Abstract
Background
Mental illness among survivors of coronavirus disease 2019 (COVID-2019) during the post-illness period is an emerging and important health issue.
Aims
We aimed to investigate the prevalence of mental illness and the associated factors for its development among COVID-2019 survivors.
Method
From 1 January to 4 June 2020, data were extracted from the National Health Insurance Service COVID-19 database in South Korea. Patients with COVID-19 were defined as those whose test results indicated that they had contracted the infection, regardless of disease severity. COVID-19 survivors were defined as those who recovered from the infection. The primary end-point was the development of mental illness, which was evaluated between 1 January and 1 December 2020.
Results
A total 260 883 individuals were included in this study, and 2.36% (6148) were COVID-19 survivors. The COVID-19 survivors showed higher prevalence of mental illness than the control group (12.0% in the COVID-19 survivors v. 7.7% in the control group; odds ratio (OR) = 2.40, 95% CI 2.21–2.61, P < 0.001). Additionally, compared with the control group, the no specific treatment for COVID-19 group (OR = 2.23, 95% CI 2.03–2.45, P < 0.001) and specific treatment for COVID-19 group (OR = 3.27, 95% CI 2.77–3.87, P < 0.001) showed higher prevalence of mental illness among survivors.
Conclusions
In South Korea, COVID-19 survivors had a higher risk of developing mental illness compared with the rest of the populations. Moreover, this trend was more evident in COVID-19 survivors who experienced specific treatment in the hospital.
Keywords: Anxiety disorders, depressive disorders, epidemiology, post-traumatic stress disorder, risk assessment
Background
On 11 March 2020, the World Health Organization declared the coronavirus disease 2019 (COVID-19) crisis to be a pandemic.1 The worldwide administration of the vaccine began on 8 December 2020.2,3 However, considering the production volume and the speed with which vaccines can be administered, achieving herd immunity may take some time.4 Thus, COVID-19 is still being considered an important global health crisis.
Approximately 2.2% of individuals worldwide who contracted COVID-19 died because of the infection,5 meaning that 97.8% of people who contracted COVID-19 are survivors. This shows that quality of life of the survivors and sequelae have emerged as important public health issues.6 Psychological sequelae has been reported as an important issue in current literature.7–9 In a previous cohort study from the USA, survivors of the diseases who had no previous psychiatric history had a higher risk of developing psychiatric disorders during the 14–90 days follow-up period.10 In South Korea, a high association of psychological sequelae in COVID-19 survivors has been reported in previous studies.8,9 However, to date, studies have only evaluated the total prevalence of mental illness during a short-term follow-up period of 1 month.9,11 Thus, there is an urgent need to evaluate the overall mental illness levels with a longer follow-up period.
Aims
This study investigates the prevalence of mental illness and the associated factors for its development in COVID-19 survivors. It hypothesises that COVID-19 survivors are more likely to develop mental illness compared with other individuals. Moreover, we hypothesised that COVID-19 survivors who experienced specific treatment for the infection in a hospital might have a higher prevalence of mental illness compared with other survivors.
Method
As a population-level cohort study, guidelines from the Strengthening the Reporting of Observational Studies in Epidemiology have been followed.12 The protocol of this study was approved by the Institutional Review Board of the Seoul National University Bundang Hospital; approval number: X-2009-636-902. The National Health Insurance Service (NHIS) sharing service also approved the study protocol and permitted the use of the NHIS COVID-19 database (NHIS-2021-1-070). The need for informed consent was waived because the data in this study were analysed retrospectively in an anonymised form from the NHIS database. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
NHIS COVID-19 database
The NHIS COVID-19 database has been created for purposes of medical research in cooperation with the Korea Disease Control and Prevention Agency (KDCA) and the NHIS. The KDCA provided data for all individuals whose polymerase chain reaction (PCR) test indicated a positive result, confirming that the individual had contracted the infection for the period of 1 January to 4 June 2020. These data included date of confirmation and results of treatment in addition to demographic information. The NHIS extracted the control population through stratification methods based on age, gender and location of their home, using ZIP code as of February 2020. Next, the KDCA provided the data on individuals who received a PCR test, and the result was negative. Therefore, the NHIS COVID-19 database contains data for three groups: a COVID-19-positive group; a control population; and PCR negative-tested individuals.
As the only public health insurance system, the NHIS possesses information regarding all disease diagnoses using ICD-1013 codes and any drug prescription and/or procedure information. The NHIS COVID-19 database was first developed on 26 June 2020, and last updated on 1 December 2020. The NHIS COVID-19 database had no missing data except for the annual income level for some individuals.
Study population
The COVID-19 survivors in this study are defined as individuals who were diagnosed with COVID-19 and then discharged from hospital after treatment. Additionally, individuals who were diagnosed with COVID-19 but were not admitted to hospital because they only had mild or no symptoms are also considered as COVID-19 survivors, if they recovered from the infection. In South Korea, individuals who were diagnosed with COVID-19 were admitted to hospital if they had severe symptoms, such as pneumonia. However, if they had no symptoms or only had mild symptoms, they were isolated with close monitoring in specific government-managed centres.
The other population in the NHIS COVID-19 database has been defined as the control group in this study, which consisted of the control group and PCR test-negative individuals. Among the study population, individuals under the age of 20 were excluded because the prevalence and risk factors for mental illness are different in children and adolescents.14 In addition, individuals who had a previous history of mental illness up until 31 December 2019, were excluded from the analysis to focus on newly developed mental disorders in 2020.
Endpoint: development of mental illness
The primary end-point of this study was the development of mental illness. To define mental illness using ICD-10 codes, the criteria used by Lee et al15 were used. Mental illness includes non-affective psychotic disorders (F20–24 and F28–29), affective psychotic disorders (F25, F30–31, F32.3 and F33.3), anxiety and stress-related disorders (F40–48), alcohol or drug misuse (F10–16 and F18–19), mood disorders without psychotic symptoms (F32–34, F38–39, excluding F32.3, F33.3), eating disorders (F50) and personality disorders (F60–63 and F68–69). The development of mental illness among the study population was determined according to registered ICD-10 codes from 1 January to 1 December 2020. Thus, the diagnosis of mental illness among the study population was determined in the approximately 6-month follow-up time as the data were from 1 January to 4 June 2020. In South Korea, the ICD-10 codes of mental illness must be registered by physicians or psychiatrists in order for patients to receive financial support for the treatment of mental illness.
Confounders
The following information was collected and considered as confounders: demographic variables (gender and age), residence and annual income level in 2020, underlying disability (registered on the NHIS database) and Charlson Comorbidity Index (CCI) score, which was calculated using registered ICD-10 diagnostic codes during the 4 years from 2015 to 2019 (Supplementary Table 1 available at https://doi.org/10.1192/bjo.2021.1001). All individuals were divided into seven groups according to age (20–29, 30–39, 40–49, 50–59, 60–69, 70–79 and ≥80 years), and residence was divided into five areas (Seoul, Gyeonggido, Daegu, Gyeongsangbukdo and other areas). In South Korea, the annual income level of all individuals must be registered in the NHIS database to determine individual insurance premiums, which is divided into quartiles (Q1, Q2, Q3, Q4 and unknown).
Additionally, treatment information for all patients with COVID-19 was collected to reflect severe COVID-19 infection similar to a previous study,16 including supplemental oxygen therapy, mechanical ventilator use, continuous renal replacement therapy, extracorporeal membrane oxygenation use and high-flow oxygen therapy. Thus, if the survivors were given any specific treatment based on the treatment information, they were considered to be a part of a specific treatment group.
Statistical methodology
The clinicoepidemiological characteristics of all individuals in the database are presented as mean values with s.d.s for continuous variables (CCI) and as numbers with percentages for categorical variables (all other variables except for CCI). To compare the characteristics between COVID-19 survivors and the control group, a t-test and chi-square test were used for continuous and categorical variables, respectively. Subsequently, uni- and multivariable logistic regression analyses were performed to examine if COVID-19 survivors were associated with a higher prevalence of development of mental illness in 2020, compared with the control group.
In the multivariable model (model 1 as main analysis), all covariates were included in the adjustment. Additionally, the COVID-19 survivors were divided into two groups (no specific treatment for COVID-19 group and specific treatment for COVID-19) and included in model 2 to examine the impact of treatment experience on the development of mental illness. Second, the duration of isolation because of COVID-19 was included in model 3 as a continuous variable. A multivariable logistic regression model was used to analyse the development of mental illness; this excluded the individuals who died in 2020, as the deaths during this period (evaluation period) could affect the development of mental illness in both the COVID-19 survivor group and the control group.
Next, for the competing risk analyses, mental illness was divided into seven types: non-affective psychotic disorders, affective psychotic disorders, anxiety and stress-related disorders, alcohol or drug misuse, mood disorders without psychotic symptoms, eating disorders and personality disorders. Seven multivariable logistic regression models were constructed using all covariates to examine which form of mental illness was mostly observed in COVID-19 survivors compared with the control group. Finally, subgroup analyses were performed using multivariable models according to gender (male and female), age (20–39, 40–59 and ≥60 years old), and CCI (0–2 and 0–3 groups). All multivariable models confirmed that there was no multicollinearity between the variables with a variance inflation factor of <2.0, and Hosmer–Lemeshow statistics were used to confirm that the goodness of fit of the models was appropriate at P > 0.05. The results of the logistic regression analyses are provided as odds ratios (ORs) with 95% CIs. R software (version 4.0.3; R Foundation for Statistical Computing, Vienna, Austria) was used for all statistical analyses, and a P-value of <0.05 was determined as statistically significant.
Results
Study population
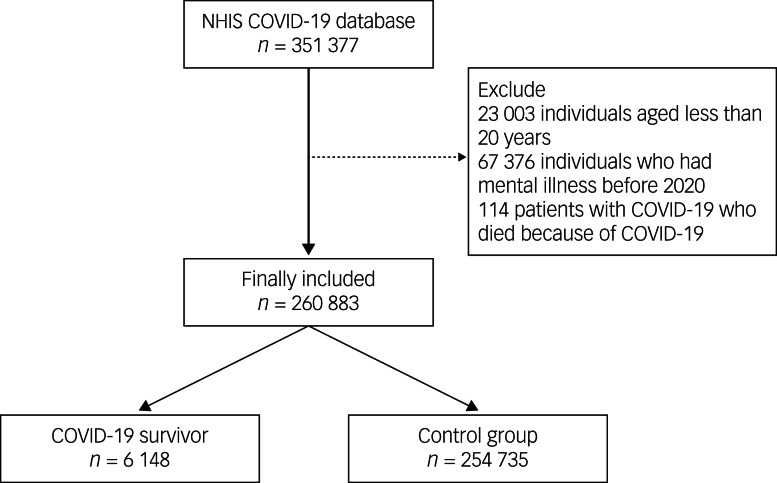
A flow chart depicting the individual selection process in this study is presented in Fig. 1. The NHIS COVID-19 cohort initially included 351 377 individuals. We then excluded from the analysis 23 003 individuals aged less than 20 years, 67 376 individuals who had a mental illness before 2020, and 114 patients with COVID-19 who died from the infection during their hospital admission. Therefore, 260 883 individuals were included in the analysis. Among these, the number of COVID-19 survivors was 6148 (2.36%), and there were 254 735 individuals in the control group. The clinicoepidemiological characteristics of the participants are presented in Supplementary Table 2.
Fig. 1.
Flow chart for the study. COVID-19, coronavirus disease 2019; NHIS, National Health Insurance Service.
Among the total study population, 20 262 (7.8%) participants were diagnosed with mental illness, and anxiety and stress-related disorders were the most common and were observed in 13 736 (5.3%) participants, followed by mood disorders without psychotic symptoms in 8089 (3.1%) participants. The results of the comparison of clinicoepidemiological characteristics between COVID-19 survivors and the control group are presented in Table 1.
Table 1.
Comparison of clinicoepidemiological characteristics between COVID-19 survivor and the control group
| Variable | COVID-19 survivor n = 6148 | Control n = 254 735 | P |
|---|---|---|---|
| Gender male, n (%) | 2414 (39.2) | 137 977 (54.2) | <0.001 |
| Age, n (%) | |||
| 20–29 | 1916 (31.2) | 62 109 (24.4) | <0.001 |
| 30–39 | 748 (12.2) | 44 794 (17.6) | |
| 40–49 | 894 (14.5) | 40 263 (15.8) | |
| 50–59 | 1229 (20.0) | 42 337 (16.6) | |
| 60–69 | 827 (13.5) | 31 875 (12.5) | |
| 70–79 | 369 (6.0) | 19 093 (7.5) | |
| ≥80 | 165 (2.7) | 14 264 (5.6) | |
| Residence, n (%) | |||
| Seoul | 458 (7.4) | 42 646 (16.7) | <0.001 |
| Gyeonggido | 369 (6.0) | 45 719 (17.9) | |
| Daegu | 4001 (65.1) | 79 501 (31.2) | |
| Gyeongsangbukdo | 621 (10.1) | 20 326 (8.0) | |
| Other area | 699 (11.4) | 66 543 (26.1) | |
| Residence, n (%) | |||
| Q1 (lowest) | 1737 (28.3) | 54 415 (21.4) | <0.001 |
| Q2 | 1224 (19.9) | 51 866 (20.4) | |
| Q3 | 1317 (21.4) | 64 048 (25.1) | |
| Q4 | 1770 (28.8) | 79 920 (31.4) | |
| Unknown | 100 (1.6) | 4486 (1.8) | |
| Underlying disability (registered on the NHIS database), n (%) | |||
| Mild to moderate | 177 (2.9) | 10 019 (3.9) | <0.001 |
| Severe | 96 (1.6) | 6432 (2.5) | <0.001 |
| Charlson Comorbidity Index, mean (s.d.) | 2.7 (2.8) | 2.1 (2.2) | <0.001 |
| Comorbid conditions, n (%) | |||
| Myocardial infarction | 119 (1.9) | 6505 (2.6) | 0.002 |
| Congestive heart failure | 259 (4.2) | 19 328 (7.6) | <0.001 |
| Peripheral vascular disease | 755 (12.3) | 38 200 (15.0) | <0.001 |
| Cerebrovascular disease | 460 (7.5) | 256 486 (10.0) | <0.001 |
| Dementia | 211 (3.4) | 10 652 (4.2) | 0.004 |
| Chronic pulmonary disease | 2982 (48.5) | 138 058 (54.2) | <0.001 |
| Rheumatic disease | 485 (7.9) | 22 605 (8.9) | 0.007 |
| Peptic ulcer disease | 2318 (37.7) | 107 902 (42.4) | <0.001 |
| Mild liver disease | 2292 (37.3) | 104 838 (41.16) | <0.001 |
| Diabetes without chronic complication | 1164 (18.9) | 59 722 (23.4) | <0.001 |
| Diabetes with chronic complication | 329 (5.4) | 18 860 (7.4) | <0.001 |
| Hemiplegia or paraplegia | 61 (1.0) | 3313 (1.3) | 0.034 |
| Renal disease | 98 (1.6) | 9444 (3.7) | <0.001 |
| Any malignancy | 402 (6.5) | 31 818 (12.5) | <0.001 |
| Moderate or severe liver disease | 18 (0.3) | 1717 (0.7) | <0.001 |
| Metastatic solid tumour | 48 (0.8) | 6045 (2.4) | <0.001 |
| AIDS/HIV | 7 (0.1) | 421 (0.2) | 0.325 |
| Mental illness development in 2020, n (%) | 738 (12.0) | 19 524 (7.7) | <0.001 |
| Non-affective psychotic disorders | 13 (0.2) | 755 (0.30) | 0.224 |
| Affective psychotic disorders | 69 (1.1) | 2845 (1.1) | 0.968 |
| Anxiety and stress-related disorder | 489 (8.0) | 13 247 (5.2) | <0.001 |
| Alcohol or drug misuse | 14 (0.2) | 665 (0.3) | 0.612 |
| Mood disorders without psychotic symptoms | 343 (5.6) | 7746 (3.0) | <0.001 |
| Eating disorders | 2 (0.0) | 167 (0.1) | 0.315 |
| Personality disorders | 2 (0.0) | 57 (0.0) | 0.601 |
COVID-19, coronavirus disease 2019.
The proportion of men in the COVID-19 survivors was higher (39.2%; 2414/6148) than that in the control group (54.2%; 137 977/254 735) with a P < 0.001. The proportion of ≥80-year-olds and 70- to 79-year-olds in the COVID-19 survivors were lower (2.7% (165/6148) and 6.0% (369/6148), respectively), compared with the control group (5.6% (14 264 of 254 735) and 7.5% (19 093 of 254 735), respectively). The prevalence of mental illness in 2020 was higher in the COVID-19 group (738/6148, 12.0%) than in the control group (19 524/254 735, 7.7%, P < 0.001).
Development of mental illness in 2020
The results of the logistic regression analysis for the development of mental illness in 2020 are presented in Table 2. In model 1, the prevalence of mental illness in the COVID-19 survivors was 2.40-fold higher than that in the control group (OR = 2.40, 95% CI 2.21–2.61, P < 0.001).
Table 2.
Logistic regression analysis for development of mental illness in 2020a
| Variable | Development of mental illness, n (%) | Logistic regression, odds ratio (95% CI) | P |
|---|---|---|---|
| Unadjusted (univariable analysis) | |||
| Control | 19 524/254 735 (7.7) | 1 | |
| COVID-19 survivors | 738/6 148 (12.0) | 1.64 (1.52–1.78) | <0.001 |
| Covariates-adjusted model 1 (multivariable analysis) | |||
| Control | 19 524/254 735 (7.7) | 1 | |
| COVID-19 survivors | 738/6148 (12.0) | 2.40 (2.21–2.61) | <0.001 |
| Covariates-adjusted model 2 (multivariable analysis) | |||
| Control (n = 254 735) | 19 524/254 735 (7.7) | 1 | |
| No specific treatment for COVID-19 (n = 5256) | 526/5256 (10.0) | 2.23 (2.03–2.45) | <0.001 |
| Specific treatment for COVID-19 (n = 892) | 212/892 (23.8) | 3.27 (2.77–3.87) | <0.001 |
| Covariates-adjusted model 3 (multivariable analysis) | |||
| Duration of isolation because of COVID-19, day | – | 1.02 (1.01–1.02) | <0.001 |
COVID-19, coronavirus disease 2019.
Other variables in the multivariable model 1 are presented in Supplementary Table 3.
In model 2, compared with the control group, the no specific treatment for COVID-19 subgroup (n = 5256) and the specific treatment for COVID-19 subgroup (n = 892) had a 2.23-fold (OR = 2.23, 95% CI 2.03–2.45, P < 0.001) and 3.27-fold times (OR = 3.27, 95% CI 2.77–3.87, P < 0.001) higher prevalence of mental illness among survivors, respectively.
In multivariable model 3, a 1-day increase in the duration of isolation (in government centres and/or days spent in hospital) because of COVID-19 was associated with a 2% higher prevalence of mental illness (OR = 1.02, 95% CI 1.01–1.02; P < 0.001). The ORs with 95% CIs for all other variables in the multivariable model 1 are presented in Supplementary Table 3. A similar trend was observed in the sensitivity analysis, excluding 6467 individuals who died in 2020, as shown in Supplementary Table 4.
The results of the logistic regression analysis for the development of mental illness in detail are presented in Table 3. The COVID-19 survivors showed higher prevalence of affective psychotic disorders (OR = 1.44, 95% CI 1.13–1.85, P = 0.003), anxiety and stress-related disorder (OR = 1.72, 95% CI 1.56–1.89, P < 0.001) and mood disorders without psychotic symptoms (OR = 2.15, 95% CI 1.92–2.41, P < 0.001) than the control group.
Table 3.
Multivariable logistic regression analysis for development of mental illness in detail
| Variable | Multivariable model, odds ratio (95% CI) | P |
|---|---|---|
| Non-affective psychotic disorder | ||
| COVID-19 survivors (versus control) | 0.89 (0.52–1.55) | 0.688 |
| Affective psychotic disorders | ||
| COVID-19 survivors (versus control) | 1.44 (1.13–1.85) | 0.003 |
| Anxiety and stress-related disorder | ||
| COVID-19 survivors (versus control) | 1.72 (1.56–1.89) | <0.001 |
| Alcohol or drug misuse | ||
| COVID-19 survivors (versus control) | 0.92 (0.54–1.56) | 0.748 |
| Mood disorders without psychotic symptoms | ||
| COVID-19 survivors (versus control) | 2.15 (1.92–2.41) | <0.001 |
| Eating disorders | ||
| COVID-19 survivors (versus control) | 0.68 (0.17–2.75) | 0.586 |
| Personality disorders | ||
| COVID-19 survivors (versus control) | 1.55 (0.38–6.38) | 0.544 |
COVID-19, coronavirus disease 2019.
The results of the subgroup analyses are shown in Table 4. The ORs for mental illness in the COVID-19 survivors were 1.67 (OR = 1.67, 95% CI 1.45–1.92, P < 0.001) in the male group and 2.06 (OR = 2.06, 95% CI 1.87–2.27, P < 0.001) in the female group. The ORs for mental illness in the COVID-19 survivors were 1.60 (95% CI 1.36–1.89, P < 0.001), 2.27 (95% CI 1.99–2.58, P < 0.001) and 1.86 (OR = 1.86, 95% CI 1.63–2.13, P < 0.001) in the 20–39, 40–59, and ≥60 years groups, respectively. Those individuals with 0–2 and ≥3 points on the CCI showed the same ORs for mental illness of 1.93.
Table 4.
Subgroup analyses
| Variable | Development of mental illness, n (%) | Multivariable model, odds ratio (95% CI) | P |
|---|---|---|---|
| Male (n = 140 391) | |||
| Control | 9656/137 977 (7.0) | 1 | |
| COVID-19 survivors | 265/2414 (11.0) | 1.67 (1.45–1.92) | <0.001 |
| Female (n = 120 492) | |||
| Control | 9868/116 758 (8.5) | 1 | |
| COVID-19 survivors | 473/3734 (12.7) | 2.06 (1.87–2.27) | <0.001 |
| Age: 20–39 (n = 109 567) | |||
| Control | 6948/106 903 (6.5) | 1 | |
| COVID-19 survivors | 213/2664 (8.0) | 1.60 (1.36–1.89) | <0.001 |
| Age: 40–59 (n = 84 723) | |||
| Control | 5782/82 600 (7.0) | 1 | |
| COVID-19 survivors | 301/2123 (14.2) | 2.27 (1.99–2.58) | <0.001 |
| Age: ≥60 (n = 66 593) | |||
| Control | 6794/65 232 (10.4) | 1 | |
| COVID-19 survivors | 224/1361 (16.5) | 1.86 (1.63–2.13) | <0.001 |
| Charlson Comorbidity Index: 0–2 (n = 158 863) | |||
| Control | 11 569/156 343 (7.4) | 1 | |
| COVID-19 survivors | 322/2520 (12.8) | 1.93 (1.72–2.15) | <0.001 |
| Charlson Comorbidity Index: ≥3 (n = 102 020) | |||
| Control | 7955/98 392 (8.1) | 1 | |
| COVID-19 survivors | 416/3628 (11.5) | 1.93 (1.71–2.17) | <0.001 |
COVID-19, coronavirus disease 2019.
Discussion
Main findings
This nationwide cohort study in South Korea established that, compared with the control group, COVID-19 survivors are associated with a 2.40-fold higher prevalence of mental illness, at least during the 6-month follow-up period. Among mental illnesses, a higher prevalence of mood disorders, anxiety and stress-related disorders, and affective psychotic disorders were associated with the survivors. Furthermore, this association was more evident in COVID-19 survivors who experienced specific treatment for the infection in hospitals. The study suggests that newly developed mental illness is a significant issue observed in COVID-19 survivors.
Comparison with findings from other studies
Using the same database (NHIS COVID-19), we recently reported that COVID-19 survivors were at higher risk of psychological sequalae.8 However, the results of the previous study differ from those of the current study in several ways. First, the previous study was based on the database from 1 January to 4 June 2020, whereas the current study used the updated data from 1 January to 1 December 2020. Therefore, we were able to evaluate in the current study the development of mental illness across a longer period of 6 months. Second, different criteria were used for determining the primary end-point. Whereas the previous study focused on the development of depression, psychosis, alcohol misuse and drug misuse, we included more mental illnesses in this study, using the criteria used in the study by Lee et al.15 Therefore, anxiety and stress-related disorders, eating disorders and personality disorders were evaluated as end-points in the current study. Finally, whereas the previous study only included data on COVID-19 survivors and a control population, extracted using stratification methods, the current study included test-negative individuals as well. Thus, we examine a significantly larger sample size compared with the previous study.
In South Korea, the association of mental illness with susceptibility and outcomes of COVID-19 have been sufficiently reported,15,17 but information regarding the new development of mental illness among survivors was lacking. Previous studies suggest that psychological sequelae are an important issue among COVID-19 survivors.7,9–11 In the USA, survivors of COVID-19 have been found to experience psychiatric disorders 14–90 days after a COVID-19 diagnosis, and anxiety disorders, insomnia and dementia were mostly observed.10 In South Korea, the development of psychological sequelae has been recently reported in COVID-19 survivors.9,11 The present study was conducted during a 6-month follow-up of COVID-19 survivors to evaluate psychiatric diagnosis and is different from previous studies that evaluated mental illness during a relatively short period.9–11 Furthermore, unlike previous studies,9–11 the impact of COVID-19 severity on the development of mental illness includes information about treatment received for COVID-19.
In the competing risk analyses, a higher prevalence of mood disorders, anxiety and stress-related disorders, and affective psychotic disorders were observed in COVID-19 survivors. Depression is a major form of mood disorder, and post-traumatic stress disorder (PTSD) and anxiety disorders are major types of anxiety and stress-related disorders. A previous cohort study reported that a high prevalence of psychiatric sequelae such as PTSD, depression and anxiety were observed among 402 COVID-19 survivors at a 1-month follow-up after admission to hospital.18 The prevalence of mental illness among COVID-19 survivors is comparable with psychiatric sequelae for other traumatic experiences. A previous cohort study in Australia reported that 22% of people experienced a new psychiatric disorder after traumatic brain injury.19 Specifically, patients were more likely to develop PTSD, panic disorder, agoraphobia and social phobia significantly at 12 months after traumatic brain injury.19 Compared with the survivors from traumatic brain injury,19 we showed that a higher prevalence of mood disorder was observed in the COVID-19 survivors in our study.
Another previous cohort study in South Korea reported that 42.9% and 27.0% of Middle East Respiratory Syndrome (MERS) survivors reported PTSD and depression, respectively, at 1 year after the MERS outbreak.20 In a multivariable analysis, anxiety and recognition of stigma during the MERS outbreak period were significant risk factors for developing PTSD at 12 months after the MERS outbreak.20 Compared with the MERS survivors,20 the COVID-19 survivors showed a significant increase in the prevalence of psychotic disorders in our study. In 2021, Taquet et al reported that COVID-19 survivors in the USA had a 1.81-fold higher prevalence of mood, anxiety or psychotic disorder compared with those diagnosed with influenza infection at 6-months follow-up.21 Considering the results in our study and those of Taquet et al, the COVID-19 survivors were at a higher risk of developing mental illnesses, which includes mood, anxiety, or psychotic disorders.21
Interpretation of our findings
This study establishes that COVID-19 survivors who did not require any specific treatment for infection were 2.23-fold more likely to have a mental illness than those in the control group. In South Korea, patients with COVID-19 who had mild or no symptoms were isolated with monitoring in government-managed centres until the results of the PCR test were negative. Individual stress could be an important factor leading to this phenomenon. First, the COVID-19 pandemic leads to changes in interpersonal relationships and lifestyles because of prolonged periods of solitude and loneliness. These psychosocial stressful conditions have detrimental effects on fragile individuals and affect their ability to modulate emotions.22,23 Second, the higher prevalence of mental illness among COVID-19 survivors might be caused by social stigma among individuals, as reported in previous studies.24,25 Among survivors in South Korea, social stigma during the MERS outbreak was an independent risk factor for developing PTSD after 12 months.20 Furthermore, a recent study in Germany reported that patients who had COVID-19 were at a higher risk of unemployment because of the social stigma attached to the infection.26 Such unemployment could lead to depression according to a previous epidemiological study.27 Therefore, this study establishes that mental health in COVID-19 survivors is a significant public health issue not only for those who were severely ill but also for patients with mild or no symptoms. However, given that we could not demonstrate the direct impact of emotional stress on mental illness development in those COVID-19 survivors with mild or no symptoms in this study, more research is needed regarding this issue.
Limitations
This study has some limitations. First, the variables body mass index, history of alcohol consumption and smoking were not included in the adjustment as the NHIS database did not include this information. Second, the difference in sample size between the control group and the COVID-19 survivor group is of a large order of magnitude: 254 735 individuals in the control group and 6148 individuals in the COVID-19 survivor group. Third, the multivariable logistic regression is known to adjust only measured confounders, and there might be unmeasured confounders that might affect the results. Fourth, although mental illnesses should be registered in the NHIS database for individuals to receive proper financial support from the government, some data for some patients may be missing because of the lack of accessibility to medical resources among the national population in South Korea. Finally, we included information about patients who required and received specific treatment for their COVID-19 infection and used this to reflect the severity of COVID-19; an accurate measure of the severity of the COVID-19 infection was not considered in this study.
To conclude, during the approximately 6-month follow-up period, COVID-19 survivors were at a higher risk of mental illness compared with the rest of the population of South Korea. Moreover, this association was more evident in COVID-19 survivors who experienced specific treatment for the infection in hospital. To enhance the quality of life of COVID-19 survivors, proper treatment of such mental illnesses should be an important health consideration in future.
Acknowledgements
None.
Funding
This research was supported by a grant of Patient-Centered Clinical Research Coordinating Center (PACEN) and COVID-19 Public Health Research funded by the Ministry of Health & Welfare, Republic of Korea (grant number : HI19C0481, HC20C0013).
Data availability
Data are available upon reasonable request. Anonymised data used in the present study may be available upon reasonable request to the corresponding author.
Author contributions
T.K.O. designed the study, analysed the data, interpreted the data and drafted the manuscript; H.Y.P. and I.-A.S. contributed to the study conceptualisation, acquisition of data and review of manuscript.; S.H.L., M.y.S., H.S.O., K.-H.S., E.-S.Y. and H.Y.P. contributed to data collection, project administration and review of manuscript. All authors have given final approval for the final version of the manuscript.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/bjo.2021.1001.
click here to view supplementary material
Declaration of interest
None
Reference
- 1.Bedford J, Enria D, Giesecke J, Heymann DL, Ihekweazu C, Kobinger G, et al. COVID-19: towards controlling of a pandemic. Lancet 2020; 395: 1015–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, et al. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med 2021; 384: 1412–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knoll MD, Wonodi C. Oxford-AstraZeneca COVID-19 vaccine efficacy. Lancet 2021; 397: 72–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fontanet A, Cauchemez SJNRI. COVID-19 herd immunity: where are we?. Nat Rev Immunol 2020; 20: 583–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). COVID-19 Dashboard. JHU CSSE, 2020. (https://www.arcgis.com/apps/dashboards/bda7594740fd40299423467b48e9ecf6). [Google Scholar]
- 6.Garrigues E, Janvier P, Kherabi Y, Le Bot A, Hamon A, Gouze H, et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Infect 2020; 81: e4–e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moradi Y, Mollazadeh F, Karimi P, Hosseingholipour K, Baghaei R. Psychological disturbances of survivors throughout COVID-19 crisis: a qualitative study. BMC Psychiatry 2020; 20: 594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oh TK, Park HY, Song IA. Risk of psychological sequelae among coronavirus disease-2019 survivors: a nationwide cohort study in South Korea. Depress Anxiety 2021; 38: 247–54. [Google Scholar]
- 9.Park HY, Jung J, Park HY, Lee SH, Kim ES, Kim HB, et al. Psychological consequences of survivors of COVID-19 pneumonia 1 month after discharge. J Korean Med Sci 2020; 35: e409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry 2021; 8: 130–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oh TK, Park HY, Song IAJD. Risk of psychological sequelae among coronavirus disease-2019 survivors: a nationwide cohort study in South Korea. Anxiety 2021; 38: 247–54. [Google Scholar]
- 12.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 2007; 147: 573–7. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision. WHO, 2010. [Google Scholar]
- 14.Park S, Kim BN, Cho SC, Kim JW, Shin MS, Yoo HJ. Prevalence, correlates, and comorbidities of DSM-IV psychiatric disorders in children in Seoul, Korea. Asia Pac J Public Health 2015; 27: NP1942–51. [DOI] [PubMed] [Google Scholar]
- 15.Lee SW, Yang JM, Moon SY, Yoo IK, Ha EK, Kim SY, et al. Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. Lancet Psychiatry 2020; 7: 1025–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shin YH, Shin JI, Moon SY, Jin HY, Kim SY, Yang JM, et al. Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: a nationwide cohort study. Lancet Rheumatol [Epub ahead of print] 18 Jun 2021. Available from: 10.1016/S2665-9913(21)00151-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee SW, Yang JM, Moon SY, Kim N, Ahn YM, Kim JM, et al. Association between mental illness and COVID-19 in South Korea: a post-hoc analysis. Lancet Psychiatry 2021; 8: 271–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mazza MG, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun 2020; 89: 594–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bryant RA, O'Donnell ML, Creamer M, McFarlane AC, Clark CR, Silove D. The psychiatric sequelae of traumatic injury. Am J Psychiatry 2010; 167: 312–20. [DOI] [PubMed] [Google Scholar]
- 20.Park HY, Park WB, Lee SH, Kim JL, Lee JJ, Lee H, et al. Posttraumatic stress disorder and depression of survivors 12 months after the outbreak of Middle East respiratory syndrome in South Korea. BMC Public Health 2020; 20: 605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry 2021; 8: 416–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. Int J Environ Res Public Health 2020; 17: 2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berg-Weger M, Morley J. Loneliness and Social Isolation in Older Adults During the Covid-19 Pandemic: Implications for Gerontological Social Work. Springer, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis 2020; 20: 782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh R, Subedi M. COVID-19 and stigma: social discrimination towards frontline healthcare providers and COVID-19 recovered patients in Nepal. Asian J Psychiatr 2020; 53: 102222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dragano N, Rupprecht CJ, Dortmann O, Scheider M, Wahrendorf MJM. Higher risk of COVID-19 hospitalization for unemployed: an analysis of 1,298,416 health insured individuals in Germany. 2020; 64: 314–21. [DOI] [PMC free article] [PubMed]
- 27.Dooley D, Catalano R, Wilson G. Depression and unemployment: panel findings from the epidemiologic Catchment Area study. Am J Community Psychol 1994; 22: 745–65. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/bjo.2021.1001.
click here to view supplementary material
Data Availability Statement
Data are available upon reasonable request. Anonymised data used in the present study may be available upon reasonable request to the corresponding author.