Abstract
Objective:
To evaluate coronavirus disease 2019 (COVID-19) vaccine hesitancy among healthcare personnel (HCP) with significant clinical exposure to COVID-19 at 2 large, academic hospitals in Philadelphia, Pennsylvania.
Design, setting, and participants:
HCP were surveyed in November–December 2020 about their intention to receive the COVID-19 vaccine.
Methods:
The survey measured the intent among HCP to receive a COVID-19 vaccine, timing of vaccination, and reasons for or against vaccination. Among patient-facing HCP, multivariate regression evaluated the associations between healthcare positions (medical doctor, nurse practitioner or physician assistant, and registered nurse) and vaccine hesitancy (intending to decline, delay, or were unsure about vaccination), adjusting for demographic characteristics, reasons why or why not to receive the vaccine, and prior receipt of routine vaccines.
Results:
Among 5,929 HCP (2,253 medical doctors [MDs] and doctors of osteopathy [DOs], 582 nurse practitioners [NPs], 158 physician assistants [PAs], and 2,936 nurses), a higher proportion of nurses (47.3%) were COVID-vaccine hesitant compared with 30.0% of PAs and NPs and 13.1% of MDs and DOs. The most common reasons for vaccine hesitancy included concerns about side effects, the newness of the vaccines, and lack of vaccine knowledge. Regardless of position, Black HCP were more hesitant than White HCP (odds ratio [OR], ∼5) and females were more hesitant than males (OR, ∼2).
Conclusions:
Although most clinical HCP intended to receive a COVID-19 vaccine, intention varied by healthcare position. Consistent with other studies, hesitancy was also significantly associated with race or ethnicity across all positions. These results highlight the importance of understanding and effectively addressing reasons for hesitancy, especially among frontline HCP who are at increased risk of COVID exposure and play a critical role in recommending vaccines to patients.
The coronavirus disease 2019 (COVID-19) pandemic has resulted in significant morbidity and mortality with >38 million cases and >629,000 deaths in the United States as of August 25, 2021.1 As disease transmission persists and vaccination coverage begins to plateau, the need for COVID-19 vaccination becomes even more imperative to reduce COVID-19 cases and reach herd immunity.
Three COVID-19 vaccines are currently authorized for emergency use in the United States.2 As of August 25, 2021, the Centers for Disease Control and Prevention (CDC) reported that 60.5% of the US population aged ≥12 years are fully vaccinated.3 As of March 19, 2021, a survey of frontline healthcare personnel (HCP) reported that 52% had received ≥1 dose of the vaccine.4 As frontline workers, HCP in the United States were among the first group to be offered vaccination. This opportunity allowed HCP to obtain early protection as well as become advocates for vaccination and encourage their patients and family members to be vaccinated once vaccines became available.5 Patients consistently rank HCP as one of their most trusted sources for vaccine information, and a provider recommendation is strongly associated with vaccine receipt.5 Thus, all HCP, regardless of their position, play a critical role in advocating for vaccination. However, it is unclear whether HCP are recommending COVID-19 vaccine, particularly if they have not made the decision to be vaccinated themselves.5,6 According to a March 2021 publication, nearly one-third of US HCP were hesitant about vaccination.7 In a survey of 1,327 HCP conducted from February 11 to March 7, 2021, 48% had not received a vaccine.4
In this study, we sought to better understand associations between specific healthcare positions and COVID-19 vaccine hesitancy and identify factors associated with intent to be vaccinated. We evaluated vaccine hesitancy among several groups of HCP who provide direct patient care.
Methods
A cross-sectional online survey was conducted from November 13 to December 6, 2020, among HCP at 2 large hospitals in Philadelphia. Details regarding methods and results of the survey have been previously published.8
The survey collected information on intentions to receive a COVID-19 vaccine and how soon the HCP intended to be vaccinated. Possible responses for intention to be vaccinated included yes, no, unsure, or previously participated in a COVID-19 trial. Possible responses for timing of vaccination included do not plan to receive a vaccine, as soon as a vaccine is available, or 3, 6, or 12 months later. Other data collected included the reasons respondents were or were not interested in vaccination, role in the hospital, COVID-19 exposure risk (including area of employment, confirmed COVID-19 exposures, and previous COVID-19 tests), and demographic characteristics. High risk of exposure to COVID-19 was defined as working in a COVID-19 unit, the emergency room, or the intensive care unit. We focused on 3 groups with clinical positions associated with direct patient care: (1) medical doctors (MDs) and doctors of osteopathy (DOs), (2) nurse practitioners (NPs) and physician assistants (PAs), and (3) nurses. The primary outcome was COVID-19 vaccine hesitancy, defined as either delaying a vaccine by 3, 6, or 12 months, being unsure about receiving the vaccine, or having no plans to be vaccinated. Our definition of hesitancy was similar to that of the World Health Organization (WHO).9 Hesitancy among HCP is particularly important because of their potential exposure to vaccine-preventable diseases on a daily basis.
Demographic characteristics for the 3 groups of HCP were summarized using frequencies and percentages and compared using χ2 tests with a significance level of 0.05. We compared vaccine hesitancy rates across each HCP group and measured associations with demographic characteristics, health status, and number of previous known COVID-19 exposures and vaccine hesitancy using bivariate regression analysis. Variables associated with significant differences in vaccine hesitancy were subsequently included in a multivariate logistic regression model. We stratified the multivariable analysis by the 3 HCP groups to determine whether factors associated with hesitancy differed within each group. Significance level 0.05 was used in all models.
The institutional review board at each hospital reviewed the protocol and determined that the study was exempt from human-subject review.
Results
Demographic characteristics of the study population
Of the 34,865 HCPs surveyed, 12,034 completed the survey (34.5% response rate) including 5,929 clinical-facing HCP: 2,253 (38.0%) MDs and DOs, 740 (12.5%) NPs and PAs, and 2,936 (49.5%) nurses. Demographic characteristics of the 3 groups are presented in Table 1. Sex distribution was significantly different (P < .0001) across groups. Nurses and NPs and PAs were mainly female (91.4% and 92.2%, respectively), whereas MDs and DOs were more evenly distributed (53.7% female). Most respondents in each group were White: MDs and DOs (71.5%), PAs and NPs (85.7%), and nurses (83.7%). Fewer respondents were Black (2.9%, 2.4%, and 3.9%, respectively), Hispanic or Latino (2.8%, 1.2%, and 1.6%, respectively), or Asian (14.7%, 5.5%, and 3.9%, respectively). Most MDs and DOs lived in an urban area (52.3%), and NPs and PAs and nurses lived primarily in suburban areas (58.6% and 62.5%, respectively). Most individuals had been employed for ≥5 years in their positions: MDs and DOs (59.1%), NPs and PAs (68.9%), and nurses (61.0%).
Table 1.
Demographics of the Survey Population by HCP Job Category: Physicians (MDs and DOs), Nurse Practitioners (NPs) and Physician Assistants (PAs), and Nurses
| Variable | MDs and DOs, No. (%) |
NPs and PAs, No. (%) |
Nurses, No. (%) |
Combined, No. (%) |
|---|---|---|---|---|
| Age | ||||
| <40 y | 1,072 (47.6) | 424 (57.3) | 1,901 (64.8) | 3,397 (57.3) |
| 40–64 y | 979 (43.8) | 294 (39.7) | 963 (32.8) | 2,236 (37.7) |
| ≥65 y | 196 (8.8) | 21 (2.8) | 44 (1.5) | 261 (4.4) |
| Prefer not to answer | 1 (0.2) | 1 (0.1) | 26 (0.9) | 32 (0.5) |
| Sex | ||||
| Male | 1,021 (45.4) | 51 (6.9) | 204 (7.0) | 1,276 (21.5) |
| Female | 1,208 (53.7) | 681 (92.2) | 2,682 (91.4) | 4,571 (77.2) |
| Other/Prefer not to answer | 21 (0.9) | 7 (0.9) | 49 (1.7) | 77 (1.3) |
| Race/Ethnicity | ||||
| White | 1,611 (71.5) | 634 (85.7) | 2,457 (83.7) | 4,702 (79.3) |
| Black | 66 (2.9) | 18 (2.4) | 114 (3.9) | 198 (3.3) |
| Hispanic or Latino | 64 (2.8) | 9 (1.2) | 48 (1.6) | 121 (2.0) |
| Asian | 331 (14.7) | 41 (5.5) | 115 (3.9) | 487 (8.2) |
| Multiple/Other | 106 (4.7) | 23 (3.1) | 78 (2.7) | 207 (3.5) |
| Education | ||||
| Less than Bachelor’s degree | 0 (0.0) | 1 (0.1) | 133 (4.5) | 134 (2.3) |
| Bachelor’s or Master’s degree | 22 (1.0)a | 659 (89.1) | 2,770 (94.4) | 3,451 (58.2) |
| Postgraduate degree | 2,230 (99.0) | 80 (10.8) | 33 (1.1) | 2,343 (39.5) |
| Area of residence | ||||
| Urban | 1,177 (52.3) | 296 (40.0) | 1,028 (35.0) | 2,501 (42.2) |
| Suburban | 1,067 (47.4) | 434 (58.6) | 1,834 (62.5) | 3,335 (56.3) |
| Rural | 8 (0.4) | 10 (1.4) | 74 (2.5) | 92 (1.6) |
| Years employed at hospital | ||||
| <1 y | 241 (10.7) | 45 (6.1) | 177 (6.0) | 463 (7.8) |
| 1–4 y | 680 (30.2) | 185 (25.0) | 966 (32.9) | 1,831 (30.9) |
| ≥5 y | 1,330 (59.1) | 509 (68.9) | 1,790 (61.0) | 3,629 (61.3) |
Note. MD, medical doctor; DO, doctor of osteopathy. All information was self-reported on the survey except for hospital of employment.
The education status of 22 respondents who reported themselves to be an MD or DO may be misclassified.
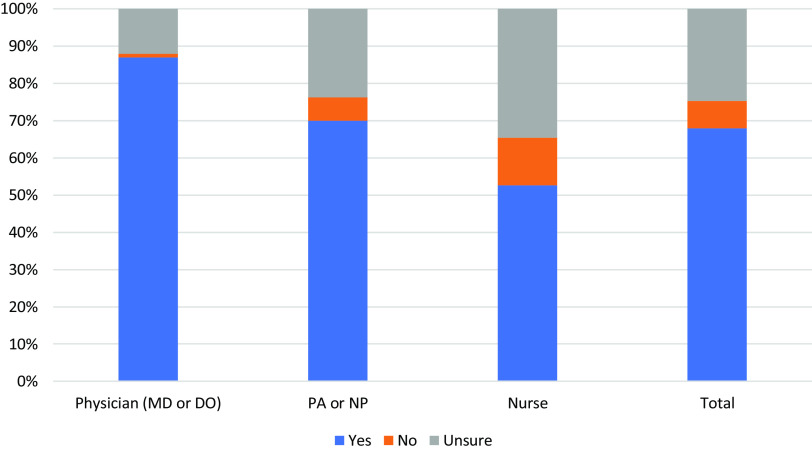
COVID-19 vaccine hesitancy by job category
Vaccine hesitancy by HCP job category is shown in Figure 1. Overall, 4,021 (67.8%) HCP planned to receive the COVID-19 vaccine; 78.5% intended to get the vaccine as soon as possible with the highest rate among MDs and DOs (86.9%). A higher proportion of nurses reported that they would refuse (12.7%) or were unsure (34.7%) of receiving vaccine compared with MDs and DOs (1.0%, 12.1%, respectively) or PAs/NPs (6.2%, 23.8%, respectively).
Fig. 1.
Intention to receive a COVID-19 vaccine by HCP job category (physicians [MDs and DOs], nurse practitioners [NPs]/physician assistants [PAs], and nurses). Intention to receive a COVID-19 vaccine is defined as yes, no, or unsure.
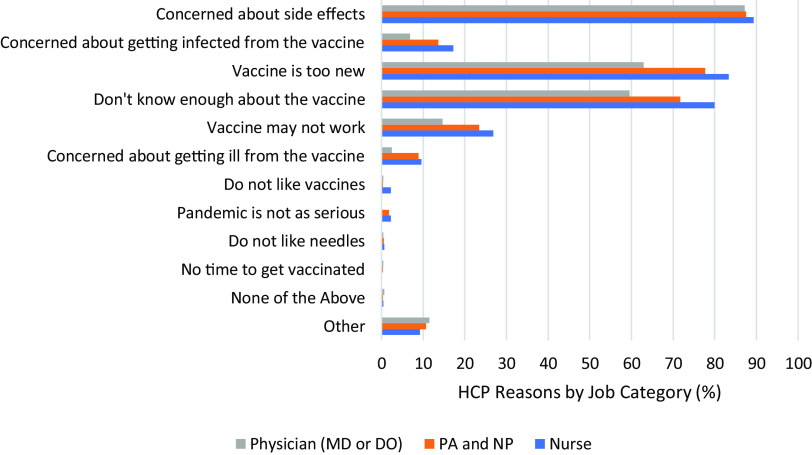
Reasons for not planning to be vaccinated as soon as vaccine available
Figure 2 shows the reasons for not planning to be vaccinated among those who were vaccine hesitant. Side effects of the vaccine were the primary concern (<87.0%) across all hesitant individuals. Among the 31.3% who reported that they would delay the vaccine, side effects were also the primary concern (85%). Nurses were more concerned about the newness of the vaccine than MDs and DOs or PAs and NPs (83.4%, 77.7%, and 62.9%, respectively) and not knowing enough about the vaccine (80.0%, 71.7%, and 59.5%, respectively). The most common concern listed as “other” was taking the vaccine during pregnancy or when trying to become pregnant (2.9% of hesitant nurses).
Fig. 2.
Reasons for not planning to receive a COVID-19 vaccine as soon as available among those who were vaccine hesitant by HCP job category: physicians (MDs and DOs), nurse practitioners (NPs) and /physician assistants (PAs), and nurses (N = 2,776 respondents). Participants could choose >1 reason. Limited to respondents who were classified as vaccine hesitant. The “other” category includes responses such as concerns about taking the vaccine while pregnant, breastfeeding or planning to get pregnant, concerns about vaccine safety, the speed of vaccine development, lack of trust in pharmaceutical companies, and political concerns about the vaccine. All information was self-reported on the survey except for hospital of employment.
Factors associated with vaccine hesitancy
In the bivariate analysis, we examined vaccine hesitancy by demographic and HCP characteristics across the 3 groups combined. Several variables were significant (Table 2). Individuals <40 years old were more likely to be vaccine hesitant than those aged 40–64 or ≥65 years (51.1%, 42.7%, and 21.8%, respectively). Vaccine hesitancy was much higher among females (53.2%) than males (22.3%). Vaccine hesitancy was highest amongst Black HCP (75.3%) followed by 51.2% among Hispanic/Latino HCP, 44.8% among White HCP, and 44.2% among Asian HCP. Those with less than a bachelor’s degree were most likely to be vaccine hesitant (66.4%) compared to only 27.4% of those with a postgraduate degree. Hesitancy was highest for those who resided in rural areas (66.3%). Hesitancy varied by years of employment: 41%, 50.3%, and 45.9 for those working <1 year, 1–4 years, and ≥5 years, respectively. Those who reported being in excellent health were less hesitant (38.1%) than those reporting good/very good health (51.8%) or fair or poor health (52.9%). Those without prior COVID-19 exposures were most hesitant (50.5%); HCP reporting a prior SARS-CoV-2 test were less likely to be vaccine hesitant (41.6%). Risk of exposure at work and prior routine vaccination history were not significantly associated with vaccine hesitancy.
Table 2.
Characteristics of HCP Who Were Hesitanta About Receiving a COVID-19 Vaccine
| Parameter | Total Respondents | Vaccine Hesitant, No. (%) |
P Value |
|---|---|---|---|
| Demographics | |||
| Age | |||
| <40 y | 3,397 | 1,736 (51.1) | <.0001 |
| 40–64 y | 2,236 | 954 (42.8) | |
| ≥65 y | 261 | 57 (21.8) | |
| Sex | |||
| Male | 1,276 | 285 (22.3) | <.0001 |
| Female | 4,571 | 2,432 (53.2) | |
| Other/Prefer not to answer | 77 | 56 (72.7) | |
| Race/Ethnicity | |||
| White | 4,702 | 2,107 (44.8) | <.0001 |
| Black | 198 | 149 (75.3) | |
| Hispanic or Latino | 121 | 62 (51.2) | |
| Asian | 487 | 215 (44.2) | |
| Multiple/Other | 207 | 95 (45.9) | |
| Education | |||
| Less than Bachelor’s degree | 134 | 89 (66.4) | <.0001 |
| Bachelor’s or Master’s degree | 3,451 | 2,045 (59.3) | |
| Postgraduate degree | 2,343 | 642 (27.4) | |
| Area of residence | |||
| Urban | 2,501 | 1,063 (42.5) | <.0001 |
| Suburban | 3,335 | 1,651 (49.5) | |
| Rural | 92 | 61 (66.3) | |
| Work location | |||
| Hospital A | 2,956 | 1,500 (50.7) | <.0001 |
| Hospital B | 2,973 | 1,276 (42.9) | |
| Years employed at hospital | |||
| <1 y | 463 | 190 (41.0) | .0006 |
| 1–4 y | 1,831 | 916 (50.0) | |
| ≥5 y | 3,629 | 1,667 (45.9) | |
| Health of individual | |||
| Self-reported health status | |||
| Excellent | 2,163 | 823 (38.1) | <.0001 |
| Good or very good | 3,662 | 1,898 (51.8) | |
| Fair or poor | 104 | 55 (52.9) | |
| Vaccination history | |||
| Employee | |||
| Up-to-date on most or all vaccines | 5,845 | 2,730 (46.7) | .3813 |
| Up-to-date on some vaccines | 53 | 27 (50.9) | |
| Unsure if up-to-date | 12 | 7 (58.3) | |
| Not up-to-date | 19 | 12 (63.2) | |
| Employee’s children | |||
| Up-to-date on most or all vaccines | 3,263 | 1,447 (44.4) | .0767 |
| Up-to-date on some vaccines | 50 | 25 (50.0) | |
| Unsure if up-to-date | 27 | 10 (37.0) | |
| Not up-to-date | 18 | 13 (72.2) | |
| COVID-19 exposures & testing | |||
| Area of employment in the hospital | |||
| High exposure to COVID-19 | 2,249 | 1,019 (45.3) | .3851 |
| Moderate exposure to COVID-19 | 3,148 | 1,464 (46.5) | |
| Low exposure to COVID-19 | 211 | 105 (49.8) | |
| Confirmed COVID-19 exposures at work, home, elsewhere | |||
| 0 | 1,385 | 700 (50.5) | .0001 |
| 1–4 | 1,814 | 855 (47.1) | |
| ≥5 | 1,954 | 845 (43.2) | |
| Previous COVID-19 test | |||
| Yes | 2,534 | 1,053 (41.6) | <.0001 |
| No | 3,315 | 1,669 (50.4) | |
| Unsure | 80 | 54 (67.5) | |
Note. HCP, healthcare personnel including physicians (MDs and DOs), nurse practitioners and physician assistants and nurses; MD, medical doctor; DO, doctor of osteopathy. All information was self-reported on the survey except for hospital of employment.
Hesitant individuals included those unsure, planning to delay vaccination, or not planning to be vaccinated.
Multivariate logistic analysis
Table 3 presents the results of the multivariate logistic analysis of vaccine hesitancy stratified by HCP group. Based upon results from bivariate analyses, covariates included age, race/ethnicity, gender, area of residence, health status, COVID-19 exposures, and prior receipt of SARS-CoV-2 tests.
Table 3.
Multiple Logistic Regression Assessing Intention to Receive a COVID-19 Vaccinea Stratified by HCP Job Category: Physicians (MDs and DOs), Nurse Practitioners (NPs) and Physician Assistants (PAs), and Nurses
| Variable | Nurses (N = 2409) |
NPs and PAs (N = 617) |
MDs and DOs (N = 1935) |
|||
|---|---|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Demographics | ||||||
| Age | .0042 | .6528 | .0121 | |||
| <40 y | Reference | Reference | Reference | |||
| 40–64 y | 0.71 (0.58–0.87) | 0.83 (0.57–1.23) | 0.74 (0.56–0.98) | |||
| ≥65 y | 0.73 (0.34–1.49) | 0.92 (0.32–2.63) | 0.48 (0.28–0.81) | |||
| Sex | <.0001 | .3143 | <.0001 | |||
| Male | Reference | Reference | Reference | |||
| Female | 2.58 (1.82–3.66) | 1.72 (0.86–3.46) | 2.12 (1.69–2.65) | |||
| Other/Prefer not to answer | 3.05 (0.68–13.63) | … | 1.18 (0.22–6.41) | |||
| Race/Ethnicity | <.0001 | .1267 | <.0001 | |||
| White | Reference | Reference | Reference | |||
| Black | 5.13 (2.87–9.16) | 5.04 (1.34–18.99) | 4.18 (2.43–7.18) | |||
| Hispanic or Latino | 3.77 (1.54–9.23) | 2.27 (0.52–9.85) | 0.81 (0.42–1.58) | |||
| Asian | 1.63 (1.04–2.57) | 1.15 (0.57–2.34) | 1.64 (1.25–2.16) | |||
| Multiple/Other | 1.37 (0.81–2.32) | 1.29 (0.53–3.14) | 1.24 (0.78–1.98) | |||
| Area of residence | .0002 | .4977 | .0799 | |||
| Urban | Reference | Reference | Reference | |||
| Suburban | 1.45 (1.20–1.76) | 1.25 (0.86–1.82) | 1.02 (0.80–1.30) | |||
| Rural | 2.16 (1.21–3.87) | 1.23 (0.31–4.91) | 8.68 (1.32–57.18) | |||
| Years employed at hospital | .0285 | .8033 | .2103 | |||
| <1 y | Reference | Reference | Reference | |||
| 1-4 y | 1.19 (0.82–1.72) | 0.99 (0.47–2.09) | 1.17 (0.80–1.72) | |||
| ≥5 y | 0.90 (0.62–1.29) | 1.14 (0.55–2.35) | 1.40 (0.94–2.08) | |||
| Health of individual | ||||||
| Self-reported health status | .0685 | .8913 | .4464 | |||
| Excellent | Reference | Reference | Reference | |||
| Good or very good | 1.26 (1.03–1.54) | 1.04 (0.74–1.45) | 1.11 (0.90–1.38) | |||
| Fair or poor | 1.08 (0.60–1.96) | 0.72 (0.15–3.54) | 1.65 (0.55–4.91) | |||
| COVID-19 exposures & testing | ||||||
| Confirmed COVID-19 exposures at work, home, elsewhere | .6904 | .3028 | .0029 | |||
| 0 | Reference | Reference | Reference | |||
| 1–4 | 0.93 (0.75–1.15) | 0.90 (0.60–1.34) | 0.90 (0.68–1.18) | |||
| ≥5 | 1.01 (0.81–1.26) | 1.23 (0.80–1.87) | 0.65 (0.49–0.85) | |||
| Previous COVID-19 test | .0007 | .0520 | .7475 | |||
| Yes | Reference | Reference | Reference | |||
| No | 1.36 (1.14–1.62) | 1.54 (1.09–2.17) | 1.07 (0.86–1.32) | |||
| Unsure | 2.19 (1.10–4.38) | 1.52 (0.30–7.81) | 1.39 (0.39–4.94) | |||
Note. MD, medical doctor; DO, doctor of osteopathy; OR, odds ratio; CI, confidence interval. The regression analysis was performed on 5,929 individuals who answered the question about their intention to be vaccinated by job category as well as all included variables. Parameters with a significant odds ratio compared to the reference are in bold. All information was self-reported on the survey except for hospital of employment.
Analysis compared vaccine hesitant individuals (those unsure, planning to delay vaccination or not planning to be vaccinated) versus those who were not vaccine hesitant (planning to be vaccinated immediately).
Nurses
Female nurses were significantly more likely to be hesitant than male nurses (odds ratio [OR], 2.58; 95% confidence interval [CI], 1.82–3.66), whereas Black (OR, 5.13; 95% CI, 2.87–9.16), Hispanic or Latino (OR, 3.77; 95% CI, 1.54–9.23), and Asian (OR, 1.63; 95% CI, 1.04–2.57) nurses were significantly more likely to be hesitant than White nurses. Nurses living in suburban or rural areas were more likely to be vaccine hesitant than those in urban areas (OR, 1.45; 95% CI, 1.20–1.76 and OR, 2.16; 95% CI, 1.21–3.87). Nurses who reported being in good or very good health were more likely to be vaccine hesitant than nurses in excellent health (OR, 1.26; 95% CI, 1.03–1.54). Nurses who reported that they did not receive a COVID-19 test or were unsure of previous testing were more hesitant than those who reported having been previously tested (OR, 1.36; 95% CI, 1.14–1.62 and OR, 2.19; 95% CI, 1.10–4.38).
NPs and PAs
Few variables were significantly associated with vaccine hesitancy among NPs and PAs, most likely due to the small number of NPs and PAs surveyed. Similar to nurses, Black NPs and PAs were more hesitant than White NPs and PAs (OR, 5.04; 95% CI, 1.34–18.99). NPs and PAs who had not received a previous SARS-CoV-2 test were more likely to be hesitant than those previously tested (OR, 1.54; 95% CI, 1.09–2.17).
MDs and DOs
Several of the variables that were associated with likelihood of being hesitant among nurses were also significant for MDs and DOs. Among MDs and DOs, women (OR, 2.12; 95% CI, 1.69–2.65), Blacks, and Asians (OR, 4.18; 95% CI, 2.43–7.18 and OR, 1.64; 95% CI, 1.25–2.16) and those living in rural areas (OR, 8.68; 95% CI, 1.32–57.18) were more likely to be vaccine hesitant than men, Whites, and those residing in urban areas. MDs and DOs aged 40–64 years or ≥65 were less hesitant than those <40 years old (OR, 0.74; 95% CI, 0.56–0.98 and OR, 0.48; 95% CI, 0.28–0.81). MDs and DOs who had ≥5 COVID-19 exposures were less hesitant than those who had no exposure (OR, 0.65; 95% CI, 0.49–0.85).
Discussion
In our analysis, we sought to understand differences in COVID-19 vaccine hesitancy among 3 groups with clinical facing job categories: (1) MDs and DOs, (2) NPs and PAs, and (3) nurses. Although 67.8% of the HCP surveyed stated that they would receive a COVID-19 vaccine, a significant portion were vaccine hesitant.
In all 3 job categories, racial or ethnic minority groups and women were the most hesitant. Race or ethnicity was significantly associated with vaccine hesitancy in this HCP population. Black HCP, regardless of whether they were nurses, NPs and PAs, or MDs and DOs, were 4–5 times more likely to be hesitant than White HCP. Hispanic nurses were 3.7 times as hesitant to be vaccinated as White nurses. Asian nurses and MDs and DOs were 1.6 times more hesitant than their White counterparts. Vaccine hesitancy in communities of color (CoCs) is well documented, especially for COVID-19 and influenza vaccines.8,10–12 Our findings are particularly concerning in light of the disproportionately high rates of COVID-19 associated morbidity and mortality within Black and Hispanic communities. Understanding hesitancy within communities at higher risk of poor outcomes who may have a higher occupational risk of exposure is critical.13 In addressing hesitancy in CoCs, it is important to recognize that vaccine hesitancy is multifactorial and can be influenced by issues related to complacency or perceived risk, confidence, and convenience.14 Factors underlying health disparities may also impact hesitancy, including longstanding structural racism and subsequent inequitable access to resources.15 Hesitancy among these racial/ethnic groups may also be a result of a history of medical mistreatment leading to mistrust in the healthcare system and providers.16
Our results also demonstrate a significant association between gender and hesitancy across all 3 job categories surveyed. Female nurses and MDs and DOs were twice as likely as their male counterparts to be vaccine hesitant. A similar trend was found among female NPs and PAs but was not significant. These results are consistent with a December 2020 survey that showed that 60% of women reported being nervous about vaccine receipt due to the newness of the vaccine.17 In the same survey, 48% of women who were not interested in receiving the vaccine stated that the risks of taking the new vaccine outweighed the benefits.17
Female HCP must become more comfortable with COVID-19 vaccines because they represent a large segment of the HCP workforce; their absence due to COVID-19 could affect the quality of healthcare delivery. Nurses are likely to be one of, if not the first, persons with whom patients discuss their healthcare, and they play an important role in vaccine communication. Additionally, women typically make most of the healthcare decisions for their families, and their willingness to be vaccinated may directly impact whether their families are vaccinated.17,18 Several factors may influence these observed gender differences. First, women may be concerned about the impact of the vaccine on pregnancy/fertility, as suggested by some of the comments from respondents. In our study, half the women were <40 years of age. Without prompting, 4% of women specifically noted pregnancy-related concerns as a reason for their hesitancy. More needs to be done to share the available data that suggests that COVID-19 vaccines do not impact pregnancy or fertility.19 A study examining factors that influence vaccine decision making during pregnancy demonstrated that pregnant women look to their HCP for trusted information about vaccines.20 During the 2009 influenza pandemic, HCP recommendations increased vaccination among pregnant women 6-fold.20
Another factor that might contribute to the higher rate of hesitancy among women is exposure to misinformation, an important contributor to vaccine hesitancy. Reasons for female vaccine hesitancy included side effects, a concern raised with other vaccines including flu.21 One possible explanation might be differential exposure to misinformation on vaccine safety which is often disseminated online and/or via social media.22 In the United States, women are more likely than men to search online for health-related information.23 A recent survey demonstrated that women are more likely than men to use ≥1 social media platform (78% vs 66%, respectively).24 Educational efforts should be enhanced to direct female HCP to more reliable sources of COVID-19 vaccine information, including accredited websites, scientific publications, and local trusted experts.25 Further research is needed to determine the primary sources of health information used by female versus male HCP in gathering vaccine information.
Nurses and MDs and DOs in our survey aged <40 years were more hesitant than their older colleagues. This finding aligns with national data that suggest younger adults are less likely to receive a COVID-19 vaccine.26 One possible explanation for this difference is that younger HCPs may recognize COVID-19 as a less serious disease for themselves compared to older HCPs.
In comparing the 3 job categories, nurses were the most (47.7%) vaccine hesitant group. Our findings were similar to 2 other surveys in which ∼40%–60% of nurses reported that they did not intend to be vaccinated.27,28 We also found that the primary reasons for vaccine hesitancy among nurses (concerns about side effects, newness of the vaccine, and not knowing enough about the vaccine) were also reported during the H1N1 pandemic.29
Our study used a definition of vaccine hesitancy similar to the WHO definition.9 Using this definition, 33% of HCPs in our survey were vaccine hesitant. This rate was surprising given that our survey population included well-educated HCP with significant clinical responsibilities. Many of the same reasons for vaccine hesitancy reported among the general population (including concerns about vaccine safety, effectiveness, and side effects, the newness of the vaccines, the vaccines may not work, not knowing enough about the vaccine, or possibly being infected by the vaccine) were also concerns expressed by this group of clinical-facing HCP.28 This finding suggests that HCP may not have had enough time to educate themselves and/or their colleagues about the vaccine before being offered the vaccine. A recent systematic review across multiple countries showed that other reasons for vaccine hesitancy among HCP include distrust of government and regulatory authorities and the information provided by public health experts.30 It is important to adjust the messaging HCP receive surrounding these vaccines based on their concerns and to better understand who their most trusted sources are for vaccine information.
We expected that this group of HCP with direct patient contact would readily seek vaccination to protect themselves while working. Although numerous HCP in each of the 3 groups reported ≥5 exposures to patients or family with COVID-19, only MDs and DOs with ≥5 exposures were more likely to seek vaccination (OR, 0.65; 95% CI; 0.49–0.85 vs 0 exposures). This finding may be the result of physicians having more intensive and/or direct exposure to seriously ill patients with complications, including those in ICUs or those who died.
It is critically important for frontline HCP to feel comfortable and confident in receiving and recommending COVID-19 vaccines. Primary care providers, family, medical websites, and nurses are among the top sources for health information.31 Clearly more work is needed to better understand and address the concerns of HCP about COVID-19 vaccines, especially among women and CoC. Selection of the appropriate messenger to deliver information about these vaccines is critical and may differ based on job category.32 Some methods to improve HCP vaccination include providing more information about the vaccines to employees via e-mail or town hall meetings and holding interactive information sessions for hesitant employees. It is also important to allow employees to voice their own concerns about the vaccines even though they are considered experts.
This study had several limitations. The survey was administered prior to the authorization of any COVID-19 vaccine; therefore, the results might differ if the same survey was administered after vaccine authorization. Conduct of the survey among HCP from 2 hospitals in Philadelphia with a 34% response rate may limit generalizability to other HCP. The number of NPs and PAs was smaller than the other 2 job categories. There was a relatively small number of Black and Hispanic respondents, though this was representative of the HCP population. We measured intention to receive the vaccine before it became available. With more of the population now vaccinated, the intentions of those who may have been more hesitant may have changed. Finally, vaccine hesitancy is complex, multifactorial, and may be driven by attitudes, beliefs, and risk perceptions that we did not measure.
This study also had several strengths. We surveyed a large, diverse sample of HCP at 2 academic hospitals prior to vaccine availability. Our results allowed us to better understand specific factors that influence hesitancy within clinical roles, providing insights on the relationship between demographics, job position, COVID-19 exposure risk, and the intention to receive the COVID-19 vaccine.
In summary, COVID-19 vaccine is an important tool by which HCP can protect themselves and their patients. Future work should build upon our findings to effectively address concerns contributing to vaccine hesitancy, particularly among HCPs of color and female HCP.
Acknowledgments
We acknowledge the hospital employees who participated in this research.
Financial support
There was no financial support for this work.
Conflicts of interest
Dr Kuter is a consultant for Moderna. Dr Feemster is an employee of Merck Research Laboratories. All other authors have no conflicts of interest to report.
References
- 1.US COVID-19 cases and deaths by State. Centers for Diseases Control and Prevention website. https://covid.cdc.gov/covid-data-tracker/#cases_casesper100klast7days. Published 2021. Accessed August 25, 2021.
- 2.COVID-19 vaccines. US Food and Drug Administration website. https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines. Published 2021. Accessed August 25, 2021.
- 3.COVID-19 vaccinations in the United States. Centers for Diseases Control and Prevention website. https://covid.cdc.gov/covid-data-tracker/#vaccinations. Published 2021. Accessed August 25, 2021.
- 4. Kirzinger A, Kearney A, Hamel L, Brodie M. KFF/The Washington Post Frontline Health Care Workers. The Washington Post/KFF Survey Project website. https://files.kff.org/attachment/Frontline%20Health%20Care%20Workers_Full%20Report_FINAL.pdf. Published 2021. Accessed August 25, 2021.
- 5.Talking to patients about vaccine safety. Centers for Diseases Control and Prevention website. https://www.cdc.gov/vaccinesafety/hcproviders/talkingtopatients.html. Published 2021. Accessed August 25, 2021.
- 6. Gadoth A, Halbrook M, Martin-Blais R, et al. Cross-sectional assessment of COVID-19 vaccine acceptance among healthcare workers in Los Angeles. Ann Intern Med 2021;174:882–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Herman AO. Nearly one-third of US healthcare workers hesitant to get COVID-19 vaccines. New England Journal of Medicine Journal Watch website. https://www.jwatch.org/fw117633/2021/03/21/nearly-one-third-us-healthcare-workers-hesitant-get-covid. Published 2021. Accessed August 25, 2021.
- 8. Kuter BJ, Browne S, Momplaisir FM, et al. Perspectives on the receipt of a COVID-19 vaccine: a survey of employees in two large hospitals in Philadelphia. Vaccine 2021;39: 1693–1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Report of the Sage Working Group on Vaccine Hesitancy. World Health Organization website. https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf. Published 2014. Accessed August 25, 2021.
- 10. Shaw J, Stewart T, Anderson KB, et al. Assessment of US healthcare personnel (HCP) attitudes towards COVID-19 vaccination in a large university health care system. Clin Infect Dis 2021. doi: 10.1093/cid/ciab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine 2020;38:6500–6507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Callaghan T, Moghtaderi A, Lueck JA, et al. Correlates and disparities of COVID-19 vaccine hesitancy. Soc Sci Med 2021; 272:113638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Owen WF Jr, Carmona R, Pomeroy C. Failing another national stress test on health disparities. JAMA 2020;323:1905–1906. [DOI] [PubMed] [Google Scholar]
- 14. Larson HJ, Jarrett C, Schulz WS, et al. Measuring vaccine hesitancy: the development of a survey tool. Vaccine 2015;33:4165–4175. [DOI] [PubMed] [Google Scholar]
- 15. Egede LE, and Walker RJ. Structural racism, social risk factors, and COVID-19—a dangerous convergence for Black Americans. N Engl J Med 2020;383(12):e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Momplaisir F, Haynes N, Nkwihoreze H, Nelson M, Werner RM, Jemmott J. Understanding drivers of COVID-19 vaccine hesitancy among blacks. Clin Infect Dis 2021. doi: 10.1093/cid/ciab102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kahn C, Beasley, D. More women than men in US nervous about fast rollout of COVID vaccine, and that’s a problem: Reuters/Ipsos poll. Reuters website. https://www.reuters.com/article/uk-health-coronavirus-vaccine-poll-idUKKBN28L0FI. Published December 2020. Accessed August 25, 2021.
- 18. Matoff-Stepp S, Applebaum B, Pooler J, Kavanagh E. Women as health care decision-makers: implications for health care coverage in the United States. J Health Care Poor Underserved 2014;25:1507–1513. [DOI] [PubMed] [Google Scholar]
- 19. Shimabukuro TT, Kim SY, Myers TR, et al. CDC v-safe COVID-19 pregnancy registry team. preliminary findings of mRNA COVID-19 vaccine safety in pregnant persons. N Engl J Med 2021;384:2273–2282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kilich E, Dada S, Francis MR, et al. Factors that influence vaccination decision-making among pregnant women: a systematic review and meta-analysis. PloS One 2020;15(7):e0234827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kempe A, Saville AW, Albertin C, et al. Parental hesitancy about routine childhood and influenza vaccinations: a national survey. Pediatrics 2020;146(1):e20193852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Annenberg Public Policy Center of the University of Pennsylvania. Vaccine misinformation and social media: people exposed to vaccine content on social media more likely misinformed than those exposed to it on traditional media. ScienceDaily website. www.sciencedaily.com/releases/2020/02/200217163004.htm. Published February 2020. Accessed August 25, 2021.
- 23. McGloin R, Richards K, Embacher K. Examining the potential gender gap in online health information-seeking behaviors among digital natives. Commun Res Repts 2016;33:370–375. [Google Scholar]
- 24.Social media fact sheet. Pew Research Center Internet and Technology website. https://www.pewresearch.org/internet/fact-sheet/social-media/?menuItem=45b45364-d5e4-4f53-bf01-b77106560d4c. Published April 2021. Accesssed August 25, 2021.
- 25. Kwok KO, Li KK, Wei WI, Tang A, Wong S, Lee SS. Editor’s Choice: Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int J Nurs Stud 2021;114:103854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nguyen KH, Srivastav A, Razzaghi H, et al. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination—United States, September and December 2020. Morbid Mortal Wkly Rept 2021;70:217–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wang K, Wong E, Ho KF, et al. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross-sectional survey. Vaccine 2020;38:7049–7056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Guidry J, Laestadius LI, Vraga EK, et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infecton Control 2021;49:137–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Henriksen Hellyer JM, DeVries AS, Jenkins SM, et al. Attitudes toward and uptake of H1N1 vaccine among health care workers during the 2009 H1N1 pandemic. PloS One 2011;6(12):e29478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Li M, Luo Y, Watson R, et al. Healthcare workers’ (HCWs) attitudes and related factors towards COVID-19 vaccination: a rapid systematic review Postgrad Med J 2021. doi: 10.1136/postgradmedj-2021-140195. [DOI] [PubMed] [Google Scholar]
- 31. Chen X, Hay JL, Waters EA, et al. Health literacy and use and trust in health information. J Health Commun 2018;23:724–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Altay S, Mercie, H. Framing messages for vaccination supporters. J Exper Psychol Appl 2020;26:567–578. [DOI] [PubMed] [Google Scholar]