Abstract
Objectives
Medical litigation resulting from diagnostic errors leads to lawsuits that are time-consuming, expensive, and psychologically burdensome. Few studies have focused on internists, who are more likely to make diagnostic errors than others, with assessments of litigation in terms of system and diagnostic errors. This study explored factors contributing to internists losing lawsuits and examined whether system or diagnostic errors were more important on the outcome.
Methods
Data regarding 419 lawsuits against internists closed between 1961 and 2017 were extracted from a public Japanese database. Factors affecting litigation outcomes were identified by comparative analysis focusing on system and diagnostic errors, environmental factors, and differences in initial diagnoses.
Results
Overall, 419 malpractice claims against internists were analyzed. The rate of lawsuits being decided against internists was high (50.1%). The primary cause of litigation was diagnostic errors (213, 54%), followed by system errors (188, 45%). The foremost initial diagnostic error was “no abnormality” (17.2%) followed by ischemic heart disease (9.6%) and malignant neoplasm (8.1%). Following cause-adjustment for loss, system errors were 21.37 times more likely to lead to a loss. Losses were 6.26 times higher for diagnostic error cases, 2.49 times higher for errors occurring at night, and 3.44 times higher when “malignant neoplasm” was the first diagnosis.
Conclusions
This study found that system errors strongly contributed to internists' losses. Diagnostic errors, night shifts, and initial diagnoses of malignant neoplasms also significantly affected trial outcomes. Administrators must focus on both system errors and diagnostic errors to enhance the safety of patients and reduce internists' risk exposure.
Keywords: diagnostic error, internal medicine, malignant neoplasm, medical malpractice claims, system error
Introduction
The impact of medical errors on healthcare is enormous and a critical issue that needs to be addressed (1-3). A report from the US suggests that medical error is the third leading cause of death (approximately 250,000 deaths annually) after heart disease and cancer (4). The authors argue that, to improve medical safety, we need to clarify and address the causes of errors at the individual and system levels. Furthermore, an estimated 40,000 to 80,000 deaths are caused by diagnostic errors in the US annually (3,5). Such errors have been the subject of focus in recent years, suggesting that they may have a significant negative impact on health economics and medical safety for both patients and medical practitioners, as exemplified by the involvement of healthcare providers in medical lawsuits (6-8).
Medical lawsuits are time-consuming and economically and psychologically burdensome. Several epidemiological and observational studies of the frequency of malpractice claims and the magnitude of awarded compensation indicate that diagnostic errors are a significant cause of medical litigation (5,8-12). In general, it is difficult to estimate the actual frequency of errors from epidemiological studies' data of medical litigation because of selection bias in the trial process and in settlements. However, it is useful to analyze the causes of errors from published detailed affidavits, including third-party medical professionals' views (9,13).
Previous studies have had several drawbacks. First, there has been little analysis of the factors contributing to litigation against internists (9,14,15). Second, no studies have examined the contribution of system and diagnostic errors to medical litigation outcomes (15,16). Therefore, we conducted a secondary analysis of medical litigation data extracted from Japanese court records.
The present study explored factors that lead to internists losing cases brought against them and examined whether system errors or diagnostic errors were more significant in predicting such losses. Ultimately, our goal was to explore the factors that need to receive focus in order to improve healthcare.
Study design
This qualitative study is a secondary analysis of data on malpractice cases against internists concluded between 1961 and June 2017 extracted from an Internet database of nationwide legal cases in Japan.
Study protocol
On June 29, 2017, we extracted data on malpractice cases against internists concluded between 1961 and June 2017 from the most extensive public database in Japan (Westlaw Japan). We used a permuted combination of keywords including “medical malpractice,” “medical claims,” “medical litigation,” and “diagnostic errors.” We extracted a total of 1,802 lawsuits against physicians in Japan. Next, we excluded 1,378 claims against non-internal medicine physicians and cases in which it was unclear whether there was a final pay-out to the patient or family (five cases). This left 419 cases for the analysis (Fig. 1). Five reviewers performed the data extraction: a lawyer, a pharmacist, two senior medical students, and the principal investigator. Finally, all claims of diagnostic and system errors were double-checked by the lawyer and the principal investigator according to a previous study (17).
Figure 1.
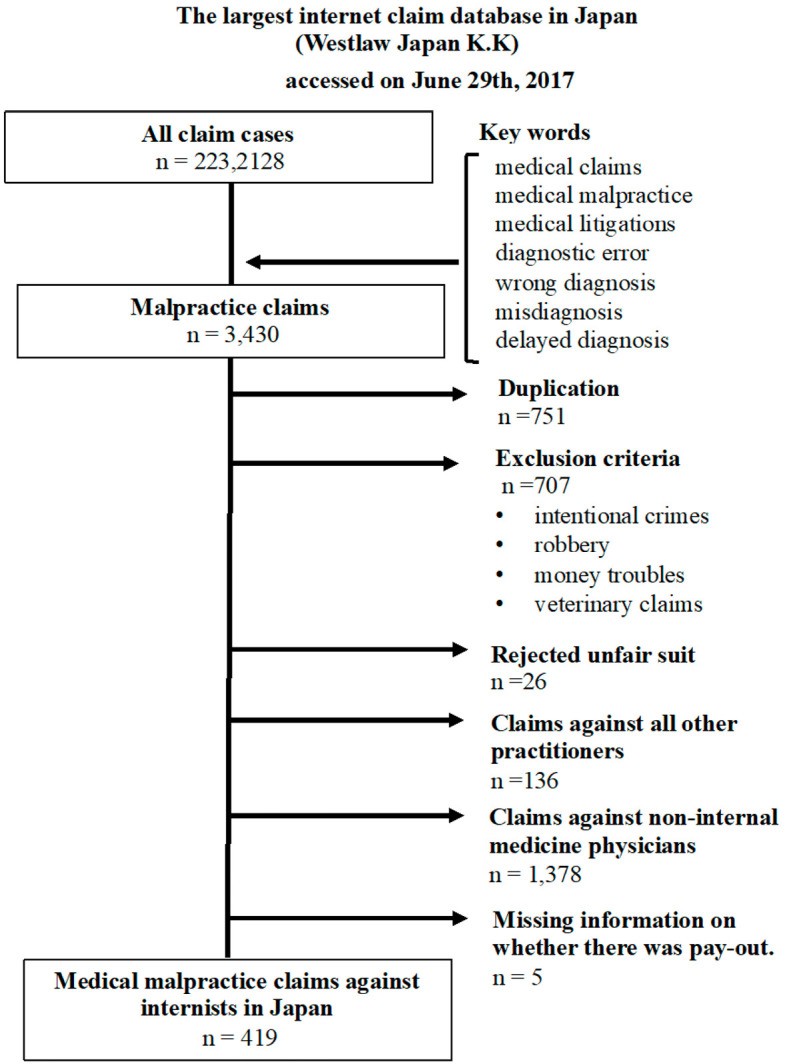
Flow diagram of the process for shortlisting the study sample.
Variables and definitions
The collected data included detailed information, such as the clinical setting of each case, time of day the error occurred (day or night shift), size of the institution, patient background, sex and age of the patient, disputed point of the claims, and relevant patient diagnosis. All eligible cases had elements of diagnostic error or system error, or both. Diagnostic error was defined as a “delayed diagnosis,” “misdiagnosis,” or “wrong diagnosis.” System errors were categorized based on descriptions in the case records as follows: 1) technical and equipment failure, 2) clustering, 3) inadequate policies and procedures, 4) inefficient and non-standard processes, 5) poor teamwork or communication, 6) patient neglect, 7) management problems, 8) poor coordination of care, 9) supervision or education problems, 10) unavailable expert consultation, 11) lack of training and orientation, 12) personnel problems (e.g., laziness and violations), and 13) external interference (17).
Outcome measures
The measured patient outcome variables were full recovery, permanent injury, death, and claims resulting (acceptance or rejection) in a final judgment and compensation for malpractice claims. All payments were adjusted based on the Japanese Consumer Price Index from Japanese yen to US dollars (110 yen to the dollar; 21 March 2020).
Statistical analyses
We used standard descriptive statistics to calculate the number, percentage, mean, and median payment amounts for each malpractice claim. A chi-squared test or Fisher's exact test was used to compare nominal variables. For continuous variables, t-tests or Wilcoxon's rank sum tests were employed, where appropriate. For multiple logistic analyses, we incorporated several important factors that were likely to be significant (p<0.1) and likely to win or lose the case, avoiding multicollinearity.
All analyses were performed using the Stata statistical software program, version. 14.0 (StataCorp. 2015. Stata Statistical Software: Release 14. StataCorp College Station, USA). All tests were two-sided, with p<0.05 considered statistically significant.
Results
A total of 419 malpractice claims from 1961 till the end of June 2017 against internists in Japan were analyzed. The patient demographics are shown in Table 1. The acceptance rate of lawsuits against internists (that is, the patient won the case) was high (50.1%). All but six of the accepted lawsuits resulted in payment orders with a median amount of $136,363 [interquartile range (IQR) $28,170-$415,454]. The most common final patient outcome was death (72.3%).
Table 1.
Patient Demographics and Characteristics of Medical Malpractice Claims against Internists in Japan.
| Demographics/Characteristics | Statistics |
|---|---|
| Patient sex (male %) | 57.5% (IQR 52.7%-62.2%) |
| Patient age (IQR) | 50 (IQR 31-61) |
| Adjusted total billing amount ($) | 448,182 (IQR 233,636-757,273) |
| Accepted claim | 210 (50.1%) |
| Adjusted median indemnity ($) | 136,363 (IQR 28,170-415,454)* |
| Duration of claim | 7 years (IQR 5-9) |
| Outcome | Total (%) |
| Deaths | 303 (72.3%) |
| Sequelae | 98 (23.4%) |
| Full recovery | 14 (3.3%) |
| Others | 4 (1.0%) |
Total billing amount and median indemnity were adjusted to their 2017 equivalent using the Japanese Consumer Price Index (shown in USD).
IQR: interquartile range
*Six cases had been accepted by the court; however, there was no payment information or no compensation to the patients.
Fig. 2 shows the causes of malpractice claims, the most common of which was diagnostic error (54%), followed by system error (45%). System errors included patient misidentification, errors in care (slips, lapses, mistakes, etc.), hospital operational problems, and educational issues. In 72 cases (17.2%), both diagnostic and system errors gave rise to the trial. There were 90 cases (21.5%) in which there were no (or unknown) medical provider errors.
Figure 2.
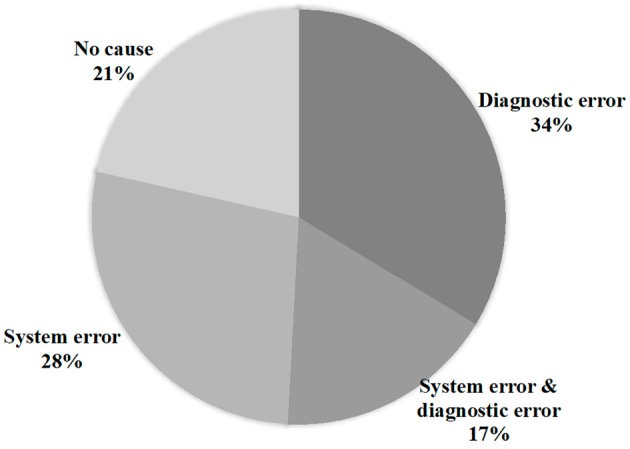
Causes of malpractice claims against internists in Japan (n=419).
Table 2 compares the initial diagnoses (top 10) in medical court cases against internists in the accepted and rejected case groups. The most common initial diagnosis in medical trials was “no abnormality” (including misdiagnosis and delayed diagnosis) (9,16,18), followed by ischemic heart disease (9.6%) and malignant neoplasm (8.1%). The top 10 initial diagnoses were relatively common ones. In particular, respiratory tract infections usually had initial diagnoses of upper respiratory tract disease, including common colds and bronchitis. Diagnoses of non-bleeding digestive tract diseases also included many common diseases, such as constipation and acute gastroenteritis. None of the top 10 initial diagnoses had a statistically significant (unadjusted) relationship with the outcome of the case.
Table 2.
Top 10 Initial Diagnoses Involved in Malpractice Claims Overall, as Well as in the Accepted and Rejected Claims (Rejected=Medical Professional Won the Case).
| The initial diagnosis in malpractice claims | Accepted | Rejected | |||||
|---|---|---|---|---|---|---|---|
| 1st diagnosis | n=419 | % | n=210 | % | n=209 | % | p value |
| No abnormality | 72 | 17.2 | 38 | 18.1 | 34 | 16.3 | 0.62 |
| Ischaemic heart disease | 40 | 9.6 | 23 | 11.0 | 17 | 8.1 | 0.326 |
| Malignant neoplasm | 34 | 8.1 | 20 | 9.5 | 14 | 6.7 | 0.29 |
| Hepatobiliary and pancreatic disease | 30 | 7.2 | 14 | 6.7 | 16 | 7.7 | 0.695 |
| Respiratory tract infection | 30 | 7.2 | 12 | 5.7 | 18 | 8.6 | 0.25 |
| Systematic infectious disease | 24 | 5.7 | 12 | 5.7 | 12 | 5.7 | 0.99 |
| Non-bleeding digestive tract disease | 24 | 5.7 | 12 | 5.7 | 12 | 5.7 | 0.99 |
| Procedure complications | 18 | 4.3 | 9 | 4.3 | 9 | 4.3 | 0.992 |
| Airway and respiratory disorders | 17 | 4.1 | 11 | 5.2 | 6 | 2.9 | 0.219 |
| Endocrine metabolic disease | 17 | 4.1 | 10 | 4.8 | 7 | 3.3 | 0.464 |
| Others | 113 | 30.0 | 49 | 23.3 | 64 | 30.6 | 0.093 |
Table 3 shows the frequency of several factors in medical litigation and the outcomes (unadjusted). The results show that system error and diagnostic error were significantly associated with patients' claims being accepted. The results for environmental factors show that smaller hospitals lost cases significantly more often than larger ones.
Table 3.
Impact of Facility Size, Place, Error Occurrence Time, and Patient Outcomes on Malpractice Claims.
| Accepted n=210 |
Rejected n=209 |
p value | ||
|---|---|---|---|---|
| System error | 145 (69.1%) | 43 (20.6%) | <0.001 | |
| Diagnostic error | 123 (58.6%) | 90 (43.1%) | 0.001 | |
| Facility size | ||||
| Clinic | 60 (28.6%) | 48 (23.0%) | 0.875 | |
| Small hospital (<200 beds) | 58 (27.6%) | 38 (18.2%) | 0.022 | |
| Medium hospital (200-399 beds) | 64 (30.5%) | 77 (36.8%) | 0.168 | |
| Large or university hospital | 28 (13.3%) | 42 (20.1%) | 0.064 | |
| Place | ||||
| Outpatient office | 82 (39.1%) | 72 (34.5%) | 0.329 | |
| Ward | 61 (29.1%) | 63 (30.1%) | 0.806 | |
| Emergency room | 18 (8.6%) | 20 (9.6%) | 0.722 | |
| Procedure room | 39 (18.6%) | 46 (22.0%) | 0.382 | |
| Time | ||||
| Day time | 146 (69.5%) | 137 (65.6%) | 0.385 | |
| Night shift | 31 (14.8%) | 25 (12.0%) | 0.400 | |
| Outcome | ||||
| Deaths | 143 (68.1%) | 160 (76.6%) | 0.053 | |
| Sequelae | 53 (25.2%) | 38 (18.2%) | 0.080 | |
| Full recovery | 11 (5.2%) | 7 (3.4%) | 0.340 | |
Next, we analyzed the factors affecting medical litigation outcomes. Diagnostic errors and system errors were significant factors leading to medical providers' losses. In addition, smaller hospitals (<200 beds) were more likely to lose claims (27.6%) than larger ones. Analyses of the clinical settings, such as the location and time of day when the error occurred, did not reveal any significant differences. No significant differences in relation to patient outcomes were found either. The adjusted total billing amount at the start of the trial for both groups was significantly higher in the accepted group than in the rejected group: $538,182 (IQR $261,818-$874,545) and $396,364 (IQR $184,545-$657,273), respectively (p<0.001). When comparing the number of years taken to reach a final decision on the litigation, there was no significant difference between the accepted and rejected groups (7.13±3.75 vs. 7.52±3.60, p=0.129).
The results of a multiple logistic regression analysis with the adjusted odds ratio (OR) of the characteristics of malpractice claims against internists are presented in Table 4. The adjusted model controls for the type of clinical setting of the initial care and diagnosis. In this adjusted model, cases of system errors were 21.37 times more likely to lead to a pay-out to the patient or his/her family than cases without system errors [95% confidence interval (CI): 11.24-40.60, p<0.001]. Claims of diagnostic errors were 6.26 times more likely to be accepted than claims without diagnostic errors (95% CI: 3.31-11.83, p<0.001). After adjusting, however, a small hospital was not more likely to experience accepted cases relative to other facility sizes, including clinics and medium-to-large hospitals (adjusted OR = 1.44, 95% CI: 0.80-2.58, p=0.224). Cases involving errors occurring at night were 2.49 times more likely to be accepted than those involving any other setting (95% CI: 1.16-1.5.36, p=0.019). However, individual doctors were not more likely to lose cases involving patient death in the ward setting than in other settings. Interestingly, if a malignant neoplasm was the initial diagnosis, the case was 3.44 times more likely to be accepted than cases involving other diagnoses (95% CI: 1.30-9.10; p=0.013). No statistically significant associations of judgments against internists were found after adjusting for other initial diagnoses.
Table 4.
Multiple Logistic Regression Analysis of Factors Causing Internists to Lose Claims Cases.
| Factors | Adjusted odds ratio |
95% CI | z | p value |
|---|---|---|---|---|
| System error | 21.37 | 11.24-40.60 | 9.35 | <0.001 |
| Diagnostic error | 6.26 | 3.31-11.83 | 5.65 | <0.001 |
| Small hospital size | 1.44 | 0.80-2.58 | 1.22 | 0.224 |
| Outpatient office | 1.78 | 0.96-3.32 | 1.83 | 0.068 |
| Ward | 1.30 | 0.69-2.47 | 0.82 | 0.415 |
| Night shift | 2.49 | 1.16-5.36 | 2.34 | 0.019 |
| Death | 0.70 | 0.40-1.23 | -1.23 | 0.217 |
| Defendant is individual doctor | 1.14 | 0.65-2.00 | 0.44 | 0.657 |
| 1st diagnosis: No abnormality | 1.13 | 0.60-2.12 | 0.37 | 0.709 |
| 1st diagnosis: Ischaemic heart disease | 1.79 | 0.76-4.23 | 1.32 | 0.185 |
| 1st diagnosis: Malignant neoplasm | 3.44 | 1.30-9.10 | 2.5 | 0.013 |
The odds ratios (OR) and 95% confidence intervals (CI) are reported. System error, diagnostic error, small hospital size, death, outpatient office, ward, night shift, and each selected initial diagnosis (no abnormality, ischaemic heart disease, malignant neoplasm) were incorporated in the multiple logistic regression analysis.
Discussion
Of the 419 malpractice claims against Japanese internists examined, approximately 50% were settled in favor of the patient. The patient outcome was death in more than 70% of cases. The key finding of this study was that system errors contributed more strongly to internists losing a lawsuit than did diagnostic errors. Although the most common initial diagnosis associated with allegations of diagnostic error was “no abnormality,” after adjusting for the multivariate analysis findings, the only initial diagnosis with a statistically significant probability of causing the patient to win the case was “malignant neoplasm,” suggesting that internists should be particularly careful when reporting a malignancy. Although some studies have examined the final diagnoses involved in medical malpractice claims in each clinical specialty (6,7,9,16,19-21), few have investigated the later identification of the initial diagnosis from the perspective of diagnostic error (9).
Studies have shown that physicians in certain specialties are at a higher risk of being involved in malpractice claims than are those with other specialties (14,22-24). Internal medicine has been shown to have an unusually high rate of diagnostic errors compared to pathology and radiology. Internists, who are the focus of this study, often have to deal with undiagnosed patients and make decisions based on complex factors (8,15,21,25,26).
The diagnostic error rate (50%) and mortality rate (70%) in our study were remarkably high, possibly due to selection bias owing to the focus on internists. In a 25-year summary of malpractice cases in the US, death was the most common outcome (5). However, mortality rates were lower in other settings. In US emergency departments (23), pediatric (19,27), and inpatient/outpatient settings, the reported death rates were 36%, 28.2%, and 30.4%, respectively (6,28). A Japanese study examining non-public malpractice claims noted that death was the most frequent outcome (45%), although in the present study of internists, this value was much higher (29). However, our findings show that death as an outcome had little bearing on whether trials were won or lost; here, the key factors were system related.
Thus, it is essential to develop a better understanding of the differences in the likelihood of litigation in Japan compared to other countries, as well as whether the medical litigation under study is truly meaningful, and differences in the likelihood of litigation and mortality by specialization. Furthermore, after adjusting, our results suggest that adverse events occurring at night are about 2.5 times more likely to result in a healthcare provider losing in court than events occurring in other settings. This result is supported by a Dutch study that found that errors often occur in the afternoon and evening (58%) (13). Therefore, it is necessary to consider the system of healthcare delivery in these settings in Japan to reduce avoidable adverse events as much as possible. Our study corroborates these prior studies and expands upon them by demonstrating the impact of system errors on malpractice claims against an internist.
In Japan, empirical evidence suggests that system error on the part of a healthcare facility may make it easier for patients' claims to be accepted in court than for individual doctors to be held accountable. Nevertheless, conclusive evidence is scarce. This study reaffirms the impact of system errors on medical trial outcomes and shows that hospital management and executives need to focus more on underlying system failures and improve physicians' diagnostic skills. Addressing this goal requires a “no-blame culture” that does not lay the burden of blame on the behavior of individuals; it is essential that critical information about the causes of errors be collected correctly and that errors be prevented and recognized early so that the entire institution can improve quickly (1,2,17,30-32).
Limitations
Several limitations associated with the present study warrant mention. First, the data do not fully quantify the epidemiology of medical litigation nor the frequency of errors. Although we used the largest claims database in Japan (as have previous studies) (9), the data are not representative of all medical malpractice claims. Second, relatively few cases in Japan reach the trial stage. The total number of medical lawsuits in Japan that have received final judgments, including those tried in summary courts and district courts, is small (1,9,29), and malpractice claims that receive final judgments number only a few hundred per year. One reason for this is that, in Japanese culture, prosecuting medical professionals is frowned upon. The low number of trials makes a thorough assessment of the situation problematic because the data used represent only a small fraction of the whole and because there may be insufficient medical transparency. Third, medical malpractice claims data are not full medical records; thus, they are not ideal sources for investigating the frequency of errors or the causal factors in actual clinical practice. Nevertheless, to the best of our knowledge, this study contains detailed clinical information from the largest database in Japan. Fourth, the results cannot be generalized to other countries with different legal systems. In addition, data on medical malpractice claims may be highly selective. To our knowledge, this study is the first to assess the contribution of system and diagnostic errors to medical malpractice litigation in internal medicine in Japan. However, it is impossible to investigate the real causes of medical accidents and prevent their recurrence if only human errors that focus on the responsibility of medical personnel are identified. Without focusing on system errors and implementing remedial measures, the goal of improving overall medical safety will not be reached.
Conclusion
Our analysis of lawsuits against internists revealed that system errors actively contributed to trial losses for medical providers. Physicians' diagnostic errors, night shifts, and physicians' first diagnoses of malignant neoplasm also significantly affected trial outcomes. To our knowledge, this is the first study to show that system failures are more likely to lead to losses in trials than individual physician diagnostic errors. A basic tenet of medical safety is a “no-blame culture” that does not blame individuals alone for their negligence; it is vital to collect accurate information on the causes of errors to enable the early identification of system problems that can be prevented and remedy them quickly.
The author states that he has no Conflict of Interest (COI).
Financial Support
This work was supported by the National Academic Research Grant Funds (JSPS KAKENHI:20H03913). The sponsor of the study had no role in the study design, data collection, analysis, or preparation of the manuscript.
Acknowledgement
The author thanks Shohei Mitsuhashi (practicing attorney and senior medical student) for contributing to the legal interpretations and for creating definitions and classifications; the author also thanks Nobuhiro Nagai, Kaori Kono, and Kazuya Otsuki for collecting the data. The author is grateful to Professor Kazumichi Onigata, Dean of the Faculty of Medicine at Shimane University and Professor Hideyuki Kanda, Okayama University, for their careful supervision of this work. the author is grateful to the team members from the Diagnostic Process Improvement Working Group of the Japanese Society of Internal Medicine and the Diagnostic Error Working Group of the Japanese Society of Hospital General Medicine for sharing their time and knowledge. Finally, the author is grateful to their classmates and supervisors at Harvard Medical School Master of Healthcare Quality and Safety, especially their great mentor Dr. Anjala Tess.
References
- 1.Leape LL. A systems analysis approach to medical error. J Eval Clin Pract 3: 213-222, 1997. [DOI] [PubMed] [Google Scholar]
- 2.Leape LL, Woods DD, Hatlie MJ, et al. Promoting patient safety by preventing medical error. JAMA 280: 1444-1447, 1998. [DOI] [PubMed] [Google Scholar]
- 3.Improving Diagnosis in Health care. Balogh EP, Miller BT, Ball JR, Eds. The National Academies Press, Washington (DC), 2015. [PubMed] [Google Scholar]
- 4.Makary MA, Daniel M. Medical error-the third leading cause of death in the US. BMJ 353: i2139, 2016. [DOI] [PubMed] [Google Scholar]
- 5.Saber Tehrani AS, Lee H, Mathews SC, et al. 25-year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf 22: 672-680, 2013. [DOI] [PubMed] [Google Scholar]
- 6.Bishop TF, Ryan AM, Casalino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA 305: 2427-2431, 2011. [DOI] [PubMed] [Google Scholar]
- 7.Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med 145: 488-496, 2006. [DOI] [PubMed] [Google Scholar]
- 8.Newman-Toker DE, Schaffer AC, Yu-Moe CW, et al. Serious misdiagnosis-related harms in malpractice claims: the ‘big three’ - vascular events, infections, and cancers. Diagnosis Berl 6: 227-40, 2019. [DOI] [PubMed] [Google Scholar]
- 9.Watari T, Tokuda Y, Mitsuhashi S, et al. Factors and impact of physicians' diagnostic errors in malpractice claims in Japan. PLOS ONE 15: e0237145, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lemoine N, Dajer A, Konwinski J, et al. Understanding diagnostic safety in emergency medicine: a case-by-case review of closed ED malpractice claims. J Healthc Risk Manag 38: 48-53, 2018. [DOI] [PubMed] [Google Scholar]
- 11.Rawal RB, Kilpatrick LA, Wood JS, et al. Trends in medical malpractice claims in patients with cleft or craniofacial abnormalities in the United States. Int J Pediatr Otorhinolaryngol 90: 214-219, 2016. [DOI] [PubMed] [Google Scholar]
- 12.Rubin JB, Bishop TF. Characteristics of paid malpractice claims settled in and out of court in the USA: a retrospective analysis. BMJ Open 3: e002985, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Noord I, Eikens MP, Hamersma AM, et al. Application of root cause analysis on malpractice claim files related to diagnostic failures. Qual Saf Health Care 19: e21, 2010. [DOI] [PubMed] [Google Scholar]
- 14.Schaffer AC, Jena AB, Seabury SA, et al. Rates and characteristics of paid malpractice claims among US physicians by specialty, 1992-2014. JAMA Intern Med 177: 710-718, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta A, Snyder A, Kachalia A, et al. Malpractice claims related to diagnostic errors in the hospital. BMJ Qual Saf 27: bmjqs-2017-006774, 2017. [DOI] [PubMed] [Google Scholar]
- 16.Singh H, Meyer AN, Thomas EJ. The frequency of diagnostic errors in outpatient care: estimations from three large observational studies involving US adult populations. BMJ Qual Saf 23: 727-731, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Graber ML, Franklin N, Gordon R. Diagnostic error in internal medicine. Arch Intern Med 165: 1493-1499, 2005. [DOI] [PubMed] [Google Scholar]
- 18.Singh H, Thomas EJ, Petersen LA, et al. Medical errors involving trainees: a study of closed malpractice claims from 5 insurers. Arch Intern Med 167: 2030-2036, 2007. [DOI] [PubMed] [Google Scholar]
- 19.Burns J, Shrader MW, Boan C, et al. Characteristics of medical professional liability claims in pediatric orthopedics. J Patient Saf, 2018. [DOI] [PubMed] [Google Scholar]
- 20.Wang F, Krishnan SK. Medical malpractice claims within cardiology from 2006 to 2015. Am J Cardiol 123: 164-168, 2019. [DOI] [PubMed] [Google Scholar]
- 21.Mangalmurti SS, Harold JG, Parikh PD, et al. Characteristics of medical professional liability claims against internists. JAMA Intern Med 174: 993-995, 2014. [DOI] [PubMed] [Google Scholar]
- 22.Hwang CY, Wu CH, Cheng FC, et al. A 12-year analysis of closed medical malpractice claims of the Taiwan civil court: a retrospective study. Medicine (Baltim) 97: e0237, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brown TW, McCarthy ML, Kelen GD, et al. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med 17: 553-560, 2010. [DOI] [PubMed] [Google Scholar]
- 24.Jena AB, Seabury S, Lakdawalla D, et al. Malpractice risk according to physician specialty. N Engl J Med 365: 629-636, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med 354: 2024-2033, 2006. [DOI] [PubMed] [Google Scholar]
- 26.Quinn GR, Ranum D, Song E, et al. Missed diagnosis of cardiovascular disease in outpatient general medicine: insights from malpractice claims data. Jt Comm J Qual Patient Saf 43: 508-516, 2017. [DOI] [PubMed] [Google Scholar]
- 27.Carroll AE, Buddenbaum JL. Malpractice claims involving pediatricians: epidemiology and etiology. Pediatrics 120: 10-17, 2007. [DOI] [PubMed] [Google Scholar]
- 28.Balla J, Heneghan C, Goyder C, et al. Identifying early warning signs for diagnostic errors in primary care: a qualitative study. BMJ Open 2: 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tokuda Y, Kishida N, Konishi R, et al. Cognitive error as the most frequent contributory factor in cases of medical injury: a study on verdict's judgment among closed claims in Japan. J Hosp Med 6: 109-114, 2011. [DOI] [PubMed] [Google Scholar]
- 30.Sheppard F. ASHRM's commitment to improving diagnosis in health care. J Healthc Risk Manag 37: 5-6, 2018. [DOI] [PubMed] [Google Scholar]
- 31.Mamede S, van Gog T, van den Berge K, et al. Why do doctors make mistakes? A study of the role of salient distracting clinical features. Acad Med 89: 114-120, 2014. [DOI] [PubMed] [Google Scholar]
- 32.Croskerry P, Singhal G, Mamede S. Cognitive debiasing 1: origins of bias and theory of debiasing. BMJ Qual Saf 22(Suppl): ii58-ii64, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]


