Abstract
Background
In revision total knee arthroplasty (TKA), information regarding perioperative mortality risk is essential for careful decision-making. This study aimed to elucidate the (1) overall 30-day mortality rate and (2) 30-day mortality rate stratified by age, comorbidity, and septic vs aseptic failure after revision TKA.
Methods
The American College of Surgeons National Surgical Quality Improvement Program was reviewed for all patients undergoing revision TKA from 2011 to 2019. A total of 32,354 patients who underwent TKA were identified and categorized as mortality (n = 115) or mortality-free (n = 32,239). Patient characteristics were compared between cohorts and further stratified by septic and aseptic failure.
Results
The overall 30-day mortality rate was 0.36%. The percentage of deaths per age group (normalized per 1000) was 0% (18-29 years), 0% (30-39 years), 0.18% (40-49 years), 0.13% (50-59 years), 0.14% (60-69 years), 0.40% (70-79 years), 1.25% (80-89 years), and 6.93% (90+ years). The percentage of deaths per American Society of Anesthesiologists (ASA) class was 0.30% (ASA 1), 0.06% (ASA 2), 0.39% (ASA 3), 2.41% (ASA 4), and 14.29% (ASA 5). Septic revision (P < .001), general anesthesia (P < .001), body mass index ≤ 24.9 (P < .001), and insulin-dependent diabetes (P = .039) were associated with an increased risk of mortality.
Conclusions
Increasing age, greater comorbidity burden, underweight or normal body mass index, insulin-dependent diabetes, septic revision, and general anesthesia were all associated with an increased risk of mortality after revision TKA. Notably, 1 in 80 patients aged 80-89 years died after revision TKA compared to 1 in 720 patients aged 60-69 years. Patients who underwent septic revision had a 4-fold increase in mortality compared to aseptic revision. Our stratified assessment of mortality provides a more individualized estimation of risk that can be used for patient counseling in revision TKA.
Keywords: Revision total knee arthroplasty, Total knee arthroplasty, Mortality, Risk assessment
Introduction
While the benefits of total knee arthroplasty (TKA) are well-documented [1,2], concerns regarding the threat of complication in the setting of TKA, and to a great degree, revision TKA, remain [3,4]. Increasing lifespan of the general population and higher prevalence of arthroplasty among younger patients has precipitated a greater demand for revision procedures, with a projected increase in revision TKA of 78%-182% over the next 10 years [5,6]. An increase in revision TKAs among patients older than 80 years has also been observed [7]. This growth in revision arthroplasty will contribute to an estimated annual burden of $13 billion by 2030 [8,9]. Previous literature surrounding revision TKA has investigated survivorship [10,11], complications [12,13], and mortality [14], yet these studies have been limited by heterogeneity of procedures and small sample size. Specifically, regarding mortality, former analysis has demonstrated mortality rates up to 18% in the setting of revision TKA [14]. However, updated literature evaluating the risk of mortality after revision TKA, particularly within the first 30 days after surgery, is sparse [12,14].
While previous studies have investigated in-hospital [3,8], midterm [2,15], and long-term [12] mortality after revision TKA, evidence suggests the first 30 postoperative days may be the most critical timeframe to investigate the risk of mortality, as it will be less confounded by deaths from causes unrelated to the index procedure [16]. In addition, revision performed due to septic failure has been reported to increase the risk of mortality 6-fold relative to revision for aseptic failure [12,14]. Still, further investigation is needed to elucidate the current burden of 30-day mortality in this setting.
Therefore, we conducted a retrospective analysis of a nationwide sample to investigate (1) the overall 30-day mortality rate for revision TKA; (2) the 30-day mortality rate for revision TKA as stratified by age, comorbidity, and septic vs aseptic failure; and (3) the distribution of patient demographics, baseline comorbidities, and septic prosthetic joint infection (PJI) among the mortality and mortality-free cohorts.
Material and methods
Study design and data source
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) was retrospectively reviewed for all patients undergoing revision TKA from January 1, 2011, to December 31, 2019. NSQIP is a publicly available, nationally validated, risk-adjusted, outcomes-based program which collects patient demographics, comorbidities, complications, and Current Procedural Terminology codes from the preoperative period to 30 days after surgery [17]. Captured variables include patient demographics, baseline comorbidities, perioperative details, International Classification of Diseases (ICD) codes, health-care utilization parameters (eg, length of stay and discharge disposition), mortality events up to postoperative day 30, and the American Society of Anesthesiologists (ASA) Physical Status Classification System score [18]. The ASA class is a validated measure of medical comorbidities categorized as class I-V in ACS NSQIP, with a higher class predicting increased perioperative risk. A modified Charlson Comorbidity Index (CCI) score [19] was calculated using only the included comorbidity variables which were available in NSQIP from 2011 to 2019. All comorbidity-related variables available in NSQIP were evaluated, but only a subset relating to preoperative conditions was included in our analysis.
Study population
Patients were included if they had undergone a revision TKA as indicated by the following Current Procedural Terminology codes: 27486, 27487, and 27488. A total of 32,354 patients were identified and divided into mortality (n = 115) and mortality-free (N = 32,239) cohorts. Inclusion criteria for the mortality cohort were mortality within 30 days after revision TKA. Exclusion criteria for both cohorts were any patient with a complication improperly coded as 30 days after the revision procedure. Cases with operative times below the first percentile and above the 99th percentile were excluded to remove outliers and incorrectly coded values.
Outcomes of interest
The primary objective of this study was to compare preoperative differences in patients who died within 30 days after revision TKA to those in patients who survived beyond 30 days. These differences were categorized as demographic, comorbidity, and septic or aseptic failure. The frequencies of patient ASA class and modified CCI scores were plotted. The modified CCI score was calculated by assigning one point for each diagnosis of congestive heart failure, chronic obstructive pulmonary disease or dyspnea, and diabetes; two points for dialysis or renal failure; three points for ascites; and six points for disseminated cancer. Age was not included in the modified CCI score, as it was a separate predictor used in the analysis. Septic failure was determined by the presence of PJI using ICD-9 codes (996.66, 711.05) and ICD-10 codes (T84.5xxx – T84.6xxx). In total, 5,846 patients underwent septic revision, and 26,508 underwent aseptic revision.
Statistical analysis
Summary statistics were computed for the cohorts as mean (standard deviation) or number (percentage). Categorical variables were summarized with frequency (%), and differences between the cohorts were analyzed using Pearson’s Chi-square test. Frequency distribution depicts the proportion of age groups and comorbidity indices between the cohorts. For demographic and comorbid variables, patients were further stratified by septic or aseptic revision, and the proportion of mortality per 1000 patients was calculated for each group. P values under 0.05 were considered statistically significant. Statistical analyses were performed using R version 4.0.3 (R Project for Statistical Computing, Vienna, Austria).
Results
A total of 32,354 patients underwent revision TKA between 2011 and 2019. Overall, 115 patients experienced mortality within 30 days after revision TKA (0.36%).
Mortality rates stratified by age, comorbidity, and septic vs aseptic failure
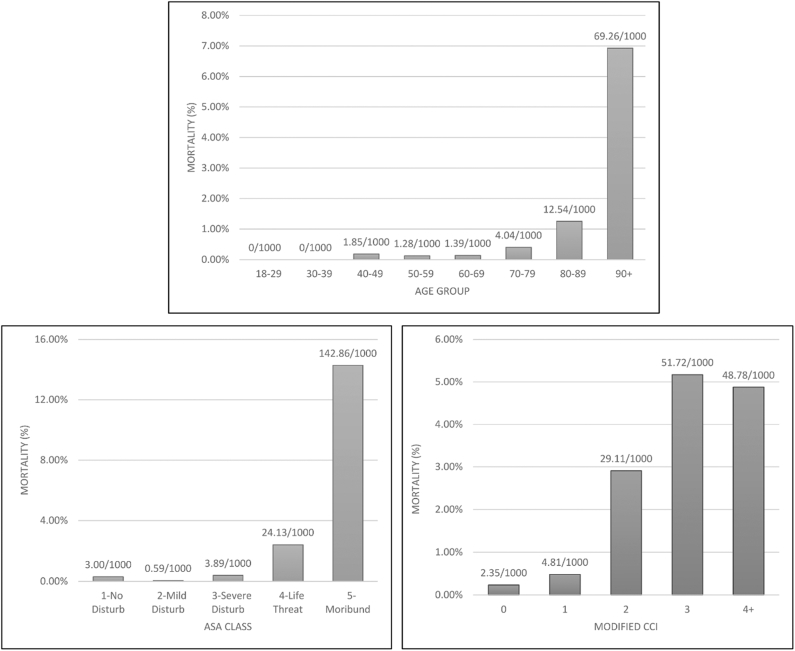
The mean age among patients who died within the first 30 postoperative days (76.3 years) was significantly higher than that among patients who survived beyond 30 days (65.6 years) (P < .001). The distribution of patient age among the mortality and mortality-free cohorts is provided in Table 1. The risk of mortality increased with advancing age, particularly in patients aged 70 years or older (60-69 years: 1.39 deaths per 1000 persons; 70-79 years: 4.04 deaths per 1000 persons; 80-89 years: 12.54 deaths per 1000 persons; 90+ years: 69.26 per 1000 persons; P < .001) (Fig. 1).
Table 1.
The demographic and baseline characteristics of patients who underwent revision TKA in the mortality and mortality-free cohorts.
| Variable | Mortality free | Mortality | P value |
|---|---|---|---|
| Age, mean (SD) | 65.66 (10.61) | 76.32 (11.33) | <.001 |
| Age group | <.001 | ||
| 18-29 | 104 (0.3) | 0 (0.0) | |
| 30-39 | 231 (0.7) | 0 (0.0) | |
| 40-49 | 1626 (5.0) | 3 (2.6) | |
| 50-59 | 7007 (21.7) | 9 (7.8) | |
| 60-69 | 11516 (35.7) | 16 (13.9) | |
| 70-79 | 8654 (26.8) | 35 (30.4) | |
| 80-89 | 2870 (8.9) | 36 (31.3) | |
| 90+ | 231 (0.7) | 16 (13.9) | |
| Sex, male (%) | 13585 (42.1) | 49 (42.6) | .996 |
| Race (%) | .267 | ||
| American Indian or Alaska Native | 200 (0.6) | 0 (0.0) | |
| Asian | 346 (1.1) | 2 (1.7) | |
| Asian or Pacific Islander | 3 (0.0) | 0 (0.0) | |
| Black or African American | 3996 (12.4) | 10 (8.7) | |
| Black, not of Hispanic origin | 1 (0.0) | 0 (0.0) | |
| Hispanic, color unknown | 4 (0.0) | 0 (0.0) | |
| Hispanic, White | 12 (0.0) | 0 (0.0) | |
| Native Hawaiian or Pacific Islander | 120 (0.4) | 2 (1.7) | |
| Unknown/not reported | 3900 (12.1) | 7 (6.1) | |
| White | 23520 (73.0) | 94 (81.7) | |
| White, not of Hispanic origin | 112 (0.3) | 0 (0.0) | |
| BMI | <.001 | ||
| Normal (≤24.9) | 3036 (9.4) | 29 (25.2) | |
| Class I obesity (≤34.9) | 8992 (27.9) | 26 (22.6) | |
| Class II obesity (≤39.9) | 6286 (19.5) | 22 (19.1) | |
| Class III obesity (>39.9) | 5605 (17.4) | 10 (8.7) | |
| Overweight (≤29.9) | 7935 (24.6) | 23 (20.0) | |
| Underweight (<18.5) | 385 (1.2) | 5 (4.3) | |
| Smoking status, yes (%) | 3616 (11.2) | 15 (13.0) | .637 |
| Surgical anesthesia (%) | <.001 | ||
| General | 19566 (60.7) | 100 (87.0) | |
| Spinal | 8221 (25.5) | 12 (10.4) | |
| MAC/IV Sedation | 3402 (10.6) | 3 (2.6) | |
| Regional/Local | 679 (2.1) | 0 (0.0) | |
| Epidural | 314 (1.0) | 0 (0.0) | |
| Unknown | 54 (0.1) | 0 (0.0) | |
| Septic vs aseptic failure | <.001 | ||
| Septic | 5788 (99.01) | 58 (0.99) | |
| Aseptic | 26451 (99.78) | 57 (0.22) |
The bold values are statistically significant P values, which indicate a statistically significant difference between cohorts for the given variable.
Figure 1.
The percentage of deaths within 30 days after revision TKA per age group, ASA class, and modified CCI score.
There was a statistically significant increase in the risk of mortality with an ASA class of 3 or greater (ASA class 3: 3.89 per 1000 persons; ASA class 4: 24.13 per 1000 persons; ASA class 5: 142.86 per 1000 persons; P < .001). Similarly, increasing CCI score was associated with an increased risk of death within 30 days after revision TKA (CCI score 0: 2.35 deaths per 1000 persons; CCI score 3: 51.72 deaths per 1000 persons; P < .001). The proportion of comorbidity scores within the mortality cohort relative to the mortality-free cohort is provided in Table 2.
Table 2.
The distribution of comorbid diagnoses among patients who underwent revision TKA in the mortality and mortality-free cohorts.
| Variable | Mortality free | Mortality | P value |
|---|---|---|---|
| Modified CCI (%) | <.001 | ||
| 0 | 26424 (82.0) | 62 (53.9) | |
| 1 | 4992 (15.5) | 24 (20.9) | |
| 2 | 584 (1.8) | 17 (14.8) | |
| 3 | 116 (0.4) | 6 (5.2) | |
| 4+ | 123 (0.4) | 6 (5.2) | |
| ASA class (%) | <.001 | ||
| 1 | 333 (1.0) | 1 (0.9) | |
| 2 | 11792 (36.6) | 7 (6.1) | |
| 3 | 18738 (58.1) | 73 (63.5) | |
| 4 | 1368 (4.2) | 33 (28.7) | |
| 5 | 7 (0.0) | 1 (0.9) | |
| Diabetes (%) | .039 | ||
| No diabetes | 25231 (78.3) | 83 (72.2) | |
| Oral medication | 139 (0.4) | 0 (0.0) | |
| Insulin dependent | 2305 (7.1) | 16 (13.9) | |
| Non-insulin-dependent | 4564 (14.2) | 16 (13.9) | |
| COPD (%) | 1760 (5.5) | 15 (13.0) | .001 |
| CHF (%) | 272 (0.8) | 10 (8.7) | <.001 |
| Renal failure (%) | 42 (0.1) | 7 (6.1) | <.001 |
| Disseminated cancer (%) | 93 (0.3) | 2 (1.7) | .045 |
| Bleeding disorder (%) | 1439 (4.5) | 26 (22.6) | <.001 |
| Wound infection (%) | 869 (2.7) | 15 (13.0) | <.001 |
CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease.
The bold values are statistically significant P values, which indicate a statistically significant difference between cohorts for the given variable.
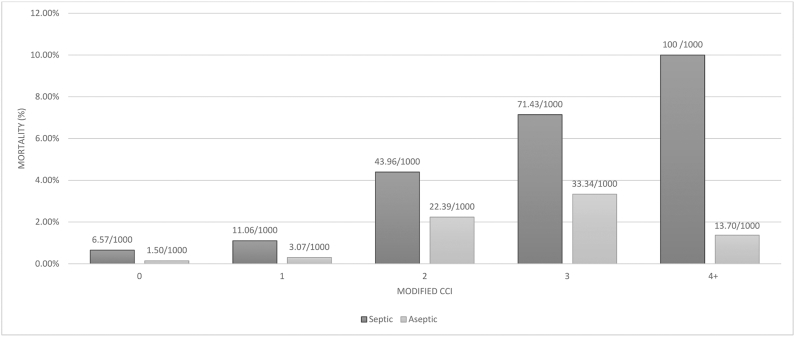
The mortality rate was higher among those who underwent septic revision (0.99%; 58/5,846) relative to those who underwent aseptic revision (0.22%; 57/26,508) (P < .001). Among patients who underwent septic and aseptic revision TKA, both age (Fig. 2) and CCI score (Fig. 3) were associated with a statistically significant increase in mortality risk.
Figure 2.
The distribution of mortality stratified by age group among patients who underwent septic and aseptic revision TKA.
Figure 3.
The distribution of mortality stratified by modified CCI score in patients who underwent septic and aseptic revision TKA.
Distribution of patient demographics and baseline comorbidities
There were no differences in sex, race, or smoking status between the mortality and mortality-free cohorts (Table 1). Patients who were underweight or had a normal BMI were more likely to experience mortality within 30 days after revision TKA than those classified as obese (P < .001). The risk of mortality was also increased among patients who received general anesthesia (P < .001). The mortality cohort had a greater proportion of individuals with comorbid diagnoses, including chronic obstructive pulmonary disease (P = .001), bleeding disorder, wound infection, congestive heart failure, and renal failure (P < .001) (Table 2). Among patients with diabetes, insulin-dependence was associated with a statistically significant increase in risk of mortality relative to non-insulin-dependence and treatment with oral medication (P = .039).
Discussion
Revision TKA represents a major economic burden and use of health-care resources [[20], [21], [22]]. Despite advances in surgical techniques and innovative implant designs, the incidence of revision arthroplasty is only projected to increase over the next decade [5,6]. Previous investigation has indicated that the occurrence of death is relatively rare in the setting of arthroplasty [12,23,24]. Still, evidence surrounding mortality after revision TKA remains scarce. Knowledge of mortality risk in revision TKA is necessary for both patient education and mitigation of its increasing strain on the health-care system [25,26]. Therefore, our study used a nationwide database to assess the overall 30-day mortality rate among 32,354 patients who underwent revision TKA.
The present study found a 30-day mortality rate of 0.36% among patients who underwent revision TKA between 2011 and 2019. This observed rate of mortality after revision TKA is twice as high as that reported in the setting of elective primary TKA (0.18%) [27] within the same timeframe [[27], [28], [29], [30]], emphasizing the need for heightened risk awareness during surgical planning of revision procedures. The mortality rate within the present study is also higher than the risk of death previously reported after revision TKA [29]. Parvizi et al. [29] noted a 30-day mortality rate of 0.24% among 18,165 patients who underwent primary TKA compared to a mortality rate of 0.09% among a cohort of 4,375 patients who underwent revision TKA between 1969 and 1997 (P < .0003). The current study observed a mortality rate that was 4 times greater than the rate reported by Parvizi et al. [29]. This discrepancy in mortality rate is likely attributable to a larger sample size within the present study than the cohort evaluated in the former analysis. In addition, the previous work considered patients who underwent arthroplasty at a single institution. In contrast, our study included patients treated at multiple institutions nationwide. Varying practices and procedures across locations may have further contributed to the observed differences between studies.
There was a significant increase in mortality with advancing age, particularly in patients aged 70 years or older at the time of the revision procedure. Notably, 1 in 80 patients aged 80-89 years died after revision TKA compared to 1 in 720 patients aged 60-69 years. This trend of increasing mortality with advancing age was observed in both aseptic and septic revision. Conflicting with these findings, a previous study conducted by Bovonratwet et al. [7] reported no statistically significant difference in mortality between patients younger than 70 years (n = 1, 0.10%) and patients aged 80 years or older (n = 5, 0.52%) in a matched cohort of 957 revision TKA cases (P = .102) [7]. Bovonratwet et al. also observed no statistically significant difference in mortality risk when comparing patients aged 70-79 years (n = 3, 0.31%) to those 80 years or older (n = 5, 0.52%) (P = .479) [7]. However, similar to our findings, a study conducted by Choi and Bedair [14] reported age greater than 65 years independently increased the risk of mortality within both aseptic and septic revision TKA (odds ratio [OR] 1.13, 95% confidence interval [CI]: 1.05-1.21, P < .001). Additional studies have also implicated advanced age in increased risk of poor clinical outcomes, including the need for higher acuity care [31,32], PJI [8], and in-hospital mortality [3]. The latter findings support those of the present study and highlight the need to consider advanced age in risk stratification for revision TKA.
The present study also demonstrated an increased risk of 30-day mortality with increasing comorbidity burden as indicated by ASA class and CCI score. Previous investigation showed a higher proportion of major comorbidity among patients who underwent revision TKA (13%) relative to patients who underwent primary TKA (5%) in a sample of all primary and revision total hip and knee arthroplasty procedures performed in the United States between 2000 and 2014 [33]. Few studies have investigated the relationship between comorbidity index score and mortality within the setting of revision TKA. Choi and Bedair [14] assessed medium-term mortality among a matched cohort of 88 patients who underwent aseptic and septic revision TKA. Similar to the findings of the present study, Choi and Bedair noted an increased risk of mortality with an ASA score of 3 or greater (OR 6.6, 95% CI: 1.7-25.7, P = .002) [14]. Investigators also reported that a higher CCI score was an independent predictor of mortality in septic revision TKA (OR 1.5, 95% CI: 1.1-2.2, P = .039) [14]. Yao et al. [12] examined long-term mortality among 4,907 patients who underwent revision TKA between 1985 and 2015. Investigators divided the study cohort into groups based on surgical indication (eg, PJI, fracture, instability, loosening, and bearing wear) [12]. Yao et al. observed the greatest mortality among those who underwent revision due to PJI (standardized mortality ratio 1.45, 95% CI: 1.33-1.57, P < .0001) [12]. The PJI group was also noted to have a higher prevalence of major comorbid diseases relative to the remaining groups, including myocardial infarction, cerebrovascular disease, diabetes mellitus, and chronic pulmonary disease [12]. Expanding the base of evidence that currently exists, the present study elucidated the impact of comorbidity on the risk of mortality within the first 30 postoperative days after revision TKA.
Unlike previous studies that have observed worse clinical outcomes with increasing BMI [34,35], the present study demonstrated a greater risk of mortality among patients classified as underweight and those with a normal BMI. Carter et al. [34] reported that 23.4% of patients classified as morbidly obese (BMI > 40) experienced a complication after revision TKA compared to 10.4% of patients with a normal BMI (18.5-25) (P = .011) [34]. Sisko et al. [35] noted a statistically significant increase in risk of reoperation (34.5% vs 16.1%, P = .005) and additional revision (27.6% vs 12.6%, P = .014) among patients with a BMI greater than 40 relative to patients with a BMI less than 40. While previous investigation has implicated obesity in the increased risk of nonfatal complications after revision TKA, these studies have rarely focused on the relationship between BMI and mortality in this setting. The findings presented in the present study suggest that a higher BMI does not contribute to the risk of fatal events within the first 30 days after revision. Instead, patients with an underweight to normal BMI who require revision TKA appear to have an increased risk of death in this setting. Examination of the relationship between BMI and mortality among a large, nationwide database in comparison to previously studied samples among single institutions likely contributed to the observed findings.
Similar to findings in previous literature, the mortality rate in the present study was higher in septic revision (0.99%) relative to aseptic revision (0.22%). The aforementioned work conducted by Choi and Bedair [14] demonstrated that septic revision was an independent predictor of mortality (septic vs aseptic revision, OR 7.7, 95% CI: 2.0-32.1, P < .001) [14]. In a study conducted by Dai et al. [8], investigators observed an in-hospital mortality rate of 0.6% and 0.3% for patients who underwent revision TKA for PJI and those without PJI, respectively [8]. As infection has been shown in up to 58.2% of revision TKA cases [36], understanding the risk of mortality in the face of septic revision has become increasingly important.
To our knowledge, no previous study has investigated the relationship between surgical anesthesia type and mortality after revision TKA. The present study found a higher proportion of mortality events among patients who received general anesthesia. However, the proportion of mortality events was decreased among patients who received spinal anesthesia. These findings agree with evidence from a recent study conducted by Sukhonthamarn et al. [31] which demonstrated an increased risk of requiring higher acuity care in the immediate postoperative setting of lower limb arthroplasty among patients who received general anesthesia relative to those who received spinal anesthesia (OR for spinal vs general 0.62, 95% CI: 0.39-0.98, P = .04) [31]. The findings presented in the present study suggest an association between anesthesia type and mortality, further emphasizing the need to include anesthesia type in risk prediction models for revision arthroplasty. It should be noted that the present study did not separate cases based on level of complexity, and the administration of general anesthesia for longer, more complex cases was a potential source of selection bias.
The present study was strengthened by using a nationwide sample to capture a greater number of revision TKA cases and associated mortality; however, limitations exist. The data provided in the ACS NSQIP database are retrospectively collected and, thus, subject to similar coding errors observed in previous database studies. Still, the ACS NSQIP is an effective tool for assessing 30-day postoperative outcomes [37]. Longer term outcomes, including 90-day and 1-year mortality, are not included in the ACS NSQIP database and, therefore, could not be assessed. Further investigation is needed to elucidate the burden of mortality during these timeframes. Missing variables within the ACS NSQIP presented further limitation, as the variables provided did not fully correspond to those needed for CCI score calculation. However, we used a modified CCI score using methods previously validated by Charlson et al. [19]. This modified index score allowed the burden of comorbidity to be assessed despite missing information within the database. While the present study obtained a large sample size for analysis, the occurrence of mortality within this cohort remained low, thereby making it difficult to conduct further investigation of the causes of mortality within the study population. This study included a variety of revision TKA cases with different levels of complexity (eg, polyethylene exchange, explant and antibiotic spacer placement, revision of femoral and tibial components). The mortality rate among cases of varying complexity may have differed; however, this information was not evaluated. Potential underreporting of mortality within the ACS NSQIP database should also be noted, as mortality events that are unknown to the primary institution would not be included.
Conclusions
Mortality after revision TKA is a rare yet serious adverse event. The projected increased demand and expansion of revision TKA to patients older than 80 years precipitate the need to understand the risk that patients face when undergoing revision arthroplasty. Few updated studies have investigated the current risk of 30-day mortality in the setting of revision TKA. Despite advances in clinical practice, the present study showed that increasing age, greater comorbidity burden, being underweight, insulin-dependent diabetes, septic revision, and general anesthesia were all associated with an increased risk of mortality within 30 days after revision TKA. Findings presented within this study are imperative for both surgeons and patients during surgical decision-making.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field whichmay be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2021.08.019.
Declaration of interests: The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: N.S.P. reports research support from Regenlab and Zimmer, is a paid consultant for Regeneron and Stryker, is in the editorial or governing board of the Journal of Hip Surgery and Journal of Knee Surgery, and is in the board or is a committee member of the American Association of Hip and Knee Surgeons (AAHKS), International Society of Cell and Gene Therapy (ISCT), and Orthopaedic Research Society. The remaining authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this article.
Supplementary data
References
- 1.Bruyère O., Ethgen O., Neuprez A. Health-related quality of life after total knee or hip replacement for osteoarthritis: a 7-year prospective study. Arch Orthop Trauma Surg. 2012;132:1583. doi: 10.1007/s00402-012-1583-7. [DOI] [PubMed] [Google Scholar]
- 2.Choi H.G., Kwon B.C., Kim J Il, Lee J.K. Total knee arthroplasty reduces the risk of mortality in osteoarthritis patients up to 12 years: a Korean national cohort longitudinal follow-up study. J Orthop Surg. 2020;28 doi: 10.1177/2309499020902589. 230949902090258. [DOI] [PubMed] [Google Scholar]
- 3.Samuel L.T., Sultan A.A., Zhou G. In-hospital mortality after septic revision TKA: analysis of the New York and Florida state inpatient databases [e-pub ahead of print] J Knee Surg. 2020 doi: 10.1055/s-0040-1715112. [DOI] [PubMed] [Google Scholar]
- 4.Anis H.K., Warren J.A., Klika A.K. Greater prevalence of mental health conditions in septic revision total knee arthroplasty: a call to action [e-pub ahead of print] J Knee Surg. 2020 doi: 10.1055/s-0040-1713756. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz A.M., Farley K.X., Guild G.N., Bradbury T.L. Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty. 2020;35:S79. doi: 10.1016/j.arth.2020.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel A., Pavlou G., Mújica-Mota R.E., Toms A.D. The epidemiology of revision total knee and hip arthroplasty in England and Wales: a comparative analysis with projections for the United States. A study using the national joint registry dataset. Bone Joint J. 2015;97–B:1076. doi: 10.1302/0301-620X.97B8.35170. [DOI] [PubMed] [Google Scholar]
- 7.Bovonratwet P., Tyagi V., Ottesen T.D., Ondeck N.T., Rubin L.E., Grauer J.N. Revision total knee arthroplasty in octogenarians: an analysis of 957 cases. J Arthroplasty. 2018;33:178. doi: 10.1016/j.arth.2017.07.032. [DOI] [PubMed] [Google Scholar]
- 8.Dai W.-L., Lin Z.-M., Shi Z.-J., Wang J. Outcomes following revision total knee arthroplasty septic versus aseptic failure: a national propensity-score-matched comparison. J Knee Surg. 2020;34(11):1227. doi: 10.1055/s-0040-1702187. [DOI] [PubMed] [Google Scholar]
- 9.Bhandari M., Smith J., Miller L.E., Block J.E. Clinical and economic burden of revision knee arthroplasty. Clin Med Insights Arthritis Musculoskelet Disord. 2012;5:89. doi: 10.4137/CMAMD.S10859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Piuzzi N.S. Patient-reported outcome measures (pain, function, and quality of life) after aseptic revision total knee arthroplasty. J Bone Joint Surg Am. 2020;102:e114. doi: 10.2106/JBJS.19.01155. [DOI] [PubMed] [Google Scholar]
- 11.Passias B.J., Adams J.B., Lombardi A.V., Berend K.R., Crawford D.A. Long-term outcomes of a Modular system in revision total knee arthroplasty. Surg Technol Int. 2020;37:259. [PubMed] [Google Scholar]
- 12.Yao J.J., Hevesi M., O’Byrne M.M., Berry D.J., Lewallen D.G., Maradit Kremers H. Long-term mortality trends after revision total knee arthroplasty. J Arthroplasty. 2019;34:542. doi: 10.1016/j.arth.2018.11.031. [DOI] [PubMed] [Google Scholar]
- 13.Higuera-Rueda C., Emara A.K., Nieves-Malloure Y. The Effectiveness of closed incision negative pressure therapy versus silver-impregnated dressings in mitigating surgical site complications in high-risk patients after revision knee arthroplasty: the PROMISES randomized controlled trial. J Arthroplasty. 2021;36(7S):S295. doi: 10.1016/j.arth.2021.02.076. [DOI] [PubMed] [Google Scholar]
- 14.Choi H.R., Bedair H. Mortality following revision total knee arthroplasty: a matched cohort study of septic versus aseptic revisions. J Arthroplasty. 2014;29:1216. doi: 10.1016/j.arth.2013.11.026. [DOI] [PubMed] [Google Scholar]
- 15.Rajgopal A., Vasdev A., Gupta H., Dahiya V. Revision total knee arthroplasty for septic versus aseptic failure. J Orthop Surg (Hong Kong) 2013;21:285. doi: 10.1177/230949901302100304. [DOI] [PubMed] [Google Scholar]
- 16.Harris I.A., Hatton A., de Steiger R., Lewis P., Graves S. Declining early mortality after hip and knee arthroplasty. ANZ J Surg. 2020;90:119. doi: 10.1111/ans.15529. [DOI] [PubMed] [Google Scholar]
- 17.Ng M., Song S., George J. Associations between seasonal variation and post-operative complications after total hip arthroplasty. Ann Transl Med. 2017;5(Suppl 3):S33. doi: 10.21037/atm.2017.11.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daabiss M. American society of anaesthesiologists physical status classification. Indian J Anaesth. 2011;55:111. doi: 10.4103/0019-5049.79879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Charlson M., Szatrowski T.P., Peterson J., Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 20.Danninger T., Rasul R., Poeran J. Blood transfusions in total hip and knee arthroplasty: an analysis of outcomes. Scientific World Journal. 2014;2014:623460. doi: 10.1155/2014/623460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bessette M.C., Westermann R.W., Davis A. Predictors of pain and function before knee arthroscopy. Orthop J Sport Med. 2019;7(5) doi: 10.1177/2325967119844265. 2325967119844265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bozic K.J., Kamath A.F., Ong K. Comparative epidemiology of revision arthroplasty: Failed THA Poses greater clinical and economic burdens than failed TKA. Clin Orthop Relat Res. 2015;473:2131. doi: 10.1007/s11999-014-4078-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berstock J.R., Beswick A.D., López-López J.A., Whitehouse M.R., Blom A.W. Mortality after total knee arthroplasty: a systematic review of incidence, temporal trends, and risk factors. J Bone Joint Surg Am. 2018;100:1064. doi: 10.2106/JBJS.17.00249. [DOI] [PubMed] [Google Scholar]
- 24.Smith E.J., Maru M., Siegmeth A. Thirty-day mortality after elective hip and knee arthroplasty. Surgeon. 2015;13:5. doi: 10.1016/j.surge.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 25.Cheuy V.A., Foran J.R.H., Paxton R.J., Bade M.J., Zeni J.A., Stevens-Lapsley J.E. Arthrofibrosis associated with total knee arthroplasty. J Arthroplasty. 2017;32:2604. doi: 10.1016/j.arth.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 26.Schairer W.W., Vail T.P., Bozic K.J. What are the rates and causes of hospital readmission after total knee arthroplasty? Knee Clin Orthop Relat Res. 2014;472:181. doi: 10.1007/s11999-013-3030-7. Springer New York LLC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Belmont P.J., Goodman G.P., Waterman B.R., Bader J.O., Schoenfeld A.J. Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am. 2014;96:20. doi: 10.2106/JBJS.M.00018. [DOI] [PubMed] [Google Scholar]
- 28.Seah V.W., Singh G., Ying Yang K. Thirty-day mortality and morbidity after total knee arthroplasty. Ann Acad Med Singap. 2007;36(12):1010. [PubMed] [Google Scholar]
- 29.Parvizi J., Sullivan T.A., Trousdale R.T., Lewallen D.G. Thirty-day mortality after total knee arthroplasty. J Bone Joint Surg Am. 2001;83:1157. doi: 10.2106/00004623-200108000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Belmont P.J., Goodman G.P., Hamilton W., aterman B.R., Bader J.O., Schoenfeld A.J. Morbidity and mortality in the thirty-day period following total hip arthroplasty: risk factors and incidence. J Arthroplasty. 2014;29:2025. doi: 10.1016/j.arth.2014.05.015. [DOI] [PubMed] [Google Scholar]
- 31.Sukhonthamarn K., Grosso M.J., Sherman M.B., Restrepo C., Parvizi J. Risk factors for unplanned admission to the intensive care unit after elective total joint arthroplasty. J Arthroplasty. 2020;35:1937. doi: 10.1016/j.arth.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 32.AbdelSalam H., Restrepo C., Tarity T.D., Sangster W., Parvizi J. Predictors of intensive care unit admission after total joint arthroplasty. J Arthroplasty. 2012;27:720. doi: 10.1016/j.arth.2011.09.027. [DOI] [PubMed] [Google Scholar]
- 33.Sloan M., Sheth N.P. Length of stay and inpatient mortality trends in primary and revision total joint arthroplasty in the United States, 2000–2014. J Orthop. 2018;15:645. doi: 10.1016/j.jor.2018.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carter J., Springer B., Curtin B.M. Early complications of revision total knee arthroplasty in morbidly obese patients. Eur J Orthop Surg Traumatol. 2019;29:1101. doi: 10.1007/s00590-019-02403-9. [DOI] [PubMed] [Google Scholar]
- 35.Sisko Z.W., Vasarhelyi E.M., Somerville L.E., Naudie D.D., MacDonald S.J., McCalden R.W. Morbid obesity in revision total knee arthroplasty: a significant risk factor for re-operation. J Arthroplasty. 2019;34:932. doi: 10.1016/j.arth.2019.01.010. [DOI] [PubMed] [Google Scholar]
- 36.Lee D.-H., Lee S.-H., Song E.-K., Seon J.-K., Lim H.-A., Yang H.-Y. Causes and clinical outcomes of revision total knee arthroplasty. Knee Surg Relat Res. 2017;29:104. doi: 10.5792/ksrr.16.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bilimoria K.Y., Liu Y., Paruch J.L. Surgical risk calculator: a decision aide and informed consent tool for patients and surgeons. J Am Coll Surg. 2013;217(5):833. doi: 10.1016/j.jamcollsurg.2013.07.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.