Abstract
Schwannomas are the most common nerve sheath tumors which are usually solitary enucleated lesions. Multiple schwannomas are a rare circumstance which may occur with or without other manifestations of neurofibromatosis.
In this study, we report the case of a 45-year-old man presenting with pain and swelling in the thigh and popliteal space without any manifestation of neurofibromatosis or neurologic problems. Surgery was performed and revealed four separated tumors in the sciatic nerve which was characteristic of schwannoma and confirmed by pathologic findings.
Although multiple schwannomas are frequently associated with neurofibromatosis, the current case demonstrated a patient with multiple schwannomas without any manifestation of neurofibromatosis.
Key Words: Nerve sheath tumor, Neurofibromatosis, Schwannomatosis
Introduction
Schwannomas, also called neurilemomas, are the most common nerve sheath tumors (1). This tumor grows slowly with malignant transformation and rare symptomatic regrowth. It affects people of all ages but is more common among those aged 30-50 years (2). Schwannomas are usually solitary and encapsulated tumors; nonetheless, multiple tumors have been reported rarely in literature (3, 4). Multiple schwannomas are very rare situations which may occur with or without other manifestations of neurofibromatosis. “Neurilemmomatosis” was firstly introduced by Shishiba et al. to describe a distinct clinicopathological disease of multiple schwannomas without manifestations of neurofibromatosis (5).
Multiple schwannomas may arise from cranial nerves, spinal roots, as well as brachial and lum-bar-sacral plexus or major peripheral nerves (6). Chronic pain is the most common symptom in schwannomatosis patients (7). Although this tumor is a nerve sheath tumor, the neurologic complaints are uncommon unless the size of the tumor is large (8). This tumor will protrude or extrude from the nerve, leading to weakness, pain, or sensory changes (9). Tumor resection is the treatment of both solitary and multiple schwannomas. Pain often subsides when tumors are completely removed. There is no neurologic alteration reported during the postoperative period, which is proof of a good prognosis of this tumor (10, 11).
Here, we present a rare case of multiple schwannomas involving the right sciatic nerve of a 45-year-old man without other manifestations of neurofibromatosis.
Case presentation
A 45-year-old man was admitted to the hospital with a complaint of pain and swelling in his right thigh and popliteal space. There was no history of radicular pain.
There was swelling in the distal aspect of the posterior thigh and popliteal space. Pain and swelling have deteriorated recently. The patient had never noticed any subcutaneous lumps of nodules. There was no history of tinnitus, hearing loss, or vestibular problems. The patient had no previous medical problems and had not taken any medicine recently. Clinical examination demonstrated some masses in the distal aspect of the thigh just above the popliteal space. There was no tenderness on palpation of the masses. The masses were mobile in mediolateral view, fixed in the proximal and distal direction, and had a rubbery consistency.
When schwannoma was considered a possible diagnosis, we looked for Cafe´ au lait spots, axillary freckling, or Lisch nodules which were not observed. The ophthalmic examination also revealed no visible evidence of cataracts. Plain radiographs of the femur and knee did not show any bony abnormality. The magnetic resonance imaging (MRI) of the thigh demonstrated multiple, fusiform, and well-circumscribed masses along the course of the sciatic nerve [Figure 1]. Based on the MRI appearance of these lesions, a neurologic consultation was requested. The neurologist ordered Head MRI scans which were normal. There was also no family history of schwannomatosis or neurofibromatosis Type 2, formerly “central neurofibromatosis”.
Figure 1 (a- c).
a: Coronal T2 weighted magnetic resonance imaging, b: Axial T2 weighted magnetic resonance imaging, c: Sagital T2 weighted magnetic resonance imaging
The laboratory tests, including peripheral blood and blood chemistry, were all normal. Surgery was performed for an open biopsy. In the prone position, the skin was incised by the posterior mid-line approach to the thigh. The fascia was splitted, and the muscles were retracted; thereafter, the sciatic nerve was revealed. There were four separate masses along the sciatic nerve. They revealed clear de-lineation from the surrounding soft tissues. After the slight incision of epineurium, the masses were easily enucleated which was highly suggestive of schwannoma. The lesions were oval-shaped multi-lobulated 4-5cm masses in the greatest dimension. Histological findings of all the removed masses revealed the classic appearance of schwannoma. The patient was discharged the day after the surgery, and the recovery period was uneventful. At the last follow-up, the patient had no complaint, and the pre-operation pain was completely relieved.
Discussion
Schwannoma is a benign nervous system tumor arising from spinal nerve roots (12). A schwannoma is usually a solitary lesion, and multiple schwannomas which have been reported in peripheral nerves in rare circumstances are usually associated with neurofibromatosis (13).Enziger and Weiss pointed out that a schwannoma occurs always as a solitary lesion, except in association with neurofibromatosis; however, our case was a patient with multiple schwannomas with no other manifestation of neurofibromatosis (3).
In literature, there are few reports of multiple schwannomas without neurofibromatosis manifestation. For instance, Traistaro et al. reported a case with multiple schwannomas on the right side of the body (9). Lewis et al. pointed to a patient with multiple schwannomas in both the median and ulnar nerves in the same extremity (14). Shank et al. presented a patient with ulnar neuropathy and four separated schwannomas along the ulnar nerve (15). J Huang et al. presented a patient with multiple Schwannoma in the sciatic nerve; nonetheless, unlike our case, the patient had motor weaknesses and other neurological problems (6).
Gonzalo et al. in 2010 reported that patients with solitary schwannoma are older than those with schwannomatosis; moreover, they found pain as the initial symptom of these patients. This tumor, as in our case, is a mobile, slow-growing, and encapsulated tumor. Multiple schwannomas may present as visible tumors or in situ. The visible tumor is excised, while the tumors in situ may be missed. The schwannomas in situ grow over time and appear to be recurrent, while in fact, they are multicentric (16, 17).
Although the neurologic symptoms are rare, clinicians should be aware that schwannomatosis could reveal variable symptoms apart from pain. For example, in a case report by Park et al., the patient had segmental schwannoma, presenting with motor weakness which was confirmed by electrodiagnostic studies (18). The possibility of neurofibromatosis type 2 should be excluded in patients with multiple schwannomas before the diagnosis of schwannomatosis.
Several studies referred to schwannomatosis as a distinct clinical entity; nevertheless, there are still arguments whether all cases of multiple schwannomas are variants of neurofibromatosis type 2 or a distinct clinicopathological entity. Schwannomatosis and neurofibromatosis should be distinguished from each other by clinical examinations, such as café-au-lait spots and neurofibromas which are only present in neurofibromatosis (8). Moreover, this distinction can be made histologically by S-100 immunostaining which is prominent and uniform in schwannomas cellular areas, whereas in neurofibromatosis, there are variable staining patterns for S-100 (19).
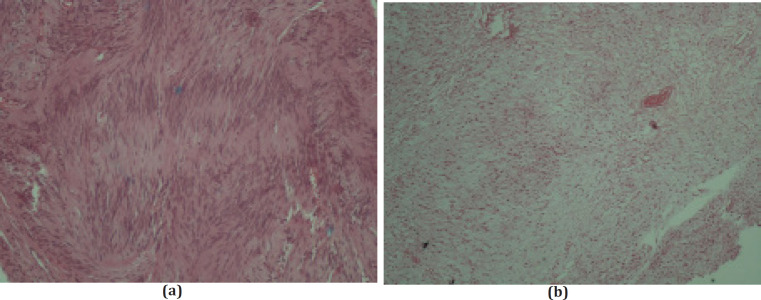
T2-weighted MRI may demonstrate a “target sign” which is a peripheral hyperintense rim with central low intensity which is characteristic of schwannoma (6). On gross pathology, there is a well-circumscribed elliptical or spherical-shaped tumor that may involve any nerve. Its location is beyond the oligodendroglial Schwann cell junction with nerve fascicles displaced around the tumor capsule (9). Histological features of schwannoma, as in our case, include two different areas, Antoni type A with compact bundles of Schwann cells and Antony type B with the loose matrix of oval cells [Figure 2] (6).
Figure 2 (a,b).
a. Antoni type A cells in histological pathology of the presented case, b. Antoni type B cells in histological pathology of the presented case
Surgery is the gold treatment for Schwannoma, and the main principle is simple enucleation of the tumor without damaging the nerve (20). In our case, we performed a surgery, four separated tumors were revealed in the sciatic nerve, and all of them were excised without damaging the nerve[Figure 3]. Pathological findings confirmed our diagnosis, and post-operation follow-up was uneventful.
Figure 3.
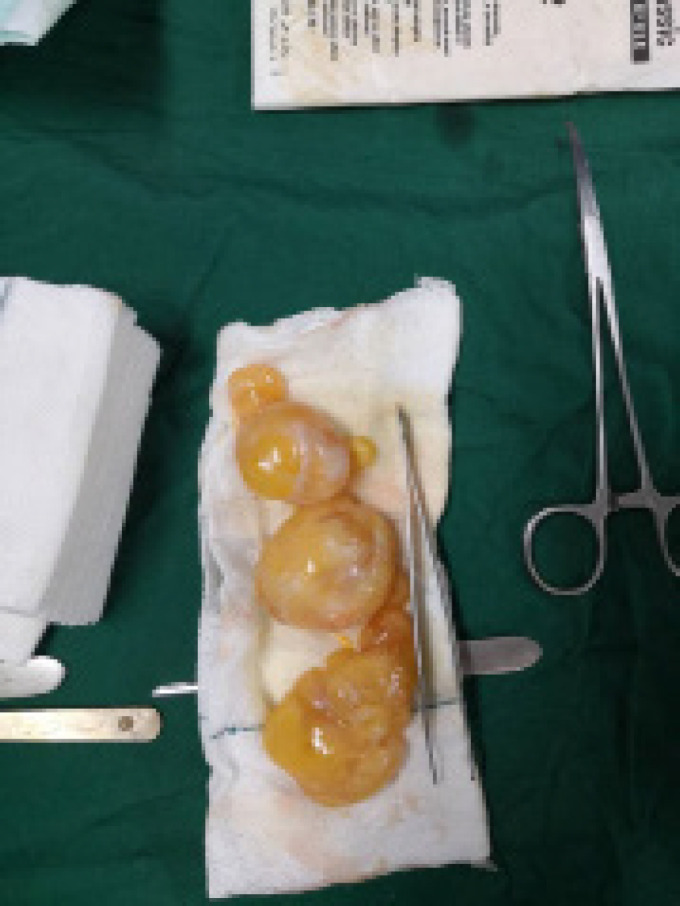
Tumors enucleated from sciatic nerve
A schwannoma is the most common nerve sheath tumor which is routinely a solitary lesion. Multiple schwannomas are frequently associated with neurofibromatosis type 2. Schwannomatosis is a rare circumstance that is presenting with multiple schwannomas without any manifestation of neurofibromatosis. In any patient with suspected schwannomatosis, the possibility of neurofibromatosis type 2 must be ruled out.
References
- 1.Lozano EAR, Mata JP, Fuller IR, Chávez J. Neurilemoma del nervio cubital: diagnóstico y tratamiento. Reporte de un caso. Cirugia Plastica. 1999;9(2):83–5. [Google Scholar]
- 2.Kleihues P, Louis DN, Scheithauer BW, Rorke LB, Reifenberger G, Burger PC, et al. The WHO classification of tumors of the nervous system. Journal of Neuropathology & Experimental Neurology. 2002;61(3):215–25. doi: 10.1093/jnen/61.3.215. [DOI] [PubMed] [Google Scholar]
- 3.Ogose A, Hotta T, Morita T, Otsuka H, Hirata Y. Multiple schwannomas in the peripheral nerves. The Journal of bone and joint surgery British volume. 1998;80(4):657–61. doi: 10.1302/0301-620x.80b4.8532. [DOI] [PubMed] [Google Scholar]
- 4.Ozdemir O, Kurt C, Coskunol E, Calli I, Ozsoy M. Schwannomas of the hand and wrist: long-term results and review of the literature. Journal of Orthopaedic Surgery. 2005;13(3):267–72. doi: 10.1177/230949900501300309. [DOI] [PubMed] [Google Scholar]
- 5.Shishiba T, Niimura M, Ohtsuka F, Tsuru N. Multiple cutaneous neurilemmomas as a skin manifestation of neurilemmomatosis. Journal of the American Academy of Dermatology. 1984;10(5):744–54. doi: 10.1016/s0190-9622(84)70089-2. [DOI] [PubMed] [Google Scholar]
- 6.Huang J, Mobbs R, Teo C. Multiple schwannomas of the sciatic nerve. Journal of clinical neuroscience. 2003;10(3):391–3. doi: 10.1016/s0967-5868(03)00021-3. [DOI] [PubMed] [Google Scholar]
- 7.Merker VL, Esparza S, Smith MJ, Stemmer-Rachamimov A, Plotkin SR. Clinical features of schwannomatosis: a retrospective analysis of 87 patients. The oncologist. 2012;17(10):1317. doi: 10.1634/theoncologist.2012-0162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pilavaki M, Chourmouzi D, Kiziridou A, Skordalaki A, Zarampoukas T, Drevelengas A. Imaging of peripheral nerve sheath tumors with pathologic correlation: pictorial review. European journal of radiology. 2004;52(3):229–39. doi: 10.1016/j.ejrad.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Trăistaru R, Enăchescu V, Manuc D, Gruia C, Ghiluşi M. Multiple right schwannoma. Rom J Morphol Embryol. 2008;49(2):235–9. [PubMed] [Google Scholar]
- 10.Komuro Y, Sekiguchi J, Ohmori K. Multiple neurilemomas of the ulnar nerve: a case report. Annals of plastic surgery. 1997;38(5):536–7. doi: 10.1097/00000637-199705000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Martinez JA, Gastaldi PR, Palomares ET. Multiple schwannoma of the sciatic nerve Apropos of a case. Revue de chirurgie orthopedique et reparatrice de l’appareil moteur. 1999;85(6):632–5. [PubMed] [Google Scholar]
- 12.Goldblum JR, Weiss SW, Folpe AL. Enzinger and Weiss’s soft tissue tumors E-book. Elsevier Health Sciences; 2013. [Google Scholar]
- 13.Huson SM, Hughes RAC. The neurofibromatoses: a pathogenetic and clinical overview: Chapman & Hall Medical; 1994. [Google Scholar]
- 14.Lewis RC, Nannini LH, Cocke WM. Multifocal neurilemomas of median and ulnar nerves of the same extremity—case report. Journal of Hand Surgery. 1981;6(4):406–8. doi: 10.1016/s0363-5023(81)80054-8. [DOI] [PubMed] [Google Scholar]
- 15.Shank CP, Friedman WA. Ulnar neuropathy in a patient with multiple schwannomas of the ulnar nerve. Surgical neurology. 1987;28(2):153–7. doi: 10.1016/0090-3019(87)90091-7. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalvo A, Fowler A, Cook RJ, Little NS, Wheeler H, McDonald KL, et al. Schwannomatosis, sporadic schwannomatosis, and familial schwannomatosis: a surgical series with long-term follow-up. Journal of neurosurgery. 2011;114(3):756–62. doi: 10.3171/2010.8.JNS091900. [DOI] [PubMed] [Google Scholar]
- 17.Patel MR, Mody K, Moradia VJ. Multiple schwannomas of the ulnar nerve: a case report. Journal of Hand Surgery. 1996;21(5):875–6. doi: 10.1016/S0363-5023(96)80207-3. [DOI] [PubMed] [Google Scholar]
- 18.Kwon NY, Oh H-M, Ko YJ. Multiple lower extremity mononeuropathies by segmental schwannomatosis: a case report. Annals of rehabilitation medicine. 2015;39(5):833. doi: 10.5535/arm.2015.39.5.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Enzinger F. Benign tumors of peripheral nerves. Soft tissue tumors. 1995:821–88. [Google Scholar]
- 20.Dyck P. Hereditary motor and sensory neuropathies. Peripheral neuropathy. 1993:1094–136. [Google Scholar]