Abstract
Background:
Proprioceptive training in the aquatic environment is more beneficial owing to water properties. The primary goal of the present study was to investigate the effectiveness of the incorporation of innovative aquatic proprioceptive training into conventional accelerated land-based rehabilitation protocol in knee function and joint position sense in male athletes after anterior cruciate ligament reconstruction (ACLR).
Methods:
A total of 38 athlete male athletes with ACLR were randomly assigned to two rehabilitation groups. The conventional therapy group (CT) (n=19) received conventional rehabilitation for 6 weeks, while the hydrotherapy group (HT) (n=19) received the same conventional rehabilitation, in addition to 12 sessions of innovative aquatic proprioceptive training. The outcomes included the joint position sense (JPS) errors, visual analog scale (VAS), and international knee documentation committee (IKDC). Repeated measures analysis of variance (ANOVA) was used to compare the means between the two groups. Cohen’s d from an independent t-test was used to calculate the effect sizes for all variables after the intervention for both groups.
Results:
Base on the results, there were a significant difference in absolute errors (AE) (FAE=56.231, P<0.001) and variable errors (VE) (FVE=60.245, P<0.001) between the two groups. No significant differences were detected in constant error (CE), VAS, and IKDC between the two groups (P>0.05). Both groups displayed a significant difference in terms of AE, VE, VAS, and IKDC after the intervention (P<0.05). Percent changes after the intervention for AE(69.19%), VE (68.20%), CE (65.20%), VAS37.50%, and IKDC (38.61%) were greater in the HT group, compared to the CT group.
Conclusion:
As evidenced by the obtained results, innovative aquatic proprioceptive training incorporate into the conventional rehabilitation accelerated protocol offers the improvement of proprioception efficiency for individuals with ACL reconstruction. Therefore, it could be useful to clinicians when designing rehabilitation protocol to ensure the optimal engagement of proprioception.
Key Words: ACL, Aquatic exercises, Anterior cruciate ligament reconstruction, Hydrotherapy, Proprioception, Rehabilitation, Sports injury
Introduction
The anterior cruciate ligament (ACL) in the knee is a key element for static and dynamic joint stabilities. Therefore, it is quite vulnerable in sports activities with an annual incidence of approximately 69 per 100,000 person-years (1). The ACL sends information mainly about the middle-range of the knee movement to the central nervous system through its receptors (2). The ACL reconstruction (ACLR) is a common procedure to improve the mechanical stability of the knee joint and regain the pre-injury level of function and dynamic neuromuscular control (3, 4). It is expected that the information received by the central nervous system be distorted due to the altered joint mechanoreceptors and nervous central connections after the ACL injury and ACLR. This, in turn, leads to clinical proprioceptive deficits with functional instability in most patients. (5, 6). Accordingly, the recovery of proprioceptive functions after ACL reconstruction is of critical importance for the restoration of the strength, range of motion (ROM), and integrity of the graft (7). Consequently, there is a wealth of research on the peculiar role of proprioception and exercise training on the improvements of functional stability of the knee joint after ACLR (8).
Aquatic training is used in many rehabilitation programs, such as cardiovascular and cardiopulmonary, musculoskeletal, geriatric, and psychiatric rehabi-litation, as well as pain control, since it is able to increase neuromuscular performance and early active mobilization. Due to the gravity reduction and buoyancy effect of water, the influences of weight-bearing and impact forces on joints are reduced during water exercises (9). Moreover, due to hydrostatic pressure and viscosity properties of water, proprioceptive training in the aquatic environment may be more beneficial to the provision of sensory feedback, compared to those felt in the ground training (10). In many cases, patients’ fear of recurrent injury may negatively affect the beneficial effects of proprioceptive exercises in ACLR rehabilitation (11). Therefore, the aquatic environment may be more suitable for doing exercises, assisting athletes in safety optimization.
The evidence on aquatic interventions is still under study. A few specific intervention models have been introduced, addressing the variables needed for athletes’ post ACL reconstruction. These models were mainly a combination of aquatic and land-based training interventions (12-16). In their study, Peultier-Celli et al. demonstrated that rehabilitation protocol incorporating both land and aquatic training improved the proprioception and limited the excessive compensation load on the uninjured limb (12). In the same context, Zamarioli et al. reported that patients subjecting to the aquatic protocol recovered faster in terms of muscle strength, swelling, pain, ROM, and muscle mass circumference, in comparison to those undergoing conventional land therapy(13).
Although the popularity of aquatic therapy has increased recently, the effect of aquatic proprioceptive training on post-ACLR proprioception improvement has not been well documented. In addition, all previous studies about aquatic training after ACLR were conducted in the very early phase of rehabilitation. The literature review yielded no study about the impact of aquatic proprioceptive training on knee joint position sense in patients with ACLR. Therefore, the current study aimed to assess the effectiveness of adding the innovative aquatic proprioceptive training to the conventional land-based accelerated rehabilitation protocol in knee function and joint position sense in male athletes after ACL reconstruction. It was hypothesized that the incorporation of innovative aquatic proprioceptive training into the conventional land-based accelerated rehabilitation protocol would result in better functional outcomes.
Materials and Methods
Design
This prospective randomized controlled study used a conventional rehabilitation group as a comparison group. All subjects were asked to sign an informed consent form approved by the Ethics Committee of Tehran University of Medical Sciences (Ethics approval ID: IR.TUMS.VCR.REC.1398.571).
Participants
A total of 38 male volunteers from physical therapy clinics of the Rehabilitation Faculty and Sports Medicine Federation participated in this study. All subjects were either professional or amateur athletes. They had undergone reconstruction surgery using a similar technique (hamstring tendon graft). The inclusion criteria were as follows: 1) athletes aged 18-35 years, 2) undergoing a unilateral ACL reconstruction, 3) no history or signs of injury in the contralateral knee, 4) less than one month from injury to the surgery date, 5) six weeks post ACLR, 6) knee ROM greater than 100° flexion and complete extension (zero degrees). On the other hand, the athletes with ACLR were excluded if they had pain at the time of the tests, any complication that prevents data collection, and any contraindication to aquatic exercises, such as hydrophobia, open wound, any active infection, and incontinence during exercise (9).
Subjects were randomly assigned to two rehabilitation groups. In doing so, 19 slips of paper were marked with the HT letters, and 19 with CT letters. Each slip of paper was randomly allocated to 38 sealed envelopes numbered 1-38 by the project manager. Subsequently, the numbered sealed envelopes were sent to the assessor who did the testing and the evaluation sessions for the subjects. After collecting the subjects, they were numbered 1-38 in the order they visit the clinic to complete the baseline testing session. The laboratory director who was not an investigator of the study opened the corresponding sealed envelope to disclose the group allocation of subjects. The first group was the conventional therapy (CT) (n=19; mean age: 24.68±3.78 years; weight: 78.57±4.94 kg) and they did the conventional land-based therapy according to accelerated rehabilitation protocol (17). The second group was the hydrotherapy (HT) (n=19; mean age: 23.79±3.04 years; weight 80.57±3.88 kg) and they did an innovative aquatic proprioceptive training with the conventional land-based accelerated rehabilitation protocol. Both groups were matched according to the demographic characteristic [Table 1].
Table 1.
Anthropometric characteristics of subjects
| Variables | HT group (n=19) | CT group (n=19) | P value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Age (years) | 23.79 ± 3.04 | 24.68 ± 3.78 | 0.514 |
| High (omit57m) | 174.64 ± 4.85 | 173.21 ± 4.74 | 0.091 |
| Weight (kg) | 80.57 ±3.88 | 78.57 ± 4.94 | 0.145 |
| BMI (kg.m2) | 26.64 ± 1.98 | 26.29 ± 1.75 | 0.994 |
Abbreviations: SD: standard deviation, BMI: body mass index
Outcomes and testing protocols
Clinical evaluations were performed pre and post-intervention for both groups as follows: 1) Proprioception assessed by active joint position sense, 2) Level of pain assessed by visual analog scale (VAS), and 3) Knee function assessed by International Knee Documentation Committee (IKDC) questionnaire.
Proprioception assessment
Proprioception was assessed by active Joint Position Sense (JPS) to test the ability to reproduce the same joint position during knee extension and flexion using Biodex Medical Systems (System 3 Pro™, New York, USA) for the affected leg (18, 19). In doing so, the subject was blindfolded and placed on a System chair, with head and back supported and the hip joints in an 80° flexed position. The upper limbs were placed along the trunk with the elbows bent and hands positioned on the thighs. The legs were relaxed in a 90° resting position. The goniometer axis of rotation was placed at the lateral femoral condyle to match the flexion/extension axis of rotation of the knee joint. Belts were used to stabilize the subject in place in the chest, hip, and thigh. Prior to test performance, the dynamometer was calibrated by asking the subject to place the knee at 0° of flexion.
The subject was then asked to place the knee in the starting point at 90° of knee flexion. Thereafter, the subject was instructed to move the limb leisurely to 45°(target angle) of extension. Following that, the subject was asked to hold the limb at the target angle for 10 sec to let him remember the position. The subject was then instructed to return the leg to the starting point (90°). After a 15-sec pause, the cycle was performed again. Once the subject believed that the position (estimated angle) had been achieved, he pressed a stop button and was not allowed to correct the angle again. The estimated angle was identified from the onscreen goniometer. Five trials were performed for each subject, and the average of these trials was used to calculate errors in each set. The absolute mean error and relative mean error were calculated as the variables of JPS using the following formulas (20):
-Absolute Error (AE) (i.e. magnitude of error) was calculated by formula 1:
AE = Σ [X-C]/K (1)
-Constant Error (CE) (i.e. the amount of bias) was calculated by formula 2:
CE = Σ(X-C)/K (2)
-Variable Error (VE) (i.e. the consistency of the performer) was calculated by formula 3:
VE = √ [Σ(X-C)2/k] – (CE)2 (3)
X= target angle, C= estimated angle, K= number of repetitions.
Pain assessment
The pain intensity of the reconstructed knee was assessed using the VAS. The scale consisted of a 10-cm line (100 mm) with the left end designed as no pain at (0) and the right end with intolerable pain at (10). All subjects were asked to determine the severity of pain by a small mark on the line (21).
Knee function assessment
All subjects responded to the IKDC questionnaire to assess the function during daily activity and the level of a symptom-free sports activity. The IKDC contains items on knee symptoms(n=7), function (n=2), and sports activities (n=2). The scores range from 0-100, with 0 and 100 points referring to the lowest and highest levels of function, respectively (22). The Persian version of IKDC is a reliable, valid, and responsive measure for patients with an ACL injury (23).
Intervention
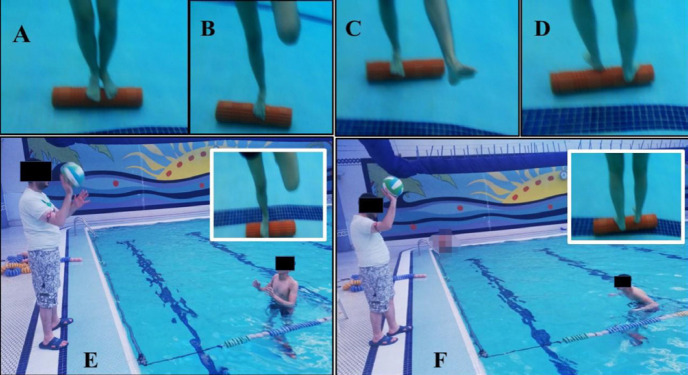
All subjects initiated similar conventional rehabilitation protocols according to the accelerated land-based rehabilitation protocol for seven weeks, starting from day 1 post-surgery till the recruitment day (17). In week seven, the subjects were randomized into two rehabilitation groups. The CT group continued to receive three weekly 60-75 min sessions of conventional rehabilitation, including strengthening, walking, and neuromuscular training for six weeks. The HT group received the same conventional rehabilitation, apart from the innovative aquatic proprioceptive training. All subjects in this group underwent two weekly 45-60 min sessions of innovative proprioception aquatic exercises for six weeks. Each hydrotherapy session consisted of three parts: warm-up, main practice, and cooling down. The subjects performed a series of stretching exercises of the soleus, hamstring, and quadriceps muscles to avoid muscular fatigue. The injured leg underwent training while the subject was barefoot during the exercises. During water exercise, the subjects were not allowed to support themselves by the contralateral limb or hands. If the subjects lost their balance, they were asked to lean on the contralateral limb. During the exercises, the subjects were asked to remain at a depth where the water level was between the waist and the sternum. The exercises were performed according to individual ability and the patient’s response to training. The progression of the training protocol was as follows: 1) Single-leg stance with eyes open, 2) Single-leg stance with eyes closed, 3) Single-leg stance with leg swing and eyes open, 4) Single-leg stance with leg swing and eyes closed, 5) Single-leg squat with eyes open and knee flexed at 30°, 6) Single-leg squat with eyes closed and knee flexed at 30°, 7) Double-leg stance on Foam Roll; subject in standing position, barefoot, double-legged support. 8) Single-leg stance on Foam Roll; subject in standing position, barefoot, one-legged support. 9) Single-leg stance with leg swing on Foam Roll; subject in standing position, barefoot, one-legged support. 10) Rollover walking forward with crossed arms on Foam Roll; subject in standing position on Foam Roll, barefoot, double leg support, walking forward and arms crossed, 11) Single-leg stance on Foam Roll and throwing the ball; subject in a standing position on Foam Roll, one-legged support, throwing the ball to the subject and throwing it back to the therapist. 12) Rollover walking forward on Foam Roll and throwing the ball; subject in standing position on Foam Roll, barefoot, double leg support, walking forward, throwing the ball to the subject and throwing it back to the therapist. The intervention was conducted in a professional swimming pool with all the needed equipment for aquatic exercises, with pool water temperature ranging from 28°-30°C [Figure 1].
Figure 1.
Aquatic training on Foam Roll. A) Double-leg stance on Foam Roll; B) Single-leg stance on Foam Roll; C) Single-leg stance with leg swing on Foam Roll; D) Rollover walking forward on Foam Roll; E) Single-leg stance on Foam Roll and throwing the ball; and F) Rollover walking forward on Foam Roll and throwing the ball
Statistical analysis
The independent t-test was used to analyze the difference in anthropometric characteristics of subjects at baseline. One-sample Kolmogorov-Smirnov test was utilized to check the normal distribution of the variables. The variables had a normal distribution; therefore, the independent t-test was employed to assess within-group differences between pre and post-intervention. Moreover, the repeated measures analysis of variance (ANOVA) was used to compare the differences between the two groups. Cohen’s d from an independent t-test was used to calculate the effect sizes to gain a deeper understanding of clinical meaningfulness after the interventions. The relative size of Cohen’s d was used: negligible effect (>= -0.15 and < 0.15), small effect (>=0.15 and < 0.40), small effect (>= 0.15 and < 0.40), medium effect (>= 0.40 and < 0.75), large effect (>=0.75 and < 1.10), very large effect (>=1.10 and < 1.45), huge effect >1.45. A p-value of 0.05 was considered statistically significant for all analyses. The data were analyzed in SPSS Statistics for Windows, version 25 (SPSS Inc., Chicago, Ill., USA).
Results
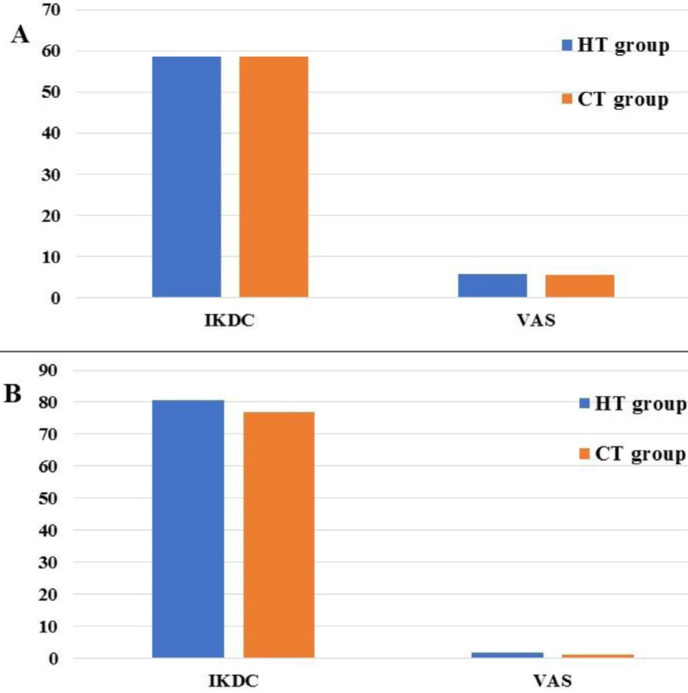
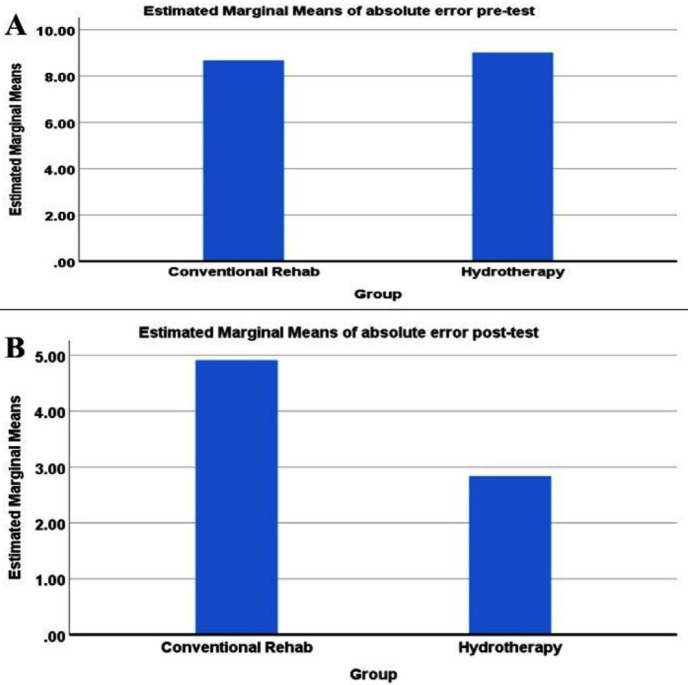
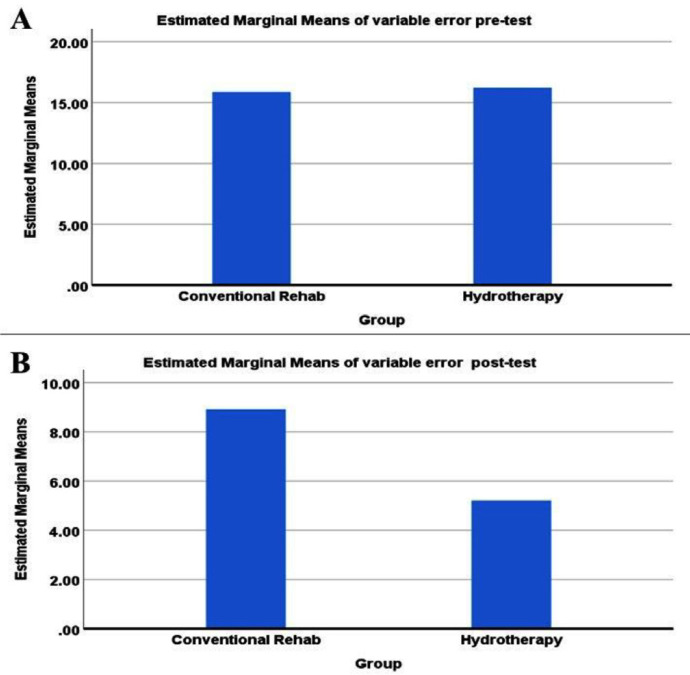
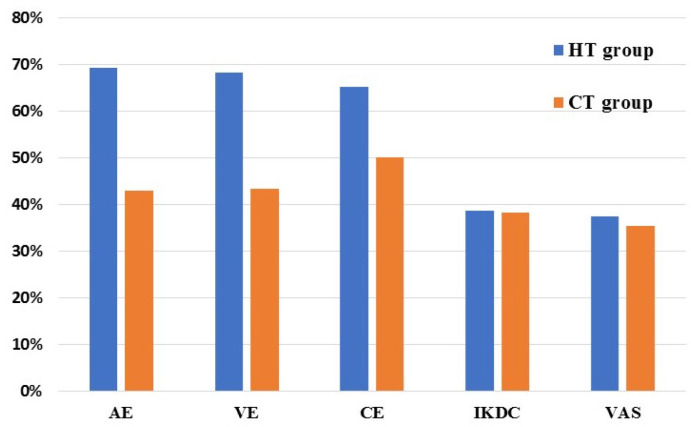
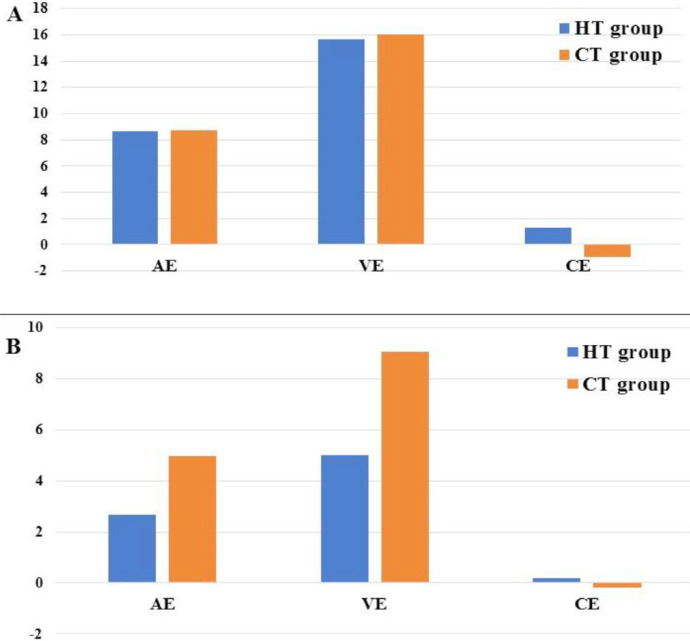
The anthropometric characteristics of subjects are presented in Table 1. No significant difference was found between the two groups regarding the anthropometric characteristics (i.e. age, height, weight, body max index) before the interventions (P>0.05). In both groups, there were significant differences in AE, VE, VAS, and IKDC between pre and post-intervention (P>0.05). Moreover, the two groups did not significantly differ in CE before and after the intervention (P>0.05) [Figures 2; 3 and Table 2].
Figure 3.
Means of international knee documentation committee and visual analog scale of both groups: A) before the intervention, B) after the intervention
Table 2.
Mean and SD of results before and after the intervention for two groups (n=19)
| Variables | Group |
Before
Mean ± (SD) |
After
Mean ± (SD) |
P value |
|---|---|---|---|---|
| AE | HT | 8.67 ± 1.11 | 2.67 ± 0.69 | 0.000 |
| CT | 8.72 ± 1.13 | 4.97 ± 1.08 | 0.000 | |
| VE | HT | 15.68 ± 2.13 | 4.99 ± 1.29 | 0.000 |
| CT | 16.03 ± 2.44 | 9.06 ± 1.79 | 0.000 | |
| CE | HT | 1.27 ± 8.29 | 0.18 ± 2.85 | 0.91 |
| CT | -0.91 ± 8.93 | -0.20 ± 5.24 | 0.49 | |
| VAS | HT | 5.86 ± 1.03 | 1.79 ± 1.12 | 0.02 |
| CT | 5.42 ± 0.93 | 1.21 ± 1.36 | 0.019 | |
| IKDC | HT | 58.61 ± 4.82 | 80.65 ± 2.38 | 0.000 |
| CT | 58.51 ± 5.08 | 76.88 ± 1.88 | 0.000 |
Abbreviations: AE: absolute error, VE: variable error, CE: constant error, VAS: visual analog scale, IKDC: international knee documentation committee
There was a significant difference in AE (FAE = 56.231, P < 0.001) and VE (FVE = 60.245, P < 0.001) between the two groups [Table 3]. The improvement of AE and VE in the HT group was significantly greater than that in the CT group [Figures 4; 5]. Nevertheless, no significant differences were observed in CE (FCE = 0.295, P> 0.05), VAS (FVAS= 0.422, P>0.05), and IKDC (FIKDC= 0.030, P>0.05) between the two groups (P>0.05) [Table 3]. Effect sizes for all variables after the intervention for both groups are reported in Table 4. The HT group showed the greatest improvement in all variables after the intervention [Figure 6]. Among all variables in the HT group, the largest percent change was found for AE and VE.
Table 3.
ANOVA results to compare between two rehabilitation groups (n=19)
| Variable | Sum of Squares | Mean Square | F | P |
|---|---|---|---|---|
| AE | 67.172 | 40.955 | 56.231 | 0.000 |
| CE | 632.595 | 5.136 | 0.295 | 0.591 |
| VE | 208.421 | 130.462 | 60.245 | 0.000 |
| VAS | 56.763 | 0.658 | 0.422 | 0.52 |
| IKDC | 164.628 | 0.139 | 0.030 | 0.862 |
Abbreviations: AE: absolute error, VE: variable error, CE: constant error, VAS: visual analog scale, IKDC: international knee documentation committee
Figure 4.
Absolute error plot of both groups: A) before the intervention, B) after the intervention
Figure 5.
Variable error plot of both groups: A) before the intervention, B) after the intervention
Table 4.
Effect size after intervention for two groups (n=19)
| Groups | Variables | Cohen’s d | Percent Change % |
|---|---|---|---|
| CT group (n=19) | AE | 3.51 | 42.96 |
| VE | 3.37 | 43.44 | |
| CE | 0.03 | 50 | |
| VAS | 1.07 | 35.42 | |
| IKDS | 6.06 | 38.22 | |
| HT group (n=19) | AE | 6.73 | 69.19 |
| VE | 6.3 | 68.20 | |
| CE | 0.1 | 65.20 | |
| VAS | 1.03 | 37.50 | |
| IKDC | 6.07 | 38.61 |
Abbreviations: AE: absolute error, VE: variable error, CE: constant error, VAS: visual analog scale, IKDC: international knee documentation committee
Figure 6.
Percent change after the intervention of both groups
Discussion
The present study aimed to make a comparison between innovative aquatic proprioceptive training incorporated into the conventional rehabilitation accelerated protocol and the conventional rehabilitation accelerated protocol concerning the impact on the improvement of proprioception and pain functional improvement in athletes with ACLR. The obtained results indicated that the incorporation of innovative aquatic proprioceptive training into the conventional rehabilitation accelerated protocol offers the improvement of proprioception efficiency for individuals with ACL reconstruction.
The proprioception assessment showed significant differences between the two groups after the intervention regarding the JPS variables. The result of the current study revealed that subjects who followed innovative aquatic proprioceptive training plus the conventional rehabilitation accelerated protocol had significantly reduced proprioception magnitude errors, signifying a reduction in proprioceptive deficit after the intervention. These differences between the groups can be attributed to several reasons. The aquatic environment imposes a continuous muscle activation to maintain the stability of the body since there is no stable resting position within it. This stability is provided by hydrostatic pressure that plays a role as an external sensory stimulus, which provides equal resistance to all activated muscle groups. Therefore, the promotion of the stimulation of the proprioceptive pathway increases sensory feedback and body awareness (9, 24). In the current study, for instance, standing on Foam Roll creates sensory information. As walking back and forth on Foam Roll, the patient challenges maintaining his/her balance, which in turn, promotes neuromuscular coordination and proprioception efficiency.
The results of the present study were inconsistent with those reported by Peultier-Celli et al. who made a comparison between the aquatic rehabilitation protocol with a reduced conventional protocol and conventional therapy. In the mentioned study, no significant difference was reported between the two groups. This discrepancy can be ascribed to the nature of aquatic rehabilitation protocol. The aquatic protocol in the current study was focused on proprioception exercises, while their protocol included rehabilitative exercises in general (12).
Furthermore, the present study made a comparison between the two groups. The result pointed out that there was no significant difference in the reduction of pain between the two groups, and a decreased pain level was found in both groups after the interventions. The mechanism of pain reduction in the aquatic environment could be due to the stimulation of the sensory nerve endings in the skin by the hydrostatic effect. Moreover, it was hypothesized that sensory overflow leads to pain modulation and probable elevation of pain threshold which increases with temperature and water turbulence (25). Pain reduction in the CT group could be due to the optimization of muscle strength and endurance around the knee joint, in addition to continuous improvement in tissue healing (17).
No significant difference was found between the two groups in IKDC. Both groups displayed a significant improvement in IKDC. However, the subjects who followed innovative aquatic proprioceptive training plus the conventional rehabilitation accelerated protocol gained higher scores in their IKDC. Therefore, it was not surprising that an increase in proprioception efficiency and the reduction of pain are reflected in the quality of life and sports activities. Owing to the unique properties of the aquatic environment, several studies were conducted to take advantage of these properties in favor of patients with ACLR (12-16). The majority of these studies compared the effect of land-based therapy with hydrotherapy using similar exercises. Nonetheless, the current research specifically focused on the incorporation of aquatic proprioception exercises into the conventional rehabilitation accelerated protocol. Except for one research (12), none of these studies used the JPS test to assess any possible changes in proprioception (13-16).
Among the notable limitations of the present study, we can refer to the recruitment of relatively a small number of subjects and the inclusion of only male subjects with a hamstring tendon graft. Therefore, the obtained results can not be generalized to all individuals who are suffering from the side effects of post ACLR. Future studies should include larger samples, both genders, and several reconstruction surgery techniques to generalize results. Furthermore, although the current study demonstrated that proprioception efficiency was improved after the innovative proprioception protocol, follow-up assessments were not carried out to observe the durability of these changes. Moreover, the present study did not include functional tests, and future studies should consider the functional tests (e.g. single-hop test, cross-over-hop test, triple-hop test) to assess the correlation between functional performance and improvement in proprioception gained after the intervention.
Innovative aquatic proprioceptive training plus the conventional rehabilitation accelerated protocol resulted in the improvement of proprioception efficiency, pain, and knee function in individuals with ACL reconstruction. The marked improvements in the JPS could be attributed to taking proprioception exercises in a combination of aquatic proprioceptive training plus conventional therapy. Therefore, the present study stressed the importance of designing special aquatic exercises to improve a specific function instead of performing aquatic exercises in general. Furthermore, the findings revealed that this protocol was an appropriate method for proprioception training in athletes, especially those who were afraid of injury recurrence during the proprioception training exercises. It is worth noting that this aquatic proprioceptive training is the first in this field, and it can be named “Hajouj’s Aquatic Proprioceptive Protocol Training”.
Figure 2.
Means of joint position sense variables of both groups: A) before the intervention, B) after the intervention
Acknowledgments
The present study was financially supported by Tehran University of Medical Sciences. The authors’ sincere appreciation goes to all the staff of the School of Rehabilitation who kindly helped us with this research project.
Conflicts of Interest:
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- 1.Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA, et al. Incidence of Anterior Cruciate Ligament Tears and Reconstruction: A 21-Year Population-Based Study. Am J Sports Med. 2016 Jun;44(6):1502–7. doi: 10.1177/0363546516629944. [DOI] [PubMed] [Google Scholar]
- 2.Solomonow M, Krogsgaard M. Sensorimotor control of knee stability A review. Scand J Med Sci Sports. 2001 Apr;11(2):64–80. doi: 10.1034/j.1600-0838.2001.011002064.x. [DOI] [PubMed] [Google Scholar]
- 3.Lephart SM, Pincivero DM, Giraldo JL, Fu FH. The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med. 1997;25(1):130–7. doi: 10.1177/036354659702500126. [DOI] [PubMed] [Google Scholar]
- 4.Beasley LS WD, Vidal AF, Chhabra A, Herzka AS, Feng MT, et al. Anterior cruciate ligament reconstruction: a literature review of the anatomy, biomechanics, surgical considerations, and clinical outcomes. Oper Tech Orthop. 2005;15:5–19. [Google Scholar]
- 5.Bonfim TR, Jansen Paccola CA, Barela JA. Proprioceptive and behavior impairments in individuals with anterior cruciate ligament reconstructed knees. Arch Phys Med Rehabil. 2003 Aug;84(8):1217–23. doi: 10.1016/s0003-9993(03)00147-3. [DOI] [PubMed] [Google Scholar]
- 6.Barrack RLL, Skinner H B. Knee joint proprioception revisited. Journal of Sports Medicine. 1994;3(1):18–43. [Google Scholar]
- 7.Riemann BL, Lephart SM. The Sensorimotor System, Part II: The Role of Proprioception in Motor Control and Functional Joint Stability. J Athl Train. 2002 Jan;37(1):80–4. [PMC free article] [PubMed] [Google Scholar]
- 8.Jiang L, Wang Y, Huang W. The effect of proprioception training on knee kinematics after anterior cruciate ligament reconstruction. Research Square. 2020 doi: 10.3233/BMR-210201. [DOI] [PubMed] [Google Scholar]
- 9.Becker BE. Aquatic therapy: scientific foundations and clinical rehabilitation applications. PM R. 2009 Sep;1(9):859–72. doi: 10.1016/j.pmrj.2009.05.017. [DOI] [PubMed] [Google Scholar]
- 10.Genuario SE, Vegso JJ. The use of a swimming pool in the rehabilitation and reconditioning of athletic injuries. Contemp Orthop. 1990 Apr;20(4):381–7. [PubMed] [Google Scholar]
- 11.Ross CA, Clifford A, Louw QA. Factors informing fear of reinjury after anterior cruciate ligament reconstruction. Physiother Theory Pract. 2017 Feb;33(2):103–14. doi: 10.1080/09593985.2016.1271847. [DOI] [PubMed] [Google Scholar]
- 12.Peultier-Celli LM D, Wein F. Comparison of an Innovative Rehabilitation, Combining Reduced Conventional Rehabilitation with Balneotherapy, and a Conventional Rehabilitation after Anterior Cruciate Ligament Reconstruction in Athletes. Front Surg. 2017;4:61. doi: 10.3389/fsurg.2017.00061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zamarioli A. The significance of water rehabilitation in patients with anterior cruciate ligament reconstruction. Physiotherapy. 2008;16(2) [Google Scholar]
- 14.Momberg BL. Accelerated hydrotherapy and land-based rehabilitation in soccer players after anterior cruciate ligament reconstruction: a series of three single subject case studies. South African Journal of Sports Medicine. 2008;20(4):109–14. [Google Scholar]
- 15.Boca IC, Mirela Dan. The effectiveness of proprioceptive neuromuscular facilitation techniques and hidrotherapy to improve knee stability after anterior cruciate ligament reconstruction. Br J Sports Med. 2013;47(10):e3–e. [Google Scholar]
- 16.Tovin BJ, Wolf SL, Greenfield BH, Crouse J, Woodfin BA. Comparison of the effects of exercise in water and on land on the rehabilitation of patients with intra-articular anterior cruciate ligament reconstructions. Phys Ther. 1994 Aug;74(8):710–9. doi: 10.1093/ptj/74.8.710. [DOI] [PubMed] [Google Scholar]
- 17.van Grinsven SvC. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010 Aug;18(8):1128–44. doi: 10.1007/s00167-009-1027-2. [DOI] [PubMed] [Google Scholar]
- 18.Beynnon BD. Proprioception and Neuromuscular Control in Joint Stability. Champaign: Human Kinetics; Validation of Techniques to Measure Knee Proprioception; pp. 127–138. [Google Scholar]
- 19.Pawlak D, Wysota A, Furmanek M, Ficek K, Juras G. Knee joint position sense in physically active patients after ACL reconstruction. Central European Journal of Sport Sciences and Medicine. 2014;7(3):65–72. [Google Scholar]
- 20.Olsson L, H Test/retest Reliability of a Knee Joint PositionSense Measurement Method in Sitting and Prone Position. Advances in Physiotherapy. 2004;6(1) [Google Scholar]
- 21.Von Korff M, Jensen MP, Karoly P. Assessing global pain severity by self-report in clinical and health services research. Spine (Phila Pa 1976) 2000 Dec;25(24):3140–51. doi: 10.1097/00007632-200012150-00009. [DOI] [PubMed] [Google Scholar]
- 22.Anderson AF. Evaluation of knee ligament rating systems. Am J Knee Surg . 1993:67–73. [Google Scholar]
- 23.Ebrahimzadeh MHM. The International Knee Documentation Committee (IKDC) Subjective Short Form: a validity and reliability study. Knee Surg Sports Traumatol Arthrosc. 2015 Nov;23(11):3163–7. doi: 10.1007/s00167-014-3107-1. [DOI] [PubMed] [Google Scholar]
- 24.Geigle PR. Aquatic physical therapy for balance: the interaction of somatosensory and hydrodynamic principles. The Journal of Aquatic Physical Therapy. 1997;5(1):4–10. [Google Scholar]
- 25.Benfield RD, Herman J, Katz VL, Wilson SP, Davis JM. Hydrotherapy in labor. Res Nurs Health. 2001 Feb;24(1):57–67. doi: 10.1002/1098-240x(200102)24:1<57::aid-nur1007>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]