Abstract
Men who have sex with men (MSM) are potentially at high risk for HIV infection, their HIV prevalence far exceeds the national prevalence rate. There are also a number of MSM who have sex with women, mostly unprotected, which can transmit HIV to their female sexual partners and even to the next generation. The purpose of this article is to evaluate the prevalence of heterosexual behaviors in Chinese men who have sex with men and the status of condom utilization as well as HIV infection among MSM with heterosexual behaviors, so as to further improve the investigation and prevention and control of AIDS in MSM population. We systematically searched China National Knowledge Infrastructure, Wanfang Data, VIP Database for Chinese Technical Calligraphy (VIP), Pubmed, and Embase following certain retrieval strategies to find relevant articles published from January 1, 2015 to November 18, 2019, The useful information extracted from qualified articles, Stata 15.1 and Review Manager 5.3 were employed for further meta analysis. The estimated prevalence of heterosexual behaviors among MSM in the past year was 19.0% (95% CI 17.0%, 22.0%). The estimated condom utilization rate of the last heterosexual behavior among MSM and condom adherence rate of heterosexual behaviors among MSM were 51.0% (95% CI 44.0%, 58.0%) and 31.0% (95% CI 25.0%, 38.0%), respectively. And the pooled HIV prevalence in MSM with heterosexual behaviors was 9% (95% CI 6%, 13%). The sensitivity analysis showed that the results were stable. No publication bias was found by Egger’s test. There is a high proportion of MSM with heterosexual behaviors and low condom utilization in China. HIV prevalence in MSM with heterosexual behaviors is also high. Therefore, adequate attention should be given to this particular group and measures should be taken in order to reduce the risk of transmission of HIV from subpopulations to the general population.
Keywords: Men who have sex with men, Heterosexual behavior, Condom use, HIV prevalence, Meta-analysis
Text
Introduction
Acquired immunodeficiency syndrome (AIDS) is an infectious disease with a high fatality rate caused by the human immunodeficiency virus (HIV). HIV destroys the body’s immune system, making infected people gradually lose their ability to fight off various diseases and eventually lead to death. There is no vaccine to prevent it and no effective drug to cure the disease. AIDS seriously endangers human health and hinders the stable development of society. “AIDS is not only a medical problem, but also a major public health problem, but also a serious social problem,“ the statement is accepted around the world. HIV infection varies markedly at national levels. Countries in southern sub-Saharan Africa had HIV prevalence rates of more than 10% in 2017. China’s overall HIV infection rate remains at a low level. It was estimated at 0.058 percent (0.046–0.070%) of the total population by the end of 2011. The total number of hiv-infected people reported to be alive accounted for 0.05% of the total population by the end of 2017. However, a high prevalence of HIV in confined areas, such as Yunnan and Guangdong, and specific groups ,such as drug users, MSM, in China [1]. It is worth noting that the positive rate of HIV antibody among MSM in China has been increasing rapidly in recent years,which was 3.0% in 2003, 5.7% in 2010, 7.3% in 2013 and 7.98% in 2015 [2]. MSM population is young and sexually active [3, 4], who usually have anal sex. Besides, anal sex is most likely to lead to the infection of HIV than vaginal sex because the anal mucosa is thin and prone to injury. MSM are characterized by multiple sexual partners and low condom utilization with their own social networks that are hard to get [5]. For these reasons, MSM forms the potentially high-risk group for HIV infection.
According to the report of Joint United Nations Programme on HIV/AIDS (UNAIDS), the key populations, including MSM and their sexual partners accounted for more than half (54%) of new HIV infections worldwide in 2018 [6]. It is reported by Several provinces in China that sexual transmission accounted for more than 90% of HIV infections and AIDS patients in 2019, and the constituent ratio of homosexual transmission varied from 6.5 to 75.66%, but this was higher than that of the previous years [7]. A certain number of MSM had or are having a sexual relation with women, which may transmit HIV to the female sexual partners and even to the next generation [8]. This study made a meta-analysis on the prevalence of heterosexual behaviors among MSM population, condom utilization and HIV prevalence in MSM population with heterosexual behaviors to understand the behavioral characteristics and HIV infection risk of MSM population with heterosexual behaviors, thereby providing a basis for targeted AIDS prevention and treatment among MSM population.
Method
Date sources and search strategy
Electronic databases such as CNKI, Wanfang, VIP, PubMed and Embase were searched on a systematic basis. The relevant studies published from January 1, 2015 to November 18, 2019 were retrieved from the above databases with the keywords and medical subject headings of “acquired immune deficiency syndrome”, “human immunodeficiency virus infection”, “MSM”, “bisexuality”, “bisexual men”, “MSMW”, and “men who have sex with men and women” .
Inclusion and exclusion criteria
The included studies were based on the following criteria: (1) cross-sectional studies or baseline studies in cohort studies; (2) participants were Chinese MSM who had oral or anal sex in the past year. (3) ages ≥ 16; (4) reported the outcome indicators, i.e. the prevalence of heterosexual behaviors among MSM in the past year, the condom utilization rate of the last heterosexual behavior among MSM, condom adherence rate of heterosexual behaviors among MSM or HIV prevalence in MSM with heterosexual behaviors, the above indicators could be calculated indirectly from the data given in studies. Exclusion criterias: (1) duplicated studies or studies based on the same data source; (2) reviews, news reports, and animal experiments; (3) post-intervention studies; (4) outcome indicators not reported; (5) Heterosexual behaviors recall windows of MSM population not reported or lasted for more than 1 year.
Study selection and data extraction
Two independent reviewers selected the articles based on the inclusion criteria, and extracted data on the first author, published year, year of study, study locations, setting, recall window of heterosexual behaviour among MSM, sampling method, survey method, sample size and reported outcome indicators with 95% confidence intervals (CIs). Moreover, we discussed any differences before reaching an agreement at last.
Quality assessment
AHRQ cross-sectional study evaluation standards were selected for the evaluation of the quality of the included studies, which consists of eleven items, specifically, a score of 1 represents “yes” and 0 refers to “no” or “unclear”. The total score is between 0 and 3, 4 and 7, as well as 8 and 11 respectively denotes “bad”, “satisfactory” and “good ” in terms of quality.
Statistical analysis
The prevalence of heterosexual behaviors among MSM and its 95% CIs extracted from studies were pooled by using the fixed-effect model or the random-effect model according to heterogeneity between studies. Similarly, a summary estimate was made for the condom utilization rate of last heterosexual behavior, condom adherence rate of heterosexual behaviors, and HIV prevalence in MSM with heterosexual behaviors.
The existence and degree of heterogeneity were detected by Cochran’s Q test and I2 statistical values. For the Q statistic, there was heterogeneity at P < 0.05; and in the case that the I2 statistic and I2 values are less than 25%, it indicates low heterogeneity, while the percentages of 50% and 75% indicate medium and high heterogeneity, respectively. If the results of the tests agree with the hypothesis of homogeneity, the fixed-effect model using inverse arcsine variance weights were used for the estimation of the overall prevalence across studies, otherwise random-effect model using DerSimoniane-Laird (D-L) weight would be used. The differences in prevalence reported in these studies may be due to differences in characteristics of the target population and the methodology. Therefore, an analysis on a subgroup of study locations, setting, sampling method, survey method, recall windows of heterosexual behaviors among MSM, sample size, study year was performed for the detection of potential sources of heterogeneity.
A sensitivity analysis was made by excluding one study at a time to check the stability of the outcomes and the sources of heterogeneity. The funnel plot was utilized to preliminarily judge whether there was publication bias, and further quantitative judgment was determined by Egger’s test. The statistical softwares of Stata version 15 and Review Manager version 5.3 were employed for further quantitative meta-analysis.
Results
Search and selection of studies
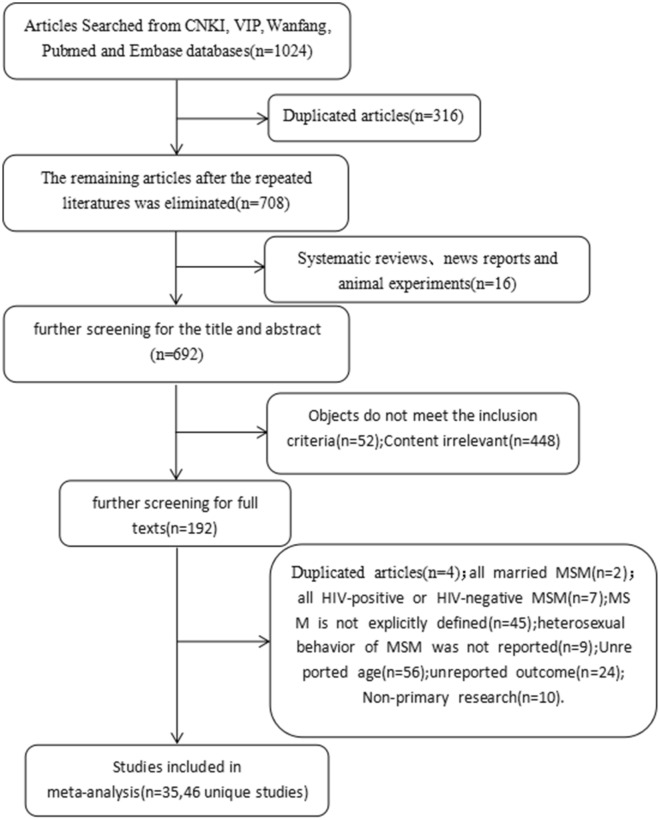
A total of 1024 articles were eventually retrieved from the above databases. After the elimination of duplicates, 708 articles were retained. These articles went through two stages of screening. In the first stage, by reading the titles and abstracts and excluding articles failed to meet the inclusion criteria, 192 articles were included in the second stage, of which the full text was required to be read the full text. After excluding the articles in which, for example, the participants were all HIV-infected or negative, or the cases were without reported outcome indicators; at last, a total of 35 articles (46 independent studies) were included in this meta-analysis (Fig. 1).
Fig. 1.
Flow chart of articles section for systematic review
There are 46 independent studies including 27,579 MSM, with the largest sample size of 2377 and the smallest one of 117. The studies covered 17 provinces or municipalities. In fact, 36.9% of the studies were conducted in the prosperous eastern China regions of Shanghai, Jiangsu, Zhejiang, Anhui, Fujian, Jiangxi and Shandong, respectively, and 23.9% of the studies were made in southern China, such as Guangdong, Guangxi and Hainan. The studies involved a variety of recruitment methods, such as working groups, MSM venues, non-governmental organizations (NGOs) and voluntary counseling and testing (VCT). Non-probability sampling was employed in these among studies, such as snowball sampling and convenience sampling. The surveys were mainly achieved by using face-to-face interviews and self-administered questionnaires, which were popular at present. For all the included studies, the descriptive characteristics are listed in Table 1, and the quality of included studies was evaluated as per through the AHRQ cross-sectional study evaluation standards with the scores shown in Table 1. The scores of all the included studies after evaluation ranged from 5 to 8 points, in another word, the quality of the included articles was of satisfactory or good.
Table 1.
The descriptive characteristics of included studies
| First author and Publication year | Study year | Study locations | Setting | Sampling method | Survey method | Recall windows(months) | Sample size | AHRQ score |
|---|---|---|---|---|---|---|---|---|
| Zhu, 2019-1[9] | 2015 | Guangdong | VCT | Not reported | Face-to-face | 6 | 520 | 5 |
| Zhu, 2019-2 [9] | 2016 | Guangdong | VCT | Not reported | Face-to-face | 6 | 516 | 5 |
| Zhu, 2019-3 [9] | 2014 | Guangdong | VCT | Not reported | Face-to-face | 6 | 163 | 5 |
| Zhu, 2019-4 [9] | 2015 | Guangdong | VCT | Not reported | Face-to-face | 6 | 357 | 5 |
| Zhu, 2019-5 [9] | 2016 | Guangdong | VCT | Not reported | Face-to-face | 6 | 344 | 5 |
| Yu, 2019-1 [10] | 2017 | Sichuan | Multiple recruitment methods | Not reported | Face-to-face | 6 | 410 | 5 |
| Yu, 2019−2 [10] | 2017 | Sichuan | Multiple recruitment methods | Snowball sampling | Face-to-face | 6 | 460 | 5 |
| Wu, 2019 [11] | Not reported | Guangdong | VCT | Snowball sampling + RDS | Face-to-face | 6 | 434 | 8 |
| Pan, 2019-1 [12] | 2015 | Guizhou | Multiple recruitment methods | Not reported | Face-to-face | 6 | 248 | 5 |
| Pan, 2019-2 [12] | 2016 | Guizhou | Multiple recruitment methods | Not reported | Face-to-face | 6 | 250 | 5 |
| Pan, 2019-3 [12] | 2017 | Guizhou | Multiple recruitment methods | Not reported | Face-to-face | 6 | 252 | 5 |
| Pan, 2019-4 [12] | 2018 | Guizhou | Multiple recruitment methods | Not reported | Face-to-face | 6 | 253 | 5 |
| Duan, 2019 [13] | 2016 | Shandong | Multiple recruitment methods | Snowball sampling | Face-to-face | 6 | 1306 | 5 |
| Ding, 2019 [14] | 2014 | Henan | MSM venues | Snowball sampling | Not reported | 6 | 205 | 5 |
| Zeng, 2019 [15] | 2016 | Guangxi | Social organization | Convenience sampling | Face-to-face | 6 | 375 | 6 |
| Wu, 2019 [16] | 2016–2017 | Hunan | Social organization | Not reported | Web based | 6 | 556 | 5 |
| Tang, 2018 [17] | 2013 | Zhejiang | Multiple recruitment methods | Convenience sampling | Face-to-face | 3 | 238 | 5 |
| Sun, 2018 [18] | 2015–2016 | Guangdong | Multiple recruitment methods | Snowball sampling | Self-administered | 6 | 334 | 6 |
| Hu, 2018 [19] | 2017 | Chongqing | MSM venues | Not reported | Face-to-face | 12 | 300 | 6 |
| Guo, 2018 [20] | 2013–2015 | Jiangsu | Multiple recruitment methods | Snowball sampling | Face-to-face | 6 | 1895 | 6 |
| Lin, 2017 [21] | 2013–2015 | Zhejiang | MSM venues | Convenience sampling | Face-to-face | 6 | 1399 | 5 |
| Guo, 2017 [22] | 2013–2015 | Jiangsu | Not reported | Snowball sampling | Face-to-face | 6 | 2377 | 6 |
| Wang, 2016 [23] | Not reported | Yunnan | NGO | Snowball sampling + RDS | Face-to-face | 6 | 557 | 5 |
| Qiu, 2016 [24] | 2012–2015 | Hubei | Not reported | Snowball sampling | Face-to-face | 6 | 1559 | 5 |
| Li 2016 [25] | 2014–2016 | Guangdong | MSM venues | TLS + Snowball sampling | Not reported | 6 | 801 | 5 |
| Lei, 2016 [26] | 2014 | Hunan | NGO | Snowball sampling RDS | Not reported | 6 | 604 | 6 |
| Gong, 2016 [27] | 2011–2015 | Shandong | MSM venues | Not reported | Face-to-face | 6 | 1350 | 6 |
| Du, 2016 [28] | Not reported | Jiangxi | Not reported | Not reported | Self-administered | 6 | 117 | 5 |
| Ding, 2016 [29] | 2014–2015 | Zhejiang | Working group | Snowball sampling + RDS | Face-to-face | 3 | 351 | 5 |
| Zhao, 2015 [30] | 2012–2014 | Liaoning | Not reported | Snowball sampling | Face-to-face | 6 | 1208 | 5 |
| Zhang, 2015 [31] | 2009 | Yunnan | Not reported | Snowball sampling | Face-to-face | 6 | 453 | 6 |
| Zhang, 2015 [32] | Not reported | Shanghai | Social organization | Snowball sampling | Face-to-face | 6 | 673 | 5 |
| Wang, 2015 [33] | 2013 | Liaoning | Not reported | RDS | Face-to-face | 6 | 900 | 5 |
| Wang, 2015 [34] | 2013–2014 | Shandong | Not reported | Not reported | Face-to-face | 6 | 408 | 5 |
| Tang, 2015 [35] | Not reported | Zhejiang | Multiple recruitment methods | RDS | Not reported | 3 | 238 | 5 |
| Sun, 2015 [36] | 2014 | Not reported | working group | non-probability sampling | Face-to-face | 6 | 524 | 5 |
| Ren, 2015 [37] | 2008–2009 | Shaanxi | Not reported | Snowball sampling | Not reported | 6 | 1365 | 5 |
| Peng, 2015 [38] | 2013–2014 | Guangdong | Not reported | Convenience sampling | Face-to-face | 6 | 369 | 6 |
| Long, 2015 [39] | 2014 | Guangdong | Multiple recruitment methods | Snowball sampling | Face-to-face | 6 | 421 | 5 |
| Li, 2015 [40] | Not reported | Heilongjiang | Multiple recruitment methods | Snowball sampling | Face-to-face | 6 | 400 | 5 |
| Gong, 2015-1 [41] | 2010 | Shandong | Multiple recruitment methods | Snowball sampling | Face-to-face | 6 | 310 | 5 |
| Gong, 2015-2 [41] | 2011 | Shandong | Multiple recruitment methods | Snowball sampling | Face-to-face | 6 | 350 | 5 |
| Gong, 2015-3 [41] | 2012 | Shandong | Multiple recruitment methods | Snowball sampling | Face-to-face | 6 | 402 | 5 |
| Gong, 2015-4 [41] | 2013 | Shandong | Multiple recruitment methods | Snowball sampling | Face-to-face | 6 | 364 | 5 |
| Gong, 2015-5 [41] | 2014 | Shandong | Multiple recruitment methods | Snowball sampling | Face-to-face | 6 | 329 | 5 |
| Chen, 2018 [42] | 2010–2017 | Zhejiang | Not reported | Non-probability sampling | Not reported | 6 | 334 | 5 |
Estimated prevalence of heterosexual behaviors among MSM
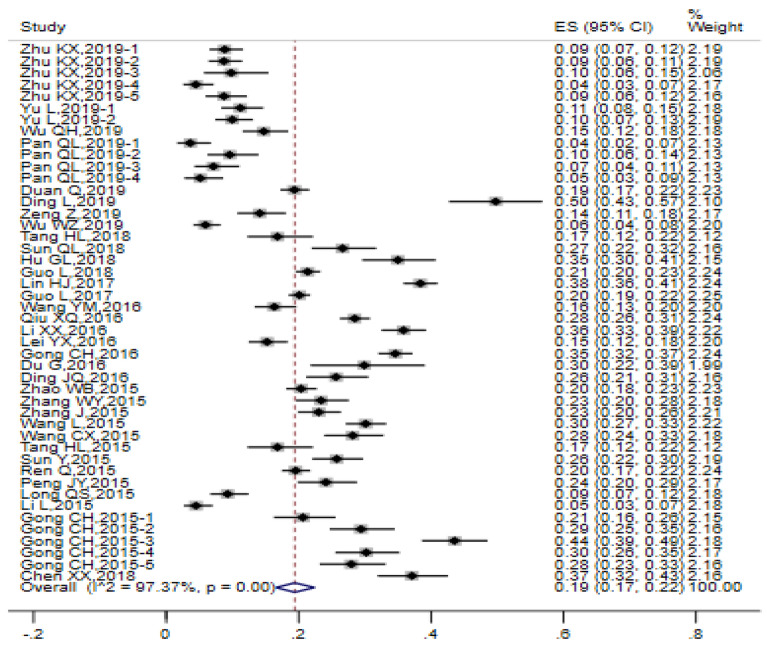
High heterogeneity was observed among the 46 studies (I2 = 97.37%, Q test P < 0.0001). D-L weight of random-effect model was employed for the estimation of the prevalence of heterosexual behaviors among MSM and the pooled prevalence was 0.19 (95% CI 0.17, 0.22). The forest chart is illustrated in Fig. 2.
Fig. 2.
Forest chart of the prevalence of heterosexual behaviors among MSM
Subgroup analysis
To explore the sources of heterogeneity in the prevalence of heterosexual behaviors among MSM, we conducted a subgroup analysis of the study locations, setting, sampling method, survey method, recall windows of heterosexual behaviors among MSM, sample size, and study year (Table 2). In general, heterogeneity remained almost unchanged after subgroup analysis, but the relevant information was still obtainable. The prevalence of heterosexual behaviors among MSM population in different regions was different, with the highest in eastern China (26.5%) followed by central China (20.6%), northwest China (19.4%), northeast China (15.3%), south China (13.0%) and southwest of China (11.5%). MSM recruited through MSM venues and working groups showed a higher prevalence of heterosexual behaviors than VCT (37.9%, 25.9% VS 9.1%). The subgroup analysis on the sampling method showed the prevalence of heterosexual behaviors among MSM recruited by respondent-driven sampling (RDS). Snowball sampling and convenience sampling were similar, respectively, i.e. 23.1%, 22.5% and 22.5%. The prevalence of heterosexual behaviors among MSM of the self-administered questionnaires was greater than that of face-to-face interviews (27.5% vs. 17.4%). In the studies with the recall windows of 6 months, the prevalence of heterosexual behaviors among MSM was higher than that in those with the recall windows of 3 months (35.1% vs. 20.6%). The subgroups with larger sample size showed higher rates of heterosexual behaviors than that of the subgroups with small sample size. The estimated prevalence of heterosexual behaviors among MSM of studies before 2016 was greater than that after 2016.
Table 2.
Subgroup analysis of heterosexual behavior in MSM population
| Variables | Subgroups | The number of studies | The prevalence of heterogeneity behaviors among MSM and 95% CI | I2 |
|---|---|---|---|---|
| Study locations | Northeast China | 3 | 15.3% (8.30%, 27.5%) | 98% |
| Northwest China | 1 | 19.4% (17.4%, 21.9%) | – | |
| East China | 17 | 26.5% (23.1%, 31.0%) | 96% | |
| Central China | 4 | 20.6% (9.90%, 37.9%) | 98% | |
| South China | 11 | 13.0% (8.30%, 20.0%) | 97% | |
| Southwest China | 9 | 11.5% (7.40%, 17.4%) | 97% | |
| Not reported | 1 | 26.0% (22.5%, 29.6%) | – | |
| setting | VCT | 6 | 9.10 (6.5%, 12.3%) | 79% |
| MSM venues | 5 | 37.9% (34.2%, 41.5%) | 79% | |
| Social organization | 3 | 13.0% (5.70%, 25.9%) | 97% | |
| NGO | 2 | 16.0% (13.8%, 18.0%) | 0% | |
| Working group | 2 | 25.9% (23.1%, 28.6%) | 0% | |
| Multiple recruitment methods | 18 | 15.3% (11.5%, 19.4%) | 96% | |
| Not reported | 10 | 25.4% (22.5%, 29.1%) | 92% | |
| Sampling method | Snowball sampling | 18 | 22.5% (18.7%, 25.9%) | 96% |
| RDS | 2 | 23.1% (12.3%, 38.7%) | 94% | |
| Snowball sampling + RDS | 4 | 17.4% (13.8%, 22.5%) | 86% | |
| Convenience sampling | 4 | 22.5% (13.0%, 36.3%) | 97% | |
| Not reported or other | 18 | 13.8% (9.9%, 19.4%) | 97% | |
| Survey method | Face-to-face | 37 | 17.4% (15.3%, 20.0%) | 97% |
| Self-administered | 21 | 27.5% (23.7%, 32.0%) | 0% | |
| Web based | 1 | 5.70% (3.80%, 8.30%) | – | |
| Not reported | 6 | 27.5% (18.7%, 38.3%) | 97% | |
| Recall windows | 3 momths | 3 | 20.6% (18.0%, 23.7%) | 79% |
| 6 months | 42 | 35.1% (23.7%, 24.8%) | 97% | |
| 12 months | 1 | 35.1% (29.6%, 40.5%) | - | |
| Sample size | < 500 | 29 | 17.4% (13.8%, 21.3%) | 96% |
| 500–1000 | 9 | 16.7% (11. 5%, 23.7%) | 97% | |
| 1000–1500 | 5 | 25.9% (18.7%, 34.6%) | 98% | |
| > 1500 | 3 | 23.1% (18.7% , 28.6%) | 95% | |
| Study year | 2016 ago | 26 | 25.9% (25.4% , 26.5% ) | 97% |
| Since 2016 | 11 | 16.7% (16.0% , 18.0%) | 97% | |
| Not reported or others | 9 | 25.4% (23.7 , 27.0%) | 96% |
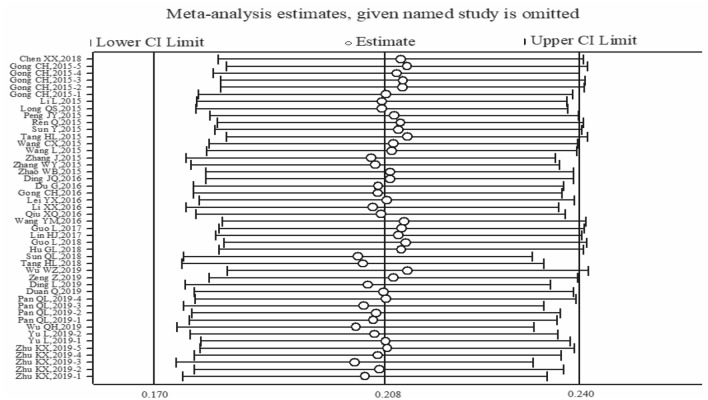
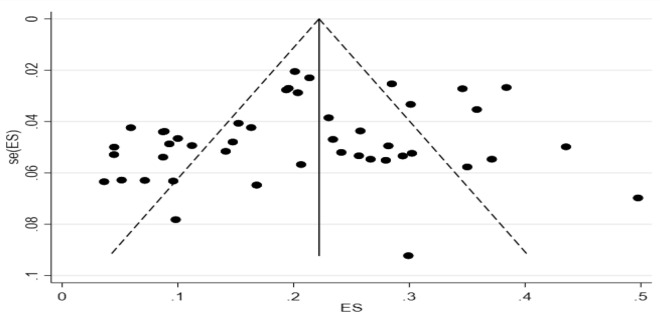
Sensitivity analysis and publication bias
It can be seen from the sensitivity analysis diagram that the included results were evenly distributed without significant deviation. The exclusion of a study at a time had no significant effect on the pooled prevalence, indicating that the aggregated results were robust and reliable. Figure 3 shows the sensitivity analysis diagram. The funnel plot in Fig. 4 is basically symmetrical, and further Egger’s test indicates that no publication bias was found in the study (P = 0.113 > 0.05).
Fig. 3.
Sensitivity analysis diagram of the prevalence of heterosexual behaviors among MSM
Fig. 4.
Funnel plot of ES, seES
Condom utilization and HIV prevalence in MSM with heterosexual behaviors
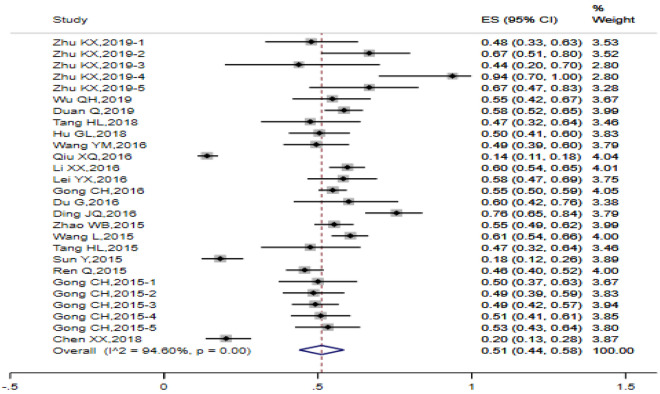
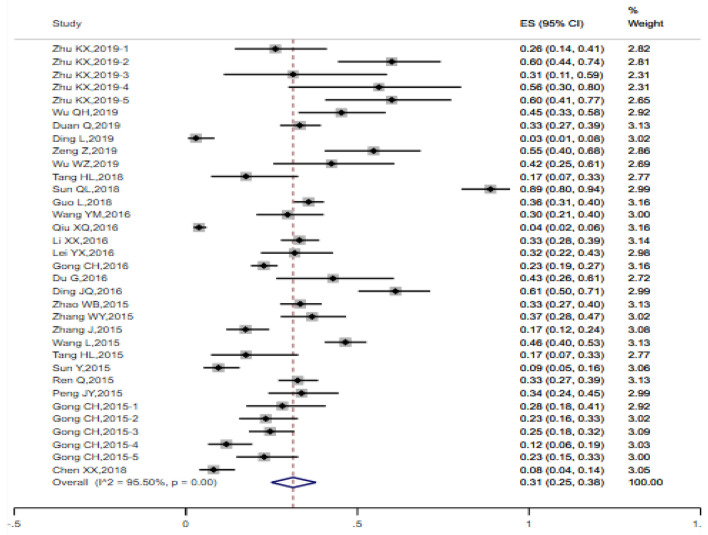
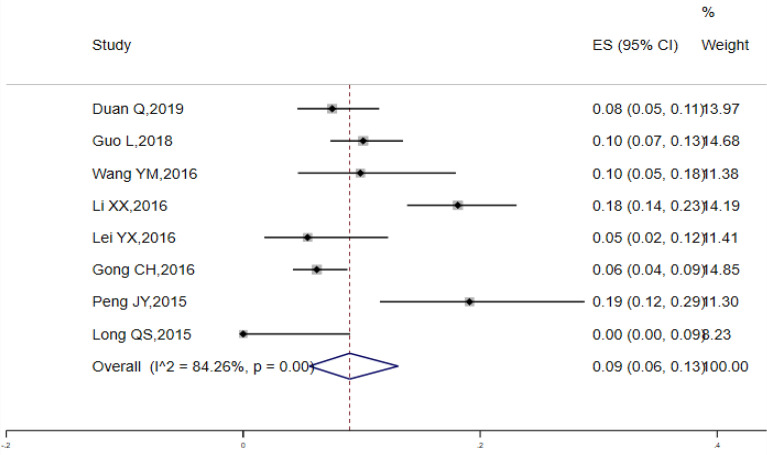
Random-effect model was employed to pool the condom utilization rate of the previous heterosexual behavior among MSM. The pooled rate among 27 studies was 0.51 (95% CI 0.44, 0.58) (I2 = 94.60%, Q test P < 0.0001) (Fig. 5). A total of 34 studies were incorporated into the analysis of condom adherence rate of heterosexual behaviors among MSM, with the estimated values 0.31 (95% CI 0.25, 0.38) (Fig. 6). The data obtained from 8 studies were included in the analysis of HIV prevalence in MSM with heterosexual behaviors and the estimated prevalence was 0.09 (95% CI 0.06, 0.13), There was a high degree of heterogeneity (I2 = 84.26%, Q test P < 0.0001) (Fig. 7).
Fig. 5.
Forest chart of the condom utilization rate of the last heterosexual behavior among MSM
Fig. 6.
Forest chart of condom adherence rate of heterosexual behaviors among MSM
Fig. 7.
Forest chart of HIV pevalence in MSM with heterosexual behaviors
Discussion
To learn Chinese MSM population with heterosexual behaviors, we systematically reviewed the cross-sectional studies on this population, and the summarized prevalence of heterosexual behaviors among MSM was 0.19 (95% CI 0.17, 0.22), which was lower than the results of meta-analysis made by K Yun et al. [43]. They systematically reviewed the relevant studies before 2011, and concluded that the prevalence of heterosexual behaviors among MSM was 0.31 (95% CI 0.28, 0.35). Similarly, it was lower than the research results of Asia 0.328 [44]. The reason may lie in the social development and progress, as well as the influence of western countries’ attitudes towards homosexuality, all of these factors have resulted in a higher level of awareness and acceptance of MSM among Chinese people, which thereby led to the improvement of MSM people’s social recognition and less discrimination, and in turn the substantially decrease of the prevalence of heterosexual behaviors. However, the absolute number of MSM with heterosexual behaviors in China’s booming population was still large.
The pooled condom utilization rate of the last heterosexual behavior and condom adherence rate of heterosexual behaviors among MSM as well as their 95% CIs were 0.51 (0.44, 0.58) and 0.31 (0.25, 0.38), respectively, indicating that condom utilization rate was low in MSM population during heterosexual behaviors. These could be explained by the fact that MSM had insufficient awareness of safe sex, and the misunderstanding that AIDS and other sexually transmitted diseases were still far away from them. Besides, they believed that using condoms meant distrust. Many MSM’s regular heterosexual partners were wives, and the abandonment of condoms was taken as part of the measures to avoid the revealing of sexual orientation. In addition, heterosexual behaviors at uncertain time and place by MSM made condoms unavailable. Some MSM even thought that condom utilization should be considered by women.
The estimated HIV prevalence in MSM with heterosexual behaviors was 0.09 (95% CI 0.06, 0.13), which was higher than the meta analysis results obtained by K Yun et al. [43] in 2011 and Hongyi Wang et al. [45] in 2015. This may be due to the fact that HIV was more prevalent among MSM with heterosexual behaviors than before or that MSM’s greater access to HIV testing and treatment has led to an increase in detection and life. The HIV prevalence in MSM with heterosexual behaviors was also higher than that among men who have sex with men only [46, 47], suggesting that heterosexual behavior was a potential risk factor for HIV infection among MSM population.
In view of the extreme heterogeneity observed, we performed a subgroup analysis of the prevalence of heterosexual behaviors among MSM, and obtained some information from each subgroup. The prevalence of heterosexual behaviors among MSM varied from region to region. Specifically, the prevalence of heterosexual behaviors among MSM in eastern China was higher than that of other regions because it is a coastal region with developed economy, as well as dense and complex population with high mobility. Heterosexuality was more common among MSM recruited in the MSM venues, such as bars, clubs and baths, providing convenience for them to exchange information, and acting as the first choice for non-local MSM to find partners with high population mobility. This reminded us to pay great attention to these places, and carry out targeted AIDS prevention and treatment operation. On the contrary, the prevalence of heterosexual behaviors among MSM obtained by VCT was lower than that obtained by MSM venues, which is because that only those with definite awareness and attention to AIDS would come for the voluntary counseling test. Due to the privacy and confidentiality involved in face-to-face inquiry of the sexual behaviors of the target population, the report rate of heterosexual behaviors of the respondents was lower than that of the self-administered questionnaire.
Heterogeneity was not reduced according to the subgroup analysis, suggesting that there were additional sources of heterogeneity. MSM population was a relatively hidden population, and it was not easy to get enough samples through traditional probability sampling. Instead, non-probability sampling, such as snowball sampling, convenient sampling, time and locations sampling was widely adopted. It was doubtful whether the subjectively selected samples could represent the target population. Moreover, the MSM population was a very complicated group, that is, the age, education, marriage, occupation and income, as well as the mobility would all subtly affect and change the cognition and behaviors of the MSM population. However, the included studies came from 17 provinces across the country, and the above features of samples obtained were different, which may be the possible sources of heterogeneity. Nevertheless, we were unable to obtain the above detailed information from the included studies. It is expected to make use of probability sampling or conduct further accurate research on MSM population with a certain demographic characteristics in the future, and even explore MSM’s potential network in cooperation with multiple departments, which also pose a challenge to our work.
As we known, MSM groups characterized by anal or oral sex are high-risk groups for HIV infection. In recent years, it has been noted that male homosexual transmission was contributing to the rapid rise of AIDS in schools [48]. Migrant workers contribute to another high incidence of male sexual behaviors. “Money buys” makes male sexual behaviors more common, and the flood of inappropriate cartoons has a great influence on adolescents, most of them were driven by curiosity and motivated by peers to have homosexual behaviors [49]. Moreover, many MSM groups have heterosexual behaviors with at least one woman, and have minimal awareness of condom utilization. Therefore, AIDS may spread from MSM groups to female partners, and even further cause mother-to-child transmission.
In this regard, following suggestions were given: (1) Sufficient attention should be paid to AIDS protection by the MSM population, and it is reported that less than 50% of key population is covered by joint prevention services, indicating that these strategic groups are still marginalized and backward in terms of the anti-aids process [6]. Fortunately, China has included the MSM population as one of the priority groups for HIV/AIDS sentinel surveillance. The regular detection of HIV in MSM is in line with the concept of “the earlier detection,the earlier treatment”. If HIV positive people in MSM receive effective antiviral treatment until the HIV viral load continues to be undetectable, they will not pass HIV to women through sexual contact. We have to ensure adequate funding for the service to this population, and strengthen the scientific research of this population by carrying out more comprehensive and targeted work. (2) When it comes to MSM, people immediately and subconsciously associate it with AIDS, syphilis, gonorrhea and other diseases, making it “stigmatized”. This will cause behavioral and emotional problems in MSM [50], which is clearly wrong. What MSM needs objective understanding of them, respect to their freedom of sexual orientation, improvement of social acceptance, and the implementation of anti-discrimination laws. The societal prejudice against MSM people should be eliminated, especially the discrimination from medical staff when they seek medical treatment. All these measures will make the MSM population transparent and easy to manage, thereby improving the efficiency of AIDS publicity and investigation work. (3) The promotion of condom utilization is a low-cost and high-benefit intervention for MSM or the general population that needs to be improved, which is able to eliminate the concept that “condom utilization is distrust between each other” [51]. The policy of “Four Frees and One Care” policy needs to be more widely propagated and accepted. Moreover, attention should be paid to the appropriate ways of publicity and education, such as the establishment of partnership with the news media. Studies have shown that peer education has a significant impact on the behavior improvement of MSM population [52]. (4) The central role of community in AIDS prevention and treatment of the MSM population should be strengthened, thereby making full use of the positive guiding role of community in MSM behaviors [53].
Limitations
This meta-analysis suffered certain limitations. At first, we did not search more studies by back-tracking references, which might leave out eligible studies. Secondly, the included studies were cross-sectional studies ones, and the demographic characteristics of the targeted population had a significant impact on the effect indicators, therefore, the inter-study heterogeneity was high. Moreover, the cross-sectional study failed to consider the sequence of time, which could not determine the causal relationship. In that case the risk of HIV prevalence in MSM with heterosexual behaviors has to be confirmed by abundant and high-quality cohort studies in the future. Thirdly, due to the limited availability of health resources, the heterosexual behaviors survey of MSM population in rural areas had not been paid enough attention and carried out. Therefore, the included studies were only limited to the urban areas, and the indicators obtained by the research could not represent the national situation.
Conclusions
To sum up, Chinese MSM population with heterosexual behaviors accounts for a large proportion. Their low condom utilization, soaring HIV infection and special sexual behaviors make them a high-risk group for HIV transmission. We should pay adequate attention to this special group and take measures to reduce their risk of HIV transmission from sub-population to the general population.
Acknowledgements
We appreciate all the people who helped us with this work.
Authors’ contributions
The authors’ responsibilities were as follows: HZ and XL conceived the study and designed the search strategy; HZ, XL, JW, WW, CY, JL, XL, RP, LC, XZ and JZ conducted the study selection, data extraction, the data analysis and interpretation of results, and evaluated the risk of bias of included studies; HZ and XL wrote the first draft of the manuscript; PL and JZ revised the manuscript. All authors read and approved the final version of the manuscript.
Funding
We have no funding information.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xi Li—Joint first author
Huan Zhao and Xi Li contributed equally to this paper
Contributor Information
Peng Luo, Email: luopeng@gmc.edu.cn.
Jiangping Zhang, Email: jiangpingzhang@126.com.
References
- 1.Jie Z, Xianhua W. Research on characteristics of AIDS epidemic and prevention and health education strategies. Med Inform Med Comput Appl. 2014;14:468. [Google Scholar]
- 2.Ministry of health of the People’s Republic of China, Joint United Nations Programme on HIV AIDS (UNAIDS), World Health Organization 2011 China HIV/AIDS epidemic estimates. China AIDS Venereal Dis. 2012;18(1):1–5. [Google Scholar]
- 3.Lin C, Wende C, Jingguang T, Xiaobing W, Xiangdong S, Jing Z, et al. Analysis on monitoring situation of sentinel sites of male sex workers in shenzhen in 2007. Chin J AIDS & STD. 2009;4:418–9. [Google Scholar]
- 4.Jing T, Jinchuan Y, Xiling Y. A survey of HIV, syphilis and HCV amalgamative infection among MSM in Xuzhou. Chin J Health Lab Technol. 2012;10:2491–2492. [Google Scholar]
- 5.Yuesheng Q, Jihua F, Xiaofei Z, Cuixia L, Xiaoguang S. Qualitative investigation on AIDS related information among MSM. Modern Prev Med. 2007;34(17):3281–2. [Google Scholar]
- 6.Joint United Nations Programme on HIV/AIDS (UNAIDS) Community engagement—Global AIDS update 2019. Geneva: Eshove; 2019. [Google Scholar]
- 7.China Red Chain net. Summary of HIV/AIDS epidemic in some provinces and cities in China in 2019. http://www.chain.net.cn/info_view/13249/.
- 8.Jixue W, Wei T, Rui L, Zhijie Z, Bangjie X, Jun G, et al. Investigation on HIV, STD serum and behaviors of Men who have sex with men. Chin J Public Health. 2004;20(11):1377–8. [Google Scholar]
- 9.Kaixing Z, Meizhen X, Ye S, Hongli H. Analysis of influencing factors on condom use among men who have sex with men in Haizhu District, Guangzhou. Chin Prim Health Care. 2019;33(02):66–9. [Google Scholar]
- 10.Lin Y, Yuling H, Tian X, Bingzhi Z, Xiaoqing H, Min H, et al. Analysis of high-risk behavior characteristics of men who have sex with men in different regions of chengdu. J Prev Med Inform. 2019;35(09):1009–13. [Google Scholar]
- 11.Qiuhong W, Weiying C, Yi D, Qing Z, Wenhui C, Lanlan Y, et al. Co-infection of syphilis and HIV and risk factors among men who have sex with men in Shenzhen. China J Leprosy Skin Dis. 2019;35(07):394–7. [Google Scholar]
- 12.Qingli P, Jian Z, Yan Z, Fei Y, Min S, Jing L. Analysis on HIV infection status and sexual behavior characteristics of men who have sex with men in guiyang from 2015 to 2018. Chin J AIDS STD. 2015;2019(8):812–815. [Google Scholar]
- 13.Qing D. Investigation and study on the status of new drug abuse and HIV and syphilis infection among men who have sex with men in shandong province. Shandong: University of Jinan; 2019. [Google Scholar]
- 14.Lin D, Xiaojian W, Tao Z, Shifu W, Qianchao L. Evaluation of AIDS prevention intervention effect and analysis of influencing factors of MSM population in nanyang city from 2014 to 2018. Henan J Prev Med. 2019;30(09):681–4. [Google Scholar]
- 15.Zi Z, Zhi L, Jianbiao L, Xueqiong C, Dongrui H, Juan Z, et al. Analysis on condom use and influencing factors of men who have sex with men in some areas of Guangxi. China Trop Med. 2019;19(04):343–7. [Google Scholar]
- 16.Wu W, Xiaochen Y, Xiaoxia Z, Goldsamt L, Yuanyuan C, Daoping H, et al. Potential HIV transmission risk among spouses: marriage intention and expected extramarital male-to-male sex among single men who have sex with men in Hunan, China (published online ahead of print, 2019 Jun 6). Sex Transm Infect. 2019; sextrans-2018-053906. [DOI] [PMC free article] [PubMed]
- 17.Tang HL. Status of HIV/AIDS knowledge and behaviors and evaluation of the effects of regular follow-up interventions among men who have sex with men in Jinhua City. Zhejiang: Zhejiang university; 2018. [Google Scholar]
- 18.Qunlu S, Yushan Tu, Bing Q, Zheng Z, Zhanhong R, Fang F. High-risk behaviors and HIV infection among men who have sex with men in Baoan district of Shenzhen. Chin J AIDS STD. 2018;24(6):573–5. [Google Scholar]
- 19.Guilin H, Qiang W, Xiangdong L, Zhen Z. Analysis of the status of AIDS infection and its influencing factors in Site type MSM population in a district of Chongqing. J Modern Med Health. 2018;34(21):3283–6. [Google Scholar]
- 20.Lu G, Min Z, Zhengping Z. Characteristics and influencing factors of heterosexual intercourse among MSM in Nanjing City. Chin J Health Educ. 2018;34(04):325–9. [Google Scholar]
- 21.Haijiang L, Yucheng Z, Weiwei S, Qionghai W, Yuanyuan X, Danhong Q, et al. Investigation of group sex in men who have sex with men in Taizhou, Zhejiang province, 2013–2015. Chin J Epidemiol. 2017;38(5):634–7. doi: 10.3760/cma.j.issn.0254-6450.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 22.Lu G, Min Z, Li L, Yuanyuan X, Sushu W, Xin L, et al. Sexual behavior and HIV/syphilis infection among MSM with different sexual roles in Nanjing. Chin J AIDS STD. 2017;23(3):232–5. [Google Scholar]
- 23.Yumiao W, Renzhong Z, Youfang L, Jue W, Zhiqing L, Ling W, et al. Sexual features of heterosexual intercourse and HIV situation among men having sex with men in Kunming. Chin J Dis Control Prev. 2016;20(6):539–42. [Google Scholar]
- 24.Xingqing Q, Jing Z, Lili M, Wensheng G, Deyong C. Factors influencing newly identified HIV infection among MSM in Xiangyang City. Pract Prev Med. 2016;23(09):1066–9. [Google Scholar]
- 25.Li X, Wende C, Qingping L, Xianqing X, Peilan Q, Xiaoyan C, et al. Factors influencing heterosexual behavior and frequency of condom use among MSM population in longgang district, Shenzhen. J Public Health Prev Med. 2016;27(4):113–115. [Google Scholar]
- 26.Yunxiao L, Xueling X, Honghong W, Jia C, Xianhong L. Characteristics and associated factors of heterosexual behavior among men who have sex with men in Changsha. J Nurs Sci. 2016;31(09):93–6. [Google Scholar]
- 27.Cuihua G, Chunzi S, Xuhong Y, Feng C, Chao H. HIV and TP infection status and its influencing factors among men who have sex with men at urban areas of Zibo city. Chin J AIDS STD. 2016;22(9):743–6. [Google Scholar]
- 28.Gang D, Rongrong Y, Xuemei G, Meizhu L. Survey on awareness rate of AIDS related knowledge and the high risk sexual behavior among MSM in Ganzhou City. J Gannan Med Univ. 2016;36(01):117–9. [Google Scholar]
- 29.Jianqiang D, Wenmin Y, Qingwei Y, Yafen Z, Jumin L, Qiongshan X. Investigation on AIDS knowledge and behavior among men who have sex with men in Zhenhai District. J Prev Med. 2016;28(8):825–6. [Google Scholar]
- 30.Wenbin Z, Qiuju S, Chunhong J. Prevalence and influencing factors of HIV infection among MSM in An’shan City from 2012–2014. Occup Health. 2015;31(22):3120–2. [Google Scholar]
- 31.Wanyue Z, Renzhong Z, Jue W, Ling W, Songfeng P, Youfang L, et al. HIV infection and its influential factors among men who have sex with men in Kunmin. Chin J Dis Control Prev. 2015;19(2):203–5. [Google Scholar]
- 32.Jing Z, Rong P, Kun C, Jiangnan H, Xian T, Cuiqing L, et al. Evaluation of AIDS/STD comprehensive interventions program among men who have sex with men in Shanghai. Chin J AIDS STD. 2015;21(01):44–7. [Google Scholar]
- 33.Wang L, Nan Y. Survey on knowledge and behavior about HIV/AIDS and HIV infection rate among men who have sex with men of different educational level in Shenyang City. Occup Health. 2015;31(03):339–41. [Google Scholar]
- 34.Chunxue W, Xuejin Z, Xiaoli G, Tongliang Z. Survey on high-risk Behavior characteristics and psychological factors among men who have sex with men in Linqu. Prev Med Tribune. 2015;21(08):632–3. [Google Scholar]
- 35.Huiling T, Yueqiang Hu, Tao Z. HIV infection and its influencing factors in baseline cohort survey of men who have sex with men in jinhua city, zhejiang province. Chin Rural Health Serv Admin. 2015;35(04):477–80. [Google Scholar]
- 36.Yang S. Study on high-risk sexual behavior, quality of life and social support in MSM population. Shandong: Dalian Medical University; 2015. [Google Scholar]
- 37.Qiang R, Guihua Z, Wenhui C. Investigation on the risk factors of HIV infection among men who have sex with men in xi'an city. China Prev Med. 2015;16(9):733–735. [Google Scholar]
- 38.Jingyu P, Fuchang H, Yumao C, Mingzhou X, Xue H, Lina L, et al. The interaction between risk factors associated with HIV infection among men having sex with men. Chinese J AIDS STD. 2015;21(02):132–7. [Google Scholar]
- 39.Qisui L. Investigation and scale estimation of HIV/AIDS status among active men who have sex with men in zhanjiang city. Guangdong: Jinan University; 2015. [Google Scholar]
- 40.Lin L, Jingli S, Simao W. Analysis of the influencing factors of HIV infection in MSM population of Qigihar City. China Health Industry. 2015;12(21):180–2. [Google Scholar]
- 41.Cuihua G, Xuhong Y, Chunzi S, Lei W, Xiaohan M, Feng C. AIDS sentinel surveillance among men who have sex with men, Zibo city, 2010–2014. Prev Med Tribune. 2015;21(10):786–78,719. [Google Scholar]
- 42.Xiaoxiao C, Xiaotong Q, Weiwei S, Yanling W, Yuanyuan X, Haijiang L, et al. Sentinel surveillance on HIV status and related factors among men who have sex with men above 50 years in Taizhou Prefecture from 2010 to 2017. Shanghai J Prev Med. 2018;30(12):980–5. [Google Scholar]
- 43.Yun K, Xu JJ, Reilly KH, Jiang YJ, Wang N, Zhang J, et al. Prevalence of bisexual behaviour among bridge population of men who have sex with men in China: a meta-analysis of observational studies. Sex Transm Infect. 2011;87(7):563–70. doi: 10.1136/sextrans-2011-050079. [DOI] [PubMed] [Google Scholar]
- 44.Bowring AL, Veronese V, Doyle JS, Stoove M, Hellard M. HIV and sexual risk among men who have sex with men and women in Asia: a systematic review and meta-analysis. AIDS Behav. 2016;20(10):2243–65. doi: 10.1007/s10461-015-1281-x. [DOI] [PubMed] [Google Scholar]
- 45.Wang HY, Xu JJ, Zou HC, Reilly KH, Zhang CM, Yun K, et al. Sexual risk behaviors and HIV infection among men who have sex with men and women in China: evidence from a systematic review and meta-analysis. Biomed Res Int. 2015;2015:850132. doi: 10.1155/2015/850132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhongrong Y, Meihua J, Zhengquan D, Zhang S, Qiu Z. Prevalence of HIV among men who have sex with men of inland high school and college students in China: a meta-analysis. J Hygiene Res. 2012;18(1):1–5. [PubMed] [Google Scholar]
- 47.Yingpeng Q, Aizhong L, Tiejian F. HIV/syphilis infections, sexual behaviors and awareness of HIV/AIDS knowledge among men who have sex with men in the mainland of China: a meta-analysis. Chin J AIDS STD. 2013;19(3):169–173. [Google Scholar]
- 48.National Health and Family Planning Commission of PRC The establishment of a notification system to further strengthen the school AIDS prevention and control work. Chin Pract J Rural Doctor. 2015;22(19):9. [Google Scholar]
- 49.Ru L. Analysis on the prevalence and influence of Rotten culture. Shanghai: East China Normal University; 2018. [Google Scholar]
- 50.Baoshan Z, Guoliang Y. Stigma phenomenon and its psychological effects. Adv Psychol Sci. 2007;15(06):993–1001. [Google Scholar]
- 51.Halkitis PN, Parsons JT, Wilton L. Barebacking among gay and bisexual men in New York City: explangtions for the emergence of intentional unsafe behavior. Arch Sex Behav. 2003;32(4):351–7. doi: 10.1023/A:1024095016181. [DOI] [PubMed] [Google Scholar]
- 52.Xing Z, Pengfei G, Xiaosong L. Meta analysis of effects of interventions for preventing HIV/AIDS among MSM in China. Modern Prev Med. 2010;37(19):3603–3607. [Google Scholar]
- 53.Qin Z. The function of city community in the prevention of HIV/AIDs. J Sichuan Univ (Social Science Edition). 2007;4:113–117. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.