Abstract
Lifestyle medicine (LM) is an emerging specialty that is gaining momentum and support from around the world. The American Medical Association passed a resolution to support incorporating LM curricula in medical schools in 2017. Since then, the American College of Lifestyle Medicine Undergraduate Medical Education Task Force has created a framework for incorporating LM into medical school curricula. This article provides competencies for medical school LM curriculum implementation and illustrates how they relate to the Association of American Medical College’s Core Entrustable Professional Activities and the LM Certification Competencies from the American Board of Lifestyle Medicine. Finally, standards are presented for how medical schools may receive certification for integrating LM into their curriculum and how medical students can work toward becoming board certified in LM through an educational pathway.
Keywords: medical school education, lifestyle medicine, standards
Incorporating LM into medical school curricula addresses the chronic disease burden by equipping the next generation of physicians with sustainable and scalable tools to treat and reverse chronic disease.
Introduction
It has been more than 10 years since the first publication on lifestyle medicine (LM) competencies. 1 Yet medical schools have been slow to incorporate LM into their curricula, despite the recent growing interest displayed by medical students and medical practitioners. Lifestyle Medicine Interest Groups (LMIGs) affiliated with the American College of Lifestyle Medicine (ACLM) grew 137% in 2020, and ACLM membership has increased by 700% in the past 5 years. 2
Based on the proposal from the American College of Preventive Medicine, the American Medical Association (AMA) House of Delegates adopted a resolution focused on equipping physicians with information and skills for prescribing healthy lifestyle change as medicine. The resolution calls for the AMA to support policies and mechanisms that incentivize or provide funding for inclusion of LM education and the social determinants of health in undergraduate, graduate, and continuing medical education. 3
According to ACLM, LM is the use of evidence-based lifestyle therapeutic interventions—including a whole-food, plant-predominant eating pattern, regular physical activity, restorative sleep, stress management, avoidance of risky substances, and positive social connection—as a primary modality, delivered by clinicians trained and certified in this specialty, to prevent, treat, and often reverse chronic disease. 4 Incorporating LM into medical school curricula addresses the chronic disease burden by equipping the next generation of physicians with sustainable and scalable tools to treat and reverse chronic disease.
In response to the AMA’s recently adopted resolution, the ACLM Undergraduate Medical Education (UME) Task Force utilized an expert consensus process for outlining LM competencies to be integrated into medical school curricula. The ACLM UME Task Force consists of diverse representatives from the University of South Carolina School of Medicine Greenville, A T Still University, Boston University, Harvard, Loma Linda University, and University of Oklahoma College of Medicine as well as administrative staff from ACLM. This article serves to
Share the mission and vision of the ACLM UME Task Force
Provide competencies for medical school LM curriculum implementation and illustrate how they relate to the Association of American Medical College’s (AAMC) Core Entrustable Professional Activities (EPAs) and LM Certification Competencies from the American Board of Lifestyle Medicine (ABLM)
Present standards for medical schools to receive certification for integrating LM into their curriculum
Define how individual medical students may receive recognition for completing LM training in medical school as part of the LM Educational Pathway for ABLM certification
Mission and Vision
The mission of the ACLM UME Task Force is to advance the implementation of LM across all medical schools and to provide strategies that align with each school’s implementation readiness and academic resources.
The vision of the ACLM UME Task Force is that, upon graduation, every medical student will be prepared to perform LM assessments and counseling as a routine standard of care.
Competencies
The following competencies were created by the ACLM UME Task Force within the organization framework of Accreditation Council for Graduate Medical Education Core Competencies 5 and were guided by the 13 Core EPAs as outlined by the AAMC 6 and the LM Certification Competencies from the ABLM. 7 EPAs are tasks or responsibilities that residents should be able to perform on their first day of residency—that is, they are entrusted to perform them unsupervised. 6 Those EPAs that align with the LM competencies are noted in parentheses and can be found in the supplemental information section of this article.
- I. Patient care and procedural skills
- Conduct a comprehensive, lifestyle-focused history and physical examination, including appropriate screenings, to assess the 6 pillars of LM (EPA 1).
- Apply evidence-based LM guidelines for the development of a comprehensive LM assessment and plan for chronic disease prevention, treatment, and reversal, including LM prescriptions (EPA 7).
- Effectively apply clinical reasoning skills when ordering and interpreting appropriate tests to screen, diagnose, and guide the prevention, treatment, and reversal of common lifestyle-related chronic diseases (EPA 3, 7).
- Utilize evidence-based models of health behavior change to assess patients’ readiness and ability to make lifestyle changes (EPA 7).
- Utilize evidence-based behavior change counseling to support patients in lifestyle changes (EPA 7).
- Collaborate in a patient-centered approach with patients and their families to develop evidence-based, achievable, specific, written action plans such as lifestyle prescriptions (EPA 9).
- Apply pharmaceutical knowledge to adjust medication doses as patients adopt a healthier lifestyle (EPA 4, 5).
- Compare effective dosing of LM strategies based on progression and severity of disease (EPA 4).
- II. Medical knowledge
- Discuss the pathophysiology of lifestyle-related chronic diseases.
- Evaluate and discuss the scientific evidence and physiological mechanisms by which lifestyle changes can treat and reverse lifestyle-related chronic disease (EPA 7).
- Discuss how lifestyle-related chronic disease treatment and reversal is dependent on disease severity and LM intervention dose.
- Discuss the 6 pillars of LM and the expected disease prevention, treatment, and reversal outcomes when LM is utilized.
- Demonstrate how the 6 pillars of LM fit into a comprehensive treatment framework, including pharmaceuticals and surgery (EPA 9, 10, 11).
- III. Practice-based learning and improvement
- Critically evaluate national guidelines for alignment with the 6 pillars of LM (EPA 7).
- Utilize resources to locate, interpret, and apply evidence from scientific studies regarding LM to prevent, treat, and reverse lifestyle-related chronic disease (EPA 7).
- Work collaboratively within an interprofessional team dedicated to multifactorial lifestyle change (EPA 9).
- Utilize information technology to optimize the delivery of lifestyle interventions and track changes over time (EPA 5).
- IV. Interpersonal and communication skills
- Collaborate with patients and their family members utilizing effective patient-centered relationship skills and shared decision-making to cultivate confidence and readiness for action (EPA 1, 11).
- Communicate and effectively lead an interprofessional health care team related to LM treatment plans and goals (EPA 8, 9).
- Educate patients, students, residents, and other health professionals on the appropriate use of LM as a sustainable approach for prevention, treatment, and reversal of lifestyle-related chronic disease.
- Tailor lifestyle education based on the health literacy and learning needs of the patient (EPA 1, 2).
- V. Professionalism
- Describe how a physician’s personal LM engagement can benefit patients’ health behaviors.
- Demonstrate compassion, respect, and autonomy for patients, regardless of their readiness or ability to engage in lifestyle change.
- Model an authentic journey of healthful lifestyle choices.
- Demonstrate the ability to perform LM counseling in a culturally competent manner.
- VI. Systems-based practice
- Describe the role of LM within the health care system framework (EPA 9, 13).
- Advocate for policies that support treating the root cause of chronic disease through LM (EPA 13).
- Describe practice systems that support and optimize LM-focused interventions (EPA 13).
- Describe costs of common lifestyle-related chronic diseases at the individual, health care system, and community levels and the impact of LM interventions on cost containment (EPA 13).
- Integrate appropriate LM referrals to community organizations and health care professionals into patient treatment plans (EPA 8, 9).
- Describe how LM can decrease health inequities among populations experiencing higher burdens of chronic disease, including adaptation strategies for patients and populations with limited resources (EPA 13).
Standards
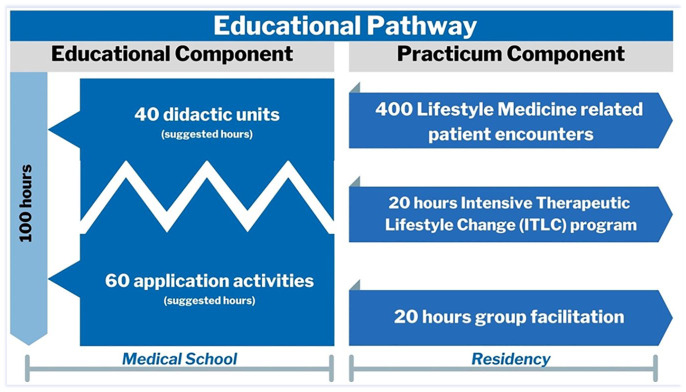
For trainees who wish to qualify for the ABLM exam, an Educational Pathway is available through medical school and residency training. This Educational Pathway in its entirety can be integrated into any residency program; however, the intent of the medical school LM standards is to enable medical students to complete the Educational Component of the Educational Pathway as a stepping stone to residency and ultimately ABLM certification (see Figure 1). The Educational Pathway requires 100 hours of LM education that covers 100% of the UME competencies. A flexible and adaptive model with approximately 40 hours of didactic and 60 hours of application activities is proposed to support the Liaison for Committee on Medical Education’s expectation that individual and unique medical school curricula exist across institutions. This enables each institution to adapt, as necessary, to their unique circumstances and teaching methods. The ACLM UME Task Force recommends that the 100 hours be divided across 10 topic areas to be in alignment with the distribution of the ABLM LM Certification Competencies: (1) introduction to LM; (2) fundamentals of health behavior change; (3) key clinical processes in LM; (4) the role of physician health and the physician’s personal health; (5) nutrition science, assessment, and prescription; (6) physical activity science and prescription; (7) emotional and mental well-being, assessment, and interventions; (8) sleep health science and interventions; (9) managing tobacco cessation and other toxic exposures; and (10) the role of connectedness and positive psychology. 7 Of note, the educational hour requirements discussed below take into consideration the minimum nutrition education recommendation put forth by the National Academy of Sciences. 8 Medical schools implementing these LM standards may apply through the ACLM for medical school certification based on the tier system outlined below and/or recognition to individual medical students based on their level of LM education engagement.
Figure 1.
Proposed Educational Pathway to lifestyle medicine board eligibility in medical school and residency training.
Institutional Tiers
Medical school standard tiers for implementation of LM were developed by the ACLM UME Task Force, an expert consensus panel of medical school faculty and leaders in the field of LM. By using a tiered approach to evaluate LM curriculum integration, the ACLM certifies institutions based on the number of hours students spend in LM training, the percentage of competencies met, and the enrichment opportunities that are available. Academic institutions may fall within 1 of 4 tiers: Platinum, Gold, Silver, or Bronze (Table 1). Institutions may also receive a Platinum Plus, Gold Plus, Silver Plus, or Bronze Plus certification. To receive the “Plus” designation, institutions must provide 100% of the competencies and 100 or more hours of LM curriculum to a subset of medical students through a supplemental LM enrichment track. An enrichment track, such as a specialty, concentration, or elective series, offers in-depth, optional education and mentoring in LM. Every tier must also have a LMIG that is affiliated with ACLM, supported by one or more sponsoring faculty, which engages students in LM educational sessions, workshops, and/or community service projects on campus or within the local community. All competencies and processes are evaluated by the ACLM, and certified institutions are required to submit interim reports to maintain their tier designation.
Table 1.
Tiers of Lifestyle Medicine Certification for Medical Schools.
| Tiers | Platinum | Gold | Silver | Bronze |
|---|---|---|---|---|
| Curriculum hours | ≥100 Hours | 75-99 Hours | 50-74 Hours | 25-49 Hours |
| UME competencies covered | 100% | >75% | >50% | >25% |
| Who/When | All medical students/across all 4 years of training | All medical students/at any point throughout medical school | ||
| Lifestyle Medicine Interest Group (LMIG) | An LMIG is established and affiliated with ACLM, supported by one or more sponsoring faculty, and engages students in Lifestyle Medicine educational sessions, workshops, and/or community service projects on campus or within the local community | |||
| Designation | Platinum Plus a | Gold Plus | Silver Plus | Bronze Plus |
| Institutions can receive a (Plus) designation, on top of their tiered rating, for meeting 100% of the competencies and providing 100 hours of curriculum through the supplementation of the core curriculum with a Lifestyle Medicine Enrichment Track. An enrichment track, such as a specialty, concentration, or elective series, offers in-depth, optional education and mentoring in lifestyle medicine | ||||
Abbreviations: ACLM, American College of Lifestyle Medicine; UME, Undergraduate Medical Education.
Platinum Plus indicates an enrichment track that exceeds the 100% of competencies and 100 hours of curriculum.
Educational Hours and Competencies
ACLM encourages implementing LM concepts and topics into the curriculum throughout all 4 years of medical school to present the content at an optimal time for shaping a student’s understanding and approach to comprehensive patient care. Medical schools may augment preexisting curriculum by incorporating UME competencies into lectures, pathophysiology review, case studies, and clinical application activities in order to meet the recommended standards of LM implementation. The ACLM UME Task Force encourages the first 2 years of medical school LM education to focus on the didactic education of LM, whereas the third and fourth clinical years present opportunities for in-depth, hands-on learning and clinical application of LM.
Certification
In collaboration with the ABLM, ACLM supports the growing demand for a LM Educational Pathway that leads to certification by considering applications from medical schools who meet the outlined standards and competencies. Through an application to ACLM, institutions must demonstrate that their core curriculum and/or enrichment track meets the Education Component of the Educational Pathway. Medical schools are responsible for providing documentation and notifying the ACLM of graduates who have completed their certified programs. To maintain certification, medical schools are required to submit updated documentation every 5 years.
Students who graduate from a Platinum program or students who complete an enrichment program at an institution with a Plus designation will receive an ACLM recognition of completion, verifying that they have fulfilled the prerequisites for the Educational Component of the Educational Pathway. Furthermore, during residency, the Practicum Component may be completed, enabling qualification to sit for the ABLM physician exam. Students interested in completing the Practicum Component requirement during residency have many opportunities across the nation through residencies that have adopted the LM Residency Curriculum (LMRC). Residency programs that offer the LM Educational and Practicum Components through the LMRC grew by 53% from 2019 to 2020. In 2020, 26 residency programs offered the LMRC, qualifying residents to sit for the ABLM exam. 9
Conclusion
The ACLM UME Task Force recognizes that there are many challenges to the implementation of new components within a medical school curriculum. These challenges are addressed and resources and examples of successful LM implementation strategies from other schools are provided in another article in this issue of the American Journal of Lifestyle Medicine. 10
By teaching LM, medical schools have the opportunity to decrease the burden of chronic disease and help train the next generation of physicians to treat the lifestyle-related root cause of disease. As such, medical schools also have the opportunity to receive certification for integrating LM into their curriculum, and medical students may pursue LM board certification through a LM Educational Pathway.
Supplemental Material
Supplemental material, sj-docx-1-ajl-10.1177_15598276211008142 for Undergraduate Medical Education: Lifestyle Medicine Curriculum Implementation Standards by Jennifer L. Trilk, Shannon Worthman, Paulina Shetty, Karen R. Studer, April Wilson, Marianna Wetherill, Lori Whelan, Shipra Bansal, Megan Alexander, Beth Frates, Sylvia Cramer and Brenda Rea in American Journal of Lifestyle Medicine
Acknowledgments
We would like to acknowledge the American College of Lifestyle Medicine, American Board of Lifestyle Medicine, and the Ardmore Institute of Health for their support.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Not applicable, because this article does not contain any clinical trials.
Contributor Information
Jennifer L. Trilk, University of South Carolina School of Medicine Greenville, South Carolina.
Shannon Worthman, American College of Lifestyle Medicine, Chesterfield, Missouri.
Paulina Shetty, American College of Lifestyle Medicine, Chesterfield, Missouri.
Karen R. Studer, Loma Linda University, Loma Linda, California.
April Wilson, Loma Linda University, Loma Linda, California.
Marianna Wetherill, University of Oklahoma, Tulsa, Oklahoma.
Lori Whelan, University of Oklahoma School of Community Medicine, Tulsa, Oklahoma.
Shipra Bansal, AT Still University-School of Osteopathic Medicine in Arizona, Mesa, Arizona.
Megan Alexander, Boston University, Massachusetts.
Beth Frates, Harvard Medical School, Boston, Massachusetts.
Sylvia Cramer, Loma Linda University, Loma Linda, California.
Brenda Rea, Loma Linda University, Loma Linda, California.
References
- 1.Lianov L, Johnson M. Physician competencies for prescribing lifestyle medicine. JAMA. 2010;304:202-203. [DOI] [PubMed] [Google Scholar]
- 2.American College of Lifestyle Medicine. 2020 ACLM annual review. Accessed February 1, 2021. https://lifestyle-medicine.foleon.com/year-in-review/2020-aclm-annual-review/cover/
- 3.American Medical Association. H-425.972 healthy lifestyles. Accessed January 21, 2021. https://policysearch.ama-assn.org/policyfinder/detail/lifestyle%20medicine?uri=%2FAMADoc%2FHOD.xml-0-3746.xml
- 4.American College of Lifestyle Medicine. Accessed January 21, 2021. https://www.lifestylemedicine.org/ACLM/About/What_is_Lifestyle_Medicine_/Lifestyle_Medicine.aspx
- 5.Accreditation Council for Graduate Medical Education. Accessed February 2, 2021. https://acgme.org/
- 6.Association of American Medical Colleges. Core entrustable professional activities for entering residency. Accessed March 23, 2021. https://www.aamc.org/media/20211/download
- 7.American Board of Lifestyle Medicine. How to certify. Accessed January 21, 2021. https://ablm.co/how/
- 8.Adams KM, Kohlmeier M, Zeisel SH. Nutrition education in US medical schools: latest update of a national survey. Acad Med. 2010;85:1537-1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American College of Lifestyle Medicine. The lifestyle medicine residency curriculum (LMRC). Accessed February 1, 2021. https://lifestylemedicine.org/LMRC
- 10.American College of Lifestyle Medicine. The why, what and how of medical education transformation: lifestyle medicine in UME, GME, fellowship and CME. Accessed March 23, 2021. https://www.lifestylemedicine.org/ItemDetail?iProductCode=LM2020_OND3&Category=LM_ONDEM&WebsiteKey=5bd6714c-c023-412c-adcf-a68f63dd5607
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-ajl-10.1177_15598276211008142 for Undergraduate Medical Education: Lifestyle Medicine Curriculum Implementation Standards by Jennifer L. Trilk, Shannon Worthman, Paulina Shetty, Karen R. Studer, April Wilson, Marianna Wetherill, Lori Whelan, Shipra Bansal, Megan Alexander, Beth Frates, Sylvia Cramer and Brenda Rea in American Journal of Lifestyle Medicine