Abstract
Background:
The slope of the tibial plateau has been proposed as a reason for failure of anterior cruciate ligament reconstruction.
Purpose:
To evaluate the interobserver reliability of measurements of tibial slope on radiographs versus magnetic resonance imaging (MRI) scans and to assess whether the modalities can be used interchangeably for this purpose.
Study Design:
Cohort study (diagnosis); Level of evidence, 3.
Methods:
This retrospective study included 81 patients aged 18 to 30 years who were evaluated in a sports medicine setting for knee pain and who had lateral knee radiographs as well as knee MRI scans on file. Medial and lateral tibial plateau slope measurements were made by 3 blinded reviewers from the radiographs and MRI scans using graphic overlay software. The paired t test was used to compare measurements of the medial tibial plateau slope (MTPS) and lateral tibial plateau slope (LTPS) from radiographs and MRI scans. Intraclass correlation coefficients (ICCs) were calculated to determine intra- and interobserver reliability of measurements within each imaging modality, and Pearson correlation coefficients were calculated to determine the relationship between measurements on radiographs versus MRI scans.
Results:
Imaging from 81 patients were included. The average MTPS was significantly larger on radiographs compared with MRI scans (8.7° ± 3.6° vs 3.7° ± 3.4°; P < .001), and the average LTPS was also significantly larger on radiographs compared with MRI scans (7.9° ± 3.4° vs 5.7° ± 3.7°; P < .001). ICC values indicated good to excellent intraobserver agreement for all imaging modalities (ICC, 0.81-0.97; P ≤ .009). The ICCs for interobserver reliability of MTPS and LTPS measurements were 0.92 and 0.85 for radiographs, 0.87 and 0.83 for MRI based off the subchondral bone, and 0.86 and 0.71 for MRI based off the cartilage, respectively (P < .001). Medium correlation was noted between radiographic and MRI measurements; Pearson correlation coefficients for radiographic versus subchondral MRI measurements were 0.30 and 0.37 for MTPS and LTPS, respectively.
Conclusion:
The average MTPS and LTPS were significantly larger on radiographs compared with MRI scans. Although tibial slope measurements using radiography and those using MRI are reliable between individuals, the measurements from radiographs and MRI scans cannot be used interchangeably, and caution should be used when interpreting and comparing studies using measurements of the tibial slope.
Keywords: medial tibial slope, lateral tibial slope, magnetic resonance imaging, radiography, reliability, correlation
Increasing evidence has demonstrated the link between posterior tibial slope (PTS) and the biomechanical function of the knee joint. 9,34,36 The tibial slope plays a role in the anteroposterior stability of the knee joint as well as the range of motion, especially in flexion. 10 Several studies have highlighted the importance of the tibial slope in preoperative planning in orthopaedics, mainly in total knee arthroplasty, high tibial osteotomy, tibial plateau fracture repair, and anterior cruciate ligament (ACL) reconstruction (ACLR). 8,10,13,19,21,30,35 Apart from being a newly recognized risk factor for ACL injury because of anteroposterior instability of the knee, 13 increased tibial slope and shallow medial tibial plateau have been shown to have a negative effect on the functional outcome after ACLR surgery. 30,36 Recent studies have indicated that an increased tibial slope may also be a factor associated with revision risk after ACLR, 5,15,22,23,29,37 reporting a slope ≥12° to be associated with a higher risk of revision. 22,29,31,37 Further, increased tibial slope on magnetic resonance imaging (MRI) scans has been correlated with accelerated knee cartilage degeneration in patients with knee pain but without severe osteoarthritic changes on radiographs. 13,34
A roentgenographic system to evaluate the tibial slope during preoperative planning was endorsed by the Knee Society in 1989. 9 The tibial slope is traditionally measured on the lateral knee radiograph by calculating the angle between a line along the articular surface of the tibia and a line perpendicular to the anterior tibial cortex or the tibial longitudinal axis, with normal measurements ranging between 5° and 15°. 4,10 During the last decade, efforts have been made to provide a more accurate estimate of the tibial slope using advanced imaging modalities, such as the 2-dimensional (2-D) or 3-dimensional (3-D) computed tomography (CT) and MRI examinations. 2,9,10 –13 With the recent advances in musculoskeletal imaging, limited data exist on the validity of the proposed methodologies to accurately measure the tibial slope in orthopaedic patients. 2,10,17,35 In addition, a consensus has yet to be reached on what is the optimal method to perform this measurement. 38
Based on current evidence, measurement of the tibial slope might be performed with greater reproducibility on the CT or MRI examination of the knee compared to radiographs. 4,14,18,33,36,38 Given the radiation exposure of CT scans, plain knee radiographs and MRI studies are the 2 most performed imaging tests in patients who present for evaluation of knee pain in a sports medicine setting. The suitability of these 2 imaging tests for the measurement of the tibial slope has been proven. 4,14,18,33,36,38 However, in discussing the role of slope, researchers will commonly discuss degree values interchangeably between studies using MRI versus radiography to measure slope. This leads to discrepancy in the literature as well as a potential misrepresentation of the so-called critical angle when the tibial slope increases failure rates too drastically and needs to be addressed. 14,36 More research is necessary to determine whether knee radiography and conventional MRI can be used interchangeably for evaluation of the tibial slope in clinical practice.
The purpose of this study was to report the reliability of lateral knee radiographs and 2-D MRI scans for the measurement of tibial slope in patients with knee pain who were evaluated in a sports medicine setting. We sought to investigate if a correlation existed between the tibial slope measurements on radiographs and MRI tests. We also investigated the difference between measuring slope on MRI scans based on the cartilage versus the subchondral bone. We hypothesized that there would be a good to excellent correlation between the measurements of the tibial slope on the lateral knee radiograph versus 2-D MRI scan in patients with knee pain.
Methods
Study Design
A retrospective review of patient charts and radiographic data was conducted after institutional review board approval. Patients aged 18 to 30 years who presented with a complaint of knee pain and who had both lateral radiographs and MRI scans of their knee were included. Patients were excluded if they had any history of fracture, infection, prior operative intervention to the knee, inadequate knee radiographs, or inadequate MRI scans. Adequate knee imaging was defined as the posterior aspects of the femoral condyles being superimposed or within 5 mm of distance, demonstration of the patellofemoral joint, and demonstration of the tibial femoral joint on the lateral radiograph (Figure 1). The quality of the MRI scans was determined based on sufficient tibial shaft length (>5 cm below the tubercle) to perform the required measurements. No dedicated MRI protocol was followed, and the images were obtained from multiple sources and using various strength magnets based on the imaging facility where the examination was performed, which had been elected by the participants.
Figure 1.

(A) Adequate lateral radiograph with superimposed posterior femoral condyles, with demonstration of the patellofemoral and tibiofemoral joints, compared to (B) “inadequate” lateral radiograph.
Tibial Slope Measurement
The medial tibial plateau slope (MTPS) and lateral tibial plateau slope (LTPS) were separately measured on the lateral radiographs and MRI scans of the knee by 3 blinded reviewers (2 senior orthopaedic residents [J.D.C, T.J.] and 1 orthopaedic fellow [R.J.]). Radiographic measurements were completed in a random order, followed by MRI measurements in a separate random order. These measurements were completed 4 weeks apart. Measurements of the LTPS and the MTPS were collected based on the method described by Hashemi et al. 13 Radiographs and MRI scans were viewed using imaging software (Synapse PACS v 4.4.2; Fujifilm), and a graphic overlay software (PixelStick v 2.10.1) was used for slope measurement.
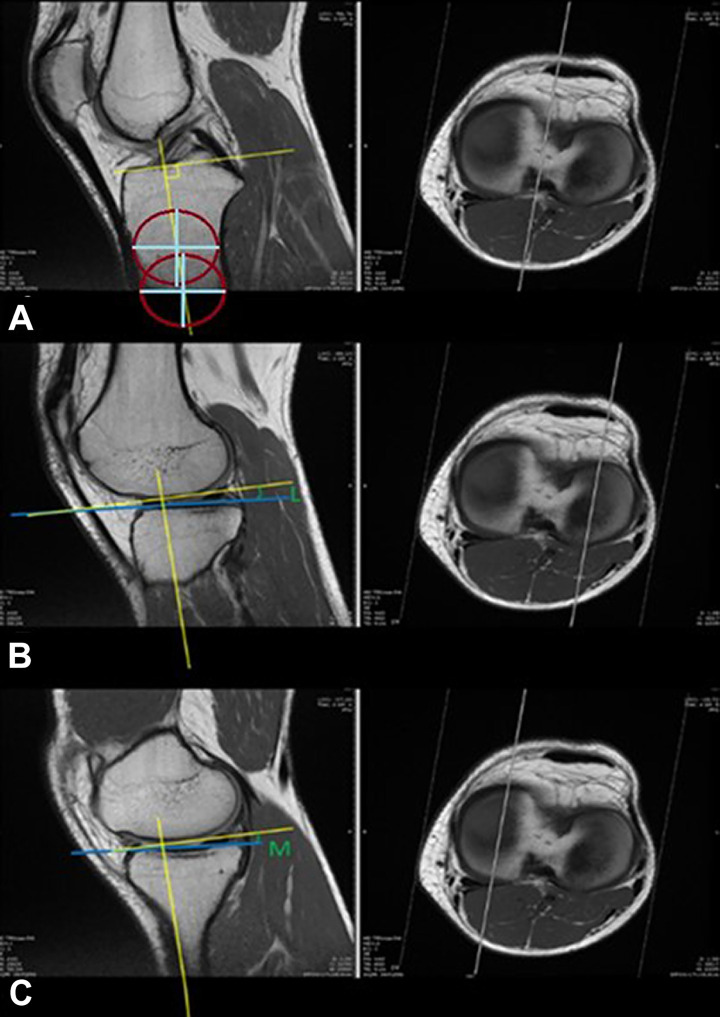
Radiographic measurements were taken from lateral view films. The center of the tibial shaft was marked at a point 1 cm below the tibial tubercle and a second point 5 cm distal; a connecting line was then used to define the tibial axis using graphic overlay software. The LTPS and MTPS were measured at the level of the bone based off the tibial axis (Figure 2). To obtain MRI measurements, the 2-D sagittal and axial images were viewed in linked panes using the proton density–weighted sequence. 28 The sagittal image was adjusted until its reference line on the axial images was in the center of the tibial plateau. On the sagittal image, the center of the tibial shaft was marked at a point 1 cm below the tibial tubercle and a second point 5 cm distal, and a connecting line was used to define the tibial axis. Once the axis was defined, the sagittal image was scrolled again until its reference line on the axial image was in the center of the lateral tibial plateau. The LTPS was then measured at the level of the subchondral bone. A second slope measurement was then taken, measuring off the articular cartilage. The process was then repeated for MTPS measurements (Figure 3).
Figure 2.
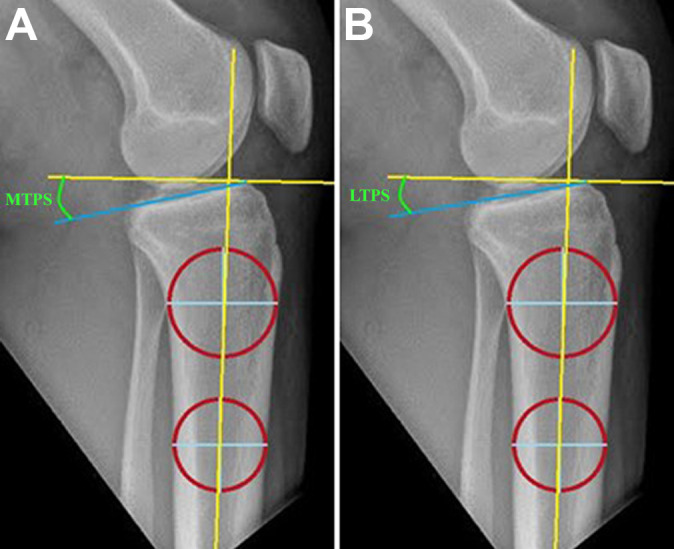
The center of the tibial shaft was marked at 2 points (center of red circles); a connecting line (vertical yellow line) was used to define the tibial axis. (A) The medial (blue line) and (B) lateral tibial plateau slopes (blue line) were measured at the level of the bone based off the tibial axis.
Figure 3.
(A) The center of the tibial plateau was found on the axial images, on the corresponding sagittal view the shaft was marked at 2 points (center of red circles), and a connecting line (vertical yellow line) was used to define the tibial axis. The linked sagittal (left) image was then scrolled until it was centered over the respective plateau on the axial (right) view. (B) The lateral and (C) medial tibial plateau slopes were measured on the sagittal view with a line drawn between 2 points based at the tip of the subchondral bone (as shown in B and C above) or cartilage (depending on the desired measurement). L, lateral; M, medial.
Statistical Analysis
All data were entered in a statistical program (SPSS, IBM Version 12.0). The intraclass correlation coefficient (ICC) was calculated for both intra- and interobserver reliability. The intraobserver reliability assessed the reproducibility of each observer for each measurement technique. The interobserver reliabilities assessed the overall agreement among the 3 observers for each measurement method. An ICC value <0.5 was considered poor agreement; 0.5 to 0.75, moderate; 0.76 to 0.90, good; and >0.90, excellent. 20 Statistical significance was determined using P < .05. The differences between values obtained using MRI and radiography were analyzed separately for the medial and lateral tibia plateaus using the paired t test. Paired t tests were also performed to determine if there was a statistical difference between the MRI measurements using subchondral bone and those using the cartilage surface as a reference for the slope. To examine correlations between slope values on radiographs versus MRI scans, the Pearson correlation coefficient (r) was computed. Pearson correlation scores were classified for level of correlation: perfect (r = ±1), strong (±0.5 ≤ r < ±1), medium (±0.3 ≤ r < ±0.5), or weak (r < ±0.29). 24
Results
Study Population
A total of 81 patients (44 women, 54%) with 90 knees (47 left, 52%) were included in the study. The mean age at the time of radiographs was 23.2 years (range, 18-30 years), and the mean age at time of MRI was 23.5 years (range, 18-30 years). Eight patients, with 10 knee images, were excluded from this study because of poor-quality images.
Slope Measurements
The average MTPS measured on radiographs was significantly larger compared to subchondral bone and cartilage MRI measurements (8.7° vs 3.7° and 4.4°, respectively; P < .001). Similarly, the average LTPS measured on radiographs was significantly larger compared to subchondral bone and cartilage MRI measurements (7.9° vs 5.7° and 6.2°, respectively; P < .001). When comparing MRI measurements using subchondral bone to those using the cartilage, a larger average slope was seen when cartilage was used as the reference (4.4° vs 3.7° for MTPS and 6.2° vs 5.7° for LTPS; P < .001) (Table 1).
Table 1.
Average Slope Measurement (in degrees) for Each Imaging Modality a
| MTPS | LTPS | |||
|---|---|---|---|---|
| Mean | P Value | Mean | P Value | |
| Radiograph | 8.7 ± 3.6 | <.001 | 7.9 ± 3.4 | <.001 |
| MRI (subchondral bone) | 3.7 ± 3.3 | <.001 | 5.7 ± 3.7 | <.001 |
| MRI (cartilage) | 4.4 ± 3.6 | <.001 | 6.2 ± 3.7 | <.001 |
a Data are reported as mean ± SD. LTPS, lateral tibial plateau slope; MRI, magnetic resonance imaging; MTPS, medial tibial plateau slope.
The ICC values indicated good to excellent intraobserver agreement for all imaging modalities (ICCs, 0.81-0.97; P ≤ .009) (Table 2). Interobserver agreement was also good to excellent based on ICC values for all imaging modalities, except for LTPS measurements using cartilage as a reference, which had only moderate reliability (0.71; P < .001). The ICCs for interobserver reliability of the MTPS measurements were significantly higher than those of the LTPS measurements on each imaging modality: 0.92 vs 0.85 for radiographs, 0.87 vs 0.83 for MRI subchondral bone, and 0.86 vs 0.71 for MRI cartilage (P < .001 for all) (Table 3).
Table 2.
Intraobserver Reliability for the Measurement of the Tibial Slope on Lateral Radiograph and MRI Scan a
| MTPS | LTPS | |||||
|---|---|---|---|---|---|---|
| ICC | 95% CI | P Value | ICC | 95% CI | P Value | |
| Radiograph | 0.96 | 0.84-0.98 | <.001 | 0.97 | 0.88-0.99 | <.001 |
| MRI (subchondral bone) | 0.89 | 0.58-0.97 | .002 | 0.81 | 0.30-0.95 | .009 |
| MRI (cartilage) | 0.84 | 0.41-0.96 | .005 | 0.93 | 0.02-0.96 | .001 |
a ICC, intraclass correlation coefficient; LTPS, lateral tibial plateau slope; MRI, magnetic resonance imaging; MTPS, medial tibial plateau slope.
Table 3.
Interobserver Reliability for the Measurement of the Tibial Slope on Lateral Radiograph and MRI Scan a
| MTPS | LTPS | |||||
|---|---|---|---|---|---|---|
| ICC | 95% CI | P Value | ICC | 95% CI | P Value | |
| Radiograph | 0.92 | 0.89-0.95 | <.001 | 0.85 | 0.78-0.89 | <.001 |
| MRI (subchondral bone) | 0.87 | 0.82-0.91 | <.001 | 0.83 | 0.76-0.88 | <.001 |
| MRI (cartilage) | 0.86 | 0.83-0.92 | <.001 | 0.71 | 0.68-0.74 | <.001 |
a ICC, intraclass correlation coefficient; LTPS, lateral tibial plateau slope; MRI, magnetic resonance imaging; MTPS, medial tibial plateau slope.
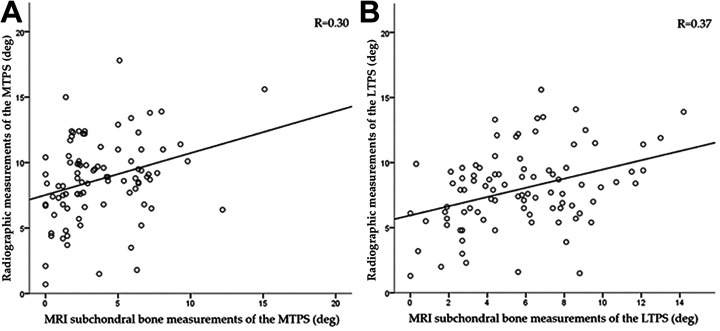
Low to negligible correlation was noted between radiographic and MRI subchondral bone measurements for both the MTPS and LTPS measurements. The Pearson correlation coefficient (r) was 0.30 and 0.37 for radiographic versus MRI subchondral bone measurements of the MTPS and LTPS, respectively (Figure 4).
Figure 4.
Medium correlation was noted between mean radiographic measurement and mean subchondral bone MRI measurement of (A) the MTPS (r = 0.30) and (B) LTPS (r = 0.37). LTPS, lateral tibial plateau slope; MTPS, medial tibial plateau slope.
Discussion
In our study, we chose to evaluate measurements of the MTPS and LTPS using MRI scans and radiographs that were available from patients presenting to a sports medicine clinic with a chief complaint of knee pain. These are the most common imaging modalities patients will already have when presenting to a sports medicine office with concern for ligamentous or meniscal injury. The most significant finding of this paper was that the lateral knee radiograph and conventional MRI scan cannot be used interchangeably for the measurement of the tibial slope when evaluating patients with knee pain. The MTPS and LTPS measurements were larger by a mean of 5.0° and 2.2° on radiographs than on MRI scans measured off the subchondral bone. Measurement of the MTPS and LTPS showed good to excellent interrater and intrarater reliability on both the radiographs and subchondral bone MRI studies, suggesting that either imaging modality can be used to reproduce reliable measurements from a single study.
The true tibial slope reflects the slope of the articular cartilage rather than the slope of the subchondral bone. The difference between MRI subchondral bone measurements and MRI cartilage measurements was statistically significant; however, with a mean difference of 0.7° and 0.5° for medial and lateral slopes, respectively, they may not be clinically significant. Furthermore, given the lower ICC scores for interobserver reliability, we recommend using MRI subchondral measurements if one wishes to measure off MRI scans. Despite this, we cannot determine which imaging modality reflects the true medial or lateral slopes of the tibia.
Our findings are comparable to the results of previous articles showing smaller tibial slope measurements on MRI scans compared to radiographs. 4,14,36 Hudek et al 14 found that the mean PTS was 3.4° smaller on MRI scans compared with lateral knee radiographs (4.8° ± 2.4° vs 8.2° ± 2.8°, respectively). The mean MTPS values on radiographs and MRI scans were similar between our study and the study by Hudek et al: 8.7° versus 8.2° on radiographs and 4.4° versus 4.8° on MRI scans (cartilage measurement), respectively. In addition, Hudek et al reported better reproducibility of the MTPS measurement on radiographs compared with the MRI scans (ICC was 0.89 for lateral knee radiographs and 0.77 for MRI scans), which was in agreement with our results (ICC for MTPS was 0.92 on radiographs, 0.87 on MRI scans using subchondral bone measurements, and 0.86 on MRI scans using cartilage measurements). Regarding the measurement of the LTPS, our results showed significantly larger measurements on radiographs (mean LTPS, 7.9°) compared to those reported by Hudek et al (mean LTPS, 5°). However, in contrast to our study, which used readily available MRI scans with no special formatting, Hudek et al used sagittal MRI slices that were set manually by the radiologist orthogonal to a line connecting the posterior femoral condyles.
Our findings contrast with a similar investigation on 14 cadaveric knees that compared the medial and lateral tibial slopes on short as well as long knee radiographs with the measurements on CT and MRI scans. 36 In that study, the medial and lateral tibial slope values did not differ between imaging modalities. Potential reasons for the differing results across studies include the following: (1) there were differences in the methodology used to perform the LTPS and MTPS measurements; (2) cadaveric samples were used, which allows for precisely control of tibial rotation on all imaging modalities; and (3) they controlled the exact plane for sagittal MRI and CT slices. Various models for PTS measurement on conventional lateral radiographs have been described. 7,12,16,18,27,36 Because of different longitudinal axis definitions, the reported mean PTS ranges from 4° to 14°. 12,26
Minor rotational changes of the tibia on lateral radiographs have been shown to influence measured tibial slopes 10,18,36 with a mean slope increase of 3° at 40° of tibial rotation. 36 Quality lateral knee radiographs are largely based off overlap of the posterior femoral condyles, which can give a reliable lateral projection of the femur; however, this may not represent a true lateral view of the tibial plateau, as this can be affected by varying degrees of knee flexion. The tibia is subject to internal rotation with knee flexion and external rotation with knee extension. 11 Chen et al 3 demonstrated approximately 11.4° of internal rotation at 40° of knee flexion. The available length of exposed tibia on lateral knee radiographs influences measured tibial slopes. Faschingbauer et al 10 found that with short lateral knee radiographs (<10 cm of exposed tibia), the slopes will be approximately 3° too high and recommended expanded lateral radiographs (20 cm of exposed tibia) to allow closer approximation of the true slope.
MRI measurements can be affected by the plane of the sagittal MRI slices. An ideal sagittal MRI slice would be orthogonal to a line connecting the posterior femoral condyles. 14 An ideal sagittal reference line is shown on the axial image in Figure 5A. MRI quality was highly variable in our study, as many patients presented with studies performed at outside facilities with varying sequencing protocols, magnet strength, and sagittal planes of imaging seen in Figure 5B. It is our belief that alterations in the plane for the sagittal slices will have effects on slope measurements similar to those seen with rotational changes on radiographs.
Figure 5.
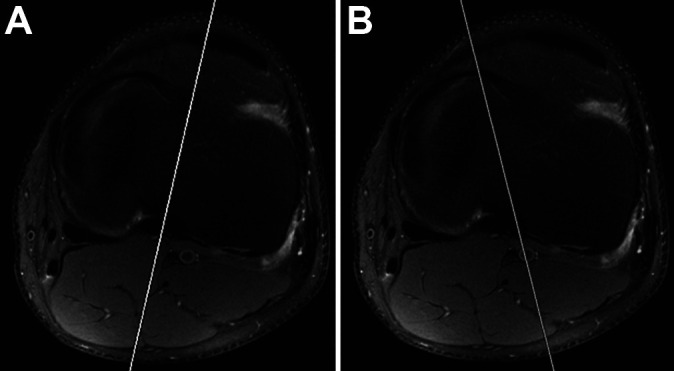
Axial magnetic resonance imaging (MRI) scan showing (A) an ideal plane (line) for sagittal MRI slices as it bisects the plateau versus (B) a nonideal plane (line) traversing the plateau at an oblique angle.
Attention must be paid during the interpretation of the tibial slope measurements using different imaging modalities in clinical practice, and larger values should be expected when measuring the MTPS on radiographs compared to MRI scans. Clinicians must always consider potential differences in the radiographic views or MRI cuts utilized to measure the tibial slope when interpreting the results of the existing studies, along with the methodology used to perform these measurements. We did not examine the correlation between the MTPS/LTPS measurements using radiographic or MRI scans with those performed on CT scans, which constitutes a limitation of this study. Given that some of the previous studies have shown good correlation between the measurements of the tibial slope on radiographs and CT scans, 33,36 more research is necessary to determine whether advanced imaging studies (such as CT or MRI) are necessary for the measurement of tibial slope. As stated previously, there is little consensus on which of the 3 imaging tests (radiograph, CT, or MRI) should be used as the gold standard examination for the measurement of the tibial slop during preoperative planning. The last should be the primary focus of future investigations on this topic.
Previous studies have used different imaging modalities to measure the PTS in patients who are candidates for deflexion osteotomy (PTS > 12° or 13°). 1,6,32 Song et al 32 reported the outcomes of patients who underwent ACLR combined with slope-reducing tibial osteotomy in patients with steep PTS (>13°), excessive anterior tibial subluxation in extension (>10 mm), and concomitant chronic meniscus posterior horn tears (>6 months). In this last study, the PTS was measured on a true lateral radiographic view of the knee under fluoroscopic control in order to ensure that the femoral condyles were superimposed. The true lateral view of the knee under fluoroscopic control was also used for the measurement of PTS in the study by Dejour et al, 6 who reported the outcomes of revision ACLR in combination with tibial deflexion osteotomy in patients who had a tibial slope of >12°. Lastly, Akoto et al 1 utilized lateral knee radiographs to measure the PTS in patients who underwent slope correction osteotomy with lateral extra-articular tenodesis and revision ACL, in a study where elevated posterior tibial slope was defined as ≥12°. 25
This study had several limitations. This was a retrospective analysis including patients with knee pain who had knee radiographs and MRI examination on file. Although our investigation aimed to be clinically useful in patients who are surgical candidates for ACLR, we did not specifically focus on this population. Another limitation, as mentioned previously, was that the axis of the sagittal MRI cuts was not standardized. This caused the slopes to be measured off varying degrees of an oblique axis. Although the intra- and interobserver reliabilities were high, human error could have influenced the angle measurements, especially when small changes to the defined tibial axis could induce large changes of the slope measurements.
As mentioned previously, our results are based off radiographs and MRI scans that were readily available from our clinic's patients. The limitation from this is that imaging was not formatted specifically to address tibial slope. Rather, our study better replicates a real-world scenario, where practitioners are commonly faced with outside and poorly formatted imaging. We have established the reproducibility of slope measurements based off either MRI scans or radiographic imaging. Unfortunately, this has not established which method is better or more accurate at measuring the tibial slope. In fact, one could question whether either method, in the clinical setting, can be used to accurately address tibial slope. Finally, measurements from CT scans were not included in this study, as most of the patients presenting with knee pain had only radiographs and MRI scans available. Full-length tibia studies for radiographs, MRI scans, or CT scans were not available, as this would require significant time, cost, and radiation exposure. The last is necessary to determine which of the 3 imaging tests (MRI, CT, or radiograph) must be established as the gold standard examination for the evaluation of the tibial slope in clinical practice.
Conclusion
The slope of the medial and lateral tibial plateau can be reliably reproduced between individuals using radiographs or MRI scans. However, tibial slope measurements from radiographs and MRI scans cannot be used interchangeably, and caution should be used when interpreting and comparing studies using measurements of the tibial slope.
Acknowledgment
The authors acknowledge the Cappo Family Research Fund.
Footnotes
Final revision submitted April 14, 2021; accepted May 4, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: H.P.K. has received education payments from Arthrex and hospitality payments from Stryker. S.C.G. has received education payments from Arthrex; hospitality payments from Micromed; and consulting fees from Arthrex, Exactech, and Zimmer. G.F.H. has received education payments from Arthrex and Micromed, consulting and speaking fees from Arthrex, and honoraria from Fidia Pharma. A.E.B. has received education payments from Arthrex and Smith & Nephew, speaking fees from Arthrex, and hospitality payments from Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Southern California Health Sciences Campus Institutional Review Board (protocol #HS-18-00465).
References
- 1. Akoto R, Alm L, Drenck TC, et al. Slope-correction osteotomy with lateral extra-articular tenodesis and revision anterior cruciate ligament reconstruction is highly effective in treating high-grade anterior knee laxity. Am J Sports Med. 2020;48(14):3478–3485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Amerinatanzi A, Summers RK, Ahmadi K, et al. Automated measurement of patient-specific tibial slopes from MRI. Bioengineering. 2017;4(3):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen HN, Yang K, Dong QR, Wang Y. Assessment of tibial rotation and meniscal movement using kinematic magnetic resonance imaging. J Orthop Surg Res. 2014;9:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Choi CH, Kim JH, Chung HK, Choi YH. Measurement of posterior slope angle of the proximal tibia by MRI and X-ray. Korean Orthop Assoc. 2001;36(6):569–573. [Google Scholar]
- 5. Christensen JJ, Krych AJ, Engasser WM, et al. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(10):2510–2514. [DOI] [PubMed] [Google Scholar]
- 6. Dejour D, Saffarini M, Demey G, Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2846–2852. [DOI] [PubMed] [Google Scholar]
- 7. Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture: two radiological tests compared. J Bone Joint Surg Br. 1994;76(5):745–749. [PubMed] [Google Scholar]
- 8. El-Azab H, Glabgly P, Paul J, Imhoff AB, Hinterwimmer S. Patellar height and posterior tibial slope after open- and closed-wedge high tibial osteotomy: a radiological study on 100 patients. Am J Sports Med. 2010;38(2):323–329. [DOI] [PubMed] [Google Scholar]
- 9. Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 10. Faschingbauer M, Sgroi M, Juchems M, Reichel H, Kappe T. Can the tibial slope be measured on lateral knee radiographs? Knee Surg Sports Traumatol Arthrosc. 2014;22(12):3163–3167. [DOI] [PubMed] [Google Scholar]
- 11. Freeman MA, Pinskerova V. The movement of the normal tibio-femoral joint. J Biomech. 2005;38(2):197–208. [DOI] [PubMed] [Google Scholar]
- 12. Genin P, Weill G, Julliard R. The tibial slope: proposal for a measurement method. Article in French. J Radiol. 1993;74(1):27–33. [PubMed] [Google Scholar]
- 13. Hashemi J, Chandrashekar N, Mansouri H, et al. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1):54–62. [DOI] [PubMed] [Google Scholar]
- 14. Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467(8):2066–2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jaecker V, Drouven S, Naendrup JH, et al. Increased medial and lateral tibial posterior slopes are independent risk factors for graft failure following ACL reconstruction. Arch Orthop Trauma Surg. 2018;138(10):1423–1431. [DOI] [PubMed] [Google Scholar]
- 16. Julliard R, Genin P, Weil G, Palmkrantz P. The median functional slope of the tibia. Principle. Technique of measurement. Value. Interest. Article in French. Rev Chir Orthop Reparatrice Appar Mot. 1993;79(8):625–634. [PubMed] [Google Scholar]
- 17. Kacmaz IE, Topkaya Y, Basa CD, et al. Posterior tibial slope of the knee measured on X-rays in a Turkish population. Surg Radiol Anat. 2020;42(6):673–679. [DOI] [PubMed] [Google Scholar]
- 18. Kessler MA, Burkart A, Martinek V, Beer A, Imhoff AB. Development of a 3-dimensional method to determine the tibial slope with multislice-CT. Article in German. Z Orthop Ihre Grenzgeb. 2003;141(2):143–147. [DOI] [PubMed] [Google Scholar]
- 19. Kiapour AM, Yang DS, Badger GJ, et al. Anatomic features of the tibial plateau predict outcomes of ACL reconstruction within 7 years after surgery. Am J Sports Med. 2019;47(2):303–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Koval KJ, Helfet DL. Tibial plateau fractures: evaluation and treatment. J Am Acad Orthop Surg. 1995;3(2):86–94. [DOI] [PubMed] [Google Scholar]
- 22. Lee CC, Youm YS, Cho SD, et al. Does posterior tibial slope affect graft rupture following anterior cruciate ligament reconstruction? Arthroscopy. 2018;34(7):2152–2155. [DOI] [PubMed] [Google Scholar]
- 23. Li Y, Hong L, Feng H, et al. Are failures of anterior cruciate ligament reconstruction associated with steep posterior tibial slopes? A case control study. Chin Med J (Engl). 2014;127(14):2649–2653. [PubMed] [Google Scholar]
- 24. Mukaka MM. Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24(3):69–71. [PMC free article] [PubMed] [Google Scholar]
- 25. Nerhus TK, Ekeland A, Solberg G, et al. Radiological outcomes in a randomized trial comparing opening wedge and closing wedge techniques of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):910–917. [DOI] [PubMed] [Google Scholar]
- 26. Noyes FR, Goebel SX, West J. Opening wedge tibial osteotomy: the 3-triangle method to correct axial alignment and tibial slope. Am J Sports Med. 2005;33(3):378–387. [DOI] [PubMed] [Google Scholar]
- 27. Paley D, Maar DC, Herzenberg JE. New concepts in high tibial osteotomy for medial compartment osteoarthritis. Orthop Clin North Am. 1994;25(3):483–498. [PubMed] [Google Scholar]
- 28. Rodrigues MB, Camanho GL. MRI evaluation of knee cartilage. Rev Bras Ortop. 2010;45(4):340–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Salmon LJ, Heath E, Akrawi H, et al. 20-year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: the catastrophic effect of age and posterior tibial slope. Am J Sports Med. 2018;46(3):531–543. [DOI] [PubMed] [Google Scholar]
- 30. Sauer S, Clatworthy M. The effect of medial tibial slope on anterior tibial translation and short-term ACL reconstruction outcome. Surg J (N Y). 2018;4(3):e160–e163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Schillhammer C. Editorial commentary: managing excessive posterior slope in anterior cruciate ligament reconstruction. Where do we draw the line? Arthroscopy. 2018;34(7):2156–2157. [DOI] [PubMed] [Google Scholar]
- 32. Song G-y, Ni Q-k, Zheng T, et al. Slope-reducing tibial osteotomy combined with primary anterior cruciate ligament reconstruction produces improved knee stability in patients with steep posterior tibial slope, excessive anterior tibial subluxation in extension, and chronic meniscal posterior horn tears. Am J Sports Med. 2020;48(14):3486–3494. [DOI] [PubMed] [Google Scholar]
- 33. Sorin G, Pasquier G, Drumez E, et al. Reproducibility of digital measurements of lower-limb deformity on plain radiographs and agreement with CT measurements. Orthop Traumatol Surg Res. 2016;102(4):423–428. [DOI] [PubMed] [Google Scholar]
- 34. Takahashi K, Hashimoto S, Kiuchi S, et al. Bone morphological factors influencing cartilage degeneration in the knee. Mod Rheumatol. 2018;28(2):351–357. [DOI] [PubMed] [Google Scholar]
- 35. Tomite T, Saito H, Kijima H, et al. The usefulness of planning using a preoperative lateral leg image to determine accurate posterior tibial slope in total knee arthroplasty. J Orthop. 2019;16(1):25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Utzschneider S, Goettinger M, Weber P, et al. Development and validation of a new method for the radiologic measurement of the tibial slope. Knee Surg Sports Traumatol Arthrosc. 2011;19(10):1643–1648. [DOI] [PubMed] [Google Scholar]
- 37. Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med. 2013;41(12):2800–2804. [DOI] [PubMed] [Google Scholar]
- 38. Zhang Y, Chen Y, Qiang M, et al. Comparison between three-dimensional CT and conventional radiography in proximal tibia morphology. Medicine (Baltimore). 2018;97(30):e11632. [DOI] [PMC free article] [PubMed] [Google Scholar]