Abstract
Background
Left atrial (LA) size and function are known predictors of new onset atrial fibrillation (AF) in hypertrophic cardiomyopathy (HCM) patients. Components of LA deformation including reservoir, conduit, and booster function provide additional information on atrial mechanics. Whether or not LA deformation can augment our ability to predict the risk of new onset AF in HCM patients beyond standard measurements is unknown.
Methods
We assessed LA size, function, and deformation on cardiovascular magnetic resonance (CMR) in 238 genotyped HCM patients and compared this with twenty age, sex, blood pressure and body mass index matched control subjects. We further evaluated the determinants of new onset AF in HCM patients.
Results
Compared to control subjects, HCM patients had higher LA antero-posterior diameter, lower LA ejection fraction and lower LA reservoir (19.9 [17.1, 22.2], 21.6 [19.9, 22.9], P = 0.047) and conduit strain (10.6 ± 4.4, 13.7 ± 3.3, P = 0.002). LA booster strain did not differ between healthy controls and HCM patients, but HCM patients who developed new onset AF (n = 33) had lower booster strain (7.6 ± 3.3, 9.5 ± 3.0, P = 0.001) than those that did not (n = 205). In separate multivariate models, age, LA ejection fraction, and LA booster and reservoir strain were each independent determinants of AF. Age ≥ 55 years was the strongest determinant (HR 6.62, 95% CI 2.79–15.70), followed by LA booster strain ≤ 8% (HR 3.69, 95% CI 1.81–7.52) and LA reservoir strain ≤ 18% (HR 2.56, 95% CI 1.24–5.27). Conventional markers of HCM phenotypic severity, age and sudden death risk factors were associated with LA strain components.
Conclusions
LA strain components are impaired in HCM and, together with age, independently predicted the risk of new onset AF. Increasing age and phenotypic severity were associated with LA strain abnormalities. Our findings suggest that the routine assessment of LA strain components and consideration of age could augment LA size in predicting risk of AF, and potentially guide prophylactic anticoagulation use in HCM.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12968-021-00793-6.
Keywords: Hypertrophic cardiomyopathy, Atrial fibrillation, Cardiovascular magnetic resonance imaging, Left atrial strain, Booster strain, Reservoir strain
Background
At least 1 in 5 patients with hypertrophic cardiomyopathy (HCM) are affected by atrial fibrillation (AF) [1], the development of which heralds an unfavourable prognosis and is associated with a significantly higher all-cause mortality due to an increased risk of heart failure and stroke [1]. Current guidelines for HCM recommend a 48-h ambulatory Holter monitor every 2 years [2], though this may be inadequate for detecting new onset AF [3]. Lifelong anti-coagulation is recommended once AF is detected as cardioembolic risk is especially high in HCM. However, given the limitations of intermittent monitoring, anticoagulation sometimes follows an embolic complication. Therefore, the initiation of anti-coagulation therapy is clearly desirable when AF is anticipated.
Previous work has identified predictors for new onset AF in HCM. These include age [4], left atrial (LA) diameter [5], indexed LA end-diastolic volume (LAEDV) [6], and more recently, LA function [7]. However, contemporary guidelines have been slow to incorporate these biomarkers into the routine clinical management of HCM patients. Currently, the American Heart Association (AHA) recommends Holter monitoring for AF if a patient complains of palpitations [8]. The European Society of Cardiology (ESC) recommends intensification of arrhythmia surveillance when the anterior–posterior diameter of the LA exceeds 45 mm on echocardiography [2]. Specific recommendations for prophylactic anticoagulation are lacking and clinicians may initiate therapy once atrial diameter exceeds a given size in anticipation of AF. However, studies are emerging that show previously reported thresholds for LA size may be too conservative; with 59% of AF cases in one study occurring in patients with LA diameter < 45 mm [7]. More refined markers that determine AF risk are therefore clearly required.
The role of LA volume and diameter in predicting AF onset in HCM is well established. However, studies assessing the link between LA function and AF risk are limited. Determinants of LA function in HCM are complex and may include direct, myopathic aspects (where the mutant sarcomeric protein is expressed in atrial muscle) as well as secondary hemodynamic forces relating to increased atrial pressures in outflow obstruction, mitral regurgitation and diastolic dysfunction [9, 10]. LA function can be assessed using LA ejection fraction (LAEF) and/or LA deformation analysis on 2-dimensional (2D) cardiovascular magnetic resonance (CMR) feature tracking such as LA strain. LA strain consists of reservoir, conduit, and booster components. Whilst LA conduit strain is derived from the motion of atrial tissue during passive ventricular filling, LA reservoir strain and booster strain reflect passive and active LA functions, respectively [11, 12]. Comprehensive studies in HCM patients examining the association between AF and LA reservoir, conduit, and booster strain parameters on (CMR are lacking, yet LA strain components are emerging as sensitive markers for detecting impairment in LA function [13–17].
In this work, we set out to test the hypothesis that LA reservoir and booster strain on CMR will improve our ability to predict risk of incident AF. We further examined the determinants of LA strain components in HCM patients.
Methods
Study population and protocol
This is a retrospective analysis of data from an observational study approved by a local ethics committee (Reference: 07/Q1607/66, 12/LO/ 1979). Patients were recruited from the Inherited Cardiac Conditions (ICC) study at the University of Oxford between 2003 and 2016. As per the ESC diagnostic criteria, the recruitment for this study captured patients with genetically diagnosed or familial HCM who had wall thickness ≥ 13 mm [2], or non-familial HCM patients with wall thickness ≥ 15 mm but no other cause of hypertrophy identified. Genetic diagnosis used a minimum of 13-gene testing and patients were stratified based on genotype status (see Additional file 1 for details). Baseline characteristics including symptoms, comorbidities, and medications were retrieved from clinic letters. Patients with any history of AF at the time of CMR were excluded from this study. This exclusion was implemented after reviewing clinic letters and the results of a 24–48 h Holter carried out on each patient. Patients taking amiodarone were excluded. Patients with coronary artery disease, moderate to severe aortic stenosis, HCM phenocopies (amyloidosis, Fabry diseases, Danon disease), or contraindications to CMR were also excluded.
Twenty age, sex, blood pressure and body mass index (BMI) matched healthy subjects from another ethically approved study [18] provided normal values in light of potential variability in published normal ranges arising from inter-vendor strain differences. These healthy controls were free of known cardiovascular disease or family history of cardiac disease and were screened for AF on a 12-lead electrocardiogram (ECG). LA data (size, function, and strain) from age, sex and BMI matched controls were also specifically included to define the extent of impairment in LA strain components between HCM and non-HCM subjects.
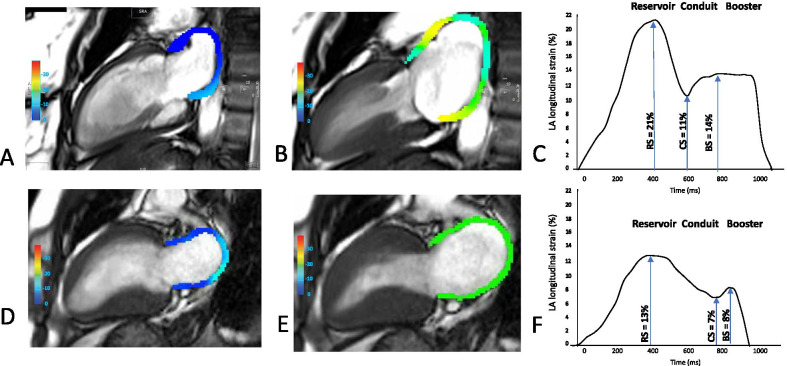
Cardiovascular magnetic resonance
CMR image acquisition including cine and late gadolinium enhancement (LGE) used established methods (see Additional file 1 for details). cvi42 software (Circle Cardiovascular Imaging Inc, Calgary, Alberta, Canada) was used as per established methods to assess left ventricular (LV) volume, function, mass and wall thickness and LA anterior–posterior diameter in the LV outflow tract (LVOT) view [19]. As previously described, LAEDV index, indexed LA end-systolic volume (LAESV), and LAEF were assessed from the horizontal and vertical long axis views [20, 21]. Similarly, LA peak longitudinal reservoir, conduit and booster strain were assessed using an automated tracking algorithm [22] (see Additional file 1 for details). 2-D feature-tracking strain analysis was averaged across the horizontal and vertical long axis views to derive strain components from cine images. Figure 1 depicts the aspect of this derivation from the vertical long axis. The LA image analysis was performed by an observer (RS) blinded to the clinical information or outcomes. LGE analysis was undertaken by setting the signal intensity threshold at six standard deviations above the mean intensity of a reference region of myocardium that had no visual evidence of enhancement [20].
Fig. 1.
Left atrial longitudinal strain components in health and hypertrophic cardiomyopathy. Illustrative example of left atrial (LA) strain assessed in the vertical long axis view at the end of diastole using cardiovascular magnetic resonance (CMR) tissue tracking analysis from a healthy control subject and hypertrophic cardiomyopathy (HCM) (A, D). Peak LA longitudinal strain in the same control subject and HCM, respectively (B, E). Graph demonstrating the three functional elements of LA deformation in a healthy control subject (C). Graph demonstrating the three functional elements of LA deformation in a HCM patient (F)
Clinical follow up
Patients in the Inherited Cardiac Conditions study, from which this study recruited, were followed up on a yearly basis either in clinic, or with a phone interview, and review of medical records and clinical letters if not followed-up in Oxford. The median follow-up time of those in this study was of 4.5 years. Follow-up was in line with clinical practice and consisted of a clinical visit and assessment, a 12-lead ECG, and 24–48 h Holter (2-yearly). The primary endpoint for this study was new onset AF, defined as an irregularly irregular heart rhythm with absent P-waves documented on a 12-lead ECG or 24–48 h Holter.
Statistical analysis
Statistical analysis utilised R (version 3.5.0, R Foundation for Statistical Computing, Vienna, Austria). Packages used were: Survival, pROC, and time ROC. Normality of data was assessed by the Shapiro–Wilk and Anderson–Darling tests, visual inspection of quantile–quantile plots, and consideration for skew and kurtosis values. Mean (standard deviation/SD) and Median [Interquartile range/IQR] are presented accordingly for normally- and non-normally distributed data, respectively. Independent t-tests and Mann–Whitney tests were used for normally- and non-normally distributed data, respectively. Categorical variables are summarised as proportions (%) and the χ2 (with continuity correction) or Fisher’s exact tests were used to compare proportions. Inter- and intra-observer variability of strain measurements was determined by the interclass correlation coefficient, and coefficient of variation.
Stratification of the main LA parameters was based on the optimal thresholds (cut-off values) of these variables for predicting new onset AF, as calculated using Youden's index in conjunction with standard Receiver Operator Characteristic (ROC) analysis. For clinical applicability we rounded these thresholds.
Time-dependent ROC estimations were used to calculate C-statistics (concordance statistics), equivalent to the area under a ROC curve (AUC) and representative of the accuracy of a single value in the diagnosis of new onset AF at 3 years.
Univariate Cox proportional hazard regression analysis was performed to identify predictors of new onset AF. Relative risks were presented as hazard ratios (HR) with 95% confidence intervals (CI). Where appropriate, the proportional hazards assumption, presence of outliers, and linearity were tested for. Parameters under a significance threshold of P < 0.05 were included in the Cox multiple regression analysis. Kaplan–Meier cumulative survival curves free of AF were constructed for LA reservoir and booster strain values stratified by the rounded cut-offs. The survival curves were compared with the log-rank test. Simple linear and multiple regression was used to determine the variables that associate with LA strain. Unless adjustments were made for multiple tests, a p-value of P < 0.05 was considered significant throughout, and all tests were 2-sided.
The Bonferroni correction was applied selectively to the analysis in Table 1 and to the parameters included in the univariate Cox proportional hazard regression analysis to adjust ‘family-wise’ error rates in multiple comparisons of related groups and reduce the risk of type I error, whilst acknowledging the conservative nature of the correction. Correction was applied to the parameters relating to the LA (10 parameters in Table 1, giving an adjusted P of 0.05/10 = P < 0.005, and 15 parameters in the univariate analysis, giving an adjusted P of 0.05/15 = P < 0.0034), and separately to those relating to the LV (7 parameters in both analyses, giving an adjusted P of P < 0.0071). In the univariate analysis correction was also applied to the remaining baseline, clinical and medication parameters (28 parameters giving an adjusted P of P < 0.0018). By contrast the Bonferroni correction was not applied to the simple linear regression for the determinants of LA strain. This decision was made as this aspect of the study involved post-hoc testing of unplanned comparisons that we deem as hypotheses for further exploratory investigation and so avoiding a type II error was of greater importance [23].
Table 1.
Baseline and CMR data: ‘controls vs HCM’; ‘No new onset AF vs new onset AF’
| Control subjects (n = 20) | HCM population, n = 238 | P value | New onset AF (n = 33) | No new onset AF (n = 205) | P value | |
|---|---|---|---|---|---|---|
| Baseline and clinical | ||||||
| Age at CMR scan | 48 [37, 64] | 54 [43, 63] | 0.362 | 61 [55, 66] | 53 [41, 61] | 0.001* |
| Men, n, % | 15, 75 | 184, 77 | 1 | 25, 76 | 159, 78 | 0.824 |
| Body mass index | 26.6 [23.4, 27.8] | 27.5 [24.6, 30.3] | 0.145 | 28.5 [25.7, 30.8] | 27.2 [24.5, 30.7] | 0.129 |
| Body surface area | 1.9 (0.2) | 2.0 (0.3) | 0.276 | 2.1 [1.8, 2.2] | 2.0 [1.8, 2.2] | 0.51 |
| Systolic blood pressure (mmHg) | 128 (13.3) | 131 (18.5) | 0.558 | 130 (14.8) | 131 (19.2) | 0.968 |
| Diastolic blood pressure (mmHg) | 72 (8.0) | 77 (10.3) | 0.077 | 78 (9.7) | 77 (10.4) | 0.586 |
| Hypertension, n, % | 4, 20 | 99, 42 | 0.479 | 18, 55 | 81, 40 | 0.130 |
| Mitral regurgitation class, %: no mitral regurgitation, 1, 2, 3, 4 | 0, 0, 0, 0, 0 | 71, 17, 7, 6, 0 | – | 73, 3, 15, 9, 0 | 71, 19, 5, 5, 0 | 0.014* |
| SCD score: ESC guidelines | N/A | 2.0 (1.6) | – | 2.3 (1.8) | 2.0 (1.4) | 0.273 |
| VT historical, n, % | N/A | 12, 5 | – | 5, 15 | 7, 3 | 0.015* |
| VT new onset, n, % | N/A | 26, 11 | – | 6, 18 | 20, 10 | 0.225 |
| TIA historical, n, % | N/A | 6, 3 | – | 1, 3 | 5, 2 | 0.596 |
| TIA new onset, n, % | 0, 0 | 5, 2 | – | 2, 6 | 3, 1 | 0.143 |
| Diabetes mellitus, n, % | 0, 0 | 18, 8 | – | 2, 6 | 16, 8 | 1 |
| Smoking history, n, % | - | 59, 25 | – | 10, 30 | 49, 24 | 0.516 |
| LGE presence, n, % | 0, 0 | 185, 77 | – | 30, 91 | 155, 76 | 0.056 |
| LGE mass (g) | 0, 0% | 15.0 [8.0, 26.0] | – | 14.0 [6.9, 29.0] | 16.0 [8.0, 26.0] | 0.687 |
| LGE (%) | 0, 0% | 10.5 [5.6, 15.5] | – | 10.0 [4.8, 14.6] | 10.7 [5.7, 15.5] | 0.601 |
| Latest NYHA class, %: 1, 2, 3, 4 | 20, 0, 0, 0 | 65, 28, 7, 0 | – | 44, 50, 6, 0 | 69, 25, 7, 0 | 0.012* |
| Sarcomeric variant present, n, % | N/A | 78, 33 | – | 8, 24 | 70, 34 | 0.239 |
| Medications | ||||||
| Beta-blockers, n, % | 0, 0 | 107, 45 | < 0.001* | 19, 58 | 88, 43 | 0.190 |
| Calcium channel blockers, n, % | 0, 0 | 59, 25 | 0.021 | 12, 36 | 47, 23 | 0.136 |
| ACE-I/ARB, n, % | 2, 10 | 57, 24 | 0.213 | 11, 33 | 46, 22 | 0.194 |
| Diuretics, n, % | 0, 0 | 9, 4 | 0.754 | 1, 3 | 8, 4 | 1 |
| Aspirin, n, % | 1, 5 | 81, 34 | 0.009* | 11, 33 | 70, 34 | 0.845 |
| Warfarin or other anticoagulation, n, % | 0, 0 | 21, 9 | 0.315 | 11, 33 | 10, 5 | < 0.001* |
| CMR: left atrium | ||||||
| LA diameter (mm) | 34.5 (4.3) | 37.2 (5.7) | 0.037 | 39.0 [34.0, 42.0] | 37.0 [33.0, 40.0] | 0.136 |
| LAEDV index (mL/m2) | 38.1 [35.9, 46.9] | 43.8 [36.2, 51.1] | 0.158 | 45.6 [39.4, 65.5] | 43.5 [35.2, 50.7] | 0.044 |
| LAEDV (mL) | 78.7 (20.4) | 90.8 (31.7) | 0.095 | 95.3 [77.7, 127.9] | 84.5 [66.2, 105.7] | 0.040 |
| LAESV index (mL/m2) | 17.3 (4.7) | 23.6 (12.4) | 0.025 | 31.5 (18.3) | 22.3 (10.7) | < 0.001* |
| LAESV (mL) | 33.5 (10.3) | 46.9 (24.8) | 0.017 | 62.9 (36.5) | 44.28 (21.3) | < 0.001* |
| LA stroke volume (mL) | 45.2 (12.9) | 44.0 (15.2) | 0.720 | 40.0 (16.9) | 44.6 (14.9) | 0.111 |
| LA reservoir strain (%) | 21.6 [19.9, 22.9] | 19.9 [17.1, 22.2] | 0.047 | 15.6 (5.4) | 19.8 (4.3) | < 0.001* |
| LA conduit strain (%) | 13.7 (3.3) | 10.6 (4.4) | 0.002* | 8.6 (3.8) | 10.9 (4.4) | 0.004* |
| LA booster strain (%) | 8.7 (1.8) | 9.2 (3.1) | 0.439 | 7.6 (3.3) | 9.5 (3.0) | 0.001* |
| LAEF (%) | 57.2 [54.6, 61.5] | 51.7 [44.8, 57.5] | 0.001* | 44.0 [26.7, 54.0] | 52.5 [46.9, 58.0] | 0.001* |
| CMR: left ventricle | ||||||
| LV maximal wall thickness (mm) | – | 19.0 [16.0, 22.0] | – | 21.0 [18.0, 23.0] | 19.0 [16.0, 22.0] | 0.068 |
| LVOT max pressure gradient (mmHg) | – | 5.2 [3.8, 7.6] | – | 5.4 [4.0, 8.1] | 5.2 [3.8, 7.4] | 0.698 |
| LVOT obstruction ≥ 30 mmHg, n, % | – | 9, 4 | – | 0, 0 | 9, 4 | – |
| LVEDV index (mL/m2) | 80.8 [65.9, 93.5] | 71.1 [62.0, 82.1] | 0.025 | 66.0 [55.0, 75.0] | 72.2 [63.5, 82.3] | 0.024 |
| LVESV index (mL/m2) | 29.0 [21.4, 35.0] | 21.3 [17.0, 27.0] | 0.008 | 19.3 [15.8, 25.0] | 21.7 [17.6, 27.0] | 0.039 |
| LV stroke volume index (mL/m2) | 51.4 [47.4, 60.0] | 49.8 [43.8, 54.9] | 0.171 | 45.4 [39.0, 53.2] | 50.1 [44.0, 55.4] | 0.066 |
| LV ejection fraction (%) | 64.9 [59.5, 71.2] | 69.6 [65.0, 74.3] | 0.024 | 70.6 (7.2) | 69.3 (6.9) | 0.292 |
| LV mass (grams) | 107.4 [88.8, 122.9] | 151.5 [127.3, 183.5] | < 0.001* | 178.8 [139.7, 200.4] | 150.3 [123.7, 176.7] | 0.024 |
Data are represented as mean ± standard deviation, or median [IQR]
Hypothesis testing via Student’s t-test or Mann–Whitney U test, as appropriate
ACEI angiotensin converting enzyme inhibitor, ARB angiotensin receptor blocker, ESC European Society of Cardiology, LA left atria, LAEDV left atrial end diastolic volume, LAESV left atrial end systolic volume, LGE late gadolinium enhancement (5-SD), LGE % percentage of tissue enhanced by gadolinium, LV left ventricle, LVEDV left ventricular end diastolic volume, LVESV left ventricular end systolic volume, LVOT left ventricular outflow tract, LVOT obstruction, when pressure ≥ 30 mmHg, NYHA New York Heart Association, SCD sudden cardiac death, TIA transient ischemic attack, VT ventricular tachycardia
*Indicates a significant difference. This significance level is P < 0.05 without Bonferroni correction for baseline clinical variables and medications, whereas with Bonferroni correction the significance values are P < 0.005 and P < 0.0071 for CMR: Left Atrium and CMR: Left Ventricle, respectively
Results
Reproducibility of LA strain measurements
Inter-observer (GT) and intra-observer variability of LA strain were within the clinically acceptable range (refer to Additional file 1 and Table S1 for details).
Baseline characteristics of HCM patients and controls
Of the 281 patients screened for study inclusion, 24 (9%) were excluded due to pre-existing AF at the time of the CMR scan, 14 (5%) were excluded due to taking amiodarone, and 5 (2%) were excluded due to issues with data collection, leaving 238 HCM patients in the study (see Additional file 1: Fig. S1).
The median subject age was 54 years with IQR[43, 63]), 184 (77%) were men, 107 (47%) were on beta blockers, the average 5-year risk of sudden cardiac death (SCD) was low based on the ESC guidelines for risk stratification (2.0 ± 1.6%), 69 (29%) had mitral regurgitation (81% of which was mild or moderate), and 9 (4%) had LVOT obstruction ≥ 30 mmHg. Thirty-three (14%) developed new onset AF during follow-up after a mean time of 3.6 years (median of 3.0 years with IQR [2.8, 6.8]). Of these, 11 were in persistent AF whereas 22 had evidence of paroxysmal AF. The baseline clinical characteristics of patients and healthy controls are summarised in Table 1.
As expected, when compared to controls, HCM patients had smaller indexed LV end-diastolic and end-systolic volumes, and higher LV ejection fraction (LVEF) and LV mass (Table 1), although after application of the Bonferroni correction only LV mass differed significantly. LA diameter in the LVOT view and LAESV index were higher in HCM than controls, whilst LAEF, reservoir and conduit strain were lower in HCM (Fig. 1) although of these findings, only those relating to conduit strain and LAEF were consistent after the Bonferroni correction was applied. There was a trend towards LAEDV index being increased in HCM, whereas consistent with a previous study, LA booster strain did not differ between HCM and healthy controls even at a significant level of P < 0.05 [17].
Patients with and without new onset AF
HCM patients who developed new onset AF were significantly older and were more likely to have mitral regurgitation, higher New York Heart Association (NYHA) scores, and non-sustained ventricular tachycardia (VT). Patients with new onset AF had higher LV wall thickness, LV mass, LAEDV index, LAESV index, and more impaired LAEF and global LA strain (reservoir, conduit, and booster) at baseline CMR than those who did not (at a P < 0.05 level). There was a non-significant trend towards a higher LA anterior–posterior diameter at baseline in patients who developed AF versus those who did not (P = 0.136). Once the Bonferroni correction was applied (Table 1), only LAESV index, LAEF and global LA strain parameters remained significantly different between groups.
Diagnostic accuracy of LA parameters in predicting new onset AF in HCM
The optimal threshold values for predicting new onset AF for the main LA parameters and age were calculated using ROC curve analysis. Additional file 1: Table S2 shows rounded optimal thresholds and measurements of diagnostic accuracy (C-statistic).
Biomarkers associated with incident AF in HCM
To assess the determinants of AF in HCM patients, we undertook a univariate analysis (see Table 2) and found the following variables to be significant predictors of new onset AF once Bonferroni corrections were applied: age at scan, LAESV index, LA reservoir, conduit, and booster strain, and LAEF. Of note, LA diameter (antero-posterior) assessed to be ≥ 45 mm on CMR (a threshold derived from transthoracic echo studies) was not significantly associated with new onset AF in our cohort even at a conventional P value of 0.05 (P = 0.348).
Table 2.
Univariate predictors of new onset AF in all patients
| Univariate analysis | ||
|---|---|---|
| HR (95% CI) | P value prior to correction | |
| Baseline and clinical | ||
| Age at scan, per year | 1.07 (1.04–1.10) | < 0.001* |
| Age ≥ 55 years (rounded ROC threshold) | 5.94 (2.50–14.09) | < 0.001* |
| Male sex | 0.95 (0.43–2.11) | 0.903 |
| Systolic blood pressure, per mmHg | 1.01 (0.99–1.03) | 0.341 |
| Diastolic blood pressure, per mmHg | 1.03 (0.99–1.06) | 0.155 |
| Body mass index, per unit | 1.03(0.96–1.12) | 0.393 |
| Hypertension | 2.00 (0.99–4.03) | 0.051 |
| Diabetes | 0.73(0.17–3.07) | 0.669 |
| Smoking history | 1.16 (0.55–2.45) | 0.692 |
| Hypercholesterolemia | 1.04 (0.36–2.96) | 0.947 |
| Family history of SCD 1st degree relative | 0.45 (0.17–2.23) | 0.454 |
| Family history of SCD 2nd degree relative | 1.21 (0.42–3.46) | 0.725 |
| SCD risk score (ESC) | 1.04 (0.86–1.26) | 0.673 |
| VT | 1.43 (0.59–3.46) | 0.433 |
| TIA stroke | 2.92 (0.69–12.31) | 0.145 |
| Syncope | 0.48 (0.11–2.02) | 0.318 |
| NYHA class | 1.79 (1.09–2.93) | 0.021 |
| LGE, presence or absence | 6.27 (0.85–46.05) | 0.071 |
| LGE mass, g | 1.00 (0.98–1.02) | 0.871 |
| LGE, % | 1.00 (0.96–1.04) | 0.926 |
| Presence of sarcomeric variant | 0.52 (0.23–1.17) | 0.113 |
| Mitral regurgitation presence (any grade) vs absence | 1.16 (0.81–1.67) | 0.407 |
| Mitral regurgitation grade 1/nomitral regurgitation vs grade 2/3/4 | 2.16 (0.97–4.79) | 0.058 |
| Medication | ||
| Beta-blockers | 1.22 (0.61–2.44) | 0.577 |
| Calcium channel blockers | 1.96 (0.95–4.02) | 0.067 |
| ACE-I/ARB | 1.61 (0.78–3.34) | 0.201 |
| Diuretics | 0.88 (0.12–6.46) | 0.899 |
| Aspirin | 1.00 (0.48–2.09) | 0.994 |
| CMR: LA | ||
| LA diameter, mm, continuous | 1.05 (0.99–1.12) | 0.046 |
| LA diameter ≥ 45 mm (ESC threshold) | 1.58 (0.61–4.12) | 0.348 |
| LA diameter ≥ 42 mm (ROC threshold rounded) | 2.11 (1.05–4.25) | 0.036 |
| LAEDV index, mL/m2, continuous | 1.02 (1.01–1.04) | 0.023 |
| LAEDV index ≥ 50 mL/m2 (ROC threshold rounded) | 2.15 (1.08–4.27) | 0.029 |
| LAESV index, mL/m2, continuous | 1.04 (1.02–1.06) | < 0.001* |
| LAESV index ≥ 27 mL/m2 (ROC threshold rounded) | 2.42 (1.22–4.82) | 0.012 |
| LA reservoir strain, % (continuous) | 0.86 (0.81–0.91) | < 0.001* |
| LA reservoir strain ≤ 18% (ROC threshold rounded) | 3.64 (1.81–7.32) | < 0.001* |
| LA conduit strain, %, continuous | 0.88 (0.81–0.95) | 0.002* |
| LA conduit strain ≤ 12% (ROC threshold rounded) | 3.15 (1.29–7.72) | 0.012 |
| LA booster strain, %, continuous | 0.87 (0.78–0.97) | 0.014 |
| LA booster strain ≤ 8% (ROC threshold rounded) | 2.93 (1.44–5.95) | 0.003* |
| LAEF (%) continuous | 0.94 (0.92–0.97) | < 0.001* |
| LAEF ≤ 45%, (ROC threshold rounded) | 3.42 (1.72–6.78) | < 0.001* |
| CMR: left ventricle | ||
| LV maximal wall thickness, mm | 1.06 (1.00–1.14) | 0.059 |
| LV mass, grams | 1.00 (1.00–1.01) | 0.180 |
| LVOT max pressure gradient, mmHg | 1.04 (0.95–1.14) | 0.350 |
| LVEDV index (mL/m2) | 0.98 (0.95–1.00) | 0.069 |
| LVESV index (mL/m2) | 0.96 (0.91–1.01) | 0.114 |
| LV stroke volume index, mL/m2 | 0.98 (0.94–1.01) | 0.163 |
| LV ejection fraction, % | 1.02 (0.97–1.07) | 0.506 |
LA left atria, LAEDV left atrial end diastolic volume, LAEF left atrial ejection fraction, LAESV left atrial end systolic volume, LGE late gadolinium enhancement (5-SD), LGE % percentage of tissue enhanced by gadolinium, LV left ventricle, LVOT left ventricular outflow tract, LVEDV left ventricular end diastolic volume, LVESV left ventricular end systolic volume, LVSV left ventricular stroke volume, NYHA New York Heart Association, SCD sudden cardiac death, TIA transient ischemic attack, VT ventricular tachycardia
*Indicates a significant difference given Bonferroni correction to the P value as stated in the methods
When undertaking Cox multiple regression analysis, we considered each of the five main LA parameters that displayed evidence of significance in the Bonferroni corrected Univariate analysis. For completeness, LA diameter was also analysed in the multiple regression analysis despite not reaching significance. A model was initially constructed for each main LA parameter to avoid collinearity between them (six models shown in Table 3). Age was included in all models due to reaching significance in univariate analysis. When analysing all HCM patients, age (≥ 55 years) was a significant predictor of new onset AF, with hazard ratios (HR) that ranged from 4.05 to 6.30. LA EF (≤ 45%) was associated with a twofold increased risk of new onset AF (Table 3). LA reservoir strain (≤ 18%) and booster strain (≤ 8%) were associated with a nearly threefold and fourfold increased risk of new onset AF. LAESV index, and conduit strain were not significant predictors.
Table 3.
Six multiple regression models: determinants of AF in all HCM patients, and in those with LA diameter < 45mm, indicating a low risk for AF development
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|
| LA diameter | LAESV index | LA reservoir strain | LA conduit strain | LA booster strain | LAEF | |
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| All HCM patients, n = 238 | ||||||
| Age ≥ 55 | 5.07 (2.23–11.55)** | 4.72 (2.06–10.95)** | 4.05 (1.73–9.46)** | 4.42 (1.76–11.06)** | 6.62 (2.79–15.70)** | 4.19 (1.80–9.76)** |
| LA diameter ≥ 42 mm | 1.92 (0.95–3.91) | – | – | – | – | – |
| LAESV index ≥ 27 mL/m2 | – | 1.82 (0.90–3.68) | – | – | – | – |
| LA reservoir strain ≤ 18% | – | – | 2.56 (1.24–5.27)* | – | – | – |
| LA conduit strain ≤ 12% | – | – | – | 1.58 (0.58–4.25) | – | – |
| LA booster strain ≤ 8% | – | – | – | – | 3.69 (1.81–7.52)** | – |
| LAEF ≤ 45% | – | – | – | – | – | 2.43 (1.20–4.92)* |
| HCM patients with LA diameter < 45 mm, n = 217 | ||||||
| Age ≥ 55 | 4.05 (1.72–9.51)** | 4.73 (2.04–10.96)** | 3.34 (1.38–8.06)** | 3.41 (1.30–8.96)* | 5.78 (2.35–14.23)** | 3.67 (1.53–8.81)** |
| LA diameter ≥ 42 mm | 1.94 (0.84–4.47) | – | – | – | – | – |
| LAESV index ≥ mL/m2 | – | 1.82 (0.90–3.68) | – | – | – | – |
| LA reservoir strain ≤ 18% | – | – | 2.49 (1.13–5.32)* | – | – | – |
| LA conduit strain ≤ 12% | – | – | – | 1.72 (0.60–4.90) | – | – |
| LA booster strain ≤ 8% | – | – | – | – | 3.74 (1.70–8.07)** | – |
| LAEF ≤ 45% | – | – | – | – | – | 1.98 (0.92–4.28) |
EF, ejection fraction, HCM, hypertrophic cardiomyopathy, HR, hazard ratio, LA, left atria, LAEDV, left atrial end diastolic volume, LAEF, left atrial ejection fraction
*Indicates a significant difference of P < 0.05
**Indicates a significant difference of P < 0.01
Further to this, we applied the same six Cox multiple regression models to a subgroup of HCM patients in whom LA diameter was less than 45 mm (n = 217), a group that would otherwise not be considered at risk of AF based on ESC guidelines [2]. Age was again a significant predictor of AF in each model. Of the LA parameters, LA reservoir (HR 2.49, CI 1.13–5.32, P = 0.023) and booster (HR 3.74, CI 1.70–8.07, P ≤ 0.001) strain were the only variables to retain significance (Table 3).
We then included all the parameters that retained significance in the Cox multiple regression models on all HCM patients in a model (Table 4). In this, only age and LA booster function retained significance, with age being a more powerful predictor than booster strain (HR of 5.22 vs 3.08).
Table 4.
Multiple regression: predicting new onset AF in all HCM patients
| HR (95% CI) | P value | |
|---|---|---|
| Age ≥ 55 years | 5.22 (2.12–12.83) | < 0.001** |
| LA reservoir strain ≤ 18% | 1.21 (0.44–3.32) | 0.717 |
| LA booster strain ≤ 8% | 3.08 (1.43–6.64) | 0.004** |
| LAEF ≤ 45% | 1.73 (0.68–4.40) | 0.252 |
LAEF left atrial ejection fraction, HR hazard ratio, LA left atria, LAEDV left atrial end diastolic volume
*Indicates a significant difference of P < 0.05
**Indicates a significant difference of P < 0.01
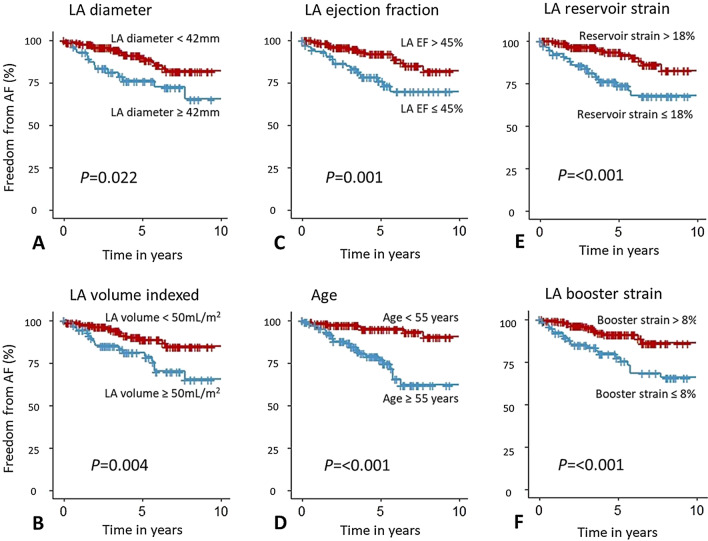
Survival analysis
Survival graphs displaying survival free from AF were produced for the variables that reached significance in the multiple regression models (Fig. 2). There was a significant difference in freedom from AF in the 10 years post follow up when stratifying by LA diameter, LAEDV index, LAEF, and in particular age. When all the HCM cases were stratified by an LA reservoir strain of 18%, the 5 years survival free of AF was 76% for those with reservoir strain ≤ 18%, compared to 96% in those with strain > 18%. Similarly, when stratifying with LA booster strain of 8%, the 5 years survival free of AF was 81% in those with booster strain ≤ 8%, compared to 94% in those with booster strain > 8%.
Fig. 2.
Kaplan Meier curves demonstrating freedom from atrial fibrillation for HCM patients. Survival curves of all HCM patients (n = 238) showing freedom from atrial fibrillation (AF) when stratified according to the variables included in the Cox multiple regression analysis: A Left atrial (LA) diameter; B LA end diastolic volume (LAEDV) index; C LA ejection fraction; D Age ; E LA reservoir strain; F LA booster strain
Determinants of LA strain components
Univariate and multivariable determinants of LA reservoir, conduit, and booster strain are shown in Table 5. On multivariable regression analysis, age at scan associated with all three of reservoir, conduit, and booster strain. In addition, NYHA class, LV maximal wall thickness, LV mass, and LV ejection fraction (LVEF) also remained significantly associated with reservoir strain. Presence of LGE, mitral regurgitation, LV mass, and LV stroke volume also independently associated with conduit strain, whilst a history of smoking also associated with booster strain.
Table 5.
Univariate and multiple linear regression showing determinants of LA strain in an AF naïve population
| Univariate linear regression | Multivariable linear regression | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reservoir strain | Conduit strain | Booster strain | Reservoir strain | Conduit strain | Booster strain | |||||||
| β | P values | β | P values | β | P values | β | P values | β | P values | β | P values | |
| Age, per year | − 0.11 | < 0.001* | − 0.19 | < 0.001* | 0.06 | < 0.001* | − 0.10 | < 0.001* | − 0.18 | < 0.001* | 0.04 | 0.018* |
| Gender | 1.17 | 0.102 | 1.45 | 0.050 | 0.66 | 0.196 | – | – | – | – | – | – |
| Systolic blood pressure, per mmHg | − 0.06 | 0.001* | − 0.07 | < 0.001* | 0.01 | 0.567 | 0.01 | 0.637 | − 0.01 | 0.891 | – | – |
| Diastolic blood pressure, per mmHg | − 0.07 | 0.027* | − 0.07 | 0.052 | − 0.01 | 0.599 | − 0.04 | 0.309 | – | – | – | – |
| Body mass index, per unit | − 0.10 | 0.120 | − 0.16 | 0.024* | 0.06 | 0.245 | – | – | 0.11 | 0.095 | – | – |
| Hypertension | − 0.52 | 0.392 | − 2.06 | 0.001* | 1.29 | 0.003* | – | – | 0.71 | 0.272 | 0.01 | 0.998 |
| Diabetes | 0.07 | 0.951 | − 2.36 | 0.044* | 2.00 | 0.014* | – | – | − 0.21 | 0.834 | 0.65 | 0.473 |
| Smoking history | 0.31 | 0.655 | − 1.38 | 0.056 | 1.59 | 0.001* | – | – | – | – | 1.33 | 0.014* |
| Hypercholesterolemia | − 0.46 | 0.626 | − 2.20 | 0.024* | 1.24 | 0.066 | – | – | − 0.21 | 0.771 | – | – |
| Familyhistory of SCD 1st degree relative | 0.67 | 0.566 | 0.24 | 0.843 | 0.68 | 0.424 | – | – | – | – | – | – |
| Family history of SCD 2nd degree relative | 0.56 | 0.540 | 0.26 | 0.786 | 0.34 | 0.613 | – | – | – | – | – | – |
| SCD risk score | − 0.24 | 0.602 | − 0.85 | 0.067 | 0.56 | 0.080 | – | – | – | – | – | – |
| VT | 0.17 | 0.864 | − 1.19 | 0.257 | 1.49 | 0.038* | – | – | – | – | 1.24 | 0.093 |
| TIA stroke | − 1.83 | 0.461 | − 1.98 | 0.442 | − 0.17 | 0.923 | – | – | – | – | – | – |
| Syncope | − 1.40 | 0.088 | − 2.34 | 0.006* | 0.60 | 0.313 | – | – | − 0.70 | 0.376 | – | – |
| NYHA class | − 1.84 | < 0.001* | − 2.63 | < 0.001* | 0.35 | 0.325 | − 1.07 | 0.042* | − 0.52 | 0.274 | – | – |
| LGE, presence/absence | − 2.15 | 0.012* | − 3.88 | < 0.001* | 1.33 | 0.030* | − 0.93 | 0.256 | − 1.86 | 0.007* | 0.71 | 0.254 |
| LGE, % | 0.02 | 0.561 | − 0.05 | 0.123 | 0.05 | 0.028* | – | – | – | – | 0.02 | 0.368 |
| LGE mass, grams | − 0.03 | 0.166 | − 0.05 | 0.017* | 0.01 | 0.409 | – | – | − 0.02 | 0.186 | – | – |
| Presence of sarcomeric variant | 0.88 | 0.166 | 2.49 | < 0.001* | − 1.37 | 0.002* | – | – | 0.24 | 0.722 | − 0.72 | 0.215 |
| Mitral regurgitation | − 3.26 | 0.001* | − 4.12 | < 0.001* | 0.16 | 0.816 | − 1.16 | 0.256 | − 2.89 | 0.001* | – | – |
| LV maximal wall thickness, mm | − 0.32 | < 0.001* | − 0.32 | < 0.001* | − 0.05 | 0.386 | − 0.20 | 0.021* | − 0.15 | 0.052 | – | – |
| LV mass, grams | − 0.03 | < 0.001* | − 0.02 | 0.003* | − 0.01 | 0.068 | − 0.01 | 0.035* | − 0.01 | 0.030* | – | – |
| LVOT max pressure gradient, mmHg | 0.08 | 0.462 | − 0.12 | 0.282 | 0.13 | 0.101 | – | – | – | – | – | – |
| LVOT obstruction ≥ 30 mmHg, n, % | − 0.88 | 0.271 | − 1.01 | 0.223 | − 0.23 | 0.693 | – | – | – | – | – | – |
| LVEDV index, mL/m2 | 0.02 | 0.383 | 0.06 | 0.003* | − 0.03 | 0.028* | – | – | − 0.04 | 0.278 | − 0.02 | 0.370 |
| LVESV index, mL/m2 | − 0.03 | 0.385 | 0.03 | 0.452 | − 0.05 | 0.088 | – | – | – | – | – | – |
| LV stroke volume index, mL/m2 | 0.06 | 0.050 | 0.12 | < 0.001* | − 0.04 | 0.055 | – | – | 0.13 | 0.011* | – | – |
| LV ejection Fraction, % | 0.10 | 0.024* | 0.08 | 0.076 | 0.02 | 0.589 | 0.131 | 0.002* | – | – | – | – |
LGE late gadolinium enhancement (5-SD), LV left ventricle, LVEDV left ventricular end diastolic volume index, LVESV left ventricular end systolic volume index, LVOT left ventricular outflow tract, LVSV left ventricular stroke volume, NYHA New York heart association, SCD sudden cardiac death, TIA transient ischemic attack, VT ventricular tachycardia
*Indicates a significant difference of P < 0.05
Discussion
In this study, we used CMR to assess the role of LA deformation when compared to standard LA parameters and baseline characteristics in predicting new onset AF in HCM. In addition to age and LAEF, we have shown that LA reservoir and booster strain have the ability to augment prediction of new onset AF in HCM. Specifically, we show that LA reservoir and booster strain dysfunction are important determinants of AF risk even in those with an LA diameter less than 45 mm, a threshold set by the ESC to escalate arrhythmia surveillance frequency. Of interest, a marginally higher risk of incident AF was specifically seen in those with booster strain dysfunction compared to other parameters. We also determined the factors that associate with markers of atrial deformation and show that age and phenotypic severity adversely influenced LA deformation.
The prediction of new onset AF in HCM allows for intensification of monitoring and prophylactic use of anticoagulation in those at high risk, thus minimising the effects of subsequent harmful sequelae, primarily stroke, myocardial infarction (embolic), and heart failure [24]. Early studies investigating the determinants of new onset AF have found LA size to be important in guiding surveillance. More recently, LA function has emerged as a useful determinant of new onset AF in HCM patients [4–7]. LA deformation or strain provides an additional measure of atrial mechanics and has been found to provide deeper insights into the risk of arrhythmia, embolic events, and other adverse outcomes in some cardiovascular diseases [25, 26]. In patients with AF, Hsu et al. demonstrated an independent association between LA strain and risk of embolic complications such as stroke [27].
Most studies to date have used transthoracic echocardiography (TTE) for the assessment of LA strain in HCM [14, 15]. However, TTE remains limited in its ability to provide consistently high quality images which are often confounded by body habitus, comorbidities such as chronic obstructive lung disease, and operator expertise [28]. In comparison, CMR provides an excellent platform to precisely and reproducibly evaluate cardiac chambers, providing additional information on myocardial tissue characteristics [29]. The high resolution images acquired by CMR enable retrospective analyses of LA dimensions and function from both LA and right atria, which are well visualised in standard cardiac planes acquired in accordance with consensus guidelines [30]. In spite of the increasing use of CMR for assessment of HCM patients, studies examining the additive value of LA strain assessment on CMR in AF prediction in HCM are lacking.
Here, we systematically examined components of LA strain as assessed on CMR, in addition to standard metrics of LA size and function. Consistent with previous studies, we found LA reservoir and conduit strain to be impaired in HCM patients [13, 31], though after correcting for multiple comparisons only conduit strain remained impaired. By contrast, LA booster strain, the active component of LA deformation, was not significantly different between HCM patients and healthy control subjects. Indeed, the evidence in support of booster dysfunction in HCM patients is conflicting. In a study by Yang and colleagues [17], LA booster strain was not different between non-obstructive HCM patients and controls. In contrast, Kowallick et al. reported a significant impairment in LA booster strain in HCM patients relative to controls [32].
A number of studies have postulated that booster function could indicate an increase in fibrotic burden of the atria [33, 34]. In a recent study by Sivalokanathan et al. [35], atrial fibrosis as detected by atrial LGE was found to be greater in those with new onset AF [35]. Likewise, in our study booster strain was reduced in those patients that developed AF compared to those that did not. Thus, the relationship between booster strain and AF may potentially reflect an increased burden of atrial fibrosis or an underlying atrial myopathy in HCM patients.
The absolute values of LA strain reported in this study were lower than those reported elsewhere [36], though comparable with some studies using CMR myocardial feature tracking. Values from healthy, yet elderly controls in studies by Evin et al. [37] and Lamy et al. [38] matched our relatively old and obese control group closely [37, 38]. The values from all HCM patients in this study are within reasonable range of those presented by Sivalokanathan et al. and Kowallick [13, 35]. In the present study, LA diameter [5], volume [6] and LAEF [7] were univariate determinants of AF risk, largely consistent with earlier work. We additionally showed that LA reservoir and booster strain are associated with a threefold and fourfold increase in new onset AF risk, respectively, and, as illustrated by the freedom-from-AF survival curves (see Fig. 2 and Additional file 1: Fig. S2), both measures discriminated risk of new onset AF with reasonable diagnostic accuracies (see Additional file 1: Table S2). Of importance, in patients with LA diameter of less than 45 mm, booster and reservoir strain remained strong independent determinants of new onset AF.
To date, there have been a number of studies of HCM patients in which age independently predicted AF risk [4, 24, 39]. Concordantly, we also found age to be a strong determinant of future risk of new onset AF. Consensus guidelines make no specific recommendations for prophylactic anticoagulation or frequency of arrhythmia monitoring in patients based on age. Our findings highlight the need to incorporate age into future risk prediction models being developed for AF or stroke risk prediction in patients with HCM and provide an argument to consider prophylactic anticoagulation therapy in elderly HCM patients who are not at risk of significant bleeding.
Wider evidence surrounding the impact of sarcomeric mutations on AF incidence is mixed; Bongini et al., found no association between HCM genetic subtype and AF [40], whereas Lee et al. report myosin heavy chain—7 (MYH7) to be predictive of AF [41]. In this study, the presence of sarcomeric variant trended towards associating with lower risk of AF on univariate analysis (HR of 0.52, P = 0.113). We believe that this may have been due to a higher prevalence of hypertension and increased age among the sarcomere negative HCM patients (Additional file 1: Table S3). Such differences in baseline characteristics of HCM patients with and without sarcomeric variants have also been observed in a recent multicentre CMR registry of HCM (HCMR study) [42].
This study assessed the determinants of LA strain in an AF naïve HCM population. Our findings in the multiple regression models suggest that age, markers of phenotypic severity (LV wall thickness, mass, mitral regurgitation, LGE) and baseline SCD risk are associated with adverse LA mechanical remodelling and could explain the emerging prognostic implications of LA strain for many cardiovascular events [11, 14, 26]. That age was negatively associated with reservoir and conduit strain and positively associated with booster strain has been noted previously in non-HCM populations—atrial emptying is more dependent on booster function in older age [43, 44]. The negative correlation between LGE and conduit strain and LV mass/wall thickness and reservoir strain in HCM is also not surprising given that both conduit and reservoir largely reflect LA compliance, which may be impacted by the burden of fibrosis and adverse remodelling [45]. Although the presence of sarcomeric variant was seen to associate with both conduit and booster strain on univariate analysis, this failed to reach statistical significance in our multivariable model. This may be because of the differences in baseline characteristics (in particular age and hypertension) of sarcomere positive and negative HCM patients. Further studies are needed to tease out the precise relationship between sarcomeric variant status and LA strain components.
Limitations
This is a retrospective single-centre study, and thus some characteristics, such as the extent of LVOT obstruction, are not reflective of the population frequency. Temporal resolution of cine imaging was not consistent (39–60 ms) in all patients (due to the retrospective nature of this study) and could in theory contribute to variability in strain measurements. Prior to the publication of ESC guidelines in 2014, TTE analysis was only done as per clinical need. Therefore, we lacked the ability to compare or correlate CMR and TTE data. Similarly, diastolic function was not available on the same day as CMR for many patients. A dedicated atrial stack on LGE imaging was not undertaken and therefore fibrosis in the atria could not be assessed. The frequency of AF monitoring is in line with current clinical practice. We did not assess atrial strain rate as this was beyond the remit of our primary hypothesis.
The LA strain values of controls presented in this paper differ from some of the wider literature. However, our healthy controls were older, obese, and matched to HCM cohort (for blood pressure) and thus different to controls from other studies. These factors may explain potential differences in magnitude of strain. Another reason for differences CMR strain measurements across studies is the lack of standardisation in strain measurements across different analysis platforms. The increasing use of fully automated machine learning algorithms is expected to significantly improve standardisation and reduce interobserver variability, at which point CMR analysis of the LA strain could become a valuable clinically tool for risk prediction of AF. Finally, we did not undertake external validation of the thresholds for LA parameters and age, hence the selected thresholds require cautious interpretation when extrapolating to all HCM patients. Nevertheless, the present study provides novel insights into the additional value of LA deformation analysis on CMR for stratifying HCM patients at risk of new onset AF.
Conclusion
We used CMR in HCM and demonstrate that LA strain components are reduced in patients who develop AF. Specifically, reservoir and booster LA strain augment risk prediction of new onset AF in HCM patients. Our work underscores the importance of age as a guide to arrhythmia surveillance and suggests that the routine assessment of LA strain in HCM patients could augment existing tools for AF and potentially stroke prediction in HCM.
Supplementary Information
Additional file 1: Table S1. Reproducibility of strain parameters. Table S2. Diagnostic accuracy of predicting new onset AF. Table S3. Differences in age and rate of hypertension between those with and without sarcomeric variants. Figure S1. Flow chart showing inclusion of subjects. Figure S2. Survival curve for HCM patients.
Acknowledgements
Not applicable.
Abbreviations
- AF
Atrial fibrillation
- AHA
American Heart Association
- AUC
Area under curve
- BMI
Body mass index
- CMR
Cardiovascular magnetic resonance
- CI
Confidence interval
- ECG
Electrocardiogram
- ESC
European Society of Cardiology
- EF
Ejection fraction
- HCM
Hypertrophic cardiomyopathy
- HR
Hazard ratio(s)
- ICC
Inherited Cardiac Conditions
- LA
Left atrium/left atrial
- LAEDV
Left atrial end-diastolic volume
- LAEF
Left atrial ejection fraction
- LAESV
Left atrial end-systolic volume
- LASV
Left atrial stroke volume
- LGE
Late gadolinium enhancement
- LV
Left ventricle/left ventricular
- LVEDV
Left ventricular end-diastolic volume
- LVESV
Left ventricular end-systolic volume
- LVOT
Left ventricular outflow tract
- NPV
Negative predictive value
- NYHA
New York Heart Association
- PPV
Positive predictive value
- ROC
Receiver Operator Characteristic
- SCD
Sudden cardiac death
- TTE
Transthoracic echocardiography
- VUS
Variant of uncertain significance
- VT
Ventricular tachycardia
Authors' contributions
BR contributed to ethics, undertook scanning of some patients, conceived the study, drafted the manuscript. RS performed image analysis, statistical analysis, and drafted the manuscript. MM, KC, CN, GT, FR contributed to data entry and image analysis. EO and RA contributed to ethics and recruitment of patient. KT, AL, AH, ECW, BC drafted the manuscript. HW and SN conceived the study and contributed to manuscript drafting and preparation. All authors read and approved the final manuscript.
Funding
This study was funded by the National Institute of Health Research (NIHR) Oxford Biomedical Research Centre and the British Heart Foundation. B.R and M.M were funded by the Oxford British Heart Foundation Centre of Research Excellence (RE/18/3/34214 ) and National Institute of Health Research Oxford Biomedical Research Centre. R.A. was funded by a British Heart Foundation Clinical Research Training Fellowship Grant (RA: 098436/Z/12/Z). SN and HW acknowledge support from the Oxford British Heart Foundation Centre of Research Excellence. BC acknowledges the support of the NIHR Oxford Biomedical Research Centre and the British Heart Foundation.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the local Oxford ethics committee (Reference: 07/Q1607/66, 12/LO/ 1979). All patient included consent for their details to be used for research purposes.
Consent for publication
Not applicable.
Competing interests
SN reports a consultancy and a grant from Cytokinetics, as well as grant support from Boehringer Ingelheim.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Betty Raman and Robert W. Smillie—joint first authors
Hugh Watkins and Stefan Neubauer—joint senior authors
References
- 1.Siontis KC, Geske JB, Ong K, Nishimura RA, Ommen SR, Gersh BJ. Atrial fibrillation in hypertrophic cardiomyopathy: prevalence, clinical correlations, and mortality in a large high‐risk population. J Am Heart Assoc. 2014;3(3):e001002. [DOI] [PMC free article] [PubMed]
- 2.Authors/Task Force m, Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(39):2733–79. [DOI] [PubMed]
- 3.Schaer BA, Zellweger MJ, Cron TA, Kaiser CA, Osswald S. Value of routine Holter monitoring for the detection of paroxysmal atrial fibrillation in patients with cerebral ischemic events. Stroke. 2004;35(3):e68–70. doi: 10.1161/01.STR.0000117568.07678.4B. [DOI] [PubMed] [Google Scholar]
- 4.Maron BJ, Haas TS, Maron MS, Lesser JR, Browning JA, Chan RH, et al. Left atrial remodeling in hypertrophic cardiomyopathy and susceptibility markers for atrial fibrillation identified by cardiovascular magnetic resonance. Am J Cardiol. 2014;113(8):1394–1400. doi: 10.1016/j.amjcard.2013.12.045. [DOI] [PubMed] [Google Scholar]
- 5.Guttmann OP, Rahman MS, O'Mahony C, Anastasakis A, Elliott PM. Atrial fibrillation and thromboembolism in patients with hypertrophic cardiomyopathy: systematic review. Heart. 2014;100(6):465–472. doi: 10.1136/heartjnl-2013-304276. [DOI] [PubMed] [Google Scholar]
- 6.Yang WI, Shim CY, Kim YJ, Kim SA, Rhee SJ, Choi EY, et al. Left atrial volume index: a predictor of adverse outcome in patients with hypertrophic cardiomyopathy. J Am Soc Echocardiogr. 2009;22(12):1338–1343. doi: 10.1016/j.echo.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 7.Debonnaire P, Joyce E, Hiemstra Y, Mertens BJ, Atsma DE, Schalij MJ, et al. Left atrial size and function in hypertrophic cardiomyopathy patients and risk of new-onset atrial fibrillation. Circ Arrhythmia Electrophysiol. 2017 doi: 10.1161/CIRCEP.116.004052. [DOI] [PubMed] [Google Scholar]
- 8.Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, et al. 2011 ACCF/AHA Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58(25):e212–60. [DOI] [PubMed]
- 9.Williams LK, Chan RH, Carasso S, Durand M, Misurka J, Crean AM, et al. Effect of left ventricular outflow tract obstruction on left atrial mechanics in hypertrophic cardiomyopathy. BioMed Res Int. 2015 doi: 10.1155/2015/481245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang X, Yue Y, Wang Y, Deng Y, Liu L, Di Y, et al. Assessment of left ventricular systolic and diastolic abnormalities in patients with hypertrophic cardiomyopathy using real-time three-dimensional echocardiography and two-dimensional speckle tracking imaging. Cardiovasc Ultrasound. 2018;16(1):23. doi: 10.1186/s12947-018-0142-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gan GCH, Ferkh A, Boyd A, Thomas L. Left atrial function: evaluation by strain analysis. Cardiovasc Diagn Ther. 2018;8(1):29–46. doi: 10.21037/cdt.2017.06.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.To AC, Flamm SD, Marwick TH, Klein AL. Clinical utility of multimodality LA imaging: assessment of size, function, and structure. JACC Cardiovasc Imaging. 2011;4(7):788–798. doi: 10.1016/j.jcmg.2011.02.018. [DOI] [PubMed] [Google Scholar]
- 13.Kowallick JT, Kutty S, Edelmann F, Chiribiri A, Villa A, Steinmetz M, et al. Quantification of left atrial strain and strain rate using Cardiovascular Magnetic Resonance myocardial feature tracking: a feasibility study. J Cardiovasc Magn Reson. 2014;16:60. doi: 10.1186/s12968-014-0060-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Essayagh B, Resseguier N, Michel N, Casalta A-C, Renard S, Donghi V, et al. Left atrial dysfunction as marker of poor outcome in patients with hypertrophic cardiomyopathy. Arch Cardiovasc Dis. 2021;114(2):96–104. doi: 10.1016/j.acvd.2020.06.004. [DOI] [PubMed] [Google Scholar]
- 15.Vasquez N, Ostrander BT, Lu D-Y, Ventoulis I, Haileselassie B, Goyal S, et al. Low left atrial strain is associated with adverse outcomes in hypertrophic cardiomyopathy patients. J Am Soc Echocardiogr. 2019;32(5):593–603.e1. [DOI] [PubMed]
- 16.Kim K-J, Choi H-M, Yoon YE, Kim H-L, Lee S-P, Kim H-K, et al. Left atrial mechanical function and global strain in hypertrophic cardiomyopathy. PLoS ONE. 2016;11(6):e0157433. doi: 10.1371/journal.pone.0157433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang Y, Yin G, Jiang Y, Song L, Zhao S, Lu M. Quantification of left atrial function in patients with non-obstructive hypertrophic cardiomyopathy by cardiovascular magnetic resonance feature tracking imaging: a feasibility and reproducibility study. J Cardiovasc Magn Reson. 2020;22(1):1–11. doi: 10.1186/s12968-019-0589-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ariga R, Tunnicliffe EM, Manohar SG, Mahmod M, Raman B, Piechnik SK, et al. Identification of myocardial disarray in patients with hypertrophic cardiomyopathy and ventricular arrhythmias. J Am Coll Cardiol. 2019;73(20):2493–2502. doi: 10.1016/j.jacc.2019.02.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li R, Yang Z-G, Xu H-Y, Shi K, Liu X, Diao K-Y, et al. Myocardial deformation in cardiac amyloid light-chain amyloidosis: assessed with 3t cardiovascular magnetic resonance feature tracking. Sci Rep. 2017 doi: 10.1038/s41598-017-03699-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raman B, Ariga R, Spartera M, Sivalokanathan S, Chan K, Dass S, et al. Progression of myocardial fibrosis in hypertrophic cardiomyopathy: mechanisms and clinical implications. Eur Heart J Cardiovasc Imaging. 2019;20(2):157–167. doi: 10.1093/ehjci/jey135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chirinos JA, Sardana M, Ansari B, Satija V, Kuriakose D, Edelstein I, et al. Left atrial phasic function by cardiac magnetic resonance feature tracking is a strong predictor of incident cardiovascular events. Circ Cardiovasc Imaging. 2018;11(12):e007512. doi: 10.1161/CIRCIMAGING.117.007512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chirinos JA, Sardana M, Ansari B, Satija V, Kuriakose D, Edelstein I, et al. Left atrial phasic function by cardiac magnetic resonance feature tracking is a strong predictor of incident cardiovascular events. Circ Cardiovasc Imaging. 2018;11(12):e007512. doi: 10.1161/CIRCIMAGING.117.007512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt. 2014;34(5):502–508. doi: 10.1111/opo.12131. [DOI] [PubMed] [Google Scholar]
- 24.Olivotto I, Cecchi F, Casey SA, Dolara A, Traverse JH, Maron BJ. Impact of atrial fibrillation on the clinical course of hypertrophic cardiomyopathy. Circulation. 2001;104(21):2517–2524. doi: 10.1161/hc4601.097997. [DOI] [PubMed] [Google Scholar]
- 25.Fujimoto K, Inoue K, Saito M, Higashi H, Kono T, Uetani T, et al. Incremental value of left atrial active function measured by speckle tracking echocardiography in patients with hypertrophic cardiomyopathy. Echocardiography. 2018;35(8):1138–1148. doi: 10.1111/echo.13886. [DOI] [PubMed] [Google Scholar]
- 26.Modin D, Biering-Sorensen SR, Mogelvang R, Alhakak AS, Jensen JS, Biering-Sorensen T. Prognostic value of left atrial strain in predicting cardiovascular morbidity and mortality in the general population. Eur Heart J Cardiovasc Imaging. 2019;20(7):804–815. doi: 10.1093/ehjci/jey181. [DOI] [PubMed] [Google Scholar]
- 27.Hsu PC, Lee WH, Chu CY, Lee HH, Lee CS, Yen HW, et al. Prognostic role of left atrial strain and its combination index with transmitral E-wave velocity in patients with atrial fibrillation. Sci Rep. 2016;6:17318. doi: 10.1038/srep17318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brenes JC, Doltra A, Prat S. Cardiac magnetic resonance imaging in the evaluation of patients with hypertrophic cardiomyopathy. Glob Cardiol Sci Pract. 2018;2018(3):22. doi: 10.21542/gcsp.2018.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zareian M, Ciuffo L, Habibi M, Opdahl A, Chamera EH, Wu CO, et al. Left atrial structure and functional quantitation using cardiovascular magnetic resonance and multimodality tissue tracking: validation and reproducibility assessment. J Cardiovasc Magn Reson. 2015;17:52. doi: 10.1186/s12968-015-0152-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hundley WG, Bluemke D, Bogaert JG, Friedrich MG, Higgins CB, Lawson MA, et al. Society for Cardiovascular Magnetic Resonance guidelines for reporting cardiovascular magnetic resonance examinations. J Cardiovasc Magn Reson. 2009;11(1):5. doi: 10.1186/1532-429X-11-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hinojar R, Zamorano JL, Fernandez-Mendez M, Esteban A, Plaza-Martin M, Gonzalez-Gomez A, et al. Prognostic value of left atrial function by cardiovascular magnetic resonance feature tracking in hypertrophic cardiomyopathy. Int J Cardiovasc Imaging. 2019;35(6):1055–1065. doi: 10.1007/s10554-019-01534-8. [DOI] [PubMed] [Google Scholar]
- 32.Kowallick JT, Silva Vieira M, Kutty S, Lotz J, Hasenfu G, Chiribiri A, et al. Left atrial performance in the course of hypertrophic cardiomyopathy: relation to left ventricular hypertrophy and fibrosis. Invest Radiol. 2017;52(3):177–185. doi: 10.1097/RLI.0000000000000326. [DOI] [PubMed] [Google Scholar]
- 33.Habibi M, Lima JA, Khurram IM, Zimmerman SL, Zipunnikov V, Fukumoto K, et al. Association of left atrial function and left atrial enhancement in patients with atrial fibrillation: cardiac magnetic resonance study. Circ Cardiovasc Imaging. 2015;8(2):e002769. doi: 10.1161/CIRCIMAGING.114.002769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gasparovic H, Cikes M, Kopjar T, Hlupic L, Velagic V, Milicic D, et al. Atrial apoptosis and fibrosis adversely affect atrial conduit, reservoir and contractile functions. Interact Cardiovasc Thorac Surg. 2014;19(2):223–30; discussion 30. doi: 10.1093/icvts/ivu095. [DOI] [PubMed] [Google Scholar]
- 35.Sivalokanathan S, Zghaib T, Greenland GV, Vasquez N, Kudchadkar SM, Kontari E, Lu DY, Dolores-Cerna K, van der Geest RJ, Kamel IR, Olgin JE. Hypertrophic cardiomyopathy patients with paroxysmal atrial fibrillation have a high burden of left atrial fibrosis by cardiac magnetic resonance imaging. JACC Clin Electrophysiol. 2019;5(3):364–75. [DOI] [PubMed]
- 36.Truong VT, Palmer C, Wolking S, Sheets B, Young M, Ngo TNM, et al. Normal left atrial strain and strain rate using cardiac magnetic resonance feature tracking in healthy volunteers. Eur Heart J Cardiovasc Imaging. 2020;21(4):446–453. doi: 10.1093/ehjci/jez157. [DOI] [PubMed] [Google Scholar]
- 37.Evin M, Cluzel P, Lamy J, Rosenbaum D, Kusmia S, Defrance C, et al. Assessment of left atrial function by MRI myocardial feature tracking. J Magn Reson Imaging. 2015;42(2):379–389. doi: 10.1002/jmri.24851. [DOI] [PubMed] [Google Scholar]
- 38.Lamy J, Soulat G, Evin M, Huber A, de Cesare A, Giron A, et al. Scan-rescan reproducibility of ventricular and atrial MRI feature tracking strain. Comput Biol Med. 2018;92:197–203. doi: 10.1016/j.compbiomed.2017.11.015. [DOI] [PubMed] [Google Scholar]
- 39.Losi MA, Betocchi S, Aversa M, Lombardi R, Miranda M, D'Alessandro G, et al. Determinants of atrial fibrillation development in patients with hypertrophic cardiomyopathy. Am J Cardiol. 2004;94(7):895–900. doi: 10.1016/j.amjcard.2004.06.024. [DOI] [PubMed] [Google Scholar]
- 40.Bongini C, Ferrantini C, Girolami F, Coppini R, Arretini A, Targetti M, et al. Impact of genotype on the occurrence of atrial fibrillation in patients with hypertrophic cardiomyopathy. Am J Cardiol. 2016;117(7):1151–1159. doi: 10.1016/j.amjcard.2015.12.058. [DOI] [PubMed] [Google Scholar]
- 41.Lee SP, Ashley EA, Homburger J, Caleshu C, Green EM, Jacoby D, et al. Incident atrial fibrillation is associated with myh7 sarcomeric gene variation in hypertrophic cardiomyopathy. Circ Heart Fail. 2018;11(9):e005191. doi: 10.1161/CIRCHEARTFAILURE.118.005191. [DOI] [PubMed] [Google Scholar]
- 42.Neubauer S, Kolm P, Ho CY, Kwong RY, Desai MY, Dolman SF, et al. Distinct subgroups in hypertrophic cardiomyopathy in the NHLBI HCM Registry. J Am Coll Cardiol. 2019;74(19):2333–2345. doi: 10.1016/j.jacc.2019.08.1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spencer KT, Mor-Avi V, Gorcsan J, 3rd, DeMaria AN, Kimball TR, Monaghan MJ, et al. Effects of aging on left atrial reservoir, conduit, and booster pump function: a multi-institution acoustic quantification study. Heart (British Cardiac Society) 2001;85(3):272–277. doi: 10.1136/heart.85.3.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maceira AM, Cosin-Sales J, Prasad SK, Pennell DJ. Characterization of left and right atrial function in healthy volunteers by cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2016;18(1):64. doi: 10.1186/s12968-016-0284-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weil BR, Techiryan G, Suzuki G, Konecny F, Canty JM. Adaptive reductions in left ventricular diastolic compliance protect the heart from stretch-induced stunning. JACC Basic Transl Sci. 2019;4:527–41. doi: 10.1016/j.jacbts.2019.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Reproducibility of strain parameters. Table S2. Diagnostic accuracy of predicting new onset AF. Table S3. Differences in age and rate of hypertension between those with and without sarcomeric variants. Figure S1. Flow chart showing inclusion of subjects. Figure S2. Survival curve for HCM patients.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.