greening the operating room. Am J Surg. 2018;216(4):683–688. doi: 10.1016/j.amjsurg.2018.07.021. [DOI] [PubMed] [Google Scholar]
- 31.Brown C, Meals C. Four ways plastic surgeons can fight climate change. Plast Reconstr Surg. 2020;8(7):e2961. doi: 10.1097/GOX.0000000000002961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives—the old, the new, and the way forward: a narrative review. Waste Manag Res. 2019;37(1):3–19. doi: 10.1177/0734242X18793937. [DOI] [PubMed] [Google Scholar]
- 33.Kagoma Y, Stall N, Rubinstein E, Naudie D. People, planet and profits: the case for greening operating rooms. CMAJ. 2012;184(17):1905–1911. doi: 10.1503/cmaj.112139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Practice Greenhealth. The business case for greening the OR. https://www.c4spgh.org/HCW1_Presentations/GOR_FullSet_Guidance%20Docs_Web_042711.pdf. Accessed Jul 8, 2021.
- 35.Bartl A. Moving from recycling to waste prevention: a review of barriers and enables. Waste Manag Res. 2014;32(9_suppl):3–18. doi: 10.1177/0734242X14541986. [DOI] [PubMed] [Google Scholar]
- 36.Kwakye G. Green surgical practices for health care. Arch Surg. 2011;146(2):131. doi: 10.1001/archsurg.2010.343. [DOI] [PubMed] [Google Scholar]
- 37.Armitage WJ, Tullo AB, Ironside JW. Risk of Creutzfeldt-Jakob disease transmission by ocular surgery and tissue transplantation. Eye. 2009;23(10):1926–1930. doi: 10.1038/eye.2008.381. [DOI] [PubMed] [Google Scholar]
- 38.Southorn T, Norrish A, Gardner K, Baxandall R. Reducing the carbon footprint of the operating theatre: a multicentre quality improvement report. J Perioper Pract. 2013;23(6):144–146. doi: 10.1177/175045891302300605. [DOI] [PubMed] [Google Scholar]
- 39.McGain F, White S, Mossenson S, Kayak E, Story D. A survey of anesthesiologistsʼ views of operating room recycling. Anesth Analg. 2012;114(5):1049–1054. doi: 10.1213/ANE.0b013e31824d273d. [DOI] [PubMed] [Google Scholar]
- 40.McGain F, Jarosz KM, Nguyen MNHH, Bates S, O’Shea CJ. Auditing operating room recycling: a management case report. A A Case Rep. 2015;5(3):47–50. doi: 10.1213/XAA.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 41.The Royal College of Ophthalmologists. New RCOphth Workforce Census illustrates the severe shortage of eye doctors in the UK. https://www.rcophth.ac.uk/2019/01/new-rcophth-workforce-census-illustrates-the-severe-shortage-of-eye-doctors-in-the-uk/. Accessed Jul 14, 2021.
- 42.NHS Digital. Hospital Outpatient Activity, 2017–18. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-outpatient-activity/2017-18. Accessed Jul 14, 2021.
- 43.MacEwen C, Davis A, Chang L. Ophthalmology GIRFT Programme National Specialty Report. https://gettingitrightfirsttime.co.uk/wp-content/uploads/2019/12/OphthalmologyReportGIRFT19P-FINAL.pdf. Accessed Jul 14, 2021.
- 44.Ratnarajan G, Newsom W, Vernon SA, et al. The effectiveness of schemes that refine referrals between primary and secondary care—the UK experience with glaucoma referrals: the Health Innovation and Education Cluster (HIEC) Glaucoma Pathways Project. BMJ Open. 2013;3(7):e002715. doi: 10.1136/bmjopen-2013-002715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shah S, Murdoch IE. NICE—impact on glaucoma case detection. Ophthalmic Physiol Opt. 2011;31(4):339–342. doi: 10.1111/j.1475-1313.2011.00843.x. [DOI] [PubMed] [Google Scholar]
- 46.Burr JM, Mowatt G, Hernández R, et al. The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation. Health Technol Assess. 2007 doi: 10.3310/hta11410. [DOI] [PubMed] [Google Scholar]
- 47.Bowling B, Chen SDM, Salmon JF. Outcomes of referrals by community optometrists to a hospital glaucoma service. Br J Ophthalmol. 2005;89:1102–1104. doi: 10.1136/bjo.2004.064378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vincent SJ, Vincent RA, Shields D, Lee GA. Comparison of intraocular pressure measurement between rebound, non-contact and Goldmann applanation tonometry in treated glaucoma patients. Clin Exp Ophthalmol. 2012;40(4):e163–e170. doi: 10.1111/j.1442-9071.2011.02670.x. [DOI] [PubMed] [Google Scholar]
- 49.Forbes H, Sutton M, Edgar DF, et al. Impact of the Manchester Glaucoma Enhanced Referral Scheme on NHS costs. BMJ Open Ophthalmol. 2019;4(1):e000278. doi: 10.1136/bmjophth-2019-000278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gunn PJG, Marks JR, Konstantakopoulou E, et al. Clinical effectiveness of the Manchester Glaucoma Enhanced Referral Scheme. Br J Ophthalmol. 2019;103(8):1066–1071. doi: 10.1136/bjophthalmol-2018-312385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tomson C. Reducing the carbon footprint of hospital-based care. Future Hosp J. 2015;2(1):57–62. doi: 10.7861/futurehosp.2-1-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yellowlees PM, Chorba K, Burke Parish M, Wynn-Jones H, Nafiz N. Telemedicine can make healthcare greener. Telemed e-Health. 2010;16(2):229–232. doi: 10.1089/tmj.2009.0105. [DOI] [PubMed] [Google Scholar]
- 53.NHS Scotland. 'Teleophthalmology Activation Guide’. 2020. http://communityeyecare.scot.nhs.uk/telemedicine. Accessed Aug 10, 2021.
- 54.Purohit A, Smith J, Hibble A. Does telemedicine reduce the carbon footprint of healthcare? A systematic review. Future Healthc J. 2021;8(1):e85–91. doi: 10.7861/fhj.2020-0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sharafeldin N, Kawaguchi A, Sundaram A, et al. Review of economic evaluations of teleophthalmology as a screening strategy for chronic eye disease in adults. Br J Ophthalmol. 2018;102(11):1485–1491. doi: 10.1136/bjophthalmol-2017-311452. [DOI] [PubMed] [Google Scholar]
- 56.Bartnik SE, Copeland SP, Aicken AJ, Turner AW. Optometry-facilitated teleophthalmology: an audit of the first year in Western Australia. Clin Exp Optom. 2018;101(5):700–703. doi: 10.1111/cxo.12658. [DOI] [PubMed] [Google Scholar]
- 57.Liu Y, Torres Diaz A, Benkert R. Scaling up teleophthalmology for diabetic eye screening: opportunities for widespread implementation in the USA. Curr Diab Rep. 2019;19(9):74. doi: 10.1007/s11892-019-1187-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Patel S, Hamdan S, Donahue S. Optimising telemedicine in ophthalmology during the COVID-19 pandemic. J Telemed Telecare. 2020 doi: 10.1177/1357633X20949796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ittoop SM, SooHoo JR, Seibold LK, Mansouri K, Kahook MY. Systematic review of current devices for 24-h intraocular pressure monitoring. Adv Ther. 2016;33(10):1679–1690. doi: 10.1007/s12325-016-0388-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Anderson AJ, Bedggood PA, George Kong YX, Martin KR, Vingrys AJ. Can home monitoring allow earlier detection of rapid visual field progression in glaucoma? Ophthalmology. 2017;124(12):1735–1742. doi: 10.1016/j.ophtha.2017.06.028. [DOI] [PubMed] [Google Scholar]
- 61.Amirsolaimani B, Peyman G, Schwiegerling J, Bablumyan A, Peyghambarian N. A new low-cost, compact, auto-phoropter for refractive assessment in developing countries. Sci Rep. 2017 doi: 10.1038/s41598-017-14507-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ciuffreda KJ, Rosenfield M. Evaluation of the SVOne: a handheld, smartphone-based autorefractor. Optom Vis Sci. 2015;92(12):1133–1139. doi: 10.1097/OPX.0000000000000726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wisse RPL, Muijzer MB, Cassano F, Godefrooij DA, Prevoo YFDM, Soeters N. Validation of an independent web-based tool for measuring visual acuity and refractive error (the manifest versus online refractive evaluation trial): prospective Open-Label Noninferiority Clinical Trial. J Med Internet Res. 2019;21(11):e14808. doi: 10.2196/14808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chew EY, Clemons TE, Harrington M, et al. AREDS2-Home Study Research Group. Effectiveness of different monitoring modalities in the detection of neovascular age-related macular degeneration: the Home Study, Report Number 3. Retina. 2016;36(8):1542–1547. doi: 10.1097/IAE.0000000000000940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Micheletti JM, Hendrick AM, Khan FN, Ziemer DC, Pasquel FJ. Current and next generation portable screening devices for diabetic retinopathy. J Diabetes Sci Technol. 2016;10:295–300. doi: 10.1177/1932296816629158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schmid MK, Thiel MA, Lienhard K, Schlingemann RO, Faes L, Bachmann LM. Reliability and diagnostic performance of a novel mobile app for hyperacuity self-monitoring in patients with age-related macular degeneration. Eye. 2019;33:1584–1589. doi: 10.1038/s41433-019-0455-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Abramoff MD, Lou YY, Erginay A, et al. Improved automated detection of diabetic retinopathy on a publicly available dataset through integration of deep learning. Investig Ophthalmol Vis Sci. 2016;57:5200–5206. doi: 10.1167/iovs.16-19964. [DOI] [PubMed] [Google Scholar]
- 68.Gulshan V, Peng L, Coram M, et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA. 2016;316:2402–2410. doi: 10.1001/jama.2016.17216. [DOI] [PubMed] [Google Scholar]
- 69.Raumviboonsuk P, Krause J, Chotcomwongse P, et al. Deep learning versus human graders for classifying diabetic retinopathy severity in a nationwide screening program. NPJ Digit Med. 2019;2:25. doi: 10.1038/s41746-019-0099-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liu H, Li L, Wormstone IM, et al. Development and validation of a deep learning system to detect glaucomatous optic neuropathy using fundus photographs. JAMA Ophthalmol. 2019;137(12):1353–1360. doi: 10.1001/jamaophthalmol.2019.3501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Li F, Wang Z, Qu GX, et al. Automatic differentiation of glaucoma visual field from non-glaucoma visual filed using deep convolutional neural network. BMC Med Imag. 2018;18:35. doi: 10.1186/s12880-018-0273-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Masumoto H, Tabuchi H, Nakakura S, Ishitobi N, Miki M, Enno H. Deep-learning classifier with an ultrawide-field scanning laser ophthalmoscope detects glaucoma visual field severity. J Glaucoma. 2018;27:647–652. doi: 10.1097/IJG.0000000000000988. [DOI] [PubMed] [Google Scholar]
- 73.Grassmann F, Mengelkamp J, Brandl C, et al. A deep learning algorithm for prediction of age-related eye disease study severity scale for age-related macular degeneration from color fundus photography. Ophthalmology. 2018;125:1410–1420. doi: 10.1016/j.ophtha.2018.02.037. [DOI] [PubMed] [Google Scholar]
- 74.Burlina PM, Joshi N, Pekala M, Pacheco KD, Freund DE, Bressler NM. Automated grading of age-related macular degeneration from color fundus images using deep convolutional neural networks. JAMA Ophthalmol. 2017;135:1170–1176. doi: 10.1001/jamaophthalmol.2017.3782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Brown JM, Campbell JP, Beers A, et al. Imaging and informatics in retinopathy of prematurity (i-ROP) research consortium. Automated diagnosis of plus disease in retinopathy of prematurity using deep Convolutional Neural Networks. JAMA Ophthalmol. 2018;136(7):803–810. doi: 10.1001/jamaophthalmol.2018.1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Abramoff MD, Lavin PT, Birch M, Shah N, Folk JC. Pivotal trial of an autonomous AI-based diagnostic system for detection of diabetic retinopathy in primary care offices. NPJ Digit Med. 2018;1:39. doi: 10.1038/s41746-018-0040-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Global Sight Alliance declares Climate Emergency and Calls for Urgent Action. IAPB, 2021. https://www.iapb.org/news/global-sight-alliance-declares-climate-emergencyand-calls-for-urgent-action/. Accessed Aug 10, 2021.
- 78.Call to Action for Environmentally Sustainable Practices in the Eye Health Sector. IAPB, 2021. https://www.iapb.org/wp-content/uploads/2021/04/IAPB_CAWG_CTAdocument.pdf. Accessed Aug 10, 2021.
- 79.Guide for Environmentally Sustainable Practices in the Eye Health Sector. IAPB, 2021. https://www.iapb.org/wp-content/uploads/2021/04/IAPB_CAWG_GUIDE-document.pdf. Accessed Aug 10, 2021.
- 80.General Medical Council. Outcomes for graduates. 2018. www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates. Accessed Aug 10, 2021.
- 81.Nursing and Midwifery Council. Standards of Proficiency for Midwives. 2021. https://www.nmc.org.uk/globalassets/sitedocuments/standards/standards-of-proficiency-for-midwives.pdf. Accessed Aug 10, 2021.
- 82.Tun MS. Fulfilling a new obligation: teaching and learning of sustainable healthcare in the medical education curriculum. Med Teach. 2019;41:1168–1177. doi: 10.1080/0142159X.2019.1623870. [DOI] [PubMed] [Google Scholar]
- 83.Association of British Dispensing Opticians. SEE Summit. 2021. https://www.abdo.org.uk/dashboard/see-hub/see-hub-2/. Accessed Aug 10, 2021.
- 84.Mortimer F. The sustainable physician. Clin Med (Lond) 2010;10(2):110–111. doi: 10.7861/clinmedicine.10-2-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gandhi V, Al-Hadithy N, Göpfert A, Knight K, van Hove M, Hockey P. Integrating sustainability into postgraduate medical education. Future Healthcare J. 2020;7(2):102–104. doi: 10.7861/fhj.2020-0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.