Abstract
A shift occurred in medical school education due to the novel coronavirus disease-19 (COVID-19) pandemic. It has been more than a year since the start of the pandemic, and many medical schools have had to adapt quickly. The medical school curriculum had to be changed in order to accommodate the risk of the virus, which has caused an interruption in clinical education for both preclinical and clinical medical students. Limited hands-on labs, remote standardized patient encounters, telemedicine education and other substitutes have been used to bridge this gap within in-person learning. This review discusses the changes in curricula that some schools have taken, and the benefits and disadvantages of these selected methods.
Introduction
The novel coronavirus disease-19 (COVID-19) has changed life in many ways all over the world. It has especially provided a challenge for the healthcare industry, and demonstrated how quickly this system can become overwhelmed by a pandemic. The future of healthcare rests with medical students as they are future medical workforce. However, the COVID-19 pandemic has had a significant impact on the usual path medical students obtain technical and clinical skill levels, and forced medicals schools to re-imagine how training should appear. While this has propelled innovations, such as, remote/virtual learning and telemedicine, it also has had detrimental effects on hands-on medical training with possible long-term consequences.
This article will present examples of the innovations and adaptations that have occurred as a result of COVID-19 for both preclinical and clinical students and discuss the benefits and pitfalls of these decisions. It will also discuss how medical school preclinical faculty and clinical faculty have changed their methods of teaching through this pandemic. For the purposes of this article, virtual and remote will be used interchangeably.
Preclinical Students
When the pandemic first began, preclinical students were plunged into complete-remote learning systems. In the early months of the pandemic, on-campus and live lectures were immediately turned into remote lectures, prerecorded lectures, voiced over powerpoint presentations, and small group interactive sessions.1,2,3 Gross anatomy turned into video dissections performed by faculty and observed by students remotely.4 With the shock of this sudden transition, faculty and staff scrambled to make this new learning environment work. Faculty and staff were forced to become familiar with web-based platforms (i.e. Zoom, Microsoft Teams, etc.) in order to interact for day to day operations between teaching staff and to deliver education to the students. For some, this was an easy shift, but for others it was a steeper learning curve.5 There was also an increased need for equipment for both students and faculty such as headsets, laptops, and other equipment, which may have been an extra financial burden.4
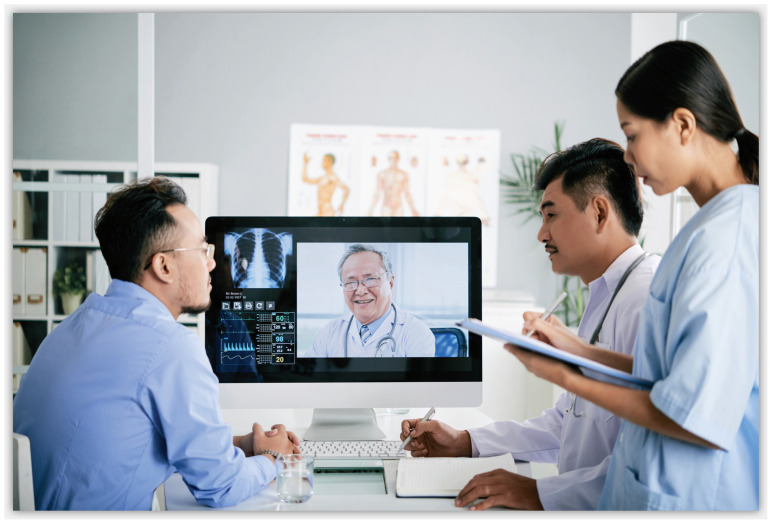
During the pandemic, some medical schools changed their curriculum to implement remote/virtual standardized patient encounter to simulate patient encounters as telemedicine or telehealth.
Although lectures were easily able to shift into remote delivery, clinical courses and skills did not have as smooth of a transition. It was observed that some clinical knowledge could be taught using these remote methods, but students were lacking hands-on training, such as physical exam and other clinical skills. As the pandemic wore on, many schools attempted to rectify this deficiency in hands-on education by implementing in-person physical exam labs. These activities came at a steep monetary and time cost. To mitigate risk and to keep students safe, these in-person activities required smaller groups of students, COVID-19 testing for students and faculty, N95/KN95 masks, goggles, social distancing and faculty monitoring the interaction within that setting. These activities also required more faculty time due to the size limitation of the cohorts who could interact at any given time. This also limited the practice of certain physical exams to reduce risk of virus transmission, such as, deferring oral or nasal exams on standardized patients, and instead using task trainer-based practice for those types of exams.
Some medical schools also changed their curriculum to implement remote/virtual standardized patient (SP) encounter to simulate patient encounters as telemedicine or telehealth.5,6 Standardized patients were trained to interact with students remotely. This required these SP to have good internet access, have a good working knowledge of web-based platforms, and have a high comfort level using this form of technology. Students were required to obtain a history and verbalize the physical exam or instruct SPs to perform certain physical exam maneuvers, if possible. By using these remote encounters, student continued to develop their humanism skills, history-taking skills, and also allowed early exposure to telemedicine/telehealth. Other methods such as virtual reality case based simulation were also implemented by some (See article, Tyler, et al., “Innovations through Virtual Reality Simulation” in this issue). Although these methods were not ideal student and patient encounters, this did fill some of the gaps in the students’ skills development. They allowed students to continue to learn how to develop differential diagnosis and practice clinical and technical skills in preparation for their clinical years.
Adapting clinical skills training were not the only obstacles medical students faced during this rapid shift to remote learning during the pandemic. During the early adaptation to the remote curriculum, many students went back home (with family) whereas others stayed where they were to continue their education. For some, this created a comfortable and familiar environment to study, but for others it created some disadvantages. Learning from home created a distraction if there were other family members or children present due to lack of child care. Some had stressors such as feeling of isolation, stress over finances, unreliable internet access, or inadequate access to digital devices.7
As the pandemic continued, freshly accepted first-year medical students started their introduction into medicine and second-year students returned back to remote lectures. First-year students were interviewed virtually before acceptance to medical school. Orientation was also virtual with attempts to do virtual ice breakers and student bonding with help of faculty and staff. Due to the very restricted student interaction through remote learning and some possible limited onsite labs, students may have had the same feeling of isolation as earlier in the pandemic. For some students, this isolation translated into anxiety and depression.4,7 For others with preexisting mental health issues, this was an added stressor to already stressful environment of a pandemic and medical school. This caused decreased morale as they did not have the feeling of camaraderie that usually comes with being familiar with your classmates. To remedy this, some students formed remote groups and found ways to message each other to provide support. Some schools provided remote access to school psychologists and other mental health providers. In other instances, students individually sought out help via telemedicine mental health providers or remote cognitive behavior therapy.4
Clinical Students
Third- and fourth-year students in their clinical years were taken out of clinics and hospitals early during the pandemic to reduce risk of infection, decrease risk of transmission of the virus, and due to shortages of personal protective equipment (PPE).5 Some clinical faculty and other teaching clinicians were also required to focus on the influx of sick patients and devote more time to patient care in general during the pandemic, and therefore were unable to dedicate time for strictly educating medical students or other learners. This raised concerns from both students, medical school faculty and accrediting bodies. There were many worries that this group of students would not be able to develop and practice the skills they learned during their preclinical years.4 Due to this removal from the clinical setting, it appeared as though students may not have had sufficient exposure to clinical practice, and they now lacked face to face patient interaction.4,6 Initially, like their preclinical counterparts, these third- and fourth-year medical students were given a remote education. This entailed completing online modules, virtual reality simulations, review assigned cases in web-based case banks, following patients in remote electronic medical records (EMR) and attending remote lectures.6 The online modules and case banks helped students develop their differential diagnosis skills. Remote lectures were in the form of remote grand rounds, remote morning reports, or remotely listening to faculty discuss patient presentation.6 Students were also able to participate in the remote standardized patient encounter to simulate telemedicine/telehealth.
During the pandemic, telemedicine or telehealth became a necessity for most clinic-based practice. United States Department of Health and Human Services (HHS) delineates telehealth or telemedicine as healthcare delivered with the use of electronic information and telecommunications technologies for communication between patient and provider when face to face encounter cannot take place.6 This is broad definition for interaction with patient using various forms of this type of technology.6 For some patients, especially those without internet access or smart phone, this can be a phone call interaction with the clinician. For other patients this can mean using a web-based platform via computer, laptop, smart phone or other digital device (i.e. ipad, tablet, etc.) to do a video based telemedicine interaction with clinician.5,6 Some clerkship faculty helped bridge the clinical gap by allowing students to also participate in telemedicine to a limited extent.1, 5, 6
In some settings, telemedicine was a learning opportunity for both the clinical faculty and the student. Although this was a good alternative to a face to face visit, there are some cons including patient privacy concerns, limited physical exam, no way to obtain vital signs, and risks of poor outcome if the reason for the visit was an urgent or emergent issue.
As the pandemic became controlled in the United States, and PPE became more readily available, students in their clinical years have cautiously entered back into clinics and hospitals. With development and release of the vaccine to healthcare workers and adults, students have now started to see patients again and fully interact with clinicians. For preclinical students, medical schools are cautiously allowing students to return to campus and have established a new normal of mask wearing and taking other necessary precautions. The larger educational events such as lectures, grand rounds, and journal clubs continue to remain remote to mitigate exposure for events with larger attendance.
Conclusion
There were many things learned from the quick adaptation of medical schools to a remote/virtual curricula. Medical schools anticipate continuing some of these learning modifications in the curriculum after the pandemic. In the event of another critical wave of the COVID or other new respiratory transmitted virus, many of the recently adapted methods can be used to bridge the gap for clinical education if students are once again quarantined. Virtual reality case simulations may continue to supplement the development of clinical and technical skills with standardized patients. Telemedicine with standardized patients for preclinical students and telemedicine with clinical students may continue in clinical education. The long-term outcome of these change in medical education on student’s abilities to practice medicine and care for patients is currently unknown. Residency program directors will most likely be the first to observe these graduates clinical knowledge and skills as these medical students move on to residency and practice.
Footnotes
Mariam Akhtar, MD, is Assistant Professor, Primary Care-Joplin Campus, Kansas City University College of Osteopathic Medicine, Joplin, Missouri.
Disclosure
None reported.
References
- 1.Cairney-Hill J, Edwards AE, Jaafar N, Gunganah K, Macavei VM, Khanji MY. Challenges and opportunities for undergraduate clinical teaching during and beyond the COVID-19 pandemic. Journal of the Royal Society of Medicine. 2021;114(3):113–116. doi: 10.1177/0141076820980714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vollbrecht PJ, Porter-Stransky Kirsten A, Wendy L. Lackey-Cornelison Lessons learned while creating an effective emergency remote learning environment for students during the COVID-19 pandemic. Advances in Physiology Education. 2020;44(4):722–725. doi: 10.1152/advan.00140.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hilburg R, Patel Niralee, Ambruso Sophia, Biewald Mollie A, Farouk Samira S. Medical Education During the Coronavirus Disease-2019 Pandemic: Learning From a Distance. Advances in Chronic Kidney Disease. 2020;27(5):412–417. doi: 10.1053/j.ackd.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma D, Bhaskar S. Addressing the Covid-19 Burden on Medical Education and Training: The Role of Telemedicine and Tele-Education During and Beyond the Pandemic. Front Public Health. 2020;8:589669. doi: 10.3389/fpubh.2020.589669.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jumreornvong O, Yang E, Race J, Appel J. Telemedicine and Medical Education in the Age of COVID-19. Acad Med. 2020 Dec;95(12):1838–1843. doi: 10.1097/ACM.0000000000003711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Franklin G, Martin C, Ruszaj M, Matin M, Kataria A, Hu J, Brickman A, Elkin PL. How the COVID-19 Pandemic Impacted Medical Education during the Last Year of Medical School. A Class Survey. Life. 2021;11:294. doi: 10.3390/life11040294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stoller JK. A Perspective on the Educational “SWOT” of the Coronavirus Pandemic. Chest. 2021;159(2):743–748. doi: 10.1016/j.chest.2020.09.087. [DOI] [PMC free article] [PubMed] [Google Scholar]