Abstract
Cervical thymic cysts (CTCs) represent 1% of all cervical cystic masses. A review of the literature found that CTCs are typically asymptomatic, with a propensity to be left sided. CTCs often require histological evaluation for diagnosis. A 27-year-old male patient presented to an outpatient otolaryngology clinic with worsening bilateral jaw and neck pain and an incidental right-sided neck mass found on cervical MRI. Preoperative differential diagnosis included venolymphatic malformation versus branchial cleft cyst. Histological examination of the excised specimen provided diagnosis of a CTC. Postoperatively, the patient reported improvement in cervical pain. CTCs are a rare cause of lateral neck mass in young adults. Typical presentation included neck enlargement with no symptoms or in some cases compressive symptoms. It is important to consider CTCs when formulating a differential for a lateral neck mass.
Keywords: ear, nose and throat/otolaryngology, pathology, radiology, surgery, head and neck surgery
Background
Cervical thymic cysts (CTCs) represent 1% of all cervical cystic masses.1 A literature review found that as of 2011, there were only 36 documented cases of CTCs in adults.2 CTCs are benign lesions that are most often asymptomatic. Most cases of CTC occur in infants or children and very rarely occur in adults. CTCs are not considered in a differential diagnosis for lateral neck masses due their rarity.3 We report a case of an atypically symptomatic CTC that was diagnosed post excision in an adult.
Case presentation
A 27-year-old man presented to the outpatient otolaryngology clinic with a 4-year history of bilateral aural fullness and otalgia, with extension of the pain through the anterior border of bilateral sternocleidomastoid muscles down to the sternum. The patient had an additional complaint of globus sensation. The pain was exacerbated by eating and speaking and alleviated with warm compress and over the counter pain medications. The patient denied dyspnoea, dysphagia and dysphonia. The patient’s medical history was non-contributory.
Investigations
Workup had been initiated at an outside medical practice for temporomandibular joint (TMJ) syndrome. Laboratory examination demonstrated no leukocytosis with no elevation of erythrocyte sedimentation rate. Viral serology, including HIV and Epstein-Barr virus (EBV), were negative. An MRI of the TMJ partially imaged an incidental finding of a right neck mass. Subsequent cervical contrast MRI identified a right neck mass of the anterior cervical space (figure 1). The mass appearance was most compatible with a venolymphatic malformation versus branchial cleft cyst, with no mass effect on adjacent structures. A CT scan with contrast was performed to further characterise the lesion and it identified a cervical mass with smooth margins and thin/imperceptible walls (figure 2). Due to chronicity of the patient’s symptoms and findings on exam, surgical excision of the mass was planned.
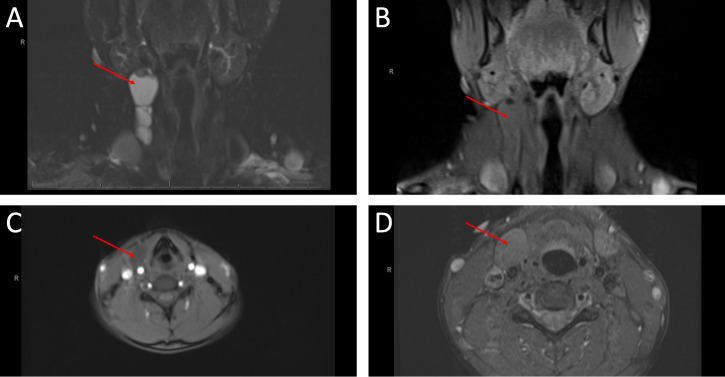
Figure 1.
MRI images, in the coronal (A, B) and transverse (C, D) planes, showing a right anterior cervical mass, measuring 2.8 cm×2.0 cm×5.7 cm with a non-contrast enhancing T2 hyperintense septated cystic component.
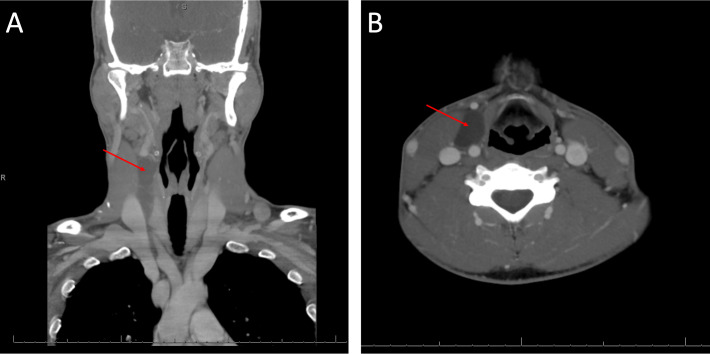
Figure 2.
CT images, in the coronal (A) and transverse (B) planes, with contrast showing no definite enhancing component. The mass ended 2.5 cm above the sternal notch at the right of the midportion of the right thyroid lobe.
Treatment
Surgical approach was through a horizontal incision over and anterior to the right sternocleidomastoid muscle at the level halfway between the hyoid bone and the cricoid cartilage. The cyst was identified to lie external to the carotid sheath with no gross attachments to surrounding structures, extending from level of the hyoid to the level of the cricoid cartilage. Blunt dissection was used to delineate the mass and it was excised with no clearly identified pedicle.
Macroscopically, the specimen consisted of a gray-purple cystic mass with prominent vasculature measuring 10.6 cm×2.0 cm×1.9 cm. The cyst cavity was multilocular, smooth and contained slightly thick and light brown material. Histologically, the cystic lesion was lined by squamous and respiratory type epithelium and the cyst wall was composed of lymphoid aggregates containing Hassall corpuscles. The cyst wall also contained cholesterol granulomas and parathyroid parenchyma. The histologic findings were consistent with a CTC (figure 3).
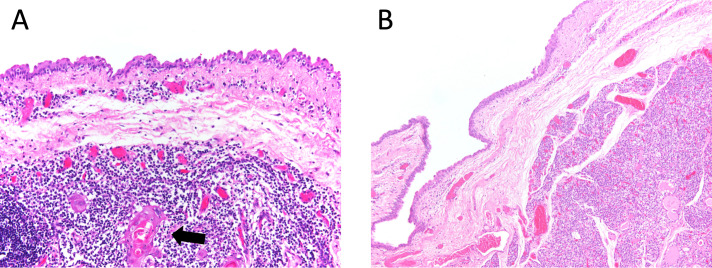
Figure 3.
Histopathological images demonstrate a squamous lined cyst with underlying lymphoid aggregates containing a Hassall corpuscle (A) and a cyst wall lined by non-keratinising squamous epithelium and underlying normocellular parathyroid gland (B).
Outcome and follow-up
At the 2-week postoperative follow-up visit, the patient reported improvement of the bilateral ear and neck pain but continued to have bilateral otalgia that improved with jaw thrust and swallowing. The patient asked to follow-up as needed.
Discussion
The thymus develops from the ventral wing of the third and fourth pharyngeal pouch and descends to the thorax during weeks 7–10 of embryogenesis. The primordial thymus is a tubular structure called the thymopharyngeal duct and it descends to the mediastinum travelling caudally and medially. Then, the thymopharyngeal duct forms the bilobed thymus which serves as the main lymphoid organ through infancy. Thymic tissue can be found later in life anywhere along the path of descent of the thymopharyngeal duct.1 4
The presence of a CTC is rare, but even more rare when found in an adult. Because of the rarity of CTCs, even in children, they are often misdiagnosed.3 A review in 2011 found only 36 documented cases of CTCs in adults. They found that the average age of diagnosis was 36 years, ranging from 18 to 77 years, and that the majority of the adult CTCs were in the left neck (64%), with the rest located on the right (19.4%) or the midline (16.6%). However, there is no explanation for the left side predominance of CTCs. The presence of a neck mass was ubiquitous; however, only 23.3% had other symptoms with the most common being dyspnoea, dysphagia and hoarseness.2 Since this review in 2011, along with this report, there have been more reported cases of CTCs in adults and another comprehensive review might be warranted.5–8
Considering that CTCs tend to appear on the left and tend to be asymptomatic or present with symptoms of dyspnoea, dysphagia and hoarseness, our patient was unique with symptoms of pain and a CTC on the right side. The patient also expressed symptoms of globus sensation, which is reported in the literature, and being a male, he aligns with the 2–3:1 male predominance in CTCs.1
Imaging modalities such as ultrasound, MRI and CT can be used in the diagnosis of CTCs. When compared with ultrasound, MRI can provide better tissue differentiation and is preferred in children with CTCs due to less radiation exposure as compared with CT scan. CT scan can better establish the lesion’s margins and relationship to the surrounding structures like the carotid sheath.1 2
The differential diagnosis of a lateral neck swelling includes thyroglossal duct lesions, branchial cyst, cervical lymphadenopathy, cystic hygroma, dermoid cyst, cystic teratoma, cystic thymoma, cystic metastasis, thyroid and parathyroid cysts, cystic neuroma, tracheo-oesophageal cyst and cervical bronchogenic cyst.1 4 Because of the low incidence of CTCs, they are often not considered in the differential diagnosis and are often diagnosed post excision using histological examination.1–3
Learning points.
Cervical thymic cysts (CTCs) are rare neck lesions, most commonly found in children or adolescents.
CTCs can be found in adults, though this is very rare.
CTCs are benign neck lesions and are often asymptomatic.
CTCs are diagnosed using histology and are often misdiagnosed preoperatively.
Footnotes
Contributors: ZJC and VNS: reviewed published literature and wrote the manuscript. BK and KRN: critically reviewed the manuscript and cared for the study patient. JMVT: wrote the manuscript and photographed the histology slides. All authors read and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Ji H, Gantwerker E. Cervical thymic cysts. Oper Tech in Head Neck Surg 2017;28:183–9. 10.1016/j.otot.2017.05.018 [DOI] [Google Scholar]
- 2.Michalopoulos N, Papavramidis TS, Karayannopoulou G, et al. Cervical thymic cysts in adults. Thyroid 2011;21:987–92. 10.1089/thy.2010.0142 [DOI] [PubMed] [Google Scholar]
- 3.Hendrickson M, Azarow K, Ein S, et al. Congenital thymic cysts in children—Mostly misdiagnosed. J Pediatr Surg 1998;33:821–5. 10.1016/S0022-3468(98)90650-9 [DOI] [PubMed] [Google Scholar]
- 4.Nguyen Q, deTar M, Wells W, et al. Cervical thymic cyst: case reports and review of the literature. Laryngoscope 1996;106:247–52. 10.1097/00005537-199603000-00001 [DOI] [PubMed] [Google Scholar]
- 5.Wahi JE, Delgado R, Medina AM, et al. Rare thymopharyngeal duct cyst presentation in an adult patient. BMJ Case Rep 2021;14:e240160. 10.1136/bcr-2020-240160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith BD, Schild MH, Jiang XS, et al. A rare case of a cervical thymic cyst presenting in adulthood. Case Rep Otolaryngol 2020;2020:1–3. 10.1155/2020/4059530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alzahrani HA, Iqbal JM, Abu Shaheen AK, et al. Cervical thymic cyst in an adult. Case Rep Surg 2014;2014:1–4 https://www.hindawi.com/journals/cris/2014/801745/ 10.1155/2014/801745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krishnamurthy A, Murhekar K, Majhi U. A rare case of multiloculated cervical thymic cyst masquerading as tuberculous adenitis. J Maxillofac Oral Surg 2016;15:375–7. 10.1007/s12663-016-0905-7 [DOI] [PMC free article] [PubMed] [Google Scholar]