Abstract
Introduction
This study connects the aggregate strength of public health policies taken in response to the COVID-19 pandemic in the U.S. states to the governors’ party affiliations and to state-level outcomes. Understanding the relationship between politics and public health measures can better prepare American communities for what to expect from their governments in a future crisis and encourage advocacy for delegating public health decisions to medical professionals.
Methods
The public health Protective Policy Index captures the strength of policy response to COVID-19 at the state level. The authors estimated a Bayesian model that links the rate of disease spread to Protective Policy Index. The model also accounted for the possible state-specific undercounting of cases and controls for state population density, poverty, number of physicians, cardiovascular disease, asthma, smoking, obesity, age, racial composition, and urbanization. A Bayesian linear model with natural splines of time was employed to link the dynamics of Protective Policy Index to governors’ party affiliations.
Results
A 10–percentage point decrease in Protective Policy Index was associated with an 8% increase in the expected number of new cases. Between late March and November 2020 and at the state-specific peaks of the pandemic, the Protective Policy Index in the states with Democratic governors was about 10‒percentage points higher than in the states with Republican governors.
Conclusions
Public health measures were stricter in the Democrat-led states, and stricter public health measures were associated with a slower growth of COVID-19 cases. The apparent politicization of public health measures suggests that public health decision making by health professionals rather than by political incumbents could be beneficial.
INTRODUCTION
In a recent American Journal of Preventive Medicine research brief, Neelon and colleagues1 show a correlation between the partisanship of a governor in U.S. states and the morbidity and mortality during the coronavirus disease 2019 (COVID-19) epidemic. They also conjecture that “the political affiliation of state leaders and specifically governors might best capture the omnibus impact of state policies.”1 Although studies to date show the impact of individual types of mitigation policies2, 3, 4 on health outcomes, they do not speak to their combined effect, nor do they look specifically into the U.S. states.
This study uses the public health Protective Policy Index (PPI)5 , 6 to connect the aggregate strength (stringency) of state-originating public health policies to both the party affiliation of its governor and to the state-level outcomes. Understanding the relationship between politics and public health measures can better prepare American communities for what to expect from their governments in future crises and encourage the medical community to advocate for greater delegation of public health policymaking to health professionals.
METHODS
The PPI is an aggregated measure of public health policy stringency, calculated for each day in each state on the basis of 15 categories of public health measures (Appendix, available online). For each observation, 3 indices are calculated. National PPI aggregates measures adopted by the federal government, according to the stringency in each of the categories. State PPI aggregates measures adopted by the state government. Finally, Total PPI aggregates the highest values from each of the 15 categories when comparing the federal- and state-originating policies.5 , 6 Although normal policymaking includes multiple political and societal actors, this attribution of policy stringency to governors is justified because >88% of all COVID-19 policies in the U.S. states came directly through executive actions rather than from the legislature, bureaucracy, or judiciary.
Estimations used the Total PPI, thus combining state-originated policies with federal-originated policies. Unlike State PPI, Total PPI does not penalize governors for failing to enact policies that would be redundant to federal policies. Although many states duplicated or exceeded federal actions in specific categories, others did not issue their own versions of otherwise available policies.5 The analysis, following Neelon et al.,1 covered mitigation policies between March 1, 2020 and November 30, 2020.
The analysis of the link between governors’ party affiliations and the dynamics of new COVID-19 cases was broken into 2 steps: (1) a study of the link between the policy stringency and the dynamics of new COVID-19 cases and (2) a study of the link between the policy stringency and governors’ party affiliations. The first step employed a Bayesian model that follows the logic of the Susceptible-Infected-Removed model.7 In this model, the expected number of newly infected is proportional to the number of the infectious and the share of the susceptible in the population:
where is the number of new infections in state j in period (t+1), is the estimated number of currently infectious, is the share of those susceptible, and is a coefficient incorporating the density of contacts and transmissibility of the infection. , , and are constructed using the statewide counts of new cases8 and additional parameters for the state-specific rates of potential undercounting of new cases and the rate of removal of the infectious. ) depends linearly on the stringency of current policies:
where is the value of Total PPI with a 3-day lag, and is a state-specific control variable. In the Appendix (available online), 7- and 14-day lags are used in robustness checks. The number of new cases was assumed to follow a negative binomial distribution. The posterior samples for the model parameters were drawn using weakly informative priors and Gibbs sampler.9 , 10 Model details, including the model specification, parameter estimates, the list of control variables, the covariates of the undercounting of new cases, and the data sources, are provided in the Appendix (available online).
To examine the association between the party affiliation of the governor and policy stringency, a Bayesian linear model was estimated, which treated the average PPI as a function of time and the governor's party affiliation. It used natural cubic splines of time and a separate set of coefficients for each state in the analysis. State-specific coefficients had multivariate normal priors with different hyperpriors for the states with Democratic and Republican governors. Gibbs sampler9 , 10 was employed to compute the posterior distribution of state-specific trajectories and the average trajectories of policy stringency in the states with Democratic and Republican governors.
RESULTS
According to the estimates of the first model, the posterior mean of was −0.839, with the central 95% posterior interval between −0.806 and −0.630. Thus, a 10–percentage point decrease in the policy stringency was associated in the model with an 8% increase in the expected number of new cases.
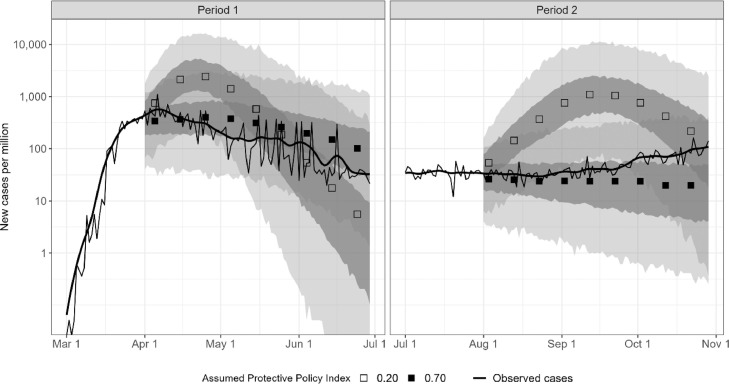
Figure 1 illustrates the estimates. The left panel shows the simulated trajectories of the new cases in New York after April 1 in continuation of the dynamic observed over March 2020. The simulations were conducted under the assumptions that the PPI was fixed at 0.70 and that the PPI was reduced to 0.20. These simulations show that a reduction of the stringency of policies would have delayed reaching the peak in the number of cases until May and lead to an overall higher number of cases. The right panel shows similar simulations conducted for the period starting on August 1, 2020.
Figure 1.
Simulated dynamics of new cases with high and low Protective Policy Index.
Note: Bands represent central 50% and 95% posterior predictive intervals.
Apr, April; Aug, August; Jul, July; Jun, June; Mar, March; Nov, November; Oct, October; Sep, September.
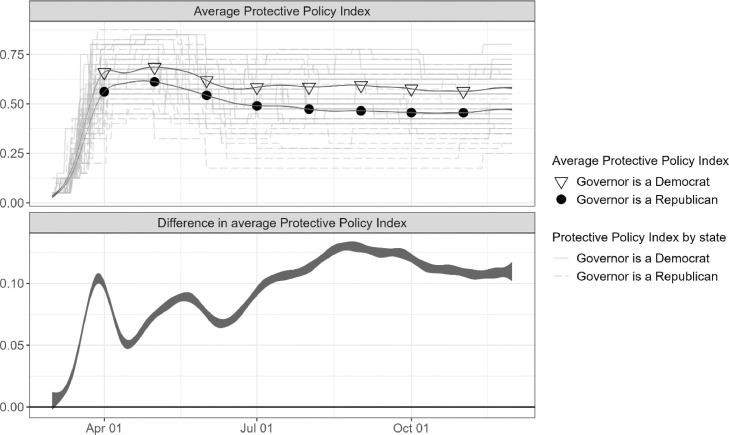
The estimates indicate that on average, the states with Republican governors had weaker public restrictions. Figure 2 plots the estimated dynamics of the averages of Total PPI in the states with Democratic and Republican governors as well as the dynamics of the difference in averages. Between late March and November 2020, the average difference was between 5 and 15 percentage points. That said, there was significant variation within both groups of states, possibly attributable to the differences in the epidemiologic situation and the ideological characteristics of state electorates. Republican governors in more liberal states (Massachusetts, Vermont, and Maryland) pursued a more aggressive COVID-19 policy.
Figure 2.
Dynamics of average Protective Policy Index in states with Democratic and Republican governors.
Note: Bands represent central 50% and 95% posterior intervals.
Apr, April; Jul, July; Oct, October.
DISCUSSION
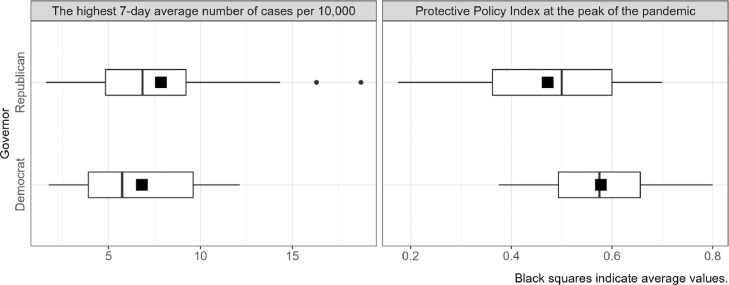
One way to parse out the ideological drivers of the pandemic policymaking from the public health expediency is by assuming that the public health incentives were at their highest (and uniformly high for all states) at the peaks of the pandemic. Figure 3 shows the distributions of new cases (left panel) and policy stringency (right panel) during the state-specific peaks of the pandemic. Although the average number of cases was at least as high in the Republican-led states as in the Democrat-led states, the average PPI was lower by about 10 percentage points.
Figure 3.
Number of new cases and Protective Policy Index at the peaks of the pandemic.
Limitations
The present study quantifies the differences in the average policy stringency between states led by Democratic and Republican governors over the year 2020 and links these differences to the dynamics of COVID-19 cases. As with most analyses of observational data, the causality cannot be inferred, and the estimates should not be interpreted without considering the employed modelling assumptions, including the constant rates of the underreporting of cases within a state, the constant rates of the removal of infected from the pool of the contagious, the absence of re-infections, and not accounting for the spread of infections across state borders.
CONCLUSIONS
This study shows that the public health measures taken in the states with Democratic governors were on average 10‒percentage points stricter over most of 2020. According to the model, these additional 10 percentage points in policy stringency reduced the expected number of COVID-19 cases by about 8%.
These conclusions reinforce and extend the findings of Neelon and colleagues1 that the application of public health policy was politicized. This information further supports the need for delegating public health policymaking to health professionals.
CRediT AUTHOR STATEMENT
Olga Shvetsova: Conceptualization, Data curation, Methodology, Project administration, Supervision, Writing - original draft. Andrei Zhirnov: Conceptualization, Data curation, Formal analysis, Methodology, Software, Visualization, Writing - original draft. Frank Giannelli: Conceptualization, Writing - original draft. Michael Catalano: Investigation, Validation, Writing - review & editing. Olivia Catalano: Investigation, Writing - review & editing.
ACKNOWLEDGMENTS
The authors wish to express thanks for the contributions from Aaron Chan and the members of the COVID-19 Policy Response Lab at Binghamton University (NY). The authors thank Binghamton University; University of Exeter (United Kingdom); and Rutgers University, the State University of New Jersey for providing an effective research environment and solid infrastructure support during this pandemic, which made this project possible. The authors acknowledge that we own any remaining deficiencies here.
No financial disclosures were reported by the authors of this paper
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2021.09.003.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.Neelon B, Mutiso F, Mueller NT, Pearce JL, Benjamin-Neelon SE. Associations between governor political affiliation and COVID-19 cases, deaths, and testing in the U.S. Am J Prev Med. 2021;61(1):115–119. doi: 10.1016/j.amepre.2021.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dehning J, Zierenberg J, Spitzner FP, et al. Inferring change points in the spread of COVID-19 reveals the effectiveness of interventions. Science. 2020;369(6500):eabb9789. doi: 10.1126/science.abb9789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flaxman S, Mishra S, Gandy A, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 4.Hsiang S, Allen D, Annan-Phan S, et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic [published correction appears in Nature. 2020;585(7824):E7] Nature. 2020;584(7820):262–267. doi: 10.1038/s41586-020-2404-8. [DOI] [PubMed] [Google Scholar]
- 5.Adeel AB, Catalano M, Catalano O, et al. COVID-19 policy response and the rise of the sub-national governments. Can Public Policy. 2020;46(4):565–584. doi: 10.3138/cpp.2020-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shvetsova O, Zhirnov A, VanDusky-Allen J, et al. Institutional origins of protective COVID-19 public health policy responses: informational and authority redundancies and policy stringency. J Pol Inst Pol Econ. 2020;1(4):585–613. doi: 10.1561/113.00000023. [DOI] [Google Scholar]
- 7.Hethcote HW. Qualitative analyses of communicable disease models. Math Biosci. 1976;28(3–4):335–356. doi: 10.1016/0025-5564(76)90132-2. [DOI] [Google Scholar]
- 8.United States COVID-19 cases and deaths by state over time. Centers for Disease and Control and Prevention. https://data.cdc.gov/Case-Surveillance/United-States-COVID-19-Cases-and-Deaths-by-State-o/9mfq-cb36. Accessed April 1, 2021.
- 9.Plummer M. JAGS: a program for analysis of Bayesian graphical models using Gibbs sampling. Proceedings of the 3rd International Workshop on Distributed Statistical Computing; Vienna, Austria; 2003 Mar 20–22. Accessed September 30, 2021. [Google Scholar]
- 10.R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/. Accessed April 1, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.