Abstract
To address the impact of COVID-19 in the state of Hawai‘i, the Hawai‘i Emergency Management Agency Medical Public Health Branch activated its’ Community Care Outreach Unit (CCO Unit). A team from this unit developed a survey to assess the impact, needs, and threats to the health and social welfare of individuals and their families as they pertain to COVID-19. This article presents key findings for the City and County of Honolulu (CCH).
A total of 5598 CCH residents responded. Approximately half of these respondents reported they or their household members experienced reduced work hours or lost their job as a result of COVID-19. In all questions related to paying for essential living costs, at the time of the survey, the percentage of participants who expected to have future problems nearly doubled. Those preparing for school in the fall school semester expected challenges centered on insufficient funds to purchase school supplies, lack of available face-coverings, and language barriers. Financial assistance, rental assistance, and food assistance seemed to be more difficult to apply for compared to health care services. The most common reasons for difficulty with applications noted by residents included that they could not figure out how to complete the form, did not have all the documents, or could not get through on the telephone.
About one-half of CCH participants reported feeling nervous more than half of the days or nearly every day in the past 2 weeks. Most perceived the severity of COVID-19 to be moderate to very high. Less than half reported knowing how to provide care for someone in their family with COVID-19. Half of the CCH participants reported that they practice social distancing usually or all of the time, and the majority reported wearing a face-covering usually or always when outside of the home. A significant portion of respondents reported barriers for providing care for a household member exposed or infected with COVID-19. Such barriers included a lack of space in their home for isolation; not having enough cleaning supplies; no working thermometer in the home, or no family member available to care for them.
The results presented may provide a baseline for understanding the impact, needs, and threats to the health and social welfare of individuals and their families in CCH and across the state of Hawai‘i. Local stakeholders can utilize this information in developing priorities, strategies, and programs to address the pandemic as it continues to unfold and learn lessons for future pandemics.
Introduction
At the time of this publication the COVID-19 pandemic continues in the state of Hawai‘i and most places across the world. Nearly all communities and countries have been adversely impacted by this historic event. As of July 1, 2021, there have been 36 052 cases, 518 deaths, and 2476 hospitalizations related to COVID-19 recorded in the state of Hawai‘i (HI) since its first case in March 2020.1 The City and County of Honolulu (CCH), which makes up the entire island of O‘ahu, has recorded approximately 27 127 (75.2%) of the state's COVID-19 cases. The CCH is the major hub for business, finance, military, and hospitality in the state, where two-thirds, (approximately 974 563), of the state's 1.41 million people reside.2 COVID-19 has impacted the economy and the health and well-being of the people residing in the CCH. Understanding challenges will help to mitigate the situation and formulate solutions for moving forward.
To address the impact of COVID-19, the state activated the Hawai‘i Emergency Management Agency (HI-EMA) and used the incident command system (ICS) structure to manage the state's pandemic response. Within the ICS Coordinated Medical Services Branch, a Community Care and Outreach Unit (CCO Unit) was formed. The mission of the CCO Unit was to monitor the health and social welfare capacity, needs, and threats to community members due to the COVID-19 pandemic, and to work with community members to recommend mitigation strategies. CCO Unit community partners included leaders from the Native Hawaiian (NH), Pacific Island (PI) and Filipino communities, and organizations that support those who are houseless, aging, or reside in rural communities. The CCO Unit worked with its community partners to develop, distribute, and analyze a survey to assess the impact of COVID-19 and identify support strategies. Assessment data was collected from individuals (N=7927) across the state during a period of 3 weeks (August 12–September 5, 2020). During this time the COVID-19 pandemic in the state was at its peak and public officials and citizens were all very concerned for the health and safety for citizens of the state. The findings for the state as a whole, as well as Maui, Kaua‘i, Hawai‘i counties, and select identified vulnerable populations, are reported elsewhere.3 This report provides findings specific to the CCH.
Methods
Subject-matter experts from the CCO Unit, along with community partners and key health and social service organizations, collaborated to develop the assessment tool, distribute it, analyze results, and develop recommendations related to the impact of COVID-19 on people across the state. The survey included 35 questions that collected information on demographics, health and well-being, finances, social welfare, beliefs, and activities regarding COVID-19.3 The survey also included questions from the Patient Health Questionnaire-4 (PHQ-4) to assess mental health.4
A convenient mixed-methods framework was utilized for the survey distribution and recruitment of adult participants (18 years or older) from across the state, with special outreach to vulnerable populations. Recruitment strategies included snowball sampling via website and social media advertisements, word-of-mouth, and paper surveys that included return postage mailers. Paper surveys were also available for in-person completion at agency sites, community meeting places, and homeless outreach clinics. Community partners were available to assist individuals with completing the survey online or in-person. More details regarding the survey tool and statewide data are available elsewhere.3 The data for the CCH are drawn from the results of the statewide survey.3
Results
Demographics
Of the 7928 responses to the statewide survey, 5960 (75.2%) were from the CCH. Respondents from all CCH zip codes were represented (Figure 1).
Figure 1.
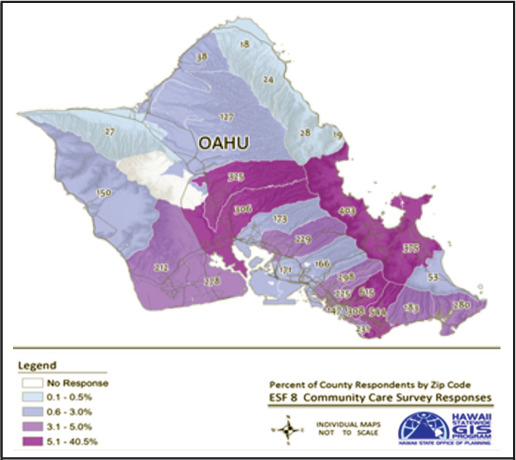
City and County of Honolulu Survey Response by Zip Code
Of the CCH participants who responded to the survey question on gender, 4,027 (68.0%) were female, 1,593 (26.9%) male, and 306 (5.2%) non-binary gender. About one-third of respondents were young adults (18–34 years), one-third were middle-aged (35–54 years), and one-third were older (55+ years). The predominant race/ethnicity groups that participants identified with were Asian, Caucasian, NH, and Filipino. Filipinos were categorized as a separate group because they represent the second largest race/ethnicity group in the state (14.5% identify as Filipino alone, and 25.1% identify as Filipino and another group), and have been identified as a vulnerable population for COVID-19 infection.5 (Table 1).
Table 1.
Demographic Characteristics of City and County of Honolulu Respondents (N=5960) and All Hawai‘i Respondents (N=7927)
| City and County of Honolulu Respondents | Statewide Respondentsa | ||
|---|---|---|---|
| nb | %c | % | |
| Gender | |||
| Male | 4027 | 26.9 | 25.4 |
| Female | 1593 | 68.0 | 69.3 |
| Non-binaryd | 306 | 5.2 | 5.3 |
| Age | |||
| 18–24 | 912 | 15.5 | 14.9 |
| 25–34 | 1039 | 17.7 | 16.6 |
| 35–44 | 1174 | 20.0 | 20.2 |
| 45–54 | 1032 | 17.6 | 17.7 |
| 55–64 | 932 | 15.9 | 16.8 |
| 65+ | 793 | 13.5 | 13.8 |
| Race/Ethnicity | |||
| Caucasian | 1825 | 31.3 | 34.8 |
| Filipino | 712 | 12.2 | 11.6 |
| Japanese | 1295 | 22.2 | 19.4 |
| Chinese | 405 | 6.9 | 5.7 |
| Other Asian | 266 | 4.6 | 3.8 |
| Native Hawaiian | 750 | 12.8 | 14.3 |
| Pacific Islander | 203 | 3.5 | 3.4 |
| African American | 53 | 0.9 | 0.8 |
| Hispanic | 151 | 2.6 | 2.8 |
| Other | 180 | 3.1 | 3.5 |
All respondents in Hawai‘i.3
Totals may not equal to 5960 due to unanswered/missing data.
Percentages may not equal 100% due to unanswered/missing data.
Non-binary refers to the self-reported sexual identity of the survey respondent.
Household Profile
Most CCH respondents lived with other people (89.6%, mean number of people 2.8 per household) vs. living alone. Nearly one-third (33.1%) reported having at least 1 older person > 65 living in their household, and 35.6% had 1 or more children < 18 years in their household. Most CCH respondents (91.8%) reported English as the language most spoken in the home. Seventy-five respondents (1.3%) reported translation needs that were not met.
The median household income range in the CCH was reported as $76,000 to $125,000. This range is consistent with the median Hawai‘i State household income of $83,102.7 About one-third of respondents reported a family income of $75 000 or less. Nearly two-thirds reported their family income decreased due to COVID-19, and about one-third reported this decrease as moderate or large. Approximately half reported they or their household members experienced reduced work hours or lost their job due to COVID-19 (Table 2).
Table 2.
Estimated Income and Impact on Employment and Work Hours Among City and County of Honolulu Respondents (N=5960) Compared to All Hawai‘i Respondents (N=7927) After COVID-19
| City and County of Honolulu Respondents | Statewide Respondentsa | ||
|---|---|---|---|
| nb | %c | % | |
| Household income range | |||
| Less than $40,000 | 897 | 15.07 | 17.19 |
| $41,000 – $75,000 | 1154 | 19.39 | 20.70 |
| $76,000 – $125,000 | 1606 | 26.99 | 26.30 |
| $126,000+ | 1450 | 24.37 | 22.13 |
| Choose not to answer | 844 | 14.18 | 13.67 |
| Impact of COVID-19 on household income | |||
| No | 2509 | 42.2 | 39.9 |
| Yes, a little | 1482 | 24.9 | 24.4 |
| Yes, a moderate amount | 1044 | 17.5 | 18.1 |
| Yes, a large amount | 916 | 15.4 | 17.6 |
| Impact on employment or work hours | |||
| No effect | 2293 | 38.6 | 37.0 |
| Increased work hours | 727 | 12.2 | 11.2 |
| Reduced work hours | 1871 | 31.5 | 32.2 |
| Lost job | 1054 | 17.7 | 19.6 |
All respondents in Hawai‘i.3
Totals may not equal to 5960 due to unanswered/missing data.
Percentages may not equal 100% due to unanswered/missing data.
Digital Connectivity
The large majority of CCH respondents reported having internet access (99.4%); and 99.1% also reported having access to a working cell phone.
Housing
Participants were asked to report where they live, and if they thought they were likely to live at that same place in 3 months. The majority of CCH respondents (96.3%) reported living in a home or condo that they own or rent, and 81.0% reported they were likely to be living in the same domicile in 3 months. Some (3.4%) reported being houseless but living in another person's home or apartment, while 4.0% expect to live in another's home in 3 months. The percentage living in a public shelter, tent, car, or outside was 0.3%, and this was projected to rise to 0.5% in 3 months’ time (Table 3).
Table 3.
Housing Situation Today and Likely in 3 Months Among City and County of Honolulu Respondents (N=5960) Compared to All Hawai‘i Respondents (N=7927)
| Housing arrangement | City and County of Honolulu Respondents | Statewide Respondentsa | ||
|---|---|---|---|---|
| TODAY where do you live? | Where are you most likely tolive in 3 MONTHS? | TODAY where do you live? | Where are you most likely tolive in 3 MONTHS? | |
| nb (%)c | nb (%)c | n (%) | n (%) | |
| A home, condo, or apartment that you OWN. | 3385 (57) | 2827 (47.6) | 4588 (58.2) | 3803 (48.2) |
| A home, condo, or apartment that you RENT. | 2336 (39.3) | 1982 (33.4) | 3005 (38.1) | 2578 (32.8) |
| Houseless, live with others that you know, in their home or apartment. | 203 (3.4) | 235 (4.0) | 272 (3.5) | 317 (4.0) |
| Houseless, live in a public shelter. | 16 (0.3) | 24 (0.4) | 22 (0.3) | 32 (0.4) |
| Houseless, live in a tent, car, or outside. | 4 (0.1) | 45 (0.8) | 13 (0.2) | 70 (0.9) |
All respondents in Hawai‘i.4
Totals may not equal to 5960 due to unanswered/missing data.
Percentages may not equal 100% due to unanswered/missing data.
Daily Essentials
Participants were asked to report any problems they were currently experiencing paying for essentials, and if they anticipated problems paying for such in 3 months. At the time of the survey, respondents were experiencing difficulty and also expected future difficulties paying for food (16% currently, 21.2% in 3 months), rent/mortgage (13.9% currently, 27.0% in 3 months), auto expenses (12.5% currently, 22.4% in 3 months), utility bills (13.0% currently, 21.6% in 3 months), cell/internet costs (12.2% currently, 20.0% in 3 months), health care/medicines (17.5% currently, 31.6% in 3 months), child/elder care (5.0% currently, 9.0% in 3 months), and public transportation (4.3% currently, 7.0% in 3 months) (Table 4).
Table 4.
Current and Expected Future Difficulties With Having Enough Money To Pay for Essentials Among City and County of Honolulu Respondents (N=5960)
| Essential | City and County of Honolulu Respondents | |
|---|---|---|
| Today | In 3 months | |
| n (%) | n (%) | |
| Food | 690 (11.7) | 1259 (21.2) |
| Rent or mortgage | 824 (13.9) | 1600 (26.9) |
| Auto expenses (e.g., gas, insurance, car payments) | 744 (12.6) | 1330 (22.4) |
| Medicines | 478 (8.06) | 874 (14.7) |
| Utility bills (e.g., electric, water, cable, internet) | 773 (13.0) | 1284 (21.6) |
| Cell phone, internet, cable bill | 727 (12.2) | 1191 (20.1) |
| Childcare/ elder care | 296 (5.0) | 535 (9.0) |
| Health care | 561 (9.5) | 1002 (16.9) |
| Public transportation | 253 (4.3) | 415 (7.0) |
| Other debts | 882 (14.9) | 1408 (23.7) |
Nearly half of CCH respondents (n=2,595) expected to have someone in the household in school in fall 2020. Expected challenges in the fall school semester centered on lack of funds to purchase school supplies (n=623; 10.5%), lack of face-coverings (n=340; 5.7%); and language barriers (n=84; 1.4%).
Attempt at Applying for Assistance Benefits
Respondents were asked about success with any applications for assistance benefits in the areas of finance, food, or health services (Table 5). Financial assistance, rental assistance, and food assistance seemed to be more difficult to apply for compared to health care services. Among CCH respondents, the most common reasons for difficulty reported were related to not being able to figure out how to complete the form, did not have all of the documents, or could not get through on the telephone.
Table 5.
Summary of Outcomes When Applying for Assistance Among City and County of Honolulu Respondents (N=5960)
| Type of Assistancea | If YES, applied for assistance, were you able to complete the application? | If you could not complete the application: Reason(s) [Check all that apply] | |||||
|---|---|---|---|---|---|---|---|
| Yes | No | No internet access | Could not figure out how to navigate the form | Did not have all the documents | Did not understand questions in English | Tried to call on phone but could not get through | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Prequalification for financial hardship relief | 457 (82.79) | 95 (17.21) | 4 (4.21) | 32 (33.68) | 42 (44.21) | 3 (3.16) | 47 (49.47) |
| Rental assistance | 129 (71.67) | 51 (28.33) | 5 (9.8) | 11 (21.57) | 19 (37.25) | 3 (5.88) | 23 (45.10) |
| Food | 406 (84.58) | 74 (15.42) | 2 (2.70) | 22 (29.73) | 26 (35.14) | 2 (2.70) | 22 (29.73) |
| Health insurance | 864 (96.21) | 34 (3.79) | 4 (12.12) | 14 (42.42) | 15 (45.45) | 4 (12.12) | 16 (48.48) |
| Healthcare benefits (e.g., Quest or WIC) | 583 (93.88) | 38 (6.12) | 2 (5.26) | 13 (34.21) | 16 (42.11) | 2 (5.26) | 16 (42.11) |
Abbreviation: WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Type of assistance applied for in Hawai‘i between August 12, 2020, and September 5, 2020.
Chronic Disease Burden
More than one-half of the CCH participants reported at least 1 person in their household had at least 1 chronic disease. Asthma, diabetes, and obesity were the most common. The burden of chronic disease in CCH households is similar to the burden statewide (Table 6).
Table 6.
Chronic Disease Burden Among Among City and County of Honolulu Respondents (N=5960) Compared to All Hawai‘i Respondents (N=7927)
| City and County of Honolulu Respondents | Statewide Respondentsa | ||
|---|---|---|---|
| n | % | % | |
| Chronic disease | |||
| Asthma | 1477 | 24.9 | 25.5 |
| Diabetes | 1172 | 19.8 | 19.1 |
| Obesity | 1098 | 18.5 | 18.8 |
| Mental health illness | 885 | 14.9 | 15.0 |
| Heart disease | 740 | 12.5 | 12.6 |
| Cancer | 325 | 5.5 | 5.3 |
| Kidney disease | 239 | 4.0 | 3.8 |
| Lung disease | 193 | 3.3 | 3.3 |
All respondents in Hawai‘i.3
Usual Source of Health Care
The majority of CCH respondents (71.0%) reported that they went to a family doctor's office for health care, followed by a hospital-based clinic (20.1%), and community health center (10.3%). Some (8.5%) reported using the emergency department as their usual source of health care or having no usual source of health care (Table 7).
Table 7.
Usual Source of Health Care Among City and County of Honolulu Respondents (N=5960) Compared to All Hawai‘i Respondents (N=7927)
| City and County of Honolulu Respondents | Statewide Respondentsa | ||
|---|---|---|---|
| n | % | % | |
| Usual source of healthcare | |||
| Family doctor office | 4221 | 71.0 | 70.9 |
| Community health center/or community | 609 | 10.3 | 12.4 |
| Hospital-based clinic | 1195 | 20.1 | 17.6 |
| Emergency department | 223 | 3.8 | 4.0 |
| Have no usual source of healthcare | 250 | 4.2 | 4.4 |
| Other | 258 | 4.4 | 4.9 |
All respondents in Hawai‘i.3
Mental Health
The survey included the 4 questions from the PHQ-4 to assess emotions related mental health.4 About half (54 %) of CCH respondents reported feeling emotions of being nervous, worried, having little pleasure, or feeling down at least several days over the past 2 weeks. About one-third (33.5%) reported feeling nervous more than half of the days or nearly every day in the past 2 weeks, and 24.3% reported feeling worried more than half or nearly every day in the past 2 weeks.
A mental health score was computed for each emotion and 26.4% of CCH respondents had moderate or severe negative mental health scores (Table 8). The mental health impact on CCH residents was found to be similar with that of respondents in other counties in Hawai‘i.
Table 8.
Mental Health Scores Among City and County of Honolulu Respondents (N=5960) Compared to All Hawai‘i Respondents (N=7927)
| City and County of Honolulu Respondents | Statewide Respondentsa | ||
| n | % | % | |
| Level of anxiety/ depression emotions | |||
| Normal (0–2) | 2727 | 45.9 | 45.5 |
| Mild (3–5) | 1644 | 27.7 | 27.6 |
| Moderate (6–8) | 915 | 15.4 | 15.5 |
| Severe (9–12) | 654 | 11.0 | 11.5 |
All respondents in Hawai‘i.3
Personal Beliefs and Activities Regarding COVID-19 Prevention
The majority of CCH respondents consider COVID-19 quite serious, 83.2% consider it highly or very highly serious. There was a moderate level of knowledge among CCH respondents about which groups are more at-risk for contracting severe COVID-19, 67.8% knew it was the elderly and those with chronic disease; 69.1% would be able to recognize if a family member with COVID-19 needed to go to the hospital; and 62.7% knew where to go for COVID-19 testing. However, only 38% reported knowing how to provide care for someone in their family with COVID-19.
More than half (58.4%) of CCH respondents reported practicing social distancing usually or all of the time; 77.5% reported wearing face-coverings usually or all of the time; and 91% reported their family members wash their hands the same or more often. About three-fourths (77%) reported they have a working thermometer in their home.
Multiple significant resource barriers for caring for a family member with COVID-19 were identified: 56.2% reported a lack of space in their home for isolation; 32.1% reported insufficient cleaning supplies; and 54.7% reported that if they got COVID-19 there would be a family member available to care for them (Table 9).
Table 9.
Factors for COVID-19 Household Preparedness and Response Among City and County of Honolulu Respondents (N=5960)
| n | % | |
|---|---|---|
| Attitude Questions | ||
| Perceived Severity of COVID-19 | ||
| Not serious | 83 | 1.4 |
| Low level | 209 | 3.5 |
| Moderate level | 701 | 11.8 |
| High level | 1788 | 30.0 |
| Very high level | 3171 | 53.3 |
| Knowledge Questions | ||
| Know vulnerable populations (elderly and chronic disease) | 4041 | 67.8 |
| Know where to go for COVID-19 testing | 3737 | 62.8 |
| Know how to provide medical care for someone at home with COVID-19 | 2285 | 38.4 |
| Able to recognize when a family member with COVID-19 would need to go to the hospital | 4096 | 69.1 |
| Behavior Questions | ||
| Usually or Always practice social distancing by staying at least 6 feet away from others when not at home | 3477 | 58.4 |
| Usually or Always wear a face-covering when outside of your home | 4615 | 77.5 |
| Family members wash hands the same frequency or More frequently since COVID-19 | 5409 | 91.0 |
| Have a thermometer that works at home | 4583 | 77.1 |
| Resources Questions | ||
| Problems would face if someone respondent lives with had COVID-19 | ||
| Lack of space for isolation | 3344 | 56.2 |
| NO face mask | 137 | 2.3 |
| NO hand sanitizer | 336 | 5.7 |
| NO access to a thermometer | 776 | 13.1 |
| Not enough cleaning supplies | 1909 | 32.1 |
| Have someone be available to care for you if you got COVID-19 | 3254 | 54.8 |
Overall household preparedness for COVID-19 scores were computed based on answers to the COVID-19 attitudes, knowledge, behaviors, and resources on hand questions. Most CCH respondents regarded COVID-19 as being highly serious (83.4%); more than half had a low level of knowledge about the disease and how to care for a family member with COVID-19 (51.9%); most had a moderate to high level of compliance with COVID-19 prevention measures (93.1%); and a significant proportion (46.5%) reported a moderate to high level of need for resources to address COVID-19 (Table 10).
Table 10.
Overall Household Preparedness for COVID-19 Among City and County of Honolulu Respondents (N=5960)
| n | % | |
|---|---|---|
| Attitude - Perceived Severity of COVID-19 (total 1 question) | ||
| Levels | ||
| Low (none-low) | 292 | 4.9 |
| Moderate (mod) | 701 | 11.8 |
| High level (high-very high) | 4959 | 83.4 |
| Knowledge (total 4 questions) | ||
| Low level of knowledge (0–2) | 3094 | 51.9 |
| Moderate level of knowledge (3) | 1684 | 28.3 |
| High level of knowledge (4) | 1182 | 19.8 |
| Behaviors – compliance with measures (total 4 questions) | ||
| Low level of compliance (0–1) | 416 | 7.0 |
| Moderate level of compliance (2–3) | 3254 | 54.7 |
| High level of compliance (4) | 2284 | 38.4 |
| Resources needed (total 6 questions) | ||
| None (0) | 1330 | 22.3 |
| Low level of needs (1) | 1859 | 31.2 |
| Moderate level of needs (2–3) | 2355 | 39.5 |
| High level of needs (4–6) | 415 | 7.0 |
Best source of Accurate Information
While many sources of information were reported, most CCH respondents used the Centers for Disease Control and Prevention (CDC) websites, followed by the Hawai‘i Department of Health websites for information about the pandemic (Table 11).
Table 11.
Usual Sources of Information About COVID 19 Among City and County of Honolulu Respondents (N=5960) Compared to All Hawai‘i Respondents (N=7927)
| City and County of Honolulu Respondents | Statewide Respondentsa | ||
|---|---|---|---|
| n | % | % | |
| Source of information | |||
| Church leader | 22 | 0.4 | 0.5 |
| Community leader | 71 | 1.2 | 1.6 |
| Local community organization | 55 | 1.0 | 1.2 |
| Department of Health website | 1060 | 18.0 | 19.1 |
| Centers for Disease Control and Prevention website | 3173 | 53.7 | 52.4 |
| TV News Reports | 751 | 12.7 | 11.6 |
| Other source | 777 | 13.2 | 13.7 |
All respondents in Hawai‘i.3
Burden of Challenges by Specific Groups in the CCH
All data in this assessment survey were further analyzed by race/ethnic group relative to capacity for COVID-19 awareness, preparedness, and response. Disparities were found among groups in terms of available resources, existing burden of chronic disease in the household, challenges for returning to school, and emotional stress related to the COVID-19 pandemic (Table 12). In general, PI respondents faced more challenges in every category, compared to other vulnerable groups in the state. NH and Filipinos experienced more challenges compared to Caucasian and Asian CCH respondents.
Table 12.
Challenges for Specific Groups Among City and County of Honolulu Respondents (N=5960)
| Caucasian n (%) | Filipino n (%) | Asian n (%) | Native Hawaiian n (%) | Pacific Islander n (%) | Other n (%) | |
|---|---|---|---|---|---|---|
| Connectivity | ||||||
| NO access to internet | 4 (0.2) | 4 (0.6) | 8 (0.4) | 6 (0.8) | 9 (4.6) | 5 (1.3) |
| NO working cell phone | 16 (0.9) | 5 (0.7) | 12 (0.6) | 3 (0.4) | 8 (4.0) | 6 (1.6) |
| Household burden of chronic disease | ||||||
| Household has one or more people living with chronic disease | 885 (48.5) | 433 (60.9) | 1081 (55.0) | 528 (70.4) | 135 (66.5) | 220 (57.3) |
| Challenges going back to school | ||||||
| Language barrier | 8 (0.4) | 15 (2.2) | 28 (1.4) | 3 (0.4) | 21 (10.7) | 7 (1.8) |
| Lack of face covering | 45 (2.5) | 65 (9.2) | 110 (5.6) | 56 (7.6) | 27 (13.7) | 26 (6.8) |
| Lack of funds to buy school supplies | 120 (6.6) | 119 (16.8) | 107 (5.5) | 136 (18.3) | 72 (35.5) | 52 (13.6) |
| Other – computer, internet, etc. | 375 (20.6) | 231 (32.6) | 412 (21.0) | 228 (30.7) | 64 (31.8) | 99 (25.9) |
| Household chronic disease | ||||||
| Household has one or more people living with chronic disease | 885 (48.5) | 433 (60.8) | 1081 (55.0) | 528 (70.4) | 135 (66.5) | 220 (57.3) |
| Emotional stress level | ||||||
| Normal | 855 (46.9) | 308 (43.4) | 976 (49.8) | 311 (41.7) | 80 (39.8) | 152 (39.7) |
| Mild | 511 (28.0) | 187 (26.4) | 524 (26.8) | 205 (27.5) | 58 (28.9) | 123 (32.1) |
| Moderate/severe | 458 (25.1) | 214 (30.2) | 459 (23.4) | 230 (30.8) | 63 (31.3) | 108 (28.2) |
Discussion
Demographics
The proportion of survey respondents from the CCH (75%) is slightly higher than the proportion of the total CCH population for the state (69%). The ethnic/racial breakdown was proportionate to that of the state, with those identifying as Asian being the highest proportion, followed by Caucasian, and NH.6 The majority of the survey participants from the CCH were female (68.0%), despite the CCH population being approximately half male.6 This higher proportion of female participants is consistent with the common pattern of females serving as the managers and reporters for their families’ health care needs.7
Household Profile
The impact of COVID-19 on household income has been quite serious. The cost of living in the CCH is among the highest in the US. The CCH serves as the major economic center of the state, and tourism is the primary industry. However, the pandemic has limited tourism and forced many businesses to furlough or lay off employees. Half of CCH respondents reported reduced household income, reduced work hours, or job loss within their household. Likewise, the unemployment rate in urban Honolulu increased from 2.8% in January 2020 to 12.4% in November 2020.9 More than a quarter (26.4%) of respondents reported a moderate to high degree of anxiety and depression emotions at the time of this survey. There is a strong relationship between economic stress and domestic violence, and during the COVID-19 pandemic, economic stress has been coupled with stay-at-home orders, which has likely exacerbated domestic stressors.8 Between March and October 2020 the Hawai‘i Domestic Violence Action Center experienced a 46% increase in calls to its helpline.9 CCH policymakers should continue to introduce measures to mitigate rising unemployment such as public job work initiatives or work retraining programs.
In the CCH, the PI population continues to be particularly vulnerable. This group had the highest unemployment rate and percentage of households living in poverty.10 Additionally, the PI population experienced 26% of all COVID-19 cases in Hawai‘i, yet constitute only 4% of the state's total population.1 To address this and other vulnerable populations, the CCH recommended widespread community involvement in COVID-19 education, emergency response, and policy planning. Cultural practices that may impact COVID-19 transmission (such as funerary practices or family traditions) have been examined, and accommodations that support health and cultural safety continue to be supported within the community.
Housing
This survey demonstrated that most (96.3%) of CCH respondents lived in a home they owned or rented; however, 15.3% fewer said that would likely be true in 3 months. Thus the percentage of houseless participants will likely increase in the future. Of all Hawai‘i counties, the CCH has the largest houseless population, with an estimated 6448 either sheltered or unsheltered homeless people in 2019.11 Participants reported they currently had difficulty paying expenses or expected to have such difficulty in the future. Community members responses suggested urgent action to extend moratoriums on rental evictions and allow delays in mortgage payments to avoid increases in homelessness in the CCH.
Mental Health
Approximately half of survey participants reported that they felt worried or stressed due to the pandemic, with a quarter reporting moderate or severe negative emotions. Furthermore, existing inequities across the social determinants of health that have been linked to higher rates of chronic conditions, such as obesity and diabetes, continue to exacerbate the risks for severe symptoms and consequences of COVID-19.12 The PI population reported the highest stress levels, followed by NH and Filipino groups. Programs to address the social determinants of health must be strengthened, and culturally appropriate mental health services need to be developed and made available to all groups across the CCH. These types of services are often best delivered by individuals with a sound understanding of the groups to be served. Community health workers from the underserved communities should be trained to assist with providing culturally appropriate care, public messaging and policies. Hawai‘i supported federal funding restoration of Medicaid for Compact of Free Association (COFA) residents in the state and now must continue its’ efforts to restore access to care for COFA residents.
Usual Source of Health Care
Eight percent of CCH respondents reported they either had no source of usual healthcare or used the emergency department as a usual source of care. This highlights the importance of community health centers (CHC) located in the CCH. Concerted efforts should be made to link all CCH residents to a source of usual health care, such as a CHC.
Personal Beliefs and Activities Regarding COVID-19 Prevention
Most CCH respondents recognized the seriousness of COVID-19, knew which groups are more at-risk, and would recognize if a family member needed testing or to go to a hospital. However, only about a third would know how to care for a family member with severe COVID-19. This is concerning as in areas where COVID-19 vaccination rates are low hospitalizations due to the disease may continue to rise. As of June 23, 2021 disparities in COVID-19 vaccination rates among race/ethnic groups and zip codes in the CCH continue. Proportionally, NH and Filipino residents as well as those from lower income zip codes are much less likely to be vaccinated.13 Culturally appropriate COVID-19 vaccination outreach must continue to reduce these vaccination rate disparities. In the survey, the PI group specifically noted a shortage of personal protective equipment and cleaning supplies. Such equipment should be made publicly available for those in need through the CHCs. Public messaging that is targeted toward different groups must be crafted and delivered across the CCH. Individuals need specific instructions and tools that make sense to them within the context of their culture to reduce the spread of COVID-19. In response to these findings, the Public Health Nursing Branch of the Hawaii Department of Health led efforts to develop a culturally appropriate booklet that focuses on home care for persons with COVID-19. This provides an example of governmental timely responsiveness to community needs during the pandemic. It is important to note that many other state agencies also made revisions or additions to services offered to support the public during the pandemic. Such efforts need to continue to be funded as the pandemic continues.
Best Source of Accurate Information
Respondents reported many sources for gathering information on COVID-19. Most CCH respondents reported that they use the CDC website, followed by the Hawai‘i Department of Health website. Public health workers should assure that information on these websites appears in multiple languages to increase access to reliable, accurate information. Only a small percentage of the CCH respondents reported that they called 211 for social service assistance, reporting mixed results for resolution of their issues. Access to assistance could be strengthened by partnerships with local community organizations that are more closely connected to vulnerable groups such as PI, NH and Filipinos in the CCH.
The COVID-19 pandemic revealed gaps in internet access. A small percentage of disadvantaged and underserved populations struggled with access as the needs for use of online portals have increased for schools, businesses, and social services.14 Cost may be a factor, as internet access requires computers and service plans. Understanding where to find information and how to decipher it requires both digital and health literacy. Lower levels of health literacy is associated with poorer health outcomes for NH, PI, and Filipino populations.15 Thus, culturally relevant information and engagement is needed to educate and inform vulnerable populations about COVID-19 prevention and response. Websites that are easy to navigate and contain relevant, understandable information must be developed for each key vulnerable group in the CCH. Community members should be involved in developing and maintaining such sites.
Limitations
A convenience-sampling frame was used; all responders were self-selected and there is no way to determine an actual response rate. Therefore, the report results must be viewed within the context of potential self- selection bias. In addition, while the survey was available in both paper form and online, the vast majority of respondents participated online. Thus, there is a chance that those with no access to the internet and hidden groups, such as the houseless, may not be adequately represented in the sample. In addition, all data were self-reported and not verified. However, there are consistent trends in responses across respondents from all of Hawai‘i counties, which lends credence to the findings. To mitigate some of these concerns, the community partners reviewed and corroborated the results.
Conclusion
Overall, the results from the CCH were consistent with statewide responses. Many challenges lay ahead for those who have reduced employment and income, as many businesses may not recover from the closures, and when tourism will fully return is still uncertain. Those in the middle class, who are used to having food and resources, may struggle in the near future. This group is generally not savvy with regards to applying for benefits and if the pandemic continues, will likely require additional support in order to access assistance services. Further, despite most participants understanding the severity of COVID-19, lack of space to isolate, pandemic fatigue, and a false sense of complacency due to the low number of cases compared to the continental US may put people at more risk. Inequities in household profile, health and well-being, living expenses, and personal beliefs and activities regarding COVID-19 prevention, show NH, PI, and Filipino groups to be at higher risk. It is clear that adverse social determinants in the CCH negatively impacted the health and social welfare of many. Knowledge may provide a source of comfort and power in dealing with COVID-19 uncertainty and decision-making. Community engagement and effective messaging delivered in a culturally relevant format are needed. Relevant topics may include quarantine and isolation, capacity building, assessments and recommendations to improve recovery and resilience for those most affected. Additionally, community groups recommended that the government should take steps to reduce income inequalities through a variety of mechanisms, such as increasing the minimum wage, assuring availability of affordable housing, creating job opportunities, and supporting workforce training programs. Moving forward in these areas will help support resilience during and in the aftermath of the COVID-19 pandemic across the CCH.
This report was distributed widely to constituent groups, policy makers, and organizations that served the health and social needs of the state's citizens in order to inform decisions regarding allocation of resources to mitigate the effects of COVID-19 on the population.
Acknowledgement
The entire CCO Unit wishes to acknowledge and thank community partners for their willingness to serve as CCO Unit team members and for their guidance and wisdom along the way.
Abbreviations
- CCH
City and County of Honolulu
- CCO Unit
Community Care Outreach Unit
- CDC
Centers for Disease Control and Prevention
- CHC
community health centers
- COFA
Compact of Free Association
- COVID-19
SARS-CoV-2
- HI
Hawai‘i
- HI-EMA
Hawai‘i Emergency Management Agency
- ICS
incident command system
- NH
Native Hawaiian
- PHQ-4
Patient Health Questionnaire-4
- PI
Pacific Island
Contributor Information
Lee E. Buenconsejo-Lum, John A. Burns School of Medicine, University of Hawai‘i at Mānoa, Honolulu, HI (LEB).
Robin G. Arndt, Thompson School of Social Work & Public Health, University of Hawai‘i at Mānoa, Honolulu, HI (RGA).
Conflict of Interest
None of the authors identify a conflict of interest.
References
- 1.Hawai‘i COVID-19 data. State of Hawai‘i – Department of Health Disease Outbreak Control Division | COVID-19 Website. https://health.hawaii.gov/coronavirusdisease2019/what-youshould-know/current-situation-in-hawaii Updated January 7, 2020. Accessed January 7, 2020.
- 2.County population facts for the state of Hawaii: July 1, 2010 through July 1, 2019. Department of Business, Economic Development & Tourism Census Website. https://census.hawaii.gov/home/data-products/. Published March 26, 2020. Accessed February 1, 2021.
- 3.Qureshi K, Buenconsejo-Lum LE, Palafox N, et al. A Report on the impact of COVID-19 on the health and social welfare in the state of Hawai‘i. Hawai’i J Health Soc Welf. 2021. In press. [PMC free article] [PubMed]
- 4.Kroenke K, Spitzer RL, Williams JB, Löwe B. An Ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50((6)):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 5.Filipino population by county, island and census tract in the state of Hawaii: 2010. State of Hawaii Department of Business, Economic Development & Tourism. Research and Economic Analysis Division, Hawaii State Data Center Website. https://files.hawaii.gov/dbedt/census/Census_2010/SF1/HSDC2010-5_Filipino.pdf Published February 2012. Accessed January 15, 2021.
- 6.QuickFacts Honolulu County, Hawaii. United States Census Bureau Website. https://www.census.gov/quickfacts/honolulucountyhawaii. Published July 1, 2019. Accessed January 12, 2021.
- 7.Kaiser Family Foundation women, work, and family health: key findings from the 2017 Kaiser women's health survey. https://www.kff.org/womens-health-policy/issue-brief/women-workand-family-health-key-findings-from-the-2017-kaiser-womens-health-survey/ Published Mar. 13, 2018. Retrieved January 16, 2021.
- 8.Renzetti CM. Economic stress and domestic violence. University of Kentucky UKnowledge, Faculty Research Reports and Papers, Center for Research on Violence Against Women. https://uknowledge.uky.edu/cgi/viewcontent.cgi?article=1000&context=crvaw_reports. Published 2009. Accessed March 8, 2021.
- 9.Hofschneider A. B. Domestic Violence is on the rise in Hawaii. Honolulu Civil Beat Website. https://www.civilbeat.org/2020/10/domestic-violence-is-on-the-rise-in-hawaii/. Published October 20, 2020. Accessed March 8, 2021.
- 10.Demographic, social, economic, and housing characteristics for selected race groups in Hawaii. Department of Business, Economic Development & Tourism Census Website. https://files.hawaii.gov/dbedt/economic/reports/SelectedRacesCharacteristics_HawaiiReport.pdf. Published March 2018. Accessed January 2, 2020.
- 11.Hawaii housing planning study, 2019. State of Hawaii Department of Business, Economic Development & Tourism Website. https://dbedt.hawaii.gov/hhfdc/files/2020/01/FINAL-State_Hawaii-Housing-Planning-Study.pdf. Published December 2019. Accessed January 12, 2021.
- 12.Kaholokula JK, Samoa RA, Miyamoto RES, Palafox N, Daniels S-A. COVID-19 Special Column: COVID-19 Hits Native Hawaiian and Pacific Islander communities the hardest. Hawai’i journal of health & social welfare. 2020;79((5)):144–146. Accessed December 23, 2020. http://search.ebscohost.com.eres.library.manoa.hawaii.edu/login.aspx?direct=true&db=cmedm&AN=32432218&site=ehost-live. [PMC free article] [PubMed] [Google Scholar]
- 13.Hawaii COVID-19 data. State of Hawaii Department of Health, Disease Outbreak Control Division Website. 2021. Jun 23, https://health.hawaii.gov/coronavirusdisease2019/currentsituation-in-hawaii/#vaccine. Accessed July 12, 2021.
- 14.Hawaii broadband strategic plan. Department of Business, Economic Development & Tourism Census Website. https://broadband.hawaii.gov/wp-content/uploads/2020/11/Hawaii-BB-Plan-2020-FINAL_10-23-20_v1.1.pdf. Published October 2020. Accessed January 2, 2021.
- 15.Sentell T, Baker KK, Onaka A, Braun K. Low health literacy and poor health status in Asian Americans and Pacific Islanders in Hawai’i. Journal of health communication. 2011;16(Suppl 3):279–294. doi: 10.1080/10810730.2011.604390. [DOI] [PubMed] [Google Scholar]


